Abstract
Background:
Katsina State Government in Northern Nigeria introduced integrated supportive supervision (ISS) in primary health centers. The study was guided by the Primary Health Care Performance Initiative Conceptual Framework. The goal of the study was to measure the impact of ISS on the quality of primary health-care delivery. The outcome variables measured include infrastructure, basic equipment, human resources for health, essential drugs, the number of pregnant women screened for HIV, and the number of children receiving immunization.
Methods:
The study was a cross-sectional survey of 34 health facilities. Kruskal-Wallis nonparametric test followed by Dunn post hoc test and analysis of variance followed by Tukey post hoc test were both employed to compare the mean values of various indicators obtained over 6 visits of the ISS program from July 2018 to December 2018.
Findings:
The study shows the positive effect of the ISS on infrastructure, human resources for health, essential drugs, and the number of pregnant women screened for HIV (P < .05). Human resources for health and the number of children receiving immunization were both not affected by ISS (P > .05).
Conclusion:
Integrated supportive supervision need to be embedded into the 3 levels (primary, secondary, and tertiary) of health-care service delivery.
Implications:
Integrated supportive supervision will strengthen the Katsina State health system, ensure efficient use of the health facility assets and resources utilization, and improve patient/client satisfaction.
Keywords: primary health care, integrated supportive supervision, Katsina state, Nigeria, effect
Introduction
Effective health systems rely on quality primary health-care (PHC) services.1 Primary health care has improved community health in low- and middle-income countries.2 The World Health Organization (WHO) recommends measures that will ensure quality PHC services for equitable and secure health services at the level of the community.3 In Nigeria, the performance of PHC services is poor despite a fair distribution of PHC centers across the country.4 The problem is attributable to a lack of adequate supply chain, patients’ financial access to PHC, infrastructure, drugs, equipment, vaccines, and health worker performance.4 These concerns translate into reduced health indicators for Nigeria, with the country bearing 10% of global disease burden in this decade and showing little signs of improvement.5 The North-western states in Nigeria consistently present below-average health-care indices.6,7 Topographical, cultural, socioeconomic, and developmental factors have been recognized as some of the causes of the poor performance of the region.8,9 Thus, the importance of public health programs at the primary level in the region cannot be overemphasized.
A few available reports indicate a positive impact of public health programs aimed at improving PHC in the North-west states of Nigeria. A program that involved training of midwives to improve maternal, newborn, and child health implemented in Katsina, Yobe, and Zamfara states resulted in positive initial outcomes. Within the first 2 years of the program, a 5-fold increase in antenatal visits and a 4-fold increase in skilled labor delivery across the states were reported.6 Another study reported that mobile clinic services in Katsina state, North-west Nigeria, resulted in consumer satisfaction and significant improvement in health-care services in some parts of the state.8 However, the authors noted that the performance of the health workers was a likely source of variance, and thus regular monitoring of the program through supportive supervision (SS) was recommended.
Supportive supervision is a practical approach to improving health-care delivery globally. When appropriately applied, SS can effectively build the capacity of human resources for health (HRH), improve the quality of care provided by HRH, and effect positive clinical outcomes. However, the extent to which SS improves clinical outcomes in Africa is still unclear.10 Katsina state in North-western Nigeria established integrated supportive supervision (ISS) employed by the state’s ministry of health aimed at improving the quality of health-care delivery within the state’s PHC centers. This study aimed to identify the impact of ISS on the quality of PHC delivery at the community level in Katsina state. The outcome can be used to improve the quality of SS and evidence-based health-care practices in Katsina state and Nigeria.
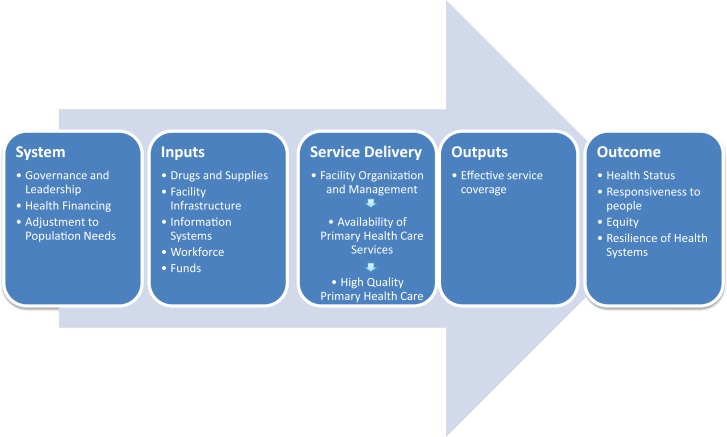
The study was guided by the Primary Health Care Performance Initiative (PHCPI) Conceptual Framework used for improving health systems in developing countries. The framework was developed to identify those components that are vital for attaining an effective PHC system performance. The concept of PHCPI Framework is that the structures of health systems operate through socioeconomic, political, and cultural elements.11 It describes the vital indicators to measure and provides us with the required data to drive improvements. As depicted in Figure 1, the components of the framework include key system-level characteristics, inputs, service delivery processes, outputs, and outcomes of an effective PHC system. This study measured ISS impact on selected Katsina state, Nigeria, health service outputs and outcomes: infrastructure, basic equipment, HRH, essential drugs, the number of pregnant women screened for HIV, and the number of children receiving immunization.
Figure 1.
Framework of the relationship between the components of the primary health-care performance initiative.
Methods
Data Collection
The study was a cross-sectional survey of ISS data collected from July 2018 to December 2018. Concerning the ISS checklist, the study sampling frame consisted of health services quality indicators in 34 comprehensive health facilities, one from each local government area (district) in the state. Details on specific quality indicators (as variables) were obtained and expressed as percentages and processed using the SPSS version 24 software.
Data Analysis
The mean values for the indicators obtained for each visit across all the health facilities involved were calculated and expressed as mean ± standard deviation. Parametric assumptions for using the analysis of variance (ANOVA) test were considered before the analysis. The assumptions were normal distribution of the dependent variable, the dependent variable should have equal variances on scores across the groups, and the dependent variable should be measured on the ratio scale. The 2 variables that met the parametric assumption were the number of pregnant women screened for HIV and the number of children receiving routine immunization. Thus, ANOVA followed by Tukey post hoc test was used to determine the effect of the 6 ISS visits on both variables in the 34 health facilities. Although the Kruskal-Wallis H nonparametric test followed by Dunn post hoc was used to determine the effect of the 6 ISS visits in the 34 health facilities, the assumption of normality was violated, and the dependent variable was measured on the nominal scale. The variables that met the nonparametric assumption include the availability of infrastructure, basic equipment, HRH, and essential drugs.
Results
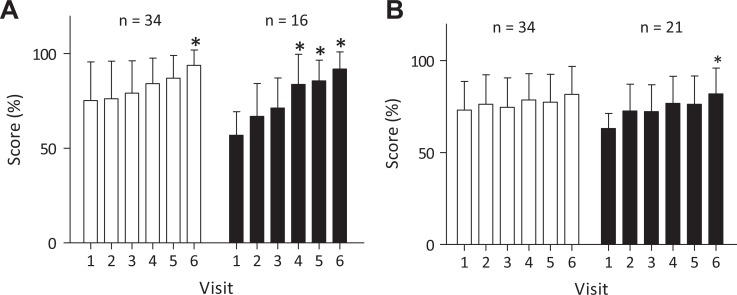
The summary of findings on the impact of ISS visits to the 34 health-care facilities is depicted in Table 1. Figure 2A shows that the average availability of infrastructure in the health facilities at the first ISS visit was 75.29% ± 20.34% (95% confidence interval [95% CI]: 68.20%-82.39%). The average score for infrastructure increased steadily between the first visit and the sixth visit, and the increase was significant at the sixth visit (P < .05). The health facilities found with mean scores of ≤70% for the availability of infrastructure (n = 16) at first visit were also measured separately. As shown in Figure 2A, the average score for infrastructure in this category significantly increased from the fourth visit onward (P < .05). Figure 2B shows that the average availability for HRH among the health facilities (n = 34) at the first visit was 73.15% ± 15.60% (95% CI: 67.70%-78.59%), and this value increased across the ISS visits, although the increase was insignificant (P > .05). The health facilities found with mean scores of ≤70% for HRH (n = 21) were also measured separately. As shown in Figure 2B, the mean score for HRH in this category significantly increased between the sixth and first visits (P < .05).
Table 1.
Summary of Findings on the Impact of ISS Visits to 34 Health-Care Facilities in Katsina State.
| Indicator | Sample Size | Scores (%) | |||||
|---|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | Visit 6 | ||
| Infrastructurea | n = 34 | 75.29 ± 20.34 | 76.18 ± 19.85 | 79.12 ± 17.12 | 84.12 ± 13.51 | 87.06 ± 11.94 | 93.82 ± 8.17* |
| n = 16b | 56.88 ± 12.50 | 66.88 ± 17.40 | 71.25 ± 15.86 | 83.75 ± 15.86* | 85.63 ± 10.94* | 91.88 ± 9.12* | |
| HRHa | n = 34 | 73.15 ± 15.60 | 76.26 ± 16.06 | 74.62 ± 16.03 | 78.56 ± 14.30 | 77.41 ± 15.21 | 81.62 ± 15.19 |
| n = 21b | 63.05 ± 8.22 | 72.67 ± 14.59 | 72.29 ± 14.62 | 76.76 ± 14.74 | 76.29 ± 15.39 | 81.95 ± 13.95* | |
| Basic equipmenta | n = 34 | 94.18 ± 09.18 | 92.94 ± 10.94 | 95.44 ± 06.97 | 98.15 ± 04.33 | 96.06 ± 06.61 | 97.12 ± 06.24 |
| Essential drugsa | n = 34 | 77.21 ± 18.43 | 83.38 ± 14.07 | 83.38 ± 16.95 | 87.50 ± 15.29 | 87.65 ± 12.69 | 90.15 ± 11.71* |
| n = 13b | 58.46 ± 14.05 | 79.62 ± 16.52* | 75.38 ± 22.22 | 82.31 ± 18.78* | 82.31 ± 14.23* | 86.54 ± 12.31* | |
| HIV screeningc | n = 34 | 84.91 ± 26.39 | 91.82 ± 21.12 | 87.35 ± 24.57 | 94.76 ± 16.05 | 92.71 ± 15.89 | 97.06 ± 11.17 |
| n = 8b | 42.88 ± 22.47 | 92.75 ± 24.22* | 92.00 ± 25.18* | 88.13 ± 22.84* | 90.88 ± 17.98* | 99.75 ± 00.71* | |
| Routine immunizationc | n = 34 | 97.65 ± 53.06 | 92.18 ± 49.66 | 100.50 ± 53.74 | 116.60 ± 78.16 | 114.90 ± 75.14 | 117.20 ± 76.76 |
Abbreviations: ANOVA, analysis of variance; HRH, human resources for health; ISS, integrated supportive supervision.
aValues marked with an asterisk (*) along rows are significantly different compared with visit 1 (P < .05). The level of significance in mean difference was determined using the Kruskal-Wallis test followed by Dunn post hoc test.
bNumber of facilities with scores of ≤70% after the first visit.
cValues marked with an asterisk (*) along rows are significantly different compared with visit 1 (P < .05). The level of significance in mean difference was determined using ANOVA followed by Tukey post hoc test.
Figure 2.
Effect of ISS on infrastructure and HRH. Mean scores for all facilities are represented by empty bars, while mean scores for the facilities with scores of ≤70% at the first visit are represented by black bars. Values on the bars with an asterisk (*) are significantly different (P < .05) compared with visit 1. Significance was determined using Kruskal-Wallis test followed by Dunn post hoc test. ISS indicates integrated supportive supervision; HRH, human resources for health.
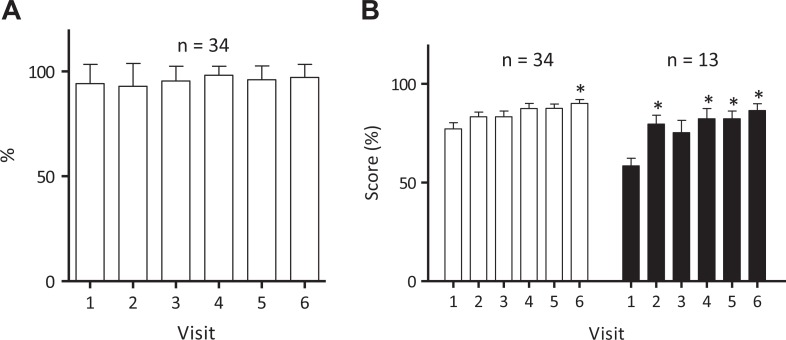
Figure 3A depicts a high average availability of basic equipment (n = 34) among the health facilities at the first visit (94.18% ± 09.18%; 95% CI: 90.97%-98.38%). There was no statistically significant difference in the availability of basic equipment among the health facilities across the 6 ISS visits (P > .05). In Figure 2B, the findings showed a steady increase in the availability of essential drugs among the health facilities from an average of 77.21% ± 18.43% (95% CI: 70.78%-83.64%) at the first ISS visit. However, there was only a statistically significant difference in the availability of basic equipment between the sixth visit compared with the first visit (P > .05). Figure 3B shows a statistically significant increase in the availability of essential drugs, starting from visit 2 (P < .05), among 13 health facilities found with less than 70% availability of essential drugs at the first visit.
Figure 3.
Effect of ISS on the availability of (A) basic equipment and (B) essential drugs. Mean scores for all facilities are represented by empty bars, while mean scores for the facilities with scores of ≤70% at the first visit are represented by black bars. Values on the bars with an asterisk (*) are significantly different (P < .05) compared with visit 1. Significance was determined using Kruskal-Wallis test followed by Dunn post hoc test. ISS indicates integrated supportive supervision.
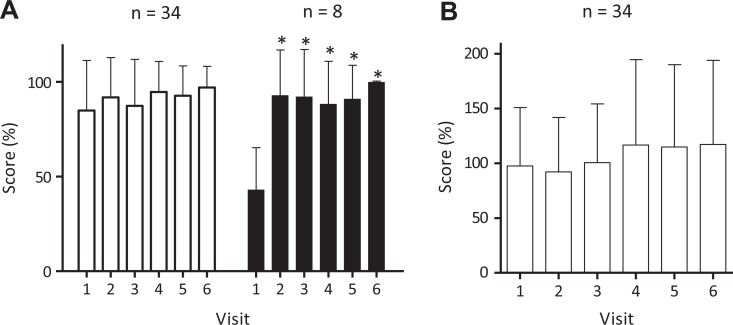
Figure 4A depicts the change in the average proportion of pregnant women screened for HIV among the health facilities (n = 34) at the first visit (84.91% ± 26.39%; 95% CI: 75.70%-94.12%) compared with other visits. The health facilities found with mean scores of ≤70% for pregnant women screened for HIV (n = 8) at the first visit were measured separately. The mean score for pregnant women screened for HIV increased significantly from the second visit (P < .05). Figure 4B shows the change in the mean routine immunization coverage among the health facilities (n = 34) at the first visit. The mean coverage at first visit was 97.65% ± 53.06% (95% CI: 79.13%-116.20%), which was not statistically significantly different from the mean routine immunization coverage of the remaining ISS visits (P > .05).
Figure 4.
Effect of ISS on (A) HIV screening of pregnant women and (B) immunization coverage. Mean scores for all facilities are represented by empty bars, while mean scores for the facilities with scores of ≤70% at the first visit are represented by black bars. The data were analyzed using ANOVA, followed by Tukey post hoc test. ANOVA indicates analysis of variance; ISS, integrated supportive supervision.
Discussion
The WHO defines SS as “a process of helping staff to improve their work performance continuously.”12 Supportive supervision is a polite way of building the capacity of health staff. It is not a fault-finding mission, rather facilitates problem-solving. Supportive supervision depends upon regular supervisory visits to health facilities to build relationships, monitor staff performance, record observations, and provide constructive feedback.12 There are reports in other parts of Africa on the positive effects of SS on clinical quality, measured by knowledge level of staff, adherence to clinical protocols, and improved record-keeping.13,14 Furthermore, SS improved worker efficiency in terms of attendance and availability of services as well as increased job satisfaction among workers.10,15 These studies employed different models to derive the conclusion. The present study reported the impact of SS of some facets of PHC service delivery. The study shows the positive effect of the ISS on HRH and basic infrastructure. The components of the infrastructure measured were sanitation, medical waste management, communication equipment, and lighting in the health facilities. The findings are similar to that of study by Adetiloye in 2017, who found a significant increase in family planning infrastructure after 2 supervisory visits in 20 health facilities from states in Nigeria.16 However, Mboya et al (2016) found a mixed outcome for the availability of infrastructure within 12 months of SS.17 The results showed a 4% to 11% increase in health facility infrastructure in some health facilities from 3 districts. Moreover, there was a decline in infrastructure in some health facilities from 2 other districts, while no difference in infrastructure was observed in health facilities from 1 district.
Regarding the availability of HRH, the study measured the retention rate of health personnel from initial visit to end the visit. The findings showed no significant increase in the number of health workers in the health facilities. The ISS approach is intended to enhance effective interpersonal relationships between the supervisors and HRH. Negative relationships tend to undermine the confidence of health workers, which may increase the attrition rate. A study conducted in Uganda by Ludwick and colleagues, in 2018, found that constructive relationships between supervisors and community health workers were essential for staff retention.18 No significant impact of ISS was observed on the availability of basic equipment in the study. The components of basic equipment measured include clinician’s stethoscope, blood pressure cuff, and thermometer, fetoscope, weighing scales for adults and children, sterile chord cutter, latex hand gloves, examination table, delivery bed, Rapid Diagnostic Test kit, Test kit for HIV, and vaccine carrier. During ISS visits, the supervisors are expected to continually supply the health workers with the basic equipment to complete their tasks. The ISS visits link the PHC services with the state ministry of health, which provides an opportunity to collect an inventory of the basic in the health facilities inventories. In 2017, Moyimane et al found that lack of monitoring and supervision were responsible for the substantial lack of basic medical equipment in a rural health center in South Africa.19
The study measured the effect of the ISS on the availability of essential drugs. According to the WHO, essential drugs are medicines that “satisfy the priority health care needs of the population.”20 The essential drugs measured for this study were selected from the Primary Health Centre Essential Drug List for Health Clinics in Nigeria.21 Findings from second visits indicated a positive impact of ISS on the availability of essential drugs. These findings are in contrast with the results obtained by Oyekale in 2017, who found low availability of some essential drugs like azithromycin, nifedipine, dexamethasone, and misoprostol in 12 PHCs across Nigeria.22 In Tanzania, Kapologwe and colleagues found an initial stockout of artemether–lumefantrine, amoxicillin syrup, and amoxicillin capsules using standardized auditing tools for SS.23 In their study, the authors provided practical evidence of the relevance of the ISS approach to preventing stockout of essential drugs among PHCs in Tanzania. The study measured the mean score for pregnant women screened for HIV, and the findings showed a significant increase from the second visit. The positive effect is because the ISS approach provided an excellent opportunity for the supervisors to build the capacity of the health workers on providing effective counseling services to pregnant women. Matseke et al, 2016, found a direct relationship between client compliance with HIV testing and satisfaction with HIV counselling and testing (HCT).24 Another vital factor for the positive effect was the role of the ISS visits on the availability of rapid test devices for HIV in the PHCs. The availability of HIV testing devices in the PHCs will facilitate the utilization of HCT and services by pregnant women. Finally, the study showed no significant improvement in coverage of routine immunization throughout the ISS visits. The reasons were because the mean coverage at first visit was already high at 97.65%. Moreover, probably, the focus of intervention likely to improve the immunization coverage is on the caregivers, not on service providers.
Limitations
Data collection for the study was conducted 6 months following the introduction of the ISS by the State Ministry of Health. The period may not have been sufficient enough to measure the impact of the intervention. The second limitation relates to sampling bias. Sample selection bias may have occurred due to the nonrandom selection of the health facilities. The sample frame comprised of only 34 comprehensive health centers where the ISS was applied, causing other primary health centers to be less likely to be included in the study. The third limitation relates to the novelty effect, which was probably responsible for the positive results obtained within 6 months of application of the ISS. There was a tendency that the staff supervised in the selected health facilities boosted their performances in response to increased interest in the new ISS approach.
Recommendations
Evidence from this study shows that the ISS approach provided better outcomes for health-care delivery in PHC in Katsina, Nigeria. Hence, the state government should extend the ISS to secondary and tertiary health centers in order to identify gaps and improve the efficacy of HRH in the state. The ISS creates a chance for building better professional relationships among all cadres of health workers in the state. The study depicted the positive effects of ISS on the availability of basic equipment in health centers. Promoting the ISS approach will secure the sustainability, efficient utilization, and durability of hospital equipment in the state. It is also apparent that the integrated supervision intervention will positively affect the quality and availability of essential drugs in the health facilities.
Production and sale of counterfeit drugs remain a significant public health concern in Nigeria.25 Quality ISS will reduce the menace and ensure that health workers in the health facilities give patients safe medicines. By utilizing the ISS approach, HCT centers in Katsina state will benefit from improved client satisfaction, sustainable supply of rapid HIV test kits, and reduction of missed opportunities for HIV screening. Contemporary literature on ISS lacks the data on morbidity and mortality. According to Bradley and colleagues, most studies on the effect of SS on the quality of health care in Africa measured “surrogate outcomes” such as interventions rather than “end outcomes” like morbidity and mortality.10 Thus, future research on ISS should focus on identifying the impact of ISS on outcome health indicators, especially of maternal and neonatal mortality. Conclusive inferences drawn from the study can be used to improve the health status of Katsina state, Nigeria.
Conclusion
Integrated supportive supervision need to be embedded into the 3 levels (primary, secondary, and tertiary) of Katsina state health-care service delivery. Sustainability of the intervention will ensure efficient use of the health facility assets and resources utilization and improve patient/client satisfaction.
Acknowledgments
The authors acknowledge, with gratitude, approval on the use of data from Katsina State Ministry of Health for the sole purpose of this study.
Author Biographies
Shafique Sani Nass is a Global Health Physician and an Epidemiologist. He received his PhD in Public Health from Walden University, Minneapolis, Minnesota, USA and a Master of Public Health degree from Usman Danfodio University, Sokoto, Nigeria. He trained as a medical doctor with an MBBS degree from Bayero University, Kano, Nigeria. Dr Nass is a member of the American College of Epidemiology and has vast experience serving as a public health officer with several reputable international organizations. His research interests lie in the area of infectious diseases, child health, and neglected tropical diseases. He currently serves as a monitoring and evaluation officer with the World Health Organization (Immunizations, Vaccines and Emergencies Cluster) in Nigeria. He is happily married with three children.
Murtala Bindawa Isah is a Biochemist with research interest in the area of infectious diseases of poverty and neglected tropical diseases. He received his PhD and MSc degrees in Biochemistry from the University of KwaZulu Natal, South Africa, and BSc Biochemistry from Ahmadu Bello University Zaria. Dr. Isah currently teaches biochemistry at Umaru Musa Yar'adua University. He is a member of Nigerian Society of Biochemistry and Molecular Biology.
Aminu Sani is a Chartered Economist and a Certified Financial Analyst. He is a PhD research student at the Nigerian Defense Academy. He holds a Master of Science Degree in Economics from the Nigerian Defense Academy with a concentration in Health Economics. His research interest lies in the area of Health Economics. He is a member of the Institute of Chartered Economists of Nigeria, Association of Financial Analysts of Nigeria and the Nigerian Institute of Management. He serves at the Research and Statistics Unit of the Department of Health Planning in the State Ministry of Health, Katsina State, Nigeria. He is happily married with a child.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shafique Sani Nass  https://orcid.org/0000-0001-5665-2591
https://orcid.org/0000-0001-5665-2591
References
- 1. Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Millwood). 2010;29(5):766–772. [DOI] [PubMed] [Google Scholar]
- 2. Kruk ME, Porignon D, Rockers PC, Van Lerberghe W. The contribution of primary care to health and health systems in low- and middle-income countries: a critical review of major primary care initiatives. Soc Sci Med. 2010;70(6):904–911. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. The World Health Report 2008: Primary Health Care (now more than ever). Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 4. Kress DH, Su Y, Wang H. Assessment of primary health care system performance in Nigeria: using the primary health care performance indicator conceptual framework. Health Syst Reform. 2018;2(4):302–318. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. Country Coordination and Facilitation Case Studies. 2011. https://www.who.int/workforcealliance/knowledge/resources/ccfresources/en/. Accessed September 08, 2019.
- 6. Doctor HV, Bairagi R, Findley SE, Helleringer S, Dahiru T. Northern Nigeria maternal, newborn, and child health program: selected analyses from the population-based baseline survey. Open Demograph J. 2010;4:11–21. [Google Scholar]
- 7. National Bureau of Statistics (NBS) and the United Nations Children’s Fund (UNICEF). Multiple Indicator Cluster Survey 2016-17, Survey Findings Report. Abuja, Nigeria: National Bureau of Statistics (NBS) and the United Nations Children’s Fund (UNICEF); 2017. [Google Scholar]
- 8. Peters G, Doctor H, Afenyadu G, Findley S, Ager A. Mobile clinic services to serve rural populations in Katsina State, Nigeria: perceptions of services and patterns of utilization. Health Policy Planning. 2013;29(5):642–649. [DOI] [PubMed] [Google Scholar]
- 9. Ariyo O, Ozodiegwu ID, Doctor HV. The influence of the social and cultural environment on maternal mortality in Nigeria: evidence from the 2013 demographic and health survey. PLoS One. 2017;12(12):e0190285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bradley J, Igras S. Improving the quality of child health services: participatory action by providers. International J Qual Health Care. 2005;17(5):391–399. [DOI] [PubMed] [Google Scholar]
- 11. Primary Health Care Performance Initiative. Methodology Note. 2015. https://improvingphc.org/sites/default/files/PHCPI%20Methodology%20Note_0.pdf. Accessed July 04, 2019.
- 12. World Health Organization. Training for mid-level managers (MLM)—WHO/IVB/08.04. 2008. https://www.who.int/immunization/documents/MLM_module4.pdf. Accessed February 09, 2019.
- 13. Bello DA, Hassan ZI, Afolaranmi TO, Tagurum YO, Chirdan OO, Zoakah AI. Supportive supervision: an effective intervention in achieving high-quality malaria case management at primary health care level in Jos, Nigeria. Ann Afri Med. 2013;12(4):243. [DOI] [PubMed] [Google Scholar]
- 14. Green A, de Azevedo V, Patten G, Davies MA, Ibeto M, Cox V. Clinical mentorship of nurse initiated antiretroviral therapy in Khayelitsha, South Africa: a quality of care assessment. PLoS One. 2014;9(6):e98389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Manzi A, Magge H, Hedt-Gauthier BL, et al. Clinical mentorship to improve pediatric quality of care at the health centers in rural Rwanda: a qualitative study of perceptions and acceptability of health care workers. BMC Health Serv Res. 2014;14(1):275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adetiloye O. The use of integrated supportive supervision (ISS) visits to strengthen family planning service delivery in two selected states of Nigeria. Texila Intl J Public Health. 2017;5(4). [Google Scholar]
- 17. Mboya D, Mshana C, Kessy F, et al. Embedding systematic quality assessments in supportive supervision at primary healthcare level: application of an electronic tool to improve quality of healthcare in Tanzania. BMC Health Serv Res. 2016;16:578 doi:10.1186/s12913-016-1809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ludwick T, Turyakira E, Kyomuhangl T, et al. Supportive supervision and constructive relationships with healthcare workers support CHW performance: use of a qualitative framework to evaluate CHW programming in Uganda. Human Res Health. 2018;16:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moyimane M, Matlala SF, Kekana MP, et al. Experiences of nurses on the critical shortage of medical equipment at a rural district hospital in South Africa: a qualitative study. Pan Afri Med J. 2017; 28:100 doi:10.11604/pamj.2017.28.100.11641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. World Health Organization. Essential Medicines Selection. 2019. https://www.who.int/selection_medicines/committees/en/ Accessed August 07, 2019.
- 21. National Primary Health Care Development Agency. Minimum Standards for Primary Health Care in Nigeria. 2017. https://www.medbox.org/countries/minimum-standards-for-primary-health-care-in-nigeria/preview. Accessed August 08, 2019.
- 22. Oyekale AS. Assessment of primary health care facilities’ service readiness in Nigeria. BMC Health Serv Res. 2017;17:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kapologwe N, Mori AT, Chilunda F, Meshack M, Kalolo A, Wiedenmayer K. Reforming supportive supervision of medicines management with an audit tool in primary health care facilities: a case study of Bahi district, Tanzania. Int J Pharm. 2014;4 (4):108–114. [Google Scholar]
- 24. Matseke G, Peltzer K, Mohlabane N. Clients’ perceptions and satisfaction with HIV counselling and testing: a cross-sectional study in 56 HCT sites in South Africa. Afri J Primary Health Care Family Med. 2016;8(1):e1–7. doi:10.4102/phcfm.v8i1.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Akinyandenu O. Counterfeit drugs in Nigeria: a threat to public health. Afri J Pharm Pharmacol. 2013;7(36):2571–2576. doi:10.5897/AJPP12.343. [Google Scholar]