Abstract
One of the biggest current challenges in managing an ageing cohort living with the HIV is handling dyslipidaemia, diabetes, metabolic syndrome and nonalcoholic fatty liver disease. Combination antiretroviral therapy decrease mortality and morbidity in HIV patients, but lead to increase in insulin resistance, dyslipidaemia, abnormalities of fat distribution and high risk of cardiovascular disease. Therefore, a metabolic clinic was established for individuals living with HIV in the Milton Keynes University Hospital NHS Foundation Trust. The clinic meets considerable demands by service users and hence has the potential to be popular. This review focuses on the importance of the development of a metabolic clinic for the purpose of audit, research, teaching and exchange of knowledge between HIV specialists and the metabolic team in the management of complex cases. Therefore, the metabolic clinic should be an integral part of HIV services especially as the cohort of the ‘older’ HIV population increases.
Keywords: dyslipidaemia, human immunodeficiency virus, insulin resistance, metabolic clinic
Introduction
HIV per se can lead to diabetes, dyslipidaemia and nonalcoholic fatty liver disease (NAFLD); therefore, it is not surprising that HIV showed an independent effect on cardiovascular risk 1–3. Each of these metabolic factors was also reported with the administration of combination antiretroviral therapy (cART) 2,4,5. For instance, dyslipidaemia is reported in around 82.3% of HIV patients receiving antiretroviral medication 6. Furthermore, in addition to dyslipidaemia, the cART medication in HIV patients is associated with an increase in the prevalence of insulin resistance and diabetes 6–8. The increase in the ageing population of HIV patients may also lead to an increase in the incidence of cardiovascular disease (CVD). The prevalence of CVD was found to be around 23% in elderly individuals with HIV 5. It is well recognized that HIV is a multisystem disorder and this may significantly lead to an increase in mortality. One study showed an increased percentage of death attributable to cardiac, renal and hepatic disease among HIV patients treated with cART 5. The aim of this article is to review the challenges of obesity, dyslipidaemia, diabetes and NAFLD in HIV patients and the potential benefits of metabolic clinic as an integral part of HIV services.
Diabetes mellitus, metabolic syndrome and HIV
Several studies from Africa, the Far East and South America showed an increase in the prevalence of insulin resistance and diabetes in particular with cART 9–13. In one study, the prevalence of diabetes mellitus was 2.1% 14. The prevalence of diabetes in Western HIV populations ranges from 2.6 to 14% in those with treated HIV in various cohort studies 15. Importantly, pre-existing hypertension, obesity and diabetes increased the risk of dyslipidaemia or the changes in body configuration associated with cART such as central obesity, truncal obesity and lipoatrophy, and these may all increase the risk of diabetes mellitus 16. This is likely because of the fact that HIV represents a chronic inflammatory condition and this may lead to both dyslipidaemia and insulin resistance 17. HIV and cART medication may impair lipid metabolism and increase triglycerides and the risk of insulin resistance. Furthermore, increased oxidative stress, impaired function of adipokines and transcript factors (adiponectin, leptin, sterol regulatory-binding proteins and peroxisomal proliferatory activator receptors α and γ lipoatrophy and lipohypertrophy) may also lead to insulin resistance and diabetes 7,18–20. Importantly, protease inhibitors (PIs) are not only associated with dyslipidaemia because of mitochondrial toxicity but also hyperglycaemia because of inhibition of glucose transporter type 4, and this leads to inhibition of adipocyte differentiation and an increase in triglyceride levels and insulin resistance 21. Furthermore, treatment with PI and nucleoside reverse-transcriptase inhibitor (NRTI)-containing regimens was associated with the risk of development of type 2 diabetes mellitus 22.
Dyslipidaemia in HIV patients
High cholesterol and triglycerides and low high-density lipoprotein (HDL) are common features of HIV dyslipidaemia 18. Common medications used in the treatment of HIV are PIs, NRTIs and non-NRTIs 23, and these can also precipitate dyslipidaemia. For instance, administration of cART is associated with decreased HDL-c, increased very low-density lipoprotein (LDL) and increased total cholesterol. PI-based regimes are associated with incidences of dyslipidaemia in 70 and 80% of patients in the form of high triglycerides, LDL and decreased HDL-c and accumulation of Apo-E and Apo-C III 24. PIs are also associated with central obesity, lipoatrophy and insulin resistance 25. The PIs mediate this effect through inhibition of lipogenesis, adipocyte differentiation and decrease in the hepatocyte clearance of hepatic chyliomicron and very LDL and stimulation of hepatic synthesis of triglycerides 24. Other medications such as NRTIs are also associated with high triglycerides and lipoatrophy, apart from tenofovir, which appears to be a good choice when dyslipidaemia is an issue with the administration of NRTIs 25. Furthermore, NRTIs such as abacavir and didanosine are associated with an independent risk of myocardial infarction in the Data Collection on Adverse Events of Anti-HIV Drug (DAD) study 4, whereas nevirapine protected against low HDL-c level and efavirenz is associated with an increase in total cholesterol and triglycerides 26. Pravastatin, atorvastatin and rousvastatin are good choices in the treatment of HIV dyslipidaemia.
Nonalcoholic fatty liver disease and HIV
The presence of insulin resistance, dyslipidaemia and lipoatrophy are all precursor factors that lead to the development of NAFLD, which refers to a wide spectrum of liver damage, ranging from simple steatosis to steatohepatitis, advanced fibrosis and cirrhosis 27. The estimated prevalence of NAFLD in a population without HIV is believed to be around 25–35% worldwide 28. The prevalence of NAFLD in Asian patients with HIV is estimated to be around 31% and was associated with high BMI, dyslipidaemia and a high alanine aminotransferase/aspartate aminotransferase ratio 29. In a population-based study, the prevalence of NAFLD was found to be around 26% and associated with an increase in γ-glutamyl transpeptidase and insulin resistance 30. Importantly, HIV patients with hepatitis C can also have NAFLD 31,32. Furthermore, NAFLD gained significant scientific attention because of the fact that it is considered a common and fast-growing liver disease worldwide, with an increase in both mortality and morbidity 28. The association between NAFLD and HIV and antiretroviral treatment has been reported in several studies 33–35. This is likely because of the association of NAFLD with insulin resistance and the high risk of CVD and dyslipidaemia 26,27. NAFLD is common in HIV patients and is associated with greater visceral adiposity and insulin resistance 36. The only effective therapy for NAFLD is weight loss and the use of statin with NAFLD appears to be safe and effective.
Cardiovascular risk and HIV disease
The increase in the risk of CVD in HIV patients was shown in several studies. In the DAD study 4 that investigated the impact of diabetes and pre-existing coronary heart disease (CHD) on the development of a new CHD episode among 33 347 HIV-infected individuals, it was shown that the rate of a CHD episode was 7.52 times higher in those with pre-existing CHD than in those without pre-existing CHD, but it was only 2.41 times higher in those with pre-existing diabetes mellitus compared with those without diabetes mellitus 37. The DAD study also showed that the prevalence of metabolic syndrome increased from 19.4 to 41.6% within 6 years 38. Triant et al. 39 showed that HIV is associated with an increased incidence of acute myocardial infarction in HIV patients in comparison with non-HIV patients, and this is likely because of the higher prevalence of hypertension, diabetes and dyslipidaemia in the HIV cohort. Importantly, PIs are also associated with a higher risk of incidence of myocardial infarction and this in part because of dyslipidaemia 40. Because of the fact that individuals with HIV live longer, an increase in comorbidities such as diabetes, dyslipidaemia, chronic kidney disease, hypertension and CVD was noted 14. It is plausible to suggest that this will lead to a significant burden on health resources in the near future unless correct strategies are planned carefully. Therefore, we have established the metabolic clinic as part of the integral HIV services in Milton Keynes University Hospital and it is one of the leading metabolic clinics for HIV patients in UK.
Why is it important to establish metabolic clinics for HIV patients?
The metabolic clinic in Milton Keynes University Hospital is a weekly clinic that runs within the HIV clinic. Patients see a specialist in metabolic medicine and a dietician. A thirty minute meeting before the beginning of the clinic is allocated for discussion of cases between the metabolic team and HIV consultants. At present, this is not a referral clinic, but is part of the future expansion of the services. It is funded by the National Health Service and the system is currently sustainable. The ‘inclusion criteria’ for entry into the metabolic clinic are as follows:
over weight and obesity,
underweight,
hypertension,
dyslipidaemia,
diabetes,
nonalcoholic fatty liver disease,
hypogonadism and low testosterone,
other endocrine disorders such as (high calcium, thyroid dysfunction).
Recently, a cardiology clinic was established for HIV patients in London 41. It is possible to suggest that a more specialist input (nephrology, neurology and oncology) will be a part of the HIV services. Several factors can be counted for why it is important to establish a metabolic clinic:
Running a metabolic clinic within the same HIV department makes patients feel more comfortable with the same staff who care for their HIV management in a seamless way.
A metabolic clinic reviews HIV patients with dyslipidaemia, type 2 diabetes, metabolic syndrome and obesity, NAFLD, hypogonadism and impotence, and we also recommend treatment for HIV patients with definitive cardiovascular risk factors (Fig. 1). As the clinic is relatively new (2 years old), we are in the process of establishing a guideline for patients with multimorbidity.
A metabolic database is available for the purpose of auditing, research and teaching.
The clinic provides a platform for exchange of ideas and knowledge between HIV specialists and the metabolic team, especially for the management of complex dyslipidaemia and CVD. The infectious disease physician is also a part of the multidisciplinary team meeting team in managing HIV and medications as part of the metabolic disease.
Fig. 1.
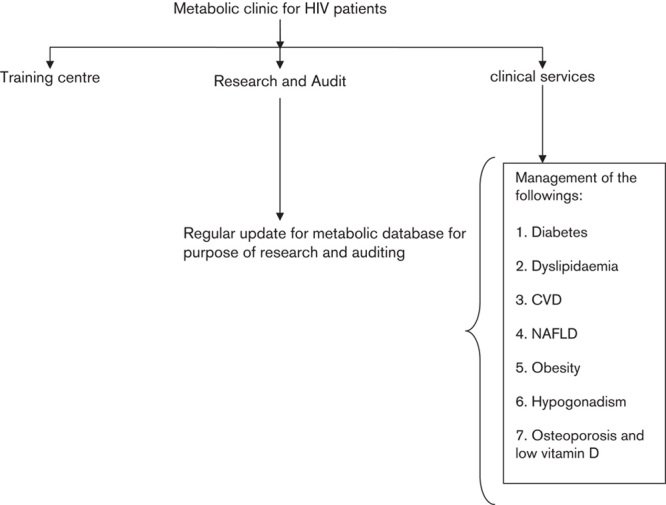
Illustration of the different roles of metabolic clinic for HIV patients. CVD, cardiovascular disease, NAFLD, nonalcoholic fatty liver disease.
Conclusion
HIV patients live longer and encounter a series of challenging metabolic disorders such as diabetes, obesity, dyslipidaemia, NAFLD, vitamin D deficiency and increased risk of CVD. The dyslipidaemia can be because of HIV infection or may be induced by HIV medication. The metabolic clinic will not only meet the clinical demand for clinical services but also provide a useful opportunity to collect data for future clinical research and auditing. In view of the fact that we will soon face the challenge of an ageing population of HIV patients, the metabolic clinic could also be used to train future HIV physicians/metabolic medicine physicians/endocrinologists and elderly care physicians in the management of these complex metabolic disorders (Fig. 1).
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zou W, Berglund L. HIV and highly active antiretroviral therapy: dyslipidemia, metabolic aberrations, and cardiovascular risk. Prev Cardiol 2007; 10:96–103. [DOI] [PubMed] [Google Scholar]
- 2.Mallewa JE, Higgins SP, Garbett S, Saxena N, Vilar FJ. Cardiovascular disease risk management in HIV patients, experiences from Greater Manchester. Int J STD AIDS 2009; 20:425–426. [DOI] [PubMed] [Google Scholar]
- 3.Calza L, Colangeli V, Manfredi R, Bon I, Re MC, Viale P. Clinical management of dyslipidaemia associated with combination antiretroviral therapy in HIV-infected patients. J Antimicrob Chemother 2016; 71:1451–1465. [DOI] [PubMed] [Google Scholar]
- 4.Sabin CA, Worm SW, Weber R, Reiss P, El-Sadr W, Dabis F, et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet 2008; 371:1417–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Penzak SR, Chuck SK, Stajich GV. Safety and efficacy of HMG-CoA reductase inhibitors for treatment of hyperlipidemia in patients with HIV infection. Pharmacotherapy 2000; 20:1066–1071. [DOI] [PubMed] [Google Scholar]
- 6.Hejazi N, Rajikan R, Choong CL, Sahar S. Metabolic abnormalities in adult HIV infected population on antiretroviral medication in Malaysia: a cross-sectional survey. BMC Public Health 2013; 13:758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grinspoon SK, Grunfeld C, Kotler DP, Currier JS, Lundgren JD, Dube MP, et al. State of the science conference: initiative to decrease cardiovascular risk and increase quality of care for patients living with HIV/AIDS: executive summary. Circulation 2008; 118:198–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chu C, Umanski G, Blank A, Meissner P, Grossberg R, Selwyn PA. Comorbidity-related treatment outcomes among HIV-infected adults in the Bronx, NY. J Urban Health 2011; 88:507–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kagaruki GB, Mayige MT, Ngadaya ES, Kimaro GD, Kalinga AK, Kilale AM, et al. Magnitude and risk factors of non-communicable diseases among people living with HIV in Tanzania: a cross sectional study from Mbeya and Dar es Salaam regions. BMC Public Health 2014; 14:904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ngala RA, Fianko K. Dyslipidaemia and dysglycaemia in HIV-infected patients on highly active anti-retroviral therapy in Kumasi Metropolis. Afr Health Sci 2013; 13:1107–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jantarapakde J, Phanuphak N, Chaturawit C, Pengnonyang S, Mathajittiphan P, Takamtha P, et al. Prevalence of metabolic syndrome among antiretroviral-naive and antiretroviral-experienced HIV-1 infected Thai adults. AIDS Patient Care STDS 2014; 28:331–340. [DOI] [PubMed] [Google Scholar]
- 12.Tesfaye DY, Kinde S, Medhin G, Megerssa YC, Tadewos A, Tadesse E, et al. Burden of metabolic syndrome among HIV-infected patients in Southern Ethiopia. Diabetes Metab Syndr 2014; 8:102–107. [DOI] [PubMed] [Google Scholar]
- 13.Paula AA, Schechter M, Tuboi SH, Faulhaber JC, Luz PM, Veloso VG, et al. Continuous increase of cardiovascular diseases, diabetes, and non-HIV related cancers as causes of death in HIV-infected individuals in Brazil: an analysis of nationwide data. PLoS One 2014; 9:e94636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menezes de Padua CA, Moura CS. Availability of data on adverse reactions to antiretroviral drugs in medical charts according to the naranjo algorithm: an example of a Brazilian historical cohort. Clin Drug Investig 2014; 34:395–402. [DOI] [PubMed] [Google Scholar]
- 15.Mascolini M. Making sense of diverse diabetes rate reports in HIV cohorts by page. A Publication of the Center for AIDS information and Advocacy. Available at: http://www.thebodypro.com/content/75944/making-sense-of-diverse-diabetes-rate-reports-in-h.html?; 2015. pp. 5–8.
- 16.Tripathi A, Jerrell JM, Liese AD, Zhang J, Rizvi AA, Albrecht H, et al. Association of clinical and therapeutic factors with incident dyslipidemia in a cohort of human immunodeficiency virus-infected and non-infected adults: 1994–2011. Metab Syndr Relat Disord 2013; 11:417–426. [DOI] [PubMed] [Google Scholar]
- 17.Dube MP, Stein JH, Aberg JA, Fichtenbaum CJ, Gerber JG, Tashima KT, et al. Guidelines for the evaluation and management of dyslipidemia in human immunodeficiency virus (HIV)-infected adults receiving antiretroviral therapy: recommendations of the HIV Medical Association of the Infectious Disease Society of America and the Adult AIDS Clinical Trials Group. Clin Infect Dis 2003; 37:613–627. [DOI] [PubMed] [Google Scholar]
- 18.Grinspoon S, Carr A. Cardiovascular risk and body-fat abnormalities in HIV-infected adults. N Engl J Med 2005; 352:48–62. [DOI] [PubMed] [Google Scholar]
- 19.Lo J, Grinspoon S. Cardiovascular disease in HIV-infected patients: does HIV infection in and of itself increase cardiovascular risk? Curr Opin HIV AIDS 2008; 3:207–213. [DOI] [PubMed] [Google Scholar]
- 20.Echeverria P, Domingo P, Llibre JM, Gutierrez M, Mateo G, Puig J, et al. Prevalence of ischemic heart disease and management of coronary risk in daily clinical practice: results from a Mediterranean cohort of HIV-infected patients. Biomed Res Int 2014; 2014:823058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hruz PW, Murata H, Mueckler M. Adverse metabolic consequences of HIV protease inhibitor therapy: the search for a central mechanism. Am J Physiol Endocrinol Metab 2001; 280:E549–E553. [DOI] [PubMed] [Google Scholar]
- 22.Ledergerber B, Furrer H, Rickenbach M, Lehmann R, Elzi L, Hirschel B, et al. Factors associated with the incidence of type 2 diabetes mellitus in HIV-infected participants in the Swiss HIV Cohort Study. Clin Infect Dis 2007; 45:111–119. [DOI] [PubMed] [Google Scholar]
- 23.Bittar R, Giral P, Aslangul E, Assoumou L, Valantin MA, Kalmykova O, et al. Determinants of low-density lipoprotein particle diameter during antiretroviral therapy including protease inhibitors in HIV-1-infected patients. Antivir Ther 2012; 17:855–860. [DOI] [PubMed] [Google Scholar]
- 24.Fauvel J, Bonnet E, Ruidavets JB, Ferrieres J, Toffoletti A, Massip P, et al. An interaction between apo C-III variants and protease inhibitors contributes to high triglyceride/low HDL levels in treated HIV patients. AIDS 2001; 15:2397–2406. [DOI] [PubMed] [Google Scholar]
- 25.Vigano A, Aldrovandi GM, Giacomet V, Merlo M, Martelli L, Beretta S, et al. Improvement in dyslipidaemia after switching stavudine to tenofovir and replacing protease inhibitors with efavirenz in HIV-infected children. Antivir Ther 2005; 10:917–924. [PubMed] [Google Scholar]
- 26.Bernal E, Masia M, Padilla S, Gutierrez F. High-density lipoprotein cholesterol in HIV-infected patients: evidence for an association with HIV-1 viral load, antiretroviral therapy status, and regimen composition. AIDS Patient Care STDS 2008; 22:569–575. [DOI] [PubMed] [Google Scholar]
- 27.Ahmed MH, Husain NE, Almobarak AO. Nonalcoholic Fatty liver disease and risk of diabetes and cardiovascular disease: what is important for primary care physicians? J Family Med Prim Care 2015; 4:45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahmed MH, Barakat S, Almobarak AO. Nonalcoholic fatty liver disease and cardiovascular disease: has the time come for cardiologists to be hepatologists? J Obes 2012; 2012:483135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nishijima T, Gatanaga H, Shimbo T, Komatsu H, Nozaki Y, Nagata N, et al. Traditional but not HIV-related factors are associated with nonalcoholic fatty liver disease in Asian patients with HIV-1 infection. PLoS One 2014; 9:e87596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sterling RK, Smith PG, Brunt EM. Hepatic steatosis in human immunodeficiency virus: a prospective study in patients without viral hepatitis, diabetes, or alcohol abuse. J Clin Gastroenterol 2013; 47:182–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Machado MV, Oliveira AG, Cortez-Pinto H. Hepatic steatosis in patients co infected with human immunodeficiency virus/hepatitis C virus: a meta-analysis of the risk factors. Hepatology 2010; 52:71–78. [DOI] [PubMed] [Google Scholar]
- 32.Bani-Sadr F, Barange K, Daoud F, Jacomet C, Bicart-See A, Rosenthal E, et al. Persistently normal alanine aminotransferase levels in HIV/HCV-coinfected patients: the role of steatosis. HIV Med 2009; 10:417–421. [DOI] [PubMed] [Google Scholar]
- 33.Lemoine M, Serfaty L, Capeau J. From nonalcoholic fatty liver to nonalcoholic steatohepatitis and cirrhosis in HIV-infected patients: diagnosis and management. Curr Opin Infect Dis 2012; 25:10–16. [DOI] [PubMed] [Google Scholar]
- 34.Arendt BM, Mohammed SS, Ma DW, Aghdassi E, Salit IE, Wong DK, et al. Non-alcoholic fatty liver disease in HIV infection associated with altered hepatic fatty acid composition. Curr HIV Res 2011; 9:128–135. [DOI] [PubMed] [Google Scholar]
- 35.Crum-Cianflone N, Krause D, Wessman D, Medina S, Stepenosky J, Brandt C, et al. Fatty liver disease is associated with underlying cardiovascular disease in HIV-infected persons(*). HIV Med 2011; 12:463–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Price JC, Seaberg EC, Latanich R, Budoff MJ, Kingsley LA, Palella FJ, Jr, et al. Risk factors for fatty liver in the Multicenter AIDS Cohort Study. Am J Gastroenterol 2014; 109:695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Worm SW, De WS, Weber R, Sabin CA, Reiss P, El-Sadr W, et al. Diabetes mellitus, preexisting coronary heart disease, and the risk of subsequent coronary heart disease events in patients infected with human immunodeficiency virus: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D Study). Circulation 2009; 119:805–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Worm SW, Friis-Moller N, Bruyand M, D'Arminio MA, Rickenbach M, Reiss P, et al. High prevalence of the metabolic syndrome in HIV-infected patients: impact of different definitions of the metabolic syndrome. AIDS 2010; 24:427–435. [DOI] [PubMed] [Google Scholar]
- 39.Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab 2007; 92:2506–2512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Friis-Moller N, Reiss P, Sabin CA, Weber R, Monforte A, El-Sadr W, et al. Class of antiretroviral drugs and the risk of myocardial infarction. N Engl J Med 2007; 356:1723–1735. [DOI] [PubMed] [Google Scholar]
- 41.Koganti S, Kinloch-de Loes S, Hutchinson S, Johnson M, Rakhit RD. Management of cardiovascular conditions in a cohort of patients with HIV: experience from a joint HIV/cardiology clinic. Clin Med (Lond) 2015; 15:442–446. [DOI] [PMC free article] [PubMed] [Google Scholar]


