Abstract
Background:
The peroneus longus tendon has been used as a graft in orthopaedic reconstruction surgery because of its comparable biomechanical strength with the native anterior cruciate ligament (ACL) and hamstring tendon. However, one of the considerations in choosing an autograft is donor site morbidity.
Purpose/Hypothesis:
This study aimed to compare ankle eversion and first ray plantarflexion strength between the donor site and its contralateral site after ACL reconstruction. The study hypothesis was that strength measurements will be different between the harvest site and contralateral healthy site.
Study Design:
Case series; Level of evidence, 4.
Methods:
Patients who underwent ACL reconstruction using a peroneus longus tendon autograft between March 2017 and December 2018 were included in this study. Patients followed a rehabilitation protocol from the first day after surgery. Ankle eversion and first ray plantarflexion strength were measured using a modified dynamometer 6 months after surgery. Donor site morbidity was assessed 6 months after surgery using the Foot & Ankle Disability Index (FADI) and American Orthopaedic Foot & Ankle Society (AOFAS) scoring system for the ankle and hindfoot.
Results:
A total of 31 patients (22 male, 9 female; mean age, 27.58 ± 8.69 years [range, 18.00-45.00 years]) fulfilled the inclusion criteria. There was no significant difference in ankle eversion strength at the donor site compared with the contralateral site (P = .55), with means of 65.87 ± 7.63 N and 66.96 ± 8.38 N, respectively. Also, there was no significant difference in ankle first ray plantarflexion strength at the donor site compared with the contralateral site (P = .68), with means of 150.64 ± 11.67 N and 152.10 ± 12.16 N, respectively. The mean FADI score of 99.71 ± 0.57 and mean AOFAS score of 98.71 ± 3.03 at the donor site were considered excellent results.
Conclusion:
Ankle eversion and first ray plantarflexion strength at the donor site were similar to those at the contralateral healthy site, with no donor site morbidity. This suggests that the peroneus longus tendon is a promising graft in ACL reconstruction.
Keywords: Eversion, first ray plantarflexion, peroneus longus, anterior cruciate ligament reconstruction
Anterior cruciate ligament (ACL) reconstruction is indicated often in young, active, and athletic patients. Nowadays, orthopaedic surgeons perform ACL reconstruction using the peroneus longus tendon as an autograft along with the common usage of hamstring tendon or bone–patellar tendon–bone grafts.5,10 The use of the peroneus longus tendon in ACL reconstruction is increasing. Orthopaedic surgeons try to use the peroneus longus tendon in deltoid ligament reconstruction16 and medial patellofemoral ligament reconstruction17 because there is a synergistic function between the peroneus longus and peroneus brevis muscles,12 which can offer some advantage if both undergo tenodesis.
A previous study has stated that there was no difference in tensile strength between the peroneus longus tendon and hamstring tendon.14 Rhatomy et al13 reported that the peroneus longus tendon can be a superior graft to the hamstring tendon in ACL reconstruction. There has been no study about donor site morbidity or particularly on eversion and first ray plantarflexion muscle strength in ACL reconstruction using the peroneus longus tendon. This study aimed to compare eversion and first ray plantarflexion muscle strength after peroneus longus tendon harvest in ACL reconstruction.
Methods
This was a retrospective cohort study with consecutive sampling of patients who underwent ACL reconstruction from March 2017 to December 2018. Patients’ medical history, physical examination results, and magnetic resonance imaging (MRI) findings were used to diagnose ACL ruptures. The inclusion criteria were patients with isolated ACL ruptures and those aged 18 to 45 years. The exclusion criteria were associated ligament injuries, chondral damage, meniscal injuries, fractures around the knee, and pathological conditions in the lower extremity or abnormal contralateral knee joints. This study was reviewed and approved by a medical and health research ethics committee.
A total of 31 patients gave informed consent to be included in this study and underwent single-bundle ACL reconstruction using a peroneus longus tendon graft. We recorded ankle functional scores (American Orthopaedic Foot & Ankle Society [AOFAS] scoring system and Foot & Ankle Disability Index [FADI]) and evaluated muscle strength using a Baseline analog hydraulic push-pull dynamometer (12-0392; Fabrication Enterprises) 6 months after surgery was performed (Figure 1). The outcomes of the muscle strength measurement between the 2 groups were compared using the Wilcoxon test with SPSS version 25.0 (IBM). Statistical significance was set at P < .05.
Figure 1.

Baseline analog hydraulic push-pull dynamometer.
A single experienced knee surgeon operated on all patients. Standard anterolateral and anteromedial portals were made. Diagnostic arthroscopic surgery for ACL ruptures was performed. Peroneus longus tendon harvest was conducted in the ipsilateral leg. The incision location was marked at 2 to 3 cm above and 1 cm behind the lateral malleolus, and the incision was made through the skin, subcutaneous tissue, and superficial fascia. The peroneus longus and peroneus brevis tendons were identified. The location of tendon division was marked at 2 to 3 cm above the level of the lateral malleolus. The distal part of the peroneus longus tendon was sutured with end-to-side suture after tenodesis was performed between the peroneus longus and peroneus brevis tendons. The peroneus longus tendon was stripped proximally using a tendon stripper until ±4 to 5 cm below the fibular head to avoid peroneal nerve injuries.
The intercondylar notch was cleared of fibrous tissue to facilitate good visualization during the preparation of the tunnels. ACL fibers were preserved as a reference for graft insertion. The femoral and tibial tunnels were drilled independently. The graft was implanted and tensioned using a graft tensioner to prevent loosening in the future. Graft fixation involved buttons (XO Button; Conmed) on the femoral side and bioabsorbable screws (BioScrew; Conmed) on the tibial side.
Rehabilitation
Postoperatively, patients underwent an ACL rehabilitation program. Patients were trained to exercise the injury site leg using partial weightbearing until 3 weeks after surgery, after which they were allowed to use full weightbearing. Knee extension was begun immediately after surgery. Knee flexion was started from 0° to 90° (increased gradually) until 3 weeks after surgery with subsequent full flexion. The patient was allowed to jog after 2 months. Patients were allowed to return to sport activity after passing functional outcome tests at 6 months. The tests consisted of the evaluation of knee stability based on the anterior drawer test, Lachman test, and serial hop test.
Isokinetic Muscle Strength Test of Ankle
The results of muscle strength tests were collected at 6 months after surgery. A Baseline analog hydraulic push-pull dynamometer was used on patients to measure isometric muscle strength. Examinations were conducted of bilateral angle eversion and first ray plantarflexion. Each muscle strength measurement was performed 3 times, and the highest strength was recorded. All muscle strength measurements were conducted by the same operator to avoid any study bias.
Eversion was measured in the contralateral decubitus position. Both medial malleoli were kissed. Patients were asked to make eversion movements of the ankle. The dynamometer was placed on the fifth metatarsal. The crural region of patients was gently pressed to minimize the movement of other muscles, and muscle strength was recorded from the dynamometer (Figure 2).
Figure 2.
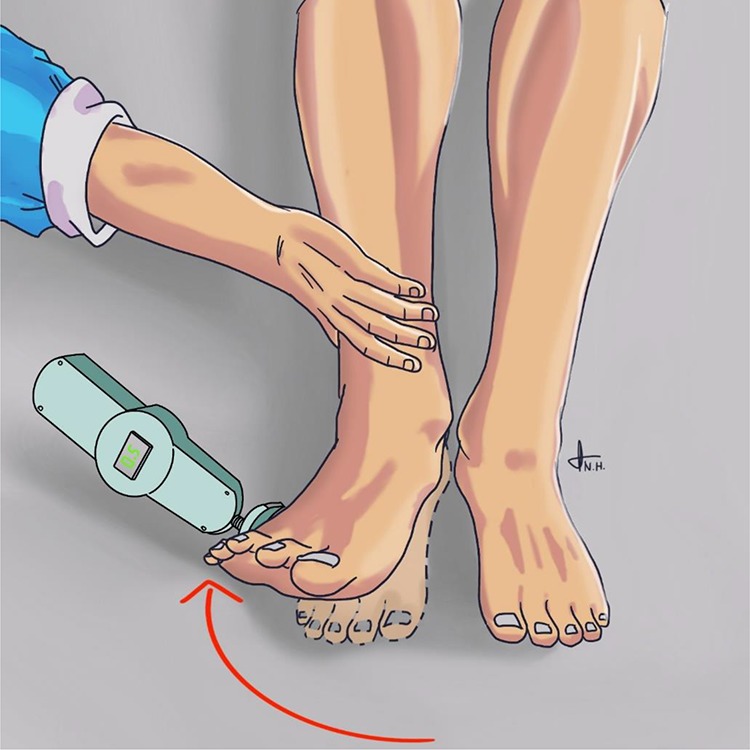
Eversion strength measurement.
First ray plantarflexion was measured in the prone position. The ipsilateral knee joint was flexed 90°. The ipsilateral distal part of the crural region was maintained using the hands of the examiner’s assistant to minimize the movement of other muscles. Patients were asked to make first ray plantarflexion movements. The dynamometer was placed on the first to fifth distal metatarsals, and muscle strength was recorded from the dynamometer (Figure 3).
Figure 3.
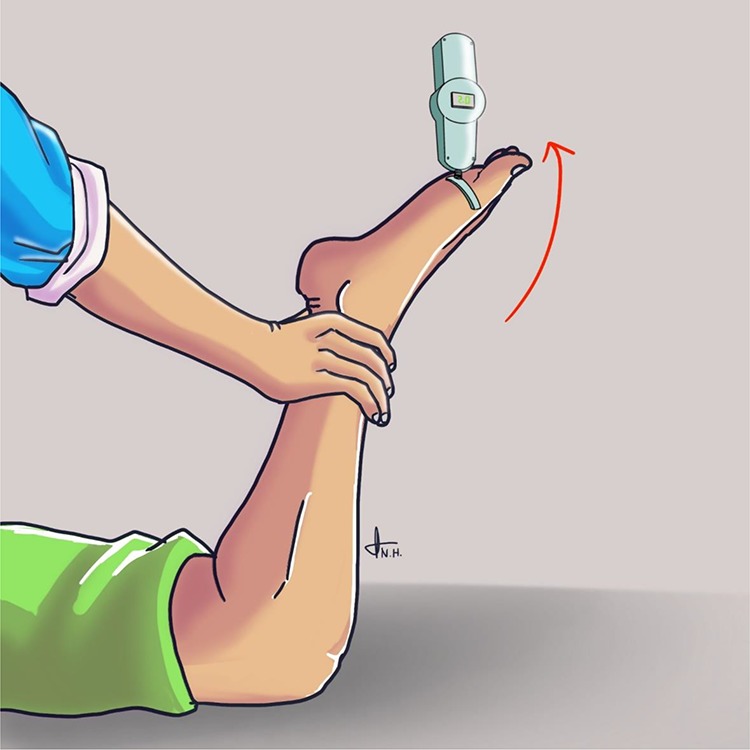
First ray plantarflexion strength measurement.
Results
Of the 31 patients who underwent single-bundle ACL reconstruction using a peroneus longus tendon autograft, 22 patients were male and 9 were female. The mean age of the patients was 27.58 ± 8.69 years (range, 18.00-45.00 years). The right knee was injured in 19 patients and the left knee in 12 patients. The injury mechanism was sports in 19 patients, traffic accident in 7 patients, and other causes in 5 patients. The diameter of the peroneus longus tendon graft was measured and recorded intraoperatively; the mean diameter was 8.74 ± 0.56 mm (range, 8.00-10.00 mm) (Table 1). No translation was seen on the Lachman test for any patient at 6 months after surgery.
Table 1.
Patient Characteristicsa
| Age, mean ± SD (range), y | 27.58 ± 8.69 (18.00-45.00) |
| Sex | |
| Male | 22 (70.9) |
| Female | 9 (29.1) |
| Site of injury | |
| Right | 19 (61.3) |
| Left | 12 (38.7) |
| Injury mechanism | |
| Sport | 19 (61.3) |
| Traffic accident | 7 (22.6) |
| Other | 5 (16.1) |
| Graft diameter, mean ± SD (range), mm | 8.74 ± 0.56 (8.00-10.00) |
aData are presented as n (%) unless otherwise specified.
Mean eversion strength was 65.87 ± 7.63 N at the donor site and 66.96 ± 8.38 N at the contralateral healthy site. There was no significant difference in eversion strength between the donor site and contralateral healthy site (P = .55). Mean first ray plantarflexion strength was 150.64 ± 11.67 N at the donor site and 152.10 ± 12.16 N at the contralateral healthy site. There was no significant difference in first ray plantarflexion strength between the donor site and contralateral healthy site (P = .68) (Table 2).
Table 2.
Ankle Eversion and First Ray Plantarflexion Strength
| Strength, N | Donor Site | Contralateral Site | P Value | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Range | Normality | Mean ± SD | Range | ||
| Eversion | 65.87 ± 7.63 | 55.00-80.00 | 0.002 | 66.96 ± 8.38 | 55.00-85.00 | .546 |
| First ray plantarflexion | 150.64 ± 11.67 | 110.0-170.0 | 0.005 | 152.12 ± 12.16 | 110.00-170.00 | .680 |
The mean FADI score was 99.71 ± 0.57 at the donor site and 99.71 ± 0.61 at the contralateral healthy site. There was no significant difference in the FADI score between the donor and contralateral healthy sites (P = .83). The mean AOFAS score was 98.71 ± 3.03 at the donor site and 99.03 ± 3.00 at the contralateral healthy site. There was no significant difference in the AOFAS score between the donor and contralateral healthy sites (P = .22) (Table 3).
Table 3.
FADI and AOFAS Scoresa
| Score | Donor Site | Contralateral Site | P Value | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Range | Normality | Mean ± SD | Range | ||
| FADI | 99.71 ± 0.57 | 98.10-100.00 | 0.000 | 99.71 ± 0.61 | 98.10-100.00 | .827 |
| AOFAS | 98.71 ± 3.03 | 90.00-100.00 | 0.000 | 99.03 ± 3.00 | 90.00-100.00 | .218 |
aAOFAS, American Orthopaedic Foot & Ankle Society; FADI, Foot & Ankle Disability Index.
Discussion
The grafts of choice in ACL reconstruction have been the hamstring tendon and bone–patellar tendon–bone, and the newest one is the peroneus longus tendon.1,13 A previous study showed that there were better functional outcomes in ACL reconstruction using the peroneus longus tendon compared with the hamstring tendon.13 Normal ACL strength is 1725 ± 269 N.3 Peroneus longus tendon strength was described as 1950 N by Kerimoǧlu et al.8 They showed that there was similar strength between the native ACL and peroneus longus tendon. Rudy et al14 reported that tensile strength of the peroneus longus tendon was 446.16 ± 233.28 N. Kerimoǧlu et al9 published an MRI study of the various regeneration stages of the peroneus longus tendon after ACL reconstruction.
The use of the peroneus longus tendon in ACL reconstruction is controversial because of donor site morbidity. A previous study investigated ankle functional outcomes using FADI and AOFAS scores.13 The results were excellent using the peroneus longus tendon.13 In this study, the FADI and AOFAS scores were also excellent. The FADI and AOFAS scores were similar to the results of Angthong et al.1
The peroneus longus tendon has an important function for the ankle and foot.4,6,11 Its main role is to strengthen first ray plantarflexion and to evert the foot.15 There is some concern about the deterioration of ankle eversion and first ray plantarflexion strength after peroneus longus tendon harvest. Shi et al15 showed that there were no differences between preoperative and postoperative ankle strength and range of motion. Harvest of the peroneus longus tendon did not affect ankle function.8
For stability, the peroneus longus tendon works in combination with the peroneus brevis tendon to distribute pressure on the forefoot.4 Karanikas et al7 found no difference in isokinetic strength for first ray plantarflexion of the donor versus contralateral ankle between 3 and 6 months or 6 and 12 months after ACL reconstruction. Zhao and Huangfu18 reported that there were no ankle or foot injuries experienced by patients after peroneus longus tendon harvest. In this study, there were no differences in eversion and first ray plantarflexion muscle strength between the donor site and contralateral healthy site. The peroneus longus tendon has a synergistic mechanism with the peroneus brevis tendon.12 The same force levels on the peroneus longus and peroneus brevis tendons showed equal strength.12 This study indicated that there was no difference if the peroneus longus tendon was harvested. We used the tenodesis technique between the peroneus longus and peroneus brevis tendons before the peroneus longus tendon was stripped. The examination of eversion and first ray plantarflexion was conducted 6 months after surgery to accommodate regeneration and muscle mass escalation during the rehabilitation program. The peroneus longus tendon is a suitable graft with comparable strength, safety, and donor site morbidity.2
The limitations of this study are the small number of participants, short time for follow-up, and no comparison between preoperative and postoperative results. This study also lacked isokinetic muscle testing and did not provide calf circumference.
Conclusion
ACL reconstruction using a peroneus longus tendon autograft revealed no muscle strength deterioration during eversion and first ray plantarflexion of the ankle joint. There was no donor site morbidity at the harvest site, and the donor site had excellent FADI and AOFAS scores.
Acknowledgment
The authors thank Rini Maya Puspita, MD, for his assistance in journal reference selection.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the medical and health research ethics committee of Gadjah Mada University (No. KE/FK/0064/EC/2019).
References
- 1. Angthong C, Chernchujit B, Apivatgaroon A, Chaijenkit K, Nualon P, Suchao-In K. The anterior cruciate ligament reconstruction with the peroneus longus tendon: a biomechanical and clinical evaluation of the donor ankle morbidity. J Med Assoc Thai. 2015;98(6):555–560. [PubMed] [Google Scholar]
- 2. Barzegar M, Hosseini A, Karimi M, Nazem K. Can we use peroneus longus in addition to hamstring tendons for anterior cruciate ligament reconstruction? Adv Biomed Res. 2014;3(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Caplan N, Kader DF. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. In: Banaszkiewicz PA, Kader DF, eds. Classic Papers in Orthopaedics. London: Springer-Verlag; 2014:145–147. [Google Scholar]
- 4. Ferris L, Sharkey NA, Smith TS, Matthews DK. Influence of extrinsic plantar flexors on forefoot loading during heel rise. Foot Ankle Int. 1995;16(8):464–473. [DOI] [PubMed] [Google Scholar]
- 5. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11. [DOI] [PubMed] [Google Scholar]
- 6. Jacob HAC. Forces acting in the forefoot during normal gait: an estimate. Clin Biomech (Bristol, Avon). 2001;16(9):783–792. [DOI] [PubMed] [Google Scholar]
- 7. Karanikas K, Arampatzis A, Bruggemann G-P. Motor task and muscle strength followed different adaptation patterns after anterior cruciate ligament reconstruction. Eur J Phys Rehabil Med. 2009;45:37–45. [PubMed] [Google Scholar]
- 8. Kerimoǧlu S, Aynaci O, Saracoǧlu M, Aydin H, Turhan AU. Anterior cruciate ligament reconstruction with the peroneus longus tendon. Acta Orthop Traumatol Turc. 2008;42(1):38–43. [DOI] [PubMed] [Google Scholar]
- 9. Kerimoǧlu S, Koşucu P, Livaoǧlu M, Yükünç I, Turhan AU. Magnetic resonance imagination of the peroneus longus tendon after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17(1):35–39. [DOI] [PubMed] [Google Scholar]
- 10. Mohtadi N, Chan D, Dainty K, Whelan D. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;9:CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. O’Connor KM, Hamill J. The role of selected extrinsic foot muscles during running. Clin Biomech (Bristol, Avon). 2004;19(1):71–77. [DOI] [PubMed] [Google Scholar]
- 12. Otis JC, Deland JT, Lee S, Gordon J. Peroneus brevis is a more effective evertor than peroneus longus. Foot Ankle Int. 2004;25(4):242–246. [DOI] [PubMed] [Google Scholar]
- 13. Rhatomy S, Asikin AIZ, Wardani AE, Rukmoyo T, Lumban-Gaol I, Budhiparama NC. Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction [published online March 15, 2019]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-019-05455-w [DOI] [PubMed] [Google Scholar]
- 14. Rudy, Mustamsir E, Yuarno K. Tensile strength comparison between peroneus longus and hamstring tendons: a biomechanical study. International Journal of Surgery Open. 2017;9:41–44. [Google Scholar]
- 15. Shi F-D, Hess DE, Zuo J-Z, et al. Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J Knee Surg. 2019;32(8):804–811. [DOI] [PubMed] [Google Scholar]
- 16. Wagshul AD, Williams BR, Ellis SJ, Pavlov H, Deland JT. Deltoid ligament reconstruction with peroneus longus autograft in flatfoot deformity. Foot Ankle Int. 2010;31(9):781–789. [DOI] [PubMed] [Google Scholar]
- 17. Xu C, Zhao J, Xie G. Medial patella-femoral ligament reconstruction using the anterior half of the peroneus longus tendon as a combined procedure for recurrent patellar instability. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2016;4:21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhao J, Huangfu X. The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med. 2012;40(3):662–671. [DOI] [PubMed] [Google Scholar]


