Abstract
Objectives
Internationally, public health strategies encourage health care professionals to deliver opportunistic behaviour change interventions. The present study: (1) examines the barriers and enablers to delivering interventions during routine consultations, and (2) provides recommendations for the design of interventions to increase delivery of opportunistic behaviour change interventions.
Design
Qualitative interview study.
Methods
Twenty‐eight semi‐structured interviews were conducted with patient‐facing health care professionals. The Behaviour Change Wheel informed a framework analysis in which findings were mapped onto the Theoretical Domains Framework (TDF). Intervention functions and behaviour change techniques (BCTs) targeting each TDF domain were identified.
Results
Health care professionals understood the importance of opportunistic behaviour change interventions (beliefs about consequences), but were sceptical about their capabilities to facilitate behaviour change with patients (beliefs about capabilities). Some clinicians were unwilling to discuss behaviours perceived as unrelated to the patient's visit (social/professional role and identity). Discipline‐specific tasks were prioritized, and delivering interventions was perceived as psychologically burdensome. One‐to‐one contact was favoured over busy hospital settings (environmental context and resources). Seven intervention functions (training, restriction, environmental restructuring, enablement, education, persuasion, and modelling) and eight BCT groupings (antecedents, associations, comparison of outcomes, covert learning, feedback and monitoring, natural consequences, reward and threat, and self‐belief) were identified.
Conclusions
Across disciplines, health care professionals see the value of opportunistic behaviour change interventions. Barriers related to workload, the clinical environment, competence, and perceptions of the health care professional role must be addressed, using appropriate intervention functions and BCTs, in order to support health care professionals to increase the delivery of interventions in routine practice.
Statement of contribution.
What is already known on this subject?
Brief, opportunistic interventions can be a cost effective way of addressing population health problems.
Public health policies compel health care professionals to deliver behaviour change interventions opportunistically.
Health care professionals do not always deliver interventions opportunistically during routine medical consultations; however the barriers and enablers are currently unclear.
What does this study add?
This is the first study to examine cross‐disciplinary barriers and enablers to delivering opportunistic behaviour change interventions.
Across diverse professional groups, working in different medical professions, participants saw the value of delivering opportunistic behaviour change interventions.
Targeting key theoretical domains that are shared across professional groups may be useful for increasing the delivery of opportunistic behaviour change interventions.
Keywords: health care professionals, behaviour change wheel, Theoretical Domains Framework, qualitative, behaviour change, COM‐B
Background
Health behaviour change is an issue of worldwide importance. Unhealthy behaviours are key risk factors for long‐term conditions such as cardiovascular diseases, diabetes, and cancer (World Health Organization, 2017). Internationally, public health strategies compel health care professionals to deliver opportunistic behaviour change interventions, emphasizing the need for preventive strategies to be at the heart of every patient contact (Public Health England, 2016). Health care professionals are expected to offer concise, opportunistic health behaviour change interventions (e.g., smoking cessation, improving diet, increasing physical activity, and reducing alcohol intake), by using the millions of day‐to‐day interactions with patients to, as a minimum, ‘raise awareness, motivate and signpost people to help them improve their health and wellbeing’ (Public Health England, 2016, p. 15).
Behaviour change interventions can be delivered by health care professionals in as few as 30‐s (Aveyard et al., 2016; Public Health England, 2016) and are cost‐effective (Vijay, Wilson, Suhrcke, Hardeman, & Sutton, 2016). However, health care professionals do not always deliver behaviour change interventions opportunistically during routine patient consultations, even in cases where they perceive patients would benefit from such interventions (Keyworth, Epton, Goldthorpe, Calam, & Armitage, 2018). The barriers and enablers to delivering interventions opportunistically, across specialisms, are currently unclear. Previous research has focused on professionals within defined specialities delivering interventions within specific contexts, such as smoking cessation for cancer patients at the time of diagnosis (Wells et al., 2017), weight management in community pharmacy settings (Um, Armour, Krass, Gill, & Chaar, 2013), and midwives implementing physical activity guidelines for obese women during pregnancy (McParlin, Bell, Robson, Muirhead, & Araujo‐Soares, 2017). Consequently, there are two important gaps in knowledge. First, the evidence base focuses on prescribed interventions and intervention development, as opposed to exploring opportunistic behaviour change interventions that are delivered by health care professionals during routine consultations with patients. Second, there is a lack of knowledge of shared barriers and enablers across different health care professional groups for delivering opportunistic behaviour change interventions: Understanding cross‐disciplinary barriers and enablers will facilitate implementation of policies designed to deliver behaviour change interventions at scale.
Although health care professionals are an expected and trusted source of behaviour change advice (McPhail & Schippers, 2012; Whitlock, Orleans, Pender, & Allan, 2002), the expectation that they will deliver health behaviour change interventions opportunistically is relatively new, and so may not be a core part of health care professional training or established practice. Systematic reviews cite knowledge and skills as barriers to addressing behaviour change with patients among GPs (Stead et al., 2009), dentists (Lala, Csikar, Douglas, & Muarry, 2017), and anaesthesiologists (Yousefzadeh, Chung, Wong, Warner, & Wong, 2016). However, although knowledge and skills are necessary for health care professionals to deliver opportunistic behaviour change interventions, they are not sufficient and health care professionals additionally require motivation and opportunity (Michie, Atkins, & West, 2014). Consequently, it is important to understand more about this area of professional practice. The purpose of the present study was to: (1) understand the barriers and enablers to health care professionals delivering opportunistic behaviour change interventions as part of routine practice, and (2) to provide recommendations for the design of future interventions to increase the delivery of opportunistic behaviour change interventions.
Method
Design
We conducted a qualitative study using semi‐structured telephone interviews with patient‐facing health care professionals working in the UK's National Health Service (NHS). The Behaviour Change Wheel (BCW; Michie et al., 2014), a synthesis of 19 behaviour change frameworks used to guide intervention development, was employed to illustrate how the qualitative findings can be utilized to inform behaviour change interventions for health care professionals. The topic guide (presented in Table S1) was informed by the capability, opportunity, motivation model of behaviour (COM‐B), which is at the heart of the BCW (Michie, Stralen, & West, 2011; Michie et al., 2014), and explored the barriers and enablers associated with delivering opportunistic behaviour change interventions. The COM‐B model comprises six components that are hypothesized to drive behaviour, namely: physical capability (e.g., skills), psychological capability (e.g., knowledge), physical opportunity (e.g., time), social opportunity (e.g., social cues), reflective motivation (e.g., intentions), and automatic motivation (e.g., emotional reactions; Michie et al., 2011, 2014). The COM‐B model has been used previously in other areas of health care professional practice (Alexander, Brijnath, & Mazza, 2014; Barker, de Lusignan, & Cooke, 2016), but not across disciplines or in the domain of opportunistic behaviour change intervention. Using the COM‐B model to tailor the interview questions allowed us to: (1) obtain a broad understanding of the barriers and enablers to opportunistic behaviour change intervention, (2) use the Theoretical Domains Framework (TDF; described below) to identify the emergent themes that were generated from the data, and (3) link the respective components of the COM‐B model directly to the analytical framework (the TDF) to provide a focused analysis that highlighted the barriers and enablers to this area of professional practice (Cane, O'Connor, & Michie, 2012).
The fourteen‐domain TDF (described in Table S2) was deemed to be the most suitable analytical framework (Atkins et al., 2017), as it prompts a detailed analysis of environmental (e.g., resources), social (e.g., interpersonal influences), cognitive (e.g., decision processes), and affective (e.g., optimism) influences on health care professional practice (Cane et al., 2012). The TDF has yet to be used to understand the cross‐disciplinary barriers and enablers to health care professionals delivering opportunistic health behaviour change interventions during routine patient consultations.
Irreducible active components of behaviour change interventions (Epton, Currie, & Armitage, 2017; Michie & Johnston, 2013) or ‘behaviour change techniques’ (BCTs) were then extrapolated from the findings. We provide illustrative examples in order to demonstrate how BCTs can be operationalized as part of interventions to increase health care professionals’ delivery of opportunistic behaviour change interventions (Michie et al., 2014). Subsequently, in line with the BCW, guidelines for mapping BCTs and intervention functions to TDF domains (Cane, Richardson, Johnston, Ladha, & Michie, 2015) were used by the research team to identify the relevant intervention functions and BCTs to be used for interventions targeting each TDF domain. Intervention functions are defined by Michie et al. (2014) as the ‘means by which an intervention can change behaviour’ (p. 109). That is, interventions with different purposes can facilitate behaviour change: Examples include education (increasing knowledge by providing information) or incentivization (providing a reward).
Sample
To gain a range of experiences, health care professionals with a patient‐facing role working in the NHS in the United Kingdom were invited to take part in the interview study. The sample was heterogeneous, and we sought to explore a wide range of views from diverse professional groups working in different medical professions (Dicicco‐Bloom & Crabtree, 2006). Participants, initially recruited through a survey panel company (YouGov), had previously taken part in a large‐scale cross‐sectional survey examining the prevalence of, and extent to which, health care professionals delivered opportunistic behaviour change interventions as part of routine practice (Keyworth et al., 2018). Participants who expressed an interest were invited to supply their contact details, so a member of the research team could arrange a convenient time to conduct the interview. Data collection ceased at the point of saturation, where the research team agreed by consensus that no new themes were emerging from the data.
Procedure
Ethical approval for the study was obtained from a university ethics committee (ref: 2017‐0739‐1780). In line with the literature (Michie et al., 2014), three specific recommendations were adhered to when conducting the interviews: (1) Open‐ended questions encouraged participants to explore their professional practice and elicit any barriers and enablers that influenced their delivery of opportunistic behaviour change interventions, (2) the interviewers (two members of the research team, CK and JG), who were trained in conducting qualitative interviews with health care professionals, proceeded with caution when asking questions about current practice in order to minimize biases as a result of social desirability and professional identity, and (3) participants were encouraged to address specific instances of current or recent practice of providing opportunistic behaviour change interventions in relation to their specific specialism (where and when). Data collection took place between March 2017 and August 2017.
Analysis
Interviews were audio‐recorded and transcribed verbatim. Microsoft Excel was used to develop the coding framework, with principles of the Framework approach (Gale, Heath, Cameron, Rashid, & Redwood, 2013) used to map the data to the relevant theoretical domains. This approach was chosen as it enabled both predetermined and emergent issues to be explored in depth whilst using the TDF as an explanatory framework. One member of the research team (CK) analysed all of the interviews. A second and third member (JG and TE) independently analysed a sample of the interviews (approximately 50% were randomly selected), to ensure the TDF was an appropriate analytical framework.
Two levels of coding were used: deductive (first level) and inductive (second level). First‐level (deductive) coding was used to generate the coding framework. Directed content analysis was used to identify and categorize instances of the TDF domains (Hsieh & Shannon, 2005). This involved reading each transcript and coding occurrences relating to each TDF domain (Ritchie & Spencer, 1994). Analysis involved coding each occurrence in the interviews of each of the COM‐B components and mapping these directly to the relevant TDF domains, using the definitions accompanying each domain (Table S3). This was done for all TDF domains. Establishing the importance of a domain was based on two criteria, which have been used in other studies (Francis et al., 2009; Gould et al., 2018): (1) specific domains mentioned frequently across professional groups (assessed quantitatively), and (2) where strong beliefs within each domain were perceived as a barrier or enabler to delivering behaviour change interventions (assessed qualitatively). The most prominent domains were those deemed to meet both criteria. Second level (inductive) coding consisted of generating explanatory themes in line with the most prominent theoretical domains identified from the first level coding (Atkins et al., 2017).
To illustrate how the findings can be used to inform future intervention design, the relevant BCTs with accompanying intervention functions were mapped to the findings in relation to each TDF domain (Cane et al., 2015; Michie et al., 2014). An overview of the analytical process is presented in Figure 1.
Figure 1.
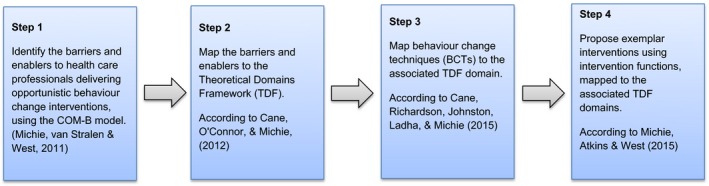
Overview of the analytical process.
To ensure validity, reliability, and accuracy of the coding process, two of the study authors who had prior knowledge of the TDF independently coded a randomly selected sample of the coded data (approximately 10% of the total number of quotes mapped to the respective TDF domains). Good agreement was obtained (k = .695) (Landis & Koch, 1977) suggesting independent coders were able to map identified barriers and enablers against the most relevant TDF domain.
Results
Participants (n = 28) represented a diverse range of health care professionals, all of whom had a patient‐facing role. Participants worked across different settings, including primary care (n = 6), acute care (n = 13), and community care (n = 8). Participant demographics are presented in Table 1. Length of interviews ranged from 22 to 42 min (mean length 30 min).
Table 1.
Participant demographics (n = 28)
| Variables | n (%) |
|---|---|
| Gender | |
| Male | 4 (14.3) |
| Female | 24 (85.7) |
| Ethnicity | |
| White British | 26 (92.9) |
| Other white background | 1 (3.6) |
| Other mixed background | 1 (3.6) |
| Age | |
| 25–34 | 3 (10.7) |
| 35–44 | 9 (32.1) |
| 45–54 | 7 (25) |
| 55–64 | 5 (17.9) |
| >65 | 4 (14.3) |
| Setting currently working in | |
| NHS Acute Care | 13 (46.4) |
| NHS Tertiary Care | 1 (3.6) |
| NHS Community Care | 8 (28.6) |
| NHS Primary Care | 6 (21.4) |
| Health care professional group | |
| Mental health nurse | 4 (14.3) |
| Nurse | 4 (14.3) |
| Dermatology nurse | 4 (14.3) |
| GP/Doctor | 4 (14.3) |
| Midwife | 3 (10.7) |
| Audiologist | 1 (3.6) |
| Health visitor | 1 (3.6) |
| Mental health worker | 1 (3.6) |
| Anaesthetist | 1 (3.6) |
| Pharmacist | 1 (3.6) |
| Chiropractor | 1 (3.6) |
| Physio | 1 (3.6) |
| Ophthalmologist | 1 (3.6) |
| Dentist | 1 (3.6) |
| Years in current profession | |
| 6 months to 1 year | 1 (3.6) |
| 2 to 5 years | 2 (7.1) |
| 5 to 10 years | 5 (17.9) |
| 10 to 15 years | 2 (7.1) |
| 15 to 20 years | 3 (10.7) |
| >20 years | 14 (50) |
| Did not state | 1 (3.6) |
Results are presented according to each theoretical domain, with explanatory themes provided alongside each domain. A conceptual diagram of the main findings is presented in Figure 2, with an illustration of the key findings mapped to relevant BCTs (presented in Table S4; a summary table is presented in Table 2). Figure 2 shows that three pairs of explanatory themes were perceived as barriers and enablers (illustrated by the connecting arrows) and related to the health care professional–patient relationship, health care professional's own health behaviour, and perceptions of the specialist health care role. Although these themes cut across domains, the specific concepts described by participants were domain‐specific and described either a barrier or an enabler.
Figure 2.
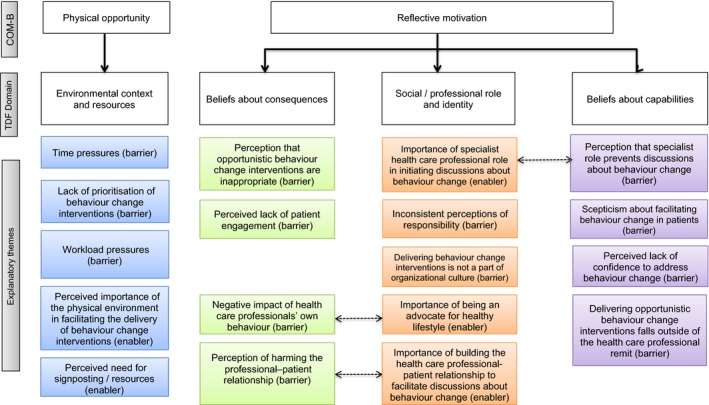
The barriers and enablers to delivering opportunistic behaviour change interventions during routine medical consultations.
Table 2.
Summary of key findings mapped to intervention functions and individual BCTs according to Michie et al. (2014)
| COM domain | TDF domain | Description of domain | Exemplar quotes | Intervention function | Individual BCTs | Exemplar interventions |
|---|---|---|---|---|---|---|
| Physical opportunity | Environmental context and resources | Environment should be conducive to delivering behaviour change interventions. Perceived need for more resources and signposting | ‘I think time constraints from an inpatient point of view because everyone is so stretched, and I think even with some of my [musculoskeletal] colleagues they feel that they have to just treat what's in front of them in the time that they have’. (24713, Physiotherapist) |
|
|
Providing on‐screen reminders and/or prompts for GPs to offer referral to a behaviour change service, such as a smoking cessation service or weight loss clinic (Intervention function: environmental restructuring; BCT: prompts/cues) |
| Reflective motivation | Beliefs about consequences | Delivering behaviour change interventions must be perceived as appropriate within the context of a routine medical consultation | ‘Because my credibility, you know, if I start saying, you know, smoking increases your risk of lung cancer or doing this does that, and I'm standing there as a skin cancer specialist nurse, I think that you, it all just turns into a bit of a blah blah blah’. (21550, Nurse) |
|
|
Provide a series of case studies demonstrating how health care professionals of varying specialisms can deliver behaviour change interventions, and asking health care professionals to list the advantages and disadvantages of each approach (Intervention function: modelling; BCT: pros and cons) |
| Beliefs about capabilities | Perception that delivering behaviour change interventions falls outside of professional remit | ‘I think there might also be an issue with confidence, about people not maybe knowing what to discuss or what advice to give people. I think again it's sometimes something that gets lost by the wayside because we're kind of focused on mental health, and it's more often than not, I would say, the service users he will work with will not bring those things up as issues themselves’. (24619, Mental Health Nurse) |
|
|
Provide information about, and examples of, brief behaviour change interventions, and inform the health care professional they can successfully incorporate these into time‐restricted consultations (Intervention function: education; BCT: verbal persuasion to boost self‐efficacy) |
|
| Social/professional role and identity | Importance of facilitating a positive health professional–patient relationship, and taking responsibility for delivering behaviour change interventions | ‘We don't talk about anything else, you know, like obesity or anything like that, or healthy eating. We just do it about smoking, because I guess we felt we had a good reason to ask about smoking. So I guess that might have been that we feel confident and able to do that’. (Audiologist, 1552) |
|
|
Inform the health care professional about the number and cost of hospital admissions related to excess alcohol intake, smoking, and obesity, emphasizing the opportunity to reduce this by delivering behaviour change interventions (Intervention function: education; BCT: information about social and environmental consequences) |
No BCTs are associated with the TDF domain social/professional role and identity; therefore for this domain, BCTs are associated with the intervention functions.
Four theoretical domains emerged that explained the barriers and enablers to delivering opportunistic behaviour change interventions: environmental context and resources (n = 104 occurrences; reported by 28 [100%] of the 28 health care professionals), beliefs about consequences (n = 73 occurrences; reported by 27 [96%] of the 28 health care professionals), beliefs about capabilities (n = 79 occurrences; reported by 22 [79%] of the 28 health care professionals), and social/professional role and identity (n = 101 occurrences; reported by 27 [96%] of the 28 health care professionals). Explanatory quotes with participant ID are presented with health care professional categories displayed in parentheses.
Environmental context and resources
Three barriers and two enablers were described in relation to the domain environmental context and resources. Health care professionals described the pressures that they face when attempting to deliver opportunistic behaviour change interventions, as well as emphasizing the need for an environment conducive to delivering behaviour change interventions, and access to appropriate resources during the consultation.
Participants described the influence of environmental context as an important driver of them providing patients with opportunistic behaviour change interventions. Participants perceived a number of barriers related to workload and the resources they had available to them during the consultation.
Time pressures (barrier)
Regardless of their discipline, participants reported they were under considerable time pressures both to see their allocation of patients and to address the primary medical problem that was the focus of the consultation. Tight schedules meant that rarely was there an opportunity to discuss any behaviour change‐related issues that fell outside of the primary presenting medical complaint.
Ideally we're very well placed to give advice about any sort of lifestyle changes. However we have such a tight schedule now with the visits, the development checks that we do, we have a limited time and we have to cover so many aspects. (24620, Health Visitor)
Lack of prioritization of behaviour change interventions (barrier)
Participants reported they did not give sufficient priority to providing opportunistic behaviour change interventions to patients, but instead focused on ensuring that the correct medication was prescribed and that the patient's presenting symptoms were addressed sufficiently. This lack of priority to providing opportunistic behaviour change interventions to patients also included organizational factors, such as lack of endorsement from senior managers.
The value isn't right up there. So it depends where you place your requirements in an area that's time poor and everybody's running around trying to knock out X, Y and Z, and staff making sure that everyone gets their drugs on time or whatever else. (23404, GP)
Workload pressures (barrier)
Competing demands, such as completing a number of clinical tasks during the consultation (biomedical measurement, diagnosis, formulating a management plan) and the pressures of discharging patients in a timely manner, meant that health care professionals were not always able to provide opportunistic behaviour change interventions. The limited amount of time allocated to a consultation meant that a discussion about behaviour change was not feasible. These additional psychological demands created low morale and a lack of motivation to engage in tasks outside of health care professionals’ immediate remit.
There's a little bit of demotivation, I would say, in the NHS at the moment. And this is extra. I mean we may not… Maybe it shouldn't be extra but it is an extra role, an extra job. (23663, Anaesthetist)
Perceived importance of the physical environment in facilitating the delivery of behaviour change interventions (enabler)
Across all professions, the need to have an environment that facilitated one‐to‐one private discussions about behaviour change was highlighted as opposed to a busy clinical environment such as a hospital setting. Certain environments were described as being more conducive to a conversation about behaviour change, such as the patient's home, within familiar surroundings (in the case of health visitors), or the clinic setting.
It helps that we see people in their own environment, because you can get a sense of how people are living day to day. (24619, Mental Health Nurse)
Perceived need for signposting/resources (enabler)
Participants described feeling unable to offer patients specific advice and information about behaviour change. Health care professionals highlighted the need for better awareness of services to which they could signpost patients, including patient information sources and availability of services that patients could access. This was believed to facilitate the process of supporting patients in changing their behaviour.
I really need some kind of centralised database of information of what's about there that's held on the intranet or something like that so that any member of staff could just go and access that easily. (24713, Physiotherapist)
Beliefs about consequences
Four barriers were described in relation to the domain beliefs about consequences. Health care professionals believed that not all patients would be receptive to behaviour change interventions, and consequently made conscious decisions concerning which patients would receive an opportunistic behaviour change intervention. Additionally, health care professionals described the influence that health care professionals’ own health behaviours may have on patients.
Perception that opportunistic behaviour change interventions are inappropriate (barrier)
Health care professionals perceived that it was not always appropriate to be talking about behaviour change during the consultation, especially if behaviour change was not directly related to the patient's medical issue. Any attempt to broach the subject may result in patients responding negatively and could compromise the health care professional–patient relationship. Additionally, the patient's own agenda for the consultation may affect the likelihood of the topic being raised.
They get annoyed with you because you've brought it up and they don't see it as being relevant to the consultation that they're having. (24516, GP)
Perceived lack of patient engagement (barrier)
Health care professionals reported consciously deciding which patients to try and engage in conversations about behaviour change, depending on how they believed they would respond. Conversely, some health care professionals suggested that patients could infer false reassurances about their health through health care professionals failing to have a conversation about behaviour change.
They will think, oh well, the midwife didn't say anything about me smoking; or the midwife didn't say anything about me being massively overweight or whatever, so it must be okay. (21547, Midwife)
Negative impact of health care professionals’ own behaviour (barrier)
An important barrier reported by the health care professionals was the influence of their own health behaviours. If they perceived themselves to be unhealthy, this was likely to affect their own practice, which made talking to patients about behaviour change a more difficult task.
How do you say to somebody, you shouldn't be smoking, and they go, well, you've just come back in from your break, and I can smell smoke off you. I am overweight, and yet, I offer diet advice to people. And very, very occasionally, it doesn't happen often, but very occasionally, somebody will turn round and say, and who are you to tell me. (25061, Nurse)
Perception of harming the professional–patient relationship (barrier)
Participants reported that delivering behaviour change interventions sometimes had a detrimental effect on the health care professional–patient relationship. This often results in health care professionals being cautious in raising the topic of behaviour change. In some specialisms, nursing, for example, health care professionals believed that patients did not expect or want information that was outside of their immediate discipline, as it was perceived to undermine their credibility as a specialist.
If I have those conversations with them and they're clearly not interested they will tell me they're not interested, they're usually quite forthcoming in that respect. (24619, Mental Health Nurse)
Beliefs about capabilities
Four barriers were described in relation to the domain beliefs about capabilities. Health care professionals believed they were not best placed to deliver opportunistic behaviour change interventions, and suggested their responsibility lay with other areas of professional practice. This consequently affected their perceived ability and confidence in their ability to deliver interventions.
Perceived lack of confidence to address behaviour change (barrier)
Health care professionals perceived a lack of confidence in their own skill set and ability to have conversations about behaviour change with patients that focused on long‐term planning of behaviour change. Building one's confidence to acquire new skills and knowledge was reported as an important factor in being able to have conversations about behaviour change.
I've had quite a lot of training now, in psychology and psycho‐dermatology; so I feel much more competent in doing that. (22694, Dermatology Specialist Nurse)
Scepticism about facilitating behaviour change in patients (barrier)
Health care professionals believed that delivering opportunistic behaviour change interventions would be poorly received by patients and was sceptical about their ability to help patients make positive changes.
They [patients] might not feel confident; they might not want to open up these issues with someone and then feel that they don't have the adequate time to deal with it’. (24713, Physiotherapist)
Delivering opportunistic behaviour change interventions falls outside of the health care professional remit (barrier)
Health care professionals reported that their role was often a specialist one, and as a result, delivering opportunistic behaviour change interventions fell outside of their professional remit. Rather, the main focus of the consultation was to address and manage the patient's primary medical complaint. Consequently, health care professionals reported a lack of empowerment to deliver interventions, where addressing patients’ behaviours was discouraged, in favour of other clinical tasks.
I would say that there is probably…I feel like I'm actively discouraged, maybe not actively, maybe passively discouraged but I feel like the hidden curriculum is that you've got better things to focus on than this. In fact people have said that to me. (21546, GP)
Perception that specialist role prevents discussions about behaviour change (barrier)
Health care professionals perceived that their role has certain parameters that meant that behaviour change would only be discussed if relevant to their discipline. In cases where behaviour change was perceived as irrelevant to their specialist role, health care professionals reported difficulty in relation to delivering interventions. The one exception, however, was midwives, who perceived themselves as being advocates for health care promotion and suggested this was an important part of their role. This view was not shared across other disciplines.
To actually start to talk to someone about them being overweight or smoking can appear challenging if they're coming in to see you with a stiff joint. It's a bit off topic and you may perceive that people might take that message in a threatening or a negative way. (22708, Chiropractor)
Social/professional role and identity
Three barriers and two enablers were described in relation to the domain social/professional role and identity. Health care professionals believed they should be seen as advocates for positive health behaviours. In addition, having a specialist role could facilitate intervention delivery, whilst in other cases, this was believed to act as a barrier, particularly in cases where behaviour change was not seen as a priority for routine practice.
Importance of being an advocate for healthy lifestyle (enabler)
Health care professionals emphasized the importance of health care professionals being an advocate for a healthy lifestyle and identified themselves as appropriate role models. In particular, observing other health care professionals engaging in unhealthy behaviours was perceived as having a detrimental effect on the credibility of the information provided to patients.
It's frustrating for example when staff members are smoking and the policies of no smoking at work aren't enforced and that's difficult. (21546, GP)
Importance of building the health care professional–patient relationship to facilitate discussions about behaviour change (enabler)
Health care professionals described the patient–professional relationship as an important factor in being able to have a discussion about behaviour change, which was often perceived as a sensitive topic. Patients not having a relationship with a health care professional may result in the absence of opportunities to discuss behaviour change. Additionally, health care professionals reported their own personal beliefs about lifestyle behaviours may also influence the likelihood of broaching the subject.
If they're given a leaflet for example or they speak to a professional they've never met before they may not feel comfortable actually exploring the issue with them. (24620, Health Visitor)
Importance of specialist health care professional role in initiating discussions about behaviour change (enabler)
Health care professionals reported that only certain aspects of behaviour change were discussed in their respective specialisms. This was particularly evident in the context of managing the patient's ‘primary’ complaint, for example, physical or psychological health, where behaviour change was only discussed if it was directly related to the presenting complaint. Some health care professionals, however, suggested that their role facilitated a discussion about behaviour change, due to their frequent contact with patients, and being in a position to support and encourage patients. This was particularly prominent in midwives, whose professional role was considered as appropriate to deliver interventions, and who were perceived as having the necessary characteristics.
The midwife's role of advocacy is very, very important. It's part of, you know, the main moulding of being a midwife and caring for women in pregnancy to, kind of, be able to encourage women to be empowered. (21551, Midwife)
Inconsistent perceptions of responsibility (barrier)
Health care professionals reported having clearly defined specialist roles, not all of which included discussing behaviour change with patients. Health care professionals described a number of factors involved in them believing they were not best placed to offer the relevant support, including patient expectations about which health care professionals should be talking about behaviour change.
I obviously can't take it further, but that's not my role here. (23663, Anaesthetist)
Delivering behaviour change interventions is not a part of organizational culture (barrier)
Health care professionals described how the organizational culture meant that talking about behaviour change was not always a priority of day‐to‐day practice. Their role was often focused on their immediate specialism, and workload pressures meant that focus was often on other areas of clinical practice.
I just think the culture we're not quite got it into the culture. For example I'm involved with a charity called [charity x] on [health behaviour] and I'm not a gastro doctor, I'm not a hepatologist, I don't work in psychiatry and I think one of my bosses they're like well why are you involved in this it's got nothing to do with you? (21546, GP)
Exemplar interventions using BCTs
Exemplar interventions are presented in Table 2 (with additional examples found in Table S3). Descriptions of each domain are provided alongside exemplar quotes, the mapped intervention functions, and BCTs, in line with the BCW.
Seven out of the nine intervention functions proposed by Michie et al. (2011) were linked to the four prominent TDF domains: training, restriction, environmental restructuring, enablement, education, persuasion, and modelling. Eight of the sixteen BCT groupings were found to be relevant: antecedents, associations, comparison of outcomes, covert learning, feedback and monitoring, natural consequences, reward and threat, and self‐belief. Within these groupings, nineteen unique BCTs were found to be relevant. For example, when targeting environmental context and resources, suggested interventions may include the following: providing on‐screen reminders and/or prompts for GPs to offer referral to a behaviour change service, such as a smoking cessation service or weight loss clinic (intervention function: environmental restructuring; BCT: prompts/cues), or providing training for health care professionals to deliver brief behaviour change interventions, with the use of readily available patient information resources (e.g., a food diary to promote greater intake of fruit and vegetables) to supplement intervention delivery (intervention function: training; BCT: restructuring the physical environment).
Discussion
This is the first study to identify the barriers and enablers across various health care professions when delivering opportunistic behaviour change interventions to patients during routine consultations (Public Health England, 2016), using a theoretically grounded framework. There were very few inconsistencies across diverse professional groups, and the study explains these using a theoretical framework specifically focusing on implementation (Atkins et al., 2017; Cane et al., 2012). This study makes two important contributions to the literature. First, we describe the four prominent TDF domains that provide the greatest insight into the challenges faced by health care professionals when delivering opportunistic behaviour change interventions. Second, we have provided recommendations as to the relevant intervention functions and BCTs to be included in future interventions to increase health care professionals’ delivery of opportunistic behaviour change interventions.
Health care professionals’ work environment was perceived to be detrimental to delivering opportunistic behaviour change interventions (Environmental context and resources). Consistent with previous literature, time and workload pressures were cited as hampering health care professionals’ opportunities to engage in conversations about behaviour change (Elwell, Povey, Grogan, Allen, & Prestwich, 2013; Elwell, Powell, Wordsworth, & Cummins, 2014; Um et al., 2013). Additionally, findings suggest that across all disciplines behaviour change interventions are not given sufficient priority as part of clinical practice. This may be due to the physical environment not being conducive to a conversation about behaviour change, and the perceived need for more resources and more effective signposting for health care professionals.
Health care professionals are an expected source of advice (McPhail & Schippers, 2012; Whitlock et al., 2002), however, our findings suggest that opportunistic behaviour change interventions were perceived by health care professionals as inappropriate in the context of routine medical consultations (Beliefs about consequences). In contrast, research suggests that patients are receptive to the idea of having a conversation about behaviour change, if done sensitively, and by the correct health care professional (Wells et al., 2017). For example, research with GPs suggests that when raising the topic of weight management, patients are not offended, with the discussions being perceived as helpful (Aveyard et al., 2016). It would be valuable to see whether patients’ experiences of receiving opportunistic behaviour change interventions chime with the view among many health care professionals that patients do not need or want information about behaviour change.
Health risk communication strategies may depend on how health care professionals perceive patient risk and patient motivation to take preventive action (Bonner et al., 2015; Jansen et al., 2017). Our findings suggest that health care professionals often consciously decided which patients to engage with in conversations about their health, depending on whether they would respond positively. As evident in our study, health care professionals not engaging in conversations about behaviour change may result in patients being given false reassurances and being ‘unrealistically optimistic’ about their health, consistent with social cognitive approaches to health risk perception (Weinstein, 1987).
Health care professionals felt restricted by their specialist role in dealing with the primary complaint only and did not feel capable of delivering behaviour change interventions (beliefs about capabilities) they perceived as not being central to their discipline. Further, ability to deliver interventions was impaired by external factors (such as discouragement) and consequently affected participants’ perceived behavioural control. Indeed, health care professionals may be confident in their abilities to deliver interventions, but our findings suggest that they are unable to because of external constraints, rather than identity. Thus, it is argued that the scope of the professional–patient consultation should be widened to encourage health care professionals to consider patients in a broader way, to deal not only with the management of presenting and continuing problems, but on delivering opportunistic behaviour change interventions.
Health care professionals’ own health behaviours impacted on their perceived image as an appropriate role model (social/professional role and identity). Health care professionals who themselves engage in unhealthy behaviours are less likely to deliver behaviour change interventions (Duaso, McDermott, Mujika, Purssell, & While, 2014; Fie, Norman, & While, 2013; Guydish, Passalacqua, Tajima, & Manser, 2007). Our study suggests this is likely to undermine the credibility of information and consequently lead patients to ignore health‐related information.
Implications for practice/implementation
Our findings suggest that supporting health care professionals to deliver opportunistic behaviour change interventions must focus on four key areas. First, the environment must be conducive to having discussions about behaviour change, including having access to the necessary resources and signposting, as reported by health care professionals in our study. Second, behaviour change must be based on patient ‘need’ as opposed to health care professionals’ judgements of how patients may respond to behaviour change interventions; the development of tools to assess patient behaviour change needs should be prioritized. Third, widening the scope of the consultation encourages health care professionals to consider patients in a broader way focusing on prevention and management of health. Fourth, enhancing health care professionals’ capabilities, opportunities, and motivations to deliver opportunistic behaviour change interventions.
This study provides recommendations for operationalizing specific BCTs, as part of intervention design, specifically linked to the TDF domains identified in the present research (Table S4). BCTs are effective in changing health care professional behaviour, for example, when used as part of technology‐based interventions (Keyworth, Hart, Armitage, & Tully, 2018), and should be used in interventions to increase health care professionals’ delivery of opportunistic behaviour change interventions. Recommendations for exemplar interventions based on our analysis may include providing on‐screen reminders for referral to smoking cessation services (intervention function: environmental restructuring; BCT: prompts/cues), or providing information about, and examples of, brief behaviour change interventions, and informing the health care professional they can feasibly be incorporated into time‐restricted consultations (intervention function: education; BCT: verbal persuasion to boost self‐efficacy). This must be done in parallel with understanding the specific content of behaviour change advice and examining its effectiveness on patient behaviour change. For example, whilst health care professionals may communicate the importance of behaviour change, specific strategies that patients can use to modify their behaviour are often absent from such discussions (Keyworth et al., 2016).
Strengths and limitations
Our findings provide a robust theoretical basis for future studies aimed at developing opportunistic behaviour change interventions in multiple health care professional groups by targeting four domains, namely beliefs about consequences, beliefs about capabilities, social/professional role and identity, and environmental context and resources. The sampling frame enabled recruitment of a wide range of views from diverse professional groups working in different medical professions, with varying priorities and opinions. Consequently, this enhances the depth and richness of the data (Dicicco‐Bloom & Crabtree, 2006). The theoretical framework enabled a synthesis of these views and identification of common barriers and enablers across all professions. Consequently, this study provides a series of recommendations for supporting health care professionals to deliver opportunistic behaviour change interventions. However, findings must also be considered in light of the workload pressures that are often faced by health care staff. There are limitations of this study. We used the COM‐B model to guide the interview questions, as opposed to the TDF. Whilst this allowed for emergent themes related to the TDF to be generated spontaneously and coded, tailoring questions directly to the TDF domains may have allowed for further insights to be obtained. This would also allow a more detailed analysis into the TDF domains that were less prominent in the current study. Our analysis adopted criteria focused on identifying the most prominent theoretical domains across professional groups (assessed quantitatively) and strong beliefs deemed to be important barriers and enablers to delivering interventions (assessed qualitatively). It is important to acknowledge: (1) using different methods for establishing domain importance may yield additional theoretical domains (Francis et al., 2014), and (2) the challenges associated with using the TDF framework, particularly given six of the constructs are allocated to more than one TDF domain (Cane et al., 2012). In addition, it is possible that by using alternative analytical approaches that focus on implementation, such as Normalization Process Theory (May et al., 2009), this may result in additional barriers that could not be explained by the TDF.
Conclusion
Health care professionals are willing and see the value of providing opportunistic behaviour change interventions as part of routine clinical interactions with patients, in accordance with public health strategies (Public Health England, 2016). However, there are a number of difficulties faced by health care professionals when attempting to deliver opportunistic behaviour change interventions. Using the BCW has: (1) identified the key targets for enhancing health care professionals’ capacity to deliver opportunistic behaviour change interventions to patients, and (2) identified BCTs that could be used as part of interventions to support this area of clinical practice. The four key theoretical domains associated with clinical practice identified in our study can be targeted by intervention designers. Internationally, public health strategies continue to compel health care professionals to deliver opportunistic behaviour change interventions as part of routine patient consultations, and for the first time, it is suggested it may be useful to target the specific barriers that are shared across professional groups. Developing health care professionals’ skills in relation to the four theoretical domains identified in our study would be an important step in increasing the delivery of opportunistic behaviour change interventions.
Supporting information
Table S1. Interview topic guide.
Table S2. The Theoretical Domains Framework. Definitions from Cane et al. (2012).
Table S3. COM‐B domains mapped to the TDF Domains. Adapted from Michie et al. (2014).
Table S4. Summary of key findings mapped to intervention functions and individual BCTs according to Michie et al. [1].
Acknowledgements
This study was funded by a research grant obtained from Tesco Plc and was supported by the NIHR Manchester Biomedical Research Centre. Tesco had no role in the design of this study and did not have any role during its execution, analyses, interpretation and storage of the data, or decision to submit results.
Conflict of interest
All authors declare no conflict of interest.
References
- Alexander, K. E. , Brijnath, B. , & Mazza, D. (2014). Barriers and enablers to delivery of the healthy kids check: An analysis informed by the Theoretical Domains Framework and COM‐B model. Implementation Science, 9, 60 10.1186/1748-5908-9-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins, L. , Francis, J. , Islam, R. , O'Connor, D. , Patey, A. , Ivers, N. , … Michie, S. (2017). A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation Science, 12, 77 10.1186/s13012-017-0605-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aveyard, P. , Lewis, A. , Tearne, S. , Hood, K. , Christian‐Brown, A. , Adab, P. , … Jebb, S. A. (2016). Screening and brief intervention for obesity in primary care: A parallel, two‐arm, randomised trial. Lancet, 388(10059), 2492–2500. 10.1016/s0140-6736(16)31893-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker, F. , de Lusignan, S. , & Cooke, D. (2016). Improving collaborative behaviour planning in adult auditory rehabilitation: Development of the I‐PLAN intervention using the behaviour change wheel. Annals of Behavioral Medicine, 52(6), 489–500. 10.1007/s12160-016-9843-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonner, C. , Jansen, J. , McKinn, S. , Irwig, L. , Doust, J. , Glasziou, P. , & McCaffery, K. (2015). How do general practitioners and patients make decisions about cardiovascular disease risk? Health Psychology, 34, 253–261. 10.1037/hea0000122 [DOI] [PubMed] [Google Scholar]
- Cane, J. , O'Connor, D. , & Michie, S. (2012). Validation of the Theoretical Domains Framework for use in behaviour change and implementation research. Implementation Science, 7, 37 10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cane, J. , Richardson, M. , Johnston, M. , Ladha, R. , & Michie, S. (2015). From lists of behaviour change techniques (BCTs) to structured hierarchies: Comparison of two methods of developing a hierarchy of BCTs. British Journal of Health Psychology, 20(1), 130–150. 10.1111/bjhp.12102 [DOI] [PubMed] [Google Scholar]
- Dicicco‐Bloom, B. , & Crabtree, B. F. (2006). The qualitative research interview. Medical Education, 40, 314–321. 10.1111/j.1365-2929.2006.02418.x [DOI] [PubMed] [Google Scholar]
- Duaso, M. J. , McDermott, M. S. , Mujika, A. , Purssell, E. , & While, A. (2014). Do doctors’ smoking habits influence their smoking cessation practices? A systematic review and meta‐analysis. Addiction, 109, 1811–1823. 10.1111/add.12680 [DOI] [PubMed] [Google Scholar]
- Elwell, L. , Povey, R. , Grogan, S. , Allen, C. , & Prestwich, A. (2013). Patients’ and practitioners’ views on health behaviour change: A qualitative study. Psychology and Health, 28, 653–674. 10.1080/08870446.2012.744008 [DOI] [PubMed] [Google Scholar]
- Elwell, L. , Powell, J. , Wordsworth, S. , & Cummins, C. (2014). Health professional perspectives on lifestyle behaviour change in the paediatric hospital setting: A qualitative study. BMC Pediatrics, 14, 71 10.1186/1471-2431-14-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epton, T. , Currie, S. , & Armitage, C. J. (2017). Unique effects of setting goals on behavior change: Systematic review and meta‐analysis. Journal of consulting and clinical psychology, 85(12), 1182. [DOI] [PubMed] [Google Scholar]
- Fie, S. , Norman, I. J. , & While, A. E. (2013). The relationship between physicians’ and nurses’ personal physical activity habits and their health‐promotion practice: A systematic review. Health Education Journal, 72(1), 102–119. 10.1177/0017896911430763 [DOI] [Google Scholar]
- Francis, J. J. , Duncan, E. M. , Prior, M. E. , Maclennan, G. , Marshall, A. P. , Wells, E. C. , … Cuthbertson, B. H. (2014). Comparison of four methods for assessing the importance of attitudinal beliefs: An international Delphi study in intensive care settings. British Journal of Health Psychology, 19, 274–291. 10.1111/bjhp.12066 [DOI] [PubMed] [Google Scholar]
- Francis, J. J. , Stockton, C. , Eccles, M. P. , Johnston, M. , Cuthbertson, B. H. , Grimshaw, J. M. , … Stanworth, S. J. (2009). Evidence‐based selection of theories for designing behaviour change interventions: Using methods based on theoretical construct domains to understand clinicians’ blood transfusion behaviour. British Journal of Health Psychology, 14, 625–646. 10.1348/135910708x397025 [DOI] [PubMed] [Google Scholar]
- Gale, N. K. , Heath, G. , Cameron, E. , Rashid, S. , & Redwood, S. (2013). Using the framework method for the analysis of qualitative data in multi‐disciplinary health research. BMC Medical Research Methodology, 13, 117 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould, N. J. , Lorencatto, F. , During, C. , Rowley, M. , Glidewell, L. , Walwyn, R. , … Francis, J. J. (2018). How do hospitals respond to feedback about blood transfusion practice? A multiple case study investigation. PLoS ONE, 13, e0206676 10.1371/journal.pone.0206676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guydish, J. , Passalacqua, E. , Tajima, B. , & Manser, S. T. (2007). Staff smoking and other barriers to nicotine dependence intervention in addiction treatment settings: A review. Journal of Psychoactive Drugs, 39, 423–433. 10.1080/02791072.2007.10399881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh, H. F. , & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15, 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Jansen, J. , McKinn, S. , Bonner, C. , Irwig, L. , Doust, J. , Glasziou, P. , … McCaffery, K. (2017). General practitioners’ decision making about primary prevention of cardiovascular disease in older adults: A qualitative study. PLoS ONE, 12(1), e0170228 10.1371/journal.pone.0170228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyworth, C. , Epton, T. , Goldthorpe, J. , Calam, R. , & Armitage, C. J. (2018). Are healthcare professionals delivering opportunistic behaviour change interventions? A multi‐professional survey of engagement with public health policy. Implementation Science, 13(1), 122 10.1186/s13012-018-0814-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyworth, C. , Hart, J. , Armitage, C. J. , & Tully, M. P. (2018). What maximizes the effectiveness and implementation of technology‐based interventions to support healthcare professional practice? A systematic literature review. BMC medical informatics and decision making, 18, 93 10.1186/s12911-018-0661-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyworth, C. , Nelson, P. A. , Chew‐Graham, C. A. , Kane, K. , Pearce, C. J. , Griffiths, C. E. , … Cordingley, L., (2016). Communicating cardiovascular disease risk to people with psoriasis: what techniques do practitioners use? International journal of behavioral medicine, 23(2), 168‐178. 10.1007/s12529-015-9517-8 [DOI] [PubMed] [Google Scholar]
- Lala, R. , Csikar, J. , Douglas, G. , & Muarry, J. (2017). Factors that influence delivery of tobacco cessation support in general dental practice: A narrative review. Journal of Public Health Dentistry, 77(1), 47–53. 10.1111/jphd.12170 [DOI] [PubMed] [Google Scholar]
- Landis, J. R. , & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- May, C. R. , Mair, F. , Finch, T. , MacFarlane, A. , Dowrick, C. , Treweek, S. , … Montori, V. M. (2009). Development of a theory of implementation and integration: Normalization Process Theory. Implementation Science, 4, 29 10.1186/1748-5908-4-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McParlin, C. , Bell, R. , Robson, S. C. , Muirhead, C. R. , & Araujo‐Soares, V. (2017). What helps or hinders midwives to implement physical activity guidelines for obese pregnant women? A questionnaire survey using the Theoretical Domains Framework. Midwifery, 49, 110–116. 10.1016/j.midw.2016.09.015 [DOI] [PubMed] [Google Scholar]
- McPhail, S. , & Schippers, M. (2012). An evolving perspective on physical activity counselling by medical professionals. BMC Family Practice, 13, 31 10.1186/1471-2296-13-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie, S. , Atkins, L. , & West, R. (2014). The behaviour change wheel: A guide to designing interventions. London, UK: Silverback. [Google Scholar]
- Michie, S. , & Johnston, M. (2013). Behavior change techniques In Gellman M. D. & Turner J. R. (Eds.), Encyclopedia of behavioral medicine (pp. 182–187). New York, NY: Springer, New York. [Google Scholar]
- Michie, S. , Stralen, M. M. , & West, R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6, 42 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Service (NHS) Yorkshire and the Humber . (2010). Prevention and Lifestyle Behaviour Change: A Competence Framework. Yorkshire and the Humber: NHS Retrieved from http://www.yorksandhumber.nhs.uk/document.php?o=5021
- Public Health England . (2016). Making Every Contact Count (MECC): Consensus statement. Leeds, UK: NHS England; Retrieved from https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/515949/Making_Every_Contact_Count_Consensus_Statement.pdf. [Google Scholar]
- Ritchie, J. , & Spencer, E. (1994). Qualitative data analysis for applied policy research In Bryman A. & Burgess R. (Eds.), Analyzing qualitative data. London, UK: Routledge. [Google Scholar]
- Stead, M. , Angus, K. , Holme, I. , Cohen, D. , Tait, G. , Peña, C. C. , … Costa, J. (2009). Factors influencing European GPs’ engagement in smoking cessation: A multi‐country literature review. British Journal of General Practice, 59, 682–690. 10.3399/bjgp09X454007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Um, I. S. , Armour, C. , Krass, I. , Gill, T. , & Chaar, B. B. (2013). Weight management in community pharmacy: What do the experts think? International Journal of Clinical Pharmacy, 35, 447–454. 10.1007/s11096-013-9761-4 [DOI] [PubMed] [Google Scholar]
- Vijay, G. C. , Wilson, E. C. , Suhrcke, M. , Hardeman, W. , & Sutton, S. (2016). Are brief interventions to increase physical activity cost‐effective? A systematic review. British Journal of Sports Medicine, 50, 408–417. 10.1136/bjsports-2015-094655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein, N. D. (1987). Unrealistic optimism about susceptibility to health problems: Conclusions from a community‐wide sample. Journal of Behavioral Medicine, 10, 481–500. 10.1007/BF00846146 [DOI] [PubMed] [Google Scholar]
- Wells, M. , Aitchison, P. , Harris, F. , Ozakinci, G. , Radley, A. , Bauld, L. , … Williams, B. (2017). Barriers and facilitators to smoking cessation in a cancer context: A qualitative study of patient, family and professional views. BMC Cancer, 17, 348 10.1186/s12885-017-3344-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock, E. P. , Orleans, C. T. , Pender, N. , & Allan, J. (2002). Evaluating primary care behavioral counseling interventions: An evidence‐based approach. American Journal of Preventive Medicine, 22, 267–284. 10.1016/S0749-3797(02)00415-4 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2017). Fact sheet: Noncommunicable diseases , June 2017 Retrieved from http://www.who.int/mediacentre/factsheets/fs311/en/.
- Yousefzadeh, A. , Chung, F. , Wong, D. T. , Warner, D. O. , & Wong, J. (2016). Smoking cessation: The role of the anesthesiologist. Anesthesia and Analgesia, 122, 1311–1320. 10.1213/ane.0000000000001170 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Interview topic guide.
Table S2. The Theoretical Domains Framework. Definitions from Cane et al. (2012).
Table S3. COM‐B domains mapped to the TDF Domains. Adapted from Michie et al. (2014).
Table S4. Summary of key findings mapped to intervention functions and individual BCTs according to Michie et al. [1].


