Abstract
Objectives
To evaluate the safety of moxa smoke, especially to provide quantitative information and details for the occupational prevention of acupuncturists.
Methods
We combined the questionnaire-based cross-sectional survey and lung function testing-based historical retrospective cohort research to investigate the safety of moxa smoke exposure (MSE) among acupuncturists. A mathematical regression model was established to quantitatively evaluate the relationship between moxa smoke exposure and the respiratory health of the acupuncturist. The smoke exposure time of the acupuncturist and the prevalence of abnormal respiratory symptoms or diseases were also evaluated.
Results
(1) The cross-sectional research showed that the incidence of expectoration (18.7%) and rhinitis (22.7%) was the most common respiratory symptom and disease after MSE. No statistical difference was found between smoke exposure time of the acupuncturist and the prevalence of abnormal respiratory symptoms or diseases, except the prevalence of rhinitis and shortness of breath (P < 0.01). Regression model for the incidence of first three symptoms (expectoration, shortness of breath, and wheezing) from the cross-sectional survey indicated that the weight coefficients of factors associated with moxa smoke were lower than those of factors unrelated to moxa smoke, such as gender and personal history of respiratory diseases. (2) Historical retrospective cohort research showed that there was no significant difference in the % predicted PEF. No statistic difference was found between the exposed and nonexposed group in large airway function indexes (% predicted FEV1, % predicted FVC, and % predicted FEV1/FVC) and small airway function indexes (% predicted FEF25, % predicted FEF50, % predicted FEF75, and % predicted MMEF), either. Especially, the % predicted MVV among males (106.23 ± 2.92 vs. 95.56 ± 1.92, P < 0.01 and % predicted VC among females (100.70 ± 1.59 vs. 95.91 ± 1.61, P < 0.05) between the two groups had statistical significance, but did not cause pulmonary ventilation dysfunction.
Conclusions
MSE has no significant effect on the respiratory health of acupuncturists.
1. Introduction
Moxibustion is one of the traditional Chinese medicine (TCM) therapies that use the heat generated by burning herbal preparations containing Artemisia vulgaris (mugwort) to stimulate acupuncture points [1]. In China and some other Asian countries, moxibustion has been used to treat various diseases such as painful disease [2], knee osteoarthritis [3, 4], gastrointestinal diseases [5], antiaging [6], immunomodulatory [7], primary dysmenorrhea [8], primary insomnia [9], chronic fatigue syndrome [10], and cancer-related fatigue [11]. Nowadays, moxibustion is being increasingly accepted as an alternative treatment for correct nonvertex presentation [12], irritable bowel syndrome [13], inflammation bowel disease [14], and neurological symptoms [15], and so on. Hence, moxibustion has attracted increasing interest in more and more countries.
With people paying more attention to environmental pollution and their own health, the security challenge caused by moxa smoke has become the focus of attention, just as incense burning produces large amounts of particulate matter (PM), nitrogen dioxide, sulfur dioxide, formaldehyde, benzene, polycyclic aromatic hydrocarbons (PAH), and so on [16]. During the past decade, a considerable number of clinical and experimental studies have indicated that moxa smoke contains a range of chemical components, including inhalable particles (PM 10 and PM 2.5), formaldehyde, naphthalene, benzene, methylbenzene, total volatile organic compounds, CO, CO2, NO, SO2, NH3, and O3 [17, 18]. However, some studies have demonstrated that the concentrations of these substances are minimal and can be controlled within a safe concentration range in clinical [17, 19]. By keeping ventilation well, the contents of CO, NO2, PM 10, and PM 2.5 in the air can be controlled within safe ranges [20]. And under normal operating conditions, neither volatile nor carbon monoxide would do harm to health and safety [21]. Based on these studies, the potential effect of moxa smoke on health is controversial.
In previous studies, we found that moxa smoke causes adverse stimulus reactions to the body and affects the compliance of patients with moxibustion [22, 23]. Besides, a number of researchers have also shown solicitude for the safety of people exposed to moxa smoke. For example, Wang et al.'s research demonstrated that the body's responses of participants after exposed to moxa smoke were most notable in areas with exposed mucous membranes, such as the eyes, nose, and throat [24]. Zhao et al. focused on the patients' heart rate and heart rate variability after MSE [25]. However, most of them were focused on patients, and little work has been undertaken with regard to whether moxa smoke is harmful to acupuncture practitioners who were frequently exposed to moxa smoke. Hence, the present study aimed at achieving the following: (1) a cross-sectional survey was carried out among acupuncture practitioners, by using the American Thoracic Society Division of Lung Disease questionnaire (ATS-DLD-78-A), to observe the incidence of abnormal respiratory symptoms and respiratory diseases after MSE. Additionally, a corresponding mathematical model was established to quantitatively analyze the relationship between MSE and the respiratory health of acupuncturist using the data collected from the cross-sectional survey. (2) A historical retrospective cohort study was carried out on the lung function health status in the moxa smoke-exposed and nonexposed group using portable pulmonary function instrument (ST-75).
2. Methods
2.1. Study Design and Population
2.1.1. The Cross-Sectional Survey
The cross-sectional survey was conducted between May 2016 and April 2017 to assess the respiratory health status of acupuncturists who practice acupuncture treatment regularly. Participants were recruited from 79 TCM hospitals, 30 prefectures (states and cities), spanning 4 provinces (including Sichuan province, Shaanxi province, Anhui province, and Hunan province) in China via face-to-face interview. Participants were enrolled if they had obtained the qualification of a Chinese medicine practitioner or assistant Chinese medicine practitioner; registered or engaged in acupuncture and moxibustion for at least one year or regularly conduct acupuncture and moxibustion diagnosis and treatment activities in TCM hospitals; between 23 and 70 years of age; and signed informed consent. The main exclusion criteria were long-term use of smokeless moxibustion or smokeless moxibustion appliances and acupuncture and moxibustion practice for less than one year.
The prevalence of respiratory health was assessed through the American Thoracic Society Division of Lung Disease adult questionnaire (ATS-DLD-78-A) which had been translated into Chinese. The questionnaire was translated by a professional translator, and another translator was asked to reassess its accuracy. They jointly determined the final Chinese version. The questionnaire has also been used in other respiratory health surveys in China [26, 27]. A structured questionnaire was used to obtain detailed information on sociodemographic characteristics, occupational factors, and confounding factors. Occupational factors contain some moxa exposure information, such as working years of moxibustion, average days of moxibustion activities per week, average number of moxibustion patients per day, average duration of receiving moxibustion therapy per patient, whether there was ventilation equipment in moxibustion clinic, subjective evaluation of moxibustion concentration in moxibustion environment, area of moxibustion clinic, and number of patients receiving treatment in the same moxibustion room at the same time. Confounding factors contain personal history of respiratory diseases, family history of respiratory diseases, smoking, second-hand smoke exposure, and so on.
The items of respiratory symptoms and diseases consisted of cough, chronic cough, phlegm, chronic phlegm, gasp for breath, wheezing, breathlessness, dyspnea on exertion, chest colds, chest illness, bronchitis, pneumonia, rhinitis, and chronic bronchitis, which were determined on the basis of positive answers to the following items:
Cough: “Do you usually have a cough?” or “Do you often cough in the morning or when you get up?” Or “Do you often cough during the day or at night?”
Chronic cough: “Do you usually cough four to six times a day, four days a week or more?” or “Do you usually cough like this for three months or more in a year?”
Expectoration: “Do you often expectorate?” or “Do you often expectorate when you get up in the morning? Or it is the first thing in the morning?” or “Do you often expectorate during the day or at night?”
Chronic expectoration: “Do you often expectorate twice a day, four days a week or more?” or “Do you have this kind of expectoration for three months or more in a year?”
Gasp for breath: “Does your chest ever wheeze or whistle when you have a cold, or when you don't catch a cold, or do you make a sound of whistling most of the day or night?”
Wheezing: “Have you ever had an attack of wheezing that has made you feel short of breath?”
Shortness of breath: “Are you troubled by shortness of breath when hurrying on the level or walking up a slight hill?”
Bronchitis, pneumonia, rhinitis, chronic bronchitis, asthma, and emphysema: “Have you ever had bronchitis/pneumonia/rhinitis/chronic bronchitis/asthma/emphysema and been confirmed by a doctor?”
A subgroup analysis was also conducted between smoke exposure time of the acupuncturist and abnormal respiratory symptoms and disease prevalence. Additionally, the corresponding mathematical model was established to quantitatively analyze the relationship between MSE and the respiratory health of acupuncturists using the data of the first three symptoms collected from the cross-sectional survey.
2.1.2. Historical Retrospective Cohort Research
The cohort study was conducted between June 2016 and March 2018 to review the lung function between the group exposed to moxa smoke and nonexposed group, by using portable spirometer (Spiroanalyzer, ST-75, Fukuda Sangyo, Japan). Participants were recruited from 16 TCM hospitals in Chongqing city and Sichuan province of China. Cluster sampling method was used in this study. 142 acupuncturists were recruited as the observation group. The inclusion and exclusion criteria were consistent with the previous test. The control group was 142 nonacupuncturists (hospital administrators or other medical staff) who were not exposed to moxa smoke. According to the ratio of 1:1, matched by gender, average age difference was <3 year old, average height difference was <3 cm, and average weight difference was <5 kg. After filling out the questionnaires of sociodemographic data, the lung function indexes of all subjects were tested by portable spirometer, including mean percentage predicted vital capacity (VC), maximal ventilatory volume (MVV), peak expiratory flow (PEF), forced expiratory volume in the first second (FEV1), forced vital capacity (FVC), forced expiratory flow between 25% and 75% of the FVC (FEF25–75%), and maximum midexpiratory flow (MMEF).
Lung function measurements were performed with the assistance of a trained, skilled physician under supervision according to the American Thoracic Society guidelines [28]. For the purpose of quality assurance, spirograms were reviewed by a pulmonologist before inclusion in the study. The mean percentage predicted value was based on individual age, weight, height, and gender as calculated and adjusted by the spirometer device. Subjects were asked not to smoke for at least 1 h before testing. Additionally, the procedure was explained to participants and they were asked to rest in a sitting position until they felt comfortable. Results of three acceptable maneuvers were performed, and the best of the three readings was used for further analysis.
2.2. Quality Control
Three postgraduate students majored in acupuncture (two of them were investigators and one was a supervisor) who received the formal training of investigating were assigned to conduct the interviews. To ensure the quality of investigation, the supervisor conducted a spot check on the completeness of questionnaires. Ten percent of the respondents were randomly selected and asked to fill in the same questionnaire through a telephone survey to verify whether their responses after 15 days were consistent with those after the first face-to-face interview. It is unacceptable that the deviations were 10% or above.
2.3. Statistical Analysis
The collected data were put into a database by two investigators and analyzed using SPSS statistics version 21.0. The prevalence of respiratory symptoms and diseases was calculated by dividing the number of individuals who responded positive by the number of questionnaires completed. Demographic characteristics are presented as numbers, mean, and standard deviation (SD). Normality was checked firstly for all data of lung function, and then the comparisons of lung function between the exposed and nonexposed group were made by t-test. Data were expressed as mean ± SD. The level of significance was set at P < 0.05. The association between moxa smoke exposure and the respiratory health of the acupuncturist was analyzed by mathematical quantitative regression models.
3. Results
3.1. Incidence of the Acupuncturist's Abnormal Respiratory Symptoms and Respiratory Diseases after MSE
3.1.1. Demographic Characteristics
A total of 825 acupuncture practitioners consented to participate in the study. After logical screening and data cleaning, 803 copies of valid data (322 males and 481 females) were obtained. Table 1 shows the details of the demographic characteristics.
Table 1.
Demographic characteristics.
| Frequency (n), mean ± SD | Constituent ratio (%) | |
|---|---|---|
| Gender | ||
| Male | 322 | 40.1 |
| Female | 481 | 59.9 |
| Age, mean | ||
| Male | 33.05 ± 0.443 | |
| Female | 30.74 ± 0.346 | |
| Age distribution | ||
| 20∼ | 393 | 49.1 |
| 30∼ | 273 | 34.0 |
| 40∼ | 101 | 12.6 |
| 50∼ | 33 | 4.1 |
| Average body mass index (BMI) | ||
| Underweight | 72 | 9.0 |
| Normal | 589 | 73.3 |
| Overweight | 119 | 14.8 |
| Obesity | 23 | 2.9 |
| Degree of education | ||
| Below undergraduate | 44 | 5.5 |
| Undergraduate and above | 759 | 94.5 |
| Ethnic | ||
| Han nationality | 782 | 97.5 |
| Others | 20 | 2.5 |
| Marital status | ||
| Unmarried | 289 | 36 |
| Married | 514 | 64 |
| Smoking status | ||
| Smoking | 92 | 11.5 |
| Used to smoke | 31 | 3.9 |
| Never smoke | 680 | 84.6 |
| Second-hand smoke exposure | ||
| No | 227 | 28.3 |
| Yes | 576 | 71.7 |
SD, standard deviation.
3.1.2. Incidence of Abnormal Respiratory Symptoms and Respiratory Diseases after MSE
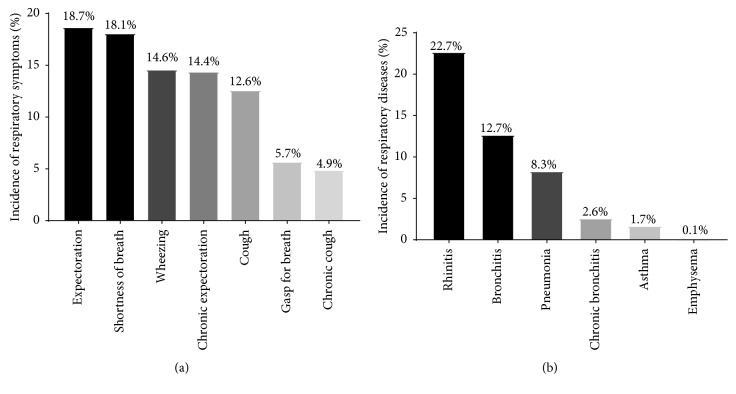
Among the 803 acupuncturists been surveyed, the incidence of expectoration (18.7%) was the highest in abnormal respiratory symptoms, followed by shortness of breath (18.1%), wheezing (14.6%), chronic expectoration (14.4%), cough (12.6%), gasp for breath (5.7%), and chronic cough (4.9%). Among the respiratory diseases, the incidence of rhinitis (22.7%) was the highest, followed by bronchitis (12.7%), pneumonia (8.3%), chronic bronchitis (2.6%), asthma (1.7%), and emphysema (0.1%) (Figure 1).
Figure 1.
Incidence of abnormal respiratory symptoms and respiratory diseases after MSE. (a) Incidence of abnormal respiratory symptoms after MSE. The highest was expectoration (18.7%), followed by shortness of breath (18.1%), wheezing (14.6%), chronic expectoration (14.4%), cough (12.6%), gasp for breath (5.7%), and chronic cough (4.9%). (b) Incidence of respiratory diseases after MSE. The highest was rhinitis (22.7%), followed by bronchitis (12.7%), pneumonia (8.3%), chronic bronchitis (2.6%), asthma (1.7%), and emphysema (0.1%).
3.2. Subgroup Analysis
For the 803 acupuncturists, we split moxa smoke exposure time into total working years and moxa smoke average exposure each day and analyzed the different moxa smoke exposure time and abnormal respiratory symptoms and diseases prevalence. It can be seen from Table 2 that the prevalence of rhinitis in different working years groups and shortness of breath in groups of average exposure each day had a statistically significant difference (P < 0.01).
Table 2.
Subgroup analysis: correlation between different MSE time of acupuncturists and abnormal respiratory symptoms and diseases prevalence.
| Cough (%) | Chronic cough (%) | Expectoration (%) | Chronic expectoration (%) | Wheezing (%) | Gasp for breath (%) | Shortness of breath (%) | Bronchitis (%) | Pneumonia (%) | Rhinitis (%) | Chronic bronchitis (%) | Emphysema (%) | Asthma (%) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Working years (years) | 1∼5 | 13.4 | 4.9 | 19.0 | 14.5 | 14.5 | 4.5 | 17.2 | 11.4 | 8.9 | 19.4 | 2.0 | NA | 1.3 |
| 6∼10 | 8.6 | 3.4 | 19.4 | 13.1 | 14.3 | 7.4 | 21.1 | 15.4 | 6.3 | 24.6 | 1.7 | NA | 1.1 | |
| 11∼20 | 11.1 | 4.4 | 18.9 | 16.7 | 14.4 | 8.9 | 12.2 | 15.6 | 7.8 | 26.7 | 5.6 | NA | 2.2 | |
| 21∼ | 20.7 | 8.6 | 22.4 | 19.0 | 13.8 | 8.6 | 24.1 | 12.1 | 5.3 | 39.7 | 3.4 | 1.7 | 3.9 | |
| P value | 0.091 | 0.456 | 0.940 | 0.692 | 0.997 | 0.206 | 0.181 | 0.472 | 0.600 | 0.004∗ | 0.237 | 0.158 | 0.104 | |
|
| ||||||||||||||
| Average exposure each day (d·person·min) | 1∼30 | 11.3 | 3.9 | 17.8 | 11.7 | 14.8 | 3.9 | 15.7 | 10.0 | 7.0 | 22.2 | 1.3 | NA | 1.3 |
| 31∼120 | 15.6 | 5.0 | 19.4 | 17.5 | 13.1 | 7.5 | 8.1 | 10.0 | 6.3 | 21.9 | 3.1 | NA | 2.5 | |
| 121∼150 | 15.3 | 6.3 | 20.7 | 16.2 | 17.1 | 9.9 | 23.4 | 10.8 | 9.0 | 27.0 | 0.9 | NA | 2.7 | |
| 150∼ | 10.9 | 5.0 | 18.2 | 14.2 | 14.2 | 4.6 | 23.2 | 16.9 | 10.3 | 21.9 | 4.0 | 0.3 | 1.3 | |
| P value | 0.363 | 0.810 | 0.917 | 0.413 | 0.830 | 0.086 | 0.001∗ | 0.053 | 0.389 | 0.704 | 0.159 | 0.646 | 0.637 | |
Notes. Average moxa smoke exposure each day = (average days of moxibustion activities per week (d) ∗average number of patients per day (person) ∗average duration of receiving moxibustion therapy per patient (min)) ÷ 7. ∗P < 0.05 was recognized as significant difference between groups.
3.3. Quantitative Model of the Effect of Moxa Smoke on the Respiratory Health of Acupuncturists
In this study, a regression model was established for the incidence of the top three symptoms from the cross-sectional survey. All predictive variables were entered and passed through logistic stepwise regression (sig < 0.05 into the equation, sig > 0.10 removed from the equation) to obtain the results. From the regression results, the regression equation of the probability of suffering from expectoration/shortness of breath/wheezing and the predictive variable group X could be obtained; that is, P(Y=1 | X) was obtained.
3.3.1. Quantitative Model Prediction of Expectoration
| (1) |
It could be seen from this regression equation that the variables associated with moxa smoke were not contained in the model, which indicated that moxa smoke-related factors were not significant effective factors on the occurrence of expectoration. The bigger the coefficients in front of the variables are, the greater the predictive power of the occurrence of symptoms will be.
3.3.2. Quantitative Model Prediction of Shortness of Breath
| (2) |
The regression model showed that although MSE and the concentration of MSE were included in the regression equation, compared with other factors unrelated to moxa smoke, such as rhinitis, second-hand smoke exposure, and so on, the weight coefficients of the effect on shortness of breath of factors related to moxa smoke were much smaller. That is, it is limited to impact the shortness of breath for factors related to moxa smoke.
3.3.3. Quantitative Model Prediction of Wheezing
| (3) |
It can be seen from this regression that the personal history of pneumonia, rhinitis, chronic bronchitis, smoking, and MSE concentration, and so on have a certain impact on the prediction of wheezing. Among them, the coefficient before the four variables of pneumonia, rhinitis, chronic bronchitis, and smoking was bigger; however, the coefficient before the variable of moxa smoke concentration was smaller. Obviously, among the factors affecting wheezing, factors unrelated to moxa smoke account for a larger proportion.
3.4. Lung Function Comparison of Acupuncturists between Moxa Smoke-Exposed Group and Nonexposed Group
3.4.1. Demographic Characteristics
284 acupuncture practitioners consented to participate in the study. Table 3 shows the demographic characteristics of the survey population. Demographics, including gender (χ2 = 0.127, P > 0.05), age distribution (χ2 = 5.368, P > 0.05), smoking status (χ2 = 0.230, P > 0.05), and BMI (χ2 = 4.638, P > 0.05) as indicated, did not differ between the two groups (P > 0.05).
Table 3.
Demographic characteristics comparison between the moxa smoke-exposed and nonexposed group.
| Exposed group | Nonexposed group | |||
|---|---|---|---|---|
| Male (n, %) | Female (n, %) | Male (n, %) | Female (n, %) | |
| Gender | 73 (51.4) | 69 (48.6) | 73 (51.4) | 69 (48.6) |
| Age distribution | ||||
| 25–34 | 37 (26.1) | 36 (25.4) | 37 (26.1) | 36 (25.4) |
| 35–44 | 22 (15.5) | 20 (14.1) | 22 (15.5) | 20 (14.1) |
| 45–54 | 13 (9.2) | 11 (7.7) | 13 (9.2) | 11 (7.7) |
| ≥55 | 2 (1.4) | 1 (0.7) | 2 (1.4) | 1 (0.7) |
| Smoking status | ||||
| Smoking | 22 (15.5) | 0 | 22 (15.5) | 0 |
| Never smoke | 51 (35.9) | 69 (48.6) | 51 (35.9) | 69 (48.6) |
| BMI | ||||
| Underweight | 2 (1.4) | 8 (5.6) | 5 (3.5) | 14 (9.9) |
| Normal | 37 (26.1) | 53 (37.3) | 38 (26.8) | 43 (30.1) |
| Overweight | 26 (18.3) | 7 (4.9) | 25 (17.6) | 12 (8.5) |
| Obesity | 8 (5.6) | 1 (0.7) | 5 (3.5) | 0 |
3.4.2. Lung Function Comparison between the Moxa Smoke-Exposed and Nonexposed Group
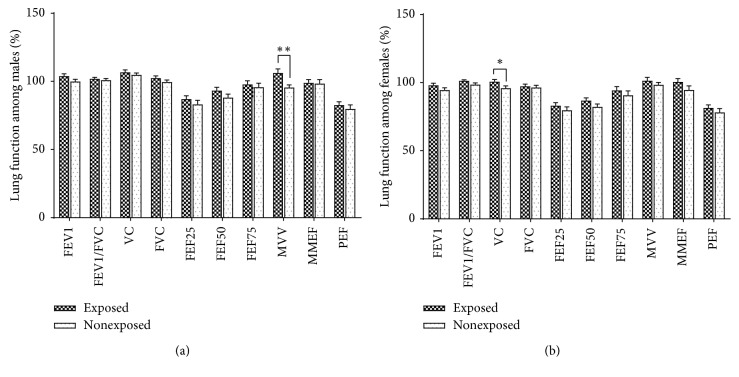
The lung function indexes comparison of the moxa smoke-exposed and nonexposed group is displayed in Table 4. When comparing the two groups, there were no significant differences in the % predicted PEF, large airway function indexes (% predicted FEV1, % predicted FVC, and % predicted FEV1/FVC), and small airway function indexes (% predicted FEF25, % predicted FEF50, % predicted FEF75, and % predicted MMEF). However, the % predicted MVV among males (106.23 ± 2.92 vs. 95.56 ± 1.92, P < 0.01) and % predicted VC among females (100.70 ± 1.59 vs. 95.91 ± 1.61, P < 0.05) between the exposed and nonexposed group had statistical significance, but it did not cause pulmonary ventilation dysfunction (Table 4 and Figure 2).
Table 4.
Lung function comparison between the moxa smoke-exposed and nonexposed group.
| Variable | Exposed group (mean ± SD) | Nonexposed group (mean ± SD) |
|---|---|---|
| Male | ||
| n = 146 | ||
| % predicted FEV1 | 103.98 ± 1.59 | 99.93 ± 1.67 |
| % predicted FEV1/FVC | 101.99 ± 0.94 | 100.92 ± 1.25 |
| % predicted VC | 106.64 ± 1.75 | 104.84 ± 1.35 |
| % predicted FVC | 102.39 ± 1.69 | 99.50 ± 1.59 |
| % predicted FEF25 | 87.11 ± 2.38 | 83.14 ± 3.03 |
| % predicted FEF50 | 93.37 ± 2.36 | 88.13 ± 2.54 |
| % predicted FEF75 | 97.78 ± 2.62 | 95.75 ± 2.99 |
| % predicted MVV | 106.23 ± 2.92∗∗ | 95.56 ± 1.92 |
| % predicted MMEF | 98.89 ± 2.37 | 98.43 ± 2.91 |
| % predicted PEF | 82.70 ± 2.34 | 79.80 ± 3.03 |
|
| ||
| Female | ||
| n = 138 | ||
| % predicted FEV1 | 98.05 ± 1.51 | 94.57 ± 1.57 |
| % predicted FEV1/FVC | 101.25 ± 0.83 | 98.59 ± 1.16 |
| % predicted VC | 100.70 ± 1.59∗ | 95.91 ± 1.61 |
| % predicted FVC | 97.29 ± 1.69 | 96.43 ± 1.60 |
| % predicted FEF25 | 83.11 ± 2.18 | 79.64 ± 2.49 |
| % predicted FEF50 | 86.78 ± 1.98 | 82.15 ± 2.18 |
| % predicted FEF75 | 94.35 ± 2.70 | 90.69 ± 3.27 |
| % predicted MVV | 101.39 ± 2.46 | 98.39 ± 1.85 |
| % predicted MMEF | 100.61 ± 2.35 | 94.67 ± 2.84 |
| % predicted PEF | 81.48 ± 2.25 | 78.22 ± 2.73 |
∗ P < 0.05 and ∗∗P < 0.01 compared with the nonexposed group.
Figure 2.
Lung function comparison between the moxa smoke-exposed and nonexposed group. (a) Male lung function indexes comparison between the exposed and nonexposed group. Compared with the nonexposed group, the % predicted MVV index had statistical significance (106.23 ± 2.92 vs. 95.56 ± 1.92, P < 0.01). (b) Female lung function indexes comparison between the exposed and nonexposed group. Compared with the nonexposed group, the % predicted VC index had statistical significance (100.70 ± 1.59 vs. 95.91 ± 1.61, P < 0.05).
4. Discussion
This epidemiological study combined cross-sectional survey and historical retrospective cohort research, focusing on the clinical safety of moxa smoke among acupuncturists. A mathematical model for predicting the respiratory health of acupuncturists was specially established. This strategy can more comprehensively demonstrate the correlation between MSE and respiratory symptoms and diseases of acupuncturists and quantitatively analyze the effects of moxa smoke on the respiratory health of acupuncturists.
The safety evaluation research of moxa smoke has been deeply studied from the aspects of component analysis, toxicological mechanism, environmental monitoring, environmental toxicity, and so on; however, the conclusions are not unanimous. In order to further search for safety evidence of moxibustion, experts proposed to expand the scope of the investigation, carry out large-scale epidemiological research, and provide direct evidence for clinical safety evaluation of moxa smoke [29]. Additionally, in view of the increasing concern about environmental pollution, little work has been undertaken with regard to whether moxa smoke is harmful to acupuncturists who frequently exposed to moxa smoke. A moxibustion frontline workers investigation is especially necessary. Xu et al. found that cough and dry eyes were the main adverse stimulus reactions after MSE [30]. It was partly in line with the research by our previous investigation [22]. Therefore, the epidemiological investigation on the safety evaluation of moxa smoke should especially focus on the effect of moxa smoke on the respiratory system.
In this epidemiological study, we found that the incidence of expectoration and rhinitis was the most common respiratory symptom and disease after MSE. After subgroup analysis, we observed that except the prevalence of rhinitis and shortness of breath, no statistical difference was found between different MSE time of the acupuncturist and the prevalence of wheezing, chronic expectoration, cough, gasp for breath, chronic cough, bronchitis, pneumonia, chronic bronchitis, asthma, and emphysema. However, the quantitative mathematical model showed that the respiratory health of acupuncturists was more closely related to their own histories of respiratory diseases, family history of respiratory diseases, gender, smoking status, and so on. In some other studies, Li found that long-term inhalation of moxa smoke can lead to increased fatigue among healthcare workers [31]. Han et al. found that high concentration of moxa smoke condensation showed toxicity to induce chromosome damage, which disappears at low concentration [32]. Additionally, at a certain concentration of 9–12 mg/m3, there was no significant effect on people's respiratory rate, blood pressure, heart rhythm, degree of blood oxygen saturation, and other physiological indicators [33]. Considering the complexity of moxibustion process, whether long-term exposure to moxibustion can lead to diseases is controversial. Data from Xu's research demonstrated that the position, duration, distance between moxa and skin, proficiency of doctors, patient conditions, stimulations from smoke, and even the environment of treatment could affect the safety evaluation of moxibustion. The exact causes of most of these adverse events cannot be determined [30]. This is consistent with the opinions of most acupuncture clinical experts. In the course of this study, we learned that most acupuncturists who have worked for more than 20 years and frequently exposed to moxa smoke did not feel any obvious adverse respiratory reaction caused by long-term exposure to moxa smoke.
The historical retrospective cohort research showed that there was no significant difference in the % predicted PEF; in addition, large airway function indexes (% predicted FEV1, % predicted FVC, and % predicted FEV1/FVC) and small airway function indexes (% predicted FEF25, % predicted FEF50, % predicted FEF75, and % predicted MMEF) between the exposed and nonexposed group did not differ, either. Recently, animal research conducted by He et al. also demonstrated that the FEV1/FVC%, inspiratory resistance, and expiratory resistance among each group after 24 weeks of MSE had no difference. It was also mentioned that MSE at low concentrations did not affect the rat's lung function and moxa smoke of low concentrations (27.45 mg/m3) is much higher than that in a regular moxibustion clinic (3.54 mg/m3) [34]. Furthermore, animal research carried out in another study indicated that long-term MSE with medium and high concentration may cause inflammatory changes in the lung and bronchi, but it was not obvious in low concentration. No significant changes were found in the FEV%, FVC%, FEV 0.3/FVC, MMEF%, and PEF% of lung function in the three concentration groups, indicating that long-term continuous moxibustion with high concentration of moxa smoke could cause some pathological changes in lung and bronchial tissues, but it has no definite effect on lung function [35]. This is basically consistent with what we have observed in clinical practice. Strikingly, for different genders, there were some differences between the exposed and nonexposed group. Statistical significances were found in the % predicted MVV index among males and % predicted VC index among females between the exposed and nonexposed group, while it did not cause pulmonary ventilation dysfunction. The reason why the association of lung function differed in men and women is uncertain, but it may relate to their different sensitivities. Additionally, the greater number of men with MSE would provide a more precise measurement of calculated lung function than in women and would be more likely to be able to detect the small differences noted.
In this study, the mathematical model of quantitative analysis was used to evaluate the relationship between MSE and the respiratory health of the acupuncturist. It has not been mentioned in other similar studies. ATS-DLD-78-A was formulated by the American Thoracic Society (ATS) in 1978. It combines the previous investigation contents and experience of the British Medical Research Council (BMRC) and the National Heart and Lung Institute (NHLI), which is widely used in the epidemiological investigation of respiratory diseases in the general population or occupational population [26, 27, 36]. In addition, the cross-sectional survey belongs to the descriptive research method and the cohort study belongs to the analytical research method, while both of them belong to the observational research method in epidemiological research methods. Commonly, cross-sectional studies should be conducted to determine whether exposure factors are associated with certain health outcomes, and then cohort studies should be used to prove the causal relationship between them. It is through cohort studies that the BMRC has confirmed the link between doctors' smoking and lung cancer [37].
Interestingly, there is also reason to suspect that women may respond differently than men when exposed to the same MSE risk factors. In addition, their own history of respiratory diseases had a great influence on the safety evaluation of moxa smoke. Therefore, it is necessary to strengthen the protection of acupuncturists with a history of respiratory diseases in clinic.
There are several limitations in the present study. In view of the weak foundation of epidemiological research on moxa smoke, cross-sectional surveys and historical retrospective cohort studies have been carried out in this study. However, in order to provide more reliable evidence and form a relatively complete epidemiological evidence chain, it is necessary to carry out prospective cohort studies in the next step. At the same time, we did not test the representative objective indicators of the respiratory system in the cross-sectional survey, such as lung function. Additionally, in the process of research, we should also strengthen the consideration of exposure duration, exposure concentration, and so on.
5. Conclusion
Moxa smoke exposure has no significant effect on the respiratory health of acupuncturists. The regression model showed that the weight coefficients of moxa smoke factors were limited. The predictive effect of moxa smoke factors on the respiratory health of acupuncturists was less significant. Our findings therefore support that the occurrence of respiratory symptoms and diseases of acupuncturists was more closely related to their own history of respiratory diseases, family history of respiratory diseases, gender, smoking status, and so on.
Acknowledgments
This work was supported by the National Basic Research Program of China (no. 2015CB554504), National Natural Science Foundation of China (nos. 81873383, 81873386, 81330087, and 81704160), fund of Science and Technology Department of Sichuan Province, China (no. 18YYJC0095), fund of Sichuan Provincial Department of Education, China (no. 18TD0018), and fund of Science and Technology Innovation and Cultivation Project of Sichuan Province, China (no. 2019042).
Contributor Information
Qiaofeng Wu, Email: 20052023@cdutcm.edu.cn.
Shuguang Yu, Email: ysg@cdutcm.edu.cn.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Disclosure
Chang Yu, Ning Zhang, and Weikang Zhu are co-first authors of this study.
Conflicts of Interest
The authors declare that they have no conflicts of interest and no financial interests related to the material of this manuscript.
Authors' Contributions
Chang Yu, Ning Zhang, and Weikang Zhu contributed equally to this work. Shuguang Yu and Qiaofeng Wu conceived and designed the experiments; Chang Yu, Ning Zhang, Weikang Zhu, Yueyue Zhang, Jiao Yang, Yong Wang, Xiaoge Song, Ling Hu, Zijian Wu, Qi Liu, Yong Tang, Qiaofeng Wu, and Shuguang Yu performed the experiments; Chang Yu, Ning Zhang, Qiaofeng Wu, and Shuguang Yu analyzed the images and the data; Shuguang Yu, Qiaofeng Wu, Weikang Zhu, Ning Zhang, and Chang Yu wrote the paper. All the authors approved the final version of the manuscript.
References
- 1.Cardini F., Weixin H. Moxibustion for correction of breech presentation. JAMA. 1998;280(18):1580–1584. doi: 10.1001/jama.280.18.1580. [DOI] [PubMed] [Google Scholar]
- 2.Lee M. S., Choi T.-Y., Kang J. W., Lee B.-J., Ernst E. Moxibustion for treating pain: a systematic review. The American Journal of Chinese Medicine. 2010;38(05):829–838. doi: 10.1142/s0192415x10008275. [DOI] [PubMed] [Google Scholar]
- 3.Xu D.-M., Xu H., Liu J., et al. Effect of thunder-fire moxibustion on pain, quality of life, and tension of multifidus in patients with primary osteoporosis: a randomized controlled trial. Medical Science Monitor. 2018;24:2937–2945. doi: 10.12659/msm.909725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi T.-Y., Lee M. S., Kim J. I., Zaslawski C. Moxibustion for the treatment of osteoarthritis: an updated systematic review and meta-analysis. Maturitas. 2017;100:33–48. doi: 10.1016/j.maturitas.2017.03.314. [DOI] [PubMed] [Google Scholar]
- 5.Zhao J.-M., Wu L.-Y., Liu H.-R., et al. Factorial study of moxibustion in treatment of diarrhea-predominant irritable bowel syndrome. World Journal of Gastroenterology. 2014;20(37):13563–13572. doi: 10.3748/wjg.v20.i37.13563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huanfang X., Baixiao Z., Yingxue C., et al. Effects of moxa smoke on monoamine neurotransmitters in SAMP8 mice. Evidence-Based Complementray and Alternative Medicine. 2013;2013:6. doi: 10.1155/2013/178067.178067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ping L., Pan X. J., Li H., et al. Effects of long-term intervention of moxa smoke on T lymphocyte subsets and CD4∼+CD25∼+Treg in peripheral blood of Wistar rats. Chinese Acupuncture & Moxibustion. 2013;33(2):145–148. [PubMed] [Google Scholar]
- 8.Yang M., Chen X., Bo L., et al. Moxibustion for pain relief in patients with primary dysmenorrhea: a randomized controlled trial. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0170952.e0170952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun Y., Yuan J. M., Yang Z. M. Effectiveness and safety of moxibustion for primary insomnia: a systematic review and meta-analysis. BMC Complementary & Alternative Medicine. 2016;16(1):1–14. doi: 10.1186/s12906-016-1179-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shu Q., Wang H., Litscher D., et al. Acupuncture and moxibustion have different effects on fatigue by regulating the autonomic nervous system: a pilot controlled clinical trial? Akupunktur & Aurikulomedizin. 2016;42(4):p. 11. doi: 10.1007/s15009-016-5429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mao H., Mao J. J., Guo M., et al. Effects of infrared laser moxibustion on cancer-related fatigue: a randomized, double-blind, placebo-controlled trial. Cancer. 2016;122(23):3667–3672. doi: 10.1002/cncr.30189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vas J., Arandaregules J. M., Modesto M., et al. Using moxibustion in primary healthcare to correct non-vertex presentation: a multicentre randomised controlled trial. Acupuncture in Medicine. 2013;31(1):31–38. doi: 10.1136/acupmed-2012-010261. [DOI] [PubMed] [Google Scholar]
- 13.Anastasi J. K., McMahon D. J., Kim G. H. Symptom management for irritable bowel syndrome. Gastroenterology Nursing. 2009;32(4):243–255. doi: 10.1097/sga.0b013e3181b2c920. [DOI] [PubMed] [Google Scholar]
- 14.Stein D. J. Massage acupuncture, moxibustion, and other forms of complementary and alternative medicine in inflammatory bowel disease. Gastroenterology Clinics of North America. 2017;46(4):875–880. doi: 10.1016/j.gtc.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 15.Satoru Y., Nobuo A. The practical use of acupuncture and moxibustion treatment cooperated with neurological practice. Rinsho Shinkeigaku. 2012;52(11):1287–1279. doi: 10.5692/clinicalneurol.52.1287. [DOI] [PubMed] [Google Scholar]
- 16.Lui K. H., Bandowe B. A. M., Ho S. S. H., et al. Characterization of chemical components and bioreactivity of fine particulate matter (PM 2.5) during incense burning. Environmental Pollution. 2016;213:524–532. doi: 10.1016/j.envpol.2016.02.053. [DOI] [PubMed] [Google Scholar]
- 17.Kwon O. S., Cho S. J., Choi K. H., et al. Safety recommendations for moxa use based on the concentration of noxious substances produced during commercial indirect moxibustion. Acupuncture in Medicine. 2017;35(2):93–99. doi: 10.1136/acupmed-2016-011105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu C., Wu Q. F., Tang Y., Yu S. G. Influence of moxa smoke on indoor air quality and strategies for its control. Acupuncture Research. 2018;43(2):103–109. doi: 10.13702/j.1000-0607.170840. [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto T., Katai S., Namiki T. Safety of smoke generated by Japanese moxa upon combustion. European Journal of Integrative Medicine. 2016;8(4):414–422. doi: 10.1016/j.eujim.2016.03.005. [DOI] [Google Scholar]
- 20.Duan W., Zijian W. U., Ling H. U., et al. Safety test of air quality in simulated moxibustion clinic. Chinese Acupuncture & Moxibustion. 2016;36(6):637–640. doi: 10.13703/j.0255-2930.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 21.Wheeler J., Coppock B., Chen C. Does the burning of moxa (Artemisia vulgaris) in traditional Chinese medicine constitute a health hazard. Acupuncture in Medicine. 2009;27(1):16–20. doi: 10.1136/aim.2009.000422. [DOI] [PubMed] [Google Scholar]
- 22.Yu C., Wang X., Yang H., et al. Small sample size epidemiological survey of the time-related exposure reaction of acupuncturists under the moxa-smoke environment. Journal of Chengdu University of TCM. 2015;38(4):6–9. [Google Scholar]
- 23.Wang X., Yu C., Tang Y., et al. Symptoms of long-term exposure to moxa smoke in acupuncturists: a correlation analysis. Journal of Traditional Chinese Medicine. 2018;38(1):132–138. doi: 10.1016/j.jtcm.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Wang X. M., Wu L. Y., Liu Y. N., et al. A survey of the body’s response to clinical exposure to moxa smoke. Proceedings of the International Conference Industrial Technology and Management; March 2015; Tianjin, China. pp. 1055–1060. [DOI] [Google Scholar]
- 25.Cui Y., Zhao B., Huang Y., et al. Effects of moxa (Folium Artemisiae argyi) smoke exposure on heart rate and heart rate variability in healthy young adults: a randomized, controlled human study. Evidence-Based Complementary and Alternative Medicine. 2013;2013:10. doi: 10.1155/2013/510318.510318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang J., Li S., Wang S., Shang K. Effects of long-term dust exposure on human respiratory system health in minqin county, China. Archives of Environmental & Occupational Health. 2015;70(4):225–231. doi: 10.1080/19338244.2013.872077. [DOI] [PubMed] [Google Scholar]
- 27.Beckett W. S., Pope C. A., Xu X. P., Christiani D. C. Women’s respiratory health in the cotton textile industry: an analysis of respiratory symptoms in 973 non-smoking female workers. Occupational and Environmental Medicine. 1994;51(1):14–18. doi: 10.1136/oem.51.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Listed N. Standardization of spirometry, 1994 update. American Thoracic Society. American Journal of Respiratory and Critical Care Medicine. 1995;152(3):1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 29.Wu H., Xiaopeng M. A., Zhou C., Bao C., Dou C. Current research status and developing strategy of moxibustion. World Chinese Medicine. 2013;8:845–851. [Google Scholar]
- 30.Xu J., Deng H., Shen X. Safety of moxibustion: a systematic review of case reports. Evidence-Based Complementary and Alternative Medicine. 2014;2014:10. doi: 10.1155/2014/783704.783704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li H. Investigation of Medical Workers’ Health Condition of Chengdu Who Do Inhalation of Moxa’s Smoke Frequently. Chengdu, China: Chengdu University of Traditional Chinese Medicine; 2012. [Google Scholar]
- 32.Han L., Hu H., Yang J., et al. Micronucleus in vitro induced by inhalable particulate matters in moxa smoke. Chinese Acupuncture & Moxibustion. 2016;36(5):499–503. [PubMed] [Google Scholar]
- 33.Huang Y., Li J., Cui Y., Liu J., Zhao B. The effect of moxa smoke on blood pressure, respiratory rate, heart rate, ECG and oxygen saturation of healthy adults. World Chinese Medicine. 2014;9(6):784–787. [Google Scholar]
- 34.He R., Han L., Liu P., et al. Lung function decline after 24 weeks of moxa smoke exposure in rats. Evidence-Based Complementary and Alternative Medicine. 2019;2019:7. doi: 10.1155/2019/9236742.9236742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duan W. X., Wu Z. Z., Hu L., et al. Effects of different concentrations of moxa-smoke on lung function and TNF-α and IL-1β in serum and lung tissue in normal rats. Acupuncture Research. 2018;43(2):98–103. doi: 10.13702/j.1000-0607.170854. [DOI] [PubMed] [Google Scholar]
- 36.Wong C. M., Hu Z. G., Lam T. H., Hedley A. J., Peters J. Effects of ambient air pollution and environmental tobacco smoke on respiratory health of non-smoking women in Hong Kong. International Journal of Epidemiology. 1999;28(5):859–864. doi: 10.1093/ije/28.5.859. [DOI] [PubMed] [Google Scholar]
- 37.Stevens R. G., Moolgavkar S. H. A cohort analysis of lung cancer and smoking in British males1. American Journal of Epidemiology. 1984;119(4):624–641. doi: 10.1093/oxfordjournals.aje.a113779. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.