Abstract
Background
Immediate provisionalization reduces chair time and improves patient comfort.
Purpose
To analyze immediate functional loading vs nonfunctional loading with restorations in the posterior mandible for marginal bone defects, implant success/survival, and patient satisfaction.
Materials and Methods
A randomized controlled clinical trial was designed to assess these parameters based on 20 adult patients who underwent implant surgery, followed by immediate delivery of screw‐retained or cemented single or splinted restorations in full occlusal contact or in infraocclusion (test and control group). A questionnaire with visual analog scales was used to assess patient satisfaction.
Results
Following 36‐month data were evaluable for 9 patients (21 implants) in the study group (immediate functional loading) and for 10 patients (31 implants) in the control group (immediate nonfunctional loading). One implant in the control group was lost, hence the overall implant survival and success rate was 98.2%. Marginal bone defects were consistent with previous studies and comparable in both groups. Periotest values did not significantly change from baseline and the 12‐month follow‐up (Friedmann test). Patient satisfaction was high and did not involve any significant intergroup differences (Mann‐Whitney U‐test).
Conclusions
Both types of immediate provisional restorations are viable in selected patients. Larger randomized controlled trials are needed to establish immediate functional loading as a standard treatment for partially edentulous jaws.
Keywords: bone loss, computer‐assisted, immediate function, immediate loading, marginal bone loss, patient satisfaction, randomized controlled trial
1. INTRODUCTION
Current strategies of implant dentistry are aimed at minimizing surgical interventions and postoperative discomfort while improving patient satisfaction regarding function and esthetics.1 Immediate loading was introduced against this background, has since been extensively discussed in the literature, and has been found to be a valid strategy of treatment offering implant survival rates of 95% to 98.8% in the posterior mandible2, 3, 4 if appropriate patient selection is ensured.5, 6, 7, 8, 9, 10, 11 In addition to these clinical parameters, patient satisfaction and well‐being is another major criterion of successful implant treatment. We have devoted attention specifically to this topic,12 but generally speaking, little data continues to be available on patient satisfaction regarding esthetics, masticatory function, access for oral hygiene, as well as restorative maintenance requirements.
Immediate loading in partially edentulous mandibles is today considered viable in the hands of experienced clinicians.13, 14 Forty implants, inserted and immediately loaded to replace lower molars, were found to yield a 5‐year survival rate of 95% and a mean crestal bone loss of 1.17 mm.15 Immediate occlusal loading of 139 implants yielded a cumulative survival of 99% after 1 year, with a mean of 1.01 mm in marginal bone resorption.11 Immediate loading of 143 implants led to a 94% cumulative survival after 1 year in function, involving a mean crestal bone loss of 0.33 mm after conventional vs 0.24 mm after flapless implant surgery, which did not seem to make a difference.9 Immediate loading yielded a 12‐month success rate of 97.5% based on 40 implants supporting splinted restorations in 20 patients with missing mandibular premolars and molars.16 In addition, a recent review has disclosed no significant differences in implant survival, marginal bone loss, and mechanical or biological complications between immediately and conventionally loaded single implants in the posterior mandible.17
Nonfunctional protocols of immediate loading have been introduced so as to protect newly inserted implants from exposure to any excessive functional or parafunctional forces in partially edentulous patients,18 as complications like bruxism and severe clenching have been suspected to increase the risk of failure among immediately loaded implants.19 Studies have reported lower implant survival rates after immediate functional loading than after both immediate nonfunctional restoration and delayed loading.20, 21 Other authors did not observe any differences between immediate functional and nonfunctional loading with regard to implant survival, bone loss, or soft‐tissue healing.4, 10, 11, 22
Hence the aim of the present randomized controlled clinical trial was to assess marginal bone defects (MBDs), implant success and survival as well as patient satisfaction associated with immediate functional vs immediate nonfunctional loading of posterior implants in partially edentulous patients. This report covers an observation period of 36 months.
2. MATERIALS AND METHODS
2.1. Design and pilot study
The design of this randomized controlled clinical trial was approved by the institutional review board (ethics commission) at Medical University of Graz (ref: 23‐202 ex 10/11 and 27‐237 ex 14/15). The study was conducted in accordance with both the ICH‐GCP Guidelines for Clinical Trials and the Declaration of Helsinki as revised in 2008. All patients included gave their informed consent after being comprehensively informed about the study, the clinical parameters included in the analysis were described in a previous report of the 12‐month data, which was published as a pilot study.23
2.2. Patient enrollment
Twenty patients, all treated at our center exclusively, were enrolled between 3/2011 and 4/2012. A total of 59 implants were initially planned. Each patient was screened by reviewing his or her medical history, obtaining a panoramic radiograph, as well as an alginate impression (Xantalgin select; Heraeus Kulzer, Hanau, Germany). Only adult patients showing partial edentulism in posterior segments with no need for extensive grafting (at least 5 mm in width and 10 mm in height) were included in the study. Minimum primary intraoperative stability for impressioning was determined with more than 20 Ncm. Heavy smokers (>10 cigarettes a day), patients with active local inflammation or metabolic disease were excluded. Also patients with a history of irradiation or chemotherapy in the head‐and‐neck area, use of bisphosphonates, pregnancy, or evidence of severe parafunction (bruxing/clenching) were excluded.
2.3. Group assignment
An independent examiner randomized each patient to the test or the control group prior to laboratory fabrication, using the tool “Randomizer for Clinical Trials” provided by our Institute for Medical Informatics, Statistics and Documentation (randomizer.at). Immediate restorations were to be used, adjusted either to full occlusal loading by shimstock (test group) or to infraocclusion in maximum intercuspidation (control group).
2.4. Planning and medication
An experienced clinician planned all restorations, using a prosthetic‐driven approach. For details on the 3D implant planning, the reader is referred to our pilot study.23 Three dimensional planning was based on computed tomography and cone beam computed tomography. Each restorative treatment plan was verified for whether it was consistent with the patient's anatomy and location of sensitive structures by using 3D implant planning software (Simplant Crystal; Materialize Dental, Leuven, Belgium). Patients were instructed to rinse with chlorhexidine digluconate 0.2% for 1 minute prior to surgery, the latter being performed under local anesthesia (Ultracain dental forte; Sanofis‐Aventis, Vienna, Austria). Antibiotic treatment was started 1 day before surgery and carried on for 5 days (Augmentin 1 g twice daily; Smithkline Beecham, Worthing, UK).
2.5. Implant placement
Stereolithographic tooth‐supported guides were made to transfer the 3D‐planned implant positions to the surgical situation (Figure 1A,B). A flapless punch technique was employed in 2 patients, whereas 18 patients were approached by flap surgery via a crestal incision. The same implant system was used in all patients (XiVE; Dentsply Sirona, New York) and insertion performed as per the manufacturer's drilling protocol (Figure 2). Primary stability was captured via insertion torque and Periotest values with healing abutments in place.
Figure 1.

A, Surgical guide, fabricated by stereolithography and supported by the natural residual dentition. B, Guided implant placement (XiVe, Dentsply Sirona, New York). The guide facilitates optimal positioning and angulation
Figure 2.

Freshly inserted implants after minimally invasive (flapless) surgery and with the temporary abutments already connected (TempBase, Dentsply Sirona, New York)
2.6. Immediate provisionalization
Single or splinted crowns were designed from resin (SR Ivocron; Ivoclar Vivadent, Schaan, Liechtenstein) for immediate delivery by screw retention on customized temporary abutments (TempBase; Dentsply Sirona, New York; ComboLign, Bredent, Senden, Germany). Screws were tightened using a ratchet as described in the user's manual until an insertion torque of 14 Ncm. They were delivered and adjusted to the randomized occlusal protocol not later than 72 hours after surgery. Any subsequent manipulations other than for occlusal adjustment, retightening loosened screws, or repair were avoided. Figure 3 illustrates an example.
Figure 3.

Immediate temporary restoration, consisting of three splinted and screw‐retained units of acrylic resin, 1 month after implant surgery
2.7. Follow‐up examinations
One week after surgery, we recorded gingival24 and plaque25 scores and checked for signs of inflammation, necrosis, dehiscence, or pyogenic infection. Follow‐up visits were scheduled for every 4 weeks to examine the soft tissue and periapical radiographs, verify the stability of the temporary restorations, and evaluate any dental problems. The same visits were used for occlusal adjustments, including those required by the randomization protocol. At the last follow‐up, we evaluated gingival and plaque scores, Periotest values evaluated with the healing abutments after removal of the superstructures, occlusal parameters, as well as radiographic parameters. The definitive splinted or single‐tooth restorations were cemented or screwed to the implants 6 to 8 months after surgery (Figure 4A‐C). Success criteria defined by Misch et al26 were evaluated 12 and 36 months after implant insertion.
Figure 4.
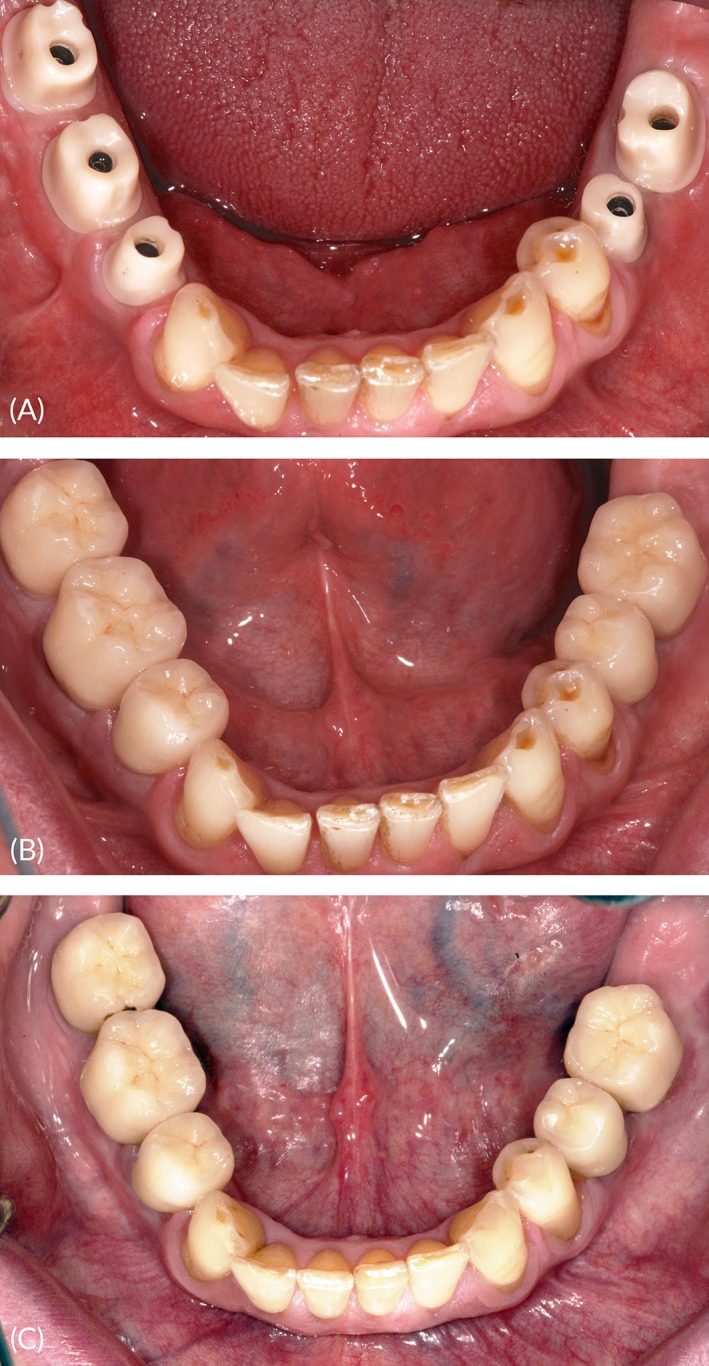
Definitive single‐tooth restorations, cemented to customized zirconia abutments, 8 and 36 months after implant surgery
2.8. Assessment of MBDs
An examiner (M. S.)––not involved in the surgical and restorative procedures––assessed the MBDs based on digital perpendicular long‐cone radiographs (Sidexis, Orthophos plus DS; Sirona) obtained immediately after implant surgery (baseline) and at 1, 2, 3, 6, 12, and 36 months. Dimensions were calibrated by the known parameters of implant diameter and length. Starting from the implant shoulder, distances were measured to the mesial and distal points of distal implant‐bone contact (magnification: ×2). Following this principle, the bone loss was calculated by resetting each distance between a crestal bone level and the implant shoulder to zero from one follow‐up visit to the next (Figure 5A‐D).
Figure 5.
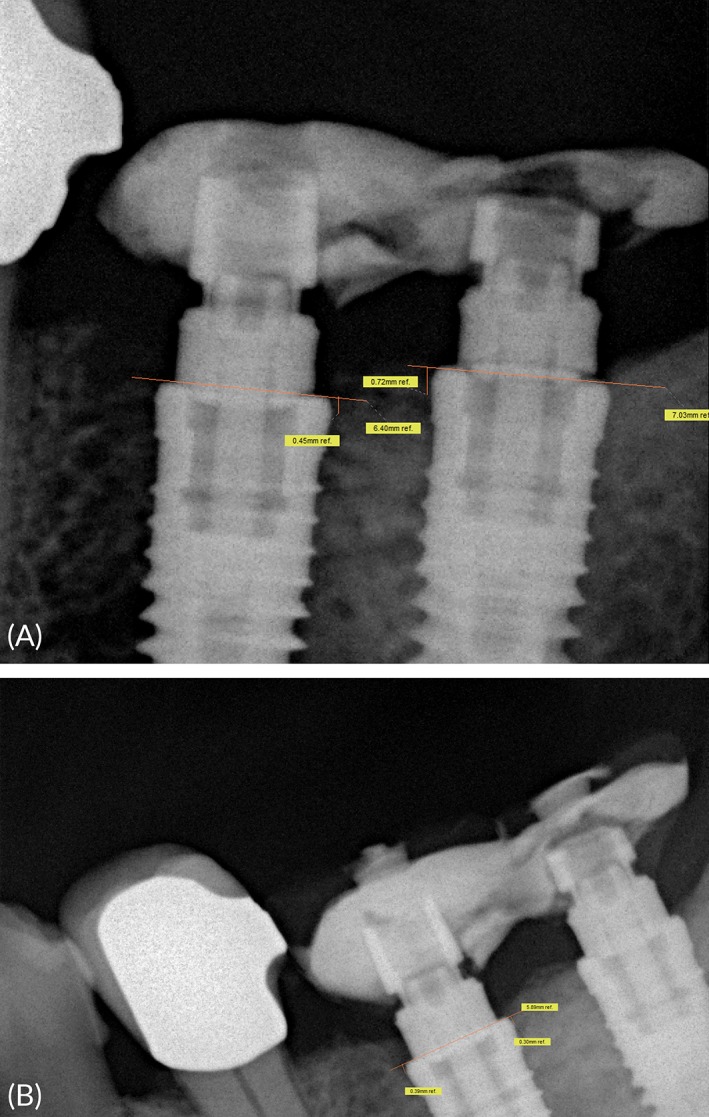
Marginal bone defects as measured in the present study, based on radiographs and using a horizontal reference line at baseline and 36 months post op
2.9. Patient satisfaction questionnaire
Given the importance of patient‐centered outcome measures, we took advantage of the 36‐month follow‐up to evaluate patient satisfaction. Using a questionnaire that included visual analog scales, we asked each patient to rate a number of parameters that concerned any restoration he or she had worn before implant treatment, the implant surgery, the provisional restorations, and the definitive prosthetic rehabilitation. Each topic was rated for esthetics, access for oral hygiene, phonetics, and chewing comfort by visual analog scales (1 = maximum satisfaction; 10 = maximum dissatisfaction).
2.10. Statistical analysis
Data were analyzed using SPSS Statistics (v. 18.0; SPSS Inc., Chicago, Illinois) and Microsoft Excel (v. 2003; Microsoft Corporation, Redmond, Washington). Descriptive statistics were contributed by a biostatistician. The bone‐level data were confirmed to be normally distributed by Kolmogorov‐Smirnov testing. A general linear model with repeated measurements was used to assess the changes in bone levels between visits in both the test and the control group. Using a Friedman test, the Periotest values were analyzed at baseline and 12 and 36 months after surgery. Intergroup comparisons of patient satisfaction were performed using a Mann‐Whitney U‐test.
3. RESULTS
3.1. Pertinent patient data
We enrolled 20 patients (13 women, 7 men) aged 54 ± 11.9 years (range: 33‐70 years). One patient withdrew for personal reasons after randomization but was replaced to bring the sample back to 20. The study was open to maxillary cases, but all consecutive implants and temporary restorations were inserted in the mandible. Upper‐jaw antagonists at baseline included natural teeth in 65% (n = 13), implant‐borne restorations in 10% (n = 2), mucosa‐supported dentures in 20% (n = 4), and periodontally supported dentures in 5% (n = 1) of cases. One patient being unavailable for the last follow‐up, the entire 36‐month observation period could be analyzed for 19 patients (occlusal study group: n = 8; nonocclusal control group: n = 11) comprising a total of 52 evaluable implants. Distribution of diameter and length of the inserted implants is presented in Figure 6.
Figure 6.
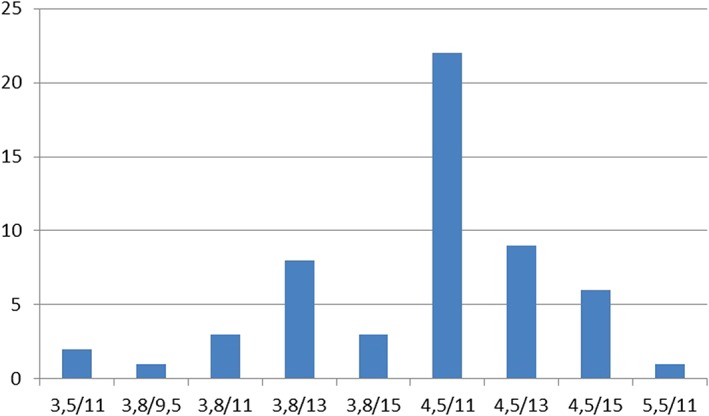
Distribution of implants inserted
3.2. Implant survival and success
One implant could not be inserted due to bone deficiency, so that 58 of the 59 initially planned implants were actually placed. Three were left unrestored due to inadequate primary stability. One implant was lost 24 months after surgery and was not reinserted for prosthetic reasons; however, this implant was recorded as failure.26 Hence the survival and success rates were 97.1% in the control and 100% in the study group, or 98.2% based on both groups. Two implants were associated with minor bone deficiencies and three with mucositis.
3.3. Bone density and implant stability
Bone quality as defined by Lekholm and Zarb27 was D2 in 87.3% and D1 in 12.7% of cases. Mucosal biotypes were normal at 31, thin at 4, and thick at 20 implant sites. Insertion torque was >35 Ncm in 85.5%, >45 Ncm in 5.5%, and <35 Ncm in only 9.1% (n = 5) of the implants. Periotest values averaged −4.48 ± 1.66 (range: −7 to +1) at baseline, −3.98 ± 1.75 (range: −7 to −1) after 12 months, and − 3.50 ± 2.13 (range: −7 to +1) after 36 months. Figure 7 illustrates Periotest values at baseline as well as at 12 and 36 months after surgery, yielding no significant difference between the two measurements (P = 0.054; Friedmann test).
Figure 7.
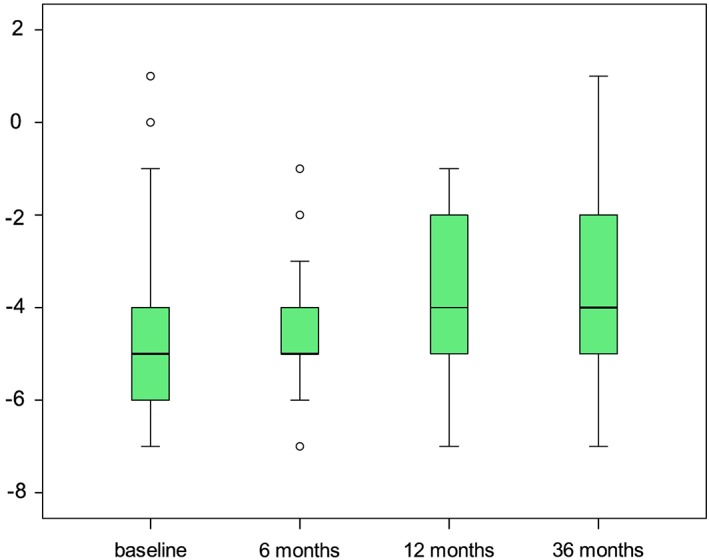
Boxplot analysis of Periotest values at baseline as well as 6, 12, and 36 months after implant surgery
3.4. Maintenance, complications, compliance
At the 36‐month follow‐up, 50%, 35.3%, or 13.7% of patients showed plaque scores of 1, 2, or 3, respectively. Gingival index scores were 0 in 51% (n = 26), 1 in 35.7% (n = 18), and 2 in 13.7% (n = 7) of implants. All clinical evaluations were performed with healing abutments. Complications among the temporary restorations were imprecise fit (n = 3), requirements for occlusal adjustments (n = 2), fracture (n = 2), and screw loosening (n = 3). All patients in the study group and 90.1% in the control group returned for the follow up‐visits as scheduled. Restorative complications of the permanent superstructures were restricted to 1 patient with a single tooth restoration (chipping).
3.5. Marginal bone defects
MBD data measured on radiographs were normally distributed (Kolmogorov‐Smirnov test). At baseline, these MBD measurements averaged 0.08 ± 0.16 mm (range: 0.00‐0.60 mm) in the test vs 0.16 ± 0.29 mm (range: 0.00‐1.42 mm) in the control group. At the 12‐month follow‐up, they averaged 0.38 ± 0.33 mm (range: 0.00‐1.22 mm) vs 0.46 ± 0.49 mm (range: 0.00‐2.28 mm) and, at the 36‐month follow‐up, 0.51 ± 0.43 mm (range: 0‐1.20 mm) in the test vs 0.51 ± 0.42 mm (range: 0‐1.19 mm) in the control group. Figure 8 illustrates how MBDs developed over time. Highly significant (P < 0.001) increases were noted in both the test and the control group but did not involve a significant intergroup difference (P = 0.319). A tendency for somewhat lower values in the test group was not significant (P = 0.803). Figure 9 illustrates these developments around single‐tooth vs splinted restorations, demonstrating that the type of superstructure did not make a difference to marginal bone levels over time (P = 0.180).
Figure 8.
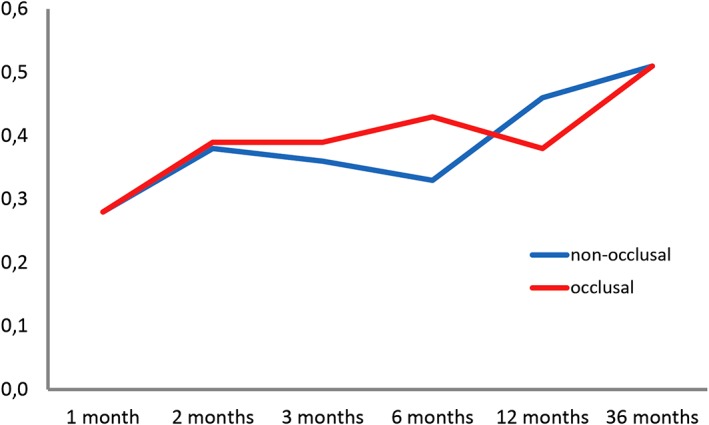
Marginal bone defects in relation to the time of implant surgery, evaluated as a general linear model with repeated measurements
Figure 9.
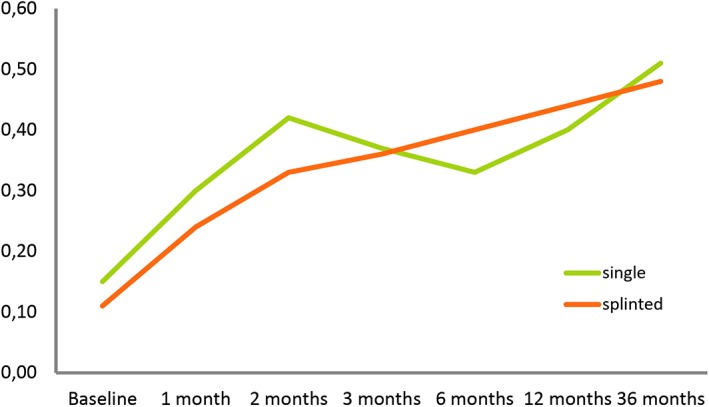
Marginal bone defects as a function of superstructure types (single vs splinted) in relation to the time of implant surgery, evaluated as a general linear model with repeated measurements
3.6. Patient satisfaction
Fifty‐two evaluable implants were inserted to replace natural dentitions in 13 patients and fixed prosthetic solutions in 6 patients. No cases of temporomandibular disorder were noted after implant and restorative treatment. All patients (both groups) affirmed their willingness to undergo implant surgery with immediate provisionalization once again if faced with a similar situation. Patients' ratings were performed on visual analog scales (1 = maximum satisfaction; 10 = maximum dissatisfaction) and averaged 1.8 ± 2.1 (range: 1‐9) for esthetics and 1.4 ± 2.2 (range: 1‐5) for function of the immediate provisionalization. Esthetics of the definitive restorations was rated as 1.4 ± 1.6 (range: 1‐4), access for oral hygiene as 1.5 ± 2.1 (range: 1‐5), phonetics as 1.4 ± 2.2 (range: 1‐5), and chewing ability as 1.2 ± 0.5 (range: 1‐2). A box plot of the descriptive analysis is illustrated in Figure 10. None of these parameters revealed any significant intergroup differences (esthetics: P = 0.442; hygiene: P = 0.395; phonetics: P = 0.395; and chewing: P = 0.177; Mann‐Whitney U‐test). All patients affirmed that the implant treatment had improved their quality of life.
Figure 10.
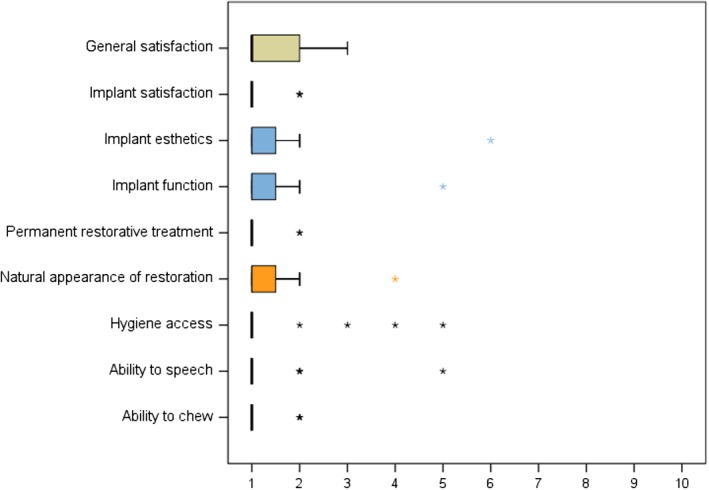
A box plot of the descriptive analysis of patient satisfaction
4. DISCUSSION
Recent studies have investigated potential effects of occlusion on immediate temporary restorations. It has been stated repeatedly that controlling occlusal forces is essential to successful immediate loading.19, 28, 29, 30 An extensive systematic review and meta‐analysis did not arrive at a conclusive statement about occlusal contacts during osseointegration of dental implants.31 Another review, indicating disagreement about occlusal guidelines in immediate loading, nevertheless recommended a concept of centric contacts only.30 No significant differences in survival rates, bone loss, or soft‐tissue parameters were identified in a randomized clinical study of 100 implants immediately loaded either in full occlusion or in mild infraocclusion.4
The sample size of our study is too small for a statistical comparison of restorations with different numbers of units. Yet our finding of no difference in survival/success rates is in contrast to a previous study of 307 implants supporting two‐ to four‐unit fixed partial dentures in 117 patients.21 Investigating any effects of different loading protocols on implant survival/success, implant stability quotient, insertion torque, and marginal bone levels over 2 years, implant survival was 100% with both immediate nonfunctional and delayed loading vs 93% with immediate functional loading. Seven implants, most of them in two‐unit restorations, accounted for this difference. As primary stability at insertion did not differ between the three groups, the authors of that study suggested loading‐related factors as accounting for the significantly higher failure rates in their group of immediate functional loading, and they also concluded that the number of units might influence implant stability during osseointegration.21
Five‐year results on immediate vs early functional loading in posterior mandibles yielded 100% implant survival and no significant differences in crestal bone loss (0.4 vs 0.8 mm), bleeding index (0.22 vs 0.25), or plaque index (0.17 vs 0.19) between both groups.32 A randomized clinical study of immediate functional vs nonfunctional loading yielded 100% survival in both groups and marginal bone losses of 1.59 mm vs 1.91 mm.33 A reported rate of implant survival even higher after immediate (100%) than delayed (93%) loading7 ran counter to 3‐year findings of poorer survival after immediate (85%) than delayed (100%) loading in the posterior mandible.20
Our 36‐month data evaluable for 19 patients with a total of 52 implants yielded an overall survival and success rate of 98.2% and MBDs at least as favorable as in previous studies.4, 10, 11, 15, 20, 21, 33, 34, 35, 36, 37 Both MBDs and the associated survival/success rates may be affected by various parameters after immediate loading in partially edentulous mandibles. Bone levels might depend on the load distribution between natural teeth and implants or on access for oral hygiene in splinted provisional restorations.2 Iatrogenic manipulation of the implant in the early phase of osseointegration might play a role.18 Even so, histological studies suggested clinically stable implants also in heavy smokers after immediate functional loading of implants.10, 38, 39 A recent split‐mouth study of immediate vs early occlusal loading in the posterior mandible, with up to 15 years of implant service, yielded intergroup differences in periodontal indices and crestal bone loss (mesial: 0.70 ± 1.09 mm vs 1.17 ± 1.27 mm; distal: 0.43 ± 1.02 mm vs 1.06 ± 1.33 mm) that were not statistically significant after 12.14 vs 12.40 years of loading.40
What might also apply to the present study is a suggestion by previous authors—who reported significant bone‐level reductions with both immediate and delayed loading over 3 years—that insertion depth may be increased in loaded implants.20 Our radiographic assessment showed that the baseline bone levels (0.08 vs 0.16 mm) were lower than we have reported previously (0.48 mm) for the same implant type,2 indicating an increased insertion depth for both groups in the present study. We also noted less radiographic resorption than previously2 in both groups from baseline to 6 and 12 months. Contributing factors remain speculative, but examples would include patient selection, guided surgery, modified platform surface, fit of restorations, or access for hygiene. This time we report a radiographic bone loss perhaps even lower than the 6‐ and 12‐month data presented by Degidi et al4 whose results of no significantly different survival/success rates or tissue reactions between both loading protocols are highly consistent with ours. We noted significant increases in marginal bone resorption within 12 months, no significant intergroup difference in the steepness of this curve, and similar defects (0.4 mm vs 0.38 mm) at the end of this period.
A recent multicenter study, designed as a randomized controlled trial, compared 10‐year results for immediate nonocclusal loading vs nonsubmerged early loading of implants, which included an analysis of peri‐implant bone and soft‐tissue levels.41 The investigators did not observe any significant intergroup differences in failed implants, failed superstructures, other complications, periimplant mucositis, peri‐implant bone loss, or soft‐tissue levels. Both groups were found to have gradually lost peri‐implant bone by a mean of 1.43 mm (immediate loading) or 1.42 mm (early loading) after 10 years, and the soft‐tissue levels had changed by 0.38 or 0.25 mm, respectively, during that time.
We observed restoration‐specific problems (resin fractures, loosening, inaccurate fit), periimplant mucositis, as well as imperfections of 3D planning and the surgical guide. All of these were readily manageable without compromising implant integration and radiographic appearance. Three implants were not evaluated as they were left to heal submerged due to rotational instability after insertion. To optimize force distribution, we splinted any adjacent implants as described in a similar way elsewhere.20, 42, 43 Esposito et al31 in their Cochrane Review, recommended immediate rather than early loading to optimize implant success, and the insertion torques which have been recommended for immediate loading range from 25 Ncm4 to 45 Ncm. In the present study, we recorded insertion torques <35 Ncm for 5 implants (study group: n = 3; control group: n = 2) without any notable effects on clinical outcomes 12 months after surgery. Splinting of the provisional restoration may well have prevented micromotion of these implants.
A systematic review has recently concluded that patients focus their expectations mainly on function, followed by esthetics.44 There was insufficient evidence to determine possible outcomes of immediate, immediate‐delayed, or delayed loading with regard to patient satisfaction, so that the pros and cons of different loading protocols may vary in this regard.44 Another review has concluded both that high patient satisfaction is the most important advantage of immediate over conventional loading and that this statement is especially true of the early healing phase.43 In accordance with our own findings, a recent study showed that patient satisfaction did not differ by gender, number of implants, survival, complications, and time in situ.45
Our finding that occlusal and nonocclusal immediate restorations did perform equally well in partially edentulous posterior mandibles is consistent with two studies4, 11 but not with others.20, 21 The 100% survival/success rate in our study group, with no major complications posing a risk to the implants, may have been due to our careful patient selection, presurgical 3D‐planning and precise intraoperative transfer, no delivery of restorations on implants with reduced primary stability, accurate laboratory and restorative procedures, as well as rigorous postoperative follow‐up. We also noted no differences between the single‐unit and the splinted multi‐unit restorations, and plaque and mucosal parameters were well within the range of similar reports.3, 46
Patients benefit from immediate loading in several ways. They are not only subjected to less chair time, no second‐stage surgery, and a shorter healing period, but they also save money. Another point in favor of patient acceptance is the postoperative comfort of not having to wear a removable denture.2, 47, 48 Given that even a “high‐load” scenario like the posterior mandible does not seem to affect the osseointegration of screw‐type implants, a case could even be made for immediate definitive restorations. That being said, temporary restorations made of resin still have their advantages in the initial phase of healing and osseointegration: they minimize the requirements for laboratory fabrication and soft‐tissue conditioning and, even more importantly, facilitate the use of definitive single‐tooth restorations in the mandible.
5. CONCLUSIONS
No clinically relevant differences in MBDs were observed between loaded and nonloaded immediate restorations in partially edentulous posterior mandibles up to 36 months. Within the limitations of our study, both treatment options can be considered a viable treatment concept in selected patients. Randomized controlled trials are needed to disclose any kind of superiority of either protocol in specific situations or jaw areas.
AUTHOR CONTRIBUTIONS
All authors made (a) substantial contributions to the conception and/or design of the work; or the acquisition, analysis, or interpretation of data for the work; and (b) drafted the article or revised it critically; and (c) approved the final version of this manuscript; and (d) agreed to be accountable for all aspects of the work.
Vogl S, Stopper M, Hof M, Theisen K, Wegscheider WA, Lorenzoni M. Immediate occlusal vs nonocclusal loading of implants: A randomized prospective clinical pilot study and patient centered outcome after 36 months. Clin Implant Dent Relat Res. 2019;21:766–774. 10.1111/cid.12770
[Corrections added on 28 June 2019 after first publication: The copyright has been corrected.]
REFERENCES
- 1. Hof M, Pommer B, Ambros H, Jesch P, Vogl S, Zechner W. Does timing of implant placement affect implant therapy outcome in the aesthetic zone? A clinical, radiological, aesthetic, and patient‐based evaluation. Clin Implant Dent Relat Res. 2015;17:1188‐1199. [DOI] [PubMed] [Google Scholar]
- 2. Payer M, Heschl A, Wimmer G, Wegscheider W, Kirmeier R, Lorenzoni M. Immediate provisional restoration of screw‐type implants in the posterior mandible: results after 5 years of clinical function. Clin Oral Implants Res. 2010;21:815‐821. [DOI] [PubMed] [Google Scholar]
- 3. Arnhart C, Kielbassa AM, Martinez‐de Fuentes R, et al. Comparison of variable‐thread tapered implant designs to a standard tapered implant design after immediate loading. A 3‐year multicentre randomised controlled trial. Eur J Oral Implantol. 2012;5:123‐136. [PubMed] [Google Scholar]
- 4. Degidi M, Nardi D, Piattelli A. A comparison between immediate loading and immediate restoration in cases of partial posterior mandibular edentulism: a 3‐year randomized clinical trial. Clin Oral Implants Res. 2010;21:682‐687. [DOI] [PubMed] [Google Scholar]
- 5. Balshi SF, Wolfinger GJ, Balshi TJ. A prospective study of immediate functional loading, following the teeth in a day protocol: a case series of 55 consecutive edentulous maxillas. Clin Implant Dent Relat Res. 2005;7:24‐31. [DOI] [PubMed] [Google Scholar]
- 6. Lindeboom JA, Frenken JW, Dubois L, Frank M, Abbink I, Kroon FH. Immediate loading vs immediate provisionalization of maxillary single‐tooth replacements: a prospective randomized study with BioComp implants. J Oral Maxillofac Surg. 2006;64:936‐942. [DOI] [PubMed] [Google Scholar]
- 7. Cannizzaro G, Leone M, Consolo U, Ferri V, Esposito M. Immediate functional loading of implants placed with flapless surgery vs conventional implants in partially edentulous patients: a 3‐year randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2008;23:867‐875. [PubMed] [Google Scholar]
- 8. Cannizzaro G, Torchio C, Leone M, Esposito M. Immediate vs early loading of flapless‐placed implants supporting maxillary full‐arch prostheses: a randomised controlled clinical trial. Eur J Oral Implantol. 2008;1:127‐139. [PubMed] [Google Scholar]
- 9. Cannizzaro G, Felice P, Leone M, Checchi V, Esposito M. Flapless vs open flap implant surgery in partially edentulous patients subjected to immediate loading: 1‐year results from a split‐mouth randomised controlled trial. Eur J Oral Implantol. 2011;4:177‐188. [PubMed] [Google Scholar]
- 10. Donati M, Botticelli D, La Scala V, Tomasi C, Berglundh T. Effect of immediate functional loading on osseointegration of implants used for single tooth replacement. A human histological study. Clin Oral Implants Res. 2013;24:738‐745. [DOI] [PubMed] [Google Scholar]
- 11. Östman PO, Wennerberg A, Ekestubbe A, Albrektsson T. Immediate occlusal loading of NanoTite tapered implants: a prospective 1‐year clinical and radiographic study. Clin Implant Dent Relat Res. 2013;15:809‐818. [DOI] [PubMed] [Google Scholar]
- 12. Hof M, Tepper G, Koller B, Krainhöfner M, Watzek G, Pommer B. Esthetic evaluation of single‐tooth implants in the anterior mandible. Clin Oral Implants Res. 2014;25:1022‐1026. [DOI] [PubMed] [Google Scholar]
- 13. Weber HP, Morton D, Gallucci GO, Roccuzzo M, Cordaro L, Grutter L. Consensus statements and recommended clinical procedures regarding loading protocols. Int J Oral Maxillofac Implants. 2009;24(Suppl):180‐183. [PubMed] [Google Scholar]
- 14. Romanos GE. Immediate Loading in the Posterior Area of the Mandible. Animal and Clinical Studies. Berlin: Quintessence Publ; 2005:140. [Google Scholar]
- 15. Calandriello R, Tomatis M. Immediate occlusal loading of single lower molars using Brånemark system wide platform TiUnite implants: a 5‐year follow‐up report of a prospective clinical multicenter study. Clin Implant Dent Relat Res. 2011;13:311‐318. [DOI] [PubMed] [Google Scholar]
- 16. Cornelini R, Cangini F, Covani U, Barone A, Buser D. Immediate loading of implants with 3‐unit fixed partial dentures: a 12‐month clinical study. Int J Oral Maxillofac Implants. 2006;21:914‐918. [PubMed] [Google Scholar]
- 17. Moraschini V, Porto Barboza E. Immediate vs conventional loaded single implants in the posterior mandible: a meta‐analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2016;45:85‐92. [DOI] [PubMed] [Google Scholar]
- 18. Romanos GE. Wound healing in immediately loaded implants. Periodontol 2000. 2015;68(1):153‐167. [DOI] [PubMed] [Google Scholar]
- 19. Glauser R, Rée A, Lundgren A, Gottlow J, Hämmerle CH, Schärer P. Immediate occlusal loading of Brånemark implants applied in various jawbone regions: a prospective, 1‐year clinical study. Clin Implant Dent Relat Res. 2001;3:204‐213. [DOI] [PubMed] [Google Scholar]
- 20. Zembic A, Glauser R, Khraisat A, Hämmerle CH. Immediate vs early loading of dental implants: 3‐year results of a randomized controlled clinical trial. Clin Oral Implants Res. 2010;21:481‐489. [DOI] [PubMed] [Google Scholar]
- 21. Margossian P, Mariani P, Stephan G, Margerit J, Jorgensen C. Immediate loading of mandibular dental implants in partially edentulous patients: a prospective randomized comparative study. Int J Periodontics Restorative Dent. 2012;32:e51‐e58. [PubMed] [Google Scholar]
- 22. Degidi M, Piattelli A. Comparative analysis study of 702 dental implants subjected to immediate functional loading and immediate nonfunctional loading to traditional healing periods with a follow‐up of up to 24 months. Int J Oral Maxillofac Implants. 2005;20:99‐107. [PubMed] [Google Scholar]
- 23. Vogl S, Stopper M, Hof M, Wegscheider WA, Lorenzoni M. Immediate occlusal vs non‐occlusal loading of implants: a randomized clinical pilot study. Clin Implant Dent Relat Res. 2015;17:589‐597. [DOI] [PubMed] [Google Scholar]
- 24. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533‐551. [DOI] [PubMed] [Google Scholar]
- 25. Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2:145‐151. [DOI] [PubMed] [Google Scholar]
- 26. Misch CE, Perel ML, Wang HL, et al. Implant success, survival, and failure: the international congress of Oral Implantologists (ICOI) Pisa Consensus conference. Implant Dent. 2008;17:5‐15. [DOI] [PubMed] [Google Scholar]
- 27. Lekholm & Zarb . In: Tissue‐Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago: Quintessence Publishing; 1985. [Google Scholar]
- 28. Gapski R, Wang HL, Mascarenhas P, Lang NP. Critical review of immediate implant loading. Clin Oral Implants Res. 2003;14:515‐527. [DOI] [PubMed] [Google Scholar]
- 29. Romanos GE. Present status of immediate loading of oral implants. J Oral Implantol. 2004;30:189‐197. [DOI] [PubMed] [Google Scholar]
- 30. Ghoul WE, Chidiac JJ. Prosthetic requirements for immediate implant loading: a review. J Prosthodont. 2012;21:141‐154. [DOI] [PubMed] [Google Scholar]
- 31. Esposito M, Grusovin MG, Achille H, Coulthard P, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2009;21(1):CD003878. [DOI] [PubMed] [Google Scholar]
- 32. Kokovic V, Jung R, Feloutzis A, Todorovic VS, Jurisic M, Hämmerle CH. Immediate vs early loading of SLA implants in the posterior mandible: 5‐year results of randomized controlled clinical trial. Clin Oral Implants Res. 2014;25:e114‐e119. [DOI] [PubMed] [Google Scholar]
- 33. Merli M, Moscatelli M, Mariotti G, Piemontese M, Nieri M. Immediate vs early non‐occlusal loading of dental implants placed flapless in partially edentulous patients: a 3‐year randomized clinical trial. J Clin Periodontol. 2012;39:196‐202. [DOI] [PubMed] [Google Scholar]
- 34. Hatano N, Yamaguchi M, Yaita T, Ishibashi T, Sennerby L. New approach for immediate prosthetic rehabilitation of the edentulous mandible with three implants: a retrospective study. Clin Oral Implants Res. 2011;22:1265‐1269. [DOI] [PubMed] [Google Scholar]
- 35. Lorenzoni M, Pertl C, Zhang K, Wegscheider WA. In‐patient comparison of immediately loaded and non‐loaded implants within 6 months. Clin Oral Implants Res. 2003;14:273‐279. [DOI] [PubMed] [Google Scholar]
- 36. Capelli M, Zuffetti F, Del Fabbro M, Testori T. Immediate rehabilitation of the completely edentulous jaw with fixed prostheses supported by either upright or tilted implants: a multicenter clinical study. Int J Oral Maxillofac Implants. 2007;22:639‐644. [PubMed] [Google Scholar]
- 37. Malo P, de Araujo Nobre M, Lopes A. The use of computer‐guided flapless implant surgery and four implants placed in immediate function to support a fixed denture: preliminary results after a mean follow‐up period of thirteen months. J Prosthet Dent. 2007;97(6 Suppl):S26‐S34. [DOI] [PubMed] [Google Scholar]
- 38. Romanos GE, Testori T, Degidi M, Piattelli A. Histologic and histomorphometric findings from retrieved, immediately occlusally loaded implants in humans. J Periodontol. 2005;76(11):1823‐1832. [DOI] [PubMed] [Google Scholar]
- 39. Romanos GE, Johansson CB. Immediate loading with complete implant‐supported restorations in an edentulous heavy smoker: histologic and histomorphometric analyses. Int J Oral Maxillofac Implants. 2005;20(2):282‐290. [PubMed] [Google Scholar]
- 40. Romanos GE, Aydin E, Locher K, Nentwig GH. Immediate vs delayed loading in the posterior mandible: a split‐mouth study with up to 15 years of follow‐up. Clin Oral Implants Res. 2016;27:e74‐e79. [DOI] [PubMed] [Google Scholar]
- 41. Zuffetti F, Esposito M, Galli F, Capelli M, Grandi G, Testori T. A 10‐year report from a multicentre randomised controlled trial: immediate non‐occlusal vs early loading of dental implants in partially edentulous patients. Eur J Oral Implantol. 2016;9:219‐230. [PubMed] [Google Scholar]
- 42. Degidi M, Nardi D, A2 P. 10‐year prospective cohort follow‐up of immediately restored XiVE implants. Clin Oral Implants Res. 2016;27(6):694‐700. 10.1111/clr.12642. [DOI] [PubMed] [Google Scholar]
- 43. De Bruyn H, Raes S, Ostman PO, Cosyn J. Immediate loading in partially and completely edentulous jaws: a review of the literature with clinical guidelines. Periodontol 2000. 2014;66(1):153‐187. 10.1111/prd.12040. [DOI] [PubMed] [Google Scholar]
- 44. Korfage A, Raghoebar GM, Meijer HJA, Vissink A. Patients' expectations of oral implants: a systematic review. Eur J Oral Implantol. 2018;11(Suppl 1):S65‐S76. [PubMed] [Google Scholar]
- 45. Walton TR, Layton DM. Satisfaction and patient‐related outcomes in 128 patients with single implant crowns in situ for up to 14 years. Int J Oral Maxillofac Implants. 2017;32:667‐674. [DOI] [PubMed] [Google Scholar]
- 46. Kielbassa AM, Martinez‐de Fuentes R, Goldstein M, et al. Randomized controlled trial comparing a variable‐thread novel tapered and a standard tapered implant: interim one‐year results. J Prosthet Dent. 2009;101:293‐305. [DOI] [PubMed] [Google Scholar]
- 47. Fortin T, Bosson JL, Isidori M, Blanchet E. Effect of flapless surgery on pain experienced in implant placement using an image‐guided system. Int J Oral Maxillofac Implants. 2006;21:298‐304. [PubMed] [Google Scholar]
- 48. Arisan V, Karabuda CZ, Ozdemir T. Implant surgery using bone‐ and mucosa‐supported stereolithographic guides in totally edentulous jaws: surgical and post‐operative outcomes of computer‐aided vs standard techniques. Clin Oral Implants Res. 2010;21:980‐988. [DOI] [PubMed] [Google Scholar]


