Abstract
Background
Children with neurodevelopmental disorders are at increased risk of developing depression. Irritability predicts depression in the general population and is common in children with neurodevelopmental disorders. Thus, it is possible that irritability in children with neurodevelopmental disorders contributes to the link with later depression. This study aimed to (a) examine the association between childhood neurodevelopmental difficulties and adolescent depression and (b) test whether irritability explains this association.
Methods
Children with any neurodevelopmental difficulty at the age of 7–9 (n = 1,697) and a selected, comparison group without any neurodevelopmental difficulty (n = 3,177) were identified from a prospective, UK population‐based cohort, the Avon Longitudinal Study of Parents and Children. Neurodevelopmental difficulties were defined as a score in the bottom 5% of the sample on at least one measure of cognitive ability, communication, autism spectrum symptoms, attention‐deficit/hyperactivity symptoms, reading or motor coordination. The Development and Well‐Being Assessment measured parent‐reported child irritability at the age of 7, parent‐reported adolescent depression at the age of 10 and 13, and self‐reported depression at the age of 15. Depression measures were combined, deriving an outcome of major depressive disorder (MDD) in adolescence. Logistic regression examined the association between childhood neurodevelopmental difficulties and adolescent MDD, controlling for gender. Path analysis estimated the proportion of this association explained by irritability. Analyses were repeated for individual neurodevelopmental problems.
Results
Childhood neurodevelopmental difficulties were associated with adolescent MDD (OR = 2.11, 95% CI = 1.24, 3.60, p = .006). Childhood irritability statistically accounted for 42% of this association. On examining each neurodevelopmental difficulty separately, autistic, communication and ADHD problems were each associated with depression, with irritability explaining 29%–51% of these links.
Conclusions
Childhood irritability appears to be a key contributor to the link between childhood neurodevelopmental difficulties and adolescent MDD. High rates of irritability in children with autistic and ADHD difficulties may explain elevated rates of depression in the neurodevelopmental group.
Keywords: ALSPAC, neurodevelopmental, irritability, depression, attention‐deficit/hyperactivity disorder, autism
Introduction
Neurodevelopmental disorders are common (Boyle et al., 2011), typically start in early life, and result in impaired functioning (Howlin, Goode, Hutton, & Rutter, 2004). According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5), this group includes intellectual disability (ID), communication disorders, autism spectrum disorder (ASD), attention‐deficit/hyperactivity disorder (ADHD), specific learning disorders and motor disorders. There is a scientific rationale for this grouping. First, clinical overlap between these disorders is high (Fombonne, 2003; Ghirardi et al., 2018; Jenson & Steinhausen, 2015; Kadesjo & Gillberg, 2001). These disorders also behave as highly correlated traits. Thus, research that focuses on a single diagnosis (e.g. autism) does not allow for testing the contribution of accompanying neurodevelopmental difficulties. Neurodevelopmental disorders also share common features: they onset early in development, tend to show a steady course and affect males more commonly than females (Bishop & Rutter, 2008; Thapar, Cooper, & Rutter, 2017). There is also strong genetic overlap across different neurodevelopmental problems (Faraone, Ghirardi, Kuja‐Halkola, Lichtenstein, & Larsson, 2017; Ghirardi et al., 2018; Wilcutt, Pennington, & DeFries, 2000). Thus, considering neurodevelopmental disorders together may be useful clinically and for research purposes (Thapar et al., 2017).
Children with neurodevelopmental disorders are at increased risk of later depression (Gadow, Guttmann‐Steinmetz, Rieffe, & DeVincent, 2012; Kim, Szatmari, Bryson, Streiner, & Wilson, 2000; Mammarella et al., 2016; Meinzer et al., 2016). This pattern extends to those with sub‐threshold neurodevelopmental problems (Kanne, Christ, & Reiersen, 2009; Roy, Oldehinkel, Verhulst, Ormel, & Hartman, 2014). Depression in young people with neurodevelopmental disorders is clinically important. For example, in those with ADHD, it is associated with greater impairment in social and academic functioning (Blackman, Ostrander, & Herman, 2005), as well as increased rates for psychiatric hospital admission, suicidality (Biederman et al., 2008) and completed suicide (James, Lai, & Dahl, 2004). Identifying mechanisms that contribute to risk of depression in individuals with neurodevelopmental disorders could inform prevention and treatment strategies; furthermore, recognizing children with neurodevelopmental disorders at highest risk of developing depression could allow early identification and intervention.
One potential mechanism that has attracted growing interest is childhood irritability; this is described as a propensity to react with anger, grouchiness or tantrums disproportionate to the situation (Stringaris & Goodman, 2009a). Irritability is a well‐established feature of oppositional defiant disorder (ODD). Recent studies highlight an irritable dimension of ODD (Stringaris, Cohen, Pine, & Leibenluft, 2009; Rowe, Costello, Angold, Copeland, & Maughan, 2010; Krieger, Polanczyk, et al., 2013; Whelan, Stringaris, Maughan, & Barker, 2013 and Burke et al., 2014). The symptoms that best define this dimension include “often loses temper,” “often touchy or easily annoyed” and “often angry and resentful” (Evans et al., 2017). Irritability, when operationalized in the context of the irritable dimension of ODD or as a separate trait, has been found to predict future emotional disorders and depression (Krieger, Polanczyk, et al., 2013; Rowe et al., 2010; Stringaris & Goodman, 2009a; Vidal‐Ribas, Brotman, Valdivieso, Leibenluft, & Stringaris, 2016; Whelan et al., 2013). Severe irritability is particularly common in children with neurodevelopmental disorders (Shaw, Stringaris, Nigg, & Leibenluft, 2014; Simonoff et al., 2012) and may contribute to later depression in this group. However, research into the role of irritability in the association between neurodevelopmental difficulties and depression is limited.
Cross‐sectional studies find evidence that irritability is associated with depressive symptoms in children with ADHD (Ambrosini, Bennett, & Elia, 2013; Eyre et al., 2017; Seymour et al., 2012). Further, in a clinical ASD sample, the irritable dimension of ODD was associated with emotional problems (Mandy, Roughan, & Skuse, 2014). However, these studies examined the association between irritability and depression prior to the typical age of onset of depressive disorder in adolescence. Their cross‐sectional design precludes any temporal relationship between irritability and depression being established.
Longitudinal population‐based studies have found the association between irritability and depression persists after controlling for ADHD (Burke, Hipwell, & Loeber, 2010; Stringaris et al., 2009), and emotion regulation (a broader construct than irritability) has been shown to mediate the longitudinal association between ADHD and depression (Seymour, Chronis‐Tuscano, Iwamoto, Kurdziel, & MacPherson, 2014). However, longitudinal studies that have specifically examined the role of irritability in the longitudinal association between neurodevelopmental difficulties and depression are lacking.
This study utilized a case‐comparison design with groups selected from a large UK population‐based cohort. Aims were to (a) test for association between childhood neurodevelopmental difficulties and adolescent MDD, and (b) test the hypothesis that childhood irritability contributes to the association between concurrent neurodevelopmental difficulties and later MDD. Finally, as the grouping of neurodevelopmental difficulties includes problems from multiple DSM‐5 diagnostic categories, we assessed whether any particular category was driving the results.
Methods
Sample
The Avon Longitudinal Study of Parents and Children (ALSPAC) is a longitudinal population‐based cohort that recruited 14,541 pregnant women resident in Avon, UK, with expected delivery dates between 1 April 1991 and 31 December 1992 (Boyd et al., 2013; Fraser et al., 2013). Of these initial pregnancies, 13,988 children were alive at 1 year.
A total of 1,697 with neurodevelopmental difficulties at the age of 7–9 years and a comparison group of 3,177 with no evidence of any neurodevelopmental difficulties were included in this study (see below). Participants were assessed at multiple time points since recruitment using questionnaire and clinic‐based measures. The study website contains details of all the data that are available through a fully searchable data dictionary (http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary/).
Ethical considerations
Ethical approval for the ALSPAC study was obtained from the ALSPAC Ethics and Law Committee and Local Research Ethics Committees. All participants provided written informed consent.
Measures
Childhood neurodevelopmental difficulties
To identify those in the ALSPAC sample with a broad group of neurodevelopmental difficulties, we selected measures that covered each of the six DSM‐5 neurodevelopmental disorder categories (intellectual disability, communication disorders, ASD, ADHD, specific learning disorders and motor disorders). Seven scales from six validated measures, covering symptoms in each of these diagnostic categories, were identified. These measures were all collected between age 7 and 9 years and included both questionnaire and clinic‐based measures. They included the Wechsler Intelligence Scale for Children (WISC‐III) (Wechsler, 1991), the Children's Communication Checklist (CCC) (Bishop, 1998), the Social Communication Disorders Checklist (SCDC) (Skuse, Mandy, & Scourfield, 2005), the Development and Well‐Being Assessment (DAWBA) (Goodman, Ford, Richards, Gatward, & Meltzer, 2000), the Wechsler Objective Reading Dimension (WORD) (Rust, Golombok, Trickey, & Wechsler, 2003) and the Movement Assessment Battery for Children (MABC) (Henderson & Sugden, 1992) (Table 1). If subjects scored in the bottom 5% on at least one measure, they were classified as having “any neurodevelopmental difficulties,” even if data from other measures were missing. A comparison group with no evidence of neurodevelopmental difficulties on any of the seven scales was also identified. Therefore, those in the comparison group were required to have data available on all neurodevelopmental measures. See Figure S1 for a flow chart detailing numbers in the neurodevelopmental difficulties and comparison groups.
Table 1.
Measures used to identify neurodevelopmental difficulties
| Measure | Description of measure used to identify ND difficulties | ND difficulty assessed | Age at completion (N with data) | N with ND difficulties based on this measure |
|---|---|---|---|---|
| WISC‐III (Wechsler, 1991) |
Test measuring cognitive ability in children Provides full‐scale IQ (range: 45–151) |
Intellectual disability | 8 years, 6 months (7,037) | 321 |
| CCC (Bishop, 1998) | 70‐item parent questionnaire assessing children's communication. | Communication disorders | 9 years, 7 months | |
| (a) Speech and syntax subscales total identifying structural language difficulties (range: 45–70) | (7,544) | (a) 408 | ||
| (b) Pragmatic composite score identifying pragmatic language difficulties (range: 96–162) | (7,085) | (b) 355 | ||
| SCDC (Skuse et al., 2005) | 12‐item parent questionnaire assessing child social cognition (range: 0–24). | Autistic spectrum disorder | 7 years, 7 months (7,886) | 373 |
| DAWBA (Goodman et al., 2000) | Structured diagnostic parent interview based on DSM‐IV diagnoses. ADHD section used to generate child ADHD symptom count (range: 0–18). | ADHD | 7 years, 7 months (8,158) | 372 |
| WORD (Rust et al., 2003) | Series of tests assessing literacy skills in children. Basic reading subtest used to identify reading impairment (range: 0–50). | Specific learning disorder: impairment in reading | 7 years, 6 months (7,606) | 401 |
| MABC (Henderson & Sugden, 1992). | Series of tests assessing motor ability. Subtests used: heel to toe walking (balance), placing pegs (manual dexterity) and throwing bean bag into a box (ball skills). Standardized scores available for each subtest (Lingham, Hunt, Golding, Jongmans, & Emond, 2009), allowing a total score to be calculated (range: 0–15). | Motor disorder: developmental coordination disorder | 7 years, 6 months (6,682) | 305 |
ADHD, attention‐deficit/hyperactivity disorder; CCC, Children's Communication Checklist; DAWBA, Development and Well‐Being Assessment; MABC, Movement Assessment Battery for Children; ND, neurodevelopmental; SCDC, Social Communication Disorders Checklist; WISC‐III, Wechsler Intelligence Scale for Children; WORD, Wechsler Objective Reading Dimension.
All questionnaire/interview measures completed by parents and all tests completed by children.
As well as deriving one overarching categorical variable identifying those with or without “any neurodevelopmental difficulties,” we generated additional, binary (yes/no), categorical variables for each of the six DSM‐5 neurodevelopmental diagnostic categories (e.g. “ID,” “ADHD” or “ASD” difficulties). These binary categorical variables for each neurodevelopmental difficulty were generated by selecting the bottom 5% for each measure of the ALSPAC sample as a cut point. The specific measures used and the neurodevelopmental difficulty they represent are described in Table 1.
Childhood irritability
Irritability was assessed using three symptoms from the ODD section of the age 7 parent Development and Well‐Being Assessment (DAWBA) (Goodman et al., 2000): having temper outbursts, being touchy or easily annoyed and being angry and resentful. These symptoms make up an irritable dimension of ODD (Stringaris & Goodman, 2009b), as previously validated in this sample (Burke et al., 2014). Symptoms occurring over the last 6 months were rated “no more than others” (score 0), “a little more than others” (score 1) and “a lot more than others” (score 2). Our primary measure, total irritable score, ranged from 0 to 6. For descriptive purposes and sensitivity analysis, we also derived a binary measure of any versus no irritability, with the presence of any irritability defined as an irritable score of ≥1. The binary cut‐off was set at ≥1. This represents above average levels of irritability in this sample, and separates those with no irritability from those with any irritability, which is easy to assess in practice.
MDD in late childhood/adolescence
The depression section of the DAWBA was completed by parents at the age of 10 and 13 years, and by adolescents at the age of 15 years. DAWBA algorithms were used to generate diagnoses of DSM‐IV MDD in the previous 4 weeks (Goodman, Heiervang, Collishaw, & Goodman, 2011). As depression is episodic and we were interested in whether irritability was associated with any episode of depression across late childhood/adolescence, we chose to define depression as the presence of diagnosis at any of the time points measured. Therefore, information was combined to provide the outcome measure: any diagnosis of MDD between ages 10 and 15.
Other study measures
The parent‐reported DAWBA at the age of 7 provided information about depression and anxiety diagnoses. Demographic measures included social class based on mother's occupation, maternal and paternal age at birth of child, and maternal and paternal education (A‐levels or higher vs. those without, that is comparing those with or without education up to at least age 18 years).
Statistical analyses
Analyses used Stata version 14. Group comparisons used chi‐square analysis for categorical variables and t tests for continuously distributed measures.
Figure 1 shows our proposed path model. Neurodevelopmental difficulties precede the onset of depression and are associated with later depression (Daviss, 2008) (path a, Figure 1). Irritability precedes the onset of depression and is associated with later depression (Stringaris et al., 2009) (path c, Figure 1). Neurodevelopmental difficulties and irritability often co‐occur (Shaw et al., 2014; Simonoff et al., 2012), and the direction of this association is unknown (i.e., path b or path d, Figure 1). However, as neurodevelopmental difficulties start very early in life, and we were interested in the contribution of irritability to the association between neurodevelopmental difficulties and depression, we tested neurodevelopmental difficulties ⟶ depression (path a) and neurodevelopmental difficulties ⟶ irritability ⟶ depression (paths b and c).
Figure 1.
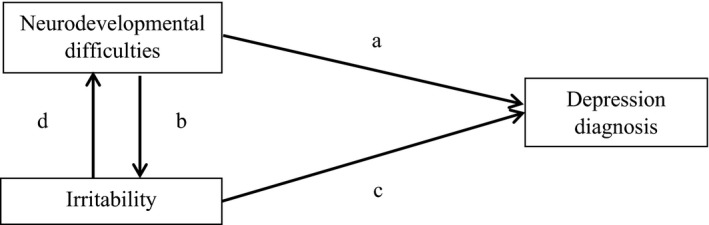
- 1. Neurodevelopmental difficulties ⟶ depression (path a)
- 2. Irritability ⟶ depression (path c)
- 3. Neurodevelopmental difficulties ⟶ irritability ⟶ depression (paths b and c)
- 4. Irritability ⟶ neurodevelopmental difficulties ⟶ depression (paths d and a)
Prior to all analyses, those with MDD at the age of 7 years were excluded to ensure we did not include those where the outcome (depression) temporally preceded assessment of the predictor variables.
Logistic regression analysis was used to examine the association between neurodevelopmental difficulties (age 7–9) and MDD (age 10–15) controlling for gender. Gender was included as a covariate as gender is associated with both neurodevelopmental difficulties and depression (Thapar, Collishaw, Pine, & Thapar, 2012; Thapar et al., 2017).
Logistic regression analysis then examined the association between irritability (age 7) and MDD (age 10–15), again controlling for gender.
The association between neurodevelopmental difficulties and irritability at the age of 7–9 was examined by calculating a polychoric correlation coefficient.
To assess the contribution of irritability to the association between childhood neurodevelopmental difficulties and adolescent depression, we used the “khb” command in Stata (Kohler, Karlson, & Holm, 2011) to decompose the path from neurodevelopmental difficulties to depression into direct (path a) and indirect (via irritability—paths b and c) effects, while controlling for gender. This is a general decomposition method that can be used to examine the degree to which a particular variable explains the relationship between an exposure and an outcome, providing information on total, direct and indirect effects. It allows the comparison of coefficients between 2 nested non‐linear probability models (Kohler et al., 2011), which was necessary due to the categorical nature of our variables.
Regression analyses were conducted on both complete case and imputed data sets (see below). As it was not possible for the khb command to be used on multiple imputed data sets in Stata, path analysis was conducted on complete cases only.
Finally, as our neurodevelopmental difficulties group was made up of multiple DSM‐5 diagnostic categories, we examined whether any particular category was driving the results. Analyses were repeated for each neurodevelopmental problem category (ID, communication disorders, ASD, ADHD, specific learning disorders, motor disorders).
Supplementary analyses
Three sensitivity analyses were undertaken. First, to assess the impact of missing data on the definition of our study groups, regression and path analyses were repeated on (a) a sample with complete neurodevelopmental data on all seven indicators (n = 3,824) and (b) a sample with neurodevelopmental data on at least one indicator (n = 9,977) (see Appendices S1 and S2).
Second, anxiety disorder at the age of 7 was added as a covariate, to establish that any association observed between neurodevelopmental difficulties and depression was explained by irritability rather than co‐occurring anxiety (see Appendix S3 and Table S1).
Third, analyses were repeated using a binary measure of irritability (individuals with no irritability (score = 0) vs. those with any irritability (score ≥ 1)) (see Appendix S4 and Table S2).
Sample selection
The case‐comparison samples for this study included participants who had any neurodevelopmental difficulty at the age of 7–9 years (n = 1,697), and a selected comparison group who had complete data on all the neurodevelopmental measures and thus we could be confident that they had no neurodevelopmental difficulties (n = 3,177) (see Figure S1), providing a total sample of 4,874. Of these individuals, 4,512 (92.6%) had irritability data at the age of 7, 2,668 (55%) had outcome data (MDD age 10–15) and 2,546 (52%) individuals had data on all variables included in the model. To minimize the bias from missing data as well as to improve precision, multiple imputation by chained equations was used to impute the missing outcomes (White, Royston, & Wood, 2011).
The imputation model included all variables in the analysis model, variables that predicted missingness in the outcome and variables associated with the outcome (full list of variables available on request). Where continuous variables were not normally distributed, predictive mean matching was applied. Fifty imputed data sets were created using 10 cycles of regression switching. Analyses were run on imputed data sets by combining estimates using Rubin's rules (White et al., 2011).
Results
Sample description
Children with neurodevelopmental difficulties at the age of 7–9 were more likely to be male, come from lower social class families, have higher rates of psychopathology, have a higher mean irritability score at the age of 7 and were more likely to be classified as having special education needs by their school than those in the comparison group (Table 2).
Table 2.
Childhood characteristics of those with neurodevelopmental (ND) difficulties compared to those without
| ND difficulties (n ≤ 1,697) | No ND difficulties (n ≤ 3,177) | Test statistic | |
|---|---|---|---|
| Gendera (% male (n)) | 63.1% (1,071) | 47.3% (1,503) | χ2 = 110.8, p < .001 |
| Social class based on mother's occupationb (% I/II (n)) | 29.2% (407) | 40.2% (1,153) | χ2 = 49.4, p < .001 |
| Oppositional defiant disorderc (% (n)) | 16.4% (228) | 0.6% (20) | χ2 = 468.8, p < .001 |
| Any anxiety disorderd (% (n)) | 4.8% (68) | 1.1% (36) | χ2 = 60.3, p < .001 |
| Major depressive disordere (% (n)) | 2.2% (30) | 0.4% (11) | χ2 = 35.7, p < .001 |
| Irritable scoref (mean) | 1.25 | 0.33 | t(4,510) = −24.5, p < .001 |
| Special educational needsg (% (n)) | 29.9% (403) | 3.2% (101) | χ2 = 672.5, p < .001 |
Numbers for analysis: a n = 4,874, b n = 4,261, c n = 4,566, d n = 4,582, e n = 4,506, f n = 4,512, g n = 4,488.
Social class based on occupation split into I/II or II/IV/V. DSM‐IV diagnoses of oppositional defiant disorder, any anxiety disorder and major depressive disorder derived using parent‐rated Development and Well‐Being Assessment (DAWBA) at the age of 7. Irritable score calculated using 3 items from parent‐rated DAWBA at the age of 7 (temper outbursts, touchy/easily annoyed, angry/resentful)—possible score = 0–6.
Childhood neurodevelopmental difficulties and adolescent depression
The neurodevelopmental group had higher rates of depression at the age of 10‐15 than the comparison group (4.5% vs. 2.0%; χ2 = 11.48, p = .001).
The association between child neurodevelopmental difficulties and later MDD remained significant after removing those with MDD at the age of 7 and controlling for gender, both using complete cases (OR = 2.11, 95% CI = 1.24, 3.60, p = .006) and imputed data sets (OR = 2.25, 95% CI = 1.54, 3.29, p < .001).
Contribution of childhood irritability to the association between neurodevelopmental difficulties and depression
There was a significant association between irritability score and the presence of neurodevelopmental difficulties (r = .50, p < .001).
Irritability at the age of 7 was associated with MDD at the age of 10–15 after controlling for gender and removing those with age 7 MDD, both using complete cases (OR = 1.48, 95% CI = 1.29, 1.72, p < .001) and imputed data sets (OR = 1.41, 95% CI = 1.28,1.56, p < .001).
The hypothesized path diagram included direct and indirect (via irritability) paths from neurodevelopmental difficulties to depression (Figure 2). Using complete cases for analysis, adding irritability reduced the coefficient (log odds) between neurodevelopmental difficulties and depression from .62 (95% CI = 0.06, 1.17, p = .029) to .36 (95% CI = 0.23, 0.95, p = .234), leaving an indirect effect of .26 (95% CI = 0.14, 0.38, p < .001). Overall, 42% of the total effect was explained by irritability.
Figure 2.
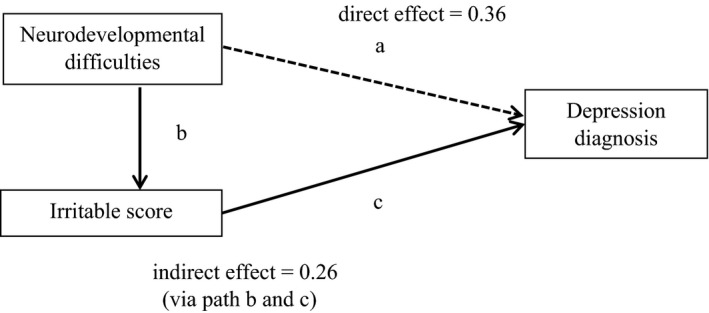
Indirect effect of irritability on the association between neurodevelopmental difficulties and depression. Interrupted line shows a path for which the magnitude of the path coefficient does not reach conventional levels of statistical significance
Testing individual neurodevelopmental disorders
Analyses of each of the neurodevelopmental categories and depression separately suggested that difficulties in pragmatic language (CCC) and social communication (SCDC) and ADHD (DAWBA symptoms) were associated with later depression (Table 3). Other neurodevelopmental indicators were not associated with later depression.
Table 3.
Examining association between each neurodevelopmental category and depression age 10–15
| Depression age of 10–15 | ||
|---|---|---|
| OR (95% CI) | p Value | |
| WISC‐III—full‐scale IQa | 0.85 (0.20, 3.5) | .824 |
| CCC—speech and syntax subscaleb | 0.98 (0.35, 2.72) | .967 |
| CCC—pragmatic composite subscalec | 5.12 (2.64, 9.92) | <.001 |
| SCDCd | 4.63 (2.34, 9.16) | <.001 |
| DAWBA ADHD symptomse | 4.27 (2.10, 8.69) | <.001 |
| WORD—basic reading subtestf | 1.83 (0.65, 5.16) | .256 |
| MABCg | 1.25 (0.45, 3.50) | .671 |
ADHD, attention‐deficit/hyperactivity disorder; CCC, Children's Communication Checklist; DAWBA, Development and Well‐Being Assessment; MABC, Movement Assessment Battery for Children; SCDC, Social Communication Disorders Checklist; WISC‐III, Wechsler Intelligence Scale for Children; WORD, Wechsler Objective Reading Dimension. The association between the bottom 5th percentile on each measure of neurodevelopmental difficulties and later depression was examined. Results are for complete cases. Analyses controlled for gender. Those with baseline depression diagnosis were removed from analysis.
a n = 2,604, b n = 2,634, c n = 2,581, d n = 2,600, e n = 2,616, f n = 2,599, g n = 2,538.
For the measures of ASD and ADHD, irritability explained a large proportion of the association. Irritability explained 29% of the association between pragmatic language difficulties and depression (indirect effect: log odds = 0.39, 95% CI = 0.20, 0.59, p < .001), 51% of the association between social communication difficulties and depression (indirect effect: log odds = 0.73, 95% CI = 0.31,1.14, p = .001) and 42% of the association between ADHD problems and depression (indirect effect: log odds = 0.55, 95% CI = 0.27, 0.83, p < .001).
Supplementary analyses
Alternative ways of defining the study groups using either complete or any available neurodevelopmental data, respectively, yielded very similar findings to the study full sample (see Appendices S1 and S2).
Controlling for anxiety disorder did not affect the results (see Appendix S3 and Table S1). Finally, the pattern of results using a dichotomous measure of (any vs. no) irritability was the same as that observed for the continuous measure (see Appendix S4 and Table S2).
Discussion
Using a longitudinal design, we observed that neurodevelopmental difficulties in childhood are associated with later adolescent depression and that a significant proportion of this association is explained by childhood irritability. In fact, when we take into account irritability, operationalized using the irritable dimension of ODD, the magnitude of association between neurodevelopmental difficulties and depression drops below the threshold for statistical significance. This suggests that irritability is a major contributor in explaining the link between neurodevelopmental problems and later depression.
Previous studies have found that individuals with neurodevelopmental disorders are at elevated risk of depression. Most of this research examined the associations between ADHD or ASD and depression (Daviss, 2008; Ghaziuddin, Ghaziuddin, & Greden, 2002; Kim et al., 2000; Meinzer et al., 2016). However, associations between other neurodevelopmental disorders and depression have also been found (e.g. reading and tic disorders) (Gadow et al., 2012; Mammarella et al., 2016). Our results are partially consistent with this literature, suggesting that while children with neurodevelopmental difficulties are at increased risk of later depression, findings may vary for specific problem types. This is clinically relevant, in terms of understanding which children with neurodevelopmental difficulties are at high risk of depression; regardless of the primary presenting problem; and elevated levels of ASD/social communication and ADHD symptoms appear to be associated with greatest risk.
Our second aim involved examining the contribution of irritability to the association between neurodevelopmental difficulties and depression. The results suggest that irritability, when measured as an irritable dimension of ODD, plays an important role. Previous studies have shown that irritability is an important predictor of future depression in the general population (Althoff, Kuny‐Slock, Verhulst, Hudziak, & van der Ende, 2014; Stringaris et al., 2009). Our results suggest it is also important for those with neurodevelopmental difficulties. Even when controlling for anxiety, the contribution of irritability was important, with 42% of the association between neurodevelopmental difficulties and depression explained by irritability.
These findings are clinically relevant. Identifying irritability in children with neurodevelopmental difficulties (particularly those with ADHD and ASD) may help to identify those at risk of later depression. This may help with early identification and treatment of depression in a group where depression is common and impairing (Daviss, 2008; Ghaziuddin et al., 2002). It may also provide an opportunity to prevent the onset of depression, for example by treating irritability early.
Understanding the mechanisms underlying irritability and its association with depression will inform the development of effective treatments. Literature suggests that genetic factors may be important. Family history of depression has been associated with irritability in a general population sample (Krieger, Leibenluft, et al., 2013) and a clinical ADHD sample (Eyre et al., 2017). Twin studies suggest irritability and depression have common genetic underpinnings (Savage et al., 2015; Stringaris, Zavos, Leibenluft, Maughan, & Eley, 2012). Environmental factors may also be of relevance in the association between irritability and depression. For example, studies of adolescent depression have found stressful life events, particularly stressors affecting relationships, to be important risk factors (Thapar et al., 2012). Irritability is associated with significant impairment in multiple areas of functioning including family relationships (Copeland, Angold, Costello, & Egger, 2013). Therefore, irritability (including the irritable dimension of ODD) could predispose to family relationship problems, which may predispose to depression. If this was the case, interventions such as parent training may be of benefit. Indeed, the effectiveness of parenting interventions has been well established in ODD (Scott & Gardner, 2015). However, more research is needed to test whether such interventions prevent depression onset in those with neurodevelopmental difficulties. Further research is also needed to examine whether mechanisms underlying irritability and their possible links with depression differ in young people with neurodevelopmental difficulties compared to those without.
Study limitations
Although the use of a large longitudinally assessed sample was a strength of the study, several limitations should be mentioned. As for any large longitudinal cohort study, there was a significant proportion of missing data in the outcome (MDD age 10–15). However, the pattern of results remained the same for complete case analyses and imputed data. Also, the way in which the neurodevelopmental difficulties categorical variable was derived meant that, in order to be categorized as having any neurodevelopmental difficulty, data on a minimum of one measure of neurodevelopmental difficulties were needed. However, to be categorized as having no neurodevelopmental difficulty, data on all neurodevelopmental measures were necessary. Despite this, the pattern of results remained the same when sensitivity analyses were undertaken firstly, including only those with complete data and secondly, allowing missing data in both neurodevelopmental and comparison groups.
There are also limitations in the measures used. The neurodevelopmental grouping variable aimed to cover a broad range of difficulties based on the DSM‐5 neurodevelopmental disorder categories. Symptoms in most but not all of the categories listed in DSM‐5 were included due to the available measures in the ALSPAC sample. Also, for the outcome, even though the measurement of depression across 3 time points was a strength of the study, the rater changed from parent report to self‐report at the age of 15. However, this reflects clinical practice, where there is greater reliance on parental reports in younger children and self‐reports in adolescents. It should also be noted that, although removing children with MDD at the age of 7 ensured that depression diagnosis did not precede the assessment of neurodevelopmental difficulties and irritability, children may still have experienced depression symptoms prior to this without meeting diagnostic criteria. Finally, our findings cannot automatically be generalized to clinical samples; further longitudinal research in clinical samples is needed.
Conclusion
This longitudinal study suggests that children with neurodevelopmental difficulties, specifically autistic and ADHD problems, are at increased risk of developing later adolescent depression. We found that irritability was an important contributor to this association. This suggests that the high rates of irritability known to be present in those with neurodevelopmental problems might explain the high rates of depression in this group. The next step is to identify the mechanisms involved in this association, which could facilitate the search for effective interventions.
Key points.
Childhood neurodevelopmental difficulties, particularly ASD/social communication and ADHD problems, are associated with later adolescent depression.
Irritability explains a significant proportion of the association between neurodevelopmental difficulties and adolescent depression.
As irritability precedes the onset of depression, there is opportunity for early identification, treatment and prevention of depression.
Future research is needed to understand mechanisms involved, to develop effective interventions and test existing ones.
Supporting information
Appendix S1. Analysis for those with complete neurodevelopmental data.
Appendix S2. Analysis for those with missing neurodevelopmental data.
Appendix S3. Controlling for anxiety.
Appendix S4. Analyses using binary measure of irritability.
Table S1. Path analysis examining the association between ND difficulties and depression, after controlling for anxiety disorder (in addition to gender and removing those with baseline depression diagnosis) at age 7.
Table S2. Path analysis examining the association between ND difficulties and depression, using a binary measure of irritability.
Figure S1. Flow chart showing how the sample for analysis was selected.
Acknowledgements
The UK Medical Research Council and Wellcome (Grant ref: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC. A comprehensive list of grants funding is available on the ALSPAC website. O.E. is a Clinical Research Fellow funded by the Wellcome Trust (Grant No: 104408/Z/14/Z). E.S. works in the Medical Research Council Integrative Epidemiology Unit at the University of Bristol which is supported by the Medical Research Council and the University of Bristol (Grant code: MC_UU_00011/1). The Cardiff authors are in a Centre funded by the UK Medical Research Council. This publication is the work of the authors, and they will serve as guarantors for the contents of this paper. The authors are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The authors have declared that they have no competing or potential conflicts of interest.
Conflict of interest statement: No conflicts declared.
References
- Althoff, R.R. , Kuny‐Slock, A.V. , Verhulst, F.C. , Hudziak, J.J. , & van der Ende, J. (2014). Classes of oppositional‐defiant behavior: Concurrent and predictive validity. Journal of Child Psychology and Psychiatry, 55, 1162–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrosini, P.J. , Bennett, D.S. , & Elia, J. (2013). Attention deficit hyperactivity disorder characteristics: II. Clinical correlates of irritable mood. Journal of Affective Disorders, 145, 70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman, J. , Ball, S.W. , Monuteaux, M.C. , Mick, E. , Spencer, T.J. , McCreary, M. , … & Faraone, S.V. (2008). New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 426–434. [DOI] [PubMed] [Google Scholar]
- Bishop, D.V.M. (1998). Development of the Children's Communication Checklist (CCC): A method for assessing qualitative aspects of communicative impairment in children. Journal of Child Psychology and Psychiatry, 39, 879–891. [PubMed] [Google Scholar]
- Bishop, D. , & Rutter, M. (2008). Neurodevelopmental disorders: Conceptual issues In Rutter M., et al. (Eds.), Rutter's child and adolescent psychiatry (pp. 32–41). Oxford, UK: Blackwell. [Google Scholar]
- Blackman, G.L. , Ostrander, R. , & Herman, K.C. (2005). Children with ADHD and depression: A multisource, multimethod assessment of clinical, social and academic functioning. Journal of Attention Disorders, 8, 195–207. [DOI] [PubMed] [Google Scholar]
- Boyd, A. , Golding, J. , Macleod, J. , Lawlor, D.A. , Fraser, A. , Henderson, J. , … & Davey Smith, G. (2013). Cohort Profile: The ‘Children of the 90s’; the index offspring of The Avon Longitudinal Study of Parents and Children (ALSPAC). International Journal of Epidemiology, 42, 111–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle, C.A. , Boulet, S. , Schieve, L.A. , Cohen, R.A. , Blumberg, S.J. , Yeargin‐Allsopp, M. , … & Kogan, M.D. (2011). Trends in the prevalence of developmental disabilities in US children, 1997‐2008. Pediatrics, 127, 1034–1042. [DOI] [PubMed] [Google Scholar]
- Burke, J.D. , Boylan, K. , Rowe, R. , Duku, E. , Stepp, S.D. , Hipwell, A.E. , & Waldman, I.D. (2014). Identifying the irritability dimension of ODD: Application of a modified bifactor model across five large community samples of children. Journal of Abnormal Psychology, 123, 841–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke, J.D. , Hipwell, A.E. , & Loeber, R. (2010). Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of the American Academy of Child and Adolescent Psychiatry, 49, 484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland, W.E. , Angold, A. , Costello, E.J. , & Egger, H. (2013). Prevalence, comorbidity, and correlates of DSM‐5 proposed disruptive mood dysregulation disorder. American Journal of Psychiatry, 170, 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviss, W.B. (2008). A review of co‐morbid depression in pediatric ADHD: Etiologies, phenomenology, and treatment. Journal of Child and Adolescent Psychopharmacology, 18, 565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans, S.C. , Burke, J.D. , Roberts, M.C. , Fite, P.J. , Lochman, J.E. , de la Pena, F.R. , & Reed, G.M. (2017). Irritability in child and adolescent psychopathology: An integrative review for ICD‐11. Clinical Psychology Review, 53, 29–45. [DOI] [PubMed] [Google Scholar]
- Eyre, O. , Langley, K. , Stringaris, A. , Leibenluft, E. , Collishaw, S. , & Thapar, A. (2017). Irritability in ADHD: Associations with depression liability. Journal of Affective Disorders, 215, 281–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone, S.V. , Ghirardi, L. , Kuja‐Halkola, R. , Lichtenstein, P. , & Larsson, H. (2017). The familial coaggregation of attention‐deficit/hyperactivity disorder and intellectual disability: A register‐based family study. Journal of the American Academy of Child and Adolescent Psychiatry, 56, 167–174. [DOI] [PubMed] [Google Scholar]
- Fombonne, E. (2003). Epidemiological Surveys of Autism and other pervasive developmental disorders: An update. Journal of Autism and Developmental Disorders, 33, 366–382. [DOI] [PubMed] [Google Scholar]
- Fraser, A. , Macdonald‐Wallis, C. , Tilling, K. , Boyd, A. , Golding, J. , Davey Smith, G. , … & Lawlor, D.A. (2013). Cohort profile: The Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. International Journal of Epidemiology, 42, 97–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow, K.D. , Guttmann‐Steinmetz, S. , Rieffe, C. , & DeVincent, C.J. (2012). Depression symptoms in boys with autism spectrum disorder and comparison samples. Journal of Autism and Developmental Disorders, 42, 1353–1356. [DOI] [PubMed] [Google Scholar]
- Ghaziuddin, M. , Ghaziuddin, N. , & Greden, J. (2002). Depression in persons with autism: Implications for research and clinical care. Journal of Autism and Developmental Disorders, 32, 299–306. [DOI] [PubMed] [Google Scholar]
- Ghirardi, L. , Brikell, I. , Kuja‐Halkola, R. , Freitag, C.M. , Franke, B. , Asherson, P. , … & Larsson, H. (2018). The familial co‐aggregation of ASD and ADHD: A register‐based cohort study. Molecular Psychiatry, 23, 257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman, R. , Ford, T. , Richards, H. , Gatward, R. , & Meltzer, H. (2000). The development and well‐being assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. Journal of Child Psychology and Psychiatry, 41, 645–655. [PubMed] [Google Scholar]
- Goodman, A. , Heiervang, E. , Collishaw, S. , & Goodman, R. (2011). The ‘DAWBA bands’ as an ordered‐categorical measure of child mental health: Description and validation in British and Norwegian samples. Social Psychiatry and Psychiatric Epidemiology, 46, 521–532. [DOI] [PubMed] [Google Scholar]
- Henderson, S.E. , & Sugden, D.A. (1992). Movement MABC. London: Psychological Corporation Harcourt Brace. [Google Scholar]
- Howlin, P. , Goode, S. , Hutton, J. , & Rutter, M. (2004). Adult outcome for children with autism. Journal of Child Psychology and Psychiatry, 45, 212–229. [DOI] [PubMed] [Google Scholar]
- James, A. , Lai, F. , & Dahl, C. (2004). Attention deficit hyperactivity disorder and suicide: A review of possible associations. Acta Psychiatrica Scandinavica, 110, 408–415. [DOI] [PubMed] [Google Scholar]
- Jenson, C.M. , & Steinhausen, H.C. (2015). Comorbid mental disorders in children and adolescents with attention‐deficit/hyperactivity disorder in a large nationwide study. ADHD Attention Deficit and Hyperactivity Disorders, 7, 27–38. [DOI] [PubMed] [Google Scholar]
- Kadesjo, B. , & Gillberg, C. (2001). The Comorbidity of ADHD in the General Population of Swedish School‐age Children. Journal of Child Psychology and Psychiatry, 42, 487–492. [PubMed] [Google Scholar]
- Kanne, S.M. , Christ, S.E. , & Reiersen, A.M. (2009). Psychiatric symptoms and psychosocial difficulties in young adults with autistic traits. Journal of Autism and Developmental Disorders, 39, 827–833. [DOI] [PubMed] [Google Scholar]
- Kim, J.A. , Szatmari, P. , Bryson, S.E. , Streiner, D.L. , & Wilson, F.J. (2000). The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism, 4, 117–132. [Google Scholar]
- Kohler, U. , Karlson, K.B. , & Holm, A. (2011). Comparing coefficients of nested nonlinear probability models. The Stata Journal, 11, 420–438. [Google Scholar]
- Krieger, F.V. , Leibenluft, E. , Stringaris, A. , Leibenluft, E. , Stringaris, A. , & Polanczyk, G.V. (2013). Irritability in children and adolescents: Past concepts, current debates, and future opportunities. Revista Brasileira de Psiquiatria, 35, S32–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger, F.V. , Polanczyk, G.V.P. , Goodman, R. , Rohde, L.A. , Graeff‐Martins, A.S. , Salum, G. , … & Stringaris, A. (2013). Dimensions of oppositionality in a Brazilian Community Sample: Testing the DSM‐5 proposal and etiological links. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 389–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingham, R. , Hunt, L. , Golding, J. , Jongmans, M. , & Emond, A. (2009). Prevalence of developmental coordination disorder using the DSM‐IV at 7 years of age: A UK population‐based study. Paediatrics, 123, e693–e700. [DOI] [PubMed] [Google Scholar]
- Mammarella, I.C. , Ghisi, M. , Bomba, M. , Bottesi, G. , Caviola, S. , Broggi, F. , & Nacinovich, R. (2016). Anxiety and depression in children with nonverbal learning disabilities, reading disabilities, or typical development. Journal of Learning Disabilities, 49, 130–139. [DOI] [PubMed] [Google Scholar]
- Mandy, W. , Roughan, L. , & Skuse, D. (2014). Three dimensions of oppositionality in autism spectrum disorder. Journal of Abnormal Child Psychology, 31, 566–573. [DOI] [PubMed] [Google Scholar]
- Meinzer, M.C. , Pettit, J.W. , Waxmonsky, J.G. , Gnagy, E. , Molina, B.S.G. , & Pelham, W.E. (2016). Does Childhood Attention‐Deficit/Hyperactivity Disorder (ADHD) predict levels of depressive symptoms during emerging adulthood? Journal of Abnormal Child Psychology, 44, 787–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe, R. , Costello, E.J. , Angold, A. , Copeland, W.E. , & Maughan, B. (2010). Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology, 119, 726–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, A. , Oldehinkel, A.J. , Verhulst, F.C. , Ormel, J. , & Hartman, C.A. (2014). Anxiety and disruptive behavior mediate pathways from attention‐deficit/hyperactivity disorder to depression. The Journal of Clinical Psychiatry, 75, 108–113. [DOI] [PubMed] [Google Scholar]
- Rust, J. , Golombok, S. , Trickey, G. , & Wechsler, D. (2003). WORD: Wechsler objective reading dimensions. London: Psychological Corporation. [Google Scholar]
- Savage, J. , Verhulst, B. , Copeland, W. , Althoff, R.R. , Lichtenstein, P. , & Roberson‐Nay, R. (2015). A genetically informed study of the longitudinal relation between irritability and anxious/depressed symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 54, 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott, S. , & Gardner, F. (2015). Parenting programs In Thapar A., Pine D.S., Leckman J.F., Scott S., Snowling M.J. & Taylor E.A. (Eds.), Rutter's child and adolescent psychiatry, 6th ed. (pp. 483–495). Hoboken, NJ: Wiley. [Google Scholar]
- Seymour, K.E. , Chronis‐Tuscano, A. , Halldorsdottir, T. , Stupica, B. , Owens, K. , & Sacks, T. (2012). Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. Journal of Abnormal Child Psychology, 40, 595–606. [DOI] [PubMed] [Google Scholar]
- Seymour, K.E. , Chronis‐Tuscano, A. , Iwamoto, D.K. , Kurdziel, G. , & MacPherson, L. (2014). Emotion Regulation Mediates the Association Between ADHD and depressive symptoms in a community sample of youth. Journal of Abnormal Child Psychology, 42, 611–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, P. , Stringaris, A. , Nigg, J. , & Leibenluft, E. (2014). Emotion dysregulation in attention deficit hyperactivity disorder. American Journal of Psychiatry, 171, 276–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonoff, E. , Jones, C.R.G. , Pickles, A. , Happe, F. , Baird, G. , & Charman, T. (2012). Severe mood problems in adolescents with autism spectrum disorder. Journal of Child Psychology and Psychiatry, 53, 1157–1166. [DOI] [PubMed] [Google Scholar]
- Skuse, D.H. , Mandy, W.P. , & Scourfield, J. (2005). Measuring autistic traits: Heritability, reliability and validity of the Social and Communication Disorders Checklist. British Journal of Psychiatry, 187, 568–572. [DOI] [PubMed] [Google Scholar]
- Stringaris, A. , Cohen, P. , Pine, D.S. , & Leibenluft, E. (2009). Adult outcomes of Youth Irritability: A 20 year prospective community based study. American Journal of Psychiatry, 166, 1048–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris, A. , & Goodman, R. (2009a). Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American academy of Child and Adolescent Psychiatry, 48, 404–412. [DOI] [PubMed] [Google Scholar]
- Stringaris, A. , & Goodman, R. (2009b). Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry, 50, 216–223. [DOI] [PubMed] [Google Scholar]
- Stringaris, A. , Zavos, H. , Leibenluft, E. , Maughan, B. , & Eley, T. (2012). Adolescent irritability: Phenotypic associations and genetic links with depressed mood. American Journal of Psychiatry, 169, 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar, A. , Collishaw, S. , Pine, D.S. , & Thapar, A.K. (2012). Depression in adolescence. Lancet, 379, 1056–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar, A. , Cooper, M. , & Rutter, M. (2017). Neurodevelopmental disorders. Lancet Psychiatry, 4, 339–346. [DOI] [PubMed] [Google Scholar]
- Vidal‐Ribas, P. , Brotman, M. , Valdivieso, I. , Leibenluft, E. , & Stringaris, A. (2016). The status of irritability in psychiatry: A conceptual and quantitative review. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 556–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler, D. (1991). The Wechsler intelligence scale for children‐third edition (WISC‐III). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Whelan, Y.M. , Stringaris, A. , Maughan, B. , & Barker, E.D. (2013). developmental continuity of oppositional defiant disorder subdimensions at ages 8, 10, and 13 years and their distinct psychiatric outcomes at age 16 years. Journal of the American academy of Child and Adolescent Psychiatry, 52, 961–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, I.R. , Royston, P. , & Wood, A.M. (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30, 377–399. [DOI] [PubMed] [Google Scholar]
- Wilcutt, E.G. , Pennington, B.F. , & DeFries, J.C. (2000). Twin study of the etiology of comorbidity between reading disability and attention‐deficit/hyperactivity disorder. American Journal of Medical Genetics, 96, 293–301. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Analysis for those with complete neurodevelopmental data.
Appendix S2. Analysis for those with missing neurodevelopmental data.
Appendix S3. Controlling for anxiety.
Appendix S4. Analyses using binary measure of irritability.
Table S1. Path analysis examining the association between ND difficulties and depression, after controlling for anxiety disorder (in addition to gender and removing those with baseline depression diagnosis) at age 7.
Table S2. Path analysis examining the association between ND difficulties and depression, using a binary measure of irritability.
Figure S1. Flow chart showing how the sample for analysis was selected.


