Abstract
Fishing communities are a most-at-risk population for HIV in Uganda. Alcohol use and abuse and economic vulnerability fuel risky sexual practices and lead to increased risk of HIV infection in these communities. Economic strengthening is an emerging intervention approach and interventions promoting saving money via mechanisms with a “soft commitment” in the form of restricting or charging small fees for withdrawals, may serve to reduce spending on alcohol and spending that leads to HIV risk behaviors in cash-based economies. However, little research has been conducted to explore the potential for commitment savings-led economic strengthening interventions to address alcohol use and sexual risk behavior among fisherfolk. This cross-sectional study explored the associations between commitment savings, HIV sexual risk behavior, and problematic alcohol among fisherfolk. We also determined whether commitment savings moderates the associations between problematic alcohol use and risky sexual behaviors. 300 (132 male, 168 female) residents of fishing communities on Lake Victoria, Uganda completed a structured interviewer-assisted interview. Over half (55.3%) used commitment savings by saving money in a bank or savings cooperative or via mobile money. Having problematic alcohol use increased the rate of risky unprotected sex with: all partners (adjIRR 6.08, 95% CI 4.30–8.60) and with casual partners and CSWs/clients (adjIRR 4.90, 95% CI 3.09–7.78), and increased the odds of having met a sex partner at an alcohol venue (adjOR 2.84, 95% CI 1.46–5.51) compared to those without problematic alcohol use. Commitment savings was associated with lower odds of: problematic alcohol use (adjOR 0.50, 95% CI 0.26–0.96), meeting a sex partner at an alcohol venue (adjOR 0.43, 95% CI 0.24–0.78), as well as lower rates of risky unprotected sex with all partners (adjIRR 0.68, 95% CI 0.48–0.96), and with causal partners, CSWs/clients (adjIRR 0.38, 95% CI 0.17–0.85). Use of commitment savings moderated the associations between problematic alcohol use and unprotected sex. However, the moderating effects of commitment savings varied by gender. These findings suggest that promoting saving money in savings mechanisms which involve a commitment may be a potentially viable avenue for HIV prevention among fishing communities and may be particularly helpful for those who have problematic alcohol use.
Keywords: economic-strengthening, sexual risk behavior, alcohol, Uganda, sub-Saharan Africa, commitment savings, fisherfolk, savings-led
INTRODUCTION
Despite successful public health efforts to combat HIV, Uganda is still considered a high burden country due to continued transmission and longevity of people living with HIV. It is estimated that in Uganda in 2017, 1.3 million people were living with HIV and 50,000 adults and children were newly infected with HIV (1). Recent HIV prevention and treatment programs in Uganda have increased their emphasis on reaching most-at-risk populations (MARPs) (2) as data suggests HIV incidence continues to be high in these populations (3, 4). Uganda’s MARPs include those who live or work in fishing communities, uniformed forces, long distance truckers, sex workers, men who have sex with men, and injection drug users (5).
The physical and social environment of fishing communities brings about complex interactions between individuals working or living in the fishing communities, who are broadly referred to as fisherfolk. Fisherfolk include fishermen, fish mongers (fish sellers), boat operators, and other occupations supporting the fishing industry in these communities, such as restaurant and bar workers and female sex workers. Residents of fishing communities are often highly mobile and spend significant amounts of time away from their families. These communities have some of the highest HIV prevalence rates in Uganda with some reports showing HIV prevalence as high as 40% (3–6). A survey of fishing communities in the Lake Victoria Basin showed that HIV prevalence in the surveyed communities was three times higher compared to the surrounding general population (4).
Alcohol use and abuse is also more prevalent in fishing communities (7, 8) and is thought to fuel risky sexual practices (7, 9) and lead to increased risk of HIV infection (10–13). The association between alcohol use and HIV sexual risk behavior is well established in literature from sub-Saharan Africa (14–19). Individuals who drink alcohol, and who drink alcohol before sex, are more likely to engage in unprotected sex and to be HIV-infected compared to those who abstain or drink at a lesser rate (16, 18). Notably, in some studies the effect of alcohol on unprotected sex and HIV infection often only exists, or is more pronounced, with hazardous drinking compared to lower risk consumption (16, 20, 21).
The physical environment in fishing communities contributes to their high rates of alcohol use and abuse and high HIV prevalence (3, 9). Fishing villages operate on a cash economy; workers get daily cash payments for their work but have limited mechanisms for savings due to a lack of a traditional banking infrastructure (9). These situations drive risky behavior as fisherfolk spend their earnings on drinking and other activities deemed stress relieving, including, among men, hiring sex workers (9, 22). Because of this kind of practice, fisherfolk remain highly economically vulnerable even when their incomes lie well above the average local income (23).
Economic vulnerability is associated with both higher risk alcohol use and HIV risk in sub-Saharan Africa (24, 25) and elsewhere (26, 27). To address the role of economic vulnerably on negative health outcomes, in recent years a number of economic strengthening programs have shown positive effects on health outcomes including reducing depressive symptoms (28) and reducing sexual risk behavior (29). A review of economic strengthening interventions among people living with HIV in developing countries including sub-Saharan Africa found studies reporting improvements in ART adherence, retention in care, and quality of life measures, though low rigor/quality of studies suggests the need for more research (30).
Economic strengthening interventions aim to improve the economic stability of a population through one or more of the following: income generation, financial literacy training, conditional cash transfers, microlending, and microsavings. A number of economic strengthening interventions focus on savings and specifically utilize saving in a financial institution such as a bank, a savings cooperative, or via mobile money services (29, 31, 32). Saving using these types of financial services involves some type of savings commitment, either by restricting withdrawals or by charging small fees for withdrawals. These “soft commitments” may help to reduce impulsive purchases for individuals with self-control issues as well as to reduce unnecessary cash withdrawals (33, 34). However, little research has been conducted to explore associations among commitment savings, risky sexual behavior, and alcohol use among fisherfolk, nor whether commitment savings-led economic strengthening interventions could help reduce alcohol use and sexual risk behavior among fisherfolk. Despite the high rate of fisherfolk spending money on alcohol, and male fisherfolk spending money on female sex workers, qualitative data demonstrate that they have a strong desire to save money for the future for such things as building a better house in their village or ensuring they can pay for their children’s education.(9)
There are a number of potential explanations for why savings may be associated with less sexual risk behavior and alcohol use. As noted above, saving using financial services that require a soft commitment may be a structural factor that reduces or deters impulsive purchases on alcohol and hiring sex workers, since there is a small fee associated with accessing the money. Consistent with principles of delayed reward discounting (35), the small cost to access the money may act to increase the salience and value of longer term goals such as saving money, and thereby reduce the perceived value of short term rewards from risk behaviors such alcohol use and risky sex (36, 37). Another related explanation is that individuals who save money may be more focused on achieving their longer-term objectives, which they view as discrepant with engaging in higher risk drinking and risky sex. Lastly, for sex workers, having savings or actively saving money may reduce the urgency of their work and their need to engage in unprotected sex with clients in order to earn more.
The literature reviewed above suggests that HIV interventions for the fisherfolk population may need to reduce alcohol use, and in addition, address underlying economic vulnerability, potentially via a commitment savings-led intervention. However, we know little about associations between commitment savings and problematic alcohol use and between commitment savings and sexual risk behavior among fisherfolk. Given these gaps in the literature, in this study our aims were to test our hypotheses that: commitment savings participation is negatively associated with: a) problematic alcohol use and b) HIV sexual risk behavior, and that problematic alcohol use is associated with sexual risk behavior among male and female fisherfolk in Uganda. In addition, we aimed to determine whether commitment savings moderates the associations between problematic alcohol use and risky sexual behaviors.
METHODS
Study area
We conducted this study in three fishing villages in Wakiso District, in central Uganda, in collaboration with the Wakiso Integrated Rural Development Association (WIRDA). In the fishing villages in Wakiso District the population is growing due to an influx of men searching for employment as fishermen, fish sellers, and related occupations and the women who engage in the sale of alcohol and sex. The district has approximately 20 fishing communities, each with a population between about 1,000 and 7,000. The population in these villages is largely comprised of fishermen, fish sellers, commercial sex workers (CSWs), alcohol-sellers, food vendors, and shopkeepers. In this study, we included fish sellers and alcohol-sellers as high-risk occupational groups in addition to fishermen and CSWs. Previous studies show that females working as alcohol-sellers engage in high-risk sexual behavior, including transactional sex (38–40). Like fishermen, male fish sellers are known to be mobile, and have access to constant flow of cash, which may increase their likelihood of engaging in risky sex including sex with CSWs and sex under the influence of alcohol (9).
Study design and participants
We conducted a cross-sectional study in three fishing communities: Kasenyi, Bugiri, and Bussi Island in Wakiso District. The study population comprised high risk groups, specifically fishermen, fish sellers, alcohol sellers, and CSWs aged 18 years or older. We used quota-based snowball sampling to recruit approximately equal numbers of participants from each of the four high-risk groups at each site. To ensure effective community mobilization and participant recruitment the research team closely worked with WIRDA, a resident community mobilizer, and the Beach Management Unit (BMU), which is an elected group of local leaders representing the community. In the fishing communities, each occupational group (e.g., fishermen, fish sellers, alcohol sellers, restaurant workers, CSWs) has a group leader who is elected by the group members. These leaders represent the interests of their respective occupational group members in the community. A half-day sensitization seminar on the importance of confidentiality in the recruitment process was provided to BMU members and group leaders. WIRDA and the community mobilizer worked with the local BMU to identify the occupational group leaders and then the group leaders identified and recruited members of their respective groups. Participants also referred other potential participants from their occupational group through word of mouth. Potential participants were referred to a research assistant who was seated in a private area within the community (e.g., community center structure).
Data collection procedures
Research assistants fluent in Luganda, the local language, conducted one-on-one interviewer-administered questionnaire interviews of up to one hour’s length with participants. Interviews were conducted used computer-assisted personal interviewing (CAPI) software.
Ethical considerations
Ethical approvals for study procedures were provided by institutional review boards at Brown University and the University of Connecticut Health Center in the U.S. and at the National HIV/AIDS Research Committee in Uganda. The study was also approved by the Uganda National Council for Science and Technology. Written informed consent was obtained from study participants. Participants received 10,000 Shillings (~ $4) as compensation for their time in participating in the study.
Measures
We collected sociodemographic information including age, gender, marital status, education, primary source of income (fishing, selling fish, working in a bar or restaurant, sex work), and monthly income. Participants self-reported their HIV testing history, date of last test, and test results (negative, positive, doesn’t know). Those who reported not knowing their HIV status, or having previously tested HIV negative through a test more than one year ago, were considered to be of unknown HIV status.
We captured detailed data on sexual behavior over the prior 30 days using the Timeline Follow-Back Sexual Behavior Interview (41, 42). Participants were shown a calendar to help them recall their sexual activities in the prior 30 days, and asked to report for each day the number of sex acts (vaginal, anal), condom use during each sex act, and type of partner (steady, casual, client, CSW). Our outcome of the number of risky unprotected sex acts was the number of vaginal or anal sex acts where no condom was used among participants who were unmarried or were married and reported extramarital partners. Those who were married and reported only unprotected sex with their marital partner(s) were considered to have zero risky unprotected sex acts. Our outcome of the number of unprotected sex acts with casual partners, clients, or CSWs, was the number of unprotected vaginal or anal sex acts with these types of partners. The final sexual risk outcome was having ever met a sex partner at a drinking establishment (y/n).
We assessed potential problematic alcohol use with two scales: the 10-item Alcohol Use Disorders Identification test (AUDIT) (43) and the alcohol module of the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS) (44).
The AUDIT assesses potential hazardous alcohol use, dependence symptoms, and harmful alcohol use, which we refer to broadly as problematic alcohol use. The first three items of the AUDIT assess typical frequency of alcohol consumption, quantity of alcohol consumed, and frequency of heavy drinking within the prior 12 months and the remaining seven items assess alcohol-related problems including: experiencing psychological, physical, or social harms resulting from drinking and symptoms of alcohol dependence. AUDIT scores of 8 or more for men and 7 or more for women were considered to reflect potential problematic drinking (43).
The alcohol module of the AUDADIS assesses the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (45) criteria for alcohol use disorders and its reliability has been studied extensively in high, middle, and lower-income country settings (46–48). The AUDADIS instrument assesses the following seven alcohol-related problems/alcohol use disorder criteria: a) tolerance, b) desire to reduce alcohol use or unsuccessful attempts to reduce use, c) drinking more or longer than intended, d) bad after effects when alcohol was wearing off, e) having given up important activities to drink, f) continued drinking despite experiencing physical or psychological problems from drinking, g) spending a lot of time to obtain alcohol, drinking, or recovering from ill effects of drinking. The AUDADIS diagnostic criterion for alcohol-related problem/potential alcohol use disorder is meeting three or more of the seven criteria during the prior 12 months (44).
Since under reporting on quantity and frequency measures of alcohol consumption is common in sub-Saharan Africa (49–51), and 3 questions of the AUDIT are quantity-frequency measures, for the purposes of this study participants were classified as having potentially problematic alcohol use if they had a score above the cutoff on either the AUDIT or the AUDADIS.
We assessed use of commitment savings products, that is, saving via mobile money or in a financial institution, with two questions, one asking if they saved money using mobile money and a second asking if they saved money via a bank, SACCO (Savings and Credit Cooperative Association), or other financial institution. Participants who reported yes to either were classified as using commitment savings. Income insecurity was assessed with one yes-no question asking if they: “often feel at risk that you may not be able to feed yourself or your family?”
Statistical Analysis
We performed all data analyses using SPSS version 24. For the first research question, the association between commitment savings and problematic alcohol use, we used logistic regression. For the second research question, the association between commitment savings and risky unprotected sex (outcomes of the number of risky unprotected sex acts with all partners; the number of unprotected sex acts with casual partners, clients, and CSWs) we used generalized linear modeling with a Poisson distribution. For the outcome of having met a sex partner in an alcohol venue we used logistic regression. For our third research question, a potential moderating effect of commitment savings on the association between problematic alcohol use and sexual risk outcomes and variations by gender, we included interaction effects in the final multivariable models for each of the three sexual risk outcomes. In particular, we were interested in the three-way interaction between problematic alcohol use, commitment savings, and gender. All two-way interactions between the variables in the three-way interaction were also included in the model. For the logistic regressions, we present odds ratios (ORs) and 95% confidence intervals (CI) for each predictor variable. For the Poisson models, we present incident rate ratios (IRR) and 95% CIs.
Other predictor variables we tested in bivariate models included: HIV status, gender, primary source of income, income level, income insecurity, education, marital status, and age. We first ran bivariate models to select variables for inclusion in multivariable models. Predictors associated with the outcome at a statistical significance level of p<0.25 in bivariate models were included in an initial multivariable model. We chose the predictors in final multivariable models by performing backward selection with a p value criterion of 0.10 for removal from the model.
RESULTS
The sample consisted of 132 male and 168 female (total n=300) residents of fishing communities located on Lake Victoria in Uganda. Average age was 31.17 (SD 8.18), less than half (43.0%) were married and 66.3% had primary school level education or less. Approximately half reported financial insecurity (54.3%) and 55.3% reported using commitment savings. Nearly 20% (19.7%) reported being HIV positive, 23.0% reported never testing for HIV or testing more than one year ago, and 57.3% reported testing HIV negative within the prior year. One fifth (20.0%) of participants were classified as having potentially problematic alcohol use, that is, they met AUDIT criteria for potential hazardous/harmful drinking (AUDIT ≥ 7 for women, ≥ 8 for men) or met criteria for a potential alcohol use disorder (AUD) on the AUDADIS (≥ 3 criteria for AUD in the prior 12 months). Participants reported an average of 4.22 (SD 14.24) risky unprotected vaginal or anal sex acts in the prior 30 days. Among those who reported sex with a casual partner, client, or CSW, (n=136, 45% of the sample), they reported an average of 7.79 unprotected vaginal or anal sex acts with causal partners, clients, or CSWs. The vast majority of sex acts reported were vaginal sex, with only two participants reporting anal sex. Approximately 20% of participants reported having met a sex partner at an alcohol-serving establishment. We report sample characteristics in detail by gender and overall in Table 1.
Table 1.
Sample descriptive statistics
| Female n=168 |
Male n=132 |
Overall N=300 |
|
|---|---|---|---|
| Age (mean, SD) | 29.59 (7.20) | 33.17 (8.92) | 31.17 (8.18) |
| Married | 17.9% (30) | 75.0% (99) | 43.0% (129) |
| Education | |||
| Some secondary or > | 25.6% (43) | 43.9% (58) | 33.7% (101) |
| Primary or < | 74.4% (125) | 56.1% (74) | 66.3% (199) |
| Primary source of income | |||
| CSW | 44.0% (74) | - | 24.7% (74) |
| Working in a bar or restaurant | 39.9% (67) | 6.8% (9) | 25.4% (76) |
| Selling fish | 16.1% (27) | 36.4% (48) | 25.0% (75) |
| Fishing | - | 56.8% (75) | 25.0% (75) |
| Monthly income | |||
| ≥$100 | 20.8% (35) | 43.2% (57) | 30.7% (92) |
| $50-<$100 | 20.2% (34) | 24.2% (32) | 22.0% (66) |
| $20-<$50 | 32.7% (55) | 17.4% (23) | 26.0% (78) |
| <$20 | 26.2% (44) | 15.2% (20) | 21.3% (64) |
| Financial insecurity | 61.9% (104) | 44.7% (59) | 54.3% (163) |
| Uses commitment savings a | 50.0% (84) | 62.1% (82) | 55.3% (166) |
| HIV status | |||
| HIV positive | 25.0% (43) | 12.9% (17) | 19.7% (59) |
| Never tested or tested neg. > 1 year ago | 16.7% (28) | 31.1% (41) | 23.0% (69) |
| HIV negative, tested ≤ 1 year ago | 58.3% (98) | 56.1% (74) | 57.3% (172) |
| Problematic alcohol use b | 17.9% (30) | 22.7% (30) | 20.0% (60) |
| Risky unprotected sex acts prior 30 days c (mean, SD) | 5.73 (18.30) | 2.30 (5.39) | 4.22 (14.24) |
| Unprotected sex acts in prior 30 days with casual partner, client or CSW d (mean, SD) | 8.94 (23.57) | 5.33 (8.32) | 7.79 (20.07) |
| Met a new sex partner at an alcohol venue | 22.0% (37) | 20.5% (27) | 21.3% (64) |
Note:
Saves money in a bank or savings cooperative or via mobile money.
Problematic alcohol use refers to hazardous/harmful drinking (AUDIT ≥ 7 for women, ≥ 8 for men) or potential alcohol use disorder (AUDADIS ≥ 3 criteria in prior 12 months).
Risky unprotected vaginal or anal sex defined as: vaginal or anal sex acts where no condom was used among participants who were unmarried or were married and reported extramarital partners.
among those reporting casual partners or clients (n=136).
CSW: Commercial Sex Worker. Income in Ugandan Shillings was converted to USD equivalents.
Association between commitment savings and problematic alcohol use
As shown in Table 2, in bivariate models, use of commitment savings and greater education were both protective factors for problematic alcohol use. Compared to those who had tested HIV negative within the prior year, those who were of unknown HIV status and those who were HIV positive had greater odds of having problematic alcohol use. Age, income insecurity, and primary source of income were associated with problematic alcohol use at p<0.25 and were included in an initial multivariable model. In the final trimmed multivariable model, compared to those who did not use commitment savings, those who did had lower odds of having problematic alcohol use (adjOR 0.50, 95% CI 0.26–0.96). In addition, those with secondary or greater education also had lower odds of problematic alcohol use (adjOR 0.40, 95% CI 0.18–0.88) than did those with primary level or less education. Compared to fish sellers, those working in a bar or restaurant as their primary source of income had nearly four times greater odds of having problematic alcohol use (adjOR 3.88, 95% CI 1.15–13.09). No other occupational groups differed significantly from fish sellers. Only the age group of 35–44 had significantly higher odds of problematic alcohol use (adjOR 3.40, 95% CI 1.09–10.60) compared to the reference group of 18–24 year olds. Compared to those who were HIV negative, those who were of unknown and of HIV positive status had higher odds of having problematic alcohol use; however, these associations were marginally significant (p<0.10).
Table 2.
Results from bivariate and multivariable logistic regression models examining the association between commitment savings and problematic alcohol use among fisherfolk on Lake Victoria, Uganda
| Problematic alcohol useb OR 95% CI |
p value | Problematic alcohol useb AdjOR 95% CI |
p value | |
|---|---|---|---|---|
| Uses commitment savings a | ||||
| Yes | 0.55 (0.31–0.97) | p=0.038 | 0.50 (0.26–0.96) | p=0.038 |
| No | Ref. | Ref | ||
| HIV status | p=0.010 | p=0.096 | ||
| HIV positive | 2.71 (1.34–5.46) | 2.09 (0.97–4.51) | ||
| Unknown status | 2.19 (1.09–4.34) | 1.91 (0.89–4.06) | ||
| HIV negative | Ref. | Ref. | ||
| Gender | p=0.296 | |||
| Female | 0.74 (0.42–1.30) | |||
| Male | Ref. | |||
| Primary source of income | p=0.221 | p=0.170 | ||
| Working in a bar or restaurant | 2.21 (0.95–5.13) | 3.88 (1.15–13.09) | ||
| CSW | 1.36 (0.56–3.34) | 2.65 (0.68–10.34) | ||
| Fishing | 2.05 (0.88–4.81) | 1.13 (0.43–3.01) | ||
| Selling fish | Ref. | Ref. | ||
| Income | p=0.98 | - | - | |
| ≥$100 | 0.87 (0.40–1.91) | |||
| $50–<$100 | 0.88 (0.38–2.05) | |||
| $20–<$50 | 0.85 (0.38–1.93) | |||
| <$20 | Ref. | |||
| Income insecurity | p=0.204 | - | - | |
| Yes | 1.46 (0.82–2.60) | |||
| No | Ref. | |||
| Education | p=0.006 | p=0.023 | ||
| Secondary or > | 0.37 (0.19–0.76) | 0.40 (0.18–0.88) | ||
| Primary or less | Ref. | Ref. | ||
| Marital status | p=0.522 | - | - | |
| Married | 1.20 (0.68–2.13) | |||
| Unmarried | Ref. | |||
| Age | p=0.078 | p=0.172 | ||
| ≥45 | 1.50 (0.39–5.81) | 1.56 (0.36–6.83) | ||
| 35–44 | 3.60 (1.29–10.02) | 3.40 (1.09–10.60) | ||
| 25–34 | 2.51 (0.99–6.33) | 2.22 (0.83–5.96) | ||
| 18–24 | Ref. | Ref. |
Note: OR=Odds ratio; AdjOR=Adjusted Odds Ratio; 95% CI=95% Confidence Interval. CSW: commercial sex work.
Saves money in a bank or savings cooperative or via mobile money.
Problematic alcohol use refers to hazardous/harmful drinking (AUDIT ≥ 7 for women, ≥ 8 for men) or potential alcohol use disorder (AUDADIS ≥ 3 criteria in prior 12 months).
alcohol use refers to hazardous/harmful drinking (AUDIT ≥ 7 for women, ≥ 8 for men) or potential alcohol use disorder (AUDADIS ≥ 3 criteria in prior 12 months).
Bivariate associations of commitment savings and problematic alcohol use with sexual risk outcomes
In bivariate models (Table 3), across the three sexual risk outcomes: risky unprotected sex with all partners, unprotected sex acts with casual partners, clients, or CSWs, and having met a sex partner at an alcohol venue, problematic alcohol use was positively associated with the outcomes. Use of commitment savings was protective for having met a sex partner at an alcohol venue but was a risk factor for both unprotected sex outcomes. In addition, demographic and other variables were associated with sexual risk outcomes. These variables included: HIV status, gender, primary source of income, income, income insecurity, education, marital status, and age. We report each of these associations in Table 3.
Table 3.
Results from bivariate Poisson and logistic regression models examining associations between commitment savings, problematic alcohol use, and risky sexual behaviors among fisherfolk on Lake Victoria, Uganda
| Number of risky unprotected sex acts IRR 95% CI | p value | Number of unprotected sex acts with casual partners/clients/CSWs IRR 95% CI | p value | Met sex partner at alcohol venue OR 95% CI | p value | |
|---|---|---|---|---|---|---|
| Uses commitment savings a | ||||||
| Yes | 1.85 (1.64–2.08) | p<0.001 | 2.00 (1.75–2.28) | p<0.001 | 0.43 (0.25–0.76) | p=0.004 |
| No | Ref | Ref. | Ref. | |||
| Problematic alcohol use b | p<0.001 | p<0.001 | p<0.001 | |||
| Yes | 2.85 (2.55–3.19) | 3.03 (2.69=3.42) | 3.02 (1.62–5.61) | |||
| No | Ref. | Ref. | Ref. | |||
| HIV status | p<0.001 | p<0.001 | p=0.002 | |||
| HIV positive | 1.03 (0.90–1.18) | 0.98 (0.85–1.13) | 2.41 (1.26–4.61) | |||
| Unknown status | 0.63 (0.52–0.76) | 0.69 (0.59–0.82) | 0.53 (0.23–1.22) | |||
| HIV negative | Ref. | Ref. | Ref. | |||
| Gender | p<0.001 | p<0.001 | p=0.742 | |||
| Female | 2.49 (2.19–2.83) | 1.68 (1.45–1.94) | 0.91 (0.52–1.59) | |||
| Male | Ref. | Ref. | Ref. | |||
| Primary source of income | p<0.001 | p<0.001 | p=0.186 | |||
| Working in a bar or restaurant | 0.52 (0.41–0.65) | 1.05 (0.72–1.52) | 2.42 (1.07–5.43) | |||
| CSW | 3.77 (3.25–4.38) | 4.26 (3.16–5.73) | 1.46 (0.62–3.42) | |||
| Fishing | 0.55 (0.44–0.69) | 2.30 (1.66–3.18) | 1.58 (0.68–3.67) | |||
| Selling fish | Ref. | Ref. | Ref. | |||
| Income | p<0.001 | p<0.001 | p=0.772 | |||
| ≥$100 | 3.00 (2.43–3.71) | 3.11 (2.37–4.10) | 1.06 (0.49–2.28) | |||
| $50-<$100 | 5.13 (4.17–6.32) | 4.87 (3.72–6.37) | 0.71 (0.30–1.72) | |||
| $20-<$50 | 1.11 (0.86–1.43) | 0.77 (0.55–1.07) | 1.07 (0.49–2.37) | |||
| <$20 | Ref. | Ref. | Ref. | |||
| Income insecurity | p<0.001 | p=0.547 | p=0.080 | |||
| Yes | 1.43 (1.28–1.60) | 0.96 (0.85–1.09) | 1.67 (0.94–2.95) | |||
| No | Ref. | Ref. | Ref. | |||
| Education | p<0.001 | p=0.011 | p=0.177 | |||
| Secondary or > | 0.74 (0.65–0.84) | 0.83 (0.72–0.96) | 0.66 (0.35–1.21) | |||
| Primary or less | Ref. | Ref. | Ref. | |||
| Marital status | p<0.001 | p<0.001 | p=0.200 | |||
| Married | 0.44 (0.39–0.50) | 0.42 (0.34–0.51) | 0.69 (0.39–1.22) | |||
| Unmarried | Ref. | Ref. | Ref. | |||
| Age | p<0.001 | p<0.001 | p=0.928 | |||
| ≥45 | 0.42 (0.30–0.57) | 0.73 (044–1.19) | 1.22 (0.40–3.70) | |||
| 35–44 | 0.71 (0.58–0.87) | 1.02 (0.81–1.29) | 1.35 (0.55–3.32) | |||
| 25–34 | 1.43 (1.24–1.66) | 1.58 (1.35–1.84) | 1.24 (0.58–2.65) | |||
| 18–24 | Ref. | Ref. | Ref. |
Note: IRR = Incident rate ratio; OR=Odds ratio; CI=95% Confidence Interval. CSW: commercial sex work.
Saves money in a bank or savings cooperative or via mobile money.
Problematic alcohol use refers to problematic drinking (AUDIT ≥ 7 for women, ≥ 8 for men) or potential alcohol use disorder (AUDADIS ≥ 3 criteria in prior 12 months)
Multivariable models associations of commitment savings and problematic alcohol use with sexual risk outcomes
As shown in Table 4 in multivariable models, those who used commitment savings had a 32% lower rate of risky unprotected sex acts with all partners (adjIRR 0.68, 95% CI 0.48–0.96) and a 62% lower rate of unprotected sex acts with casual partners, clients, and CSWs (adjIRR 0.38, 95% CI 0.17–0.85) and had 57% lower odds of having met a sex partner at an alcohol venue (adjOR 0.43, 95% CI 0.24–0.78) than did those who did not use commitment savings.
Table 4.
Results from multivariable Poisson and logistic regression models examining associations between commitment savings, problematic alcohol use, and risky sexual behaviors among fisherfolk on Lake Victoria, Uganda
| Number of risky unprotected sex acts AdjIRR 95% CI | p value | Number of unprotected sex acts with casual partners/clients/CSWs AdjIRR 95% CI | p value | Met sex partner at alcohol venue Ad.jOR 95% CI | p value | |
|---|---|---|---|---|---|---|
| Uses commitment savings a | ||||||
| Yes | 0.68 (0.48–0.96) | p=0.029 | 0.38 (0.17–0.85) | p=0.017 | 0.43 (0.24–0.78) | p=0.006 |
| No | Ref | Ref. | Ref. | |||
| Problematic alcohol use b | p<0.001 | p<0.001 | p=0.003 | |||
| Yes | 6.08 (4.30–8.60) | 4.90 (3.09–7.78) | 2.84 (1.46–5.51) | |||
| No | Ref. | Ref. | Ref. | |||
| HIV status | p<0.001 | p<0.001 | p=0.003 | |||
| HIV positive | 0.72 (0.63–0.84) | 0.71 (0.60–0.83) | 1.99 (1.01–3.95) | |||
| Unknown status | 0.73 (0.60–0.90) | 0.91 (0.74–1.11) | 0.39 (0.16–0.92) | |||
| HIV negative | Ref. | Ref. | Ref. | |||
| Gender | p=0.001 | p<0.001 | ||||
| Female | 0.42 (0.29–0.62) | 0.29 (0.15–0.57) | ||||
| Male | Ref. | Ref. | ||||
| Primary source of income | p<0.001 | p<0.001 | ||||
| Working in a bar or restaurant | 0.97 (0.73–1.29) | 4.09 (2.45–6.82) | ||||
| CSW | 4.25 (3.20–5.64) | 6.25 (3.94–9.92) | ||||
| Fishing | 0.34 (0.26–0.44) | 1.75 (1.14–2.68) | ||||
| Selling fish | Ref. | Ref. | ||||
| Income | p<0.001 | |||||
| ≥$100 | 2.48 (1.97–3.12) | |||||
| $50-<$100 | 3.93 (3.13–4.93) | |||||
| $20-<S50 | 1.02 (0.78–1.32) | |||||
| <$20 | Ref. | |||||
| Income insecurity | p<0.001 | |||||
| Yes | 1.25 (1.10–1.41) | |||||
| No | Ref. | |||||
| Education | p<0.001 | |||||
| Secondary or > | 1.69 (1.38–2.06) | |||||
| Primary or less | Ref. | |||||
| Marital status | p<0.001 | |||||
| Married | 1.54 (1.23–1.94) | |||||
| Unmarried | Ref. | |||||
| Age | p<0.001 | p=0.072 | ||||
| ≥45 | 0.41 (0.29–0.58) | 1.83 (0.99–3.40) | ||||
| 35–44 | 0.56 (0.44–0.70) | 0.90 (0.68–1.19) | ||||
| 25–34 | 0.86 (0.73–1.01) | 0.89 (0.74–1.07) | ||||
| 18–24 | Ref. | Ref. | ||||
| Interactions | ||||||
| Alcohol × commitment savings | 0.81 (0.51–1.29) | p=0.372 | 0.33 (0.14–0.79) | p=0.013 | ||
| Commitment savings × gender | 4.82 (3.23–7.18) | p<0.001 | 6.82 (3.39–13.70) | p<0.001 | ||
| Alcohol × gender | 0.66 (0.42–1.02) | p=0.059 | 2.47 (1.22–4.99) | p=0.012 | ||
| Commitment savings × alcohol × gender | 0.50 (0.29–0.89) | p=0.019 | 0.28 (0.08–0.95) | p=0.041 |
Note: AdjIRR = Adjusted incident ratio ratio. AdjOR=Adjusted Odds Ratio; 95% CI=95% Confidence Interval. CSW: commercial sex work.
Saves money in a bank or savings cooperative or via mobile money.
Problematic alcohol use refers to hazardous/harmful drinking (AUDIT ≥ 7 for women, ≥ 8 for men) or potential alcohol use disorder (AUDADIS ≥ 3 criteria in prior 12 months).
Having problematic alcohol use increased the rate of risky unprotected sex acts with all partners and unprotected sex acts with casual partners, clients, and CSWs by more than four and a half times (adjIRR 6.08, 95% CI 4.30–8.60; adjIRR 4.90, 95% CI 3.09–7.78, respectively) and increased the odds of having met a sex partner at an alcohol venue by nearly three times (adjOR 2.84, 95% CI 1.46–5.51) compared to those who did not have problematic alcohol use.
Compared to those who were HIV negative, those who were HIV positive had lower rates of risky unprotected sex with all partners (adjIRR 0.72, 95% CI 0.63–0.84) and unprotected sex with casual partners, clients, and CSWs (adjIRR 0.71, 95% CI 0.60–0.83) but had nearly two time higher odds of having met a sex partner at an alcohol venue (adjOR 1.99, 95%CI 1.01–3.95). Those of unknown HIV status had lower rates of risky unprotected sex with all partners (adjIRR 0.73, 95% CI 0.60–0.90) and lower odds of having met a sex partner at an alcohol venue (adjOR 0.39, 95% CI 0.16–0.92) than did those who were HIV negative.
Females had lower rates of risky unprotected sex with all partners (adjIRR 0.42, 95% CI 0.29–0.62) and with casual partners, clients, and CSWs (adjIRR 0.29, 95% CI 0.15–0.57) than did males. Compared to fish sellers, CSWs had higher rates (adjIRR 4.25, 95% CI 3.20–5.64), whereas fishermen had lower rates (adjIRR 0.34, 95% CI 0.26–0.44) of risky unprotected sex acts with all partners. CSWs, alcohol sellers/restaurant workers, and fishermen all had higher rates of unprotected sex with casual partners and clients/CSWs than did fish sellers (adjIRR 6.25, 95% CI 3.94–9.92; adjIRR 4.09, 95% CI 2.45–6.82; adjIRR 1.75, 95% CI 1.14=2.68, respectively).
Compared to those in the lowest income category, those with moderate and high income had higher rates of risky unprotected sex acts with all partners (adjIRR 3.93, 95% CI 3.13–4.93 and adjIRR 2.48, 95% CI 1.97–3.12). Having income insecurity was associated with higher rates of risky unprotected sex with all partners (adjIRR 1.25, 95% CI 1.10–1.41).
Greater education was a risk factor for unprotected sex with casual partners, clients, and CSWs (adjIRR 1.69, 95% CI 1.38–2.06). Married individuals had higher rates of risky unprotected sex with all partners than did unmarried individuals (adjIRR 1.54, 95% CI 1.23–1.94). Those aged 45 or older and those 35–44 years of age, had lower rates of risky unprotected sex with all partners (adjIRR 0.41, 95% CI 0.29–0.58 and adjIRR 0.56, 95% CI 0.44–0.70) but those aged 45 or older had higher rates of unprotected sex with casual partners, clients, and CSWs, (adjIRR 1.83, 95% CI 0.99–3.40) than did those aged 18–24, however the latter association was marginally significant.
In the multivariable models there were no statistically significant (p<0.05) differences in the rate of unprotected sex with casual partners, clients, and CSWs based on income, income insecurity, or age. There were also no statistically significant differences in the odds of having met a sex partner at an alcohol venue by gender, primary source of income, income, income insecurity, education, marital status, or age.
Moderation of the association between problematic alcohol use and unprotected sex by savings
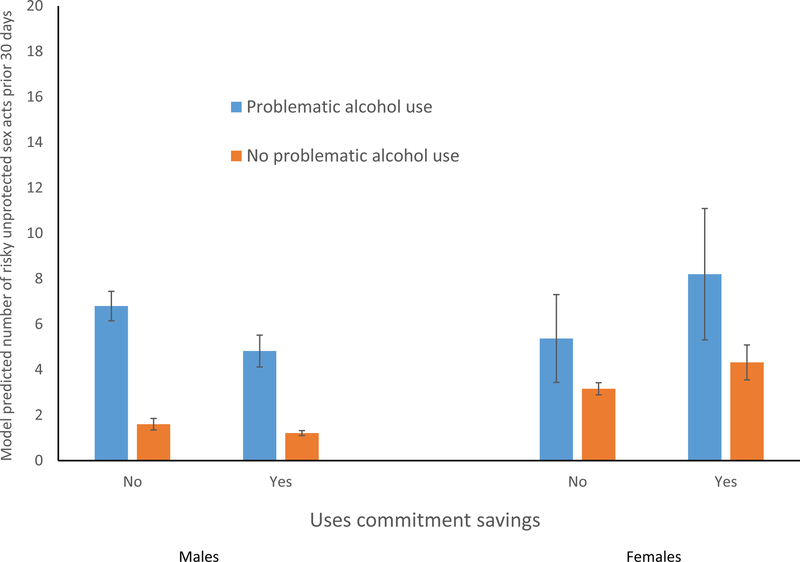
Use of commitment savings moderated the associations between problematic alcohol use and unprotected sex acts with casual partners, clients, and CSWs (alcohol × savings adjIRR 0.33, 95% CI 0.14–0.79). However, we also found that moderating effects of commitment savings varied by gender for risky unprotected sex with all partners and unprotected sex with casual partners, clients, and CSWs. We report the three-way interaction and all two-way interactions at the bottom of Table 4. As we show in Figure 1, among males, use of commitment savings decreased the rate of risky unprotected sex acts with all partners for both those with alcohol problems and those without, but the magnitude of the decrease is significantly greater among those with problematic alcohol use (6.8 to 4.8 vs 1.6 to 1.2). However, for females those who used commitment savings had slightly higher rates of risky unprotected sex than those who did not use commitment savings and the increase was greater among those with problematic alcohol use (5.4 to 8.2) than for those without problematic alcohol use (3.2 to 4.3), however these increases were not statistically significant.
Figure 1.
Moderation of the association between problematic alcohol use and risky unprotected sex by use of commitment savings (n=300)
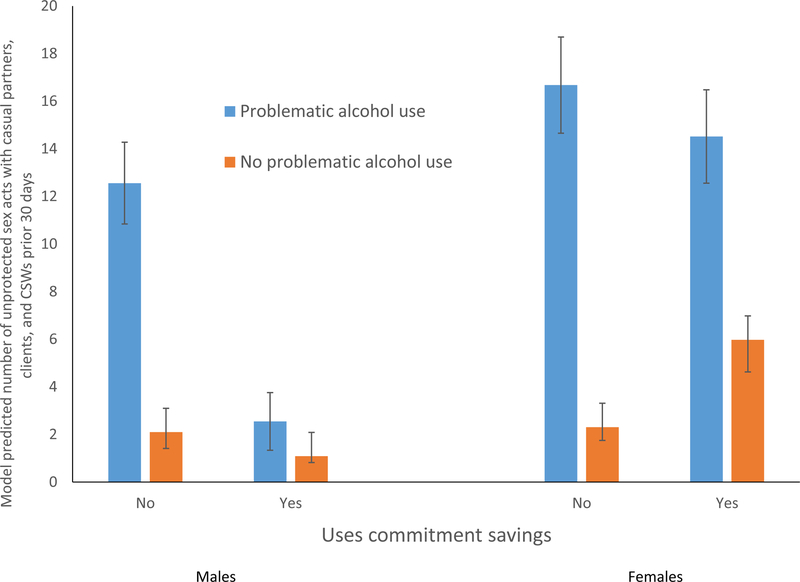
For males, we found somewhat similar patterns for unprotected sex with casual partners, clients, and CSWs as we did for risky unprotected sex with all partners. As Figure 2 illustrates, among men with problematic alcohol use, use of commitment savings dramatically decreased the rate of unprotected sex acts with causal partners and CSWs (12.6 to 2.6), however among men without problematic alcohol use, the decrease was smaller and non-significant (2.1 to 1.1). Among women with problematic alcohol use there was a slight, but non-significant decrease in the rate of unprotected sex with casual partners and clients among those who used commitment savings (16.7 to 14.5). Among females without problematic alcohol use, use of commitment savings increased the rate of unprotected sex with casual partners and clients (2.3 to 5.9).
Figure 2.
Moderation of the association between problematic alcohol use and unprotected sex with causal partners, clients, and CSWs by use of commitment savings (n=136)
DISCUSSION
In this sample of high risk groups from fishing communities on Lake Victoria in Uganda, consistent with our hypotheses, the use of commitment savings was associated with 50% lower odds of problematic alcohol use, 57% lower odds of meeting a sex partner at an alcohol venue, as well as a 32% lower rate of risky unprotected sex with all partners, and a 62% lower rate of unprotected sex with causal partners, CSWs, and clients. More than half of the sample reported using commitment savings, which are savings mechanisms that involve a “soft commitment” by restricting withdrawals or by charging small fees for withdrawals. These findings are consistent with a previous study which found that saving, particularly in a savings group, was significantly associated with nearly two times greater odds of consistent condom use (52), although the mode of savings in that study was different than conceptualized in the present study. The possible explanation for this finding could be that when individuals in these fishing populations save money using methods that require a soft commitment, they reduce the amount of ready to spend cash that they have. This in turn may reduce the spending on things such as alcohol, and among men, buying sex from CSWs.
As expected based on existing literature (7, 9, 14–18), and consistent with our hypotheses, problematic alcohol use was associated with higher rates of sexual risk behavior among both males and females. However, the use of commitment savings moderated these relationships and the moderating effects varied by gender. Among males with problematic alcohol use, those who used commitment savings had lower rates of risky unprotected sex with all partners and with casual partners or CSWs than did those who did not use commitment savings. Among males who did not have problematic alcohol use, the protective effect of commitment savings was smaller. This finding may reflect that for men, especially among those who have problematic alcohol use, using commitment savings may indicate that they have less available cash to spend on hiring CSWs or engaging in other activities that lead to having unprotected sex.
The findings for females were different than for males and somewhat unexpected. Among females with problematic alcohol use, those who used commitment savings had slightly lower rates of unprotected sex with casual partners and clients than did those who did not use commitment savings but this difference was not statistically significant. However, the opposite pattern was observed for risky unprotected sex with all partners, and these differences were also not statistically significant. The findings among women may be influenced by the large proportion of the female sample who were CSWs. It is possible that women use commitment savings in conjunction with sex work, which may explain the inconsistent findings. We were unable to further stratify the female sample by primary occupation due to small cell sizes for testing the interaction effects of interest. However, it is important to note that women without problematic alcohol use had markedly lower rates of unprotected sex than did those with problematic alcohol use regardless of use of commitment savings. Further research is needed to understand how women in this setting use commitment savings, which would help elucidate these unexpected findings.
Our study was not designed to test potential theoretical explanations or mechanisms behind the observed negative associations between use of commitment savings and risky sexual behavior and problematic alcohol. These mechanisms could include that the soft commitment increases the salience of long-term benefits of saving money, greater consideration of future consequences of risk behavior and recognizing the discrepancy between risk behavior and achieving one’s long term goals, or that commitment savings reduces available cash which in turn reduces spending including for things which may lead to risk behavior (e.g., alcohol, hiring CSWs). Future research using a prospective design should investigate such potential mechanisms to guide our understanding of the observed associations. A randomized trial would be most suitable to determine if savings behavior in general, or only specifically commitment savings, produces reductions in risk behavior. In-depth qualitative research could also yield insights on potential mechanisms.
Limitations
This study is limited in a few different ways. First, the cross-sectional design limits our ability to infer causation between alcohol use, savings, and risky sexual behavior. Second, all data were self-reported which likely resulted in an underreporting of risky sexual activity and risky alcohol use. Specifically, 20% of our participants reported problematic alcohol use which is low compared to other studies (3, 7). Sexual behavior was assessed via timeline follow back which may be subject to recall bias. Third, the commitment savings variable was not quantified by frequency or amount of savings, therefore, we cannot infer whether the amount or frequency of savings matters. In addition, how we assessed commitment savings may have excluded those who use informal commitment savings such as through small savings groups. Not all unprotected sex acts may represent sexual risk since we did not assess the HIV serostatus of the partners. Finally, due to the unique physical and social characteristics of fishing communities, findings are likely only generalizable to similar settings and not the general population of Uganda. Another reason for non-generalizability is the quota-based snowball sampling which did not offer an equal probability of selection of participants.
Conclusions
Finding that the use of commitment savings was associated with lower rates of sexual risk behavior, particularly among men who had alcohol problems, suggests that promoting commitment savings may be a potential avenue for HIV prevention interventions for this high-risk population in Uganda. However, longitudinal studies are needed to confirm the observed associations and further investigate gender differences. Future research should explore commitment savings as an intervention to reduce sexual risk behavior among alcohol users as well as whether such an intervention may affect alcohol use. However, our findings suggest that gender tailored interventions may be needed. Overall, these findings suggest that promoting saving money in savings mechanisms which involve a commitment such as with mobile money or a financial institution may be a potentially viable avenue for HIV prevention among fishing communities and may be particularly helpful for those who have problematic alcohol use.
Funding:
This study was supported by National Institute on Alcohol Abuse and Alcoholism Grant P01 AA019072 awarded to Peter M. Monti. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors declare no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional (University of Connecticut Health Center and Brown University) and national research committee (National HIV/AIDS Research Committee, Uganda National Council for Science and Technology) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All participants provided written informed consent.
Ethical approval: This article does not contain any studies with animals performed by any of the authors.
REFERENCES
- 1.Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004;23(5):443–51. [DOI] [PubMed] [Google Scholar]
- 2.Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health 2010;55(3):159–66. [DOI] [PubMed] [Google Scholar]
- 3.Kiwanuka N, Ssetaala A, Mpendo J, Wambuzi M, Nanvubya A, Sigirenda S, et al. High HIV-1 prevalence, risk behaviours, and willingness to participate in HIV vaccine trials in fishing communities on Lake Victoria, Uganda. J Int AIDS Soc 2013;16(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Opio A, Muyonga M, Mulumba N. HIV infection in fishing communities of Lake Victoria basin of Uganda – a cross-sectional sero-behavioral survey. PLoS ONE 2013;8(8):e70770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uganda AIDS Commission. The Uganda HIV and AIDS Country Progress Report - July 2015-June 2016 Kampala, Uganda: Uganda AIDS Commission; 2016. [Google Scholar]
- 6.Chang LW, Grabowski MK, Ssekubugu R, Nalugoda F, Kigozi G, Nantume B, et al. Heterogeneity of the HIV epidemic in agrarian, trading, and fishing communities in Rakai, Uganda: an observational epidemiological study. Lancet 2016;3(3):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tumwesigye NM, Atuyambe L, Wanyenze RK, Kibira SP, Li Q, Wabwire-Mangen F, et al. Alcohol consumption and risky sexual behaviour in the fishing communities: evidence from two fish landing sites on Lake Victoria in Uganda. BMC Public Health 2012;12:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asiki G, Mpendo J, Abaasa A, Agaba C, Nanvubya A, Nielsen L, et al. HIV and syphilis prevalence and associated risk factors among fishing communities of Lake Victoria, Uganda. Sex Transm Infect 2011;87(6):511–5. [DOI] [PubMed] [Google Scholar]
- 9.Sileo KM, Kintu M, Chanes-Mora P, Kiene SM. “Such behaviors are not in my home village, I got them here”: A qualitative study of the influence of contextual factors on alcohol and HIV risk behaviors in a fishing community on Lake Victoria, Uganda. AIDS Behav 2016;20(3):537–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiwanuka N, Ssetaala A, Nalutaaya A, Mpendo J, Wambuzi M, Nanvubya A, et al. High incidence of HIV-1 infection in a general population of fishing communities around Lake Victoria, Uganda. PLoS One 2014;9(5):e94932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiwanuka N, Ssetaala A, Ssekandi I, Nalutaaya A, Kitandwe PK, Ssempiira J, et al. Population attributable fraction of incident HIV infections associated with alcohol consumption in fishing communities around Lake Victoria, Uganda. PLoS One 2017;12(2):e0171200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ssekandi I, Ssetaala A, Mpendo J, Nanvubya A, Nielsen L, Kiwanuka N. Alcohol and illicit drug use among potential HIV vaccine efficacy trial volunteers along Lake Victoria, Uganda. Retrovirology 2012;9(Suppl 2):P219. [Google Scholar]
- 13.Kiene SM, Sileo KM, Dove M, Kintu M. Hazardous alcohol consumption and alcohol-related problems are associated with unknown and HIV-positive status in fishing communities in Uganda. AIDS Care 2019;31(4):451–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tumwesigye NM, Wanyenze RK, Greenfield TK. Intoxication before last sexual encounter and HIV risk behavior among men and women in Uganda: Evidence from a nationwide survey. Int J Alcohol Drug Res 2012;1(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kiene SM, Lule H, Sileo KM, Silmi KP, Wanyenze RK. Depression, alcohol use, and intimate partner violence among outpatients in rural Uganda: vulnerabilities for HIV, STIs and high risk sexual behavior. BMC Infect Dis 2017;17(1):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kiene SM, Simbayi LC, Abrams A, Cloete A, Tennen H, Fisher JD. High rates of unprotected sex occurring among HIV-positive individuals in a daily diary study in South Africa: the role of alcohol use. J Acquir Immune Defic Syndr 2008;49(2):219–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kiene SM, Subramanian SV. Event-level association between alcohol use and unprotected sex during last sex: evidence from population-based surveys in sub-Saharan Africa. BMC Public Health 2013;13:583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woolf-King SE, Maisto SA. Alcohol use and high-risk sexual behavior in Sub-Saharan Africa: a narrative review. Arch Sex Behav 2011;40(1):17–42. [DOI] [PubMed] [Google Scholar]
- 19.Kiene SM, Simbayi LC, Abrams A, Cloete A. Alcohol Expectancies and Inhibition Conflict as Moderators of the Alcohol-Unprotected Sex Relationship: Event-Level Findings from a Daily Diary Study Among Individuals Living with HIV in Cape Town, South Africa. AIDS Behav 2016;20 Suppl 1:S60–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health 2010;55(3):159–66. [DOI] [PubMed] [Google Scholar]
- 21.Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav 2009;13(6):1021–36. [DOI] [PubMed] [Google Scholar]
- 22.Kissling E, Allison EH, Seeley JA, Russell S, Bachmann M, Musgrave SD, et al. Fisherfolk are among groups most at risk of HIV: cross-country analysis of prevalence and numbers infected. AIDS 2005;19(17):1939–46. [DOI] [PubMed] [Google Scholar]
- 23.Béné C Are fishers poor or vulnerable? Assessing economic vulnerability in small-scale fishing communities. The Journal of Development Studies 2009;45(6):911–33. [Google Scholar]
- 24.Morojele NK, Kachieng’a MA, Mokoko E, Nkoko MA, Parry CDH, Nkowane AM, et al. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med 2006;62(1):217–27. [DOI] [PubMed] [Google Scholar]
- 25.MacPherson EE, Sadalaki J, Njoloma M, Nyongopa V, Nkhwazi L, Mwapasa V, et al. Transactional sex and HIV: understanding the gendered structural drivers of HIV in fishing communities in Southern Malawi. J Int AIDS Soc 2012;15(S1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology 2011;218(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reed E, Gupta J, Biradavolu M, Devireddy V, Blankenship KM. The context of economic insecurity and its relation to violence and risk factors for HIV among female sex workers in Andhra Pradesh, India. Public Health Rep 2010;125(4_suppl):81–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ssewamala FM, Neilands TB, Waldfogel J, Ismayilova L. The impact of a comprehensive microfinance intervention on depression levels of AIDS-orphaned children in Uganda. J Adolesc Health 2012;50(4):346–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Witte S, Aira T, Tsai LC, Riedel R, Offringa R, Chang M, et al. Efficacy of a savings-led microfinance intervention to reduce sexual risk for HIV among women engaged in sex work: A randomized clinical trial. Am J Public Health 2015;105(3):e95–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bateganya MH, Dong M, Oguntomilade J, Suraratdecha C. The impact of social services interventions in developing countries: a review of the evidence of impact on clinical outcomes in people living with HIV. J Acquir Immune Defic Syndr 2015;68 Suppl 3:S357–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jennings L, Ssewamala FM, Nabunya P. Effect of savings-led economic empowerment on HIV preventive practices among orphaned adolescents in rural Uganda: results from the Suubi-Maka randomized experiment. AIDS Care 2016;28(3):273–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ssewamala FM, Karimli L, Torsten N, Wang JS, Han CK, Ilic V, et al. Applying a Family-Level Economic Strengthening Intervention to Improve Education and Health-Related Outcomes of School-Going AIDS-Orphaned Children: Lessons from a Randomized Experiment in Southern Uganda. Prev Sci 2016;17(1):134–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dupas P, Robinson J. Why Don’t the Poor Save More? Evidence from Health Savings Experiments. Am Econ Rev 2013;103:1138–71. [DOI] [PubMed] [Google Scholar]
- 34.Ky S, Rugemintwari C, Sauviat A. Does mobile money affect saving behavior? Evidence from a developing country Limoges Cedex, France: Université de Limoges; 2016. [Google Scholar]
- 35.Rachlin H, Raineri A, Cross D. Subjective probability and delay. J Exp Anal Behav 1991;55(2):233–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bickel WK, Landes RD, Christensen DR, Jackson L, Jones BA, Kurth-Nelson Z, et al. Single- and cross-commodity discounting among cocaine addicts: the commodity and its temporal location determine discounting rate. Psychopharmacology 2011;217(2):177–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yoon JH, Higgins ST, Bradstreet MP, Badger GJ, Thomas CS. Changes in the relative reinforcing effects of cigarette smoking as a function of initial abstinence. Psychopharmacology 2009;205(2):305–18. [DOI] [PubMed] [Google Scholar]
- 38.Lubega M, Nakyaanjo N, Nansubuga S, Hiire E, Kigozi G, Nakigozi G, et al. Understanding the socio-structural context of high HIV transmission in Kasensero fishing community, South Western Uganda. BMC Public Health 2015;15:1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.MacPherson EE, Sadalaki J, Njoloma M, Nyongopa V, Nkhwazi L, Mwapasa V, et al. Transactional sex and HIV: understanding the gendered structural drivers of HIV in fishing communities in Southern Malawi. J Int AIDS Soc 2012;15 Suppl 1:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sileo KM, Kintu M, Kiene SM. The intersection of intimate partner violence and HIV risk among women engaging in transactional sex in Ugandan fishing villages. AIDS Care 2018;30(4):444–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sobell LC, Sobell M. Timeline Followback Method (Drugs, Cigarettes, and Marijuana) 1996. Available at: https://cde.drugabuse.gov/instrument/d89c8e23-16e5-625a-e040-bb89ad43465d. Accessed January 13, 2019.
- 42.Weinhardt LS, Carey MP, Maisto SA, Carey KB, Cohen MM, Wickramasinghe SM. Reliability of the timeline follow-back sexual behavior interview. Ann Behav Med 1998;20(1):25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care Geneva: World Health Organization; 2001. [Google Scholar]
- 44.Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 45.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 46.Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule--Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend 1997;47(3):171–85. [DOI] [PubMed] [Google Scholar]
- 47.Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend 1995;39(1):37–44. [DOI] [PubMed] [Google Scholar]
- 48.Ustun B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, et al. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug Alcohol Depend 1997;47(3):161–9. [DOI] [PubMed] [Google Scholar]
- 49.Muyindike WR, Lloyd-Travaglini C, Fatch R, Emenyonu NI, Adong J, Ngabirano C, et al. Phosphatidylethanol confirmed alcohol use among ART-naive HIV-infected persons who denied consumption in rural Uganda. AIDS Care 2017;29(11):1442–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hahn JA, Fatch R, Kabami J, Mayanja B, Emenyonu NI, Martin J, et al. Self-Report of Alcohol Use Increases When Specimens for Alcohol Biomarkers Are Collected in Persons With HIV in Uganda. J Acquir Immune Defic Syndr 2012;61(4):e63–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bajunirwe F, Haberer JE, Boum Y 2nd, Hunt P, Mocello R, Martin JN, et al. Comparison of self-reported alcohol consumption to phosphatidylethanol measurement among HIV-infected patients initiating antiretroviral treatment in southwestern Uganda. PLoS One 2014;9(12):e113152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mantsios A, Galai N, Mbwambo J, Likindikoki S, Shembilu C, Mwampashi A, et al. Community savings groups, financial security, and HIV risk among female sex workers in Iringa, Tanzania. AIDS Behav 2018:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]