Abstract
目的
探讨外周血中性粒细胞-淋巴细胞比值(neutrophil-lymphocyte ratio, NLR)和血小板-淋巴细胞比值(plateletlymphocyte ratio, PLR)在支气管哮喘急性发作期患者中的变化及临床意义。
方法
选取2013年1月~2016年5月期间确诊的支气管哮喘急性发作期患者262例为病例组及130例健康体检者为正常对照组。根据其急性发作期病情严重程度,将哮喘患者分为危重组87例、非危重组175例。记录病例组和健康对照组性别、年龄等临床资料和血常规结果,并计算NLR和PLR。比较3组间中性粒细胞绝对值、淋巴细胞绝对值、血小板计数、NLR、PLR的差异,以ROC曲线评价各指标对哮喘的诊断价值。
结果
各组间中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR差异具有统计学意义(P < 0.0001),各组血小板计数差异无统计学意义(P=0.971)。哮喘危重组淋巴细胞绝对值低于哮喘非危重组、健康对照组(P < 0.0001),而中性粒细胞绝对值、NLR、PLR显著高于哮喘危重组、健康对照组(P < 0.0001)。哮喘非危重组中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR与健康对照组相比差异无统计学意义(P>0.05)。中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR对支气管哮喘急性发作期危重患者诊断的曲线下面积分别为0.802、0.784、0.873、0.795(均P < 0.01)。NLR诊断支气管哮喘急性发作期危重患者的最佳临界值为2.58,敏感度为82.8%,特异度为81.1%。
结论
支气管哮喘患者外周血NLR、PLR均升高,对支气管哮喘的诊断和病情监测有一定临床指导意义。
Keywords: 支气管哮喘, 中性粒细胞-淋巴细胞比值, 血小板-淋巴细胞比值
Abstract
Objective
To investigate the changes of peripheral blood neutrophil-lymphocyte ratio (NLR) and plateletlymphocyte ratio (PLR) in patients in acute stage of bronchial asthma and their clinical significance.
Methods
A total of 262 patients with acute asthma, including 97 critical and 175 non-critical patients, were recruited from our hospital between January, 2013 and May, 2016, with 130 healthy individuals as the control group. The absolute neutrophil count, absolute lymphocyte count, platelet, NLR and PLR were compared among different groups, and their diagnostic values were evaluated using the area under the receiver-operating characteristic (ROC) curve.
Results
The absolute neutrophil count, absolute lymphocyte count, PLR and NLR (P < 0.0001), but not platelet count (P=0.971), differed significantly among the 3 groups. The absolute lymphocyte count was significantly lower while the absolute neutrophil count, NLR and PLR were significantly higher in asthmatic patients in critical condition than in patients in non-critical condition and the control subjects (P < 0.0001), and these parameters showed no significant differences between latter two groups (P>0.05). The areas under the curve of absolute neutrophil count, absolute lymphocyte count, NLR and PLR for the diagnosis of acute exacerbation of bronchial asthma were 0.802, 0.784, 0.873 and 0.795, respectively (all P < 0.01); the optimal cut-off value of NLR was 2.58 for the diagnosis with a sensitivity of 82.8% and a specificity of 81.1%.
Conclusion
Peripheral blood NLR and PLR are increased in asthmatic patients, and their variations offer assistance in the diagnosis and assessment of bronchial asthma.
Keywords: bronchial asthma, neutrophil-lymphocyte ratio, platelet-lymphocyte ratio
支气管哮喘(简称哮喘),是由多种细胞(如嗜酸性粒细胞、中性粒细胞、淋巴细胞、巨噬细胞等)及细胞组分参与的慢性气道炎症性疾病[1]。有文献报道,全球有3亿以上哮喘患者,中国哮喘患病率为1%~4%,哮喘已成为危害人类健康的重要疾病[2]。炎症反应是导致哮喘气道高反应和气道重塑的主要病理机制,在哮喘病情的发生发展中起着重要作用[3]。因此及时监测和评估哮喘炎症水平,对控制哮喘病情发展及治疗方案的选择有重要意义。临床上常用评估哮喘病情的方法如痰涂片观察嗜酸性粒细胞、肺功能试验、血气分析等,但不易检测、费时、不经济。中性粒细胞-淋巴细胞比值(neutrophil-lymphocyte ratio, NLR)和血小板-淋巴细胞比值(platelet-lymphocyte ratio, PLR)是近年来研究较多的反应机体免疫和慢性炎症状态的标志物,因其易于检测而备受关注,在呼吸系统、消化系统、生殖系统肿瘤中得到广泛研究,与肿瘤诊断、病情监测和预后密切相关[4-5]。除此之外,NLR、PLR在急性阑尾炎[6]、过敏性鼻炎[7]、慢性阻塞性肺疾病[8]、系统性红斑狼疮[9]、慢性丙型病毒肝炎[10]等炎症相关疾病中也异常升高,在病情评估中有潜在应用价值。研究表明,与健康者相比,NLR在儿童哮喘中升高[11]。然而NLR、PLR水平在支气管哮喘中的诊断和病情评估中的作用尚不十分明确。因此本研究的目的是探讨NLR、PLR水平在支气管哮喘诊断中的作用和临床意义,从而为支气管哮喘的诊断和治疗提供理论依据。
1. 资料和方法
1.1. 研究对象
收集2013年1月~2016年5月在郑州大学第一附属医院确诊的成人支气管哮喘患者262例,其中男99例,女163例,年龄49±14岁。同时收集同时期年龄、性别无统计学差异的健康体检者130例。入组的哮喘患者均符合2008年中华医学会制定的哮喘诊断标准和全球哮喘防治创议(GINA2010版)的哮喘诊断标准[12-13],所有入组患者支气管舒张试验均为阳性。排除标准:排除有急性或慢性炎症、感染,肺栓塞、慢性支气管炎、肺结核、慢性阻塞性肺疾病及血液系统疾病的患者;合并有其他系统疾病如肝脏、肾脏、心血管疾病、糖尿病,癌症;近一个月内服用激素类药物患者。另外,全血细胞分析发现有贫血、红细胞增多,白细胞减少、白细胞增多症患者不予纳入。盐酸奈必洛尔可影响NLR比值[14],因此接受盐酸奈必洛尔治疗者不予纳入。本研究符合医学伦理学标准,并经医院伦理委员会批准,所有受试者均签署知情同意书。
1.2. 研究方法
记录所有患者的年龄、性别、患病情况等一般临床资料。病例组根据急性发作期病情严重程度参照中华医学会制定的支气管哮喘防治指南的诊断标准,将其分为哮喘危重组87例(包括危重患者),哮喘非危重组175例(包括轻度、中度、重度患者)。所有患者均于确诊次日上午8~9点采集EDTA-K2抗凝静脉血2 mL,采用DxH800血细胞分析仪进行检测,记录病例组和健康对照组血常规检测结果,并计算NLR、PLR。NLR=中性粒细胞绝对值/淋巴细胞绝对值,PLR=血小板计数/淋巴细胞绝对值。
1.3. 统计学方法
采用SPSS17.0软件进行统计学分析,计量资料以均数±标准差表示,采用单因素方差分析进行计量资料的组间比较,采用受试者工作曲线(ROC曲线)评估中性粒细胞绝对值、淋巴细胞绝对值、PLR和NLR在哮喘急性发作期不同严重程度中的诊断价值,并分别计算其最佳临界值、曲线下面积,比较对哮喘诊断的敏感性和特异性,以P < 0.05为差异具有统计学意义。
2. 结果
2.1. 各组一般临床资料比较
哮喘危重组、哮喘非危重组和健康对照组年龄、性别差异无统计学意义(表 1)。
1.
各组一般临床资料比较
Comparison of general clinical data between the 3 groups
| Group | Severe asthma group | Non-severe asthma group | Health group | P |
| Age (year) | 49.9±13.60 | 47.94±12.63 | 49.51±13.58 | 0.109 |
| Male (%) | 39 (44.8%) | 60 (34.3%) | 40 (38.1%) | 0.253 |
2.2. 各组PLT计数、中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR比较
如表 2所示,哮喘危重组、哮喘非危重组和健康对照组中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR比较差异具有统计学意义(P < 0.001),各组血小板计数比较差异无统计学意义(P=0.971)。哮喘危重组淋巴细胞绝对值低于哮喘非危重组、健康对照组(P < 0.001),而中性粒细胞绝对值、NLR、PLR显著高于哮喘非危重组、健康对照组(P < 0.001)。哮喘非危重组中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR与健康对照组相比差异无统计学意义(P>0.05)。
2.
各指标在不同组间的比较
Comparison of neutrophils, lymphocytes, platelets, NLP, and PLR among the 3 groups
| Group | Severe asthma group | Non-severe asthma group | Health group | P |
| Neutrophil absolute value (×109/L) | 8.06±5.27 | 3.90±1.64 | 3.55±1.07 | 0.000 |
| Lymphocyte absolute value (×109/L) | 1.34±0.86 | 2.21±0.89 | 2.15±0.48 | 0.000 |
| Platelets (×109/L) | 233.77士76.74 | 231.37±66.28 | 226.38±37.06 | 0.971 |
| NLR | 9.69±9.84 | 1.99±1.15 | 1.68±0.51 | 0.000 |
| PLR | 248.91±170.15 | 119.25±60.89 | 109.56±26.32 | 0.000 |
2.3. 各指标对危重哮喘诊断的ROC曲线及其诊断价值分析
各指标对危重哮喘诊断的曲线下面积、最佳临界值及其敏感性、特异性、阳性预测值、阴性预测值见表 3。NLR对危重哮喘诊断的曲线下面积为0.873,诊断临界值为2.58,敏感性82.8%,特异性81.1%。PLR对危重组哮喘诊断的曲线下面积为0.795,诊断的临界值为157.08,敏感性70.1%,特异性81.7%。中性粒细胞绝对值、NLR、PLR越大(图 1),淋巴细胞绝对值越小(图 2),哮喘急性发作期病情就越严重。
3.
各指标对哮喘急性发作期危重组诊断的效果评价
Assessment of the value of neutrophils, lymphocytes, NLP, and PLR in diagnosis of acute exacerbation of critical asthma
| Paramater | AUC | P | Cut off value | Sensitivity (%) | Specificity (%) | Positive predicitive value (%) | Negative predicitive value (%) |
| Neutrophil absolute value (×109/L) | 0.802 | < 0.001 | 6.30 | 57.5 | 93.7 | 88.3 | 72.6 |
| Lymphocyte absolute value (×109/L) | 0.784 | < 0.001 | 1.30 | 60.9 | 87.4 | 80.0 | 72.9 |
| NLR | 0.873 | < 0.001 | 2.58 | 82.8 | 81.1 | 78.4 | 85.1 |
| PLR | 0.795 | < 0.001 | 151.33 | 70.1 | 81.7 | 76.9 | 76.4 |
1.

外周血中性粒细胞绝对值、NLR、PLR对危重支气管哮喘诊断的ROC曲线
ROC curves of peripheral blood neutrophil count, NLR, and PLR in critical asthma.
2.
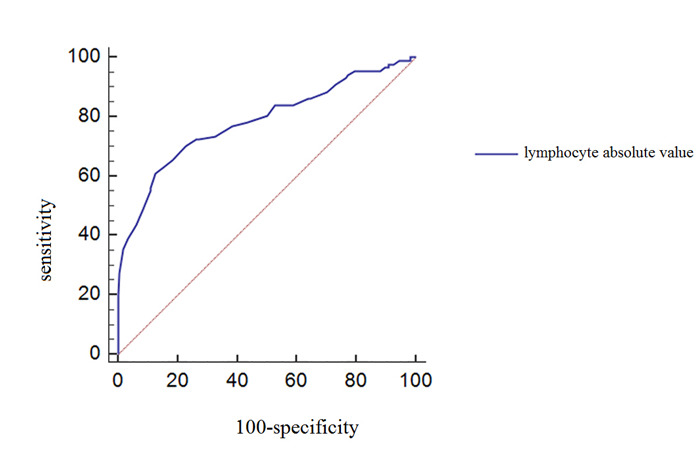
外周血淋巴细胞绝对值对危重支气管哮喘诊断的ROC曲线
ROC curve of peripheral blood absolute lymphocyte count in critical asthma.
3. 讨论
支气管哮喘是一种慢性气道炎症性疾病,其持久性和反复性是长期困扰哮喘患者的重要原因。机体炎症反应增强是急性发作期的重要特征,从而加重哮喘患者病情。近年来一些炎症标志物,如诱导痰、呼出气一氧化氮[15]、尿液嗜酸性粒细胞X蛋白[16]、外周血MMP-9 [17]等被提出用来反应支气管哮喘病情严重程度。呼出气一氧化氮检测方便、迅速,但价格昂贵,增加患者负担。NLR、PLR作为炎症标志物,检测起来更加方便、经济。NLR、PLR最初作为肿瘤标志物已在不同肿瘤疾病中被广泛发现[5]。最近,NLR、PLR也被证实在多种炎症疾病中能够反应机体炎症水平,并与疾病的分期、分级有关[7-8]。本研究表明NLR、PLR作为非特异性炎症指标能够有效诊断出支气管哮喘急性发作期患者,且与急性发作期病情严重程度有关,具有高灵敏度和准确性,对支气管哮喘的诊断、疗效监测、病情评估有重要价值。
本研究分别探讨了中性粒细胞-淋巴细胞比值、血小板-淋巴细胞比值、中性粒细胞绝对值、淋巴细胞绝对值、血小板计数在支气管哮喘诊断及监测急性发作期病情严重程度中的价值。最终发现支气管哮喘危重组、非危重组、健康对照组3组之间中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR比较差异具有统计学意义(p < 0.001),各组血小板计数比较差异无统计学意义(P=0.971)。哮喘危重组淋巴细胞绝对值低于哮喘非危重组、健康对照组,而中性粒细胞绝对值、NLR、PLR显著高于哮喘危重组、健康对照组。哮喘非危重组中性粒细胞绝对值、淋巴细胞绝对值、NLR、PLR与健康对照组相比差异无统计学意义。通过ROC曲线下面积分析比较,发现与NLR相比,PLR在诊断及监测支气管哮喘病情中具有较大的应用价值。
全身炎症伴随着循环外周血白细胞亚群如中性粒细胞、淋巴细胞绝对值的相对变化。近年来,在一些疾病中如急性阑尾炎[6]、过敏性鼻炎[7]、过敏性紫癜[18]、慢性阻塞性肺疾病[8]、急性肺栓塞[19],白细胞及其亚群计数被用作反映炎症程度的标志物。中性粒细胞是免疫防御系统中的重要细胞,其可以调节肥大细胞、上皮细胞、巨噬细胞的功能,且在炎症反应中发挥重要作用[20]。在细菌和病毒感染的早期,外周血NLR比值已经发生改变[21]。NLR是亚临床炎症标志物,在一些炎症疾病中与其他炎症标志物一起判断机体病情严重程度。在慢性阻塞性肺疾病中,NLR水平与气流受限指标如FEV1%预测值呈负相关,并且是COPD患者急性加重的预测指标[8]。呼吸道感染是导致支气管哮喘急性发作的主要诱因,机体炎症反应增强会加重哮喘患者病情[22]。而炎症的重要标志是中性粒细胞计数的升高。NLR评估哮喘的优势在于它是两种不同但又互补的免疫途径的比率,结合了中性粒细胞对非特异性炎症的活化因素和淋巴细胞调控炎症的重要作用,其比率综合反映了机体免疫炎症平衡状态。本研究表明,哮喘危重组NLR比值显著高于哮喘非危重组和健康对照组,而淋巴细胞绝对值低于哮喘非危重组和健康对照组,从而导致哮喘危重组NLR比值升高。有研究表明,儿童哮喘外周血NLR比值高于健康儿童,可用于评估哮喘患者全身炎症。本研究结果NLR水平可在成人支气管哮喘外周血中升高与其一致[11]。
血小板是来自骨髓巨核细胞的无核碎片,通常被认为是凝血和血栓的重要介质,在调节免疫和过敏性炎症方面发挥重要作用[23-25]。近年来,大量临床研究表明,支气管哮喘患者体内凝血与纤溶系统失调,使机体处于高凝状态,并由此加重哮喘病情[26]。在卵清蛋白诱导的哮喘小鼠模型中,血小板通过CD154(CD40L)的表达上调而活化,释放δ颗粒、α颗粒、λ颗粒,最终导致肺部炎症部位白细胞渗出增多,IgE产生增多,加强Th2免疫反应,从而使哮喘小鼠病情加重[25]。由于血小板可以辅助调节多种炎症反应,因此PLR比值的改变可能有助于诊断和评估哮喘病情严重程度。
总之,外周血NLR、PLR作为新型炎症标志物,具有简便、经济、快捷等优点,对监测哮喘病情、调整治疗方案有一定的敏感度和特异性,具有重要的临床应用价值。
Biography
时光, 硕士研究生, E-mail: shiguang2013@126.com
Funding Statement
国家自然科学基金(81501715);河南省科技攻关项目(162102310142,152102410067)
Supported by National Natural Science Foundation of China (81501715)
Contributor Information
时 光 (Guang SHI), Email: shiguang2013@126.com.
明 亮 (Liang MING), Email: mingliang2016@126.com.
References
- 1.Durack J, Boushey HA, Lynch SV. Airway microbiota and the implications of disbiosis in asthma. Curr Allergy Asthma Rep. 2016;16(8):52. doi: 10.1007/s11882-016-0631-8. [Durack J, Boushey HA, Lynch SV.Airway microbiota and the implications of disbiosis in asthma[J].Curr Allergy Asthma Rep, 2016, 16(8): 52.] [DOI] [PubMed] [Google Scholar]
- 2.Ding B, DiBonaventura M, Karlsson N, et al. Asthma-chronic obstructive pulmonary disease overlap syndrome in the urban Chinese population: prevalence and disease burden using the 2010, 2012, and 2013 China National Health and Wellness Surveys. https://www.dovepress.com/asthma-chronic-obstructive-pulmonary-disease-overlap-syndrome-in-the-u-peer-reviewed-article-COPD. Int J Chron Obstruct Plumon Dis. 2016;11:1139–50. doi: 10.2147/COPD.S103873. [Ding B, DiBonaventura M, Karlsson N, et al.Asthma-chronic obstructive pulmonary disease overlap syndrome in the urban Chinese population: prevalence and disease burden using the 2010, 2012, and 2013 China National Health and Wellness Surveys[J].Int J Chron Obstruct Plumon Dis, 2016, 11: 1139-50.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Locksley RM. Asthma and allergic inflammation. Cell. 2010;140(6):777–83. doi: 10.1016/j.cell.2010.03.004. [Locksley RM.Asthma and allergic inflammation[J].Cell, 2010, 140(6): 777-83.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tural Onur S, Sokucu SN, Dalar L, et al. Are neutrophil/lymphocyte ratio and platelet/lymphocyte ratio reliable parameters as prognostic indicators in malignant mesothelioma https://www.researchgate.net/publication/301634735_Are_neutrophillymphocyte_ratio_and_plateletlymphocyte_ratio_reliable_parameters_as_prognostic_indicators_in_malignant_mesothelioma. ? Ther Clin Risk Manag. 2016;12:651–6. doi: 10.2147/TCRM.S104077. [Tural Onur S, Sokucu SN, Dalar L, et al.Are neutrophil/lymphocyte ratio and platelet/lymphocyte ratio reliable parameters as prognostic indicators in malignant mesothelioma[J]? Ther Clin Risk Manag, 2016, 12: 651-6.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu H, Yao X, Xie X, et al.Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients[J].World J Urol, 2016, [Epub ahead of print].
- 6.Yazar FM, Bakacak M, Emre A, et al. Predictive role of neutrophilto-lymphocyte and platelet-to-lymphocyte ratios for diagnosis of acute appendicitis during pregnancy. Kaohsiung J Med Sci. 2015;31(11):591–6. doi: 10.1016/j.kjms.2015.10.005. [Yazar FM, Bakacak M, Emre A, et al.Predictive role of neutrophilto-lymphocyte and platelet-to-lymphocyte ratios for diagnosis of acute appendicitis during pregnancy[J].Kaohsiung J Med Sci, 2015, 31(11): 591-6.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiwanitkit V. Neutrophil to lymphocyte ratio in allergic rhinitis. Eur Arch Otorhinolaryngol. 2016;273(10):3443. doi: 10.1007/s00405-015-3886-0. [Wiwanitkit V.Neutrophil to lymphocyte ratio in allergic rhinitis[J].Eur Arch Otorhinolaryngol, 2016, 273(10): 3443.] [DOI] [PubMed] [Google Scholar]
- 8.Lee H, Um SJ, Kim YS, et al. Association of the Neutrophil-toLymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016;11(6):e0156511. doi: 10.1371/journal.pone.0156511. [Lee H, Um SJ, Kim YS, et al.Association of the Neutrophil-toLymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease[J].PLoS One, 2016, 11(6): e0156511.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Y, Chen Y, Yang X, et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were associated with disease activity in patients with systemic lupus erythematosus. Int Immunopharmacol. 2016;36:94–9. doi: 10.1016/j.intimp.2016.04.006. [Wu Y, Chen Y, Yang X, et al.Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were associated with disease activity in patients with systemic lupus erythematosus[J].Int Immunopharmacol, 2016, 36: 94-9.] [DOI] [PubMed] [Google Scholar]
- 10.Abdel-Razik A, Mousa N, Besheer TA, et al. Neutrophil to lymphocyte ratio as a reliable marker to predict insulin resistance and fibrosis stage in chronic hepatitis C virus infection. http://pubmed.cn/26712048. Acta Gastroenterol Belg. 2015;78(4):386–92. [Abdel-Razik A, Mousa N, Besheer TA, et al.Neutrophil to lymphocyte ratio as a reliable marker to predict insulin resistance and fibrosis stage in chronic hepatitis C virus infection[J].Acta Gastroenterol Belg, 2015, 78(4): 386-92.] [PubMed] [Google Scholar]
- 11.Dogru M, Yesiltepe Mutlu RG. The evaluation of neutrophil-lymphocyte ratio in children with asthma. Allergol Immunopathol (Madr) 2016;44(4):292–6. doi: 10.1016/j.aller.2015.09.005. [Dogru M, Yesiltepe Mutlu RG.The evaluation of neutrophil-lymphocyte ratio in children with asthma[J].Allergol Immunopathol (Madr), 2016, 44(4): 292-6.] [DOI] [PubMed] [Google Scholar]
- 12.中华医学会呼吸病学分会哮喘学组 支气管哮喘防治指南(支气管哮喘的定义、诊断、治疗和管理方案. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zhnk200311028. 中华哮喘杂志:电子版. 2008;2(1):3–13. [中华医学会呼吸病学分会哮喘学组.支气管哮喘防治指南(支气管哮喘的定义、诊断、治疗和管理方案[) J].中华哮喘杂志:电子版, 2008, 2(1): 3-13.] [Google Scholar]
- 13.Bateman ED, Hurd SS, Barnes PJ, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31(1):143–78. doi: 10.1183/09031936.00138707. [Bateman ED, Hurd SS, Barnes PJ, et al.Global strategy for asthma management and prevention: GINA executive summary[J].Eur Respir J, 2008, 31(1): 143-78.] [DOI] [PubMed] [Google Scholar]
- 14.Fici F, Celik T, Balta S, et al. Comparative effects of nebivolol and metoprolol on red cell distribution width and neutrophil/lymphocyte ratio in patients with newly diagnosed essential hypertension. J Cardiovasc Pharmacol. 2013;62(4):388–93. doi: 10.1097/FJC.0b013e31829f716a. [Fici F, Celik T, Balta S, et al.Comparative effects of nebivolol and metoprolol on red cell distribution width and neutrophil/lymphocyte ratio in patients with newly diagnosed essential hypertension[J].J Cardiovasc Pharmacol, 2013, 62(4): 388-93.] [DOI] [PubMed] [Google Scholar]
- 15.Karrasch S, Linde K, Rücker G, et al. Accuracy of FENO for diagnosing asthma: a systematic review. https://www.researchgate.net/publication/305039950_Accuracy_of_FENO_for_diagnosing_asthma_A_systematic_review. Thorax. 2016;10:208704. doi: 10.1136/thoraxjnl-2016-208704. [Karrasch S, Linde K, Rücker G, et al.Accuracy of FENO for diagnosing asthma: a systematic review[J].Thorax, 2016, 10: 208704.] [DOI] [PubMed] [Google Scholar]
- 16.Nuijsink M, Hop WC, Sterk PJ, et al. Urinary eosinophil protein X in childhood asthma: relation with changes in disease control and eosinophilic airway inflammation. Mediators Inflamm. 2013;2013:532619. doi: 10.1155/2013/532619. [Nuijsink M, Hop WC, Sterk PJ, et al.Urinary eosinophil protein X in childhood asthma: relation with changes in disease control and eosinophilic airway inflammation[J].Mediators Inflamm, 2013, 2013: 532619.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grzela K, Litwiniuk M, Zagorska WA. Airway remodeling in chronic obstructive pulmonary disease and asthma: the role of matrix metalloproteinase-9. Arch Immunol Ther Exp (Warsz) 2016;64(1):47–55. doi: 10.1007/s00005-015-0345-y. [Grzela K, Litwiniuk M, Zagorska WA.Airway remodeling in chronic obstructive pulmonary disease and asthma: the role of matrix metalloproteinase-9[J].Arch Immunol Ther Exp (Warsz), 2016, 64(1): 47-55.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park CH, Han DS, Jeong JY, et al. The optimal Cut-Off value of Neutrophil-to-Lymphocyte ratio for predicting prognosis in adult patients with Henoch-Schonlein purpura. PLoS One. 2016;11(4):e0153238. doi: 10.1371/journal.pone.0153238. [Park CH, Han DS, Jeong JY, et al.The optimal Cut-Off value of Neutrophil-to-Lymphocyte ratio for predicting prognosis in adult patients with Henoch-Schonlein purpura[J].PLoS One, 2016, 11(4): e0153238.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma Y, Mao Y, He X, et al. The values of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in predicting 30 day mortality in patients with acute pulmonary embolism. BMC Cardiovasc Disord. 2016;16:123. doi: 10.1186/s12872-016-0304-5. [Ma Y, Mao Y, He X, et al.The values of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in predicting 30 day mortality in patients with acute pulmonary embolism[J].BMC Cardiovasc Disord, 2016, 16: 123.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Vietinghoff S, Ley K. Homeostatic regulation of blood neutrophil counts. J Immunol. 2008;181(8):5183–8. doi: 10.4049/jimmunol.181.8.5183. [von Vietinghoff S, Ley K.Homeostatic regulation of blood neutrophil counts[J].J Immunol, 2008, 181(8): 5183-8.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.李 斌, 张 周良, 杨 珍珍, et al. 中性粒细胞与淋巴细胞壁纸在呼吸道感染性疾病中的应用价值. 中国血液流变学杂志. 2012;3:522–4. [李斌, 张周良, 杨珍珍, 等.中性粒细胞与淋巴细胞壁纸在呼吸道感染性疾病中的应用价值[J].中国血液流变学杂志, 2012, 3: 522-4.] [Google Scholar]
- 22.党 强, 仝 建, 周 小果. 肺炎衣原体感染与哮喘急性发作的相关性研究. http://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201504031.htm. 中华医院感染学杂志. 2015;25(4):794–5, 801. [党强, 仝建, 周小果.肺炎衣原体感染与哮喘急性发作的相关性研究[J].中华医院感染学杂志, 2015, 25(4): 794-5, 801.] [Google Scholar]
- 23.Takeda T, Unno H, Morita H, et al. Platelets constitutively Express IL-33 protein and modulate eosinophilic airway inflammation. J Allergy Clin Immunol. 2016;138(5):1395–403. doi: 10.1016/j.jaci.2016.01.032. [Takeda T, Unno H, Morita H, et al.Platelets constitutively Express IL-33 protein and modulate eosinophilic airway inflammation[J].J Allergy Clin Immunol, 2016, 138(5): 1395-403.] [DOI] [PubMed] [Google Scholar]
- 24.Balta S, Aparci M, Ozturk C, et al. Mean platelet volume as one part of platelet function determining inflammation. https://www.researchgate.net/publication/303669610_Mean_platelet_volume_as_one_part_of_platelet_function_determining_inflammation. Ann Saudi Med. 2016;36(3):234. doi: 10.5144/0256-4947.2016.234. [Balta S, Aparci M, Ozturk C, et al.Mean platelet volume as one part of platelet function determining inflammation[J].Ann Saudi Med, 2016, 36(3): 234.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tian J, Zhu TY, Liu J, et al. Platelets promote allergic asthma through the expression of CD154. Cell Mol Immunol. 2015;12(6):700–7. doi: 10.1038/cmi.2014.111. [Tian J, Zhu TY, Liu J, et al.Platelets promote allergic asthma through the expression of CD154[J].Cell Mol Immunol, 2015, 12(6): 700-7.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Esnault S, Kelly EA, Sorkness RL, et al. Airway factor XⅢ associates with type 2 inflammation and airway obstruction in asthmatic patients. J Allergy Clin Immunol. 2016;137(3):767–73. doi: 10.1016/j.jaci.2015.05.053. [Esnault S, Kelly EA, Sorkness RL, et al.Airway factor XⅢ associates with type 2 inflammation and airway obstruction in asthmatic patients[J].J Allergy Clin Immunol, 2016, 137(3): 767-73.] [DOI] [PMC free article] [PubMed] [Google Scholar]


