Abstract
Aims
Despite increased recognition as a chronic disease, obesity remains greatly underdiagnosed and undertreated. We aimed to identify international perceptions, attitudes, behaviours and barriers to effective obesity care in people with obesity (PwO) and healthcare professionals (HCPs).
Materials and methods
An online survey was conducted in 11 countries. Participants were adults with obesity and HCPs who were primarily concerned with direct patient care.
Results
A total of 14 502 PwO and 2785 HCPs completed the survey. Most PwO (68%) and HCPs (88%) agreed that obesity is a disease. However, 81% of PwO assumed complete responsibility for their own weight loss and only 44% of HCPs agreed that genetics were a barrier. There was a median of three (mean, six) years between the time PwO began struggling with excess weight or obesity and when they first discussed their weight with an HCP. Many PwO were concerned about the impact of excess weight on health (46%) and were motivated to lose weight (48%). Most PwO (68%) would like their HCP to initiate a conversation about weight and only 3% were offended by such a conversation. Among HCPs, belief that patients have little interest in or motivation for weight management may constitute a barrier for weight management conversations. When discussed, HCPs typically recommended lifestyle changes; however, more referrals and follow‐up appointments are required.
Conclusions
Our international dataset reveals a need to increase understanding of obesity and improve education concerning its physiological basis and clinical management. Realization that PwO are motivated to lose weight offers an opportunity for HCPs to initiate earlier weight management conversations.
Keywords: ACTION‐IO, attitudes, barriers, international, obesity, perceptions
1. INTRODUCTION
Obesity is a serious, chronic, relapsing disease with a high prevalence and a substantial unmet medical need.1, 2 This complex disease is influenced by multiple factors including genetics, physiological factors, psychological issues and environmental variables, both physical and social, and it affects individuals of all ages and regions.2, 3, 4 Obesity is associated with multiple complications and an increased risk of disability and mortality.5, 6, 7 Individuals living with obesity experience stigma, discrimination and a negative impact on both mental and health‐related quality of life.4, 7, 8
Treatment guidelines for people with obesity (PwO) typically recommend lifestyle interventions with addition of pharmacotherapy if response to dietary, physical activity and behavioural changes alone is insufficient to reach or maintain the recommended goal of 5%–10% loss in body weight.9, 10, 11, 12, 13, 14, 15 Bariatric surgery should be considered for severe cases (body mass index [BMI] ≥40 kg/m2 or ≥35 kg/m2 with obesity‐related complications) and may be considered for PwO (BMI ≥30 kg/m2) with poorly controlled type 2 diabetes.9, 10, 11, 12, 13, 14, 15 Despite the availability of these guidelines, in practice, PwO experience variable care.16, 17, 18 The Awareness, Care, and Treatment In Obesity maNagement (ACTION) survey study conducted in the USA identified low rates of obesity diagnosis and management.19 In another survey of 1506 healthcare professionals (HCPs) in the USA, most (84%) demonstrated limited knowledge of obesity treatment guidelines.20 An international study of 335 HCPs suggested a disconnect between HCPs' confidence in their ability to manage patients with excess weight and their effectiveness in achieving weight loss goals.21
To improve the quality of, and access to, obesity care globally, a better understanding of the disease and the way those with obesity are currently, and should be, managed is required. The objective of the ACTION International Observation (ACTION‐IO) study was to identify the perceptions, attitudes and behaviours of PwO and HCPs and to assess the potential barriers to effective obesity care on an international scale. Here we report the primary results from the ACTION‐IO study which, to our knowledge, is the largest international survey of PwO and HCPs to date.
2. METHODS
2.1. Study design and participants
The ACTION‐IO study was a cross‐sectional, non‐interventional, descriptive study that collected data via an online survey conducted by a third‐party vendor (KJT Group, Honeoye Falls, New York), utilizing existing databases/panels in 11 countries across different world regions (Australia, Chile, Israel, Italy, Japan, Mexico, Saudi Arabia, South Korea, Spain, the UAE and the UK) between 4 June 2018 and 15 October 2018. It was intended to also include Brazil, but it was not possible to obtain local ethics committee approval within the required timelines.
Eligible PwO were 18 years or older and were residents of a participating country, with a current BMI, based on self‐reported height and weight, of at least 30 kg/m2 or at least 25 kg/m2 in Japan and South Korea, as per country‐specific definitions of obesity.22 PwO were excluded if they declined to provide information concerning income, with the exception of Mexico as required by the local ethics committee, or concerning race/ethnicity, in Australia and the UAE only, if they were pregnant, if they participated in intense fitness or body building programmes or if they had experienced significant, unintentional weight loss during the past 6 months. Eligible HCPs were medical practitioners in a participating country, who had been in practice for 2 years or more, with at least 70% of their time involved in direct patient care and who had seen 100 or more patients during the past month, at least ten of whom had a BMI of at least 30 kg/m2, or 25 kg/m2 in Japan and South Korea. HCPs specializing in general, plastic or bariatric surgery were excluded.
All respondents provided electronic informed consent prior to initiation of the screening questions and survey. A local ethics committee/independent review board approved the questionnaires in Australia, Israel, Mexico, Saudi Arabia, South Korea, Spain, the UAE and the UK, where such approval was required. For Chile, Italy and Japan, ethical approval was determined to be non‐essential for a study of this nature based on regulatory standards and precedent. The study complied with all laws and regulations regarding management of personal information as required by the participant's country of residence and the European General Data Protection Regulation. The study was conducted in accordance with the Guidelines for Good Pharmacoepidemiology Practices23 and is registered with ClinicalTrials.gov, number NCT03584191.
2.2. Survey development and pre‐testing
Two questionnaires, one for PwO and one for HCPs (Appendix S1, pages 28–139), were developed by an international steering committee of obesity experts, representing primary care, medical specialities and psychology, from the participating countries, in addition to three medical doctors employed by the sponsor, Novo Nordisk. The questionnaires were based on those used in the ACTION US19 and ACTION Canada studies,24 with minor modification or removal of some original questions to reduce survey length, increase data quality and ensure that questions were relevant to the study objectives. KJT Group conducted 60‐minute web‐assisted pre‐tests with four PwO and four HCPs in each country; participants took the survey online while speaking with a moderator by telephone, or in‐person in Japan, Saudi Arabia, South Korea, and the UAE. This was to assess clarity, face validity and relevance of the questions. Surveys were designed to facilitate comparisons within and across respondent types.
2.3. Procedures
KJT Group oversaw all aspects of data collection and reporting. Data were collected through an online survey programmed by KJT Group, using Decipher Survey Software (FocusVision Worldwide Inc., Stamford, Connecticut). To reduce PwO sampling bias and ensure that the group was largely representative of the general population, the outbound sample was sent according to pre‐determined demographic targets based on gender, age, income, race/ethnicity, in select countries, and region. Targets were established based on data from the 2011 International Standard Classification of Education and the US Census Bureau, International Data Base and other public data. Prior to participation, respondents were blinded to the specific study goals, being informed that the purpose was “to determine treatment experiences of patients with a specific condition”. All individuals could access the first part of the survey, and an initial set of screening questions determined eligibility based on the demographic targets; subsequently, only respondents who had obesity, as determined from their self‐reported height and weight, and who met the other eligibility requirements as detailed in the Study design and participants section, proceeded into the full survey. Demographic targets were monitored throughout data collection to ensure population representativeness.
Respondents were compensated for their time and were recruited, for the most part, via online panel companies to whom they had given permission to be contacted for research purposes (Appendix S1, page 2). Respondents were recruited through email where possible, with telephone and in‐person recruitment also used for PwO in Saudi Arabia and the UAE and for HCPs in Chile, Japan, Israel, Mexico, Saudi Arabia, South Korea and the UAE. Respondents completed the survey in the native language of their country. In‐person administration of the online survey was permitted for PwO in Saudi Arabia and the UAE and for HCPs in Chile, Japan, Israel, Mexico, Saudi Arabia, South Korea and the UAE (Appendix S1, page 2). All respondents could suspend taking the survey at any time and for any reason at any part of the survey. Participants were allowed to complete the survey only once, as assessed by prior online consent and digital fingerprinting (Appendix S1, page 2). To avoid bias, questionnaire items were carefully phrased and presented in the same order for each respondent and items in a list were displayed alphabetically, categorically, chronologically or randomly, as relevant for each response set.
2.4. Outcomes
Outcomes were measured by multiple item selection (weight loss motivators, effective weight loss methods, types of weight management goals, most helpful information for patients concerning weight loss, responsibility for improving health of PwO, most helpful support for weight loss and ways information concerning weight loss management is received), numeric response (proportion of PwO who made a serious weight loss effort), single item selection (response to weight loss discussions), end‐anchored 5‐point Likert agreement scales (attitudes toward obesity, attitudes toward prescription weight loss medication and surgery, weight loss barriers, obesity and weight management, and the degree to which healthcare and society are meeting the needs of PwO), fully anchored 5‐point Likert scales (effectiveness of guidelines for treating obesity) and by ranking (top factors for improving weight loss outcomes). Some of these outcomes will be published separately.
2.5. Analysis
The target sample size, based on 12 participating countries, was 19 700 completed surveys, comprising 16 500 PwO (750–2000 per country) and 3200 HCPs (200–300 per country; 1600 primary care professionals [PCPs] plus 1600 non‐PCP specialists), to balance statistical power, recruitment feasibility and cost.
Analysis of de‐identified data was conducted by KJT Group using SPSS (IBM, version 23.0), Stata (StataCorp LLC, version IC 14.2) and Excel (Microsoft, version 2016). Data were summarized using univariate descriptive statistics (means, medians, frequencies) and tests of differences (chi square, t‐tests) within PwO or HCP respondent types were performed. Statistical significance was set at P < 0.05, using 2‐tailed tests. Adjustment for multiple testing was not undertaken as this research was exploratory and descriptive in nature. Only data from those who completed the survey were included in the analyses.
The final PwO sample, including those failing to qualify for the survey, was weighted to representative demographic targets within each country for age, gender, household income, education and region (Appendix S1, page 4). HCP data were not weighted.
3. RESULTS
A total of 14 502 PwO and 2785 HCPs completed the survey (Table 1 and Figure S1) as per the target sample size for 11 participating countries. The mean response rate was 20% for PwO and 17% for HCPs; the mean eligibility rate was 19% for PwO and 61% for HCPs; and the mean completion time was 28 minutes for PwO and 35 minutes for HCPs (Appendix S1, page 5).
Table 1.
Sample demographics and characteristics
| PwO (n = 14 502) | HCPs (n = 2785) | |
|---|---|---|
| Age, years | 43 (18–88) | 48 (26–74) |
| Gender | ||
| Male | 7438 (51%) | 1958 (70%) |
| Female | 7050 (49%) | 827 (30%) |
| Other | 14 (<1%) | 0 |
| Country | ||
| Australia | 1000 (7%) | 200 (7%) |
| Chile | 1000 (7%) | 200 (7%) |
| Israel | 750 (5%) | 169 (6%) |
| Italy | 1501 (10%) | 302 (11%) |
| Japan | 2001 (14%) | 302 (11%) |
| Mexico | 2000 (14%) | 400 (14%) |
| Saudi Arabia | 1000 (7%) | 200 (7%) |
| South Korea | 1500 (10%) | 200 (7%) |
| Spain | 1500 (10%) | 306 (11%) |
| UAE | 750 (5%) | 200 (7%) |
| UK | 1500 (10%) | 306 (11%) |
| BMI classification for Australia, Chile, Israel, Italy, Mexico, Saudi Arabia, Spain, UAE and UKa | ||
| Respondents | 11 001 (100%) | 1778 (78%) |
| Underweight or healthy range (<25 kg/m2) | – | 971 (55%) |
| Overweight (25–29.9 kg/m2) | – | 668 (38%) |
| Obesity Class I (30–34.9 kg/m2) | 6930 (63%) | 103 (6%) |
| Obesity Class II (35–39.9 kg/m2) | 2416 (22%) | 12 (1%) |
| Obesity Class III (≥40 kg/m2) | 1655 (15%) | 24 (1%) |
| BMI classification for Japan and South Koreab | ||
| Respondents | 3501 (100%) | 418 (83%) |
| BMI <25 kg/m2 | – | 325 (78%) |
| Obesity Class 1 (25–29.9 kg/m2) | 2696 (77%) | 83 (20%) |
| Obesity Class 2 (30–34.9 kg/m2) | 530 (15%) | 9 (2%) |
| Obesity Class 3 (35–39.9 kg/m2) | 134 (4%) | 0 |
| Obesity Class 4 (≥40 kg/m2) | 141 (4%) | 1 (<1%) |
| Number of comorbidities | ||
| 0 | 3829 (26%) | |
| 1 | 3610 (25%) | |
| 2 | 2868 (20%) | |
| 3 | 2060 (14%) | |
| ≥4 | 2136 (15%) | |
| HCP category | ||
| PCP | 1415 (51%) | |
| Specialist | 1370 (49%) | |
| Diabetologist/endocrinologist | 488 (18%) | |
| Cardiologist | 301 (11%) | |
| Internal medicine (non‐PCP) | 272 (10%) | |
| Gastroenterologist | 160 (6%) | |
| Obstetrician/gynaecologist | 133 (5%) | |
| Nutritionist (Italy only) | 9 (<1%) | |
| Bariatrics/obesity medicinec | 5 (<1%) | |
| Hepatologist (Australia only) | 2 (<1%) | |
| Obesity specialistd | ||
| Yes | 1868 (67%) | |
| No | 917 (33%) | |
Data are median (range) or number (%) and are reported for the final unweighted sample.
Abbreviations: BMI, body mass index; HCP, healthcare professional; PwO, people wth obesity; PCP, primary care physician.
Classes I (BMI 30–34.9 kg/m2), II (BMI 35–39.9 kg/m2) and III (BMI ≥40 kg/m2) apply to Australia, Chile, Israel, Italy, Mexico, Saudi Arabia, Spain, the UAE and the UK.
Classes 1 (BMI 25–29.9 kg/m2), 2 (BMI 30–34.9 kg/m2), 3 (BMI 35–39.9 kg/m2) and 4 (BMI ≥40 kg/m2) apply to Japan and South Korea.
Bariatric surgeons were ineligible per protocol pre‐specified criteria.
A physician who meets at least one of the following criteria: at least 50% of their patients are seen for obesity/weight management, or has advanced/formal training in treatment of obesity/weight management beyond medical school, or considers themself to be an expert in obesity/weight loss management, or works in an obesity service clinic.
A total of 68% of PwO and 88% of HCPs agreed with the statement that obesity is a chronic disease (Figure S2A). Most PwO (82%) and HCPs (76%) believed that obesity has a large impact on overall health (Figure S2B). In comparison, 75%–85% of PwOs and 82%–93% of HCPs stated that diabetes, stroke, cancer or chronic obstructive pulmonary disease has a large impact on overall health. Despite recognizing obesity as a disease that impacts overall health, most PwO assumed full responsibility for weight loss (81%) and considered lifestyle a key factor in their struggle with obesity (63%) (Figure 1; see Figure S3 for complete data). Also, 30% of HCPs placed the responsibility for weight loss on PwO, and 79% agreed that their patients would need to completely change their lifestyle to lose weight. Only 31% of HCPs thought their patients were motivated to lose weight, whereas 48% of PwO said they were motivated to lose weight (Figure 1) and only 20% of PwO had no plans for weight loss within the next 6 months (Figure S4). Most PwO and HCPs considered unhealthy eating habits (62% of PwO; 89% of HCPs) and lack of exercise (73% of PwO; 88% of HCPs) as barriers to weight loss, whereas fewer than half considered the genetic factors underlying obesity (33% of PwO; 44% of HCPs) to be a barrier (Figure S5).
Figure 1.
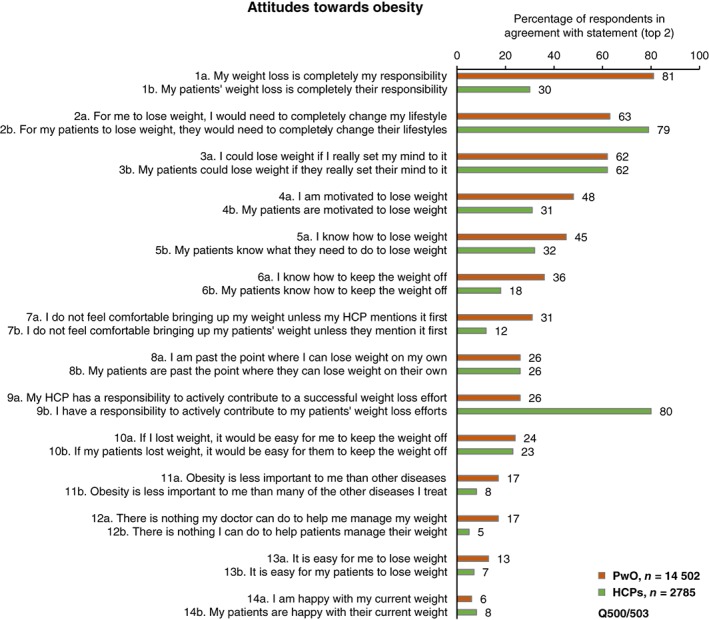
PwO and HCP agreement with statements regarding attitudes towards obesity. Rated on a scale of 1–5. HCPs = green; PwO = orange. Abbreviations: HCP, healthcare professional; PwO, people with obesity
A total of 81% of PwO stated that they had made at least one serious weight loss effort in the past (Figure 2A). Conversely, on average, HCPs reported that only 35% of their patients with obesity had made a serious weight loss effort (Figure 2B). Of patients who had made a serious weight loss attempt in the past year, the mean proportion defined by HCPs as responding successfully was 30% (Figure S6). A substantial proportion of PwO (62%) believed they could lose weight if they set their mind to it (Figure 1). However, many PwO struggled to lose weight and to maintain weight loss (Figure 2C,D); only 37% of PwO reported weight loss of at least 5% body mass over the past 3 years and, among those, only 29% were able to maintain the weight loss for at least 1 year (11% of PwO total).
Figure 2.
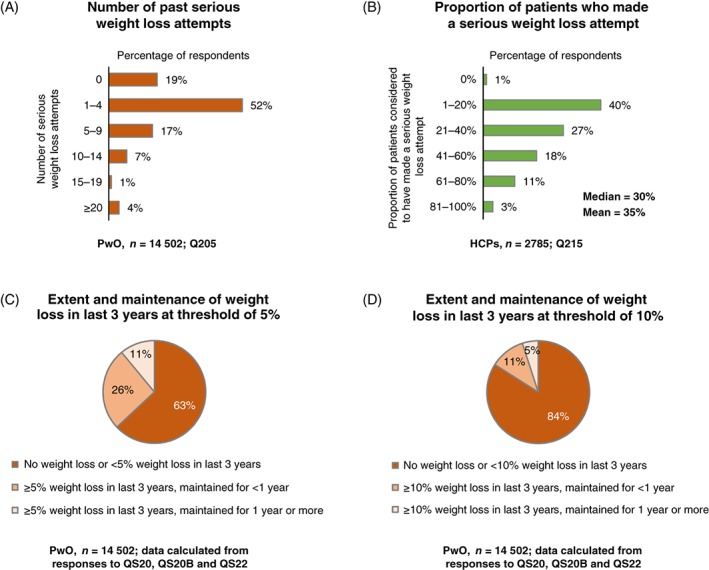
Weight loss efforts and response to intervention. A, Number of previous serious weight loss attempts (PwO). B, Proportion of patients considered to have made a serious weight loss attempt reported by HCPs. C,D, PwO extent and maintenance of weight loss in previous 3 years at threshold of C, 5% or D, 10% of total body weight. HCPs = green; PwO = orange. Abbreviations: HCP, healthcare professional; PwO, people with obesity
Only approximately half of all PwO had discussed their weight with an HCP in the past 5 years (Figure 3A). It took a median of 3 years and a mean of 6 years between the reported time that PwO first began struggling with excess weight or obesity and when they first had a weight management conversation with an HCP (Figure 3B). Moreover, 46% of the PwO who discussed weight with an HCP initiated the conversation themselves (Figure S7A). In contrast, on average, HCPs reported discussing weight with 68% of their patients with obesity, with the patient initiating the conversation only one third of the time (Figure S7B). The main reason provided by HCPs for initiating a weight management conversation was obesity‐related complications (Figure S8).
Figure 3.
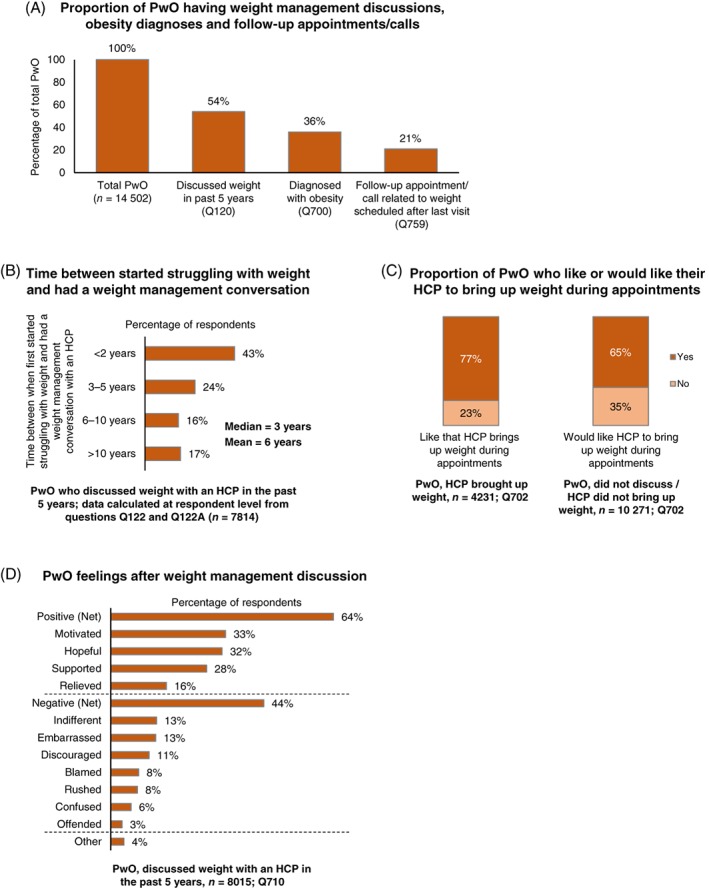
Weight management conversations and outcomes. A, Proportion of PwO having had weight management discussions with an HCP, obesity diagnoses and follow‐up appointments/calls. B, Of PwO who had discussed their weight with an HCP during the past 5 years, proportion who had the discussion less than 2 years, 3–5 years, 6–10 years or more than 10 years after they first began struggling with their weight. C, Proportion of PwO who like or would like their HCP to bring up weight during appointments. D, PwO feelings after discussing their weight with an HCP. Abbreviations: HCP, healthcare professional; PwO, people with obesity
Among PwO who had discussed their weight with an HCP during the past 5 years, 67% had been diagnosed with obesity in the past (36% of PwO in total) (Figure 3A). On average, HCPs informed their patients with obesity that they had a diagnosis of obesity 75% of the time and 6% of HCPs never informed their patients of a diagnosis of obesity (Figure S9). Only 39% of PwO who had discussed their weight with an HCP were scheduled for a follow‐up appointment (21% of PwO in total) (Figure 3A); however, 94% of PwO reported attending or planning to attend a follow‐up appointment if scheduled (Figure S10A). On average, HCPs scheduled follow‐up appointments with 44% of their patients to discuss obesity; 55% of HCPs reported that patients kept these follow‐up appointments always or most of the time (Figure S10B).
Among all PwO, 41% would set themselves an ambitious weight loss target of 11%–20% (overall mean 16%) (Figure S11A). PwO reported receiving similar recommended targets from HCPs (overall mean 17%) (Figure S11B). The weight management goals most frequently selected by PwO were to reduce the risks associated with excess weight and to prevent a health condition (46%) and to improve appearance (33%) (Figure S12).
The most frequent methods for managing weight discussed between PwO and HCPs were general improvement in eating habits and general increase in physical activity level, whereas specific diet or exercise programmes, tracking, weight loss medications and bariatric surgery were less likely to have been discussed (Figure S13A). Referrals to specialists were recommended infrequently (Figure S13A). General improvements in eating habits and physical activity were perceived to be highly effective by most PwO and HCPs; however, more PwO than HCPs perceived weight loss medications and bariatric surgery to be effective (Figure S13B).
A total of 35% of PwO found that conversations with an HCP concerning weight management were very or extremely helpful (Figure S14); and 68% of PwO liked the fact that their HCP brought up the subject of weight, or would like them to do so (Figure 3C). Conversations with HCPs concerning weight management can be quite motivating and positive for PwO, with 64% reporting positive feelings after such a conversation (Figure 3D). Negative feelings after a conversation concerning weight loss were reported by 44% of PwO. However, only 3% of PwO reported feeling offended (Figure 3D).
The main reason provided by PwO for not discussing weight management with their HCP was a belief that it was their own responsibility to manage their weight (reported by 44% of PwO vs 9% of HCPs), whereas the main reason provided by HCPs for not discussing obesity with a patient was their perception that the patient was not interested in losing weight (reported by 71% of HCPs vs 7% of PwO) (Figure 4; see Figure S15 for complete data). More than half of the HCPs surveyed indicated that the limited appointment time is also a factor in not discussing weight loss (Figure 4). Data concerning other outcomes are presented in Figures S16–S19.
Figure 4.
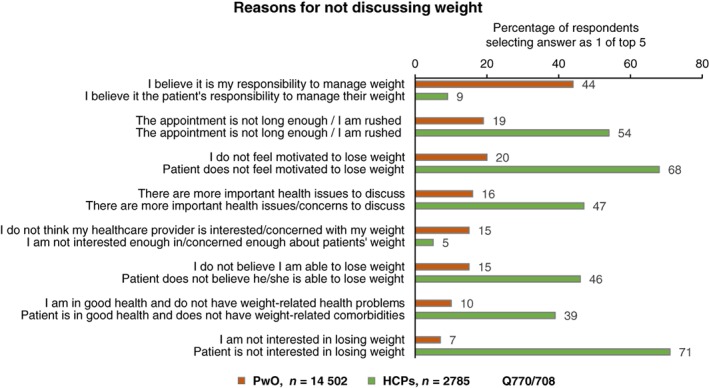
Reasons for not discussing weight with an HCP (PwO, orange) or patient (HCPs, green), with at least 10% difference between PwO and HCPs. See Supporting Information Figure S15 for all reasons. HCPs = green; PwO = orange. Abbreviations: HCP, healthcare professional; PwO, people with obesity
4. DISCUSSION
The ACTION‐IO study identified several key gaps in obesity care and a misalignment between the perceptions and attitudes of PwO and HCPs. Both PwO and HCPs stated that they recognized obesity as a chronic disease; however, most PwO assumed complete responsibility for weight loss. Furthermore, both PwO and HCPs put emphasis on lifestyle‐related factors rather than biological factors, including genetic predisposition, as being significant barriers to weight loss. The results suggest that many PwO are concerned about the impact of excess weight on their health and are making serious efforts to lose weight, but they have a limited response to such weight loss efforts on their own. In contrast, the fact that HCPs believe that PwO are not interested or motivated to lose weight may be preventing conversations concerning weight loss. This might reflect the actual experience of HCPs or may represent an unconscious negative bias.
Obesity is recognized as a chronic disease by several national and international organizations including the World Obesity Federation,1 the European Association for the Study of Obesity,11 The Obesity Society,25 the American Medical Association26 and the UK Royal College of Physicians.27 Obesity involves a genetic predisposition and specific pathophysiological alterations, and it is not simply the result of lifestyle.3, 4 However, only 26% of PwO in this study believed that their HCP has a responsibility to actively contribute to their weight loss efforts. Other studies have previously highlighted a disconnection between perceptions and actions. In a study in Australia, 78% of PwO agreed that their HCP had a role in their weight management, but only 58% would ask their HCP for advice concerning weight loss.28
Compared with the US ACTION study, a smaller proportion of PwO in this international study had discussed their weight with an HCP in the past 5 years (US ACTION, 71%; ACTION‐IO, 54%); but among those, a greater proportion had received a diagnosis of obesity (US ACTION, 55%; ACTION‐IO, 67%).19 A similar proportion of PwO in the USA and internationally thought weight loss was completely their responsibility (US ACTION, 82%; ACTION‐IO, 81%), and this was the main reason that PwO did not initiate a weight management conversation with an HCP in both studies.19 In the USA, HCPs cited lack of time as a main reason for not initiating weight loss conversations,19 whereas, internationally, HCPs cited limited patient motivation or patient disinterest in losing weight as the main reasons, in stark contrast to the responses of PwO, and reflecting a need for education.
A potential barrier to effective obesity care that was identified here was the length of time (years) between when PwO began struggling with their weight and when they first had a weight management conversation with an HCP. Decreasing this time gap could reduce the complications of obesity experienced by PwO and, ultimately, would lessen the economic burden of the disease.6, 7 Appropriate and supportive weight management conversations should be initiated earlier as a preventive approach, before complications occur. Jointly agreeing that a patient has overweight or obesity, with a BMI calculation in the context of their personal health profile, may be an effective way to initiate such a conversation.29 Discussing the genetic component and biological contributors to obesity4, 30 with the patient, using explanatory illustrations that are tailored to the patient's knowledge base, where relevant, could help to diminish self‐blame and could encourage a continued dialogue and receptiveness to support from the HCP. Recognizing positive patient responses to conversational cues may allow for therapeutic intervention or development of a management plan.9, 15, 31
Our data suggest that PwO are motivated to engage in weight loss efforts and would like their HCPs to initiate a conversation about weight. This is consistent with a UK study showing that most patients found discussing their weight with an HCP appropriate and helpful.32 As obesity is a chronic disease, there is also a need to improve referrals and follow‐up appointments for management of obesity. Part of this effort calls for eradication of the prevalent stigmatizing attitudes that are highlighted in prior studies33 and for eradication of HCPs' misperception that PwO are not motivated, as shown here.
The weight loss targets reported in this study were higher than those achievable for most PwO with existing non‐surgical interventions, as demonstrated by the low proportion of PwO who achieved and maintained a weight loss of at least 10%. Setting realistic and achievable weight loss goals could contribute to management of expectations, with collaborative communication and more manageable targets potentially providing encouragement for continued patient engagement. Guidelines suggest a weight loss goal of 5%–10%, depending on the severity of obesity, over a period of 6 months.10 However, even a 3%–5% reduction in weight can provide clinically meaningful health benefits.34 Opportunities for improving obesity management include: improving education of PwO, HCPs, HCP students, governments and the public in general concerning the biological basis of obesity; challenging the misperception that obesity is under an individual's control;33 obtaining unanimous recognition of obesity as a chronic progressive disease; addressing HCPs' attitudes towards PwO; promoting earlier initiation of helpful weight loss conversations; improving education of HCPs and HCP students concerning clinical management of obesity, including effective advice on diet and physical activity, as well as medical and surgical therapy, while emphasizing the value of a multidisciplinary approach;9, 10, 11, 12, 13, 14, 15 and increasing the frequency of diagnosis, follow‐up appointments and referrals for effective evidence‐based treatment. Obesity is an adiposity‐based chronic disease, the complexity of which cannot be reflected by BMI alone,35 and this may contribute to the reluctance of HCPs to provide a diagnosis of obesity. However, as recommended by current clinical practice guidelines, BMI is used for the initial assessment and diagnosis of obesity, taking into account factors such as age, ethnicity and muscularity.9, 10, 11, 12, 13, 14, 15
Limitations of this study include the cross‐sectional and descriptive nature, reliance on self‐reported height and weight, which could underestimate BMI, and the accuracy of respondent recall. The fairly low response rates are typical for survey‐based research (Appendix S1, page 5). Low response rates can affect sample representativeness and are a known limitation of this type of study. Internet access could also have restricted participation in some countries. Strengths of the study include the large number of respondents, the international nature of the study and the scientific rigor with which the survey was designed and implemented, including stratified sampling to provide a cohort representative of the general population.
Overall, our data suggest that PwO are motivated to lose weight and that there is an opportunity for HCPs to initiate earlier, effective weight loss conversations with minimal fear of offence. PwO may not recognize the need to reduce excess weight until it has an impact on their health, further supporting the requirement for HCPs to raise the topic of weight before such obesity‐related complications occur. Our study also reveals a global need for improved education of both PwO and HCPs concerning the biological basis and clinical management of obesity, and for a more positive attitude on the part of HCPs towards initiating discussions with PwO concerning weight and weight management.
CONFLICT OF INTEREST
All authors received funding for travel expenses from Novo Nordisk to attend author meetings during the conduct of the study. I. D. C. reports personal fees from Novo Nordisk (as chair of the ACTION‐IO steering committee) during the conduct of the study, grants from Novo Nordisk, Bristol‐Myers Squibb, Pfizer and Australian Eggs outside the submitted work, and personal (lecture) fees from Servier Laboratories and Novo Nordisk outside the submitted work. A. A. reports financial support from Novo Nordisk to attend an obesity conference during the conduct of the study, and personal (consultancy) fees and non‐financial support from Novo Nordisk outside the submitted work. W. C. reports personal (consultancy and speaker) fees from Novo Nordisk, EMS, Germed Pharma and Janssen Pharmaceutica outside the submitted work. A. C. reports personal fees from Abbott, Novo Nordisk, Teva Pharmaceutical Industries and Saval Pharmaceuticals during the conduct of the study; she is a member of the Strategic Centre for Obesity Professional Education (SCOPE) of the World Obesity Federation and a SCOPE International Fellow. D. D. reports personal (consultancy and speaker) fees from Novo Nordisk during the conduct of the study and personal (consultancy and speaker) fees from Novo Nordisk and Teva Pharmaceutical Industries outside the submitted work. C. H. reports financial support from Novo Nordisk to attend an obesity conference during the conduct of the study, grants from the Rona Marsden Fund at Fakenham Medical Practice and personal fees from Orexigen Therapeutics, Consilient Health, Nestlé and Ethicon outside the submitted work; she was previously a member of the World Obesity education committee, is a current member of the Association for the Study of Obesity (ASO) and is involved in meetings to facilitate recognition of obesity as a disease in the UK. R. N. reports financial support from Novo Nordisk to attend an obesity conference during the conduct of the study, and personal (consultancy and speaker) fees from Novo Nordisk outside the submitted work. G. R. reports personal (consultancy) fees from Apollo Endosurgery (previously known as Allergan), Medtronic (previously known as Covidien), mdBriefCase Global & Australia, NSW Health and the Australian Department of Health, personal fees and non‐financial support (consultancy/meetings and travel expenses) from the Royal Australian College of General Practitioners (RACGP), Novo Nordisk and iNova Pharmaceuticals outside the submitted work; she is Chair of the RACGP Obesity Management Network. J. S. reports personal (consultancy) fees from Novo Nordisk outside the submitted work. P. S. reports personal fees from Novo Nordisk during the conduct of the study. V. V. V. reports personal fees and non‐financial support from Novo Nordisk during the conduct of the study. J. H. reports personal fees (honoraria) from Novo Nordisk during the conduct of the study. P. A., R. R. and N. R. are employees of Novo Nordisk, and N. R. and R. R. own shares in Novo Nordisk. M. I. and J.‐H. K. disclose no conflits of interest.
AUTHOR CONTRIBUTIONS
All authors contributed to the design of the study. All authors participated in interpretation of the data and drafting and revision of the manuscript. All authors reviewed and approved the final, submitted version.
Supporting information
Appendix S1.
ACKNOWLEDGMENTS
We gratefully acknowledge the study participants and all personnel involved in the study. We thank Craig Radley and Lynn Clement of KJT Group, especially, for data collection and analysis.
This study was sponsored by Novo Nordisk which also provided financial support for medical editorial assistance from Abbie Saunders, PhD CMPP of Articulate Science.
Caterson ID, Alfadda AA, Auerbach P, et al. Gaps to bridge: Misalignment between perception, reality and actions in obesity. Diabetes Obes Metab. 2019;21:1914–1924. 10.1111/dom.13752
Funding information This study was sponsored by Novo Nordisk.
Peer Review The peer review history for this article is available at https://publons.com/publon/10.1111/dom.13752.
REFERENCES
- 1. Bray GA, Kim KK, Wilding JPH, World Obesity Federation . Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18:715‐723. [DOI] [PubMed] [Google Scholar]
- 2. Ralston J, Brinsden H, Buse K, et al. Time for a new obesity narrative. Lancet. 2018;392:1384‐1386. [DOI] [PubMed] [Google Scholar]
- 3. Bray GA, Fruhbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387:1947‐1956. [DOI] [PubMed] [Google Scholar]
- 4. Ghanemi A, Yoshioka M, St‐Amand J. Broken energy homeostasis and obesity pathogenesis: the surrounding concepts. J Clin Med. 2018;7:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Prospective Studies Collaboration , Whitlock G, Lewington S, et al. Body‐mass index and cause‐specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083‐1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14:E435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. GBD 2015 Obesity Collaborators , Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sikorski C, Luppa M, Kaiser M, et al. The stigma of obesity in the general public and its implications for public health ‐ a systematic review. BMC Public Health. 2011;11:661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Institute of Health and Care Excellence . Obesity: identification, assessment and management; 2014. https://www.nice.org.uk/guidance/cg189/resources/obesity-identification-assessment-and-management-pdf-35109821097925. Accessed January 15, 2019. [PubMed]
- 10. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S102‐S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yumuk V, Tsigos C, Fried M, et al. European guidelines for obesity management in adults. Obes Facts. 2015;8:402‐424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Abusnana S, Fargaly M, Alfardan SH, et al. Clinical practice recommendations for the management of obesity in The United Arab Emirates. Obes Facts. 2018;11:413‐428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alfadda AA, Al‐Dhwayan MM, Alharbi AA, et al. The Saudi clinical practice guideline for the management of overweight and obesity in adults. Saudi Med J. 2016;37:1151‐1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22:842‐884. [DOI] [PubMed] [Google Scholar]
- 15. Welbourn R, Hopkins J, Dixon JB, et al. Commissioning guidance for weight assessment and management in adults and children with severe complex obesity. Obes Rev. 2018;19:14‐27. [DOI] [PubMed] [Google Scholar]
- 16. Glauser TA, Roepke N, Stevenin B, Dubois AM, Ahn SM. Physician knowledge about and perceptions of obesity management. Obes Res Clin Pract. 2015;9:573‐583. [DOI] [PubMed] [Google Scholar]
- 17. Rurik I, Torzsa P, Ilyés I, et al. Primary care obesity management in Hungary: evaluation of the knowledge, practice and attitudes of family physicians. BMC Fam Pract. 2013;14:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bocquier A, Verger P, Basdevant A, et al. Overweight and obesity: knowledge, attitudes, and practices of general practitioners in France. Obes Res. 2005;13:787‐795. [DOI] [PubMed] [Google Scholar]
- 19. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26:61‐69. [DOI] [PubMed] [Google Scholar]
- 20. Turner M, Jannah N, Kahan S, Gallagher C, Dietz W. Current knowledge of obesity treatment guidelines by health care professionals. Obesity (Silver Spring). 2018;26:665‐671. [DOI] [PubMed] [Google Scholar]
- 21. Leiter LA, Astrup A, Andrews RC, et al. Identification of educational needs in the management of overweight and obesity: results of an international survey of attitudes and practice. Clin Obes. 2015;5:245‐255. [DOI] [PubMed] [Google Scholar]
- 22. International Association for the Study of Obesity (IASO) . The Asia‐Pacific perspective: redefining obesity and its treatment; 2000. http://www.wpro.who.int/nutrition/documents/docs/Redefiningobesity.pdf. Accessed January 15, 2019.
- 23. International Society for Pharmacoepidemiology . Guidelines for Good Pharmacoepidemiology Practices (GPP); 2015. https://www.pharmacoepi.org/resources/policies/guidelines-08027/. Accessed January 15, 2019.
- 24. National Institutes of Health . ClinicalTrials.gov record NCT03235102; 2017. https://clinicaltrials.gov/ct2/show/NCT03235102. Accessed January 15, 2019.
- 25. Allison DB, Downey M, Atkinson RL, et al. Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obesity (Silver Spring). 2008;16:1161‐1177. [DOI] [PubMed] [Google Scholar]
- 26. Kyle TK, Dhurandhar EJ, Allison DB. Regarding obesity as a disease: evolving policies and their implications. Endocrinol Metab Clin North Am. 2016;45:511‐520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Royal College of Physicians . RCP calls for obesity to be recognised as a disease; 2019. https://www.rcplondon.ac.uk/news/rcp-calls-obesity-be-recognised-disease. Accessed February 17, 2019.
- 28. Tan D, Zwar NA, Dennis SM, Vagholkar S. Weight management in general practice: what do patients want? Med J Aust. 2006;185:73‐75. [DOI] [PubMed] [Google Scholar]
- 29. Speer SA, McPhillips R. Initiating discussions about weight in a non‐weight‐specific setting: what can we learn about the interactional consequences of different communication practices from an examination of clinical consultations? Br J Health Psychol. 2018;23:888‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. van der Klaauw AA, Farooqi IS. The hunger genes: pathways to obesity. Cell. 2015;161:119‐132. [DOI] [PubMed] [Google Scholar]
- 31. Albury C, Stokoe E, Ziebland S, Webb H, Aveyard P. GP‐delivered brief weight loss interventions: a cohort study of patient responses and subsequent actions, using conversation analysis in UK primary care. Br J Gen Pract. 2018;68:e646‐e653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Aveyard P, Lewis A, Tearne S, et al. Screening and brief intervention for obesity in primary care: a parallel, two‐arm, randomised trial. Lancet. 2016;388:2492‐2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Flint S. Obesity stigma: prevalence and impact in healthcare. Br J Obes. 2015;1:14‐18. [Google Scholar]
- 34. Donnelly JE, Blair SN, Jakicic JM, et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41:459‐471. [DOI] [PubMed] [Google Scholar]
- 35. Fruhbeck G, Busetto L, Dicker D, et al. The ABCD of obesity: an EASO position statement on a diagnostic term with clinical and scientific implications. Obes Facts. 2019;12:131‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1.


