Abstract
Objective:
Our goal was to evaluate treatment attendance patterns, including both treatment completion and premature termination from treatment, for two evidence based psychotherapies for major depressive disorder (MDD) delivered in a community mental health setting. We explored rates of premature termination across the course of treatment as well as the factors that predicted and moderated premature termination and treatment completion.
Method:
This investigation included 237 patients with MDD who participated in a non-inferiority trial comparing short-term dynamic psychotherapy (DT) to cognitive therapy (CT). Patients in both conditions were offered 16 sessions of treatment and had up to 5 months to complete treatment. All patients completed an extensive self-report battery at treatment baseline as well as measures of the therapeutic alliance and opinions about treatment following session 2.
Results:
Premature termination from both treatments was high with 27% of patients discontinuing treatment very early after only an intake session or a single treatment session. Patients in CT were significantly more likely to terminate treatment prematurely, χ2(3) = 14.35, p = .002. Baseline physical health functioning, subthreshold psychotic symptoms, Session 2 ratings of agreement on tasks, and Session 2 ratings of treatment sensibility all independently predicted premature termination of services. Trauma history significantly moderated very early termination of treatment, χ2(3) = 10.26, p = .017, with patients with high trauma histories more likely to complete DT but terminate prematurely from CT.
Conclusions:
Very early termination from services was higher in CT compared to DT. Including techniques to improve engagement in both therapies and matching patients to treatment based on predictors/moderators may be effective ways to optimize treatment engagement.
Keywords: attrition, dropout, attendance, community mental health, depression
Premature termination from mental health services is an enduring problem (Barrett, Chua, Crits-Christoph, Gibbons, & Thompson, 2008; Olfson et al., 2009) across service sectors that impacts the successful dissemination and effectiveness of interventions to those in need. Estimates from nationally representative samples (Olfson et al., 2009) suggest that outpatients receiving mental health treatment in specialty mental health centers receive only a median of 7 psychotherapy sessions. Of those who discontinue treatment early, 70% do so after only 1 or 2 sessions. The problem is even worse in the community mental health setting, which was created to specifically serve minority and economically disadvantaged individuals. An examination of a Medicaid claims database for the Philadelphia region (Connolly Gibbons et al., 2011) indicated that patients receiving outpatient psychotherapy for major depressive disorder receive only a median of 5 psychotherapy sessions with the modal number of sessions being only 1. Premature termination from services has been associated with poor treatment outcome (Lambert, 2007) especially for those who discontinue treatment very early (Pekarik, 1992).
Although these statistics paint a dire picture of service delivery for mental health interventions, the presentation of global statistics to represent skewed data leave the impression that few, if any, individuals are receiving adequate treatment in the community. Complicating our ability to draw conclusions from the research literature further is the fact that most attempts to estimate premature termination from services have aggregated across diagnostic groups and service settings, which may have different rates of premature termination. Studies have also used a variety of broad definitions for the construct. The terms engagement, attendance, attrition, and dropout have been used interchangeably in the literature but often refer to a variety of constructs, including failure to attend the last session, termination of treatment within a specified period of time, and consumer initiated termination (Barrett, Chua, Crits-Christoph, Gibbons, Thompson, 2008). Becker, Boustani, Gellatly, and Chorpita (2018) define the broad concept of engagement as a multifaceted construct with the most common behavioral dimension measured as treatment attendance. Recent reviews more precisely define the construct of non-attendance, which includes both treatment refusal (Oldham, Kellett, Miles, & Sheeran, 2012) and premature termination (Oldham et al., 2012; Ogrodniczuk, Joyce, & Piper, 2005), defined as discontinuing treatment before the agreed upon number of sessions. A final methodological flaw with studies of premature termination is that most investigations assess this construct globally, collapsing across the full course of treatment. Oldham et al. (2012) and Barrett et al. (2008) suggest that premature termination should be studied separately across the stages of psychotherapy, since reasons for disengaging at different points across treatment may be very different.
Our goal was to conduct a more complex evaluation of treatment attendance patterns for evidence based psychotherapies delivered in a community mental health setting in order to have a more complete understanding of how many patients are terminating prematurely across each phase of treatment as well as completing these evidence-based treatments. The current article uses data from a recently completed randomized non-inferiority effectiveness trial (Connolly Gibbons et al., 2014; Connolly Gibbons et al., 2016) in the community mental health setting comparing short-term dynamic psychotherapy (DT) and cognitive therapy (CT) in the treatment of major depressive disorder (MDD). The treatment was delivered by Master’s level clinicians employed by the community mental health clinic who were trained in these evidence based psychotherapies using intensive training methods more consistent with efficacy trial methods (Connolly Gibbons et al., 2014). The results indicated that DT was statistically not inferior to CT in the treatment of MDD, yet consistent with national treatment attendance patterns many patients prematurely terminated treatment. Although these interventions may be equivalent in terms of treatment effectiveness, an in-depth exploration of premature termination patterns for patients receiving these evidence-based psychotherapies for MDD may specifically inform the dissemination of these treatments in the CMHC setting.
Our exploration of the broad construct of treatment attendance was guided by two questions that are important to community agencies delivering evidence-based psychotherapies. First, who are the individuals who seek out treatment yet terminate services very early? Second, once patients are initially engaged in the treatment process, why do some individuals complete the treatment while others terminate prematurely at different points across treatment? Patients in the effectiveness trial were offered a maximum of 16 sessions of therapy and outcome monitoring investigations (Hansen, Lambert, & Forman, 2002; Lambert, 2007) suggest that between 11 and 13 sessions of an evidence-based psychotherapy are needed for over 50% of patients to be considered recovered. For this reason, our definition of treatment attendance included both “treatment completion” defined as attending at least 12 sessions and “premature termination” defined as attending fewer than 12 sessions. We examined three clinically meaningful categories of premature termination across the phases of treatment. We first defined the clinically important category of “very early termination” consisting of patients who were randomized to treatment but terminated after only the intake appointment or a single session of therapy. We further evaluated patients who terminated treatment prematurely after only receiving between two and six sessions and patients who terminated treatment prematurely after receiving between seven and eleven sessions.
Our second goal was to uncover the predictors and moderators of treatment attendance groups across DT and CT to aid in understanding how premature termination may be targeted in the dissemination of these evidence-based interventions. The review of predictors of premature termination by Barrett and colleagues (2008) was guided by Andersen’s (1968; 1995) model of health service utilization that included patient characteristics, enabling factors, factors related to need, and environmental factors as determinants of service utilization. Barrett et al (2008) further considered newer models of utilization that also included perceptions of mental health and treatment as important factors that influence utilization (Owens, Hoagwood, Horwitz, Leaf, Poduska, Kellams, & Ialongo, 2002).
The review by Barrett et al. (2008) provides some evidence, albeit mixed, in support of patient demographic characteristics, including gender, age, minority status, and socioeconomic status. For need factors, there was some evidence for severity of diagnosis, personality disorder, and motivation as predictors of premature termination. There was also consistent support for enabling factors, such as distance traveled, waitlist placement, and longer wait for services. There was minimal evidence to support environmental factors such as staff attitudes and access to care and very little research supporting perceptions of mental health as predictors of premature termination. Finally, for perceptions of treatment, there was some evidence that attitudes and expectations of treatment were predictive of premature termination.
Although there is some evidence of factors predictive of premature termination, methodological limitations including poor construct definitions and aggregation of results across different treatments and settings limit our ability to draw meaningful conclusions regarding how best to adapt treatments to improve treatment attendance. In addition to the methodological limitations described above, most studies of factors predictive of premature attrition have attended to only one or few potential variables at a time. It’s likely that the reasons any patient chooses to terminate treatment prematurely are complex and multifaceted. In addition, there may be very different factors that account for patient attrition across the stages of psychotherapy. By looking at predictors of attrition collapsed across the full treatment course, we might miss the important variables that are specifically predictive of premature termination during specific phases of treatment. Our goal was to address the limitations of previous research by evaluating the predictors and moderators of attrition across 4 stages of treatment to specifically answer two questions: (a) What variables differentiate those who terminate treatment very early? and (b) What variables differentiate those who complete a treatment from those who engage in treatment initially but discontinue treatment prematurely? This more refined approach to exploring premature termination may contribute information that might be more useful in thinking about how to refine current evidence based approaches to decrease premature termination.
In order to study the broad array of patient factors that might contribute to the complex decision to terminate treatment prematurely, we included patient demographic characteristics, baseline symptoms and functioning to represent need factors, and pretreatment attitudes and expectations to represent perceptions about treatment. In addition to these factors, we examine here the baseline skills variables specifically targeted by CT and DT as possible predictors of premature termination, including cognitive dysfunction and interpersonal problems that may differentially influence the symptom course across these two therapies (Connolly Gibbons et al., 2015). We also examined early treatment process variables like the alliance (Horvath, Del Re, Fluckiger, & Symonds, 2011) as well as treatment and clinical history variables (Fournier, DeRubies, Shelton, Hollon, Amsterdam, et al., 2009) that have been shown to significantly influence mental health treatment course.
Method
All study procedures were conducted in compliance with the University of Pennsylvania Institutional Review Board. Details of the methods utilized in the randomized non-inferiority trial and effectiveness results are provided by Connolly Gibbons et al. (2014) and Connolly Gibbons et al. (2016).
Setting
All data was collected in collaboration with Merakay (previously NHS Human Services), a large, private, non-profit, community organization that provides mental health and substance abuse services across seven states with a concentration in the mid-Atlantic region of the United States to primarily publicly funded patients. The randomized non-inferiority trial was conducted at an outpatient community mental health center (CMHC) in Sharon Hill, Pennsylvania that services approximately 4,900 mental health patients per year. The site employs 80 clinicians and three to four psychiatrists.
Participants
Patients.
Patient participants for the randomized non-inferiority trial sample were recruited from those seeking services for depression at the CMHC. The Quick Inventory for Depressive Symptomatology (QIDS; Rush et al., 2003) was completed by all adult patients attending an intake assessment at the clinic. The intake clinician scored the QIDS and completed a short eligibility checklist. Names and contact information for patients ages 18 to 65 who scored at least 11 on the QIDS and were able to read English at the fourth grade level were then provided to the research team. A member of the research team conducted a brief phone screening for each patient referred and scheduled patients for a research baseline assessment at the CMHC.
Informed consent and self-report batteries were collected by a study research assistant at the baseline assessment. A research clinical evaluator blind to the study design conducted the Structured Clinical Interview for the DSM-IV Axis I disorders interview (SCID; First, Spitzer, Gibbon, & Williams, 1997) as well as the interview for the Hamilton Depression Rating Scale (HAM-D; Hamilton, 1960). Patients who met criteria for MDD were included in the study if they did not have: (a) a diagnosis of bipolar disorder, (b) current or past diagnosis of schizophrenia, psychosis, MDD with psychotic features, or seizure disorder, (c) depression due to organic pathology, (d) symptoms of substance/alcohol abuse requiring immediate referral to substance abuse treatment, (e) problems requiring immediate referral to a partial hospitalization program, or (f) suicidal thoughts judged by the clinic to require services more intensive than once per week psychotherapy.
Two hundred and thirty-seven patients were randomized to either 16 sessions of DT or CT. Of the 118 patients randomized to DT, 103 (87%) attended at least one treatment session and 104 (88%) received at least one post baseline assessment. Of the 119 patients randomized to CT, 99 (83%) attended at least one treatment session and 105 (88%) received at least one post baseline research assessment. The majority of patients were female (75%), single (57%), not employed full time (94%), and had a high school diploma or less education (59%). The average age was 36.18 (SD = 12.05) years. Forty-nine percent of patients were members of a minority group. Patients attended on average 6.27 (SD = 5.32, Mdn = 5.00) sessions of psychotherapy.
Clinicians.
Clinicians employed by Merakey with at least a master’s degree were recruited to participate in this trial through advertisement at the site. For the non-inferiority trial, clinicians were assigned to treatment groups in order to match groups on skill, allegiance, and motivation. Clinicians were only included in a training group if they identified their theoretical orientation consistent with the treatment, had previous graduate school classes and supervised training in the modality, and indicated that they wanted training in the treatment. Nine clinicians delivered CT and 11 clinicians were included in the DT condition.
Interventions
Supportive-expressive dynamic psychotherapy.
The DT for the non-inferiority sample consisted of supportive-expressive DT (Book, 1998; Luborsky, 1984). The treatment includes both techniques to build a positive working alliance and expressive techniques to help patients gain self-understanding of their repetitive maladaptive relationship patterns. The treatment is an active, focused exploration of current relationship conflicts, including an explicit socialization to treatment and focus on specific interpersonal goals.
Cognitive therapy.
The CT (Beck, 1995; Beck, Rush, Shaw, & Emery, 1979) implemented in the non-inferiority sample consisted of structured sessions focused on both behavioral activation and the exploration of negative thought patterns. Specific interventions included activity scheduling, evaluating automatic thoughts, and behavioral experiments. Treatment progressed to include exploration of underlying beliefs and attitudes.
Training and supervision.
The training and supervision for the non-inferiority trial was provided by expert supervisors who had substantial experience delivering the respective treatments in clinical practice, delivering the treatment as part of research study protocols, and supervising the delivery of the treatment. All clinicians first participated in a training workshop with the respective expert supervisor, delivered in a flexible format to meet the needs of busy community clinicians. Supervisors for each condition provided both individual supervision across the first three training cases to each clinician as well as ongoing bimonthly group supervisions that continued across the randomization phase of the protocol.
Clinical Evaluators
Nine advanced graduate students in clinical psychology administered the Structured Clinical Interview for the DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1997) and the Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1960) for the non-inferiority trial. The clinical evaluators were blind to treatment condition and study hypotheses. They were trained to competence by a master’s level clinician with expertise in delivering and training clinicians to utilize the SCID and HAM-D.
Diagnostic and Outcome Measures
Quick Inventory of Depressive Symptomatology–Self Report (QIDS; Rush et al., 2003).
This 16-item self-report measure was used to assess the severity of depressive symptoms at baseline. The QIDS has demonstrated good internal consistency (Cronbach’s α = .86) in patients with chronic major depression (Rush et al., 2003) and total scores were highly correlated (r = .81) with the 17-item Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1960). In the current sample, the QIDS demonstrated modest internal consistency (Cronbach’s α = .59) but this finding was based on the restricted range of patients selected for inclusion in the protocol.
The Structured Clinical Interview for DSM-IV (SCID; First et al., 1997).
The SCID-I for DSM-IV was administered at baseline to provide diagnoses. Inter-judge agreement for the diagnosis of MDD has been good with kappa coefficients ranging from .61–93 (Lobbestael, Leurgans, & Arntz, 2011; Segal, Kabacoff, Hersen, Van Hasselt, & Ryan, 1995; Skre, Onstad, Torgersen, & Kringlen, 1991; Williams et al., 1992; Zanarini & Frankenburg, 2001; Zanarini et al., 2000).
The Hamilton Depression Inventory.
The HAM-D was administered at baseline and Months 1, 2, 4, and 5 to evaluate the severity of common symptoms of depression. The 24-item version of the HAM-D was completed by applying the Structured Interview Guide proposed by Williams (1988) to enhance reliability. A recent meta-analysis reports a Cronbach’s alpha of .79, as well as good inter-rater and test-retest reliability (Trajković et al., 2011). The internal consistency for the HAM-D at the Month 5 assessment was adequate for the current sample (Cronbach’s α = .78).
Potential Predictors
Demographic characteristics.
Seven demographic variables were included in the patient characteristics domain. All variables were assessed via a brief self-report demographic questionnaire administered at baseline. Age was included as a continuous variable while gender was a categorical variable representing male or female. Five demographic variables were included as categorical variables with two levels including whether or not the patient was: in a long term relationship, currently married, a minority, currently employed fulltime, and educated above a high school degree.
Pretreatment attitudes and expectations.
Five variables from the self-report Attitudes and Expectations Questionnaire (AAE; Elkin et al., 1989) were included in this domain. Two items representing the degree to which patients thought it would be helpful to learn about their negative thoughts and helpful to learn about relationship patterns were each rated on a 7-point Likert scale ranging from 1 (not at all helpful) to 7 (extremely helpful). Two items representing patient attitudes towards talking with a therapist and towards taking medication were each rated on a 7-point Likert scale ranging from 1 (very positive) to 7 (very negative). Finally, patients rated the overall degree of improvement they expected on a 7-point Likert scale ranging from 1 (expect to feel much worse) to 7 (expect to feel much better).
Baseline symptoms and functioning.
Twelve variables were included in the baseline symptoms and functioning domain. The total score from the self-report Alcohol Use Disorders Identification Test (AUDIT; Babor, de la Fuente, Saunders, & Grant, 1989; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) was used to assess problems with alcohol. For the current project, parallel items were developed for each AUDIT item to assess problems with drug use. The number of concurrent Axis I diagnoses and the Global Assessment of Functioning (GAF; American Psychiatric Association, 2002) were derived from the SCID assessment. The depression, interpersonal relationships, psychotic symptoms, self-harm, and emotional lability subscales of the 24-item self-report Behavior and Symptom Identification Scale (BASIS-24; Eisen, Normand, Belanger, Spiro, & Esch, 2004) were included to assess baseline mental health status. The BASIS-24 has demonstrated good reliability, concurrent validity, and sensitivity across racial groups (Eisen, Gerena, Ranganathan, Esch, & Idiculla, 2006). Quality of life was assessed via the total score from the 32-item Quality of Life Inventory (QOLI; Frisch, Cornell, Villanueva, & Retzlaff, 1992). Functioning was assessed via the two summary scores (Ware, Kosinski, & Keller, 1994; Ware et al., 1995) of the Medical Outcomes Study 36-item Short Form (SF-36; Ware & Sherbourne, 1992), including the mental component summary (MCS) and the physical component summary (PCS).
Treatment and clinical history.
Four variables were included in the treatment and clinical history domain. Patients were asked at baseline to list the number of trials of medication they had completed and the number of times they had tried psychotherapy to address their symptoms. Patients were also asked to complete the Trauma and Life Events Questionnaire (TLEQ; Kubany et al., 2000). Trauma history was represented by the number of types of trauma experienced in the past. A two-level categorical variable was including representing whether or not the depression was recurrent.
Early treatment process.
The early treatment process domain included the tasks, bond, and goals subscales of the self-report Working Alliance Inventory (WAI; Horvath & Greenberg, 1989) as well as 3 items from the Opinions About Treatment questionnaire (OAT; Borkovec & Nau, 1972) administered at Session 2. Patients were asked to rate how sensible they found the treatment, how confident they were in the treatment, and whether they would recommend the treatment on 7-point Likert scales ranging from 1 (not at all) to 7 (extremely).
Interpersonal problems.
Three variables were included in the interpersonal problems domain. The self-understanding score and the recognition score from the Self-Understanding of Interpersonal Patterns Scale-Revised (SUIP-R; Connolly et al., 1999) were included, as well as the Inventory of Interpersonal Patterns 32-item total score (IIP; Barkham, Hardy, & Startup, 1996).
Cognitive dysfunction.
Cognitive dysfunction was assessed by four variables, including the positive and negative subscales of the Ways of Responding self-report (Yin, Diehl, Gallop, Crits-Christoph, & Connolly Gibbons, 2016) and the performance evaluation and approval by others subscales from the Dysfunctional Attitudes Scale (DAS; Weissman, 1980; Weissman & Beck, 1978).
Data Analytic Strategy
Multinomial logistic regressions were used to evaluate the predictors and moderators of treatment attendance. The dependent variable for all analyses was the attendance group variable consisting of 4 categories (very early termination after only the intake or 1 session, premature termination after only two to six sessions, premature termination after seven to eleven sessions, treatment completion of twelve to sixteen sessions). This multinomial outcome allowed us to evaluate the predictors of premature termination assuming that the complex set of predictors was not homogenous across the stages of treatment. Analyses were conducted both comparing (a) patients who terminated treatment very early to patients who terminated after two to six sessions, terminated after seven to eleven sessions, or completed twelve to sixteen sessions, and (b) patients who completed twelve to sixteen sessions of treatment compared to those who terminated after only 2 to six sessions and terminated after seven to eleven sessions. Although patients were nested within clinicians, the ICC (2, 1) for differences between clinicians predicting the number of treatment sessions was only .015. Raundenbush and Bryk (2002) indicate that in cases where the ICC falls below .05, there is not sufficient variability in the random term to be included as a random effect. For this reason, clinician was not included as a factor in the current analyses. A simple model using backward multinomial logistic regression was first conducted within each domain of possible predictors using a p value .05 to remove a predictor from the model. To address each of the two research questions, a final model using backward regression was then conducted using only the variables that were predictive within the domain analyses again using a p value of .05 to remove a predictor from the final predictive model. The significance of the omnibus test evaluating whether the final model fit the data better than the simple model was evaluated at an adjusted p of .025 to account for the two logistic regressions computed to address two distinct research questions. Six domains were included as predictors of very early termination: demographic characteristics, pretreatment attitudes and expectations, baseline symptoms and functioning, treatment and clinical history, interpersonal problems, and cognitive dysfunction. One additional domain, early treatment process, was included to predict treatment completion. This domain was not included in the models predicting very early treatment termination because patients who discontinued treatment very early did not have the process measures administered following Session 2. All possible predictors were examined as possible main effect predictors of attendance and as moderators of treatment attendance (i.e., differential prediction of attrition for CT vs DT). All main effect variables were centered to allow for interpretation of both main effects and interactions with treatment in the predictive models. A generalized R2 index was derived for each final model using the corrected Cox & Snell (1989) formula. To test for the possibility that patients included in the very early termination group were heterogeneous, we conducted a sensitivity analysis for our final model predicting very early termination excluding the patients who were randomized to treatment but attended only the intake session.
Results
Descriptive Statistics for Session Attrition by Treatment
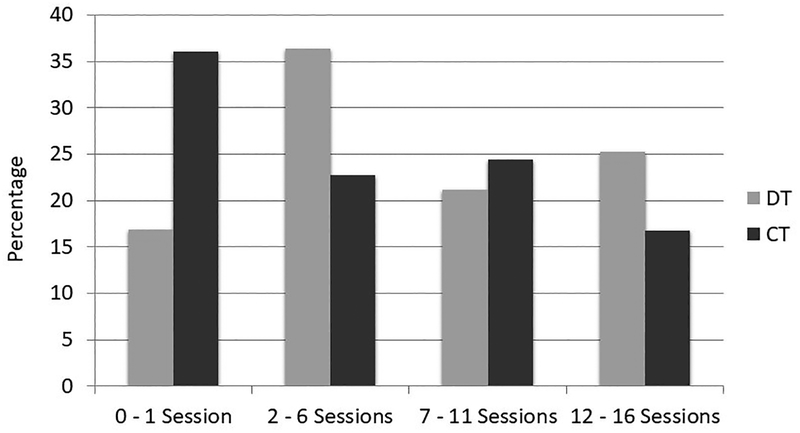
Patients in the DT condition attended a mean of 7 sessions (Mdn = 6, SD = 5) and patients in the CT condition attended a mean of 6 sessions (Mdn = 4, SD = 5). There was no significant difference between treatments in the average number of treatment sessions attended, t(235) = 1.47, p = .142. Across treatments, 27% of patients were in the very early termination group, discontinuing services after only an intake session or 1 psychotherapy session. In contrast, 21% of patients completed psychotherapy, attending between 12 and 16 sessions across 5 months. Twenty-nine percent terminated treatment after attending between 2 and 6 sessions, while 23% terminated treatment after attending between 7 and 11 sessions of psychotherapy. The percentage of patients in each treatment attendance group by treatment condition are presented in Figure 1. Overall, CT and DT had significantly different attendance patterns, χ2(3, 237) = 14.35, p = .002. Thirty-six percent of patients assigned to CT discontinued treatment after only an intake or single treatment session compared with only 17% of patients assigned to DT. In comparison, 25% of patients in the DT group completed between twelve and sixteen session of treatment compared to only 17% of patients in the CT group.
Figure 1:
Attendance Patterns by Treatment.
Predictors and Moderators of Early Treatment Termination
Step-wise analyses for predictor domains.
For three of the six domains examined, the final model fit the data better than the simple model. These domains were: demographic characteristics, χ2(6, 237) = 25.81, p < .001, symptoms and functioning, χ2(6, 216) = 21.67, p = .001, and treatment and clinical history, χ2(15, 234) = 31.53, p = .007. Within the demographic characteristics domain, only patient education significantly uniquely predicted very early termination of treatment after only an intake session or a single treatment session, χ2(3, 237) = 11.22, p = .011. Within the baseline symptoms and functioning domain, the physical component score of the SF-36, χ2(3, 216) = 12.54, p = .006, and the psychotic symptoms score of the BASIS-24, χ2(3, 216) = 9.35, p = .025, uniquely predicted very early termination of treatment. Within the treatment and clinical history domain, the interaction of treatment with trauma history, χ2(3, 234) = 9.40, p = .024, and the interaction of treatment with recurrence of depression, χ2(6, 234) = 16.13, p = .013, significantly predicted very early termination of services. No variables from the attitudes and expectations, interpersonal problems, or cognitive dysfunction domains significantly predicted or moderated very early treatment termination.
Final predictive models of attrition group.
All variables significant in the within-domain analyses were then entered into a final stepwise multinomial logistic regression using backwards elimination. For significant interactions of predictors with treatment, the main effect for the predictor was also included in the model. The results are presented in Table 1. Education level, recurrence of depression, and the interaction of treatment with recurrence of depression were removed from the final model because they did not meet the backwards elimination criterion. The final model fit the data significantly better than the simple model, χ2(15, 230) = 46.41, p < .001, with a R2 of .18.
Table 1.
Final Model With All Significant Predictors From the Domain Models Differentiating Patients Who Terminated Treatment Very Early From Those Who Attended At Least Two Sessions
| Predictor | Wald Chi-Square | df | p | OR | 95% CI |
|---|---|---|---|---|---|
| Comparing very early termination to termination after two to six sessions | |||||
| Physical functioning | 6.09 | 1 | .014 | .963 | [.934, .992] |
| Psychotic symptoms | 5.35 | 1 | .021 | .614 | [.406, .928] |
| Trauma history | .77 | 1 | .379 | 1.060 | [.931, 1.208] |
| TX | 9.99 | 1 | .002 | 3.420 | [1.595, 7.331] |
| Trauma history × TX | .59 | 1 | .444 | .929 | [.770, 1.122] |
| Comparing very early termination to termination after seven to eleven sessions | |||||
| Physical functioning | 4.24 | 1 | .040 | .968 | [.938, .998] |
| Psychotic symptoms | .15 | 1 | .697 | 1.081 | [.730, 1.601] |
| Trauma history | 1.88 | 1 | .171 | .909 | [.792, 1.042] |
| TX | 2.09 | 1 | .148 | 1.791 | [.813, 3.943] |
| Trauma history × TX | 4.01 | 1 | .045 | 1.225 | [1.004, 1.494] |
| Comparing very early termination to completion of twelve to sixteen sessions | |||||
| Physical functioning | .01 | 1 | .904 | 1.002 | [.970, 1.035] |
| Psychotic symptoms | 4.08 | 1 | .044 | .617 | [.387, .986] |
| Trauma history | .04 | 1 | .834 | .984 | [.850, 1.140] |
| TX | 8.42 | 1 | .044 | 3.345 | [1.480, 5.561] |
| Trauma history × TX | 2.00 | 1 | .158 | 1.159 | [.994, 1.423] |
Note. OR = odds ratio; CI = confidence interval; TX = treatment group.
There was a large effect for treatment group, χ2(3, 230) = 13.46, p = .004, on very early treatment termination following the intake sessions or a single treatment session. Patients in DT were 3 times as likely as patients in CT to either terminate treatment after only two to six sessions or to complete twelve to sixteen sessions than to be in the very early treatment termination group. There was a small effect for physical health functioning, χ2(3, 230) = 11.07, p = .011, with patients with poor physical health functioning more likely to prematurely terminate treatment after two to six sessions or seven to eleven sessions than to be in the very early treatment termination group. There was a significant effect for subthreshold baseline psychotic symptoms as measured by the BASIS-24 subscale, χ2(3, 230) = 11.66, p = .009, with patients with lower psychotic symptom scores 39% more likely to terminate treatment after only two to six sessions than to be in the very early treatment termination group. Twenty-five percent of patients with low psychotic symptoms (defined using a median split of 0.76 on the BASIS-24 psychotic symptoms subscale) were in the very early termination group compared to 37% who terminated treatment after only two to six sessions. In contrast, patients with higher levels of psychotic symptoms were 38% more likely to be in the very early termination group than to complete twelve to sixteen sessions. Only 20% of patients with high psychotic symptoms were treatment completers compared to 27% who were in the very early termination group.
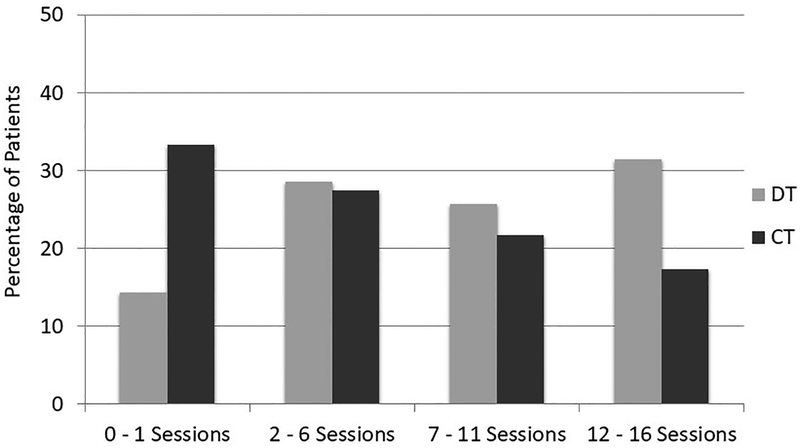
There was a significant effect for the interaction of treatment and trauma history, χ2(3, 230) = 10.26, p = .017, predicting treatment attendance group. To unpack this moderator effect, the predictive model including all predictor variables was computed separately within each treatment group. Patients in the DT group with high trauma levels were 11% (OR =1.11, 95% CI [0.96, 1.29]) more likely to terminate treatment after seven to eleven session than to be in the very early termination group and 13% (OR =1.13, 95% CI [0.98, 1.31]) more likely to complete twelve to sixteen sessions than to be in the very early termination group. Figure 2 presents the percentage of patients in each attendance group by treatment group for patients with high trauma levels at the treatment baseline (high trauma history was defined as greater than or equal to the median of 8 types of traumas on the TLEQ). In the dynamic therapy group, only 10% of patients with high trauma histories were in the very early treatment termination group compared to 36% who were treatment completers. In contrast, 38% of patients with high trauma history in the CT group prematurely terminated treatment after the intake or a single session and only 18% completed between twelve and sixteen sessions.
Figure 2:
Attendance Patterns by Treatment for Patients with High Levels of Trauma.
Sensitivity analysis.
A sensitivity analysis was conducted to evaluate whether the final predictive model remained consistent when we excluded the patients who discontinued treatment after only the intake session. The stepwise multinomial logistic regression using backwards elimination including only patients who had at least one treatment session fit the data significantly better than the simple model, χ2 (15, 230) = 44.43, p < .001, with a R2 of .20. As in the model with the full randomized sample, education level, recurrence of depression, and the interaction of treatment with recurrence of depression were removed from the final model because they did not meet the backwards elimination criterion. Subthreshold psychotic symptoms and physical health functioning remained significant (p < .05) predictors of attendance group and trauma history remained a significant moderator of attendance group (p < .05) when patients who terminated treatment after only the intake session were excluded.
Predictors and Moderators of Treatment Completion
Step-wise analyses for predictor domains.
For three of the seven domains, the final model fit the data better than the simple model. These domains were: symptoms and functioning, χ2(12, 158) = 31.54, p = .002, early treatment process, χ2(4, 161) = 14.57, p = .006, and treatment and clinical history, χ2(4, 172) = 10.53, p = .032. For the baseline symptoms and functioning domain, the physical component score of the SF-36, χ2(2, 158) = 7.21, p = .027, the psychotic symptoms score of the BASIS-24, χ2(2, 158) = 8.89, p = .012, the interaction of treatment with baseline quality of life, χ2(2, 158) = 7.77, p = .021, and the interaction of treatment with alcohol problems assessed via the AUDIT, χ2(2, 158) = 6.74, p = .034, predicted premature termination of treatment. For the early treatment process domain, the agreement on tasks alliance subscale, χ2(2, 161) = 10.42, p = .005, and the opinions about treatment sensibility rating, χ2(2, 161) = 6.00, p = .050, were significant predictors of treatment completion of twelve to sixteen sessions. For the treatment and clinical history domain, only the interaction of treatment with trauma history, χ2(2, 172) = 8.66, p = .013, significantly differentiated those who terminated treatment prematurely from those who completed twelve to sixteen sessions. No variables from the demographic characteristics, attitudes and expectations, interpersonal problems, or cognitive dysfunction domains significantly predicted or moderated treatment completion.
Final predictive models of attrition group.
All variables significant in the within-domain analyses predicting completion of twelve to sixteen sessions were entered into a final stepwise logistic regression using backwards elimination. For significant interactions of predictors with treatment, the main effect for the predictor was also included in the model. The results are presented in Table 2. Alcohol use problems and the interaction of treatment with alcohol use problems were removed from the final model. The final model fit the data significantly better than the simple model, χ2(18, 156) = 49.12, p < .001 with a R2 of .27.
Table 2.
Final Model with All Significant Predictors from the Domain Models Differentiating Patients Who Completed Treatment from Those Who Terminated Treatment Prematurely
| Predictor | Wald Chi-Square | df | p | OR | 95% CI |
|---|---|---|---|---|---|
| Comparing completers to those who terminated after two to six sessions | |||||
| Physical functioning | 6.14 | 1 | .013 | .956 | [.923, .991] |
| Psychotic symptoms | .53 | 1 | .467 | .815 | [.470, 1.414] |
| Agreement of tasks | 3.25 | 1 | .071 | 1.597 | [.960, 2.656] |
| Opinions about TX | 6.34 | 1 | .012 | .547 | [.342, .875] |
| Trauma history | 1.31 | 1 | .253 | 1.108 | [.929, 1.321] |
| Quality of life | 1.48 | 1 | .224 | 1.234 | [.879, 1.731] |
| Treatment | .25 | 1 | .620 | 1.246 | [.521, 2.980] |
| Trauma history × TX | 4.79 | 1 | .029 | .784 | [.630, .975] |
| Quality of Life × TX | 3.54 | 1 | .060 | .649 | [.413, 1.018] |
| Comparing completers to those who terminated after seven to eleven sessions | |||||
| Physical functioning | 4.80 | 1 | .029 | .958 | [.922, .996] |
| Psychotic symptoms | 4.73 | 1 | .030 | 1.848 | [1.062, 3.215] |
| Agreement of tasks | 9.45 | 1 | .002 | 3.202 | [1.525, 6.724] |
| Opinions about TX | 4.78 | 1 | .029 | .536 | [.306, .938] |
| Trauma history | .15 | 1 | .701 | .963 | [.794, 1.167] |
| Quality of life | 1.08 | 1 | .298 | 1.199 | [.852, 1.689] |
| TX | .35 | 1 | .552 | .753. | [.296, 1.918] |
| Trauma history × TX | .08 | 1 | .773 | .996 | [.762, 1.224] |
| Quality of Life × TX | 5.65 | 1 | .018 | .555 | [.342, .902] |
Note. OR = odds ratio; CI = confidence interval; TX = treatment group.
There was a small effect for physical health functioning, χ2(2, 156) = 7.66, p = .022, with patients with lower physical health functioning less likely to complete twelve to sixteen sessions of therapy than to terminate treatment prematurely. There was a small effect for baseline subthreshold psychotic symptoms, χ2(2, 156) = 11.13, p = .004, with patients with higher psychotic symptoms 85% less likely to complete treatment than to terminate treatment after only seven to eleven sessions. Of those with high subthreshold psychotic symptoms, 40% terminated treatment after seven to eleven sessions while only 28% completed twelve to sixteen sessions of treatment.
Two early treatment process variables also differentiated those who completed therapy from those who terminated treatment prematurely. There was a large effect for agreement on the tasks of treatment, χ2(2, 156) = 11.13, p = .004. The results indicate a complex relation between level of agreement on tasks and treatment attendance. Patients with low agreement on tasks were more likely to either terminate treatment after two to six sessions or to complete twelve to sixteen sessions, with 44% terminating after two to six sessions, 20% terminating after seven to eleven sessions, and 36% completing twelve to sixteen sessions of treatment. In addition, patients with low ratings of treatment sensibility at session 2 were 45% less likely to complete treatment than to terminate after only two to six sessions and 46% less likely to complete treatment than to terminate treatment after seven to eleven sessions, χ2(2, 156) = 8.01, p = .018. Of the patients who completed treatment, 70% rated the treatment high on the sensibility scale (defined as greater than or equal to the median of 6 on the sensibility scale) while only 30% rated the treatment as relatively low on the sensitivity scale.
There was a small significant interaction between treatment and trauma history predicting treatment completion, χ2(2, 156) = 6.45, p = .040. To unpack the moderator effects, models including all predictor variables were computed separately within each treatment group. Within DT, patients with high trauma histories were 13% (OR = .87, 95% CI [0.76, .99]) more likely to complete twelve to sixteen sessions of treatment than to terminate treatment after two to six sessions. In contrast, CT patients with high trauma were 11% (OR = 1.11, 95% CI [0.92, 1.33]) more likely to terminate treatment after only two to six sessions than to complete treatment. Figure 2 presents the percentage of patients in each attendance group by treatment group for patients with high trauma levels at the treatment baseline (high trauma history was defined as greater than or equal to the median of 8 types of traumas on the TLEQ). For patients with high trauma histories, 36% of patients in DT and only 18% of those in CT completed twelve to sixteen sessions of treatment.
There was also a small significant interaction of baseline quality of life with treatment group in predicting treatment completion, χ2(2, 156) = 6.45, p = .040. Models computed within treatment groups indicate that in DT patients with low quality of life were 18% (OR = .82, 95% CI [0.60, 1.12]) more likely to complete treatment than to terminate treatment after only two to six sessions, and 34% (OR = .66, 95% CI [0.46, 0.95]) more likely to complete treatment than to terminate treatment after seven to eleven sessions. In contrast, patients in CT were 20% (OR = 1.20, 95% CI [0.85, 1.69]) more likely to terminate treatment after only two to six sessions than to be treatment completers.
Discussion
Consistent with national trends (Olfson et al. 2009), a substantial number of patients discontinued evidence-based psychotherapies prematurely in the context of our comparative effectiveness trial in the community mental health setting. Most concerning to providers and administrators in these settings, more than a quarter of patients who come to treatment in distress discontinue after only an intake session or a single treatment session. Of those who engage in treatment initially, many fail to complete the treatment. It should be noted however that this high attrition rate in the community mental health setting doesn’t necessarily translate to nobody receives the treatment. Rather, over 40% received at least 7 sessions of these evidence based therapies for MDD and 21% completed between twelve and sixteen sessions.
The main outcome results of the effectiveness trial (Connolly Gibbons et al., 2016) were consistent with previous studies (Driessen et al., 2013) and meta-analyses (Fonagy, 2015) indicating that DT is not inferior to CT in the treatment of MDD. Although these results suggest that these treatments produce equivalent outcomes at the population level, our results show that patients assigned to CT were more likely to terminate treatment very early compared to those who were assigned to DT. This finding is consistent with a recent meta-analysis that demonstrated a significantly higher risk of attrition from cognitive behavioral treatments compared to other types of psychotherapy in the treatment of depression (Cuijpers, van Straten, Andersson, & van Oppen, 2008). Although one might expect poorer outcomes in CT given this very early premature termination rate, there was a high premature termination rate after only two to six sessions for the DT group resulting in no statistically significant difference between treatments in the average number of sessions attended.
The high premature termination rate across these evidence-based psychotherapies in the community setting leave open the possibility that treatment dissemination in community mental health settings could be personalized to the needs of individual patients to optimize outcomes. Most efforts to personalize treatment delivery in medicine focus on matching patients to the specific treatment that is most likely to result in the greatest symptom reduction. Our results suggest that efforts to personalize the delivery of psychotherapy should also take into account the treatment that is most likely to initially engage the patient in services.
We explored the patient factors that contribute to this very early discontinuation of services as well as the factors that might account for the differential very early attrition across treatments. We found that patients seeking services for depression with relatively higher levels of subthreshold psychotic symptoms at baseline were more likely to terminate treatment very early. We can speculate that the early focus on teaching the treatment model and delineating the goals of treatment that is common to both treatments may not adequately engage patients with mild disordered thinking. In addition, patients with poor physical health functioning were more likely to initially engage in therapy. It may be that the supportive environment provided by both interventions is useful for patients with physical health problems, but the question remains why patients with relatively better physical health functioning discontinued treatment very early. One option for decreasing premature termination across these evidence based psychotherapies is to add interventions known to increase psychotherapy attendance. A recent meta-analysis (Oldham et al., 2012) reports small to medium effects for interventions specifically designed to improve attendance, with the most effective interventions including motivational interventions, preparation for psychotherapy, informational interventions, attendance reminders, and case management. Both CT and DT delivered in community settings might benefit from inclusion of these techniques specifically targeting patients with subthreshold psychotic symptoms.
Treatment delivery in community settings might also be personalized by matching patients with the specific evidence based treatments most likely to engage them in the treatment. Patients with high trauma histories were more likely to engage in DT yet more likely to prematurely terminate CT very early, accounting in part for the differential very early attrition between these treatments. The early alliance-enhancing techniques implemented in the DT may have been a better match for patients who come to treatment wanting to explore their traumatic experiences. These results indicate that premature termination might be minimized by providing patients with high trauma histories with supportive techniques to begin treatment.
Many of the patients who engaged in the treatment beyond a single session did not go on to complete the psychotherapy. Related to this aspect of attendance, our second goal was to understand what patient factors differentiated those who completed treatment from those who terminated prematurely. Once again, subthreshold psychotic symptoms predicted premature discontinuation of treatment, suggesting that techniques targeting motivation, preparation, and education for those with subthreshold disordered thinking might be necessary to both engage these patients in treatment and keep them in treatment to completion. Physical health functioning was also an important predictor. Although patients with poorer physical health functioning were more likely to engage initially in treatment, they were also less likely to complete treatment. Both treatments may need to incorporate patients’ physical health concerns within the treatment exploration and adjust shared treatment goals accordingly. While DT clinicians might help patients explore how their interpersonal problems intersect with their physical health problems, clinicians delivering CT might work with patients to decrease depressotypic thoughts and increase compensatory cognitive strategies specifically regarding their physical health concerns.
Early treatment process was also important in determining whether patients, once engaged in treatment, were likely to complete therapy. Patients with low agreement on the tasks of therapy following Session 2 were more likely to terminate treatment after only two to six sessions, highlighting the need for clinicians in both CT and DT to enhance their exploration of agreement on tasks and to work to improve agreement before moving forward with the treatment. Likewise, patients who rated the treatment lower on sensibility were less likely to complete treatment. Both CT and DT provide an overview of the treatment model during the initial sessions of treatment. These model descriptions might need to be simplified for delivery in CMHC settings and more effort might be spent exploring the patient’s understanding of the model during the early sessions.
Patients with relatively higher trauma histories and poorer baseline quality of life were more likely to complete DT but were more likely to terminate treatment after only two to six sessions of CT. These findings suggest that the combination of supportive techniques and techniques focused on helping patients explore their interpersonal problems in the DT model was better suited to engaging some patients in treatment initially and keeping them engaged in treatment until completion. Some patients with high trauma histories might need the supportive environment of DT to engage initially but could benefit from either treatment modality once engaged. However, patients with high trauma histories and poor functioning might benefit from remaining in DT to ensure treatment completion.
Although both CT and DT have demonstrated effectiveness in the treatment of MDD at the population level, both treatments might need to be modified to optimize engagement in services in the CMHC setting. In addition to the core techniques described in each model, clinicians delivering these interventions in community setting will need to adapt the treatments to adequately address co-morbid physical health problems, subthreshold psychotic symptoms, early agreement on the tasks of therapy, and patient opinions about the sensibility of the treatment. These results also suggest that we might optimize treatment attendance, and ultimately treatment effectiveness, by personalizing the delivery of psychotherapy techniques to match the needs of specific patients in the CMHC setting. In this setting, patients with trauma histories and poor overall functioning might better engage in DT.
This investigation has limitations that should be considered when interpreting results. Although we evaluated a comprehensive set of possible predictors and moderators of treatment attendance, there may be variables not assessed that determine whether a patient terminates treatment prematurely. Certainly, the models derived from our sample do not account for all of the variance in treatment attendance indicating that other important variables were not assessed. Although we controlled for Type I error by correcting our significance levels for the omnibus tests used to evaluate each predictive model, we included a wide range of possible predictors in order to build a comprehensive model of attendance predictors and did not correct significance levels for each predictor. Future analyses will need to confirm the significance of each of the predictors and moderators of attendance identified here. These models might not generalize to other treatment settings and we have no information about why patients did not attend sessions. In addition, our analyses evaluated only predictors of treatment attendance defined in terms of the number of agreed upon sessions attended. There are other aspects to the broad construct of treatment engagement, such as involvement in the treatment session, which might also be important to consider when personalizing treatment. Further, our very early termination group includes patients randomized to a treatment who attended only the intake session or the first treatment session. This group includes patients who discontinued services before receiving a session of the evidence based psychotherapy, although our sensitivity analysis confirms that our model of predictors and moderators is still relevant for the subset of patients who attended at least one treatment session. Finally, we examined predictors of attendance in two evidence-based psychotherapies for MDD. There are additional therapeutic approaches that have demonstrated improved engagement of patients in psychotherapy in other settings (Oldham et al., 2012). These treatments might improve engagements in services in the CMHC setting. Our results do suggest that treatment attendance might be optimized by adapting treatments delivered in the CMHC setting to better address physical health problems, subthreshold psychotic symptoms, and early treatment process. Engagement might be further optimized by matching patients with significant trauma histories and poor functioning to treatments that include a strong alliance focus and exploration of interpersonal problems.
Public Health Significance:
This study suggests that depressed patients with high trauma histories were more likely to discontinue cognitive therapy early compared to short-term dynamic therapy. It may be that dynamic techniques are useful to initially engage some patients in the treatment process.
References
- American Psychiatric Association. (2002). Multiaxial assessment In DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders (4th ed., text revision). Washington, DC: American Psychiatric Association. [Google Scholar]
- Andersen RM (1968). Behavioral model of families’ use of health services research (Series No. 25). Chicago: Center for Health Administration Studies, University of Chicago. [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10. [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, & Grant M (1989). The Alcohol Use Disorders Identification Test: Guidelines for Use in the Primary Health Care. WHO Publication No. 89.4, Geneva: World Health Organization. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG, & World Health Organization. Dept. of Mental Health and Substance Dependence. (2001). AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care, 2nd ed. Geneva: World Health Organization. [Google Scholar]
- Barkham M, Hardy GE, & Startup M (1996). The IIP-32: A short version of the Inventory of Interpersonal Problems. British Journal of Clinical Psychology, 35, 21–35. doi: 10.1111/j.2044-8260.1996.tb01159.x. [DOI] [PubMed] [Google Scholar]
- Barrett MS, Chua WJ, Crits-Christoph P, Gibbons MB, & Thompson D (2008). Early withdrawal from mental health treatment: Implications for psychotherapy practice. Psychotherapy, 45(2), 247–267. doi: 10.1037/0033-3204.45.2.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, & Emery G (1979). Cognitive therapy of depression. New York, NY: Guilford Press. [Google Scholar]
- Beck JS (1995). Cognitive therapy: Basics and beyond. New York, NY: Guilford. [Google Scholar]
- Becker KD, Boustani M, Gellatly R, & Chorpita BF (2018). Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology, 47, 1–23. Doi: 10.1080/15374416.2017.1326121 [DOI] [PubMed] [Google Scholar]
- Book HE (1998). How to practice brief dynamic psychotherapy: The CCRT method. Washington, DC: American Psychological Association. [Google Scholar]
- Borkovec TD, & Nau SD (1972). Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry, 3(4), 257–260. doi: 10.1016/0005-7916(72)90045-6. [DOI] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models (2nd Ed.). London: Sage. [Google Scholar]
- Connolly MB, Crits-Christoph P, Shelton RC, Hollon S, Kurtz J, Barber JP, … Thase ME (1999). The reliability and validity of a measure of self-understanding of interpersonal patterns. Journal of Counseling Psychology, 46(4), 472–482. doi: 10.1037/0022-0167.46.4.472. [DOI] [Google Scholar]
- Connolly Gibbons MB, Gallop R, Thompson D, Luther D, Crits-Christoph K, Jacobs J, … Crits-Christoph P (2016). Comparative effectiveness of cognitive and dynamic therapies for major depressive disorder in a community mental health setting: A randomized clinical non-inferiority trial. JAMA Psychiatry, 73(9), 904–912. doi: 10.1001/jamapsychiatry.2016.1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly Gibbons MB, Kurtz JE, Thompson DL, Mack RA, Lee JK, Rothbard A, … Crits-Christoph P (2015). The effectiveness of clinician feedback in the treatment of depression in the community mental health system. Journal of Consulting and Clinical Psychology, 83(4), 748–759. doi: 10.1037/a0039302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly Gibbons MB, Mack R, Lee J, Gallop R, Thompson D, Burock D, Crits-Christoph P (2014). Comparative effectiveness of cognitive and dynamic therapies for major depressive disorder in a community mental health setting: study protocol for a randomized non-inferiority trial. BMC Psychology, 2(1), 47. doi: 10.1186/s40359-014-0047-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly Gibbons MB, Rothbard A, Farris KD, Stirman SW, Thompson SM, Scott K, … Crits-Christoph P (2011). Changes in psychotherapy utilization among consumers of services for major depressive disorder in the community mental health system. Administration and Policy in Mental Health and Mental Health Services Research, 38(6), 495–503. doi: 10.1007/s10488-011-0336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox DR, & Snell EJ (1989) Analysis of Binary Data (2nd ed.). London: Chapman & Hall. [Google Scholar]
- Cuijpers P, van Straten A, Andersson G, & van Oppen P (2008). Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J Consult Clin Psychol, 76(6), 909–922. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- Driessen E, Van HL, Don FJ, Peen J, Kool S, Westra D, … & Dekker JJ (2013). The efficacy of cognitive-behavioral therapy and psychodynamic therapy in the outpatient treatment of major depression: a randomized clinical trial. American Journal of Psychiatry, 170(9), 1041–1050. doi: 10.1176/appi.ajp.2013.12070899. [DOI] [PubMed] [Google Scholar]
- Eisen SV, Gerena M, Ranganathan G, Esch D, & Idieulla T (2006). Reliability and validity of the BASIS-24 Mental Health Survey for Whites, African Americans, and Latinos. Journal of Behavioral Health Services & Research, 33, 304–323. doi: 10.1007/s11414-006-9025-3. [DOI] [PubMed] [Google Scholar]
- Eisen SV, Normand SL, Belanger AJ, Spiro A, & Esch D (2004). The Revised Behavior and Symptom Identification Scale (BASIS-R): Reliability and validity. Medical Care, 42(12):1230–1241. doi: 10.1097/00005650-200412000-00010. [DOI] [PubMed] [Google Scholar]
- Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky JF, Collins DR, … Parloff MB(1989). National Institute of Mental Health Treatment of Depression Collaborative Research Program: General effectiveness of treatments. Archives of General Psychiatry, 46, 971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1997). Structured Clinical Interview for DSM-IV Axis I disorders (SCID I). New York: Biometric Research Department. [Google Scholar]
- Fonagy P (2015). The effectiveness of psychodynamic psychotherapies: An update. World Psychiatry, 14(2), 137–150. doi: 10.1002/wps.20235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Shelton RC, Hollon SD, Amsterdam JD, et al. (2009). Prediction of response to medication and cognitive therapy in the treatment of moderate to severe depression. Journal of Consulting and Clinical Psychology, 77(4): 775–787. doi: 10.1037/a0015401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, & Retzlaff PJ (1992). Clinical validation of the Quality of Life Inventory: A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment, 4, 92–101. doi: 10.1037/1040-3590.4.1.92. [DOI] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen NB, Lambert MJ, & Forman EV (2002). The psychotherapy dose-response effect and its implications for treatment delivery services. Clinical Psychology:Science and Practice, 9, 329–343. doi: 10.1093/clipsy.9.3.329. [DOI] [Google Scholar]
- Hatchett GT, Han K, & Cooker PG (2002). Predicting premature termination from counseling using the Butcher Treatment Planning Inventory Assessment. Counseling Psychologist, 9, 156–163. [DOI] [PubMed] [Google Scholar]
- Horvath AO, & Greenberg LS (1989). Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology, 36(2), 223–233. doi: 10.1037/0022-0167.36.2.223. [DOI] [Google Scholar]
- Horvath AO, Del Re AC, Flückiger C, & Symonds D (2011). Alliance in individual psychotherapy. Psychotherapy, 48(1), 9–16. doi: 10.1037/a0022186 [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens A, Kaplan AS, Watson SB, & Burns K (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess, 12(2), 210–24. doi: 10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lambert M (2007). Presidential address: What we have learned from a decade of research aimed at improving psychotherapy outcome in routine care. Psychother Res, 17(1), 1–4. doi: 10.1080/10503300601032506. [DOI] [Google Scholar]
- Lobbestael J, Leurgans M, & Arntz A (2011). Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clin Psychol Psychother, 18(1), 75–9. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Luborsky L (1984). Principles of psychoanalytic psychotherapy: A manual for supportive- expressive (SE) treatment. New York, NY: Basic Books. [Google Scholar]
- Ogrodniczuk JS, Joyce AS, & Piper WE (2005). Strategies for reducing patient-initiated premature termination of psychotherapy. Harvard Review of Psychiatry, 13, 57–70. [DOI] [PubMed] [Google Scholar]
- Oldham D Kellett S, Miles E et al. (2012). Interventions to increase attendance at psychotherapy: A meta-analysis of randomized controlled trials. Journal of Consulting and Clinical Psychology, 80(5), 928–939. doi: 10.1037/a0029630 [DOI] [PubMed] [Google Scholar]
- Olfson M, Mojitabai R, Sampson NA, Hwang I, Druss B, Wang PS,… Kessler RC, (2009). Dropout from outpatient mental health care in the United States. Psychiatr Serv. 60(7), 898–907. doi: 10.1176/appi.ps.60.7.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens PL, Hoagwood K, Horwitz SM, Leaf PJ, Poduska JM, Kellam SG, & Ialongo NS (2002). Barriers to children’s mental health services. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 731–738. [DOI] [PubMed] [Google Scholar]
- Pekarik G (1992). Posttreatment adjustment of clients who drop out early vs. late in treatment. Journal of Clinical Psychology, 48(3), 479–487. doi: [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN,….Keller MB (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Segal DL, Kabacoff RI, Hersen M, Van Hasselt VB, & Ryan CF (1995). Update on the reliability of diagnosis in older psychiatric outpatients using the Structured Clinical Interview for DSM-III-R. J of Clinical Geropsychology, 1, 313–321. [Google Scholar]
- Skre I, Onstad S, Torgersen S, & Kringlen E (1991). High interrater reliability for the Structured Clinical Interview for DSM-III-R Axis I (SCID-I). Acta Psychiatr Scand, 84(2), 167–73. doi: 10.1111/j.1600-0447.1991.tb03123.x. [DOI] [PubMed] [Google Scholar]
- Trajković G, Starčević V, Latas M, Leštarević M, Ille T, Bukumirić Z, & Marinković J (2011). Reliability of the Hamilton Rating Scale for Depression: A meta-analysis over a period of 49 years. Psychiatry Res, 189(1), 1–9. doi: 10.1016/j.psychres.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers W,H, & Reczek A (1995). Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: Summary of results from the Medical Outcomes Study. Medical Care, 33(4), 264–79. [PubMed] [Google Scholar]
- Ware JE Jr, Kosinski M, & Keller SD (1994). SF-36 physical and mental health summary scales: A user’s manual. Boston: Health Institute, New England Medical Center. [Google Scholar]
- Ware JE, & Sherbourne CD (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30, 473–483. [PubMed] [Google Scholar]
- Weissman AN (1980). Assessing depressionogenic attitudes: A validation study. Paper presented at 51st Annual Meeting of the Eastern Psychological Association, Hartford, CT. [Google Scholar]
- Weissman AN, & Beck AT (1978). Development and validation of the dysfunctional attitude scale. Paper presented at the Annual Meeting of the American Educational Research Association, Toronto, Canada. [Google Scholar]
- Williams JBW (1988). A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry, 45, 742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- Williams JBW, Gibbon M, First MB, Spitzer RL, Davis M, Borus J, …. Wittchen H (1992). The Structured Clinical Interview for DSM-III-R (SCID) II. Multi-site test-retest reliability. Arch Gen Psychiatry, 49, 630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- Yin S, Diehl CK, Gallop R, Crits-Christoph P, & Connolly Gibbons MB (2016). A self-report version of the ways of responding: Reliability and validity in a clinical sample. Psychotherapy Research, 1–12. doi: 10.1080/10503307.2016.1233367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC & Frankenburg FR (2001). Attainment and maintenance of reliability of axis I and axis II disorders over the course of a longitudinal study. Comprehensive Psych, 42(5), 369–374. doi: 10.1053/comp.2001.24556. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, …. McGlashan TH, Gunderson JG (2000). The Collaborative Longitudinal Personality Disorders Study: Reliability of axis I and II diagnoses. J Personal Disord, 14(4), 291–9. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]