Abstract
Background
There is a global decline in interest in careers in renal medicine. This is concerning given the increasing global burden of kidney disease. Previous studies in the USA and Australia have identified factors such as a poor work–life balance, lack of role models and the challenging nature of the speciality as possible reasons behind recruitment struggles. This study aimed to identify factors associated with declining interest among trainees in the UK.
Methods
We conducted a survey of 150 National Health Service Foundation trainees (interns) and Core Medical Trainees in Health Education West Midlands. Participants completed a 14-part paper-based questionnaire capturing data on trainee demographics, medical school and postgraduate exposure to renal medicine and perceptions of a career in renal medicine.
Results
There was limited early clinical exposure to renal medicine both in terms of time spent in the speciality and perceived exposure to the range of domains of the speciality. Trainees perceived the speciality as complex with a heavy workload. Very few trainees considered the speciality to be lifestyle oriented. There was also disinterest in taking on the associated general medicine commitments of the training programme. Job experience and identification of role models increased the likelihood of consideration of the speciality.
Conclusion
This survey has identified key areas to drive interest in the speciality, including early engagement, enthusiastic supervision and increased training flexibility. Urgent attention is required to address these areas and make renal medicine careers more appealing.
Keywords: qualitative study, recruitment, renal medicine, training, United Kingdom
INTRODUCTION
There is growing concern globally over declining interest in renal medicine as a career. The USA, for example, has experienced a significant decrease in nephrology training post fill rates from 94.8% in 2009 to 59.8% in 2016 [1]. Similarly, in the UK, the fill rate has decreased from 100% in 2013 to 74% in 2017. In 2017, the applicant:post ratio for dermatology was 5.58 as compared with 1.58 in renal medicine [2]. The perceived clinical challenge of the speciality known to attract intelligent and hardworking individuals is transforming into a recruitment struggle failing to meet the increasing workforce demands to counter the rising burden of kidney disease. Previous surveys in the USA and Australia have identified factors such as a poor work–life balance, lack of role models, lack of procedures and the perceived difficulty of the speciality as deterrents of interest in renal medicine [3, 4]. However, there have not been any recent studies exploring this in the UK.
In the National Health Service (NHS) in the UK, enrolment into renal medicine training programmes requires postgraduate applicants to have completed the 2-year Foundation Training (FT) programme, an intern generic training scheme and the 2-year Core Medical Training (CMT) programme, the first stage of internal medicine training. The CMT consists of a combination of six 4-month medical subspeciality rotations over 2 years and requires trainees to achieve membership in the Royal College of Physicians through examination. Renal medicine specialist training lasts for 3 years, with the majority of trainees opting to do an additional 2 years as the medical registrar to dual accredit in general internal medicine. Doctors in training are collectively referred to as junior doctors.
We carried out a survey of foundation year and core medical trainees in Health Education West Midlands, a training region within the UK, to investigate training doctors’ perceptions of renal medicine as a speciality as well as factors influencing the choice of renal medicine as a career.
MATERIALS AND METHODS
A 14-part paper-based questionnaire (Supplementary data) was distributed at hospital FT and CMT induction programmes in August 2017. The questionnaire captured data on trainees’ age, grade of training, gender, previous clinical exposure to renal medicine in medical school and after graduation, domains of renal medicine with clinical experience, perception of role models, impression of workload and lifestyle orientation, complexity of speciality and perceptions of a career in renal medicine. We incorporated free-text comment areas for respondents to document their intended speciality choice, reasons for considering and not considering a career in renal medicine and suggestions on changes that could be made to the training programme to make a career in renal medicine more appealing.
The data are categorical and presented as counts and percentages. The 95% confidence interval for proportions was calculated as where p = percentage and n = sample size. Between-group comparisons between categorical data are performed using the chi-squared test. Statistical analysis was performed using SPSS version 22 (IBM, Armonk, NY, USA). Figure graphs were designed using GraphPad Prism 5 (GraphPad Software, San Diego, CA, USA).
RESULTS
We had 150 responses in total from 79 FT and 71 CMT trainees. There were 67 male and 69 female respondents. Fourteen junior doctors did not provide details of their gender. The median age of the respondents was 26 (interquartile range 25–28) years.
Limited early exposure to renal medicine
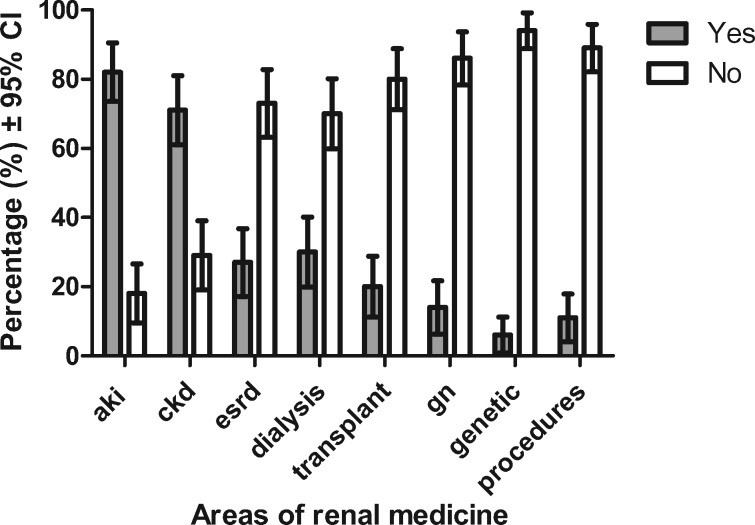
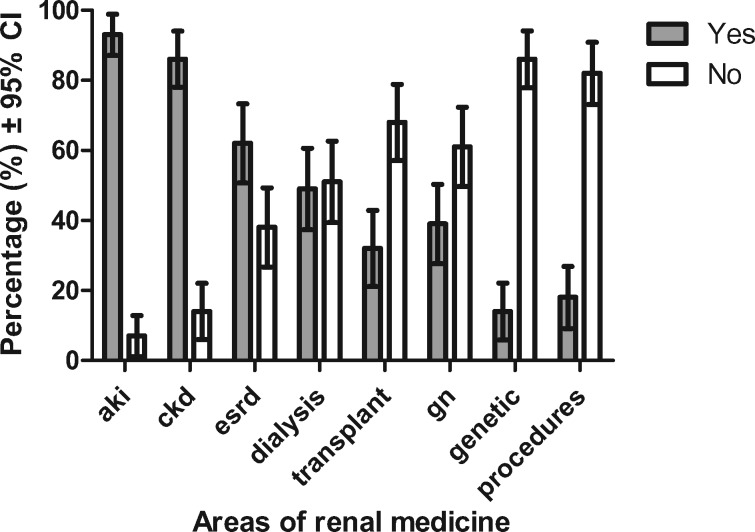
Of the respondents, 19% had no clinical exposure to renal medicine in medical school. The mode duration of exposure in medical school was between 0 and 2 weeks (42%). There was improved exposure to renal medicine in postgraduate training; 44% of CMT trainees had done or were scheduled to rotate through renal medicine. The perceived exposure, however, remained limited for both FT and CMT trainees with less than half of the respondents citing experience in renal transplant, glomerulonephritis, renal genetic disease and renal procedures, suggesting these as underserved areas in junior training (Figures 1 and 2). Furthermore, less than a third of trainees (27%) were able to identify role model nephrologists.
FIGURE 1.
FT trainees’ clinical exposure to different domains of renal medicine.
FIGURE 2.
CMT trainees’ clinical exposure to different domains of renal medicine.
Perception of renal medicine as a complex speciality with a heavy workload
The majority of respondents (86%) felt that the renal medicine speciality is highly complex. In addition, 60 and 17% of respondents considered the workload in renal medicine to be heavy and moderate, respectively. Importantly, 65% of respondents considered the work–life balance of their chosen speciality to be very important in decision making, while only 12% of respondents felt that a career in renal medicine was lifestyle oriented.
Number considering the career is not materializing into applications
Overall, 20 and 27% of FT and CMT trainees, respectively, stated that they would consider a career in renal medicine. However, only 4% of all higher medical speciality applications in 2017 were to renal medicine, suggesting that this consideration is not materializing into applications [2]. Only 0 and 8% of FT and CMT trainees, respectively, listed renal medicine as a first-choice speciality. A very low proportion (13%) of FT trainees stated that they would consider a career as a medical registrar. Moreover, even among CMT trainees, only 61% said that they would consider a career as a medical registrar. Interestingly, all the CMT trainees who stated renal medicine as their first-choice speciality were ‘not sure’ as to whether they would be trained in a speciality with general medical commitments. The female:male ratio of respondents in CMT (1.27:1) was higher than the female:male ratio of CMT trainees considering a career in renal medicine (0.72:1), which demonstrates lower interest among female trainees.
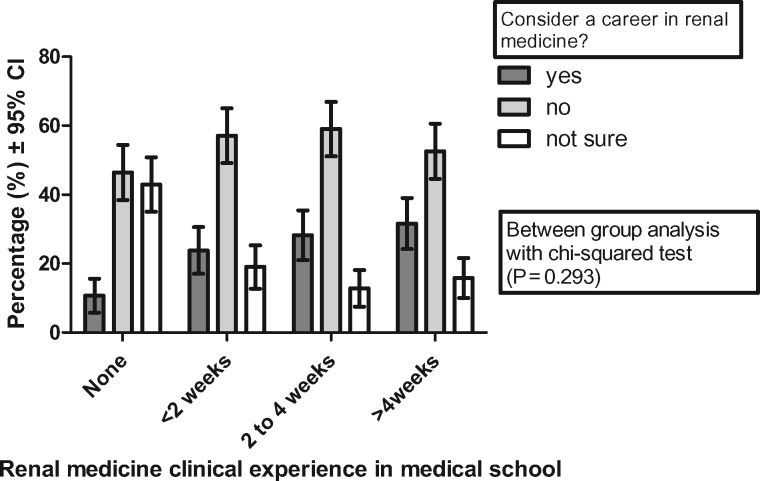
Early exposure, training jobs and identification of role models increase interest in a renal medicine career
The proportion of trainees who would consider a career in renal medicine increased with the duration of exposure in medical school (Figure 3). Thirty-two percent of trainees with >4 weeks of experience would consider a career in renal medicine as compared with 11% with no exposure; however, this difference was not statistically significant (P = 0.293). Trainees who had previously done or were scheduled for a job in renal medicine were more likely to consider a career in the speciality (42%) compared with those who had not (17%) (P = 0.001). Trainees who were able to identify a role model in renal medicine were also more likely to consider a career in renal medicine (38%) compared with those who did not (15%) (P = 0.007).
FIGURE 3.
Effect of duration of experience in medical school on whether trainees would consider a career in renal medicine.
Other first-choice specialities
Among CMT trainees, there was a wide spread of first-choice speciality interest. Six (8%) of the trainees stated renal medicine as a first-choice interest, 10 (14%) respiratory, 9 (10%) gastroenterology, 8 (11%) acute medicine, 5 (7%) geriatric medicine and 3 (4%) cardiology, among other choices. Interests expressed in the survey were not representative of the actual speciality competition ratios [2]. Trainees choosing cardiology stated attractions to cardiology such as procedures, job experience and pathology, and barriers to interest in renal medicine such as lack of exposure to the speciality and work–life balance; however, the latter was not further elaborated.
Free-text comments
Trainees considering a career in renal medicine cited the speciality’s interesting pathology, physiology base, the mix of acute and chronic work, opportunity for procedures and effective lifesaving and prolonging interventions as positives.
Reasons cited against a career in renal medicine included the heavy workload, its complexity, a lack of previous exposure to the speciality, the preference of an alternate speciality and disinterest in taking on the role of a medical registrar. The free-text comments included one respondent who described the speciality as ‘complicated, intense, [with a] heavy workload [and that trainees and consultants] all look depressed’. Another respondent said that the ‘consultant body is generally not friendly’. One of the respondents had the impression that ‘the renal consultants are always in hospital’. A variety of suggestions to enhance attractiveness were given, including more clinical exposure, more teaching, more role models and a better lifestyle balance.
DISCUSSION
The increasing global burden of kidney disease, including the increasing number of patients with end-stage kidney disease, requires an increase in workforce. In the UK, there are 8.5 nephrologists per million population, which sits at the lower end among European countries [5]. While there has been an increase in advertised training posts in renal medicine between 2013 and 2017, from 43 to 66, there has been a decrease in the fill rate from 100% to 74% [6]. This is in contrast to other general medical specialities, such as cardiology and gastroenterology, which have similarly had an increase in training numbers to reflect workforce demands but have excelled at maintaining fill rates >95% [7, 8]. The reasons for the enduring popularity in these specialities are not apparent from our survey. Training pathways in these specialities are similar to renal medicine, with an equivalent length of training and hours worked per week. Moreover, fully trained cardiologists and gastroenterologists generally do more urgent out-of-hours interventional work than renal physicians, which we speculate could act as a lifestyle disincentive. Further qualitative research using techniques such as focus groups would be useful to identify job and lifestyle-specific aspects that enhance interest or act as barriers. It is notable, however, that fewer cardiology trainees (74%) dual accredit in general internal medicine when compared with renal trainees (87%) [9]. This may be due to greater availability of cardiology consultant jobs without general medicine commitments.
Our survey has demonstrated that trainees have limited exposure to renal medicine in medical school. This is supported both by trainees demonstrating limited clinical time spent and limited exposure to less common clinical domains of renal medicine, such as renal transplant, glomerulonephritis, renal genetic disease and renal procedures. Previous studies have cited a lack of early exposure as a cause for declining interest in renal medicine [10, 11]. We found that longer clinical exposure to renal medicine in medical school increased the proportion of trainees considering a career in the speciality. Trainees who were able to identify a role model were more likely to consider the speciality. We also found that postgraduate job exposure increased the likelihood of trainees considering a career in nephrology; however, this finding may be confounded by trainees who already have an interest in the speciality selecting advertised jobs that included it. It is key that we increase medical student and postgraduate exposure to renal medicine through a wide range of clinical experience delivered by enthusiastic renal physicians.
The majority of renal medicine trainees dual accredit in general internal medicine, taking on the role of the medical registrar. Very few FT trainees in this survey stated that they would consider a career as a medical registrar. A previous study found that the majority felt the work–life balance was a deterring factor [12, 13]. Even among CMT trainees, less than two-thirds stated that they would consider taking on the medical registrar role. This is considerably lower than the 76.5% figure found in a survey of 728 CMT trainees in 2011 and raises concern of a further decline in interest [13]. This is further compounded by increasing service demands in the NHS and trainees struggling to find dedicated time for teaching and training [14]. There is the need to make internal medicine more attractive and appealing through championing the role and improving the working environment [12]. Our finding that trainees selecting renal medicine as their first choice were unsure about training in general medicine would, however, arguably support the need to increase the opportunity for renal-only training programmes.
Furthermore, the traditional perception of renal medicine as an acute, academic, interventional speciality with a heavy workload leading to long hours may be a disincentive to recruitment, especially for those with flexible training needs. Currently very few registrars train flexibly [15]. Indeed, we found lower interest among female trainees and very few respondents found the speciality lifestyle friendly. Increasing flexibility could predictably increase the attractiveness of renal medicine. Urgent attention is required to address the recruitment struggles and drive interest in our speciality.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank all the trainees who participated in our survey as well as Lucy Higginbotham and Sarah Page, who helped with distribution of our questionnaire at induction.
FUNDING
This study received no direct funding. AHKK is supported by a NIHR academic clinical fellowship.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Daniels MN, Maynard S, Porter I. et al. Career interest and perceptions of nephrology: a repeated cross-sectional survey of internal medicine residents. PLoS One 2017; 12: e0172167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Competition Ratios. Health Education England 2017. https://specialtytraining.hee.nhs.uk/portals/1/Content/Resource%20Bank/Competition%20Ratio's/Competition%20Ratios%202017%20ST3.pdf (10 October 2018, date last accessed)
- 3. Lane CA, Brown MA.. Nephrology: a specialty in need of resuscitation? Kidney Int 2009; 76: 594–596 [DOI] [PubMed] [Google Scholar]
- 4. Jhaveri KD, Sparks MA, Shah HH. et al. Why not nephrology? A survey of US internal medicine subspecialty fellows. Am J Kidney Dis 2013; 61: 540–546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sharif MU, Elsayed ME, Stack AG.. The global nephrology workforce: emerging threats and potential solutions! Clin Kidney J 2016; 9: 11–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Royal College of Physicians. Renal Medicine – 2013–17 Fill Rates http://www.st3recruitment.org.uk/webapp/data/media/5a5662df0a32d_Renal_fill-rates_2013-17.pdf (2 March 2018, date last accessed)
- 7.Royal College of Physicians. Cardiology – 2013–2017 Fill Rates http://www.st3recruitment.org.uk/webapp/data/media/5a564a09e97b6_Cardio_fill-rates_2013-17.pdf cardiology recruitment (2 March 2018, date last accessed)
- 8.Royal College of Physicians. Gastroenterology – 2013–2017 Fill Rates http://www.st3recruitment.org.uk/webapp/data/media/5a565696350ad_Gastro_fill-rates_2013-17.pdf (2 March 2018, date last accessed)
- 9.Joint Royal Colleges of Physicians Training Board. Dual Training and Award of CCT in General (Internal) Medicine (GIM) and Medical Speciality https://www.jrcptb.org.uk/sites/default/files/Dual%20Training%20and%20award%20of%20CCT%20in%20General%20internal%20medicine%2001_10_14.pdf (5 December 2018, date last accessed)
- 10. Lane CA, Healy C, Ho MT. et al. How to attract a nephrology trainee: quantitative questionnaire results. Nephrology (Carlton) 2008; 13: 116–123 [DOI] [PubMed] [Google Scholar]
- 11. Owens S. The changing nephrology workforce. ASN Kidney News, 2009. https://www.asn-online.org/publications/kidneynews/archives/2009/KN_2009_04_jul.pdf (10 October 2018, date last accessed)
- 12. Chaudhuri E, Mason NC, Logan S. et al. The Medical Registrar Empowering the Unsung Heroes of Patient Care. London: Royal College of Physicians, 2013 [Google Scholar]
- 13. Chaudhuri E, Mason NC, Newbery N. et al. Career choices of junior doctors: is the physician an endangered species? Clin Med 2013; 13: 330–335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rimmer A. Junior doctors’ low morale is putting patients at risk, Royal College of Physicians warns. BMJ 2016; 355: i6493. [DOI] [PubMed] [Google Scholar]
- 15. Monson JP; Working Party of the Royal College of Physicians and the Renal Association. The changing face of renal medicine in the UK. Clin Med (Lond) 2007; 7: 103–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.