Introduction
Suicide is the second leading cause of death among United States youths ages 10-24, accounting for nearly 5000 deaths annually, more deaths than any single medical illness in this age group. Despite reductions in other causes of mortality, age-adjusted suicide death rates increased 24% from 1999 through 2014 and exceeded those from motor vehicle accidents among youth ages 10-14.1
Emergency Department (ED) visits offer a window of opportunity to deliver life-saving suicide prevention interventions.2 Estimates suggest that up to 25% of patients who visit EDs following suicide attempts (SAs) make another attempt, between 5-10% later die by suicide, and a substantial proportion of patients who die by suicide have ED visits during the year before death.2–4
This article focuses on the ED as a service delivery site for suicide prevention, and improving access to behavioral health care more generally. The term behavioral health (BH) is used throughout this article and refers broadly to health promotion related to mental health and substance use/addiction. The article proceeds in six sections. First, we discuss the ED as a site for suicide prevention. Second, we examine models for emergency services. Third, we review research on ED screening, therapeutic assessments, and brief interventions. Fourth, we turn to current ED practice guidelines and parameters. Fifth, we consider emergency care processes and offer a care process model of emergency services for suicide and self-harm (SU/SH). Finally, we offer conclusions and suggestions for future directions aimed at optimizing emergency care for SU/SH prevention.
The ED
EDs provide a safety net in the U.S. health system, due to federal law (the Emergency Medical Treatment and Labor Act) guaranteeing access to ED-care regardless of insurance or ability to pay. Roughly 1.5 million U.S. youth, particularly lower income individuals from underserved populations, receive their primary healthcare in the ED,3 and the prevalence of ED visits for BH has increased.5 Given this increased need for BH treatment within EDs, integrating BH within ED services has potential for suicide prevention in particular, and addressing unmet need for BH care more generally.
Despite the clear need and value of delivering effective BH-care in EDs, an Institute of Medicine report suggested that ED-care for children and adolescents may be substandard, and shortcomings in training and availability of staff with BH expertise contribute to quality of care problems.6 The ED setting poses challenges. EDs are often crowded, noisy, lack private space, and youths may be hesitant to honestly discuss sensitive issues with staff they just met. There are other medically and psychiatrically ill patients in the ED, which can be scary and uncomfortable.
Limitations of our health system also create challenges, increased costs, frustration, and lost time for youths and families. Shortages of psychiatric/BH staff and inpatient beds contribute to longer waiting times for BH versus general medical patients, often leading to youths leaving EDs without needed evaluations.7 While ED wait/boarding times vary, estimates indicate an average of 6.8 to 34 hours,7 with delays extending from hours to days when patients are waiting for hospital beds. This creates strains on EDs, patients, and families leading to negative experiences/attitudes about BH/psychiatric care.5
Models of Emergency Psychiatric/BH Care
Table 1 summarizes models of emergency care. These models have generally been established for adults, with little developmental adaptation, although some applications of the mobile crisis response and intensive community-based treatment models have been developed specifically for youth.8
Table 1.
Models of Emergency Psychiatric/Behavioral Health Care
| Care Model | Care Process |
|---|---|
| Consultant | BH specialists consult to ED |
| Psychiatric Emergency Services (PES) | BH service |
| Comprehensive Psychiatric Emergency Program (CPEP) | BH service, extended care options |
| Psychiatric Urgent Care | BH service, walk-in outpatient |
| Mobile Emergency Psychiatric Services | Emergency BH mobile team |
| Community Based Services | BH Team, available 24/7 |
The traditional ED consultant model is used in many hospitals. In this approach, when SU/SH risk is identified, a BH specialist, who consults to the ED, is called to do an assessment (now sometimes done using telepsychiatry).9,10 The BH consultant evaluates safety/imminent risk, followed by triage to appropriate levels of care based on evaluation results.9 Youths judged to be unsafe for outpatient care or needing further evaluation are generally admitted to inpatient care - either hospitalized on medical units when medical consequences of the SA/SH behavior require intervention, or if available, on psychiatric units when youths are medically stable. When risk is lower and youths are judged to be safe, patients are discharged home with rapid referral to outpatient care.
Major challenges with the consultant model include: shortages of BH consultants and psychiatric hospital beds, inadequate continuity of care, and low rates of post-discharge follow-up. With national statistics indicating that roughly half of youths presenting to EDs for SU/SH receive no outpatient treatment after discharge,11–13 improving continuity of care is a national priority (National Strategy for Suicide Prevention, Objective 8.4).14
Another model, the Dedicated Psychiatric Emergency Service (PES), uses stand-alone Psychiatric EDs, often affiliated with adjacent medical EDs. PES programs offer more extended observation/care (23-hour model) with the goal of stabilizing acute symptoms and avoiding hospitalization when safe/appropriate. While data are still limited and not fully consistent, a recent demonstration project in Alameda County indicated that a regional PES was associated with a substantially lower average boarding time (1 hour, 48 minutes) and an estimated 75% reduction in psychiatric hospitalizations.7
Expanding on the PES model, the Comprehensive Psychiatric Emergency Program (CPEP) provides more extended observation and care/treatment options. As implemented in New York state, CPEP programs are required to include:
hospital-based crisis intervention services in the ED, including triage, referral, and psychiatric and medical evaluations and assessments;
extended observation beds to provide evaluation, monitoring, and stabilization of acute symptoms for up to 72 hours;
crisis outreach services in the community; and
temporary residential and other required support services for ≤ five consecutive days.
State evaluation data suggest that the CPEP model has begun to address targeted quality of care problems and provide a range of treatment alternatives to hospitalization.15
Mobile emergency psychiatric services are included in the CPEP model, have been evaluated as a means of responding to psychiatric emergencies, and have shown promise for improving rates of outpatient follow-up care. One randomized controlled trial (RCT)16 with an adult CPEP population evaluating follow-up by a CPEP mobile crisis team, compared to clinic referral (similar services offered across programs), found that mobile crisis team patients were significantly more likely to receive an outpatient visit (69.6%), compared to patients in the clinic group (29.6%).16 Like other data questioning the value of community treatment as usual,17,18 linkage to treatment was not associated with improvements on measures of clinical or functioning outcomes.
Considerable work has been done on the intensive community based treatment model for youths. Importantly, a large RCT evaluating multisystemic therapy (MST), an intensive home and community-based treatment, compared to hospitalization for youths presenting with psychiatric emergencies, found advantages for MST on measures of functioning and symptoms including lower rates of youth-reported SH, relative to hospitalization, with lower costs.19,20 Other intensive community based treatments that aim to reduce SU/SH risk and minimize hospitalizations have also shown advantages in RCTs, relative to comparator conditions. These community-based treatments include: DBT, delivered as a 4 or 6-month program21,22; SAFETY, a 12-week DBT-informed cognitive-behavioral family treatment designed to be incorporated within emergency services23; and a 12-month Integrated-CBT with designed for youths with both suicidality and substance use problems.24 These interventions include intensive work with the family and youth and availability for emergency coaching.
The high costs and questionable effectiveness of traditional ED/hospital-based services have stimulated interest in the alternatives to the ED-Consultant model described above. More extensive evaluation and rigorously designed demonstration projects are needed.
Screeninq/Brief ED Interventions
All of the emergency service models begin with risk-screening/evaluation. Due to high acuity and limited resources, the most feasible and efficient approach is to use brief self-report screeners followed by more extensive evaluation for youths with positive screens. Such screeners, like the Ask Suicide-Screening Questions (ASQ), have shown predictive validity.25 Adaptive screening algorithms that ask additional questions after positive responses, combined with objective behavioral tasks,26 could enhance the accuracy and efficiency of screening, allowing more time for therapeutic intervention. Readers are referred elsewhere for more detailed review of screening strategies.27
Adding therapeutic components to ED-evaluations, can mitigate risk, stabilize patients, facilitate triage decisions, and improve continuity of care. Because low rates of post-discharge follow-up can make the ED the only point of BH care access, these therapeutic assessments (TAs) as described below can offer a “vital link in the suicidal patient’s chain of survival”.2
The Specialized Emergency Room (now ED) and second-generation Family Intervention for Suicide Prevention (ED/FISP)18,28,29 balance the need for evaluation and treatment using a brief behavioral assessment of imminent risk which evaluates the youth’s ability to generate behaviors incompatible with SU/SH, specifically:
recognizing personal strengths;
identifying ≥3 persons from whom to seek support;
discriminating emotional states and identifying SU/SH prompting situations using an “emotional thermometer”;
developing a SAFETY plan with concrete steps for safe-coping (activities, thoughts, behaviors, support persons);
committing to using the SAFETY plan versus SU/SH for a specified period.
Thus, the ED/FISP aims to develop/strengthen youths’ skills for down-regulating SU/SH urges, and mobilize support and feelings of connectedness within the family. The SAFETY plan is shared with parents/caregivers with the goals of facilitating parents/caregivers’ abilities to support the youth in using the safety plan, and support youths in accepting support. Parents and youths are counseled regarding the importance of restricting access to potentially lethal SH methods and dangers associated with disinhibition after substance use. The ED/FISP also aims to enhance motivation and commitment to attend follow-up treatment. After discharge, phone contacts are used (≤ 3 calls) to support linkage to follow-up care, through enhancing motivation and addressing barriers to care. This combination of strong family and youth components enhances youth skills and hopefulness, while also helping parents/caregivers to function like “protective seatbelts” if youths experience intense unbearable emotions and suicidal urges. In a RCT, when compared to usual ED care, the ED/FISP increased the likelihood of receiving outpatient services, with 92% of youths successfully linked to outpatient care. However, linkage to community outpatient treatment “as usual” was not associated with improved clinical outcomes.18 Alternatively, in two trials where the initial ED/FISP was combined with guaranteed access to a structured cognitive-behavioral family intervention, clinical outcomes were improved.23,28 Indeed, when incorporated as a first in-home session within the SAFETY Program (a cognitive-behavioral family treatment designed to be incorporated within emergency services for youths presenting with SAs/SH), the intervention was associated with significantly lower risk of SAs, supporting the benefits of the intervention for protecting against future SAs.23
Another TA17 used a 30-minute cognitive-analytic intervention (with parent involvement when possible) and featured:
construction of a diagram incorporating three elements - reciprocal roles, core pain, and maladaptive processes;
identification of a target problem contributing to suicidality;
generating possible “exits” from the problem; and
writing an “understanding letter” that summarizes the diagram and exits.
In an RCT, TA youth were significantly more likely to attend a first outpatient follow-up appointment and ≥ four treatment sessions, than youths receiving usual ED-care.17 However, again, there were no between-group differences in clinical outcomes.
The Compliance Enhancement Intervention30 is a brief motivational enhancement intervention with youths and parents that includes:
review of treatment expectations/misconceptions;
problem-solving treatment barriers; and
a verbal contract to attend ≥ four outpatient sessions.
After ED-discharge, separate phone calls to youths and parents (weeks 1,2, 4, 8) assess suicidality, enhance motivation for care, and assist with problem-solving treatment barriers. RCT results indicate that at 3-months post-discharge, intervention youths attended significantly more treatment sessions than usual care youths, controlling for treatment barriers (e.g., insurance coverage, waiting lists).
Similarly, the TeenScreen-ED31 intervention aims to enhance motivation and address treatment barriers, by scheduling an outpatient appointment and sending appointment reminders. RCT results indicate that intervention youths were significantly more likely to attend a mental health appointment by 60 days post-discharge, relative to comparison youths receiving standard referrals.31
Teen Options for Change (TOC),32 another motivational enhancement intervention, targets adolescents presenting to EDs for non-psychiatric complaints screening positive for suicide-risk. TOC combines personalized feedback on normative risk factors (e.g. suicidal ideation, substance use) with identification of youths’ values/behavioral goals and development of personalized action plans for achieving goals. Follow-up contacts by handwritten note plus phone check-ins during the five days post-discharge support youths with action plan implementation. In a randomized trial, when compared to usual ED-care, TOC youths showed greater reductions in depression at 2-months post-discharge; however, groups were similar in rates of BH service use. Here, it is important to note, that unlike the other TAs/interventions, TOC emphasized youth outcomes, with less attention to improving rates of post-ED care.
Caring contacts using non-demanding letters/postcards after ED discharge has been emphasized with adults given evidence indicating reduced suicide deaths, SAs, and ED visits.33,34 However, evaluations with adolescents are limited to one study with negative results35 and the inclusion of a limited number of older adolescents (typically >16 years) in adult samples.
Current Guidelines and Practice Parameters
Practice guidelines, as a representation of evidenced-based practice, have achieved substantial credibility in medicine, are an integral part of emergency medicine, and combined with training can help improve quality of care. Guidelines are available online, and a Committee of the American College of Emergency Physicians (ACEP) develops and reviews published guidelines (http://www.acepnow.com/tag/clinical-guidelines/).
Available clinical guidance emphasizes adults. Consensus guidelines for adults were developed by the Suicide Prevention Resource Center (2015) and support clinicians with decisions, initial intervention, and discharge planning (http://www.sprc.org/resources-programs/caring-adult-patients-suicide-risk-consensus-guide-emergency-departments). A 2016 Clinical Policy article (https://www.acep.org/Clinical---Practice-Management/ACEP-Current-Clinical-Policies/) summarizes evidence on the management of adult suicidal patients.36
Recent guidance on SU/SH risk in children/adolescents is limited. The AACAP practice parameters date from 2001(http://www.jaacap.com/article/S0890-8567(09)60355-5/pdf). Other recommendations/reports focus on ED management of pediatric mental health crises, including two clinical reports37,38 supporting previous joint policy statements of the American Academy of Pediatrics (AAP) and ACEP on pediatric mental health emergencies, and one 2015 review including recommendations for youths with SU/SH.10
Although these practice guidelines/parameters/recommendations have differences, they generally emphasize evaluation and assessment of risk levels; triage/management to prevent death/injury;continuity of care; restricting access to dangerous SU/SH methods; and treatment of BH conditions.
Universal screening of all ED patients is controversial. Current Joint Commission on Accreditation of Healthcare Organizations (JCAHO) standards require that all patients in psychiatric EDs and patients presenting with psychiatric symptoms to general EDs be screened for suicidality.39 This standard does not require universal screening for suicidality in medical EDs. Further, the US Preventive Services Task Force’s review concluded that current evidence is insufficient to recommend for or against primary care screening for suicide risk (https://www.uspreventiveservicestaskforce.org/).
Care Process Model for Youths Presenting with SU/SH Risk
Figure 1 presents a care process model for youths presenting to ED/emergency services with SU/SH, based on evidence and clinical guidance reviewed above. This process begins when patients with suspected SU/SH risk are identified, at which time safety precautions are needed, including close monitoring in a safe setting to prevent SU/SH and/or patients leaving without evaluation. Secondary screening and medical clearance is conducted by ED staff, which may lead ED clinicians to request psychiatric/BH consultation. The youth and family should be informed about what will be done in the ED in a “collaborative therapeutic assessment and planning process.” For child/adolescent patients it is critical that the evaluation include both the youth’s condition/characteristics and environmental risk and protective factors. Because youth may deny and minimize symptoms, sometimes in response to fears that accurate reporting of SU/SH may lead to hospitalization, it is critical to obtain information from parents/caregivers about suicidality and other risk and protective factors. When imminent risk is a concern, the top priority is patient safety. Clinicians may disclose information to protect youths, while following existing laws and HIPAA regulations. However, collaborating with youths to help them share information or gaining their permission for disclosure can enhance trust and therapeutic interactions. Disclosing information can increase risk by increasing stress or shame in the youth and/or family, requiring careful consideration of potential consequences and protective action as needed.
Figure 1.
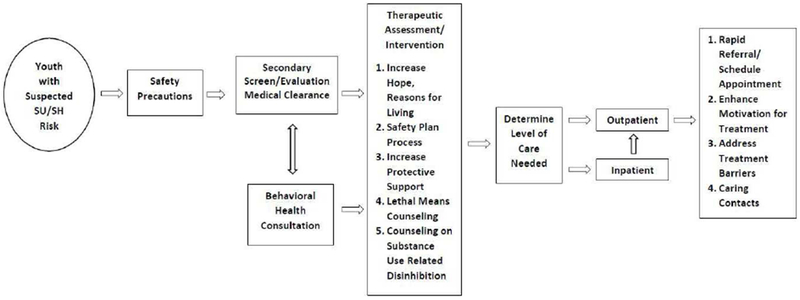
Care process model for youths presenting with suicide and self-harm risk.
Courtesy of J. Asarnow, PhD, Los Angeles, CA.
Clinicians should assess the chain of events leading to presenting SU/SH events, the consequences of the SU/SH event, and identify behaviors, thoughts, and support persons that youths can turn to if he/she experiences SU/SH urges again. As in the ED/FISP, and other DBT/CBT approaches, this assessment can be used to develop a SAFETY plan, practice the plan, obtain a commitment to use the plan, and trouble-shoot potential obstacles.21–23 There are a number of resources to help with SAFETY planning.40 This differs from a “no suicide contract” which has not been proven effective.40 Youths’ primary care providers and BH providers should be considered as potential support persons, and 24/7 crisis services (e.g. National Suicide Prevention Lifeline) should be included. Efforts are needed to enhance protective support, including: increasing supportive listening and communication between youths and parents/caregivers; increasing protective monitoring of the youth; counseling parents and youths about the importance of restricting access to dangerous SH methods (questions about guns and ammunition should be asked of parents alone to ensure that youth does not learn how to access); and counseling of parents and youths regarding the potential dangers of disinhibition due to substance use. Work aimed at strengthening motivation to pursue follow-up treatment and addressing barriers to care is important for all youth and families. For youth discharged home, outpatient referral should be facilitated, scheduled before discharge if possible and within the next 7 days (best within 24 hours). Treatment barriers should also be identified and addressed. Post-discharge contact to enhance motivation for care and address treatment barriers have been shown to contribute to increased likelihood of follow-up treatment17,18,28 and non-demanding caring contacts (e.g. calls, postcards, email, texts) can be automated and may improve outcomes.40
A critical issue for this process is whether BH care can be integrated within ED workflow patterns. This is important because EDs are often busy, with multiple priorities and limited BH resources.41,42 Enhanced BH training will provide part of the solution, improving comfort and skill among ED staff and enabling more emergency clinicians to perform initial evaluations, determine the need for consultation, and deliver some brief interventions, as they do for other medical conditions. For instance when patients come to EDs with chest pain, ED clinicians routinely complete initial risk evaluations/stratifications and with guidance from consultants decide on treatment and disposition.41 A “connected” psychiatric/BH service can provide consultation to ED clinicians (live or through telemedicine), and when needed evaluate patients. There will still be patients that need more thorough psychiatric/BH evaluation and these patients will need to be transferred to facilities that have these resources.
Medical and psychiatric EDs with onsite/co-located BH services can more easily integrate interventions for SU/SH, with BH staff delivering the intervention. This could involve regular ED-BH staff, or specialized “suicide prevention crisis teams”. Ideally, there is some integration of medical and BH care and communication/collaboration to provide effective care, and clear consistent messages to patients and families.
Finally, the Zero suicide (ZS; http://zerosuicide.sprc.org/) initiative aims to improve care within health systems, including EDs, to achieve the aspirational goal of ZS within defined health system populations.41 Grounded in the belief that suicide deaths among individuals receiving care in health/BH systems can be prevented, ZS practices align culture and care to address suicide-risk as a threat to health and a health system responsibility. Core elements of ZS practices include:
a leadership-driven, safety-oriented culture committed to reducing suicide and involving SA and loss survivors;
systematic identification and evaluation of suicide-risk levels;
timely and adequate pathways to care;
a competent, confident, and caring workforce;
evidence-based care, including collaborative safety planning, restriction of lethal means, and effective treatment of suicidality;
continued contact/support, especially after acute care; and
data-driven quality improvement.
This whole system approach has strong potential for addressing many of the problems discussed above, like inadequate continuity of care.
Conclusions
EDs can offer life-saving suicide prevention care, yet hospital-based ED care is at a breaking point and under-resourced to serve as a safety net for youth with BH problems.6 This article reviewed characteristics of EDs, models of emergency care, ED screening/evaluation and intervention models, and practice guidelines/parameters. We offered a care process model for youths presenting with SU/SH risk with guidance for clinicians based on current scientific evidence. While recent service trends are shifting from medical EDs to alternative models that emphasize psychiatric/BH specialty care and community-based services, our care process model can be incorporated within these different models. The trend to community-based emergency services is likely motivated by the high costs of ED and hospital-based care, and accumulating data supporting advantages of community-based care.19–24 Nevertheless, there will continue to be youths seen in EDs for SU/SH and other BH problems. It is critical, therefore, that the emergency infrastructure be strengthened through: training and building comfort and skill among ED clinicians in evaluating/managing suicidal patients; addressing shortages of psychiatric/BH specialists with child/adolescent expertise; and increasing availability of effective inpatient and outpatient services. Although effective strategies for youth SU/SH prevention are emerging from the scientific literature, youth suicide rates are not decreasing. It is time to put our knowledge to work and bring evidence-based care to emergency and community services.
KEY POINTS.
Emergency services can offer life-saving suicide prevention care.
Brief therapeutic interventions initiated in the ED for youths presenting with suicide/self-harm risk can improve continuity of care/connections to outpatient follow-up treatment, a national suicide prevention objective.
A care process model and clinical guidance are offered based on current scientific evidence.
Effective treatment strategies for youth suicide/self-harm prevention are emerging from the scientific literature; increasing availability of these treatments in community settings is crucial for advancing suicide prevention goals.
SYNOPSIS.
Emergency departments can offer life-saving suicide prevention care. This article focuses on the Emergency Department and emergency services as service delivery sites for suicide prevention. Characteristics of EDs, models of emergency care, ED screening and brief intervention models, and practice guidelines/parameters are reviewed. A care process model for youths with suicide/self-harm-risk is presented, with guidance for clinicians based on the scientific evidence. Strengthening emergency infrastructure and integrating effective suicide prevention strategies derived from scientific research are critical for advancing suicide prevention objectives.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE STATEMENT
Dr. Asarnow discloses consulting on quality improvement for depression and suicide prevention.
Drs. Babeva and Horstmann have nothing to disclose.
Contributor Information
Joan Rosenbaum Asarnow, David Geffen School of Medicine, Semel Institute for Neuroscience & Human Behavior, University of California, Los Angeles, United States.
Kalina Babeva, Department of Psychiatry & Biobehavioral Sciences, Semel Institute for Neuroscience & Human Behavior, University of California, Los Angeles, United States.
Elizabeth Horstmann, Department of Psychiatry & Biobehavioral Sciences, Semel Institute for Neuroscience & Human Behavior, University of California, Los Angeles, United States.
References
- 1.Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999-2014. NCHS data brief. http://www.cdc.gov/nchs/products/databriefs/db241.htm Published 2016. Accessed April 7, 2017. [PubMed]
- 2.Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1–6. doi: 10.1027/0227-5910/a000001. [DOI] [PubMed] [Google Scholar]
- 3.Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolesc Med 2000;154(4):361–365. doi: 10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]
- 4.Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: Retrospective study. Br J Psychiatry. 2003;183(JULY):28–33. doi: 10.1192/bjp.183.1.28. [DOI] [PubMed] [Google Scholar]
- 5.Dolan MA, Fein JA, Committee on Pediatric Emergency Medicine. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics. 2011. ;127(5):e1356–e1366. doi: 10.1542/peds.2011-0522. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine, Board on Health Care Services, Committee on the Future of Emergency Care in the United States Health System. Hospital-Based Emergency Care: At the Breaking Point. Washington, D.C.: National Academies Press; 2007. doi: 10.17226/11621. [DOI] [Google Scholar]
- 7.Zeller S, Calma N, Stone A. Effects of a dedicated regional psychiatric emergency service on boarding of psychiatric patients in area emergency departments. West J Emerg Med 2014;15(1):1–6. doi: 10.5811/westjem.2013.6.17848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janssens A, Hayen S, Walraven V, Leys M, Deboutte D. Emergency psychiatric care for children and adolescents: a literature review. Pediatr Emerg Care. 2013;29(9):1041–1050. doi: 10.1097/PEC.0b013e3182a393e7. [DOI] [PubMed] [Google Scholar]
- 9.Betz ME, Boudreaux ED. Managing Suicidal Patients in the Emergency Department. Ann Emerg Med 2016;67(2):276–282. doi: 10.1016/j.annemergmed.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chun TH, Katz ER, Duffy SJ, Gerson RS. Challenges of managing pediatric mental health crises in the emergency department. Child Adolesc Psychiatr Clin N Am 2015;24(1):21–40. doi: 10.1016/j.chc.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Doshi A, Boudreaux ED, Wang N, Pelletier AJ, Camargo CA Jr National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997-2001. Ann Emerg Med 2005;46(4):369–375. doi: 10.1016/j.annemergmed.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 12.Olfson M, Gameroff MJ, Marcus SC, Greenberg T, Shaffer D. Emergency treatment of young people following deliberate self-harm. Arch Gen Psychiatry. 2005;62(10):1122–1128. doi: 10.1001/archpsyc.62.10.1122. [DOI] [PubMed] [Google Scholar]
- 13.Hughes JL, Anderson NL, Wiblin JL, Asarnow JR. Predictors and outcomes of psychiatric hospitalization in youth presenting to the emergency department with suicidality. Suicide Life-Threatening Behav 2016;47(April):193–204. doi: 10.1111/sltb.12271. [DOI] [PubMed] [Google Scholar]
- 14.Office of the Surgeon General, National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, D.C.: US Department of Health and Human Services; 2012. http://nbda.com/articles/industry-overview-2012-free-version-pg34.htm. [PubMed] [Google Scholar]
- 15.New York State Office of Mental Health. Annual report to the governor and legislature of New York State on comprehensive psychiatric emergency programs. NYS Office of Mental Health. https://www.omh.ny.gov/omhweb/statistics/cpep_annual_report/2012.pdf Published 2012. Accessed April 7, 2017.
- 16.Currier GW, Fisher SG, Caine ED. Mobile crisis team intervention to enhance linkage of discharged suicidal emergency department patients to outpatient psychiatric services: A randomized controlled trial. Acad Emerg Med 2010;17(1):36–43. doi: 10.1111/j.1553-2712.2009.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ougrin D, Zundel T, Ng A, Banarsee R, Bottle A, Taylor E. Trial of Therapeutic Assessment in London: Randomised controlled trial of Therapeutic Assessment versus standard psychosocial assessment in adolescents presenting with self-harm. Arch Dis Child. 2011. ;96(2):148–153. doi: 10.1136/adc.2010.188755. [DOI] [PubMed] [Google Scholar]
- 18.Asarnow JR, Baraff LJ, Berk M, et al. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatr Serv 2011. ;62(11):1303–1309. doi: 10.1176/appi.ps.62.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henggeler SW, Schoenwald SK, Rowland MD, Cunningham PB. Serious Emotional Disturbance in Children and Adolescents: Multisystemic Therapy. New York, NY: The Guilford Press; 2002. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc4&NEWS=N&AN=2002-18214-000. [Google Scholar]
- 20.Huey SJ, Henggeler SW, Rowland MD, et al. Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. J Am Acad Child Adolesc Psychiatry. 2004;43(2):183–190. doi: 10.1097/00004583-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Mehlum L, Tormoen AJ, Ramberg M, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: A randomized trial. J Am Acad Child Adolesc Psychiatry. 2014;53(10):1082–1091. doi: 10.1016/j.jaac.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 22.Linehan MM, McCauley E, Berk MS, et al. Dialectical behavior therapy compared to supportive treatment: A randomized controlled trial for adolescents at high risk for suicide. Paper presented at: 50th Annual Convention of the Association for Behavorial and Cognitive Therapies; October 28, 2016; New York, NY. [Google Scholar]
- 23.Asarnow JR, Hughes JL, Babeva KN, Sugar CA. Cognitive-behavioral family treatment for suicide attempt prevention: A randomized controlled trial. J Am Acad Child Adolesc Psychiatry. In press. doi: 10.1016/j.jaac.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized trial. J Consult Clin Psychol 2011. ;79(6):728–739. doi: 10.1037/a0026074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horowitz LM, Bridge JA, Teach SJ, et al. Ask Suicide-Screening Questions (ASQ): A brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med 2012;166(12):1170–1176. doi: 10.1001/archpediatrics.2012.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, Banaji MR. Measuring the suicidal mind: implicit cognition predicts suicidal behavior. Psychol Sci 2010;21 (4):511–517. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Babeva K, Hughes JL, Asarnow J. Emergency department screening for suicide and mental health risk. Curr Psychiatry Rep 2016;18(11). doi: 10.1007/s11920-016-0738-6. [DOI] [PubMed] [Google Scholar]
- 28.Rotheram-Borus MJ, Piacentini J, Cantwell C, Belin TR, Song J. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. J Consult Clin Psychol 2000;68(6):1081–1093. doi: 10.1037/0022-006X.68.6.1081. [DOI] [PubMed] [Google Scholar]
- 29.Asarnow JR, Berk MS, Baraff LJ. Family Intervention for Suicide Prevention: A specialized emergency department intervention for suicidal youths. Prof Psychol Res Pract 2009;40(2):118–125. doi: 10.1037/a0012599. [DOI] [Google Scholar]
- 30.Spirito A, Boergers J, Donaldson D, Bishop D, Lewander W. An intervention trial to improve adherence to community treatment by adolescents after a suicide attempt. J Am Acad Child Adolesc Psychiatry. 2002;41(4):435–442. doi: 10.1097/00004583-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Grupp-Phelan J, McGuire L, Husky MM, Olfson M. A randomized controlled trial to engage in care of adolescent emergency department patients with mental health problems that increase suicide risk. Pediatr Emerg Care. 2012;28(12):1263–1268. doi: 10.1097/PEC.0b013e3182767ac8. [DOI] [PubMed] [Google Scholar]
- 32.King CA, Gipson PY, Horwitz AG, Opperman KJ. Teen options for change: an intervention for young emergency patients who screen positive for suicide risk. Psychiatr Serv 2015;66(1):97–100. doi: 10.1176/appi.ps.201300347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv 2001. ;52(6):828–833. doi: 10.1176/appi.ps.52.6.828. [DOI] [PubMed] [Google Scholar]
- 34.Carter GL, Clover K, Whyte IM, Dawson AH, D’Este C. Postcards from the EDge: 5-year outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Psychiatry. 2013;202(5):372–380. doi: 10.1192/bjp.bp.112.112664. [DOI] [PubMed] [Google Scholar]
- 35.Robinson J, Yuen HP, Gook S, et al. Can receipt of a regular postcard reduce suicide-related behaviour in young help seekers? A randomized controlled trial. Early Interv Psychiatry. 2012;6(2):145–152. doi: 10.1111/j.1751-7893.2011.00334.x. [DOI] [PubMed] [Google Scholar]
- 36.American College of Emergency Physicians Clinical Policies Subcommittee. Clinical policy: critical issues in the diagnosis and management of the adult psychiatric patient in the emergency department. Ann Emerg Med 2017;69(4):480–498. doi: 10.1016/j.annemergmed.2017.01.036. [DOI] [PubMed] [Google Scholar]
- 37.Chun TH, Mace SE, Katz ER, American Academy of Pediatrics Committee on Pediatric Emergency Medicine, American College of Emergency Physicians Pediatrics Emergency Medicine Committee. Evaluation and management of children and adolescents with acute mental health or behavioral problems. Part I: Common clinical challenges of patients with mental health and/or behavioral emergencies. Pediatrics. 2016;138(3):980–989. doi: 10.1542/peds.2016-1570. [DOI] [Google Scholar]
- 38.Chun TH, Mace SE, Katz ER, American Academy of Pediatrics Committee on Pediatric Emergency Medicine, American College of Emergency Physicians Pediatrics Emergency Medicine Committee. Evaluation and management of children with acute mental health or behavioral problems. Part II: Recognition of clinically challenging mental health related conditions presenting with medical or uncertain symptoms. Pediatrics. 2016;34(3):643–660. doi: 10.1542/peds.2016-1573. [DOI] [PubMed] [Google Scholar]
- 39.Joint Commission on Accreditation of Healthcare Organizations. National patient safety goals. http://www.jointcommission.org/assets/1/6/2015_NPSG_HAP.pdf Published 2015. Accessed April 7, 2017.
- 40.Capoccia L, Labre M. Caring for adult patients with suicide risk: A consensus-based guide for emergency departments. Suicide Prevention Resource Center; http://www.sprc.org/resources-programs/caring-adult-patients-suicide-risk-consensus-guide-emergency-departments Published 2015. Accessed April 7, 2017. [Google Scholar]
- 41.Betz ME, Wintersteen M, Boudreaux ED, et al. Reducing suicide risk: Challenges and opportunities in the emergency department. Ann Emerg Med 2016;68(6):758–765. doi: 10.1016/j.annemergmed.2016.05.030. [DOI] [PubMed] [Google Scholar]
- 42.Baraff LJ, Janowicz N, Asarnow JR. Survey of California emergency departments about practices for management of suicidal patients and resources available for their care. Ann Emerg Med 2006;48(4). doi: 10.1016/j.annemergmed.2006.06.026. [DOI] [PubMed] [Google Scholar]


