Abstract
Gossypiboma is an uncommon but avoidable condition, which is mostly asymptomatic initially and difficult to diagnose but can cause serious postoperative complications. It is a mass lesion due to surgical sponge or swab if retained in the body after the surgery. Gossypiboma has a vague presentation, and it is difficult to diagnose. In patients with a prior history of surgery having soft-tissue masses or localized pain abdomen, gossypiboma should be included in the differential diagnosis. We are reporting a case of a 33-year-old woman referred to our center with a complaint of vague abdominal pain, mild distension for the past 7 days, and discharge from the stitch line for the past 1 day. After investigation, diagnosis of gossypiboma was made and an exploratory laparotomy was performed to remove the retained surgical mop.
KEYWORDS: A surgical sponge, gossypiboma, retained foreign bodies
INTRODUCTION
Gossypiboma is a term used when a surgical sponge or a laparotomy pad is left unknowingly in the patient body after a surgical procedure. The term gossypiboma is derived from a Latin word “Gossypium” that is cotton and Swahili word “boma” that means place of concealment.[1] Gossypiboma is a rare surgical complication, but it is a nightmare for a surgeon. Textiloma, muslinomas, cottonoid, and gauzeoma are few terminologies that can be used for gossypiboma.[2] Gossypiboma is an avoidable condition but if it occurs it poses serious morbidity and mortality.[3] The actual incidence of gossypiboma is difficult to establish due to underreporting of such type of cases due to fear of legal issues. In reported literature, it is found the abdomen is the most common site for retained surgical mop after abdominal surgeries. The incidence of retained foreign bodies such as sponge, needle, or any part of instrument following surgery is 0.01%–0.001%. Out of all these foreign bodies, the major chunk is of gossypiboma, that is, 80% of cases.[4] Mostly, the cases of gossypiboma may be detected within few days after surgery, but some may remain undetected after many years also. Various imaging modalities are there such as plain radiography, ultrasonography (USG), computed tomography (CT), and magnetic resonance imaging (MRI) that can help in making the diagnosis. Surgery is the recommended treatment for gossypiboma.[1] We are reporting a case of a 33-year-old woman referred to our center with a complaint of vague abdominal pain, mild distension for the past 7 days, and discharge from the stitch line for the past 1 day. After investigation, diagnosis of gossypiboma was made and an exploratory laparotomy was performed to remove the retained surgical mop.
CASE REPORT
A 33-year-old woman presented to our hospital with a complaint of epigastric pain, loss of appetite, mild distension, and constipation for the past 7 days. The patient also complains of discharge from the stitch line for the past 1 day. She had a history of total abdominal hysterectomy along with bilateral salpingooophorectomy done 15 days back in some private hospital because of heavy menstrual bleeding. Postoperative period was uneventful, and the patient was discharged on the 17th day. The patient was asymptomatic 7 days back and after that she developed pain in the abdomen and bloating after intake of meals. She also complains of mild distension and constipation for the past 7 days. The patient also gave a history of discharge from the stitch line for the past 1 day.
On examination, vitals were stable, a vertical infraumbilical scar was present, and there was a vague tender mass with restricted mobility and smooth surface. There was pus discharge from the upper 1 cm of the stitch line. The pus was sent for culture and sensitivity. On per-vaginal examination, vault seems to be healthy. The patient was started on conservative management, and meanwhile, various laboratory tests were done. Her laboratory parameters came within normal limits. Plain abdominal radiograph was suggestive of linear radiopaque shadow in the right side of the upper abdomen [Figure 1a]. USG revealed intraabdominal collection with echogenic shadows within the collection [Figure 1b]. To confirm the diagnosis of gossypiboma, contrast-enhanced CT was done which revealed well-defined, peripherally enhancing capsulated collection (7.6 cm × 7.3 cm × 7.6 cm) with multiple air foci and hyperdense material seen in the peritoneal cavity [Figure 2a and b]. This collection has a connection with the skin surface exteriorly (infraumbilical) along the suture line. The uterus is not visualized (postoperative status). The final diagnosis was suggestive of gossypiboma. The decision for exploratory laparotomy was taken.
Figure 1.
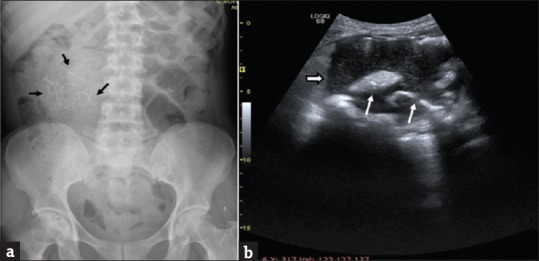
(a) Abdominal radiograph showing linear radiopaque foreign body (black arrows) in the right side of upper abdomen (b) ultrasound showing collection with internal echoes (arrowhead) and echogenic foreign body (white arrows) within the collection
Figure 2.
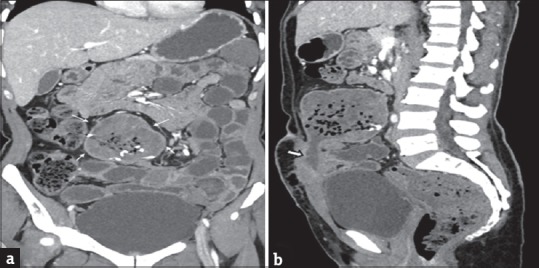
(a) Coronal reformatted contrast-enhanced computed tomography images reveal gossypiboma lesion as a collection with mottled air specks (arrows) and hyperdense serpiginous structure. (b) Sagittal computed tomography scan showing hypodense linear tract (arrowhead) extending along the incision site
The abdomen was opened through a midline vertical incision. On exploration, a retained surgical sponge was found along with 500 cc of pus lying in a walled-off cavity in the lower abdomen. A pus sample was collected and sent for culture and sensitivity. The pus was sucked out with the help of suction. There were multiple dense adhesions of the bowel loop. The retained surgical cotton mop of 30 cm × 15 cm was surrounded by the omentum [Figure 3a]. The surgical mop along with the surrounding omentum was removed [Figure 3b] and peritoneal lavage was done. As the upper part of the abdominal wound was infected, it was left open at that time and the dressing was done regularly. Suturing was done after 10 days. The patient did well after the surgery. The resected specimen was sent for histopathology, which revealed features of acute granulomatous inflammation, foci of necrosis and hemorrhage, sheets of foamy histiocytes, and lymphoid aggregates. Postoperative period was uneventful, and the patient recovered well. The patient was discharged on postoperative day 15 and advised for follow-up. We thereafter informed the hospital where the primary surgery was conducted to facilitate initiation of preventive steps to prevent this type of negligence in future.
Figure 3.
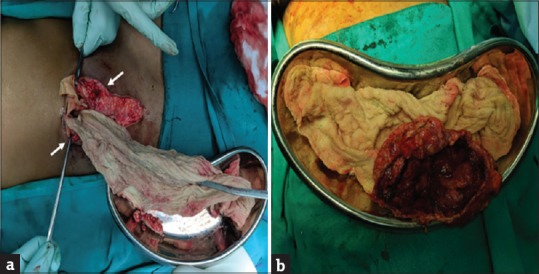
(a) Intraoperative picture showing the retained surgical sponge being removed from the abdomen (arrows). (b) Picture of the resected specimen along with the retained sponge
DISCUSSION
Gossypiboma is rare and infrequent, but if it occurs it causes a serious complication that may lead to medicolegal issues. These types of cases lead to embarrassment, loss of job, humiliation, and lawsuit worldwide.[3] The incidence reported so far is 1 in 1000–1500 abdominal operation.[1] However, its actual number is difficult to say because mostly these cases are not reported due to its medicolegal implications.[4] One of the articles is published in the New England Journal of Medicine about the risk factors of the retained foreign body. Mentioned risk factors for the retained foreign body are emergency surgeries, surgeries that involve more than one team, change of nursing staff during surgery, inexperienced staff, more blood loss, hurried surgical count, long operations, increased body mass index, and unexpected change in the procedure.[5] Retained surgical mop in the abdominal cavity leads to two types of reaction. The first response that is an exudative inflammatory reaction with pus formation leads to early discovery and surgical intervention and the second response is usually an aseptic reaction to the cotton material, which leads to fibrosis and development of mass.[6] Nearly, one-third of the patients remains asymptomatic and diagnosed incidentally. This complication can occur in any surgery, but it is found that incidence is more after hysterectomy, appendectomy, and cholecystectomy. Pain is the most common presenting complaint of gossypiboma. The patient can sometimes present with abdominal distension, fever, lump, diarrhea, abscess, nausea, vomiting, anorexia, and weight loss.[4] Laparoscopic retrieval is possible if diagnosis was made early.[3] Imaging modalities such as plain radiography, USG, CT, and MRI help in making a diagnosis of gossypiboma.[7] Particularly in long-standing cases, sometimes it is difficult to distinguish gossypiboma from an intra-abdominal abscess on CT findings, as air bubbles, calcification of the cavity and contrast enhancement of the rim may be seen in both conditions.[2] Once diagnosed, surgical removal of the foreign body is the mainstay of treatment. Adhesions, abscess, fistula formation, and migration of foreign body are complications of gossypiboma. The omentum is known as the policeman of the abdomen. The omentum and small intestine tends to surround the foreign body, as a result the encapsulated foreign body causes pressure necrosis and later on leads to fistula formation.[4] Gossypiboma has its own medico-legal implications, so important preventive steps at the end of the surgery, like separate count for sponge, sharps and instrument should be taken. It has been recommended that four separate counts be done. First, count when the set and sponges are unpacked, second just before the start of surgery, third as the closure begins, and the final count during skin closure [6] Newer technologies like the electronic article surveillance system and the radiofrequency chip identification by barcode scanner will help in decreasing the incidence of retained foreign bodies.[8]
CONCLUSION
Gossypiboma is an uncommon but avoidable condition, which is mostly asymptomatic and difficult to diagnose but causes serious postoperative complications, particularly in long-standing cases where radiological findings mimic that of intraabdominal abscess. Because of serious complications and medicolegal implications, it is very important to take measures to prevent it. Although it is difficult to avoid human errors completely, it is very important to strictly adhere to the rules of operation theater and proper medical training should be given to reduce the incidence of gossypiboma. In patients with prior history of surgery having soft-tissue masses or localized pain abdomen, gossypiboma should be included in the differential diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Srivastava KN, Agarwal A. Gossypiboma posing as a diagnostic dilemma: A case report and review of the literature. Case Rep Surg. 2014;2014:713428. doi: 10.1155/2014/713428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kataria SP, Garg M, Marwah S, Sethi D. Acute abdomen by gossypiboma. Ann Trop Med Public Health. 2012;5:511. doi: 10.4103/2141-9248.105677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lata I, Kapoor D, Sahu S. Gossypiboma, a rare cause of acute abdomen: A case report and review of literature. Int J Crit Illn Inj Sci. 2011;1:157–60. doi: 10.4103/2229-5151.84805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garg MK, Zeya MT, Garg U, Goyal S, Yadav M. Gossypiboma a diagnostic dilemma or medical negligence a case report. Journal of Indian Academy of Forensic Medicine. 2014;36:100–3. [Google Scholar]
- 5.Aminian A. Gossypiboma: A case report. Cases J. 2008;1:220. doi: 10.1186/1757-1626-1-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quraishi AH. Beyond a gossypiboma. Case Rep Surg. 2012;2012:263841. doi: 10.1155/2012/263841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malhotra MK. Migratory surgical gossypiboma-cause of iatrogenic perforation: Case report with review of literature. Niger J Surg. 2012;18:27–9. doi: 10.4103/1117-6806.95486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Macario A, Morris D, Morris S. Initial clinical evaluation of a handheld device for detecting retained surgical gauze sponges using radiofrequency identification technology. Arch Surg. 2006;141:659–62. doi: 10.1001/archsurg.141.7.659. [DOI] [PubMed] [Google Scholar]


