Abstract
Objective:
To provide national estimates of Donor Insemination (DI) use in the United States and a description of the population of users.
Design:
Population estimates were generated from nationally-representative data through weighted proportions and count estimates.
Setting:
Surveys were conducted on samples selected in 1995, 2002, and continuously in the years 2006–2010, 2011–2013, 2013–2015, and 2015–2017 in the United States.
Patients:
Participants were U.S. women of childbearing age (15–44) sampled for interview in the National Survey of Family Growth.
Interventions:
No interventions were conducted in this descriptive study.
Main Outcome Measures:
Respondents who reported having received artificial insemination were asked the origin of the sperm; responses could include husband/partner, donor only, or mixed donor and husband/partner.
Results:
In 1995, an estimated 170,701 [95% CI: 106,577 – 234,825] women had undergone DI using donor or mixed sperm. In 2015–2017, 440,986 [95% CI: 108,458 – 773,513] were estimated to have used it. DI users were mostly White, urban, older, college-educated, and had high family incomes.
Conclusions:
DI use changed over time, from a drop between 1995 and 2013 to a precipitous growth in 2015–2017. In recent years, nearly half a million women may be dealing with personal, relationship, and familial issues born of DI use. The U.S. does not maintain records on the usage of donor sperm, but better tracking of the use and outcomes of treatment would provide better estimates of the size of the population affected.
Keywords: NSFG, infertility, donor sperm
Capsule:
In recent years, nearly half a million U.S. women have used donor insemination, up from earlier decades. New estimates of the population will aid practitioners, clinicians, and researchers in this area.
Donor conception involves the use of sperm, eggs, both, or even whole embryos, sourced from a person or persons other than the intended parents of the resulting child. Families formed through donated gametes or embryos represent a unique population with special considerations including health, social, and emotional outcomes of individuals who were donor conceived (DC), recipient parents (1, 2), and perhaps the donors themselves (3). Highlighting the multiple levels involved in these issues, scholars in this area have focused on topics ranging from the individual to the dyadic to the familial. For example, research has tracked the pregnancy and birth outcomes of children conceived through various methods (4). Scholars have examined outcomes in families and individuals from parents sharing information regarding the child’s unique conception with the child (1, 5, 6). Within families, research suggests a link between DC offspring’s attachment to parents and curiosity about their donor conception (25). Despite the attention towards family and individual outcomes involved in donated reproduction, we are missing a fundamental piece of the puzzle: the U.S. has no recent estimates of the size of the population using or born of donated gametes, limiting our understanding of the scope of the population affected.
Sperm donation, specifically as used in artificial insemination (usually referred to as Donor Insemination, or DI), is the oldest form of reproductive donation and donor conception, with the first recorded instance in the U.S. performed in the 1880s (7). From the beginning, the practice has been shrouded in secrecy (7), limiting the ability of population scientists to enumerate the sperm-donor conceived community and their families (8). For more than a quarter century, “30,000 to 60,000 annual births” from donated sperm has been the figure used in the literature, but this estimate is suspect when applied to present circumstances (8). An estimate of thirty-thousand births from DI was put forth in 1986–1987 by the Office of Technology Assessment (9). This was similar to estimates of DI births obtained by a private survey in 1987 (10), which estimated between 11,400 and 23,400 DI births had occurred; this seemed to be a large (possibly two-fold) increase from previous estimates of DI use a decade before (10). Without updated numbers in the past 20 years, it is hard to understand how DI use may have changed in the ensuing decades, or to estimate how many families are currently involved. A direct and recent number may be hard to come by due to the lack of mandated record keeping regarding donated gametes in the United States (2, 8). However, we may be able to track the number of women reporting having used DI in national surveys of fertility to make an educated estimate from which to start.
Infertility treatments that involve the handling of oocytes or embryos outside the body (including In-Vitro Fertilization [IVF], among others) make up the group of techniques referred to as Assisted Reproductive Technologies, or ART (11). The use and success of these technologies has been tracked due to a congressional mandate in 1992. This surveillance shows that use of donor sperm within ART has generally increased over time (4). These estimates do not account for DI, however, as DI is a relatively non-invasive procedure that does not fall into the ART definition, as it only requires the handling of sperm.
The purpose of the present study was to provide a population estimate and description of women who have received donated sperm during treatment with artificial insemination using a population-representative study of United States women of childbearing age (15–44 years old), the National Survey of Family Growth (NSFG). A national estimate and description of the women who have utilized donated sperm provide an updated picture of the scope of DI usage, hint at the potential size of the DC population, and inform future work on the development and wellbeing of DC individuals and their families.
Method
Data were drawn from multiple cross-sectional samples of the NSFG: Cycle V (1995), 2002, 2006–2010, 2011–2013, 2013–2015, and 2015–17. The use of this publicly available data was deemed exempt from further Internal Review Board (IRB) review under University of North Carolina at Chapel Hill IRB Number 18–2677. The NSFG is a multi-stage probability-based nationally-representative survey of women ages 15–44 (15–49 in 2015–2017 sample) in the United States. Black, Hispanic, and adolescent respondents were oversampled. Thus, all estimates were adjusted given the complex sampling design and weighted with provided survey weights (12) meant to provide accurate estimates of the population of U.S. women of childbearing age in each survey. In the multi-year continuous surveys, the weighted populations represent the mid-point of the survey years. All respondents in the 1995 to 2013–2015 cohorts were used in the analyses; in 2015–2017, respondents over age 45 at the time of interview were removed (n = 547) for comparability with prior waves. Total unweighted N = 47,076. Estimates of each cross-sectional sample alone (Figure 1 and Table 1) were conducted using the appropriate sample-specific weights.
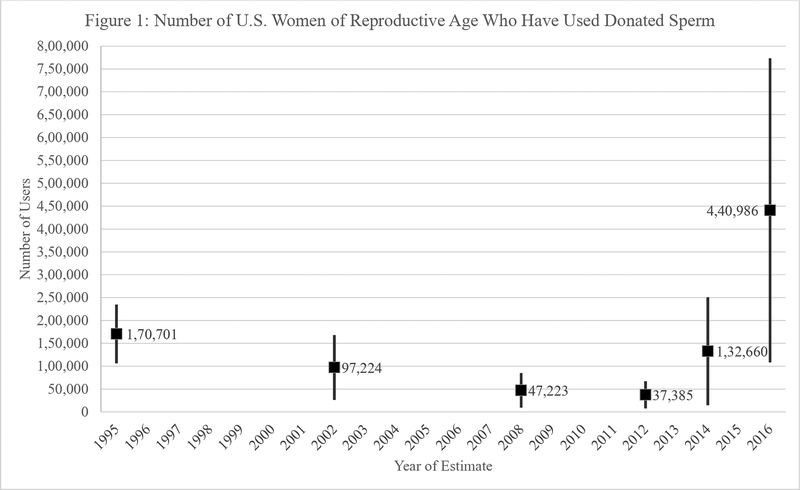
Figure 1:
Estimated Number of Women Reporting having used Donated Sperm or Mixed Husband/Partner with Donor. Weighted Estimates and 95% Confidence Intervals for each Cross-Sectional Sample.
Table 1:
Use of Donated Sperm by U.S. Women of Reproductive Age
| Year(s) | Low Estimate | 95% CI |
|---|---|---|
| 1995 | 170,701 | [ 106,577 – 234,825 ] |
| 2002 | 97,224 | [ 26,404 – 168,044 ] |
| 2006–2010 | 47,223 | [ 9,377 – 85,068 ] |
| 2011–2013 | 37,385 | [ 7,735 – 67,034 ] |
| 2013–2015 | 132,660 | [ 14,590 – 250,731 ] |
| 2015–2017 | 440,986 | [ 108,458 – 773,513 ] |
To better understand the population who reported donated sperm use and generate a larger sample, we combined the files from 2011–2013, 2013–2015, and 2015–2017 using the NSFG-provided 6-year combined weight; the estimates presented in Table 2 use this weight. These estimates apply to the mid-point of the years, July 2014.
Table 2:
Descriptive Statistics of Low-estimate Sperm-using Sample (“Used Donor Sperm” and “Mixed” Responses). Sperm Users in 2011–2017, unweighted n = 36 and weighted n = 200,197 [95% CI: 89,176 – 311,219].
| Estimate (%) | 95% CI | |
|---|---|---|
| Race/Ethnicity | ||
| Hispanic | 9 | [ 2 – 27 ] |
| Non–Hispanic White | 67 | [ 38 – 87 ] |
| Non–Hispanic Black | 19 | [ 4 – 55 ] |
| Non–Hispanic Other or Multiple Race | 5 | [ 2 – 14 ] |
| Urbanicity at Interview | ||
| Principle City of MSA (urban) | 51 | [ 25 – 76 ] |
| Other MSA or Not MSA (less urban or rural) | 49 | [ 24 – 75 ] |
| Parity at Interview | ||
| No Births | 42 | [ 19 – 70 ] |
| 1 Birth | 13 | [ 5 – 28 ] |
| 2+ Births | 45 | [ 21 – 71 ] |
| Marital History at Interview | ||
| Never Married | 46 | [ 23 – 71 ] |
| Ever Married | 54 | [ 29 – 77 ] |
| Age at Interview | ||
| <35 | 20 | [ 7 – 43 ] |
| 35–39 | 46 | [ 22 – 72 ] |
| 40–44 | 34 | [ 15 – 62 ] |
| Education at Interview | ||
| High School to 2-year Degree | 24 | [ 11 – 43 ] |
| 4-year Degree or More | 76 | [ 57 – 89 ] |
| Household % of Poverty Line, Year Before Interview | ||
| < 200% | 16 | [ 6 – 36 ] |
| 200–399% | 13 | [ 5 – 28 ] |
| 400% + | 71 | [ 49 – 86 ] |
| Sexual Orientation | ||
| Straight | 57 | [ 32 – 80 ] |
| Sexual Minority | 43 | [ 20 – 68 ] |
Measures
Use of Donated Sperm.
The unweighted counts of respondents flowing from the total samples to the use of donated sperm is detailed in Supplemental Table 3. Respondents who had reported having sex with a man at least once or who were at least 18 years of age were asked if they (or any husband or partner) had “ever been to a doctor or other medical care provider to talk about ways to help you become pregnant.” If they indicated yes, they were asked what services they had received and could select artificial insemination. If they did, they were asked the origin of the sperm as, “Were you inseminated with sperm from your husband or partner only, from some other donor only, or from both?” Respondents could also indicate they did not know the origin of the sperm or refuse to answer. Respondents were not asked to differentiate between sources of donor sperm (anonymous, known, relative, etc.) or if sperm was fresh or frozen. Weighted estimates are presented below; absolute cell values are available in supplemental Table 2. In total across the samples, 81 women indicated using donated sperm. Of these, 36 were from the samples represented in Table 2 under the combined 6-year weight (2011–2017).
Exploratory Variables.
To generate the profile of users presented in Table 2, we used the recoded variables provided by the NSFG, which account for inconsistences in reports and missing data (see Supplemental Table 1). Race/Ethnicity was measured as Hispanic, Non-Hispanic White Single Race, Non-Hispanic Black Single Race, and Non-Hispanic Other or Multiple Race according to respondent self-report and classified according to the 1997 Office of Management and Budget guidelines, listing respondents who reported multiple races separately from those reporting one. Respondent’s local population size, as a proxy measure for rurality versus urbanicity, was recorded as living in a principal city of Metropolitan Statistical Area (MSA – considered most urban) versus other MSA or non-MSA (less urban to rural). Parity was an overall count of live births reported by the respondent by the time of interview, and coded as 0, 1, and 2 or more (respondents did not specify the children’s conception method, however). Respondent’s formal marital status was recorded as current or formerly married versus never married. Marriage in this variable refers only to legal marriages to different-sex partners at the time of the interview, but it should be noted that retrospective reports of sperm use, as described above, were not dependent on previous or present marital status. Respondent’s age at interview was classified as under age 35, 35 to 39, and 40 to 44 years of age at time of interview. Respondents reported their educational attainment (classified as up to 2-year college degree and 4-year degree or more; no users of donor sperm reported less than high school) at the time of interview. The respondents’ family income in the year prior to the interview was compared to the national poverty guidelines of that year and categorized as < 200% of poverty line, 200–399%, or 400% and more. Finally, respondents reported their sexual orientation at the time of interview. In the 2011–2013 and 2013–2015 cohorts, all respondents received the same form of the question; in the 2015–2017 cohort, the sample was randomly divided in half, with one half receiving the same question as the previous cohorts and the other receiving a slightly different wording (both questions are shown in Supplementary Table 1). For compatibility, responses in all waves were coded as sexual minority (any gay, lesbian, or bisexual answer) versus straight.
Results
Figure 1 and Table 1 show the estimated number of users of donated sperm in each cross sectional sample with 95% confidence intervals. In 1995, an estimated 170,701 [CI: 106,577–234,825] women had used donated sperm, 0.28% of reproductive-aged U.S. women (not shown). The population dropped to a low of about 37,385 [CI: 7,735–67,034] in the 2011–2013 cohort. The population then grew to an estimated 440,986 [CI: 108,458–773,513] women in the latest cohort, 2015–2017, representing 0.69% of reproductive-aged U.S. women.
Table 2 shows selected characteristics of the women who reported donated sperm use, with 95% confidence intervals. Among DI users in the population in July 2014, the majority (67%) were non-Hispanic White. About half (51%) lived in a Principle MSA city. Of users, 42% reported having no live births, 13% reported having had one live birth, with the remainder reporting two or more, though not necessarily donor-conceived offspring, as direct outcomes of the donated sperm use were not assessed. Of the women represented in the 2011–2017 combined cohorts, an estimated 33,566,865 had experienced at least one live birth. Of those reporting parity 1 or more, 115,394 [CI: 30,103–200,684] had used donor or mixed sperm (not shown in table). Users were about evenly split in marital history, with 54% currently or formerly married. Users were concentrated among older ages, with only 20% of users under age 35 at interview and 34% between ages 40 and 44. Over three-quarters of donated sperm users reported having a college degree or more and 71% reported a family income over 400% of the poverty line. Finally, sexual minority women made up slightly less than half the reported users, 43%.
Discussion
Historically, there have been few estimates of the prevalence of donor sperm utilization in the United States, despite recent attempts to describe national trends with respect to specific services such as IVF (4). To better understand the patterns in donor sperm use outside of ART, the present study provides trends and estimates for DI use among women in the United States using nationally representative data from the NSFG. Though the NSFG data on infertility service use are not contingent on the diagnosis of infertility or a fertility problem, estimates such as these present a benchmark from which to gauge the prevalence for specific infertility services in the United States. That is, it provides an updated best estimate of the size of this unique population. The relatively small unweighted sample sizes, 81 women across all the included samples and 36 in the 6-year combined estimates, result in very large confidence intervals, both when estimating overall numbers and in describing the characteristics of the users. We acknowledge that this is a limitation of our study, but the NSFG data nonetheless provide one of the best opportunities to study women who have used artificial insemination, let alone donated sperm, in a national U.S. sample.
Even with the large confidence intervals, we see significant differences in estimates over time. Overall, our results suggest a growing trend in the use of donated sperm since the mid-2000s. It is possible that the decrease in use observed after 1995 can be attributed to the fact that Intracytoplasmic Sperm Injection (ICSI) was introduced in the mid-90s (13). This technique, a form of ART, allowed for the use of previously nonviable sperm in some cases, limiting the necessity of donor sperm for different-sex couples who were willing to use a more intensive procedure to potentially have a child biologically related to both parents. Interestingly, the estimates for 2011–2013 were remarkably low, prior to the surge in donor sperm observed with the most recent cohort (2015–2017). As to why the number increased in the latest cohort, we can only speculate. It is possible that the larger number of women utilizing donor sperm is a result of increased social awareness, evidenced by, for example, popular press books on related topics (14, 15). Another reason may be attributed to greater encouragement for parents to be open and share information about donor conception with their children (1), which may be encouraging greater disclosure by those who previously used the services but were unwilling to indicate so in the past.
The profile of users uncovered in the combined 2011–2017 data is similar to other studies’ description of those most likely to access reproductive technologies: mostly White, older, and higher SES individuals (16). There are almost certainly financial and access considerations that help to drive these profiles (17, 18), but there may also be social factors limiting reproductive technology usage, especially among racial and ethnic minorities (18). Because of this, women of minority statuses who choose to move forward with reproductive technology care, like DI, may face additional challenges. Interestingly, we found that a majority of the users were not sexual minority women, although sexual minorities made up a substantial portion of the users given that only about 8% of the overall sample reported a minority sexual orientation (results not shown).
Like any study, this one is not without limitations. First and foremost, the small raw numbers of DI users prevented more in-depth analyses and resulted in the large confidence intervals discussed above. Additionally, our findings are limited to women; the NSFG has collected data for men from 2002 on, but even fewer males (4 or fewer cases in each sample) reported DI use (by a partner). Thus, we restricted our analyses to the women’s data for greater confidence in and stability of estimates. It should also be noted the estimates we have reported do not capture use of donated gametes in IVF and other ART treatments, and we are thus limited to donated sperm rather than including oocyte or embryo donation. This prevents us from making inferences about the estimated size of the DC community at large. Finally, we were unable to clearly estimate the number of annual sperm-DC births from these data, limiting comparability to previous estimates. Future research should address these shortcomings.
Despite these challenges, the present findings contribute new insights to the literature on assisted reproduction. Most importantly, our results suggest that in recent years, nearly half a million women and their families could be dealing with issues related to donor sperm use. This is an important consideration, although its full discussion is beyond the scope of this paper. Some of the issues at the forefront involve, but are not limited to: needing to address if, when, and how to disclose the use of a donor (5, 6); issues related to identifying or contacting the donor and genetic relatives (19, 20); and other costs (e.g., monetary, time, emotional energy) inherent in seeking treatment for infertility or striving to conceive a child in a non-traditional way (21, 22). Although donor conceived families represent a small percentage of the overall population, our work suggests this unique community is growing in large numbers. It is our hope that this work can inspire professionals in the U.S. to keep more complete records on DI and other infertility practices, as other countries already are (23, 24).
Supplementary Material
Funding:
This research received support from the Population Research Training grant (T32 HD007168) and the Population Research Infrastructure Program (P2C HD050924) awarded to the Carolina Population Center at The University of North Carolina at Chapel Hill by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ethics Committee of the American Society for Reproductive Medicine. Informing offspring of their conception by gamete or embryo donation: An Ethics Committee opinion. Fertility and Sterility 2018;109:601–5. [DOI] [PubMed] [Google Scholar]
- 2.Ravitsky V Conceived and deceived: The medical interests of donor-conceived individuals. Hastings Center Report 2014;42:17–22. [DOI] [PubMed] [Google Scholar]
- 3.Almeling R Sex cells: The medical market for eggs and sperm: Univ of California Press, 2011. [Google Scholar]
- 4.Gerkowicz SA, Crawford SB, Hipp HS, Boulet SL, Kissin DM, Kawwass JF. Assisted reproductive technology with donor sperm: National trends and perinatal outcomes. American Journal of Obstetrics and Gynecology 2018;218:421e1–.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pennings G Disclosure of donor conception, age of disclosure and the well-being of donor offspring. Human Reproduction 2017;32:969–73. [DOI] [PubMed] [Google Scholar]
- 6.Pasch LA, Benward J, Scheib JE, Woodward JT. Donor-conceived children: the view ahead. Human Reproduction 2017;32:1534-. [DOI] [PubMed] [Google Scholar]
- 7.Hard AD. Artifical impregnation. The Medical World 1909;27:163–4. [Google Scholar]
- 8.Kramer W 30k–60k US sperm and egg donor births per year? In: Huffingtonpostcom retrived from https://wwwhuffingtonpostcom/wendy-kramer/a-call-to-to-stop-using-t_b_8126736html, 2017.
- 9.Congress U.S. Office of Technology Assessment. Artificial insemination: Practice in the United States: Summary of a 1987 Survey —Background Paper, OTA-13P-BA-48. In: Washington, DC: U.S: Government Printing Office, 1988. [Google Scholar]
- 10.Shapiro S, Saphire DG, Stone WH. Changes in American A.I.D. practice during the past decade. International Journal of Fertility 1990;35:284–91. [PubMed] [Google Scholar]
- 11.National Center for Chronic Disease Prevention and Health Promotion DoRH. Assisted Reproductive Technology (ART).
- 12.National Center for Health Statistics. 2015–2017 National Survey of Family Growth Public-Use Data and Documentation. In: CDC National Center for Health Statistics; Hyattsville, MD, 2018. [Google Scholar]
- 13.Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. The Lancet 1992;340:17–8. [DOI] [PubMed] [Google Scholar]
- 14.Mroz J Scattered Seeds: In Search of Family and Identity in the Sperm Donor Generation. Berkeley, CA: SEAL PRESS, 2017. [Google Scholar]
- 15.Shapiro D Inheritance: A memoir of genealogy, paternity, and love. New York: Alfred A. Knopf, 2019. [Google Scholar]
- 16.Chandra A, Copen CE, Stephen EH. Infertility service use in the United States: Data from the National Survey of Family Growth, 1982–2010 In: National Center for Health Statistics Reports Vol. 73 U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, 2014. [PubMed] [Google Scholar]
- 17.Chandra A, Stephen EH. Infertility service use among U.S. women: 1995 and 2002. Fertility and Sterility 2010;93:725–36. [DOI] [PubMed] [Google Scholar]
- 18.Greil AL, McQuillan J, Shreffler KM, Johnson KM, Slauson-Blevins KS. Race-ethnicity and medical services for infertility: Stratified reproduction in a population-based sample of U.S. women. Journal of Health and Social Behavior 2011;52:493–509. [DOI] [PubMed] [Google Scholar]
- 19.Henriques M Sperm bank warns against tracing anonymous donor via DNA test. In: BioNews retrieved from: https://wwwbionewsorguk/page_141189, 2019.
- 20.Nelson MK, Hertz R. Random Families: Genetic Strangers, Sperm Donor Siblings, and the Creation of New Kin. New York: Oxford University Press, 2019. [Google Scholar]
- 21.Katz P, Showstack J, Smith JF, Nachtigall RD, Millstein SG, Wing H et al. Costs of infertility treatment: Results from an 18-month prospective cohort study. Fertility and Sterility 2011;95:915–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greil AL, Slauson-Blevins K, McQuillan J. The experience of infertility: A review of recent literature. Sociology of Health & Illness 2010;32:140–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fertilisation Human & Authority Embryology. Welcome to the HFEA. https://www.hfea.gov.uk/.
- 24.Victorian Assisted Reproductive Treatment Authority. Home. https://www.varta.org.au/.
- 25.Lozano EB, Fraley RC, Kramer W Attachment in donor-conceived adults: curiosity, search, and contact. Person Relation. 2019;:1–14 (Available at: https://onlinelibrary.wiley.com/doi/full/10.1111/pere.12273). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.