Abstract
Introduction:
Lithium “the magic pill” past its discovery remained the respite for patients with bipolar disorders for decades. The prescriptions of lithium were replaced by other drugs because of the cumbersome monitoring, adverse effect profile, narrow therapeutic index, and frequent comorbidities in patients. The objectives of this study were to understand the knowledge, attitude, and practice of lithium by a subset of psychiatrists in India, which will help us understand the theory–practice gap and for devising strategies to bridge the existing gap.
Materials and Methods:
The current study was an online survey which included 103 psychiatrists from India of either gender and any age group. Predesigned questionnaire about the knowledge, attitude, and practice of lithium use was circulated for 1 month (March 2018). We received 135 responses (31% response rate), of which 32 were incomplete. Hence, the total sample of psychiatrists included in the study was 103.
Results:
The results suggest that most practitioners included in the survey had knowledge about the effects, adverse effects, and the monitoring protocols and were comfortable in using lithium in patients on outpatient basis. Despite being aware of the indications, the psychiatrists were skeptical in starting lithium due to multitude of perceived barriers such as comorbidities, patient's low adherence to blood monitoring, and adverse effects.
Conclusions:
Clinicians should be well aware of the adverse effects, monitoring protocols, which will help them to use lithium in a more appropriate manner.
Key words: Attitude, knowledge, lithium, practice, psychiatrists
INTRODUCTION
Lithium remained the gold standard treatment for patients with bipolar disorders for several decades. During the past six-seven decades, the efficacy and tolerability of lithium in bipolar disorders have been established strongly. It is considered as a first-line drug in acute phases of both mania and depression by the current clinical practice guidelines. Lithium remains the only medication that has been approved by the Food and Drug Administration for maintenance treatment of bipolar disorder. The same was confirmed by the Cochrane collaborative and meta-analyses simultaneously finding equivocal evidence for divalproex and valproic acid as maintenance treatments.[1,2,3]
Slowly but steadily, the prescriptions of lithium were replaced by the recent psychotropics. This was mainly because of the cumbersome monitoring, adverse effect profile, narrow therapeutic index, and frequent comorbidities in patients, making lithium a second choice drug.[4,5] Despite psychiatrists being aware of the beneficial effects and monitoring protocols, the place of lithium in their original practice has always been behind. Some studies were done on patients receiving lithium therapy in which they assessed the knowledge and attitude toward treatment using lithium knowledge test. They were done mainly in elderly patients with bipolar disorder.[6,7] However, the focus on this area had been declining in the recent past and has been shifting toward the understanding of molecular mechanisms of its action and neurotrophic properties.[8,9] We could not find studies which assessed the knowledge and attitude of psychiatrists toward lithium therapy.
Studies done from India focused on assessing the adverse effects and safety/tolerability profile of lithium,[10,11,12,13,14,15] and most of the data are in the form of case reports.[16,17,18] The issue of pattern of lithium prescription from India is underexplored till now. Hence, we decided to understand the knowledge, attitude, and practice of lithium by a subset of psychiatrists in India, which will help us understand the theory–practice gap and for devising strategies to bridge the existing gap.
MATERIALS AND METHODS
The current study was an online survey which included psychiatrists from India (post-MD/DNB) of either gender and any age group. For the purpose of the study, we have designed a set of 25 questions which had either multiple choice answers or multiple options and some questions based on Likert scale. These questions mainly assessed about the knowledge, attitude, and practice of lithium use among psychiatrists apart from sociodemographic details. This predesigned questionnaire was circulated among the contacts of investigators through E-mail, WhatsApp, Facebook, and other messenger systems. It was done over a period of 1 month (March 2018), and the principal investigators belonged to department of psychiatry, AIIMS Raipur. Only one reminder was sent to all the contacts those who were circulated the survey and anonymity was maintained. Survey was circulated to 424 contacts overall. Respondents could fill the survey through the predesigned questionnaire only once. Among them, we received 135 responses (31% response rate), of which 32 were incomplete. Hence, the total sample of psychiatrists included in the study was 103.
RESULTS OF THE STUDY
Sociodemographic distribution
As shown in Table 1, the sample which included 103 psychiatrists from India is male predominant, with mean age and duration of experience being 39 years and 12.5 years, respectively. Most of them worked in urban area and more or less equally distributed among institution based, private setup, and both the sectors.
Table 1.
Sociodemographic distribution
| Variable | Frequency (%)/mean (SD) |
|---|---|
| Age (years) | 39.7 (10.8) |
| Gender | |
| Male | 86 (83.5) |
| Female | 17 (16.5) |
| Current work | |
| Institution based | 40 (38.8) |
| Private practice | 36 (35) |
| Both | 27 (26.2) |
| Place of work | |
| Rural | 5 (4.9) |
| Semiurban | 25 (24.3) |
| Urban | 73 (70.9) |
| Experience (years) | 12.5 (10.31) |
SD – Standard deviation
Knowledge about lithium use
When the knowledge about stabilization of lithium doses in acute stage and prophylaxis was assessed, almost 75% of the respondents did that on a dose-dependent basis rather than blood level dependent (25%). More than 60% of those who preferred dose-dependent titration opined that patients in acute stage needed doses more than 900 mg whereas same proportion of them opined that most patients need doses <900 mg in their maintenance stage.
About 12% of the psychiatrists from the sample preferred to use lithium once daily compared to multiple times a day (88%), irrespective of the phase of bipolar disorder [Table 2a].
Table 2a.
Dosing in acute stage and maintenance
| Variable | Frequency (%) |
|---|---|
| Acute | |
| Dose dependent | 78 (75.7) |
| <900 mg | 29 (37) |
| >900 mg | 49 (63) |
| Blood level dependent | 25 (24.3) |
| Maintenance | |
| Dose dependent | 77 (74.8) |
| <900 | 64 |
| >900 | 13 |
| Blood level dependent | 26 (24.2) |
| Frequency of monitoring lithium levels in maintenance phase | |
| 3 monthly | 42 (40.8) |
| 6 monthly | 46 (44.7) |
| 1 monthly | 4 (3.9) |
| Yearly | 6 (5.8) |
| Based on feasibility | 5 (4.9) |
| Dosing frequency | |
| Once daily | 12 (11.7) |
| >Once daily | 91 (88.3) |
Nearly, 96% of the psychiatrists were of the opinion that at least lithium was moderately effective in lowering the suicidal risk due to any cause [Table 2b].
Table 2b.
Perceived effectiveness of lithium in lowering the suicidal risk
| Variable | Frequency (%) |
|---|---|
| Don’t use lithium for that purpose | 2 (1.9) |
| Ineffective | 2 (1.9) |
| Moderate effective | 40 (38.8) |
| Somehow effective | 14 (13.6) |
| Very effective | 45 (43.7) |
Attitude about using lithium
When asked about their level of comfort in using lithium on an outpatient basis, around 70% of them opined that they are very comfortable in using lithium.
In case of using lithium as an augmenting agent for treatment-resistant depression, around 50% of the psychiatrists were very comfortable in prescribing lithium for that purpose [Figure 1].
Figure 1.
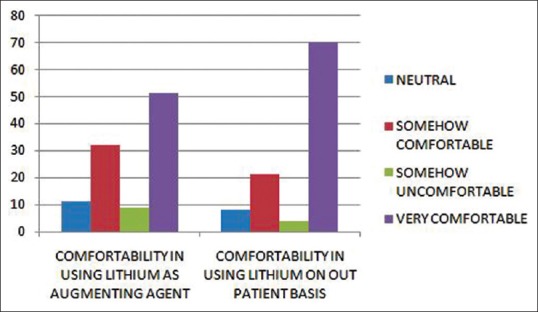
Perceived level of comfort in using lithium
Most of the psychiatrists preferred using lithium in patients aged between 20 and 39 years (94%) which was followed by 40–64 age group who constituted up to 59% whereas psychiatrists were not comfortable in using lithium in elderly (3%) and in adolescents (17%).
Practice of lithium prescription
When asked about the option of preferred agent as followed in their actual clinical practice, following were the responses received [Figure 2].
Figure 2.
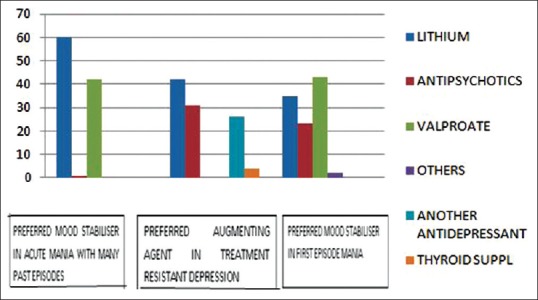
Preferred treating agent in clinical practice
In a patient presenting with acute mania and past history of bipolar disorder, 60% of them preferred starting lithium compared to valproate and other mood stabilizers (40%). In first episode mania patients, valproate (40%) was preferred as a first choice followed by lithium (35%) and antipsychotics (20%). Lithium was the first choice as augmenting agent in treatment-resistant depression followed by antipsychotics, another antidepressant, and thyroid supplementation, respectively.
Lithium was used more frequently in both first episode and multiepisode mania by psychiatrists with duration of experience more than 5 years. Furthermore, psychiatrist with higher duration of experience used lithium more frequently in cases of mild cognitive impairment [Table 2c].
Table 2c.
Relation of lithium use and duration of experience
| Variable | Experience (%) |
χ2 (P) | |
|---|---|---|---|
| <5 years | >5 years | ||
| Drug commonly used in first episode mania | |||
| Lithium | 9 (8.8) | 26 (25) | 104.32 (<0.001) |
| Others | 21 (20.3) | 47 (45.6) | |
| Drug commonly used in multiepisode mania | |||
| Lithium | 20 (19.4) | 40 (38.8) | 105.22 (<0.001) |
| Others | 10 (9) | 33 (32.0) | |
| Use of lithium for mild cognitive impairment | |||
| Yes | 16 (15.5) | 30 (29.1) | 105.30 |
| No | 14 (13.5) | 43 (41.7) | (<0.001) |
The most common obstacle as perceived by psychiatrists in prescribing lithium was patient's clinical comorbidities followed by low adherence rate to serum level monitoring. Other frequent reasons preventing starting of lithium were burden of adverse effect monitoring and slow action of lithium [Table 2d].
Table 2d.
Obstacles perceived by psychiatrists in prescribing lithium
| Obstacles in prescribing lithium | Frequency (%) |
|---|---|
| Adverse effect monitoring | 19 (18.4) |
| Difficulty in dose titration | 2 (1.9) |
| Lack of experience | 3 (2.9) |
| Patient’s clinical comorbidities | 33 (32.0) |
| Patient’s low adherence to serum-level monitoring | 30 (29.1) |
| Slow action of lithium | 16 (15.5) |
As a part of prelithium workup [Table 2e], more than half of the sample preferred in investigating renal function tests (93%), thyroid function tests (91%), electrocardiography (58%), and weight monitoring (56%) while estimated glomerular filtration rate (25%) is the least preferred among all. When asked about management of polyuria associated with lithium, 43.7% of respondents said that they would reassure the patient first, which was followed by discontinuing lithium (31.1%) and starting thiazide diuretics (11.7%). Regarding hypothyroidism associated with lithium, 75.7% of psychiatrists preferred to continue lithium by adding thyroxine, 31.1% preferred to add thyroxine but to discontinue lithium whereas 22.3% preferred to change mood stabilizer. Following lithium toxicity, a third of psychiatrists preferred not to rechallenge, one-third of them wanted to rechallenge, whereas one-third were not sure about the same.
Table 2e.
Prelithium workup and management strategies for adverse effects of lithium
| Variable | Frequency (%) |
|---|---|
| Prelithium workup (multiple responses permitted) | |
| Thyroid function tests | 94 (91) |
| Renal function tests | 96 (93) |
| eGFR | 26 (25) |
| ECG | 60 (58) |
| Weight | 58 (56) |
| How do you manage polyuria associated with lithium | |
| Reassurance | 45 (43.7) |
| Discontinue lithium | 32 (31.1) |
| Start thiazides | 12 (11.7) |
| Others | 14 (13.6) |
| How do you manage hypothyroidism associated with lithium | |
| Add thyroxine and continue lithium | 78 (75.7) |
| Add thyroxine and discontinue lithium | 32 (31.1) |
| Discontinue lithium and change mood stabilizer | 23 (22.3) |
| Would you rechallenge following lithium toxicity | |
| May be | 40 (38.8) |
| Yes | 32 (31.1) |
| No | 31 (30.1) |
ECG – Electrocardiography; eGFR – Estimated glomerular filtration rate
DISCUSSION
In this study, we attempted to assess the knowledge, attitude, and practices of lithium therapy among psychiatrists in India. This way, we tried to indirectly assess the factors responsible for theory–practice gap for the prescription of lithium in bipolar disorders.
The current study unfolded several important practical difficulties in using lithium in various settings. The majority of psychiatrists who completed the survey were of the opinion that lithium dosing should be done both in the acute phase and maintenance phase on a dose-dependent basis rather than the blood level-dependent basis. Despite the evidence-based recommendations[5,19,20] by guidelines that dose adjustment of lithium should be done on the basis of serum lithium levels irrespective of the phase of the illness, this contrary finding of ours suggests that the busy schedules, hectic outpatient clinics, cost factor, and poor adherence to blood monitoring by the patients might be contributory to this view.
Majority of the psychiatrists were of the view that lithium is useful in patients with suicidal risk/attempts, treatment-resistant depression, and bipolar mania. Their views were in line with the current existing evidence for the abovementioned indications.[21,22,23] Despite this, they were skeptical in starting lithium in such patients due to multitude of barriers such as comorbidities, patient's low adherence to blood monitoring, and adverse effects. These could be the reasons behind psychiatrists preferring valproate to lithium in first episode mania.
A review done to understand the safety and tolerability profile of lithium in bipolar disorder patients clearly replicates the fact that there are definite adverse effects due to the drug. However, the proportion of those who do not develop them is higher than the ones who develop and most of them can be avoided or managed by simple strategies if one is aware about them.[24,25] For example, once-daily dosing and keeping lithium levels low prevent the development of renal impairment in a multitude of patients.[26,27] However, in our study, psychiatrists preferred using multiple dosing to once-daily dose, suggesting theory–practice gap in the prescription patterns.
Bipolar treatment guidelines suggest that side effects such as hypothyroidism (both overt and subclinical) can be easily treated with thyroxine supplementation and our study finding represented the same. The dilemma in this regard is whether the patient developed hypothyroid state due to the preexisting mood disorder itself or the drug exerts an independent effect on the person. Furthermore, evidence about the teratogenicity of lithium is not confirmatory. Although we cannot rule out the teratogenic nature of the drug, the risk has been definitely overestimated. Furthermore, one has to bear in mind the fact that the newer drugs which are being used widely in place of lithium are not devoid of adverse effects although their profile of side effects is different from that of lithium.[28,29]
Limitations
Our study has certain limitations; the small sample of psychiatrists included in the study and the relatively poor response rate might not exactly depict the situations. It is not representative of psychiatrists from all over India. Furthermore, there might be a discrepancy between the responses given and the actual practice. It might be due to the hectic outpatient clinics, bothersome monitoring of adverse effects, and the fall in popularity of the lithium due to promotion of newer drugs by pharmaceutical companies. As it was an online survey, it might not have included the experienced psychiatrists who were using lithium in their actual practice more than the current generation ones, which is reflected on by the mean age of 39 years. The options that were given for the questions might be limited as we have used a semistructured questionnaire for assessment rather than a validated scale.
CONCLUSIONS AND FUTURE DIRECTIONS
In conclusion, our study found certain factors which might be a hindrance for the use of lithium in clinical settings. Duration of experience as a psychiatrist was the factor which affected the higher use of lithium in indicated conditions. Most psychiatrists in the survey preferred using lithium multiple times a day and on a dose-dependent basis contrary to the guidelines. And also, we found that although the participants were aware of the indications and monitoring techniques, they perceived certain obstacles while actually using lithium in their clinical practice. Therefore, improving the knowledge of psychiatrists about the incidence of adverse effects and techniques of managing the side effects can reduce their reluctance in starting lithium therapy.
Contrary to the usual notion, psychiatrists should understand that the side effects of lithium are not as malignant as presumed to be, particularly at therapeutic doses. Side effects such as tremors can be easily managed by reducing dose to below one's side effect threshold, as clinical effects can be seen at lower levels or with β-blockers. Lithium-induced hypothyroidism can be easily corrected by addition of thyroid supplementation, and use of minimum effective doses with monitoring can reduce the renal damage due to lithium. Despite its side effects, it is one of the few drugs which has been approved for the treatment of suicidality.[30]
Particularly, the young psychiatrists should receive necessary training in starting and monitoring patients on lithium therapy.[1] There is a need to emphasize to physicians about the cost-effectiveness of lithium therapy. This should be achieved through education programs and workshops. This will help them to use lithium in a more appropriate manner in their clinical practice. That way, we can save the “magic molecule” from its downfall, utilizing it for the needy. Also, the recent evidence from preclinical studies that documented the neuroprotective effects of lithium both by preventing apoptosis and promoting neurogenesis has suggested the potential benefits of using it in the management of neurodegenerative diseases, neurodevelopmental disorders, and hypoxic-ischemic/traumatic brain injury.[31,32,33] Further studies should be conducted on a large scale to explore the usefulness of lithium and to help psychiatrists get over the barriers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dwight-Johnson M, Lagomasino IT, Simpson GM. Underuse of evidence-based pharmacotherapies for affective disorders. Psychiatr Serv. 2003;54:1076–8. doi: 10.1176/appi.ps.54.8.1076. [DOI] [PubMed] [Google Scholar]
- 2.Miura T, Noma H, Furukawa TA, Mitsuyasu H, Tanaka S, Stockton S, et al. Comparative efficacy and tolerability of pharmacological treatments in the maintenance treatment of bipolar disorder: A systematic review and network meta-analysis. Lancet Psychiatry. 2014;1:351–9. doi: 10.1016/S2215-0366(14)70314-1. [DOI] [PubMed] [Google Scholar]
- 3.Vieta E, Günther O, Locklear J, Ekman M, Miltenburger C, Chatterton ML, et al. Effectiveness of psychotropic medications in the maintenance phase of bipolar disorder: A meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2011;14:1029–49. doi: 10.1017/S1461145711000885. [DOI] [PubMed] [Google Scholar]
- 4.Fieve RR. Lithium therapy at the millennium: A revolutionary drug used for 50 years faces competing options and possible demise. Bipolar Disord. 1999;1:67–70. doi: 10.1034/j.1399-5618.1999.010201.x. [DOI] [PubMed] [Google Scholar]
- 5.Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Beaulieu S, Alda M, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: Update 2013. Bipolar Disord. 2013;15:1–44. doi: 10.1111/bdi.12025. [DOI] [PubMed] [Google Scholar]
- 6.Rej S, Schuurmans J, Elie D, Stek ML, Shulman K, Dols A, et al. Attitudes towards pharmacotherapy in late-life bipolar disorder. Int Psychogeriatr. 2016;28:945–50. doi: 10.1017/S1041610215002380. [DOI] [PubMed] [Google Scholar]
- 7.Enudi W, Lawlor B, O'Connell HP. A survey of patients' knowledge about lithium therapy in the elderly. Prim Care Companion CNS Disord. 2014;16:pii: PCC13m01550. doi: 10.4088/PCC.13m01550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mulligan KA, Cheyette BN. Neurodevelopmental perspectives on Wnt signaling in psychiatry. Mol Neuropsychiatry. 2017;2:219–46. doi: 10.1159/000453266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valvassori SS, Resende WR, Dal-Pont G, Sangaletti-Pereira H, Gava FF, Peterle BR, et al. Lithium ameliorates sleep deprivation-induced mania-like behavior, hypothalamic-pituitary-adrenal (HPA) axis alterations, oxidative stress and elevations of cytokine concentrations in the brain and serum of mice. Bipolar Disord. 2017;19:246–58. doi: 10.1111/bdi.12503. [DOI] [PubMed] [Google Scholar]
- 10.Halder T, Datta U, Basu S, Mukherjee P. Is lithium essential for epididymal sperm maturation? Med Hypotheses. 2016;96:48–50. doi: 10.1016/j.mehy.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Makhija S, Gupta R, Toteja R. Lithium-induced developmental anomalies in the spirotrich ciliate stylonychia lemnae (Ciliophora, hypotrichida) Eur J Protistol. 2015;51:290–8. doi: 10.1016/j.ejop.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Maddu N, Raghavendra PB. Review of lithium effects on immune cells. Immunopharmacol Immunotoxicol. 2015;37:111–25. doi: 10.3109/08923973.2014.998369. [DOI] [PubMed] [Google Scholar]
- 13.Singh LK, Nizamie SH, Akhtar S, Praharaj SK. Improving tolerability of lithium with a once-daily dosing schedule. Am J Ther. 2011;18:288–91. doi: 10.1097/MJT.0b013e3181d070c3. [DOI] [PubMed] [Google Scholar]
- 14.Shetty SJ, Desai PB, Patil NM, Nayak RB. Relationship between serum lithium, salivary lithium, and urinary lithium in patients on lithium therapy. Biol Trace Elem Res. 2012;147:59–62. doi: 10.1007/s12011-011-9295-3. [DOI] [PubMed] [Google Scholar]
- 15.Thirthalli J, Harish T, Gangadhar BN. A prospective comparative study of interaction between lithium and modified electroconvulsive therapy. World J Biol Psychiatry. 2011;12:149–55. doi: 10.3109/15622975.2010.504860. [DOI] [PubMed] [Google Scholar]
- 16.Singh LK, Praharaj SK, Munda SK, Khess CR. Lithium-induced sinus node dysfunction at therapeutic serum levels. Natl Med J India. 2011;24:151–2. [PubMed] [Google Scholar]
- 17.Mohapatra S, Sahoo MR, Rath N. Lithium-induced motor neuropathy: An unusual presentation. Indian J Psychol Med. 2016;38:252–3. doi: 10.4103/0253-7176.183076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shetty RK, Vivek G, Parida A, Chetty S. Lithium-induced sinus node dysfunction at therapeutic levels. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2012-008107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kendall T, Morriss R, Mayo-Wilson E, Marcus E. Guideline Development Group of the National Institute for Health and Care Excellence. Assessment and management of bipolar disorder: Summary of updated NICE guidance. BMJ. 2014;349:g5673. doi: 10.1136/bmj.g5673. [DOI] [PubMed] [Google Scholar]
- 20.American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision) Am J Psychiatry. 2002;159:1–50. [PubMed] [Google Scholar]
- 21.Latalova K, Kamaradova D, Prasko J. Suicide in bipolar disorder: A review. Psychiatr Danub. 2014;26:108–14. [PubMed] [Google Scholar]
- 22.Cipriani A, Girlanda F, Agrimi E, Barichello A, Beneduce R, Bighelli I, et al. Effectiveness of lithium in subjects with treatment-resistant depression and suicide risk: A protocol for a randomised, independent, pragmatic, multicentre, parallel-group, superiority clinical trial. BMC Psychiatry. 2013;13:212. doi: 10.1186/1471-244X-13-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou X, Ravindran AV, Qin B, Del Giovane C, Li Q, Bauer M, et al. Comparative efficacy, acceptability, and tolerability of augmentation agents in treatment-resistant depression: Systematic review and network meta-analysis. J Clin Psychiatry. 2015;76:e487–98. doi: 10.4088/JCP.14r09204. [DOI] [PubMed] [Google Scholar]
- 24.Wang D, Osser DN, Mohammad O, Tondo L, Giakoumatos CI, Ghaemi N. Lithium: Key issues for practice. Program and abstracts of the American Psychiatric Association 2017 Annual Meeting; 20-24 May, 2017; San Diego, California. [Google Scholar]
- 25.Vestergaard P, Licht RW. 50 years with lithium treatment in affective disorders: Present problems and priorities. World J Biol Psychiatry. 2001;2:18–26. doi: 10.3109/15622970109039980. [DOI] [PubMed] [Google Scholar]
- 26.Plenge P, Mellerup ET, Bolwig TG, Brun C, Hetmar O, Ladefoged J, et al. Lithium treatment: Does the kidney prefer one daily dose or two? Acta Psychiatr Scand. 1982;66:121–8. doi: 10.1111/j.1600-0447.1982.tb00920.x. [DOI] [PubMed] [Google Scholar]
- 27.Gitlin M. Lithium and the kidney: An updated review. Drug Saf. 1999;20:231–43. doi: 10.2165/00002018-199920030-00004. [DOI] [PubMed] [Google Scholar]
- 28.Gitlin M. Lithium side effects and toxicity: Prevalence and management strategies. Int J Bipolar Disord. 2016;4:27. doi: 10.1186/s40345-016-0068-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ivan A, Teixeira de SR, da Costa Lane VL, Rodrigo MV, Vicente FO. Lithium safety and tolerability in mood disorders: A critical review. Rev Psiquiatr Clín. 2014;41:9–14. [Google Scholar]
- 30.Post RM. The new news about lithium: An underutilized treatment in the United States. Neuropsychopharmacology. 2018;43:1174–9. doi: 10.1038/npp.2017.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quiroz JA, Machado-Vieira R, Zarate CA, Jr, Manji HK. Novel insights into lithium's mechanism of action: Neurotrophic and neuroprotective effects. Neuropsychobiology. 2010;62:50–60. doi: 10.1159/000314310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dwivedi T, Zhang H. Lithium-induced neuroprotection is associated with epigenetic modification of specific BDNF gene promoter and altered expression of apoptotic-regulatory proteins. Front Neurosci. 2014;8:457. doi: 10.3389/fnins.2014.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dell'Osso L, Del Grande C, Gesi C, Carmassi C, Musetti L. A new look at an old drug: Neuroprotective effects and therapeutic potentials of lithium salts. Neuropsychiatr Dis Treat. 2016;12:1687–703. doi: 10.2147/NDT.S106479. [DOI] [PMC free article] [PubMed] [Google Scholar]


