Abstract
Objectives
Persons engaged in the sex industry are at greater risk of HIV and other sexually transmitted infections than the general population. One major factor is exposure to higher levels of risky sexual activity. Expanding condom use is a critical prevention strategy, but this requires negotiation with those buying sex, which takes place in the context of cultural and economic constraints. Impoverished individuals who fear violence are more likely to forego condoms.
Methods
Here we tested the hypotheses that poverty and fear of violence are two structural drivers of HIV infection risk in the sex industry. Using data from the European Centre for Disease Prevention and Control and the World Bank for 30 countries, we evaluated poverty, measured using the average income per day per person in the bottom 40% of the income distribution, and gender violence, measured using homicide rates in women and the proportion of women exposed to violence in the last 12 months and/or since age 16 years.
Results
We found that HIV prevalence among those in the sex industry was higher in countries where there were greater female homicide rates (β = 0.86; P = 0.018) and there was some evidence that self‐reported exposure to violence was also associated with higher HIV prevalence (β = 1.37; P = 0.043). Conversely, HIV prevalence was lower in countries where average incomes among the poorest were greater (β = −1.05; P = 0.046).
Conclusions
Our results are consistent with the theory that reducing poverty and exposure to violence may help reduce HIV infection risk among persons engaged in the sex industry.
Keywords: HIV, poverty, sex work, violence
Introduction
HIV prevalence among those persons engaged in the sex industry – hereafter referred to, reflecting widespread usage, as “sex workers” – appears to be higher in some countries than others 1, 2. For example, although nationally representative data on HIV prevalence among sex workers are rare, in Armenia 1.2% of sex workers are estimated to have HIV infection while in Lithuania 6.7% are estimated to be HIV positive. But what explains this variation?
Patterns of high‐risk behaviours – which vary across countries – may explain some of these cross‐national differences in the prevalence of HIV infection among sex workers 3, 4, 5. Two main risks for HIV infection are injecting drug use and unprotected sex, and the frequency of both activities may vary in the sex worker population in different countries 6, 7. Similarly, the prevalence of irregular condom use is also correlated with a higher risk of contracting HIV infection. For example, irregular condom use is more frequent in Lithuania (23%) than in Armenia (7.1%) and, consequently, all other things being equal, HIV prevalence among sex workers would be expected to be higher in Lithuania than Armenia 1, 7, 8, 9.
Those seeking to reduce HIV transmission among sex workers have often employed individual‐level interventions, such as those seeking to encourage or empower sex workers in ways that increase condom use. These interventions have achieved positive results but the effects are often modest 1, 10, 11. This has turned attention to the importance of structural factors, such as legalization or decriminalization of sex work, which may shape the context in which decisions about potentially risky behaviours are made 7, 12. For example, if selling sex is illegal and police use confiscated condoms as evidence of sex work, then women may be discouraged from carrying condoms lest they be arrested for doing so 13. In short, if the structural constraints on condom use are alleviated then this might also increase the prevalence of regular condom use, thereby reducing HIV prevalence among sex workers 1.
Two major structural factors may affect condom use among those engaged in the sex industry. First, across Europe, “reasons for not using condoms [are] generally economically motivated” 14. Sex workers are making decisions about condom usage according to widely different sets of criteria and constraints 15. Some sex workers may willing forego condoms if a client offers them more money for their services 16, 17. Precarious economic circumstances will probably alter prices in two important ways. First, poverty may lead a sex worker to accept a price for condomless sex that they would reject under less precarious economic circumstances. As one sex worker reports, “Sometimes I feel compelled to agree when I'm desperately in need of money” 18. Secondly, poverty may reduce the price differential between condom‐protected sex and condomless sex 19. Poverty is expected to shift the constraints surrounding this negotiation in ways that lead to behaviours with greater HIV infection risk 14, 20. The distribution of income in a society and the overall level of economic development can serve as proxies for these economic constraints 21, 22, particularly because women are often more likely to experience poverty than men 23. In these situations, sex workers face a constrained set of choices in condom negotiations or in rejecting possible clients because they ask for unprotected sex 24, 25. Individual‐level evidence consistent with this process has been obtained in China, the Democratic Republic of Congo, and the Philippines 4, 15, 19. This, of course, assumes some level of volition which may not be the case if these men or women are subjected to indentured servitude, and in these circumstances irregular condom use may not be a choice 26. Financial constraints are only one driver of sex work but economically vulnerable sex workers (of various kinds) may be more likely to have unprotected sex (for more money or because they are coerced to do so) and so may also be at greater risk of HIV infection 27.
The second main factor leading sex workers to forego using a condom with clients is pressure or the fear of violence 13, 15, 16, 17. Violence is coercive and is used to push some people into the sex industry – especially among individuals who are trafficked in connection with the sex industry. Violence may also force sex workers into particular kinds of sexual encounters 20, 26. Even when there is no physical harm, the threat of violence remains coercive 28. Those in the sex industry, whether willingly or unwillingly, are particularly vulnerable to violence and, in societies where women face greater violence, they may be even more fearful 20. This may lead individuals to feel unable to reject pressure to engage in unprotected sex, and, for those who are trafficked, rape may occur without condoms if acquiescence is not forthcoming. This has been observed in such diverse settings as South African mining communities 24, 25, 29, 30, 31, 32 and Armenian female sex workers who had histories of physical abuse 30. Female sex workers in Moscow, for example, were three times more likely to test HIV positive if they reported experiencing violence or the threat of violence in the last year 20, 33.
There are other important drivers of condom negotiation in sex work, such as access to condoms and other services, injecting drug use, and legal regulations around sex work 6, 14. However, in this paper we focus our attention on how two structural determinants of HIV infection, i.e. cultural norms and economic development, may affect HIV prevalence among sex workers across the European region 27, 34, 35.
Methods
Sources of data
Data on HIV infection among sex workers are derived from the European Centre for Disease Prevention and Control (ECDC)'s latest estimates for 30 countries 2. In this study, we used data on HIV prevalence provided to the ECDC in connection with the Dublin Declaration and the Global Aids Response Progress Reporting (GARPR). Despite this being the best available data, it does contain several sources of measurement error and potential bias. First, the true number of active sex workers is unknown, and likely to be underestimated, especially in countries where sex work is criminalized. For example, some countries report that they have no sex workers with HIV infection, which is highly unlikely and almost certainly reflects a lack of data 2. Secondly, although the ECDC data primarily measure HIV prevalence among female sex workers, which serves as the focus of our analysis, there are three countries where male sex workers are included in the prevalence estimates 2. However, male sex workers appear to be only a small fraction in these data sets. For example, in Bulgaria they form less than 5% of the total sample. Finally, survey procedures vary across countries, in terms of how data are collected and the sizes of the samples. To address this, we weighted samples based on their size to reduce measurement error. More details on data sources and collection can be found in Appendix S1.
Measuring exposure to gender violence and poverty
To measure gender violence, we used two indicators: first, female homicide rates per 100 000 women from the World Health Organization European Health for All Cause‐Specific Mortality Database 2016 edition (WHO‐MDB) 36. Secondly, we used the prevalence of violence against women developed by the European Institute for Gender Equality (EIGE) 37. This scale is based on a cross‐national survey on self‐reported exposure to (i) physical violence by a partner since the age of 15 years or (ii) in the last 12 months, (iii) sexual violence by a partner since the age of 15 years or (iv) in the last 12 months, (v) sexual violence by a nonpartner since the age of 15 years, and (vi) psychological violence by a partner since the age of 15 years. We followed their coding for the purposes of these analyses (see Appendix S2 for more details). These gender norms are predominantly concerned with relations between men and women and are pertinent here because female sex workers are the vast majority in our data 27.
To measure economic development and poverty, we used two indicators. First, we collected data on average incomes per person among the bottom 40% of the population, adjusted for inflation and purchasing power. Secondly, and as a sensitivity test, we collected data on gross domestic product (GDP) per capita, again adjusted for inflation and purchasing power. Both economic development indicators come from the World Bank data 38. Data for all covariates are listed in Appendix S2.
Statistical analyses
To test whether cultural norms or economic development is associated with HIV prevalence among sex workers, we first present unadjusted models of the association between each of our main predictors; for example:
| (1) |
where i is the country, HIV is the log prevalence of HIV infection among sex workers drawn from the latest available data, and Risk represents four separate indicators which are examined sequentially in four separate regression models. We explored two measures of gender violence (i.e. female homicide rates per 100 000 women and the prevalence of violence against women) and two measures of economic development (i.e. average income per person among the bottom 40% of the population and GDP per capita in 2005, adjusted for inflation and purchasing power (PPP)). β 0 is the constant and ε is the error term. β 1 is the coefficient of interest, measuring the difference in the average HIV prevalence rate among sex workers across these risk factors.
As a sensitivity test, we also examined whether the HIV prevalence among sex workers was associated with the EIGE's index of gender violence, which measures the prevalence of various forms of violence across the life‐course and within the last 12 months from partners and nonpartners, although we only had data on 16 countries 37. As additional robustness checks, we examined whether the female homicide rate remained associated with the HIV prevalence among sex workers after controlling for average income per person among the bottom 40%, GDP per capita, and the legislative environment (contrasting countries where sex work is unregulated, criminalized, an administrative offence, and legalized or decriminalized) 14.
Equation 1 – and all other regression models – are weighted according to the sample size of the country‐specific data. To reduce the possible influence of measurement error, this places greater weight on HIV prevalence estimates derived from large samples, while recognizing that larger sample sizes are still potentially biased. Our assumption is that larger samples of this hard‐to‐reach population are still more representative of this population as a whole than smaller samples. All models were estimated using stata v13.0 (STATA Corp, College Station, Texas, USA).
Results
Gender violence
It is striking that the country with the highest HIV prevalence among sex workers (i.e. 22.2% in Latvia) was also among the countries with the highest female homicide rate (3.48 per 100 000 women). In contrast, the Czech Republic, the country with the lowest HIV prevalence among sex workers (0.1%), had a far lower female homicide rate (0.88 per 100 000 women). Looking across our whole sample, we saw a similar trend. Figure 1 shows the association between the log female homicide rate per 100 000 women and the log HIV prevalence among sex workers. We observed a positive association (β = 0.86; P = 0.018). In countries where the female homicide rate was 1% higher, the HIV prevalence was 0.86% higher among sex workers.
Figure 1.
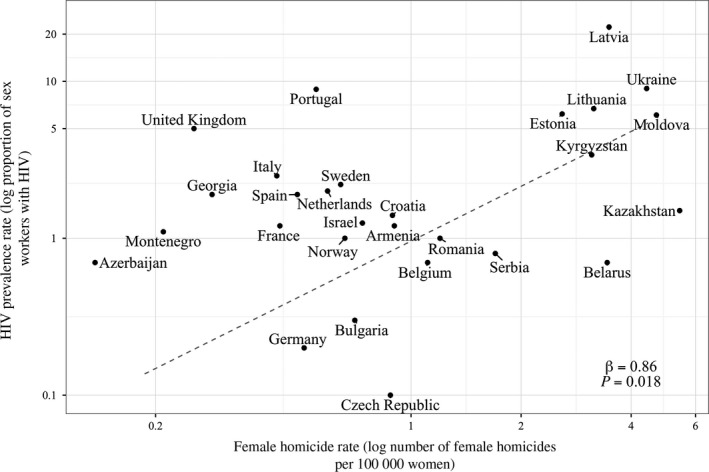
Countries with higher female homicide rates also have higher HIV prevalence among sex workers in European and Central Asian countries. Source: European Centre for Disease Prevention and Control (ECDC) and World Health Organization (WHO). The regression line is weighted by the sample size of the HIV prevalence data.
We also observed that, in countries where disclosed violence against women was greater than the European average (38% or higher), the HIV prevalence rate was higher (β = 1.37; P = 0.043; Table 1). We then split this measure into those indicators that capture the experience of violence in the last 12 months compared with those indicators that capture the experience of violence since the age of 15 years. We observed that HIV prevalence among sex workers was most closely associated with the experience of violence in the last 12 months (β = 1.32; P = 0.073) rather the experience of violence since the age of 15 years (β = −0.032; P = 0.972), pointing to the apparent importance of the current situation.
Table 1.
Violence against women is associated with higher HIV prevalence among sex workers in 16 European and Central Asian countries
| Log HIV prevalence among sex workers (standard error) | |
|---|---|
| Countries with above average rates of disclosed violence towards women (A) | 0.49 (0.28) |
| Countries with average or below average rates of disclosed violence towards women (B) | −0.88 (0.55) |
| Difference (A − B) | 1.37* (0.62) |
| P‐value for the difference (A − B) | 0.043 |
| Number of countries | 16 |
| R 2 | 0.21 |
Source: European Centre for Disease Prevention and Control (ECDC) and European Institute for Gender Equality (EIGE). The regression line was weighted by the sample size of the HIV prevalence data. Standard errors are in parentheses. *p < 0.05
Taken together, these results suggest that, in countries where violence towards women is more common, the HIV prevalence among sex workers is higher.
Poverty
Consistent with the HIV prevalence among sex workers, people in the bottom 40% of the income distribution in Latvia were much poorer [average spending = (PPP) $8.3 per capita per day in 2011] than the same group in the Czech Republic [average spending = (PPP) $15.8 per capita per day in 2011]. Figure 2 shows the association between the log average income of those in the bottom 40% of the population and the log HIV prevalence among sex workers (Fig. 2). We found a negative association between these variables (β = −1.05; P = 0.043), suggesting that the HIV prevalence among sex workers is lower in countries where the poorest in society have higher incomes. As a sensitivity test, we also examined whether variation between countries in log GDP per capita, adjusted for inflation and purchasing power, was associated with the log HIV prevalence among sex workers (Fig. 3). Our measure of GDP had more observations and enabled us to see whether we observed a consistent relationship between indicators. We observed a negative association (β = −0.44; P = 0.022), such that a 1% increase in GDP was associated with a 0.44% decline in the HIV prevalence among sex workers. However, note that the coefficient for GDP is approximately half of the coefficient for average incomes among the poorest groups. This is consistent with the hypothesis that average incomes across the whole population matter less than average incomes among the poorest.
Figure 2.
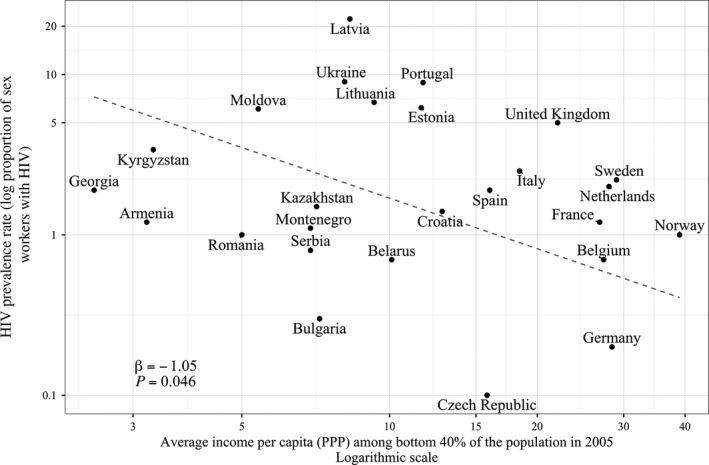
Higher average income among the poorest groups is associated with lower HIV prevalence among sex workers in European and Central Asian countries. Source: European Centre for Disease Prevention and Control (ECDC) and World Health Organization (WHO). The regression line is weighted by the sample size of the HIV prevalence data.
Figure 3.
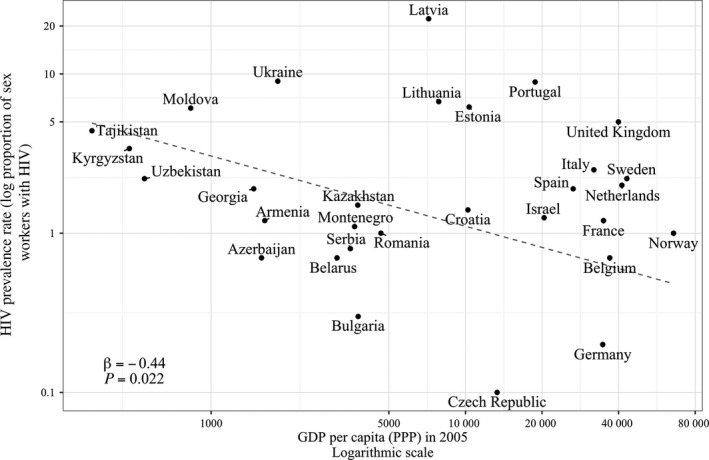
Higher gross domestic product (GDP) is associated with lower HIV prevalence among sex workers in European and Central Asian countries. Source: European Centre for Disease Prevention and Control (ECDC) and World Health Organization (WHO). The regression line is weighted by the sample size of the HIV prevalence data.
One possible confounder for the relationship between economic development and HIV infection is historical exposure to communism. Post‐communist countries tend to be poorer than the other countries included in the sample and, although they promoted labour market equality for women, these countries also enabled a flourishing sex trade, which may in turn have increased exposure to HIV 39. However, we found that the relationship between average income among the poorest and HIV prevalence among sex workers became stronger but increased the standard errors (β = −1.91; P = 0.054), even after we controlled for a dummy variable signifying countries that had communist governments prior to 1989–1991.
Alternative explanations
Although economic factors and pressure are the two primary motivations for inconsistent condom use among sex workers, other factors may also play an important role. Female sex workers who are also injecting drug users are more likely to forego protection while with clients 14. However, even after we controlled for the proportion of sex workers who were injecting drug users, we found that both the female homicide rate and the level of income among the bottom 40% of the income distribution remained associated with HIV prevalence among sex workers (Appendix S1).
Access to health information and free condoms may also influence condom usage, and these services are largely provided by charities and other nongovernmental organizations aimed at helping sex workers 6. We included a measure of the prevalence of these services per 1000 female sex workers and found that this too did not alter the observed relationship between the female homicide rate and the average level of income among the poorest in society (Appendix S2).
Finally, the legislative environment may change how sex workers seek and meet clients 1, 14. Sex workers may be more vulnerable in contexts where sex work is criminalized because condoms can be used as evidence of illegal activity and so sex workers may be disincentivized to carry them. Further, if sex workers cannot turn to the police for help then punters may be more willing to use or threaten to use force in condom negotiations. However, even after controlling for legal regulation, we found that our results remained largely unchanged (Appendix S3).
While these factors may be important in their own right, they did not attenuate the observed associations of HIV prevalence among sex workers with economic constraints and violence towards women.
Discussion
Our analysis yielded several important observations. First, we found a clear association between HIV prevalence among those engaged in the sex industry and gender violence. This association was consistent when measuring gender violence using objective and subjective measurements. Secondly, where incomes were greater, particularly for people at the bottom of the income distribution, HIV prevalence among sex workers was lower. Thirdly, these associations endured even after we adjusted for other factors that may alter condom negotiations, such as access to health and legal services, the prevalence of injecting drug use among sex workers, and legal regulations pertaining to the sex industry.
Of course, there are important limitations to this study. First, it is possible to conduct representative sampling of hidden populations, but regrettably HIV prevalence estimates are often based on unrepresentative samples of these hard‐to‐reach groups 2. Among this set of countries, data collection procedures between surveys are not consistent and so the representativeness of the data analysed here may vary in important ways. Secondly, it is also important to recognize that sex workers are often extremely heterogeneous, both in the settings in which they work and in the control that they have over their working conditions, factors that vary according to cultural norms, the legislative framework, and much else. Our analysis has tried to address some of these differences, but more work will be needed as new data become available. Thirdly, these ecological measures are not perfect proxies of the economic circumstances of sex workers, or their perceptions of the risk of violence. However, these cross‐national associations are consistent with a wealth of individual‐level data which has demonstrated that condom negotiations are primarily influenced by economic motivations and pressure from those attempting to buy sex 14. Moreover, when we checked our results with a more precise measure of the prevalence of violence towards women, albeit this was available for fewer countries, we obtained similar results 37. Fourthly, our measures do not capture change over time, limiting our ability to move beyond documenting correlations. Finally, our study has focussed on violence towards women – and specifically women engaged in the sex industry – and so may have limited relevance to the many male or transsexual sex workers who experience violence or the threat of violence in their work. More work is needed to explore the economic and cultural determinants of HIV prevalence among these groups.
Given these limitations, our findings can only be considered to be suggestive. However, they serve as a reminder of why it is so important to obtain high‐quality data on all vulnerable populations, as a basis for understanding the epidemiology of HIV not only among such groups but also in the wider population 10.
Perhaps the most important conclusion from our study is that, although individual‐level risk factors for HIV infection are important, structural factors may be as important, influencing the pattern of individual‐level risk factors within a country. Our results suggest that gender violence and poverty at the country level may influence micro‐interactions between those individuals engaged in the sex industry and those buying sex, particularly around condom negotiation.
Despite these limitations, our results have important complementarities with the Sustainable Development Goals (SDGs) and suggest measures that can contribute to achieving the WHO's target of reducing new adult HIV infections to 500 000 in 2020 40, 41. Reducing poverty (SDG 1), especially among vulnerable populations, may alter the dynamics of sex work in general and condom negotiations in particular, potentially empowering sex workers to increase condom usage in order to minimize the number of new infections 41. However, our results do not provide guidance on how any specific country may reduce the economic vulnerability of sex workers, but they do suggest that economic growth alone will not necessarily improve the economic situation of sex workers. In addition to growth, our results suggest reducing contemporary gender violence (SDG 5) may also reduce the risk of HIV infection among sex workers. This is particularly important in countries where sex work is a criminal offence or legally prohibited (even if there is no criminal penalty) 42. Only when sex workers are able to communicate with police services about (the threat of) violence without incriminating themselves will they be spared the risk of physical abuse and HIV exposure. Both structural drivers and individual agency impact on condom use and HIV infection risk, and thus future HIV intervention programmes must adopt a more holistic view in order to meet the needs of those engaged in sex work. Long‐term sustainable reductions in HIV/AIDS (SDG 3.3) may require effective steps towards reduction of poverty, in particular female poverty, and reduction of violence towards women.
Funding
This project was funded by the European Centre for Disease Control. The funder had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the article; or in the decision to submit it for publication. Although funded by the ECDC, this study does not necessarily reflect the ECDC's views and in no way anticipates the ECDC's future recommendations in this area.
Supporting information
Appendix S1 Raw data on HIV prevalence among sex workers.
Appendix S2 Index of gender violence.
Appendix S3 Raw data on covariates.
Appendix S4 Gender violence (A), poverty (B), and HIV prevalence among sex workers adjusted for the prevalence of injecting drug use among sex workers.
Appendix S5 Gender violence (A), poverty (B), and HIV prevalence among sex workers adjusted for the number of services offered to sex workers.
Appendix S6 Gender violence (A), poverty (B), and HIV prevalence among sex workers adjusted for legal regulation of sex work.
The copyright line for this article was changed on 4 September 2019 after original online publication.
References
- 1. Shannon K, Strathdee SA, Goldenberg SM et al Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet 2015; 385: 55–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. European Centre for Disease Prevention and Control . Thematic Report: Sex Workers. Monitoring Implementation of the Dublin Declaration on Partnership to Fight HIV/AIDS in Europe and Central Asia: 2014 Progress Report. Stockholm, ECDC, 2015. [Google Scholar]
- 3. Dias S, Gama A, Fuertes R, Mendao L, Barros H. Risk‐taking behaviours and HIV infection among sex workers in Portugal: results from a cross‐sectional survey. Sex Transm Infect 2015; 91: 346–352. [DOI] [PubMed] [Google Scholar]
- 4. Urada LA, Morisky DE, Pimentel‐Simbulan N, Silverman JG, Strathdee SA. Condom negotiations among female sex workers in the Philippines: environmental influences. PLoS ONE 2012; 7: e33282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shannon K, Csete J. Violence, condom negotiation, and HIV/STI risk among sex workers. JAMA 2010; 304: 573–574. [DOI] [PubMed] [Google Scholar]
- 6. Platt L, Jolley E, Rhodes T et al Factors mediating HIV risk among female sex workers in Europe: a systematic review and ecological analysis. BMJ Open 2013; 3: e002836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. UNAIDS . UNAIDS Guidance Note on HIV and Sex Work. Geneva, UNAIDS, 2012. [Google Scholar]
- 8. Choi SYP. Heterogeneous and vulnerable: the health risks facing transnational female sex workers. Sociol Health Illn 2011; 33: 33–49. [DOI] [PubMed] [Google Scholar]
- 9. ECDC . Thematic Report: Sex Workers: Monitoring Implementation of the Dublin Declaration on Partnership to Fight HIV/AIDS in Europe and Central Asia: 2012 Progress. Stockholm, European Centre for Disease Control, 2013. [Google Scholar]
- 10. Shannon K, Montaner JS. The politics and policies of HIV prevention in sex work. Lancet Infect Dis 2012; 12: 500–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patterson TL, Mausbach B, Lozada R et al Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. Am J Public Health 2008; 98: 2051–2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beyrer C, Crago AL, Bekker LG et al An action agenda for HIV and sex workers. Lancet 2015; 385: 287–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Erausquin JT, Reed E, Blankenship KM. Change over time in police interactions and HIV risk behavior among female sex workers in Andhra Pradesh, India. AIDS Behav 2015; 19: 1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Platt L, Jolley E, Hope V et al HIV Epidemics in the European Region: Vulnerability and Response. Washington, D.C., World Bank, 2015. [Google Scholar]
- 15. Choi SY, Holroyd E. The influence of power, poverty and agency in the negotiation of condom use for female sex workers in mainland China. Cult Health Sex 2007; 9: 489–503. [DOI] [PubMed] [Google Scholar]
- 16. Gertler P, Shah M, Bertozzi SM. Risky business: the market for unprotected commercial sex. J Polit Econ 2005; 113: 518–550. [Google Scholar]
- 17. Cawley J, Ruhm CJ. The economics of risky health behaviors In: Arrow KJ, ed. Handbook of Health Economics. London, Elsevier, 2011: 95–199. [Google Scholar]
- 18. Wojcicki JM, Malala J. Condom use, power and HIV/AIDS risk: sex‐workers bargain for survival in Hillbrow/Joubert Park/Berea. Johannesburg. Soc Sci Med 2001; 53: 99–121. [DOI] [PubMed] [Google Scholar]
- 19. Ntumbanzondo M, Dubrow R, Niccolai LM, Mwandagalirwa K, Merson MH. Unprotected intercourse for extra money among commercial sex workers in Kinshasa, Democratic Republic of Congo. AIDS Care 2006; 18: 777–785. [DOI] [PubMed] [Google Scholar]
- 20. Rekart ML. Sex‐work harm reduction. Lancet 2005; 366: 2123–2134. [DOI] [PubMed] [Google Scholar]
- 21. Deaton A. Health, inequality, and economic development. J Econ Lit 2003; 41: 113–158. [Google Scholar]
- 22. Deaton A. The Great Escape: Health, Wealth, and the Origins of Inequality. Princeton, Princeton University Press, 2013. [Google Scholar]
- 23. Nations U. The World's Women 2015: Trends and Statistics. In: Affairs DoEaS, ed. New York: UN; 2015.
- 24. Shannon K, Strathdee SA, Shoveller J, Rusch M, Kerr T, Tyndall MW. Structural and environmental barriers to condom use negotiation with clients among female sex workers: implications for HIV‐prevention strategies and policy. Am J Public Health 2009; 99: 659–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shannon K, Kerr T, Strathdee SA, Shoveller J, Montaner JS, Tyndall MW. Prevalence and structural correlates of gender based violence among a prospective cohort of female sex workers. BMJ 2009; 339: b2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. UNODC . Global Report on Trafficking in Persons. Vienna, United Nations, 2014. [Google Scholar]
- 27. Strathdee SA, Crago AL, Butler J, Bekker LG, Beyrer C. Dispelling myths about sex workers and HIV. Lancet 2015; 385: 4–7. [DOI] [PubMed] [Google Scholar]
- 28. Simic M, Rhodes T. Violence, dignity and HIV vulnerability: street sex work in Serbia. Sociol Health Illn 2009; 31: 1–16. [DOI] [PubMed] [Google Scholar]
- 29. Hunter M. The changing political economy of sex in South Africa: the significance of unemployment and inequalities to the scale of the AIDS pandemic. Soc Sci Med 2007; 64: 689–700. [DOI] [PubMed] [Google Scholar]
- 30. Markosyan K, Lang DL, Darbinyan N, Diclemente RJ, Salazar LF. Prevalence and correlates of inconsistent condom use among female sex workers in Armenia. Sexual Health 2011; 8: 259–261. [DOI] [PubMed] [Google Scholar]
- 31. Wirtz AL, Schwartz S, Ketende S et al Sexual violence, condom negotiation, and condom use in the context of sex work: results from two West African countries. J Acquir Immune Defic Syndr 2015; 68 (Suppl. 2): S171–S179. [DOI] [PubMed] [Google Scholar]
- 32. Tounkara FK, Diabate S, Guedou FA et al Violence, condom breakage, and HIV infection among female sex workers in Benin, West Africa. Sex Transm Dis 2014; 41: 312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Decker MR, Wirtz AL, Baral SD et al Injection drug use, sexual risk, violence and STI/HIV among Moscow female sex workers. Sex Transm Infect 2012; 88: 278–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Saggurti N, Verma RK, Halli SS et al Motivations for entry into sex work and HIV risk among mobile female sex workers in India. J Biosoc Sci 2011; 43: 535–554. [DOI] [PubMed] [Google Scholar]
- 35. Pando MA, Coloccini RS, Reynaga E et al Violence as a barrier for HIV prevention among female sex workers in Argentina. PLoS ONE 2013; 8: e54147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. WHO . WHO European Health for All Database. Geneva, World Health Organization, 2016. [Google Scholar]
- 37. Bonfils LD, Humbert AL, Ivaškait≐‐Tamošiūn≐ V et al Gender equality index report. In: Equality EIfG, ed. Brussels, EIGE, 2013.
- 38. World Bank . World Bank Indicators. In: Bank W, ed. Washington, DC, 2016.
- 39. Havelkova B. Blaming all women: on regulation of prostitution in state socialist Czechoslovakia. Oxford J Legal Stud 2016; 36: 165–191. [Google Scholar]
- 40. UN . Transforming Our World: The 2030 Agenda for Sustainable Development. New York, United Nations, 2015. [Google Scholar]
- 41. WHO . Global Health Sector Strategy on HIV, 2016–2021: Towards Ending AIDS. Geneva, Switzerland, World Health Organization, 2016. [Google Scholar]
- 42. Reeves A, Steele S, McKee M, Amato‐Gauci A, Semenza JC, Stuckler D. National sex work policy and HIV prevalence among sex workers: an ecological regression analysis of 27 European countries. Lancet HIV 2017; 4(3): e134–e140. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Raw data on HIV prevalence among sex workers.
Appendix S2 Index of gender violence.
Appendix S3 Raw data on covariates.
Appendix S4 Gender violence (A), poverty (B), and HIV prevalence among sex workers adjusted for the prevalence of injecting drug use among sex workers.
Appendix S5 Gender violence (A), poverty (B), and HIV prevalence among sex workers adjusted for the number of services offered to sex workers.
Appendix S6 Gender violence (A), poverty (B), and HIV prevalence among sex workers adjusted for legal regulation of sex work.


