Summary
Background
The prevalence of obesity in childhood is of high concern, especially in deprived populations. We explored trends in obesity following the introduction of a citywide strategy focused on preschool children.
Methods
Analysis of obesity prevalence using the National Child Measurement Programme 2009 to 2017 for primary‐school children in Leeds using 5‐year aggregated data for Leeds, comparable cities, and England as a whole.
Results
Prevalence of obesity in Leeds for school entry children fell significantly (9.4% to 8.8%), whilst comparable cities (CC) and England as a whole showed no change (comparison of trends: P < 0.001 and P < 0.001). The reduction in Leeds was primarily in the most deprived (11.5% to 10.5%; trend comparison CC: P < 0.001, Eng: P < 0.001), but also amongst the affluent (6.8% to 6.0%; trend comparison CC: P = 0.087, Eng: P = 0.012).
Prevalence in older children in Leeds was unchanged whilst it increased for comparable cities and England (trend comparison CC: P < 0.001, Eng: P < 0.001). In the deprived, obesity increased: Leeds by 1.4%; CC 1.3%, England 1% (trend comparison Eng: P = 0.004). In the affluent, obesity prevalence reduced more in Leeds than elsewhere: 2% in Leeds, 0.8% in CC, and 0.7% in England (trend comparison CC: P < 0.001, Eng: P ≤ 0.001).
Conclusions
There has been a notable decrease in the prevalence of obesity especially amongst the most disadvantaged children at entry to primary school in Leeds. How this was achieved merits in‐depth consideration.
Keywords: childhood obesity, national child measurement programme, obesity prevalence, health disparities, health inequalities
1. INTRODUCTION
Childhood obesity is one of the greatest public health challenges of our time. More than one third of children are affected by overweight or obesity by the time they leave primary school, and severe obesity within this group has reached its highest point yet, with stark social inequalities continuing to increase.1 The high risk of persistence of excess weight into adulthood heralds the development of comorbidities, lower quality of life, and reduced life expectancy. Successful interventions to prevent obesity in childhood should allow children to live longer, healthier lives, reduce health inequalities, and bring about future savings to health care systems and the wider economy. Childhood obesity prevention is a priority for the World Health Organization and national governments around the world. In England, the government has recently published Chapter 2 of its childhood obesity plan2 with an ambitious target to halve child obesity by 2030 and to reduce obesity inequalities between the least and most deprived.
As part of its strategy to monitor obesity in children, England has a comprehensive surveillance scheme—the National Child Measurement Programme (NCMP).3 Since 2006, local authorities have been required to measure and report children's weight and height in state‐maintained schools annually. The measurements are taken at school entry (Reception) when children are aged 4 to 5 years and in their final year of primary school at 10 to 11 years old. National coverage is over 95% of eligible children allowing accurate mapping of the prevalence of obesity nationally and at a local level. The data is cleaned, analysed, and reported at a national level, and anonymized data is made available for additional analyses.
The most recent data from the NCMP (2016/17) show that 9.6% of children in England are affected by obesity on starting school (defined as equal to or above the 95th centile for BMI on the UK 1990 national references4) with the prevalence of obesity increasing to 20% in children aged 10 to 11 years.5 Two thirds (68%) of children who have obesity at school entry continue to be affected 6 years later.6 Health disparities are stark with the prevalence of obesity in the most deprived decile of the population more than twice that in the least deprived, a gap which has widened over the last 10 years.5
Leeds is an industrial city in the North of England with a population of over 800 000 with significant areas of disadvantage within its boundaries. In 2009, the city enacted a local obesity strategy which focused heavily on preschool children. The strategy was underpinned by the concept of progressive universalism, as propounded in England's National Service Framework for Children,7 offering population‐level interventions but aiming to provide disproportionate benefit to those in the most deprived areas.
We used data from the NCMP to examine secular trends in childhood obesity in the City of Leeds and relate our findings to the national picture and to local authorities of similar sociodemographic make‐up, focusing in particular on the differences in prevalence between areas of disadvantage and affluence. We were interested to explore if the focus of the Leeds obesity strategy would result in more positive outcomes for children in Leeds than in comparative cities or the country as a whole, particularly regarding Reception children and those in more deprived communities.
2. METHODS
The NCMP surveys primary school children annually and involves Reception children who are between 4.0 and 5.9 years of age and Year 6 children who are between 10.0 and 11.9 years of age. The NCMP is currently directed by Public Health England. Local Authority Public Health Departments commission, train, and oversee the measuring of weights and heights. All state primary schools in England are invited to participate; pupils are invited to participate on an opt‐out basis. Data are entered by using the NCMP electronic system and are collated by the Health and Social Care Information Centre.
We used Public Health England's online NCMP “Fingertips” data tool,8 which provides anonymized and “cleaned” data on the prevalence of underweight, healthy weight, overweight, obesity, and severe obesity for Reception and Year 6 children from 2006 to 2007 school year, when the NCMP was first implemented, until 2016/7.5 We focused on children identified as having obesity, defined as BMI >95% on the UK 1990 growth reference.4
We analysed the prevalence of obesity for both Reception (school entry, aged 4‐5 years) and Year 6 (10‐11 years) children from 2009‐2010 to 2016‐2017 using 5‐year aggregate data provided in the tool. The aggregate data, which provides information by local authority for quintiles of deprivation, is only available from 2009 to 2010 school year. Accordingly, this date was used as our baseline for the analysis, with data up to the latest figures available for 2016 to 2017 school year. This is similar to a moving average over the 8‐year study period (2009 to 2017) providing four data points. The data available, and used in our analyses, are only estimates of prevalence of obesity and their associated standard errors (sample sizes for all groups were not available).
We examined data for Leeds and compared this to the whole of England and also to the areas defined as Leeds' closest sociodemographic comparators on the NCMP tool. The NCMP utilises the “Nearest Neighbours” measure,9 which was developed independently by the Chartered Institute of Public Finance and Accountancy (CIPFA) and is a commonly used public health comparator. It is based on a number of established indicators including population size, output area density, taxbase per head, proportion aged 0 to 17 years, proportion unemployed, in lower NS‐SEC (social) groups, in receipt of housing benefit, born outside the UK, and standardised mortality ratio. This score, created by CIPFA, is based on traditional Euclidean distance for any pair of local authorities using the (standardised) variables described above (see Appendix for further information on this method). The NCMP tool identifies only the 15 closest “neighbours” as an option when comparing ANY area (eg, Leeds, Birmingham, Warwick, etc.).
For Leeds, the 15 closest “neighbours” at the start of the study period in 2009 were Sheffield, Kirklees, Bristol, Newcastle upon Tyne, Coventry, Bolton, Wakefield, Derby, Bradford, Dudley, Medway, Liverpool, Swindon, County Durham, and Warrington.
We present the results descriptively for the whole population and for the most, middle, and least deprived quintiles based on the English Government Index of Multiple Deprivation (IMD) for small areas or neighbourhoods,10 to compare prevalence and trends. We used a simple linear model weighted by the standard errors reported for the prevalence estimates and compared unstandardized beta coefficients for the modelled trends using simple z‐scores. These are reported as P‐values where the null hypothesis is of equivalent trends. All three paired comparisons, Leeds vs Neighbours, Leeds vs England, and Neighbours vs England, are reported.
Ethical permission for this secondary analysis of anonymised data was not required.
3. RESULTS
In 2016 to 17, data were available for 95% of eligible children across England (see Table 1). In Leeds 9675 (91.4%) Reception children were measured and 7889 (90.4%) Year 6 children. Mean coverage for Leeds over the 8‐year period was 94.9% for Reception children (range 93.4%‐95.6%) and 87.6% for Y6 (range 66.9%‐96.5%); the lower coverage in Y6 being due to a data entry error involving entire schools in the system in two separate years and assumed to have occurred at random.
Table 1.
Levels of obesity in school children in England, Leeds, and Leeds' 15 statistical neighbours: 5‐year aggregate data (prevalence [SE]) at start and end of the observation period 2009 to 2017: Figures are presented for the population and according to quintiles of deprivation`. Obesity is defined as BMI >95th centile on the UK 1990 growth charts
| Reception | Year 6 | |||||
|---|---|---|---|---|---|---|
| 9/10 to 13/14 | 12/13 to 16/17 | p | 9/10 to 13/14 | 12/13 to 16/17 | p | |
| Leeds | 9.4 (0.14) | 8.8 (0.13) | <0.005 | 19.7 (0.22) | 19.6 (0.21) | 0.6 |
| Neighbours | 9.8 (0.06) | 9.8 (0.05) | 0.8 | 20.2 (0.08) | 20.9 (0.08) | 0.005 |
| England | 9.5 (0.02) | 9.4 (0.02) | 0.3 | 19.0 (0.02) | 19.4 (0.02) | 0.02 |
| Most deprived | ||||||
| Leeds | 11.5 (0.25) | 10.5 (0.23) | 0.01 | 22.6 (0.39) | 24.0 (0.37) | 0.009 |
| Neighbours | 11.6 (0.11) | 11.7 (0.10) | 0.5 | 23.6 (0.16) | 24.9 (0.16) | 0.007 |
| England | 12.0 (0.04) | 12.0 (0.04) | 0.8 | 23.9 (0.05) | 24.9 (0.05) | 0.004 |
| Average level of deprivation | ||||||
| Leeds | 8.3 (0.36) | 8.4 (0.35) | 0.9 | 19.3 (0.60) | 18.1 (0.55) | 0.03 |
| Neighbours | 9.0 (0.15) | 8.7 (0.15) | 0.1 | 19.3 (0.22) | 19.3 (0.22) | 0.7 |
| England | 9.1 (0.04) | 8.9 (0.04) | 0.2 | 18.7 (0.06) | 18.8 (0.06) | 0.02 |
| Most affluent | ||||||
| Leeds | 6.8 (0.34) | 6.0 (0.29) | 0.03 | 14.9 (0.53) | 12.9 (0.45) | 0.008 |
| Neighbours | 6.5 (0.19) | 6.1 (0.15) | 0.1 | 13.9 (0.26) | 13.1 (0.21) | 0.02 |
| England | 6.7 (0.04) | 6.3 (0.03) | 0.03 | 13.4 (0.05) | 12.7 (0.05) | 0.003 |
p < 0.02. Bold figures indicate statistical significance.
From 2009‐2010 to 2016‐2017 in Leeds, the prevalence of obesity for children in Reception fell significantly from 9.4% to 8.8% (P < 0.005), representing a 6.4% reduction in the proportion of children with obesity. By comparison, data from Leeds' statistical neighbours and England overall showed no change in the prevalence of obesity (Figure 1). The prevalence of obesity in children in Year 6 in Leeds remained stable over the period of the study but increased in the statistical neighbouring cities and for England as a whole (see Figure 2).
Figure 1.
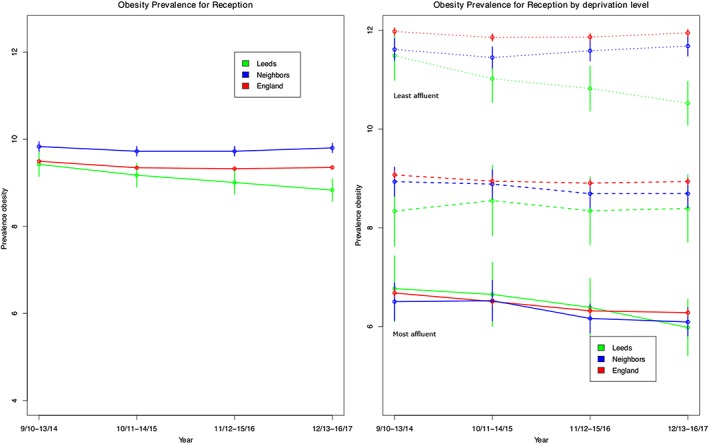
Levels of obesity in children in reception year (aged 4‐5 yrs) in England, Leeds, and Leeds' 15 statistical neighbours: 5‐year aggregate data between 2009 and 2017. Obesity is defined as BMI >95th centile on the UK 1990 growth charts
Figure 2.
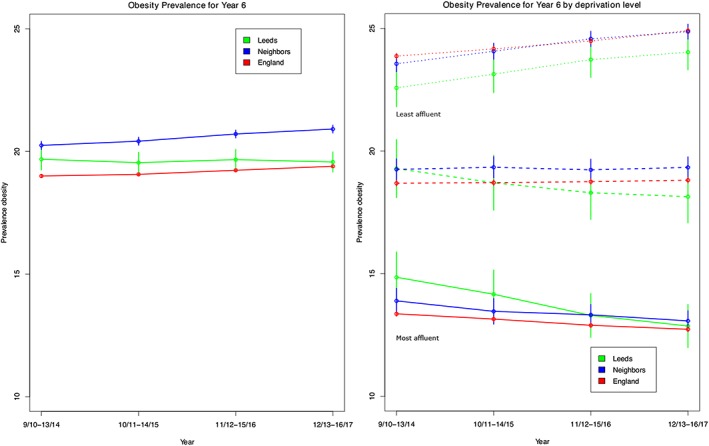
Levels of obesity in children in year 6 (aged 10‐11 yrs) in England, Leeds, and Leeds' 15 statistical neighbours: 5 year aggregate data between 2009 and 2017. Obesity is defined as BMI >95th centile on the UK 1990 growth charts
In Leeds, the reduction in the prevalence of obesity amongst children in Reception occurred principally in the most deprived quintile where it fell significantly from 11.5 to 10.5% (P = 0.01) representing a relative reduction of 8.7% in children affected by obesity (Table 1 and Figure 1). By contrast, there was no change in the prevalence of obesity for children from the most deprived areas in Leeds' statistical neighbours or for England overall. There was also a reduction in the prevalence of obesity in children from the most affluent areas in Leeds of 0.8 percentage points (6.8% to 6% [P = 0.03]). This compared with a reduction of 0.4% for England as a whole and no significant change for Leeds' statistical neighbours.
Amongst children in Year 6, the prevalence of obesity increased amongst children from the most deprived areas in all three populations. For children from the most affluent quintile in Leeds, there was a reduction of 2% (14.9% to 12.9%; P = 0.008), whereas the decrease in England and Leeds' statistical neighbours was less than 1%. Only Leeds showed a reduction in the prevalence of obesity for children in the middle quintile of deprivation.
3.1. Statistical comparison of trends
In reception aged children, direct statistical comparisons of trends corroborate the descriptive findings. There were statistically significant differences in the trends in obesity in Leeds compared with England overall and in the most and least deprived group. A similar pattern was observed when comparing Leeds vs statistical neighbours with a significantly different trend in the overall prevalence of obesity and in the most deprived groups. Comparisons between England and Leeds' statistical neighbours showed no significant differences between trends across all deprivation levels or overall (see Table 2).
Table 2.
P‐values for comparison of trendsa (9/10 to 16/17) between Leeds, Leeds' statistical neighbours, and England. Comparisons presented by the two age groups overall and stratified by deprivation level (values rounded to four decimal places)
| Leeds vs neighbours | Leeds vs England | Neighbours vs England | |
|---|---|---|---|
| Reception | |||
| Overall | <0.001 | <0.001 | 0.3861 |
| Least deprived | 0.0873 | 0.0122 | 0.6872 |
| Avg deprived | 0.1430 | 0.5201 | 0.1701 |
| Most deprived | <0.001 | <0.001 | 0.4448 |
| Year 6 | |||
| Overall | <0.001 | <0.001 | <0.001 |
| Least deprived | <0.001 | <0.001 | 0.2669 |
| Avg deprived | <0.001 | <0.001 | 0.3468 |
| Most deprived | 0.4016 | 0.0041 | 0.0224 |
These are based on a simple z‐score obtained from comparing the two unstandardized beta coefficients equivalent to the estimated trend for each locality and using their associated standard errors. For example, for Reception, the estimated linear trend (SE) for Leeds was −0.2 (0.013) whilst for its neighbours was −0.01 (0.03) giving a Z‐score = ((−.2) – (−0.01) /sqrt((0.013^2)+(0.03^2)) = −5.75; P‐val < 0.001.
For children in Year 6, comparisons between Leeds and other areas by quintile of deprivation were significantly different in all except when comparing trends for Leeds vs statistical neighbours in the most deprived group. Comparison between England vs statistical neighbours was significant in the most deprived group and overall but not for the other two deprivation groups (see Table 2).
4. DISCUSSION
Our analysis has shown that trends in the prevalence of obesity amongst children in Leeds differ significantly from its closest statistical neighbours and for England as a whole. The difference is most marked for children in Reception, where there has been a statistically and clinically significant reduction in the prevalence of obesity of 6.4%, representing 1 in 16, or approximately 625, fewer Reception children with obesity in the city in 2016 to 2017. Of particular note is the finding that this reduction in the prevalence of obesity was principally amongst the most disadvantaged populations in the city, leading to reduced socioeconomic inequalities in the prevalence of obesity. Older children in Leeds also fared better than elsewhere, with no significant increase in the prevalence of obesity, whilst the prevalence increased for its closest sociodemographic neighbours, and for England as a whole. However, this relative advantage was mostly attributable to reductions in the prevalence of obesity in children from the most affluent families, and, at this age, in common with other parts of the country, socioeconomic inequalities in obesity increased.
The prevalence of obesity in childhood has risen dramatically worldwide in less than one generation.11 However, there are recent reports of cities that are demonstrating noteworthy declines in childhood obesity. Amsterdam, a city equivalent in size to Leeds, and renowned for its resolve to eradicate child obesity by 2030, has reported a reduction in obesity of 1.7% for 5 to 10 year olds in disadvantaged areas over 3 years.12 Although the decline in Leeds is smaller, at 1% (with the data confined to younger children), it is the first report of its kind in the UK.
Also worthy of comparison is data reported in the American Child Obesity Declines Project (CODP).13 In this study, four cities that demonstrated a decline in child obesity prevalence were chosen for special in‐depth study to identify lessons that could assist others in their attempts to reduce obesity. Leeds' relative decline of 6.4% in school entry children compares well with these US cities whose relative declines over a 4 to 7‐year period were 2.2% in grades K, 1, and 3 in Anchorage, AK; 4.7% in obesity in grades K‐8 in Philadelphia, PA; 5.5% in obesity in Grades K‐8 in New York City, NY, and 17.5% (for overweight and obesity) in 2 to 4 year olds in Granville County, NC.
Why might Leeds be showing such different trends in childhood obesity compared with the rest of England and particularly its statistical neighbours? One hypothesis might be that Leeds is becoming increasingly gentrified. However, data from the Index of Multiple Deprivation, calculated from the national census, indicate that this is not a plausible explanation as the IMD for Leeds in fact rose from 25.8 to 26.6 over the period of this study, representing an increase in disadvantage for the city as a whole. In any event, gentrification would not account for the reduction in the gap that was found between the affluent and the deprived. It is however noteworthy that Leeds' citywide childhood obesity strategy, implemented in 2009, focused on preschool children. This might explain the discordance between findings for 4 to 5 and 10 to 11 year olds. At its core was the delivery of HENRY,14, 15, 16, 17, 18 a preschool obesity prevention intervention that trains health and early years' practitioners working with young families in its approach, along with a range of programmes for parents and young children in community settings. In Leeds, HENRY was primarily implemented in Children's Centres in the city's most disadvantaged neighbourhoods,19 which provides a putative explanation for reduction in disparities observed amongst children in Reception classes.
Our report's strengths lie in the use of robust growth data which is collected nationally with high coverage across the country and allows comparison between local authorities that have been independently assessed to be statistically similar. We used data accessed via the NCMP Fingertips tool as the basis of the analysis, which presents the data on health disparities in 5‐year aggregate form only starting from 2009 to 2010, giving an 8‐year spread. This precluded more in‐depth analysis of trends and limits the complexity of the models that could be used for its analysis. The use of aggregate data also meant that these comparisons are not independent because the data for England includes Leeds as well as its statistical neighbours. This increases the biases in our comparisons towards the null for the comparison between statistical neighbours and England. By the nature of this observational study using routine data collection, we cannot ascertain how actions taken in Leeds might relate to the differences observed with its nearest neighbours or England as a whole.
In summary, Leeds has shown an impressive decline in childhood obesity when compared with the rest of England and its closest sociodemographic neighbours. This decline is particularly evident in preschool children living in the city's most disadvantaged neighbourhoods. A recent evidence synthesis from the European Commission exploring the impact of interventions on health disparities shows a remarkable lack of interventions reported according to socioeconomic status and disadvantage.20 The USA has taken a lead in pragmatically studying cities showing declines in child obesity. Given the findings reported here, the obesity strategy in Leeds merits further exploration to understand the factors that may have led to its success in reducing the prevalence of obesity and narrowing social inequalities, and to compare this with approaches taken in other cities. Lessons learned may well inform action elsewhere.
FUNDING
The NCMP is funded by the Department of Health in England. S.A.J. is an NIHR Senior Investigator. R.P. and S.A.J. are supported by the Oxford National Institute for Health Research (NIHR) Biomedical Research Centre and NIHR Collaboration for Leadership in Applied Health Research and Care Oxford at Oxford Health NHS Foundation Trust.
CONFLICTS OF INTEREST
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf. All authors declare no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work. J.B. is the Head of Public Health Children and Families Directorate in Leeds. M.C.J.R. was the initial founder of HENRY, K.R. is the chief executive, and D.S. is the policy and communication manager of HENRY.
CONTRIBUTORS
All authors were involved in the design of the paper and approved the final version. M.C.J.R. conceived the paper, initiated the collaborative project, designed the analysis plan, wrote the first draft of the paper, and revised further drafts. She is a guarantor. R.P. analysed the data and revised the paper. D.S. revised the paper for important intellectual content. J.B. revised the paper for content relating to collection of data. K.R. conceived the paper, initiated the collaborative project, and revised the paper. S.J. provided intellectual input to the analysis plan, drafting, and revisions of the paper.
Supporting information
Table S1: Prevalence (SE) of Obesity by temporal grouping in the Reception group.
Table S2: Prevalence (SE) of Obesity by temporal grouping in Year 6.
Rudolf M, Perera R, Swanston D, Burberry J, Roberts K, Jebb S. Observational analysis of disparities in obesity in children in the UK: Has Leeds bucked the trend? Pediatric Obesity. 2019;14:e12529 10.1111/ijpo.12529
REFERENCES
- 1. Trends in childhood BMI between 2006/07 and 2016/17. https://app.box.com/s/og3q86aqejc99okxe9xyvpfvo21xai21/file/306723044116 Published 10 July 2018. Accessed 9 February 2019
- 2. HM Government . Childhood obesity: a plan for action. Chapter 2. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/718903/childhood‐obesity‐a‐plan‐for‐action‐chapter‐2.pdf Published 25 June 2018. Accessed 9 February 2019
- 3. National Child Measurement Programme https://digital.nhs.uk/services/national‐child‐measurement‐programme/ Last edited 2 August 2018. Accessed 9 February 2019
- 4. Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child. 1995;73(1):25‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Child Measurement Programme England 2016/7 school year. https://files.digital.nhs.uk/publication/j/n/nati‐chil‐meas‐prog‐eng‐2016‐2017‐rep.pdf Published 19 October 2017. Accessed 9 February 2019
- 6. Mead E, Batterham AM, Atkinson G, Ells LJ. Predicting future weight status from measurements made in early childhood: a novel longitudinal approach applied to Millennium Cohort Study data. Nutr Diabetes. 2016;6(3):e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Healthy Child Programme: pregnancy and the first five years of life. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/167998/Health_Child_Programme.pdf Published 27 October 2009, Accessed 9 February 2019
- 8. NCMP and child obesity profile. https://fingertips.phe.org.uk/profile/national‐child‐measurement‐programme. Accessed 9 February 2019.
- 9. Chartered Institute of Public Finance and Accountancy (CIPFA) Nearest Neighbours model http://www.cipfastats.net/resources/nearestneighbours/. Accessed 9 February 2019.
- 10. The English Index of Multiple Deprivation (IMD) 2015—Guidance . Department of communities and local government. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/464430/English_Index_of_Multiple_Deprivation_2015_‐_Guidance.pdf Published 2015. Accessed 9 February 2019
- 11. Lobstein T, Jackson‐Leach R, Moodie M, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385(9986):2510‐2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hawkes C, Russell S, Isaacs A, Rutter H, Viner R. Obesity Policy Research Unit (OPRU) briefing paper December 2017. What can be learned from the Amsterdam Healthy Weight programme to inform the policy response to obesity in England? https://www.ucl.ac.uk/obesity‐policy‐research‐unit/sites/obesity‐policy‐research‐unit/files/what‐learned‐from‐amsterdam‐healthy‐weight‐programme‐inform‐policy‐response‐obesity‐england.pdf Published 18 December 2017. Accessed 9 February 2019
- 13. Ottley PG, Dawkins‐Lyn N, Harris C, et al. Childhood obesity declines project: an exploratory study of strategies identified in communities reporting declines. Child Obes. 2018;14(S1):s12‐s21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roberts K. Growing up not out: the HENRY approach to preventing childhood obesity. Br J Obes. 2015;1:87‐92. [Google Scholar]
- 15. Rudolf MCJ, Hunt C, George J, Hajibagheri K, Blair M. HENRY: development, pilot and long term evaluation of a programme to help practitioners work more effectively with parents of babies and preschool children to prevent childhood obesity. Child Care Health Dev. 2010;36(6):850‐857. [DOI] [PubMed] [Google Scholar]
- 16. Willis TA, George J, Hunt C, et al. Combating child obesity: impact of HENRY on parenting and family lifestyle. Pediatr Obes. 2013;9:339‐350. [DOI] [PubMed] [Google Scholar]
- 17. Brown R, Willis TA, Aspinall N, Hunt C, Rudolf MCJ. Preventing child obesity: a long‐term evaluation of the HENRY approach. Community Pract. 2013;86(7):23‐27. [PubMed] [Google Scholar]
- 18. Willis TA, Roberts K, Bryant MJ, Berry T, Rudolf MCJ. The impact of HENRY on parenting and family lifestyle: a national service evaluation of a preschool obesity prevention programme. Public Health. 2016;136:101‐108. [DOI] [PubMed] [Google Scholar]
- 19. Willis TA, Potrata B, Hunt C, Rudolf MCJ. Training community practitioners to work more effectively with parents to prevent childhood obesity: the impact of HENRY upon Children's Centres and their staff. J Hum Nutr Diet. 2012;25(5):460‐468. [DOI] [PubMed] [Google Scholar]
- 20. European Commission . Health Equity Pilot Project (HEPP). https://ec.europa.eu/health/sites/health/files/social_determinants/docs/hepp_screport_exe_en.pdf Published 2017. Accessed 9 February 2019
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Prevalence (SE) of Obesity by temporal grouping in the Reception group.
Table S2: Prevalence (SE) of Obesity by temporal grouping in Year 6.


