Abstract
Background: Health literacy (HL) is an important factor in improving health inequalities in poor and marginalized groups. Assessing comprehensive HL is critical. In this study, we validated the use of a comprehensive short-form HL survey tool (HLS-SF12) and examined the determinants of HL among people in rural areas. Methods: A cross-sectional study was conducted in July 2019 on 440 people residing in mountainous areas in Vietnam. Health literacy was measured using the HLS-SF12. Personal characteristics were also collected. We analyzed data using confirmatory factor analysis, internal consistency analysis, and regression analysis. Results: The questionnaire demonstrated a good construct validity with satisfactory goodness-of-fit indices and item-scale convergent validity. The tool was reliable and homogeneous with Cronbach’s alpha = 0.79, with no floor/ceiling effects. People who were married had lower HL (regression coefficient B = −3.12; 95% confidence interval (CI) = −5.69, −0.56; p = 0.017) compared with those who never married. Higher education attainment (B = 3.41 to 10.44; p < 0.001), a better ability to pay for medication (B = 4.17 to 9.89; p < 0.001), and a tendency to view health-related TV/radio more often (B = 5.23 to 6.15; p < 0.001) were associated with higher HL. Conclusions: The HLS-SF12 is a valid survey tool for the evaluation of HL in rural populations. A number of personal characteristics were strongly associated with HL.
Keywords: health literacy, HLS-SF12, validation, determinant, mountaineer, rural areas, education, health-related TV, ability to pay for medication, Vietnam
1. Introduction
The commitment of the 2030 Sustainable Development Goals (SDGs) agenda is that “no one will be left behind” [1]. Education and literacy are set as one of the main goals of the plan [1]. Literacy and schooling can empower people’s awareness and improve critical thinking skills about their sustainable health, especially in vulnerable groups [1,2]. In addition, health literacy is also considered to be an integral part of policy domains aimed at improving health inequalities within the context of SDGs [3]. Health literacy (HL) has been comprehensively defined as “the knowledge, motivation, and competence to access, understand, appraise, and apply information in everyday life to make judgments and decisions about health care, disease prevention, and health promotion, and to maintain and promote quality of life throughout the life course” [4].
Non-communicable diseases (NCDs) are a heavy burden to Vietnam and the world [5,6]. The strategical interventions to prevent and manage NCD and its burden is essential to advance SDGs, especially in low- and middle-income countries [7,8]. The trend of disease in Vietnam shifted from communicable to non-communicable during the socio-economic reforms of the country from a poor to a low- to middle-income country [9,10,11]. Among NCDs, cardiovascular disease is one of the top 10 leading causes of death in Vietnam [5,12]. Access to health care services in Vietnam is at a low level [13]. In addition, the medication adherence rate, level of awareness, and treatment are relatively low in people with NCDs, and are significantly lower in rural settings [14,15,16].
Health literacy is an important component of public health practice, and it is needed to enable effective health promotional activities/programs and behavior changes [17,18,19,20,21,22]. Better HL is associated with better self-care, better health outcomes, and lower health care expenditure [21,23,24,25,26]. Health literacy is strongly associated with quality of life [27], morbidity, and mortality in rural patients [28]. However, HL level was found to be low in either developing or developed countries [29,30,31]. Vietnam was shown to have the lowest HL level among studied countries [29,32]. Moreover, HL was alarmingly low in people living in rural areas [33].
It is critical to assess HL and its associated factors that may provide helpful evidence when it comes to appropriate health resource allocation. This could improve the effectiveness of health promotion programs and further reduce health inequalities in the context of SDGs. However, a valid, comprehensive survey tool has not been available for use in rural settings. Our aim in this study was to validate the comprehensive short-form health literacy questionnaire (HLS-SF12) and examine the potential determinants of HL among people living in rural areas.
2. Methods
2.1. Study Design and Settings
A cross-sectional study was conducted in July 2019 at two community health stations at the Nham commune in the A Luoi district and the Thuong Long commune in the Nam Don district, both of which are located in the Thua Thien Hue province, Vietnam. These two communes are located in poor mountainous areas in the center of Vietnam, with limited resources, such as health stations, for providing adequate examinations and medication to residents.
2.2. Sampling and Sample Size
The sample size required for conducting the structural equation model (confirmatory factor analysis) was recommended to be 10 times the item number [34]. A sample of 120 participants was adequate for 12 items of the short-form health literacy questionnaire (HLS-SF12). However, our aim was to examine associated factors of health literacy. Therefore, the sample size was calculated using G-Power version 3.1 software (Heinrich-Heine-University, Düsseldorf, Germany) [35]. It was calculated that a sample size of 416 people was required, with a precision or effect size of 0.04, as suggested for a cross-sectional design [36], type I error of 5%, power of 80%, and with 10 predictors investigated in the current study.
Residents visiting community health stations were recruited during the medical tours of Hue University of Medicine and Pharmacy in July 2019. The people selected were those who resided in two mountainous communes in two districts in a central province in Vietnam, were aged 18 and above, did not have any emergency conditions or any mental health problems, and were able to listen and understand the local language or dialect. A total sample of 440 people was collected and analyzed.
2.3. Health Literacy Assessment
The short-form health literacy questionnaire (HLS-SF12), which has been validated in the general population of six Asian countries [32], was used to measure health literacy (HL). The values of Cronbach’s alpha and the goodness-of-fit index of the HLS-SF12 in the general Vietnamese population were 0.87 and 0.97, respectively [32]. People rated the perceived difficulty of each item on four-point Likert scales (1 = very difficult, 2 = difficult, 3 = easy, and 4 = very easy). The indices for HL were standardized to unified metrics from 0 to 50 using the formula; Index = (mean − 1) × (50/3), where Index is the specific index calculated, mean is the mean of all participating items for each individual, 1 is the minimal possible value of the mean (leading to a minimum value of the index of 0), 3 is the range of the mean, and 50 is the chosen maximum value of the new metric. Thus, an index value is obtained where 0 represents the lowest HL and 50 the highest HL [37]. The indices examined in the current study were general HL (GHL) and indices of three domains including health care HL (HC-HL), disease prevention HL (DP-HL), and health promotion HL (HP-HL).
2.4. Personal Characteristics
The following variables were also assessed; age, gender, ethnicity, marital status, education, occupation, the ability to pay for medication, social status, tendency to view health-related TV/radio, and community involvement.
2.5. Data Collection Procedure
The medical students who were utilized as interviewers were trained in data collection by a senior researcher. A four-hour training session took place on the university campus. A daily meeting was conducted in order to improve the quality of the data collected. The research team (researcher and medical students/interviewers) had a two-hour meeting with the medical tour team (volunteer doctors and nurses) and local volunteers regarding the surveys in order to organize the health check and interview sessions. The face to face interviews were conducted at the community health stations using printed questionnaires. Local volunteers helped with interpretation for participants who used the local dialect (about one fifth to one fourth of participants). A consent form was obtained by each participant, while adequate time (15–30 min) was allowed for answering all the questions.
2.6. Ethical Approval
The study was approved by the Institutional Ethical Review Committee of Hanoi School of Public Health, Vietnam (No. 379/2019/YTCC-HD3). All participants were asked for their permission and signed consent forms before their participation.
2.7. Statistical Analysis
Firstly, descriptive analysis was conducted to examine the distribution of study variables. The frequency and percentage, mean and standard deviation were reported. The independent-samples T-test and one-way ANOVA test were used to compare the distribution of health literacy between categories of participants’ characteristics, appropriately. Secondly, to evaluate the validity of the HLS-SF12, we used confirmatory factor analysis (CFA), with a maximum likelihood algorithm estimation to assess the construction of the questionnaire, focusing on three domains of health including health care, disease prevention, and health promotion [38]. The goodness-of-fit indices were reported, including: (i) Absolute model fit, root mean square error of approximation (RMSEA), and goodness-of-fit index (GFI); (ii) Incremental fit, adjusted goodness-of-fit index (AGFI), comparative fit index (CFI), incremental fit index (IFI), and normal fit index (NFI); and (iii) Parsimonious fit, or the chi-square goodness-of-fit test, and the chi-square/degrees of freedom ratio (χ2/df ratio). This method has also been used in a previous study [29]. In addition, the Pearson correlation coefficient was used to assess item-scale convergent validity [39]. Thirdly, the reliability of the HLS-SF12 was assessed using the internal consistency test (Cronbach’s alpha) [40], and the split-half reliability test [41,42]. Fourthly, we examined the floor and ceiling effects of the HLS-SF12 to reflect the responses of participants with the lowest and highest possible scores, respectively. A percentage of 15% or less at the floor or ceiling levels was recommended [43]. Finally, bivariate and multivariate linear regression models were used to explore the determinants of health literacy. The significance level was set at p-value < 0.05. Data were analyzed using the IBM SPSS Version 20.0 (IBM Corp, Armonk, NY, USA), and AMOS version 22.0 (IBM Corp, Armonk, NY, USA)[44].
3. Results
The average age of the study participants was 40.8 ± 13.4 years old; 43.6% were men, 85.9% were an ethnic minority, 87.7% were married, 19.1% were illiterate, 77.7% had participated in agroforestry work, 73% had difficulty paying for medication, 38.1% were perceived to have low social status, 40.2% never or rarely viewed health-related television or radio, and 52.7% were never or were rarely involved in community activities (Table 1). The overall HL index score was 24.2 ± 9.0. The distribution of HL differed among groups depending on age, gender, marital status, education, occupation, the ability to pay for medication, social status, those with a tendency to view health-related television/radio, and those involved with community activities (Table 1).
Table 1.
Characteristics and health literacy index score of participants.
| Total (N = 440) | GHL Index | ||
|---|---|---|---|
| Frequency (%) | Mean ± SD | p-Value 1 | |
| Age | 0.007 | ||
| 18–39 | 223 (50.7) | 25.0 ± 9.0 | |
| 40–59 | 179 (40.7) | 24.1 ± 8.6 | |
| ≥60 | 38 (8.6) | 20.1 ± 10.1 | |
| Gender | <0.001 | ||
| Women | 248 (56.4) | 22.5 ± 9.3 | |
| Men | 192 (43.6) | 26.4 ± 8.2 | |
| Ethnicity attainment | 0.376 | ||
| Kinh (Vietnamese) | 62 (14.1) | 23.3 ± 9.5 | |
| Ethnic minority | 378 (85.9) | 24.4 ± 8.9 | |
| Marital status | <0.001 | ||
| Never married | 54 (12.3) | 31.7 ± 8.2 | |
| Married | 386 (87.7) | 23.2 ± 8.6 | |
| Education | 0.004 | ||
| Illiterate | 84 (19.1) | 17.2 ± 8.8 | |
| Elementary School | 102 (23.2) | 20.9 ± 8.7 | |
| Secondary School | 128 (29.1) | 26.1 ± 7.1 | |
| High School | 102 (23.2) | 29.0 ± 7.1 | |
| Vocational/University | 24 (5.5) | 32.6 ± 5.4 | |
| Occupation | 0.002 | ||
| Agroforestry | 342 (77.7) | 23.5 ± 8.8 | |
| Others (Officers/Small trade/Craft/Housework) | 98 (22.3) | 26.7 ± 9.3 | |
| Ability to pay for medication | <0.001 | ||
| Very difficult | 143 (32.5) | 19.2 ± 8.4 | |
| Fairly difficult | 178 (40.5) | 24.8 ± 8.2 | |
| Fairly easy | 87 (19.8) | 28.9 ± 7.3 | |
| Very easy | 32 (7.3) | 30.7 ± 8.8 | |
| Social status | <0.001 | ||
| Low | 167 (38.1) | 21.5 ± 8.9 | |
| Middle or High | 271 (61.9) | 26.0 ± 8.7 | |
| Tendency to view health-related TV/radio | <0.001 | ||
| Never | 67 (15.2) | 19.1 ± 9.8 | |
| Rarely | 110 (25.0) | 25.3 ± 7.3 | |
| Sometimes | 192 (43.6) | 24.9 ± 9.0 | |
| Often | 71 (16.1) | 25.7 ± 9.3 | |
| Community involvement | 0.003 | ||
| Never | 148 (33.6) | 23.2 ± 9.0 | |
| Rarely | 84 (19.1) | 22.3 ± 9.8 | |
| Sometimes | 157 (35.7) | 25.2 ± 8.1 | |
| Often | 51 (11.6) | 27.4 ± 9.6 |
Abbreviations: GHL, general health literacy; SD, standard deviation; TV, television. 1 p-values were calculated to compare the distribution of the general health literacy index between different categories of participants’ characteristics using the independent-samples T-test or One-way ANOVA test, appropriately.
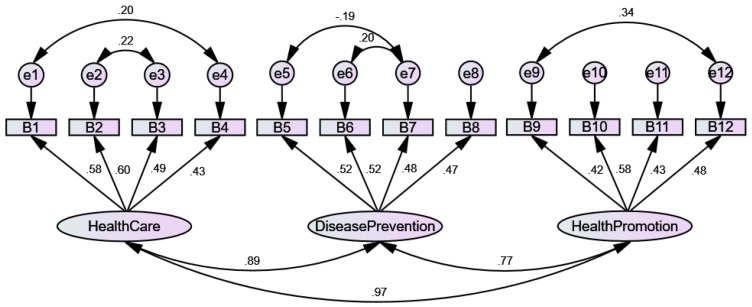
The psychometric properties of the HLS-SF12 are presented in Table 2. Firstly, the construct validity was analyzed by CFA, and the results indicated a good model-data-fit [45]. The absolute model fit was satisfactory, with an RMSEA value of 0.09, and a GFI of 0.94. The incremental fit was adequate, with values of AGFI, CFI, IFI, and NFI ranging from 0.82 to 0.89. The parsimonious fit (χ2/df = 4.34) was also adequate (Table 2). The correlations among three HL domains of healthcare, disease prevention, and health promotion were significantly strong with values ranging from 0.71 to 0.96 (Figure 1).
Table 2.
Goodness-of-fit indices, item-scale convergent validity, internal consistency reliability, and floor/ceiling effects of the HLS-SF12.
| Total Sample (N = 440) |
|
|---|---|
| Absolute model fit 1 | |
| RMSEA | 0.09 |
| GFI | 0.94 |
| Incremental fit 1 | |
| AGFI | 0.89 |
| CFI | 0.85 |
| IFI | 0.86 |
| NFI | 0.82 |
| Parsimonious fit 1 | |
| χ2/df | 4.34 |
| Item-scale convergent validity, range of correlations (rho) | |
| GHL | 0.49–0.64 |
| HC-HL | 0.66–0.74 |
| DP-HL | 0.62–0.73 |
| HP-HL | 0.63–0.73 |
| Reliability, Cronbach’s alpha | |
| GHL | 0.79 |
| HC-HL | 0.65 |
| DP-HL | 0.56 |
| HP-HL | 0.60 |
| Floor effects, % | |
| GHL | 0.50 |
| HC-HL | 7.70 |
| DP-HL | 1.40 |
| HP-HL | 1.80 |
| Ceiling effect, % | |
| GHL | 0.00 |
| HC-HL | 1.40 |
| DP-HL | 1.40 |
| HP-HL | 5.00 |
1 Structure Equation Model of the HLS-SF12 with 12 items loading into three domains of health (health care, disease prevention, health promotion). Abbreviations: HLS-SF12, short-form health literacy questionnaire; RMSEA, root mean square error of approximation; GFI, goodness-of-fit index; AGFI, adjusted goodness-of-fit index; CFI, comparative fit index; IFI, incremental fit index; NFI, normal fit index; χ2/df, relative chi-square; GHL, general health literacy; HC-HL, health care health literacy; DP-HL, disease prevention health literacy; HP-HL, health promotion health literacy.
Figure 1.
Structure equation model of the HLS-SF12 with 12 items loading into three domains of health (health care, disease prevention, health promotion). The questions from B1 to B12 of the HLS-SF12 are stated below. On a scale from very easy to very difficult, how easy would you say it is to: B1…find information on treatments of illnesses that concern you? B2…understand the leaflets that come with your medicine? B3…judge the advantages and disadvantages of different treatment options? B4…call an ambulance in an emergency? B5…find information on how to manage mental health problems like stress or depression? B6…understand why you need health screenings (such as breast exam, blood sugar test, blood pressure)? B7…judge which vaccinations you may need? B8…decide how you can protect yourself from illness based on advice from family and friends? B9…find out about activities (such as meditation, exercise, walking, Pilates, etc…) that are good for your mental well-being? B10…understand information in the media (such as Internet, newspaper, magazines) on how to get healthier? B11…judge which everyday behavior (such as drinking and eating habits, exercise, etc…) is related to your health? B12… join a sports club or exercise class if you want to?
Item-scale convergent validity was satisfactory, with the correlations of 12 items with overall HLS-SF12 scales ranging from 0.49–0.64. The item-scale correlations were stronger in three domains of healthcare (0.66–0.74), disease prevention (0.62–0.73), and health promotion (0.63–0.73), respectively (Table 2). The internal consistency reliability of the HLS-SF12 was adequate, with a Cronbach’s alpha value of 0.79. There was no floor or ceiling effect, as the percentages of people with the lowest scores or the highest scores of HL were 0.50% and 0.00%, which were less than 15% (Table 2).
Finally, the determinants of HL were examined using linear regression models. The results showed that HL was significantly lower in people who were married (regression coefficient, B = −3.12; 95% confidence interval (CI) = −5.69, −0.56, p = 0.017) as compared with those who had never married. In comparison with illiterate people, those with higher education attainment at Elementary School (B = 3.41; 95% CI = 1.33, 5.49; p = 0.001), Secondary School (B = 7.11; 95% CI = 5.07, 9.15; p < 0.001), High School (B = 7.64; 95% CI = 5.31, 9.97; p < 0.001), or Vocational/University (B = 10.44; 95% CI = 6.67, 14.22; p < 0.001) had higher HL scores. Compared with people with the ability to pay for medication at the very difficult level, those with the ability at the levels of fairly difficult (B = 4.17; 95% CI = 2.51, 5.83; p < 0.001), fairly easy (B = 5.64; 95% CI = 3.57, 7.72; p < 0.001), and very easy (B = 9.89; 95% CI = 6.97, 12.80; p < 0.001) had higher HL scores. Compared to people who had never viewed health-related TV/radio, those who viewed rarely (B = 5.23; 95% CI = 2.97, 7.49; p < 0.001), sometimes (B = 4.13; 95% CI = 2.10, 6.16; p < 0.001), and often (B= 6.15; 95% CI = 3.70, 8.60; p < 0.001) had higher HL scores (Table 3).
Table 3.
Determinants of health literacy of people living in rural areas (N = 440).
| Bivariate Model | Multivariate Model | |||
|---|---|---|---|---|
| B (95% CI) | p-Value | B (95% CI) | p-Value | |
| Age | ||||
| 18–39 | Reference | Reference | ||
| 40−59 | −0.92 (−2.68, 0.84) | 0.306 | 0.82 (−0.61, 2.25) | 0.259 |
| ≥60 | −4.98 (−8.06, −1.89) | 0.002 | −2.31 (−4.89, 0.28) | 0.080 |
| Gender | ||||
| Women | Reference | Reference | ||
| Men | 3.90 (2.24, 5.57) | <0.001 | 0.14 (−1.40, 1.67) | 0.860 |
| Ethnicity | ||||
| Kinh (Vietnamese) | Reference | Reference | ||
| Ethnic minority | 1.10 (−1.33, 3.53) | 0.376 | 1.43 (−0.51, 3.37) | 0.148 |
| Marital status | ||||
| Never married | Reference | Reference | ||
| Married | −8.52 (−10.97, −6.07) | <0.001 | −3.12 (−5.69, −0.56) | 0.017 |
| Education attainment | ||||
| Illiterate | Reference | Reference | ||
| Elementary School | 3.73 (1.49, 5.97) | 0.001 | 3.41 (1.33, 5.49) | 0.001 |
| Secondary School | 8.89 (6.76, 11.03) | <0.001 | 7.11 (5.07, 9.15) | <0.001 |
| High School | 11.79 (9.55, 14.03) | <0.001 | 7.64 (5.31, 9.97) | <0.001 |
| Vocational/University | 15.43 (11.91, 18.95) | <0.001 | 10.44 (6.67, 14.22) | <0.001 |
| Occupation | ||||
| Agroforestry | Reference | Reference | ||
| Others (Officers/Small trade/Craft/Housework) | 3.13 (1.12, 5.14) | 0.002 | −1.21 (−3.10, 0.68) | 0.209 |
| Ability to pay for medication | ||||
| Very difficult | Reference | Reference | ||
| Fairly difficult | 5.55 (3.75, 7.34) | <0.001 | 4.17 (2.51, 5.83) | <0.001 |
| Fairly easy | 9.70 (7.53, 11.88) | <0.001 | 5.64 (3.57, 7.72) | <0.001 |
| Very easy | 11.49 (8.36, 14.62) | <0.001 | 9.89 (6.97, 12.80) | <0.001 |
| Social status | ||||
| Low | Reference | Reference | ||
| Middle or High | 4.53 (2.84, 6.22) | <0.001 | 1.37 (−0.13, 2.87) | 0.073 |
| Tendency to view health-related TV/radio | ||||
| Never | Reference | Reference | ||
| Rarely | 6.19 (3.52, 8.87) | <0.001 | 5.23 (2.97, 7.49) | <0.001 |
| Sometimes | 5.75 (3.30, 8.20) | <0.001 | 4.13 (2.10, 6.16) | <0.001 |
| Often | 6.63 (3.69, 9.57) | <0.001 | 6.15 (3.70, 8.60) | <0.001 |
| Community involvement | ||||
| Never | Reference | Reference | ||
| Rarely | −0.91 (−3.30, 1.48) | 0.454 | −0.43 (−2.38, 1.51) | 0.662 |
| Sometimes | 1.99 (−0.02, 3.99) | 0.052 | −0.63 (−2.31, 1.05) | 0.460 |
| Often | 4.21 (1.36, 7.05) | 0.004 | 2.05 (−0.43, 4.53) | 0.105 |
Abbreviations: B, regression coefficient; CI, confidence interval; TV, television.
4. Discussion
The HLS-SF12 was shown to have satisfactory construct validity with a good model-data-fit [45]. In addition, all items correlated with an overall scale and had their own domain scales at moderate and high levels [46], which satisfied the criterion of item-scale convergent validity [39].
The internal consistency of the HLS-SF12 was at an adequate level (Cronbach’s alpha = 0.79) in the current study population, which was slightly lower than previous studies conducted in Europe (Cronbach’s alpha = 0.87 to 0.97) [37] and Asia (Cronbach’s alpha = 0.79 to 0.96) [29,32,47]. In addition, the reliability of the HLS-SF12 was strengthened by the minimal floor/ceiling effect [43].
In the current study, age was negatively associated with HL in the unadjusted model. However, the association was attenuated in the adjusted model. This indicates that age might not be a predictor of HL in rural areas, even though age was one of the important factors of HL in populations in Austria, Bulgaria, Greece, Poland, and Spain, and was partially important in the Netherlands [30,37,48], the USA [49,50], Canada [51], and Taiwan [19,47].
Education attainment and the ability to pay for medication were both highly associated with HL in both the current study and in previous studies in Europe [30,48] and Asia [29,47,52]. In addition, the tendency to view health-related television/radio was positively associated with health literacy, as it was also found to be in a previous study [19]. In the current study, people who were married had lower HL compared with those who had never married. However, marital status has not been significantly associated with HL in previous studies [47,53]. This indicates that in order to improve people’s HL in rural areas, particularly for those who are married, interventions to improve the economic, educational, and health-promoting mass media are highly important.
Health literacy was not significantly different between ethnic minority groups in the current study. This was also found in a previous study in the Netherlands [54]. In addition, HL was also not significantly different between groups of occupation and social status. On one hand, this might indicate that among social demographic factors, ethnic minority is not an important factor. On the other hand, this partly reflect the fact that people living in the same geographical area with the same infrastructure of healthcare systems likely receive the same information and in turn achieve the same level of HL [4]. Finally, community involvement was found to be a predicator of HL in the general population in Taiwan [19,47], but it was not found to be a predicator in people living in mountain areas in the current study. This suggests that health-promoting activities need to be integrated into community activities in rural areas.
The current study has some limitations. Firstly, the study was conducted during the medical tour that provided free health checks and medication for people who live in rural areas. Therefore, the sample collected might not be representative for the whole population, and the external validity of the survey tool may be limited. Secondly, the findings of the current study were based on a sample of 440 people who resided in two mountainous communities in Vietnam. Therefore, the association between personal characteristics and health literacy may not be generalizable to all rural areas in Vietnam. In addition, the associations found in a cross-sectional study can only raise the phenomenon or hypothesis for future study; the causality cannot be generated. Future study with a larger study population in rural areas is required to explore the health literacy levels and the associated factors that might contribute to potential interventions in order to improve the quality of healthcare services and people’s health in rural areas in Vietnam and across the Globe and to achieve SDGs by the year 2030 [2,55].
5. Conclusions
The HLS-SF12 was shown to be valid as a comprehensive survey tool to measure health literacy in a rural setting. Marital status, education, the ability to pay for medication, and the tendency to view health-related television/radio were all determinants of health literacy. The findings may be helpful for effective public health interventions to enhance people’s HL and reduce health inequalities in rural areas.
Acknowledgments
The authors would like to thank the doctors, nurses, medical students, and local volunteers who helped with data collection.
Author Contributions
Conceptualization, T.V.D., T.T.P.N., K.M.P., K.T.N., M.H.G., T.D.X.T., C.X.N., S.-H.Y., and C.-T.S.; data curation, T.V.D., T.T.P.N., K.M.P., K.T.N., M.H.G., T.D.X.T., and C.X.N.; formal analysis, T.V.D.; funding acquisition, T.V.D., S.-H.Y., and C.-T.S; investigation, T.V.D., T.T.P.N., K.M.P., K.T.N., M.H.G., T.D.X.T., C.X.N., S.-H.Y., and C.-T.S.; methodology, T.V.D., T.T.P.N., K.M.P., K.T.N., M.H.G., T.D.X.T., C.X.N., S.-H.Y., and C.-T.S.; project administration, T.V.D. and K.T.N.; resources, T.V.D, S.-H.Y, and C.-T.S.; software, T.V.D.; supervision, T.V.D., K.M.P., S.-H.Y., and C.-T.S.; validation, T.V.D., T.T.P.N., K.M.P., K.T.N., M.H.G., T.D.X.T., C.X.N., S.-H.Y., and C.-T.S.; visualization, T.V.D.; writing—original draft preparation, T.V.D., S.-H.Y., and C.-T.S.; writing—review and editing, T.V.D., T.T.P.N., K.M.P., K.T.N., M.H.G., T.D.X.T., C.X.N., S.-H.Y., and C.-T.S.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.United Nations Development Group . United Nations; 2015. [(accessed on 31 December 2015)]. Transforming our world: The 2030 Agenda for Sustainable Development. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication. [Google Scholar]
- 2.Wagner D.A. Learning, Literacy and Sustainable Development: Inclusion, Vulnerability and the SDGs. In: Battro A.M., Léna P., Sánchez Sorondo M., Von Braun J., editors. Children and Sustainable Development: Ecological Education in a Globalized World. Springer International Publishing; Cham, Switzerland: 2017. pp. 45–65. [Google Scholar]
- 3.Rowlands G., Dodson S., Leung A., Levin-Zamir D. Global health systems and policy development: Implications for health literacy research, theory and practice. Stud. Health Technol. Inform. 2017;240:359–391. [PubMed] [Google Scholar]
- 4.Sørensen K., Van den Broucke S., Brand H., Fullam J., Doyle G., Pelikan J., Slonszka Z. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nhung N.T.T., Long T.K., Linh B.N., Vos T., Huong N.T., Anh N.D. Estimation of Vietnam national burden of disease 2008. Asia Pac. J. Public Health. 2014;26:527–535. doi: 10.1177/1010539513510556. [DOI] [PubMed] [Google Scholar]
- 6.Roth G.A., Abate D., Abate K.H., Abay S.M., Abbafati C., Abbasi N., Abbastabar H., Abd-Allah F., Abdela J., Abdelalim A., et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global burden of disease study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nugent R., Bertram M.Y., Jan S., Niessen L.W., Sassi F., Jamison D.T., Pier E.G., Beaglehole R. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet. 2018;391:2029–2035. doi: 10.1016/S0140-6736(18)30667-6. [DOI] [PubMed] [Google Scholar]
- 8.Niessen L.W., Mohan D., Akuoku J.K., Mirelman A.J., Ahmed S., Koehlmoos T.P., Trujillo A., Khan J., Peters D.H. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018;391:2036–2046. doi: 10.1016/S0140-6736(18)30482-3. [DOI] [PubMed] [Google Scholar]
- 9.Son P.T., Quang N.N., Viet N.L., Khai P.G., Wall S., Weinehall L., Bonita R., Byass P. Prevalence, awareness, treatment and control of hypertension in Vietnam—Results from a national survey. J. Hum. Hypertens. 2012;26:268. doi: 10.1038/jhh.2011.18. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen Q.N., Pham S.T., Nguyen V.L., Weinehall L., Bonita R., Byass P., Wall S. Time Trends in blood pressure, body mass index and smoking in the Vietnamese population: A meta-analysis from multiple cross-sectional surveys. PLoS ONE. 2012;7:e42825. doi: 10.1371/journal.pone.0042825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The World Bank . Country Profile: Vietnam. World Bank Group; Washington, DC, USA: 2018. [(accessed on 8 August 2019)]. Available online: https://data.worldbank.org/country/vietnam. [Google Scholar]
- 12.Hoa N.P., Rao C., Hoy D.G., Hinh N.D., Chuc N.T.K., Ngo D.A. Mortality measures from sample-based surveillance: Evidence of the epidemiological transition in Viet Nam. Bull. World Health Organ. 2012;90:764–772. doi: 10.2471/BLT.11.100750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meiqari L., Nguyen T.-P.-L., Essink D., Zweekhorst M., Wright P., Scheele F. Access to hypertension care and services in primary health-care settings in Vietnam: A systematic narrative review of existing literature. Glob. Health Action. 2019;12:1610253. doi: 10.1080/16549716.2019.1610253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen T.-P.-L., Schuiling-Veninga C.C.M., Nguyen T.B.Y., Vu T.-H., Wright E.P., Postma M.J. Adherence to hypertension medication: Quantitative and qualitative investigations in a rural Northern Vietnamese community. PLoS ONE. 2017;12:e0171203. doi: 10.1371/journal.pone.0171203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meiqari L., Essink D., Wright P., Scheele F. Prevalence of hypertension in Vietnam: A systematic review and meta-analysis. Asia Pac. J. Public Health. 2019;31:101–112. doi: 10.1177/1010539518824810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hien H.A., Tam N.M., Tam V., Derese A., Devroey D. Prevalence, Awareness, Treatment, and Control of Hypertension and Its Risk Factors in (Central) Vietnam. Int. J. Hypertens. 2018;2018:12. doi: 10.1155/2018/6326984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guntzviller L.M., King A.J., Jensen J.D., Davis L.A. Self-efficacy, health literacy, and nutrition and exercise behaviors in a low-income, Hispanic population. J. Immigr. Minor. Health. 2016;19:489–493. doi: 10.1007/s10903-016-0384-4. [DOI] [PubMed] [Google Scholar]
- 18.Yokokawa H., Fukuda H., Yuasa M., Sanada H., Hisaoka T., Naito T. Association between health literacy and metabolic syndrome or healthy lifestyle characteristics among community-dwelling Japanese people. Diabetol. Metab. Syndr. 2016;8:30. doi: 10.1186/s13098-016-0142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duong T.V., Sørensen K., Pelikan J., Van den Broucke S., Lin I.F., Lin Y.-C., Huang H.-L., Chang P.W. Health-related behaviors moderate the association between age and self-reported health literacy among Taiwanese women. Women Health. 2017;58:632–646. doi: 10.1080/03630242.2017.1333074. [DOI] [PubMed] [Google Scholar]
- 20.Mackert M. Introduction to a colloquium: Challenges and opportunities in advancing health literacy research. Health Commun. 2015;30:1159–1160. doi: 10.1080/10410236.2015.1037427. [DOI] [PubMed] [Google Scholar]
- 21.Pelikan J.M., Ganahl K., Roethlin F. Health literacy as a determinant, mediator and/or moderator of health: empirical models using the European Health Literacy Survey dataset. Glob. Health Promot. 2018;25:57–66. doi: 10.1177/1757975918788300. [DOI] [PubMed] [Google Scholar]
- 22.Truman E., Bischoff M., Elliott C. Which literacy for health promotion: Health, food, nutrition or media? Health Promot. Int. 2019 doi: 10.1093/heapro/daz007. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.İlgün G., Turaç İ.S., Orak S. Health literacy. Procedia Soc. Behav. Sci. 2015;174:2629–2633. doi: 10.1016/j.sbspro.2015.01.944. [DOI] [Google Scholar]
- 24.Mackey L.M., Doody C., Werner E.L., Fullen B. Self-management skills in chronic disease management: What role does health literacy have? Med. Decis. Mak. 2016;36:741–759. doi: 10.1177/0272989X16638330. [DOI] [PubMed] [Google Scholar]
- 25.Rasu R.S., Bawa W.A., Suminski R., Snella K., Warady B. Health literacy impact on national healthcare utilization and expenditure. Int. J. Health Policy Manag. 2015;4:747–755. doi: 10.15171/ijhpm.2015.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haun J.N., Patel N.R., French D.D., Campbell R.R., Bradham D.D., Lapcevic W.A. Association between health literacy and medical care costs in an integrated healthcare system: A regional population based study. BMC Health Serv. Res. 2015;15:249. doi: 10.1186/s12913-015-0887-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang C., Lang J., Xuan L., Li X., Zhang L. The effect of health literacy and self-management efficacy on the health-related quality of life of hypertensive patients in a western rural area of China: a cross-sectional study. Int. J. Equity Health. 2017;16:58. doi: 10.1186/s12939-017-0551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moser D.K., Robinson S., Biddle M.J., Pelter M.M., Nesbitt T.S., Southard J., Cooper L., Dracup K. Health literacy predicts morbidity and mortality in rural patients with heart failure. J. Card. Fail. 2015;21:612–618. doi: 10.1016/j.cardfail.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duong T.V., Aringazina A., Baisunova G., Nurjanah, Pham T.V., Pham K.M., Truong T.Q., Nguyen K.T., Oo W.M., Mohamad E., et al. Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries. J. Epidemiol. 2017;27:80–86. doi: 10.1016/j.je.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sørensen K., Pelikan J.M., Röthlin F., Ganahl K., Slonska Z., Doyle G., Fullam J., Kondilis B., Agrafiotis D., Uiters E., et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU) Eur. J. Public Health. 2015;25:1053–1058. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nakayama K., Osaka W., Togari T., Ishikawa H., Yonekura Y., Sekido A., Matsumoto M. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy. BMC Public Health. 2015;15:505. doi: 10.1186/s12889-015-1835-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duong T.V., Aringazina A., Baisunova G., Nurjanah N., Pham T.V., Pham K.M., Truong T.Q., Nguyen K.T., Oo W.M., Su T.T., et al. Development and validation of a new short-form health literacy instrument (HLS-SF12) for the general public in six Asian countries. Health Lit. Res. Pract. 2019;3:e91–e102. doi: 10.3928/24748307-20190225-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li X., Ning N., Hao Y., Sun H., Gao L., Jiao M., Wu Q., Quan H. Health literacy in rural areas of China: Hypertension knowledge survey. Int. J. Environ. Res. Public Health. 2013;10:1125–1138. doi: 10.3390/ijerph10031125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kline R.B. Principles and Practices of Structural Equation Modeling. 4th ed. The Guilford Press; New York, NY, USA: 2015. [Google Scholar]
- 35.Faul F., Erdfelder E., Lang A.-G., Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 36.Pourhoseingholi M.A., Vahedi M., Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench. 2013;6:14–17. [PMC free article] [PubMed] [Google Scholar]
- 37.HLS-EU Consortium . Comparative Report of Health Literacy in Eight EU Member States. The European Health Literacy Project 2009–2012. Maastricht University; Maastricht, The Netherlands: 2012. [(accessed on 22 October 2012)]. Available online: https://www.healthliteracyeurope.net/hls-eu. [Google Scholar]
- 38.Kline R.B. Applied Quantitative Analysis in the Social Sciences. Routledge; New York, NY, USA: 2013. Exploratory and confirmatory factor analysis; pp. 171–207. [Google Scholar]
- 39.Hays R.D., Hayashi T. Beyond internal consistency reliability: Rationale and user’s guide for multitrait analysis program on the microcomputer. Behav. Res. Methods Instr. Comput. 1990;22:167–175. doi: 10.3758/BF03203140. [DOI] [Google Scholar]
- 40.Cronbach L.J., Shavelson R.J. My current thoughts on coefficient alpha and successor procedures. Educ. Psychol. Meas. 2004;64:391–418. doi: 10.1177/0013164404266386. [DOI] [Google Scholar]
- 41.Hays R.D., Anderson R.T., Revicki D. Quality of Life Assessment in Clinical Trials: Methods and Practice. Oxford University Press; New York, NY, USA: 1998. Assessing reliability and validity of measurement in clinical trials; pp. 169–182. [Google Scholar]
- 42.Tsai T.-I., Lee S.-Y.D., Tsai Y.-W., Kuo K.N. Methodology and Validation of health literacy scale development in Taiwan. J. Health. Commun. 2010;16:50–61. doi: 10.1080/10810730.2010.529488. [DOI] [PubMed] [Google Scholar]
- 43.Terwee C.B., Bot S.D.M., de Boer M.R., van der Windt D.A.W.M., Knol D.L., Dekker J., Bouter L.M., de Vet H.C.W. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 44.IBM SPSS . IBM SPSS Statistics for Windows, Version 20.0. IBM Corp; New York, NY, USA: 2011. [Google Scholar]
- 45.Floyd F.J., Widaman K.F. Factor analysis in the development and refinement of clinical assessment instruments. Psychol. Assess. 1995;7:286–299. doi: 10.1037/1040-3590.7.3.286. [DOI] [Google Scholar]
- 46.Taylor R. Interpretation of the correlation coefficient: A basic review. J. Diagn. Med. Sonogr. 1990;6:35–39. doi: 10.1177/875647939000600106. [DOI] [Google Scholar]
- 47.Duong T.V., Lin I.-F., Sørensen K., Pelikan J.M., Van den Broucke S., Lin Y.-C., Chang P.W. Health literacy in Taiwan: A population-based study. Asia Pac. J. Public Health. 2015;27:871–880. doi: 10.1177/1010539515607962. [DOI] [PubMed] [Google Scholar]
- 48.Van der Heide I., Rademakers J., Schipper M., Droomers M., Sørensen K., Uiters E. Health literacy of Dutch adults: A cross sectional survey. BMC Public Health. 2013;13:1–11. doi: 10.1186/1471-2458-13-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Paasche-Orlow M.K., Parker R.M., Gazmararian J.A., Nielsen-Bohlman L.T., Rudd R.R. The prevalence of limited health literacy. J. Gen. Intern. Med. 2005;20:175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rudd R.E. Health literacy skills of US adults. Am. J. Health Behav. 2007;31:S8–S18. doi: 10.5993/AJHB.31.s1.3. [DOI] [PubMed] [Google Scholar]
- 51.Rootman I., Gordon-El-Bihbety D. A Vision for a Health Literate Canada: Report of the Expert Panel on Health Literacy. Canadian Public Health Association; Ottawa, ON, Canada: 2008. [(accessed on 16 June 2017)]. Available online: https://www.cpha.ca/vision-health-literate-canada-report-expert-panel-health-literacy. [Google Scholar]
- 52.Liu Y.-B., Liu L., Li Y.-F., Chen Y.-L. Relationship between health literacy, health-related behaviors and health status: A survey of elderly Chinese. Int. J. Environ. Res. Public Health. 2015;12:9714–9725. doi: 10.3390/ijerph120809714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kayupova G., Turdaliyeva B., Tulerayev K., Duong T.V., Chang P.W., Zagulova D. Health literacy among visitors of district polyclinics in Almaty, Kazakhstan. Iran. J. Public Health. 2017;46:1062–1070. [PMC free article] [PubMed] [Google Scholar]
- 54.Van der Gaag M., van der Heide I., Spreeuwenberg P.M.M., Brabers A.E.M., Rademakers J.J.D.J.M. Health literacy and primary health care use of ethnic minorities in the Netherlands. BMC Health Serv. Res. 2017;17:350. doi: 10.1186/s12913-017-2276-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.United Nations . The Sustainable Development Goals Report 2019. United Nations Statistics Division; New York, NY, USA: 2019. [(accessed on 30 June 2019)]. Available online: https://unstats.un.org/sdgs/report/2019/The-Sustainable-Development-Goals-Report-2019.pdf. [Google Scholar]