Abstract
Ventricular remodelling can make the heart more susceptible to ventricular arrhythmias like torsades de pointes. Understanding the underlying mechanisms of initiation of ventricular arrhythmias and the determining factors for its severity has the potential to uncover new interventions. Beat-to-beat variation of repolarisation, quantified as short-term variability of repolarisation (STV), has been identified as an important factor contributing to arrhythmogenesis. This article provides an overview of experimental data about STV in relation to the initiation of torsades de pointes in a canine model of complete chronic atrioventricular block susceptible to torsades de pointes arrhythmias. Furthermore, it explores STV in relation to the severity of the arrhythmic outcome.
Keywords: Short-term variability of repolarisation, beat-to-beat variation of repolarisation, ventricular arrhythmias, torsades de pointes
The plasticity of the heart enables it to adapt to certain pathological insults and to maintain the cardiac output necessary to satisfy the metabolic requirements of the body.[1] Although beneficial at first, this process of ventricular remodelling can have detrimental effects on cardiac function and contribute to arrhythmogenesis.[2] Sudden cardiac death due to ventricular tachyarrhythmias accounts for up to 60% of cardiovascular deaths.[3] Despite improvements in cardiovascular risk management and therapeutic strategies for heart failure, sudden cardiac death remains an important healthcare issue.[4] A considerable number of patients rely on the ICD for the prevention of sudden cardiac death.[5] While ICD therapy is highly effective in ending ventricular arrhythmias, it does not prevent malignant arrhythmias from occurring.[6–8] Experiencing ICD-shocks – either appropriate or inappropriate – can result in psychosocial distress for the patient and a reduced quality of life.[9,10] Additional treatment, such as antiarrhythmic drugs or radio frequency ablation, are often used as adjunctive therapy to reduce the number of ICD-shocks, but both therapeutic modalities expose the patient to potentially adverse effects.[11,12] This underscores the importance of finding alternative therapies that intervene to prevent the arrhythmia (and concomitant shock therapy).
Beat-to-beat variation of repolarisation (BVR) quantified as short-term variability of repolarisation (STV), has been studied extensively in relation to arrhythmogenesis in the chronic complete atrioventricular block (CAVB) dog model.[13] STV has been proposed as a novel electrophysiological parameter for the monitoring of imminent ventricular arrhythmias.[14,15] This review explains the influence of ventricular remodelling on BVR and how it can lead to a higher susceptibility for arrhythmias. The severity of arrhythmias is diverse; therefore, this review also explores the relation of STV to the severity of the arrhythmic outcome. It will also discuss the clinical implications of STV.
Ventricular Remodelling in the Chronic Complete Atrioventricular Block Dog Model
The CAVB dog model is a widely used animal model to study ventricular remodelling and its relation with ventricular arrhythmias.[16–18] It is a model of compensated biventricular hypertrophy with a long QT phenotype and is reproducibly inducible for torsades de pointes (TdP) arrhythmias when challenged with a delayed rectifier outward potassium current (IKr)-blocker such as dofetilide.[19–21] Creation of complete atrioventricular block, by means of His bundle ablation, forces the ventricles to activate from an infranodal focus of the conduction system resulting in a slow idioventricular rhythm. As a result of this bradycardia, the cardiac output drops abruptly and there is volume overload. The decrease in cardiac output and the altered asynchronous activation form insults to the heart and trigger electrical, contractile and structural ventricular remodelling as compensatory mechanisms.
Whereas structural remodelling forms slowly and reaches a stable condition between 12 and 16 weeks of CAVB, electrical and contractile remodelling are present from 2 weeks of CAVB and coincide with the inducibility of TdP arrhythmias in the CAVB dog model.[13,22–28] The most striking feature of electrical remodelling is the prolongation of repolarisation time.[15,18,28] On a cellular level, this is explained by the downregulation of the slow and rapid components of the delayed rectifier outward potassium currents (IKs and IKr).[29] The prolonged action potential duration (APD) provides more time for the contractile process of the cardiomyocyte. In combination with altered Ca2+ handling this leads to Ca2+ overload in the CAVB dog model.[30–32] In an electrically remodelled heart, the Ca2+ overload can lead to early after depolarisations (EADs) that can trigger TdP arrhythmias in this animal model.
Repolarisation Reserve is Reflected by Beat-to-beat Variation of Repolarisation
The normal cardiomyocyte possesses a redundancy in repolarising currents, enabling it to withstand internal and external challenging factors on the repolarisation, which is also called the repolarisation reserve.[33] The duration of repolarisation is within normal limits and fluctuates slightly between subsequent beats. Repolarisation reserve diminishes due to electrical remodelling, causing the heart to become more susceptible to repolarisation-related ventricular arrhythmia. This phenomenon is reflected by the increased temporal dispersion of repolarisation, or BVR, which can be quantified as STV. This should not be confused with heart rate variability (HRV), which reflects the balance of the activity of the autonomic nervous system and can serve as an indicator of cardiovascular integrity and prognosis.[34,35]
In a Poincaré plot, the repolarisation duration of a predetermined number of consecutive beats (n=31) is plotted against the duration of each previous beat (Figure 1). The difference in repolarisation between two subsequent beats is reported by each deviation from the line of identity. The average deviation of repolarisation from the line of identity for a number of beats reports STV, expressed in milliseconds (ms). STV is calculated according to the formula ![]() , where D represents repolarisation duration and N is the total number of beats.[36]
, where D represents repolarisation duration and N is the total number of beats.[36]
Figure 1: Poincaré Plot Depicting Left Ventricular Monophasic Action Potential Durations.
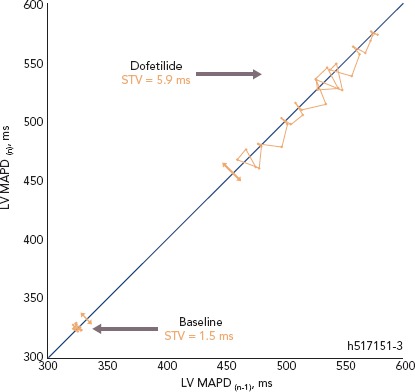
Poincaré plot depicting 31 consecutive left ventricular monophasic action potential durations in milliseconds at baseline and after infusion of dofetilide but prior to the first ectopic beat. LV = left ventricular; h517151-3 = dog number; MAPD = monophasic action potential duration; STV = short-term variability of repolarisation.
Increased Temporal Dispersion of Repolarisation as a Substrate and Trigger for Torsades de Pointes
There are two fundamental requirements for ventricular arrhythmias such as TdP. The first being the need for a substrate that renders the heart susceptible to the development of arrhythmias. Electrical remodelling in the CAVB dog model diminishes the repolarisation reserve, thereby forming part of the substrate. During sinus rhythm and acute AV-block in the absence of remodelling, TdP arrhythmias cannot be induced when the animals are challenged with dofetilide.[13,26] It is also evident that STV is higher at baseline in CAVB dogs where TdPs can be induced repetitively compared with resistant CAVB dogs.[37,38] Sudden cardiac death can occur in the canine CAVB model and is associated with a higher STV at baseline.[39] This indicates that proarrhythmic ventricular remodelling is associated with an increased STVbaseline which reflects the decreased repolarisation reserve.
The second fundamental for ventricular arrhythmias is the presence of a trigger. Temporal dispersion of repolarisation also fulfils this second role. Alongside ventricular remodelling, anaesthesia and bradycardia further challenge the repolarisation reserve in the canine CAVB model.[14,21,40] When the ‘final hit’ in the form of an IKr-blocker is infused, the absolute value of STV increases abruptly in the minutes preceding a storm of TdPs (STVarrhythmic).[13–15,36,41,42] Moreover, STV has been shown to be a superior repolarisation parameter to predict the imminent proarrhythmic outcome, compared with repolarisation prolongation and interventricular dispersion of repolarisation.[25,40]
Relation of Short-term Variability of Repolarisation to Severity of Arrhythmic Outcome
The arrhythmic outcome in the inducible CAVB dogs is diverse and can range from self-terminating TdPs to TdPs requiring defibrillation for termination. Therefore, we investigated the relation of STV to the severity of the arrhythmic outcome. Articles studying STV in relation to TdP arrhythmias upon dofetilide challenge in the CAVB dog model at our lab were considered for pooled analysis (n=28). Only original articles that reported STV of the left ventricular monophasic action potential duration (STVLV, MAPD) in idioventricular rhythm-remodelled CAVB dogs and that used a standard anaesthetic regimen were considered. The QT-interval was measured on lead II of the ECG and corrected for heart rate using the van de Water formula or the Bazett formula.[43,44] Original data from the remaining 11 articles was obtained. After removing duplicates, data from 64 inducible dogs was pooled.
Definition of Inducibility and Quantification of Arrhythmia Severity
A decreased repolarisation reserve enables the occurrence of single ectopic beats (sEB), multiple ectopic beats (mEB), and TdPs. A TdP has been defined as ≥5 consecutive EBs with a twisting QRS vector around the isoelectric line. A dog is considered to be inducible when ≥3 TdPs occur within 10 minutes after the start of infusion with an IKr-blocker such as dofetilide.[41] When a TdP lasts for 10–12 seconds, defibrillation with thoracic patches is performed to restore normal heart rhythm.
The arrhythmia score (AS) has been developed in an effort to quantify the severity of the arrhythmias.[45] The AS is calculated by averaging the three most severe arrhythmias that occur during 10 minutes from the start of dofetilide infusion. Figures 2A and B show how the individual arrhythmic event is scored: 1 point is given by default for each regular beat in the absence of arrhythmic events. An ectopic beat or run of ectopic beats is scored with 1 additional point per ectopic beat to a maximum of 50. Hence, 2 points for sEB, 3–5 points for mEB, and 6–50 points for TdP. A TdP requiring defibrillation is perceived as the most severe individual arrhythmic episode in the CAVB dog model and is applied for TdPs that last ≥10 seconds and contain ≥50 beats. Therefore, defibrillation is scored with 50, 75 or 100 points depending on the number of consecutive defibrillations necessary to terminate one TdP episode (1, 2, ≥3, respectively).[40,46]
Figure 2: Quantification of Arrhythmia Severity During 10 Minutes Using the Arrhythmia Score.
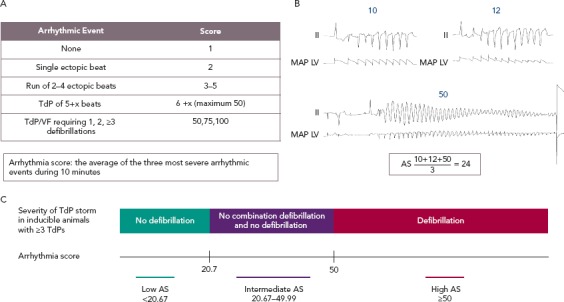
A. Scoring of the arrhythmic events using the AS. B. Example of calculation of the AS using ECG lead II and the monophasic action potential of the left ventricle. C. Categories of severity of a torsades de pointes storm and the corresponding AS in inducible animals based on the necessity of defibrillation for termination. AS = Arrhythmia score; LV = left ventricle; MAP = monophasic action potential; TdP = torsades de pointes. Source: Stams et al. 2013.[45]
Figure 2C illustrates how the AS corresponds with the severity of a storm of TdPs in inducible animals with ≥3 TdPs. We consider a storm of self-terminating TdPs less severe than a storm of TdPs requiring at least one defibrillation. In an inducible animal with one defibrillated TdP (50 points), the lowest possible AS is 20.67 when the other two TdPs have the minimal duration corresponding to 6 points each (![]() ).
).
Therefore, all inducible animals with an AS ≤20.67 only have self-terminating TdPs and are part of the low AS group. An example of ECG tracings of an inducible animal with no defibrillations is shown in Figure 3A, where the AS is 16.3. The most severe storm of TdPs consists of TdPs requiring defibrillation (in the high AS group). The AS is 50, when all three most severe arrhythmic events require defibrillation (Figure 3B). However, an average of 50 points can also be obtained with three long-lasting TdPs of ≥49 beats that terminate spontaneously before 10 seconds. The AS can reach a maximum of 100 points when the three most severe arrhythmic events require ≥3 consecutive defibrillations for termination. A combination of self-terminating and defibrillated arrhythmias corresponds to an AS of ≥20.67 and <50. An example in Figure 2B shows the intermediate AS group.
Figure 3: Examples of the Three Most Severe Arrhythmic Episodes in Two Inducible Chronic Atrioventricular Block Dogs.
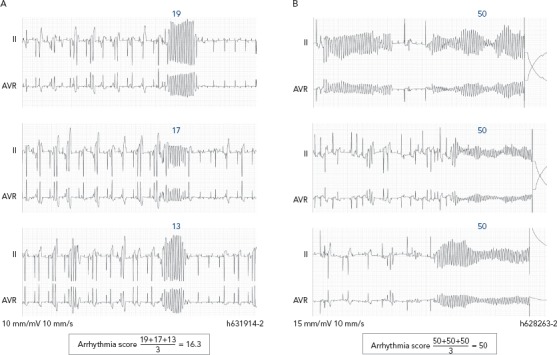
Examples of the three most severe arrhythmic episodes within 10 minutes in two inducible chronic atrioventricular block dogs, one representative of a low arrhythmia score (A) and another of a high arrhythmia score (B). h631914-2 and h628263-2 both refer to the dog numbers.
STV and QTc Increase Before Torsades de Pointes
It has been described previously that STVarrhythmic is higher compared with STVbaseline in inducible CAVB dogs. As shown in Figure 4A, STVarrhythmic is significantly increased compared with STVbaseline in the three different AS groups. STV increases from 0.98±0.72 to 1.71 ± 1.18 (p=0.0020) in the low AS group, from 1.34 ± 0.61 to 3.78 ± 2.02 (p<0.0001) in the intermediate AS group, and from 1.37 ± 0.63 to 3.55 ± 1.40 (p<0.0001) in the high AS group (Table 1). STVbaseline values do not differ between the three AS groups. Whereas previous research reports that STVbaseline is significantly higher in inducible dogs compared with non-inducible dogs, STVbaseline does not seem to contribute to the severity of the arrhythmias in inducible dogs.[37,38] STVarrhythmic shows a trend for higher values in the group with an intermediate and high AS compared with the low AS group, but fails to reach statistical significance. Arrhythmic QTc is also significantly increased compared with QTc baseline in the three AS groups (Figure 4B and Table 1). Neither the values of QTc baseline nor the values of arrhythmic QTc differ between AS groups.
Figure 4: Short-term Variability of Repolarisation of the Left Ventricular Monophasic Action Potential Duration in Relation to the Arrhythmic Outcome in the Inducible Chronic Atrioventricular Block Dog Model.
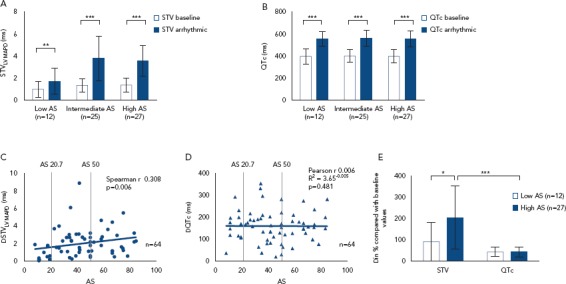
A. STVbaseline and STVarrhythmic categorised by AS. B. Baseline QTc and arrhythmic QTc categorised by AS. C. Correlation between ΔSTV and AS. D. Correlation between ΔQTc and AS. E) Relative ΔSTV and ΔQTc grouped by AS. Low AS <20.67 and high AS ≥50. *p<0.05, **p<0.01, ***p<0.0001. AS = arrhythmia score; LV = left ventricular; MAPD = monophasic action potential duration; LV = left ventricular; MAPD = monophasic action potential duration; STV = short-term variability of repolarisation.
Source: Oosterhoff et al. 2010;[14] Sprenkeler et al. 2018;[26] Bossu et al. 2017[40]; Van de Water et al. 1989;[43] Sandhu et al. 2008;[67] Bossu et al. 2018;[68] Ji et al. 2017;[69] Varkevisser et al. 2013;[70] Bourgonje et al. 2012;[71] Stams et al. 2011;[72] Oros et al. 2010.[73]
Table 1: Pooled Experimental Data of Short-term Variability (STV) of Repolarisation of the Left Ventricular Monophasic Action Potential Duration and QTc Prior to Torsades de Pointes STVarrhythmic and Arrhythmic QTc, Compared With Baseline in the Chronic Atrioventricular Block Dog Model.
| STVLV, MAPD (ms) | ΔSTV | QTc (ms) | ΔQTc | ||||||
| Baseline | Arrhythmic | Absolute (ms) | Relative (%) | Baseline | Arrhythmic | Absolute (ms) | Relative (%) | ||
| Overall | 1.28 ± 0.65 | 3.30 ± 1.79** | 2.01 ± 1.59 | 182.8 ± 145.3 | 398.60 ± 59.80 | 557.6 ± 69.43** | 159.1 ± 72.22 | 42.04 ± 22.87 | |
| AS | Low (n=12) | 0.98 ± 0.72 | 1.71 ± 1.18* | 0.73 ± 0.70 | 90.83 ± 90.28 | 397.20 ± 68.89 | 555.1 ± 68.52** | 157.9 ± 67.60 | 42.03 ± 21.95 |
| Intermediate (n=25) | 1.34 ± 0.61 | 3.78 ± 2.02** | 2.44 ± 1.87 | 211.10 ± 155.10*** | 400.60 ± 57.82 | 562 ± 70.20** | 161.60 ± 82.22 | 42.83 ± 26.67**** | |
| High (n=27) | 1.37 ± 0.63 | 3.55 ±1.40** | 2.18 ± 1.32 | 197.50 ± 143.60*** | 397.40 ± 59.70 | 554.6 ±71.49** | 157.2 ± 66.73 | 41.31 ± 20.14**** |
Data are expressed as mean ± standard deviation. *p<0.01, **p<0.0001 compared with the same electrophysiological parameter in baseline, ***p<0.05 compared with the same electrophysiological parameter in the low arrhythmia score group, ****p<0.0001 compared to relative ΔSTV of the same arrhythmia score group. All comparisons between the same electrophysiological parameter were not significant between the intermediate and high arrhythmia score group. Statistics between STV and QTc have not been calculated for absolute Δ, because these are not comparable. CAVB = chronic atrioventricular block; LV = left ventricular; MAPD = monophasic action potential duration; STV = short-term variability of repolarisation.
The Rise in Short-term Variability of Repolarisation is Associated with the Severity of the Arrhythmic Outcome
Figure 4A indicates that the change from STVbaseline to STVarrhythmic (ΔSTVLV, MAPD) is greater in the intermediate and high AS groups compared with the low AS group. Further quantification of this observation shows a significant correlation between ΔSTVLV, MAPD and the AS (Spearman r 0.308, p=0.006; Figure 4C), indicating an association between the increment of STV and the severity of the arrhythmic outcome. This correlation is absent for the change in QTc (ΔQTc), whereby QTc is equally prolonged in dogs with a low AS and a high AS (Pearson r 0.006, R2 3.65-0.005, p=0.481; Figure 4D).
The AS has a heterogeneous nature, in the intermediate AS group the same AS score can be the result of a diverse combination in severity of arrhythmias. The group with an intermediate AS shows a big variation in ΔSTVLV, MAPD with some outliers (Figure 2C and Figure 4C). Therefore, the relative ΔSTVLV, MAPD and ΔQTc have been compared in dogs with a low AS and high AS (Figure 4E). The dogs discussed in this review with an AS score of 50 all had ≥3TdPs requiring defibrillation. Relative ΔSTVLV, MAPD increases with 90.83 ± 90.28% in the low AS group and with 197.50 ± 143.60% in the high AS group (p=0.0414). This discriminative capacity is not found in the relative ΔQTc, which prolongs almost equally with 42.03 ± 21.95% in the low AS group and 41.31 ± 20.14% in the high AS group (p>0.9999). In the high AS group, the relative ΔSTVLV, MAPD is significantly higher than the relative ΔQTc (p<0.0001) (Table 1, Figure 4E).
Severity of Torsades de Pointes
A higher ΔSTV contributes to the severity of a storm of TdPs, but is unlikely to be determinant for the duration of an individual TdP. The mechanism of initiation of an individual TdP episode has been attributed to EAD-dependent focal activity due to reduced repolarisation reserve.[47–54] The significant increase in STV before a storm of TdPs can therefore be expected. However, the mechanism underlying the perpetuation of a TdP episode is still under debate. Extensive mapping experiments have been performed in animal hearts, whereby on the one hand focal activity has been proposed as the dominant underlying mechanism.[48,52–56] On the other hand, it has been suggested that nonstationary re-entry perpetuates TdPs.[50,51,57] Others have observed both mechanisms to be present when TdP is perpetuated.[47,49] These different observations may be due to the moment of measurement during a TdP. A TdP can deteriorate into ventricular fibrillation, which is most likely to be driven by re-entry. Therefore Boulaksil et al. clearly defined the moment of measurement, whereupon they based the conclusion that focal activity is the dominant mechanism in the perpetuation of self-terminating TdPs and during the early phase of a TdP episode, indicating triggered activity.[58] Vandersickel et al. confirmed that all observed TdPs were perpetuated by focal activity in the early phase and in the case of short-lasting TdPs, but added that the longer-lasting TdP episodes were re-entry driven.[59]
It is important to note that the STV measured by the studies incorporated in Figure 4 preceded the first arrhythmic episode of a storm of sEB, mEB, or TdP and was correlated to the AS that was observed for 10 minutes. A higher ΔSTV is therefore not associated with a longer individual episode of a TdP, but rather with the severity of the complete electrical storm of TdPs in a short period of time. The positive correlation between ΔSTV and the AS can be explained in several ways. First of all, a more severely decreased repolarisation reserve reflected by a higher ΔSTV, may give rise to more EADs and therefore more focal activity. The bigger amount of focal activity can in turn simply improve the odds that a proportion of the focal activity is perpetuated into a long-lasting TdP. Second, the circumstances during the early phase of a TdP may influence the perpetuation and/or degeneration into ventricular fibrillation. The increased repolarisation lability and propensity for competing foci may create a more chaotic activation pattern, and the consequences on the initiation of re-entry have not yet been explored.
One of the factors that is believed to promote the initiation of re-entry is spatial dispersion of repolarisation. However, Dunnink et al. demonstrated that spatial dispersion of repolarisation contributes to the initiation and early phase continuation of a TdP, whereby focal activity was the underlying mechanism. In mapping experiments in the CAVB dog, sEBs and the first beat of the TdP arose at the site of maximal dispersion of repolarisation and demonstrated a focal origin. The TdPs continued with a second focal beat that arose from a different location in a region of maximal repolarisation heterogeneity.[56] The complex interplay between temporal and spatial dispersion of repolarisation in relation to arrhythmogenesis needs further investigation.
Clinical Implications
The observed change in STV before arrhythmia, and especially the correlation between ΔSTV and severity of the imminent arrhythmic outcome, confirm the potential of STV as a possible electrophysiological marker for the monitoring of imminent ventricular arrhythmias. Data from the canine CAVB model cannot readily be extrapolated to humans, therefore clinical studies need to further investigate STVarrhythmic. In this review STV was measured with an intracardiac MAP-catheter in the left ventricle. There are also other modalities to measure STV that can be applied in humans more easily, namely the QT-interval on the non-invasive ECG and the activation recovery interval on intracardiac electrogram (EGM) in devices. The ECG has been used in descriptive studies in humans to study if STVbaseline of the QT-interval can identify the individual at risk for repolarisation-dependent ventricular arrhythmias.[60–64] However, longer registrations are necessary to capture sustained ventricular arrhythmias in patients to investigate STVarrhythmic. The EGM is a promising candidate for the continuous monitoring of STV and to study STV before arrhythmia. In the CAVB dog, the STV can be reliably derived from the activation recovery interval of the EGM in the right ventricle (RV), and it increases before TdP.[15] Other repolarisation parameters have been studied in patients on the RV EGM, which indicates that it is a feasible method to further investigate STVarrhythmic in patients.[65–67]
Conclusion
Temporal dispersion of repolarisation, quantified as STV, plays an important role in the initiation of ventricular arrhythmias like TdP. A sudden increase in STV precedes imminent TdP in the canine CAVB model. A higher increment of STV compared with baseline is associated with a more severe arrhythmic outcome, in contrast to QTc. These findings confirm the potential of STV for the monitoring of imminent pro-arrhythmic risk of the ventricles and create new options for interventions.
Clinical Perspective
Beat-to-beat variation of repolarisation quantified as short-term variability (STV) of repolarisation reflects the diminished repolarisation reserve of the heart.
The extent of the increase in STV before ventricular arrhythmia is correlated to the severity of the arrhythmia in the complete chronic AV-block dog model, in contrast to the change in QTc.
STV is a promising electrophysiological parameter for the monitoring of imminent proarrhythmic risk, further clinical studies are needed to confirm this potential.
References
- 1.Hill JA, Olson EN. Cardiac plasticity. N Engl J Med. 2008;358:1370–80. doi: 10.1056/NEJMra072139. [DOI] [PubMed] [Google Scholar]
- 2.Konstam MA, Kramer DG, Patel AR et al. Left ventricular remodeling in heart failure current concepts in clinical significance and assessment. J Am Coll Cardiol Cardiovasc Imaging. 2011;4:98–108. doi: 10.1016/j.jcmg.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Adabag AS, Luepker RV, Roger VL et al. Sudden cardiac death: epidemiology and risk factors. Nat Rev Cardiol. 2010;7:216–25. doi: 10.1038/nrcardio.2010.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2013;125:620–37. doi: 10.1161/CIRCULATIONAHA.111.023838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ponikowski P, Voors AA, Anker SD et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 6.Connolly SJ, Hallstrom AP, Cappato R et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. Eur Heart J. 2000;21:2071–8. doi: 10.1053/euhj.2000.2476. [DOI] [PubMed] [Google Scholar]
- 7.Moss AJ, Zareba W, Hall WJ et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–83. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 8.Bardy GH, Lee KL, Mark DB et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–37. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 9.Sola CL, Bostwick JM. Implantable cardioverter-defibrillators, induced anxiety, and quality of life. Mayo Clin Proc. 2005;80:232–7. doi: 10.4065/80.2.232. [DOI] [PubMed] [Google Scholar]
- 10.Tomzik J, Koltermann KC, Zabel M Quality of life in patients with an implantable cardioverter defibrillator: a systematic review. Front Cardiovasc Med. 2015. pp. 2–34. [DOI] [PMC free article] [PubMed]
- 11.van Herendael H, Pinter A, Ahmad K et al. Role of antiarrhythmic drugs in patients with implantable cardioverter defibrillators. Europace. 2010;12:618–25. doi: 10.1093/europace/euq073. [DOI] [PubMed] [Google Scholar]
- 12.Reddy VY, Reynolds MR, Neuzil P Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007. pp. 2657–65. [DOI] [PMC free article] [PubMed]
- 13.Thomsen MB, Oros A, Schoenmakers M et al. Pro-arrhythmic electrical remodelling is associated with increased beat-to-beat variability of repolarisation. Cardiovasc Res. 2007;73:521–30. doi: 10.1016/j.cardiores.2006.11.025. [DOI] [PubMed] [Google Scholar]
- 14.Oosterhoff P, Thomsen MB, Maas JN et al. High-rate pacing reduces variability of repolarization and prevents repolarization-dependent arrhythmias in dogs with chronic AV block. J Cardiovasc Electrophysiol. 2010;21:1384–91. doi: 10.1111/j.1540-8167.2010.01824.x. [DOI] [PubMed] [Google Scholar]
- 15.Wijers SC, Sprenkeler DJ, Bossu A et al. Beat-to-beat variations in activation-recovery interval derived from the right ventricular electrogram can monitor arrhythmic risk under anesthetic and awake conditions in the canine chronic atrioventricular block model. Heart Rhythm. 2018;15:442–8. doi: 10.1016/j.hrthm.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Oros A, Beekman JD, Vos MA. The canine model with chronic, complete atrio-ventricular block. Pharmacol Ther. 2008;119:168–78. doi: 10.1016/j.pharmthera.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Zhou S, Jung B, Tan AY et al. Spontaneous stellate ganglion nerve activity and ventricular arrhythmia in a canine model of sudden death. Heart Rhythm. 2008;5:131–9. doi: 10.1016/j.hrthm.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Wada T, Ohara H, Nakamura Y et al. Impacts of surgically performed renal denervation on the cardiovascular and electrophysiological variables in the chronic atrioventricular block dogs. Circ J. 2016;80:1556–63. doi: 10.1253/circj.CJ-16-0198. [DOI] [PubMed] [Google Scholar]
- 19.Volders PG, Sipido K, Vos MA et al. Cellular basis of biventricular hypertrophy and arrhythmogenesis in dogs with chronic complete atrioventricular block and acquired torsade de pointes. Circulation. 1998;98:1136–47. doi: 10.1161/01.cir.98.11.1136. [DOI] [PubMed] [Google Scholar]
- 20.Vos MA, de Groot SH, Verduyn SC et al. Enhanced susceptibility for acquired torsade de pointes arrhythmias in the dog with chronic, complete AV block is related to cardiac hypertrophy and electrical remodeling. Circulation. 1998;98:1125–35. doi: 10.1161/01.cir.98.11.1125. [DOI] [PubMed] [Google Scholar]
- 21.Dunnink A, Sharif S, Oosterhoff P et al. Anesthesia and arrhythmogenesis in the chronic atrioventricular block dog model. J Cardiovasc Pharmacol. 2010;55:601–8. doi: 10.1097/FJC.0b013e3181da7768. [DOI] [PubMed] [Google Scholar]
- 22.Schoenmakers M, Ramakers C, van Opstal JM et al. Asynchronous development of electrical remodeling and cardiac hypertrophy in the complete AV block dog. Cardiovasc Res. 2003;59:351–9. doi: 10.1016/s0008-6363(03)00430-9. [DOI] [PubMed] [Google Scholar]
- 23.Verduyn SC, Ramakers C, Snoep G et al. Time course of structural adaptations in chronic AV block dogs: evidence for differential ventricular remodeling. Am J Physiol Heart Circ Physiol. 2001;280:2882–90. doi: 10.1152/ajpheart.2001.280.6.H2882. [DOI] [PubMed] [Google Scholar]
- 24.Verduyn SC, Vos MA, van der Zande J et al. Further observations to elucidate the role of interventricular dispersion of repolarization and early afterdepolarizations in the genesis of acquired torsade de pointes arrhythmias: a comparison between almokalant and d-sotalol using the dog as its own control. J Am Coll Cardiol. 1997;30:1575–84. doi: 10.1016/s0735-1097(97)00333-1. [DOI] [PubMed] [Google Scholar]
- 25.Thomsen MB, Volders PG, Beekman JD et al. Beat-to-beat variability of repolarization determines pro-arrhythmic outcome in dogs susceptible to drug-induced torsades de pointes. J Am Coll Cardiol. 2006;48:1268–76. doi: 10.1016/j.jacc.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 26.Sprenkeler DJ, Bossu A, Beekman HDM et al. An augmented negative force-frequency relationship and slowed mechanical restitution are associated with increased susceptibility to drug-induced torsade de pointes arrhythmias in the chronic atrioventricular block dog. Front Physiol. 2018;9:1–13. doi: 10.3389/fphys.2018.01086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dunnink A, Van Opstal JM, Oosterhoff P et al. Ventricular remodelling is a prerequisite for the induction of dofetilide-induced torsade de pointes arrhythmias in the anaesthetized, complete atrio-ventricular-block dog. Europace. 2012;14:431–6. doi: 10.1093/europace/eur311. [DOI] [PubMed] [Google Scholar]
- 28.Thomsen MB, Oros A, Schoenmakers M et al. Pro-arrhythmic electrical remodelling is associated with increased beat-to-beat variability of repolarisation. Cardiovasc Res. 2007;73:521–30. doi: 10.1016/j.cardiores.2006.11.025. [DOI] [PubMed] [Google Scholar]
- 29.Volders PG, Sipido KR, Vos MA et al. Downregulation of delayed rectifier K+ currents in dogs with chronic complete atrioventricular block and acquired torsades de pointes. Circulation. 1999;100:2455–61. doi: 10.1161/01.cir.100.24.2455. [DOI] [PubMed] [Google Scholar]
- 30.Sipido KR, Volders PG, de Groot SH et al. Enhanced Ca2+ release and Na/Ca exchange activity in hypertrophied canine ventricular myocytes. Circulation. 2000;102:2137–LP-2144. doi: 10.1161/01.cir.102.17.2137. [DOI] [PubMed] [Google Scholar]
- 31.Verdonck F, Volders PG, Vos MA et al. Increased Na+ concentration and altered Na/K pump activity in hypertrophied canine ventricular cells. Cardiovasc Res. 2003;57:1035–43. doi: 10.1016/s0008-6363(02)00734-4. [DOI] [PubMed] [Google Scholar]
- 32.van Borren MM, Vos MA, Houtman MJC et al. Increased sarcolemmal Na+/H+ exchange activity in hypertrophied myocytes from dogs with chronic atrioventricular block. Front Physiol. 2013;4:1–9. doi: 10.3389/fphys.2013.00322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roden DM. Taking the ‘idio’ out of ‘idiosyncratic’: predicting torsades de pointes. Pacing Clin Electrophysiol. 1998;21:1029–34. doi: 10.1111/j.1540-8159.1998.tb00148.x. [DOI] [PubMed] [Google Scholar]
- 34.Singh N, Moneghetti KJ, Christle JW et al. Heart rate variability: an old metric with new meaning in the era of using mhealth technologies for health and exercise training guidance. part one: physiology and methods. Arrhythmia Electrophysiol Rev. 2018;7:193–8. doi: 10.15420/aer.2018.27.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh N, Moneghetti KJ, Christle JW et al. Heart rate variability: an old metric with new meaning in the era of using mhealth technologies for health and exercise training guidance. part two: prognosis and training. Arrhythmia Electrophysiol Rev. 2018;7:247–55. doi: 10.15420/aer.2018.30.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomsen MB, Verduyn SC, Stengl M et al. Increased short-term variability of repolarization predicts d-sotalol-induced torsades de pointes in dogs. Circulation. 2004;110:2453–9. doi: 10.1161/01.CIR.0000145162.64183.C8. [DOI] [PubMed] [Google Scholar]
- 37.Varkevisser R, Wijers SC, van der Heyden MAG et al. Beat-to-beat variability of repolarization as a new biomarker for proarrhythmia in vivo. Heart Rhythm. 2012;9:1718–26. doi: 10.1016/j.hrthm.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 38.Oosterhoff P, Oros A, Vos MA. Beat-to-beat variability of repolarization: a new parameter to determine arrhythmic risk of an individual or identify pro-arrhythmic drugs. Anadolu Kardiyol Derg. 2007;7 (Suppl 1):73–8. [PubMed] [Google Scholar]
- 39.Thomsen MB, Truin M, van Opstal JM et al. Sudden cardiac death in dogs with remodeled hearts is associated with larger beat-to-beat variability of repolarization. Basic Res Cardiol. 2005;100:279–87. doi: 10.1007/s00395-005-0519-6. [DOI] [PubMed] [Google Scholar]
- 40.Bossu A, Varkevisser R, Beekman HDM et al. Short-term variability of repolarization is superior to other repolarization parameters in the evaluation of diverse antiarrhythmic interventions in the chronic AV block dog. J Cardiovasc Pharmacol. 2017;69:398–407. doi: 10.1097/FJC.0000000000000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wijers SC, Bossu A, Dunnink A et al. Electrophysiological measurements that can explain and guide temporary accelerated pacing to avert (re)occurrence of torsade de pointes arrhythmias in the canine chronic atrioventricular block model. Heart Rhythm. 2017;14:749–56. doi: 10.1016/j.hrthm.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 42.Antoons G, Oros A, Beekman JDM et al. Late Na+ current inhibition by ranolazine reduces torsades de pointes in the chronic atrioventricular block dog model. J Am Coll Cardiol. 2010;55:801–9. doi: 10.1016/j.jacc.2009.10.033. [DOI] [PubMed] [Google Scholar]
- 43.Van de Water A, Verheyen J, Xhonneux R. Reneman RS. An improved method to correct the QT interval of the electrocardiogram for changes in heart rate. J Pharmacol Methods. 1989;217:207–17. doi: 10.1016/0160-5402(89)90015-6. [DOI] [PubMed] [Google Scholar]
- 44.Mohan N, Niyogi D, Singh HN. Analysis of relationship between Q-T and R-R interval in the electrocardiogram of goats. Indian J Anim Sci. 2009;79:362–5. [Google Scholar]
- 45.Stams TRG, Winckels SKG, Oros A et al. Novel parameters to improve quantification of repolarization reserve and arrhythmogenesis using a dofetilide challenge. Heart Rhythm. 2013;10:1745–6. doi: 10.1016/j.hrthm.2013.09.027. [DOI] [Google Scholar]
- 46.Bossu A, Kostense A, Beekman HDM et al. Istaroxime, a positive inotropic agent devoid of pro-arrhythmic properties in sensitive chronic atrioventricular block dogs. Pharmacol Res. 2018;133:132–40. doi: 10.1016/j.phrs.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 47.Asano Y, Davidenko JM, Baxter WT et al. Optical mapping of drug-induced polymorphic arrhythmias and torsade de pointes in the isolated rabbit heart. J Am Coll Cardiol. 1997;29:831–42. doi: 10.1016/s0735-1097(96)00588-8. [DOI] [PubMed] [Google Scholar]
- 48.Choi B-R, Burton F, Salama G. Cytosolic Ca2+ triggers early afterdepolarizations and torsade de pointes in rabbit hearts with type 2 long QT syndrome. J Physiol. 2002;543:615–31. doi: 10.1113/jphysiol.2002.024570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.el-Sherif N, Caref EB, Yin H, Restivo M. The electrophysiological mechanism of ventricular arrhythmias in the long QT syndrome. Circ Res. 1996;79:474–92. doi: 10.1161/01.res.79.3.474. [DOI] [PubMed] [Google Scholar]
- 50.El-Sherif N, Chinushi M. Caref, et al. Electrophysiological mechanism of the characteristic electrocardiographic morphology of torsade de pointes tachyarrhythmias in the long-QT syndrome: detailed analysis of ventricular tridimensional activation patterns. Circulation. 1997;96:4392–9. doi: 10.1161/01.cir.96.12.4392. [DOI] [PubMed] [Google Scholar]
- 51.Kozhevnikov DO, Yamamoto K, Robotis D et al. Electrophysiological mechanism of enhanced susceptibility of hypertrophied heart to acquired torsade de pointes arrhythmias. Circulation. 2002;105:1128–34. doi: 10.1161/hc0902.104711. [DOI] [PubMed] [Google Scholar]
- 52.Murakawa Y, Sezaki K, Yamashita T et al. Three-dimensional activation sequence of cesium-induced ventricular arrhythmias. Am J Physiol Circ Physiol. 1997;273:H1377–85. doi: 10.1152/ajpheart.1997.273.3.H1377. [DOI] [PubMed] [Google Scholar]
- 53.Schreiner KD, Voss F, Senges JC et al. Tridimensional activation patterns of acquired torsade-de-pointes tachycardias in dogs with chronic AV-block. Basic Res Cardiol. 2004;99:288–98. doi: 10.1007/s00395-004-0469-4. [DOI] [PubMed] [Google Scholar]
- 54.Senges JC, Sterns LD, Freigang KD et al. Cesium chloride induced ventricular arrhythmias in dogs: three-dimensional activation patterns and their relation to the cesium dose applied. Basic Res Cardiol. 2000;95:152–62. doi: 10.1007/s003950050177. [DOI] [PubMed] [Google Scholar]
- 55.Kim TY, Kunitomo Y, Pfeiffer Z et al. Complex excitation dynamics underlie polymorphic ventricular tachycardia in a transgenic rabbit model of long QT syndrome type 1. Heart Rhythm. 2015;12:220–8. doi: 10.1016/j.hrthm.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dunnink A, Stams TRG, Bossu A et al. Torsade de pointes arrhythmias arise at the site of maximal heterogeneity of repolarization in the chronic complete atrioventricular block dog. Europace. 2017;19:858–65. doi: 10.1093/europace/euw087. [DOI] [PubMed] [Google Scholar]
- 57.Akar FG, Yan GX, Antzelevitch C et al. Unique topographical distribution of M Cells underlies reentrant mechanism of torsade de pointes in the long-QT syndrome. Circulation. 2002;105:1247–53. doi: 10.1161/hc1002.105231. [DOI] [PubMed] [Google Scholar]
- 58.Boulaksil M, Jungschleger JG, Antoons G et al. Drug-induced torsade de pointes arrhythmias in the chronic AV block dog are perpetuated by focal activity. Circ Arrhythmia Electrophysiol. 2011;4:566–76. doi: 10.1161/CIRCEP.110.958991. [DOI] [PubMed] [Google Scholar]
- 59.Vandersickel N, Bossu A, De Neve J Short-lasting episodes of torsade de pointes in the chronic atrioventricular block dog model have a focal mechanism, while longer-lasting episodes are maintained by re-entry. JACC Clin Electrophysiol. 2017. p. 3. [DOI] [PubMed]
- 60.Hinterseer M, Thomsen MB, Beckmann BM et al. Beat-to-beat variability of QT intervals is increased in patients with drug-induced long-QT syndrome: a case control pilot study. Eur Heart J. 2008;29:185–90. doi: 10.1093/eurheartj/ehm586. [DOI] [PubMed] [Google Scholar]
- 61.Hinterseer M, Beckmann BM, Thomsen MB et al. Relation of increased short-term variability of QT interval to congenital long-QT syndrome. Am J Cardiol. 2009;103:1244–8. doi: 10.1016/j.amjcard.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 62.Ritsema van Eck HJ, Broeyer FJ, van Herpen G Short-term QT variability: a marker for reduced repolarization reserve in anthracyclin therapy. Computers in Cardiology. 2009. pp. 585–8.
- 63.Hinterseer M, Beckmann BM, Thomsen MB et al. Usefulness of short-term variability of QT intervals as a predictor for electrical remodeling and proarrhythmia in patients with nonischemic heart failure. Am J Cardiol. 2010;106:216–20. doi: 10.1016/j.amjcard.2010.02.033. [DOI] [PubMed] [Google Scholar]
- 64.Lengyel C, Orosz A, Hegyi P et al. Increased short-term variability of the QT interval in professional soccer players: possible implications for arrhythmia prediction. PLoS One. 2011;6:e18751. doi: 10.1371/journal.pone.001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tereshchenko LG, Fetics BJ, Domitrovich PP et al. Prediction of ventricular tachyarrhythmias by intracardiac repolarization variability analysis. Circ Arrhythmia Electrophysiol. 2009;2:276–84. doi: 10.1161/CIRCEP.108.829440. [DOI] [PubMed] [Google Scholar]
- 66.Paz O, Zhou X, Gillberg J et al. Detection of T-wave alternans using an implantable cardioverter-defibrillator. Heart Rhythm. 2006;3:791–7. doi: 10.1016/j.hrthm.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 67.Sandhu RK, Costantini O, Cummings JE et al. Intracardiac alternans compared to surface T-wave alternans as a predictor of ventricular arrhythmias in humans. Heart Rhythm. 2008;5:1003–8. doi: 10.1016/j.hrthm.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 68.Bossu A, Houtman MJC, Meijborg VMF et al. Selective late sodium current inhibitor GS-458967 suppresses torsades de pointes by mostly affecting perpetuation but not initiation of the arrhythmia. Br J Pharmacol. 2018;175:2470–82. doi: 10.1111/bph.14217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ji Y, Varkevisser R, Opacic D et al. The inward rectifier current inhibitor PA-6 terminates atrial fibrillation and does not cause ventricular arrhythmias in goat and dog models. Br J Pharmacol. 2017;174:2576–90. doi: 10.1111/bph.13869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Varkevisser R, van der Heyden MA, Tieland RG et al. Vernakalant is devoid of pro-arrhythmic effects in the complete AV block dog model. Eur J Pharmacol. 2013;720:49–54. doi: 10.1016/j.ejphar.2013.10.054. [DOI] [PubMed] [Google Scholar]
- 71.Bourgonje VJA, Schoenmakers M, Beekman JD et al. Relevance of calmodulin/CaMKII activation for arrhythmogenesis in the AV block dog. Heart Rhythm. 2012;9:1875–1883. doi: 10.1016/j.hrthm.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 72.Stams TR, Oros A, van der Nagel R et al. Effects of K201 on repolarization and arrhythmogenesis in anesthetized chronic atrioventricular block dogs susceptible to dofetilide-induced torsade de pointes. Eur J Pharmacol. 2011;672:126–34. doi: 10.1016/j.ejphar.2011.09.180. [DOI] [PubMed] [Google Scholar]
- 73.Oros A, Houtman MJ, Neco P et al. Robust anti-arrhythmic efficacy of verapamil and flunarizine against dofetilide-induced TdP arrhythmias is based upon a shared and a different mode of action. Br J Pharmacol. 2010;161:162–75. doi: 10.1111/j.1476-5381.2010.00883.x. [DOI] [PMC free article] [PubMed] [Google Scholar]