Abstract
The aim of this study was to analyse the management of Gartland type III supracondylar humerus fractures in children older than 10 years at our paediatric orthopaedics and to determine the clinical and radiographic long-term effects following open reduction by the small medial approach and cross-fixation with three kirschner wires. Eighty-three cases of Gartland type III supracondylar humerus fractures in children older than 10 years were treated by open reduction by the small medial approach and cross-fixation with three kirschner wires from January 2010 to December 2015. All patients were followed up from 12 to 15 months (mean: 13 months). Assessments after 1 year included neurovascular examination, Flynn’s criteria (elbow function and carrying angle), pain and complications (infections, growth disturbances or iatrogenic nerve injuries). All fractures healed within 2 months. According to Flynn’s criteria, 80 (96.4%) patients achieved satisfactory outcomes, whereas three (3.6%) were graded as unsatisfactory because of limited elbow motion. The mean carrying angle measured 9.4° (1°–16°) compared with 10.8° on the contralateral side (5°–16°). No case of cubitus varus was noted. No wound infection and displacement of bone fracture occurred. No case of iatrogenic ulnar nerve injury and vascular deficits was noted. There were no cases of myositis ossificans or Volkmann’s ischaemic contracture. It is safe and effective to treat Gartland type III paediatric supracondylar humerus fractures in older children with open reduction by the medial approach and crossed K-wires fixation.
Keywords: cross-fixation, medial incision, older children, open reduction, supracondylar humerus fractures
Introduction
Supracondylar humerus fractures, the second most common type of paediatric fractures [1], according to Gartland’s criteria, are classified as nondisplaced fractures (type I), hinged fractures with the posterior cortex intact (type II) and completely displaced fractures (type III) [2]. Supracondylar humerus fractures occur most commonly during the first decade of life, but can also occur in children older than 10 years. Several studies showed higher incidence of displacement of supracondylar humerus fractures in older children and indicated that the number and configuration of the internal fixation should be modified according to age [3]. However, very few studies on the approach and internal fixation of the supracondylar humerus fractures for the older children have been carried out. We retrospectively analysed all the data of older children aged older than 10 years with Gartland type III supracondylar humerus fractures in our clinics between January 2010 and December 2015, and reported the clinical and radiographic long-term results.
Nonoperative and operative methods include long-arm plaster immobilization, axial traction applied using tape or a transolecranon pin, external fixation and percutaneous pinning with or without open reduction [4–6]. Percutaneous pinning after closed reduction is the most widely advocated technique, which usually produces a satisfactory cosmetic and functional result, and has become a standard method of treatment. However, sometimes, anatomical reduction is difficult to achieve by closed reduction when the patients with Gartland type III fracture present after a delay of a few days with swollen elbows. Also, the lack of fluoroscopy and radiation protective equipment precludes successful closed management. Residual dislocation may lead to cubitus varus, especially in older children [7]. At the same time, iatrogenic ulnar nerve injury may occur during the procedure of cross pinning [8]. Therefore, open surgery that ensures anatomical restoration is suggested in patients with severely displaced Gartland type III fractures when closed reduction fails. Posterior open reduction showed worst results, whereas medial and lateral open reduction groups showed good to excellent results [9–11]. At our institution, the medial mini-open approach is applied routinely for open reduction.
Although the skeletons of the older children are similar to adults, they still have growth potential because the epiphyseal plate is open. Kirschner wire was preferred in the fixation of the fracture, but the mechanical strength of the internal fixation needs be higher in older children. Several studies have shown the biomechanical superiority of crossed K-wires [12,13]. At our institution, three crossed K-wires were used for fixation in older children. In this study, we reported the clinical and radiographic long-term effects of children older than 10 years of age with Gartland type III supracondylar humerus fractures who were treated with open reduction by the medial approach, followed by crossed K-wires fixation.
Patients and methods
Our Institutional Review Board approved the protocol for this project. We retrospectively reviewed the medical records and radiographs of 607 children who underwent open reduction for type III supracondylar humerus fractures at our institution between January 2010 and December 2015. Ninety patients were older than 10 years of age. Patients were included if they fulfilled the following criteria: widely displaced supracondylar humerus fractures (Gartland type III injuries) without vascular injury (Fig. 1), older than 10 years of age with open epiphyseal plates of the distal humerus, with a minimum follow-up of 1 year. Skeletally mature adults and patients with associated bony injuries in the same limb and fractures treated with closed reduction and incomplete data were excluded. A total of five patients could not be traced and their data were excluded. One patient with associated radius fracture in the same limb was excluded. One patient with vascular injury was excluded. Eighty-three patients fulfilled these criteria and there were 61 (73.5%) boys and 22 (26.5%) girls. Seventy-one (85.5%) patients had extension-type fracture and 12 (14.5%) had a flexion-type fracture. The mode of trauma was as follows: fall while playing in 50 (60.2%), fall from height in 23 (27.7%), traffic accidents in seven (8.4%) and blunt trauma in three (3.6%). Associated nerve palsy was radial nerve palsy in two (2.4%), median nerve palsy in two (2.4%) and ulnar nerve palsy in one (1.2%). All of the patients were hospitalized and cross pinning after open reduction by the medial approach was applied.
Fig. 1.
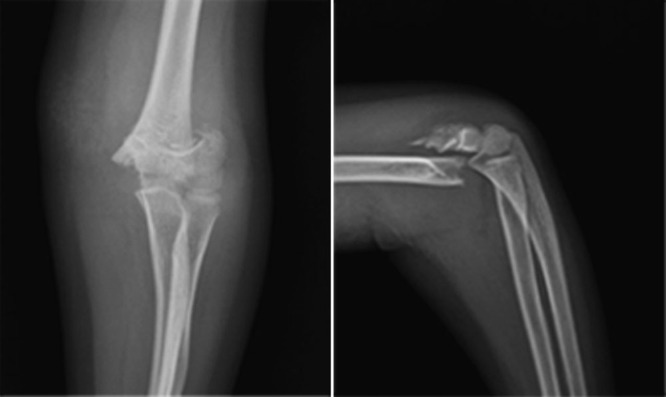
Anteroposterior and lateral radiographic views showing a Gartland type III supracondylar fracture of the humerus in a 10-year-old girl.
Surgical technique
Surgery was performed under general anaesthesia by a senior surgeon in all 83 patients. With the patient supine, the injured limb was placed on the operating table in abduction and external rotation. A medial incision was made starting from the medial epicondyle and extending proximally for 3–4 cm. The ulnar nerve, often displaced anteriorly in a flexed elbow, was identified and protected. The fracture site was then approached by the intermuscular interstice and the fracture haematoma was drained. The entire anterior and medial bone was well visualized. The elbow was flexed and gentle traction was applied to disengage and visualize the distal fragment. After achieving anatomical reduction, two k-wires (1.5 mm or 2.0 mm in diameter) were inserted percutaneously from lateral to medial. The medial wire (1.5 mm in diameter) was placed percutaneously 0.5–1 cm from the edge of the incision and beginning at the medial epicondyle to engage the lateral cortex. The distance between the crossed k-wires on the fracture plane is more than 1/3 of the width of the humerus on the same plane (Fig. 2). After checking for the capillary refill of the subcutaneous tissue and elbow movements, the wound was irrigated with saline and closed in two planes with a continuous intradermal suture. The wires were bent and cut long to facilitate subsequent removal without anaesthesia. A check radiograph was obtained postoperatively. A long-arm plaster cast with the elbow flexed at 90° was used in all patients for 30 days. Both the parents and the children were instructed on rehabilitative exercises to be continued at home.
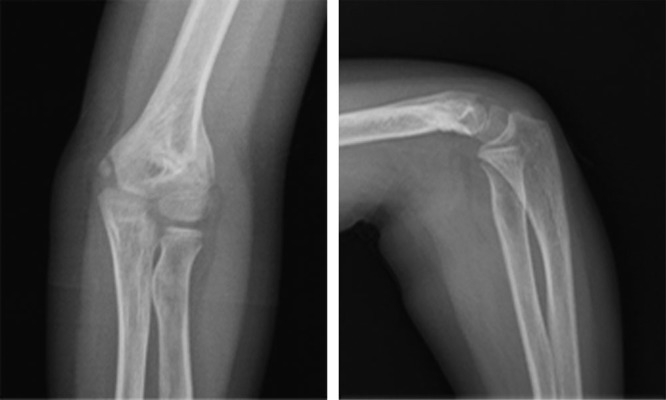
Fig. 2.

Radiography was used for confirmation of the reduction and location of the K-wires. Anteroposterior and lateral views showed satisfactory fracture reduction.
Clinical and radiographic examination
All patients were followed up for at least 1 year after the initial treatment. Follow-up monitoring included regular clinical and radiographic examination of the patients at 1 and 2 and 12 months after surgery. The cast and the wires were removed at the 4–6-weeks follow-up appointment when osteal callus formed and the fracture line blurred. K-wires would be kept for two more weeks if there was not enough callus around the fracture line.
Radiographic evaluation included anteroposterior and lateral radiographs of the injured elbow, which were prepared at each follow-up examination. The healing processes of fracture were confirmed by the radiographs (Fig. 3). The humeroulnar angle was calculated on the anteroposterior radiograph. The humeroulnar angle was defined by the intersection of the midhumeral line with the line drawn from the proximal midpoint of the ulna to the distal midpoint of the ulna in the anteroposterior view on a radiograph with the elbow extended to 0° and the forearm supinated.
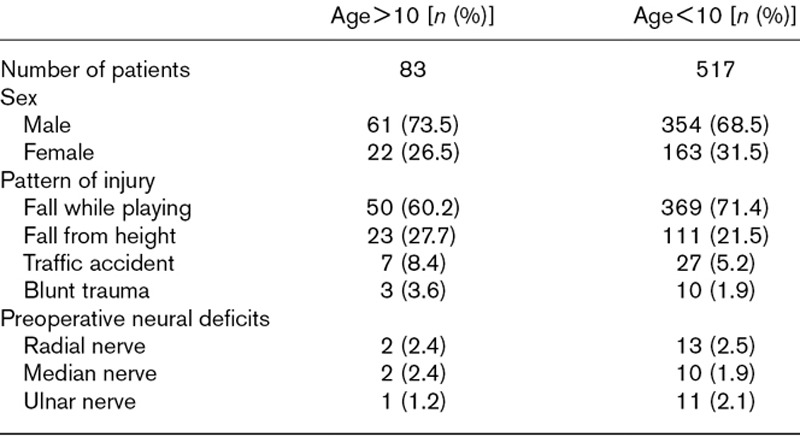
Fig. 3.
Radiography was used to evaluate the healing of the fracture. Anteroposterior and lateral views 2 months after surgery showed satisfactory fracture restoration.
Clinical evaluation included neurovascular examination, measurement of the range of motion of the injured elbow, assessment of the carrying angle, pain and determination of any complications such as infections or iatrogenic nerve injuries. The range of motion of the injured elbow was measured using a manual full-circle goniometer. The clinical results were graded according to Flynn’s criteria, which are based on the carrying angle and the elbow motion [14]. The carrying angle was measured using a full-circle goniometer and compared with that of the contralateral arm.
Statistical analysis
Statistical analysis was carried out using the SPSS statistical package program (SPSS 19.0 version; SPSS Inc., Chicago, Illinois, USA). The t-test was performed to compare the injured and uninjured elbows. The null hypothesis was that the mean extension and carrying angle in the injured elbows after fixation would be the same as those in the uninjured elbows (controls). We used a P value less than 0.05 to determine statistical significance of the corresponding variables.
Results
During the study period, 83 surgically treated paediatric patients with supracondylar humerus fractures fulfilled the criteria for inclusion and were finally enroled in this series (Table 1). Incomplete primary reduction was not encountered in any of our patients. Osteal callus formed and the fracture line blurred at the 30-day follow-up appointment in all patients. Successful fracture healing was achieved 2 months after surgery in all of our patients (100%). The humeroulnar angle averaged 10.1° (range: 1°–17°). No malunions was found in our series (cubitus varus).
Table 1.
Demographics of the patients
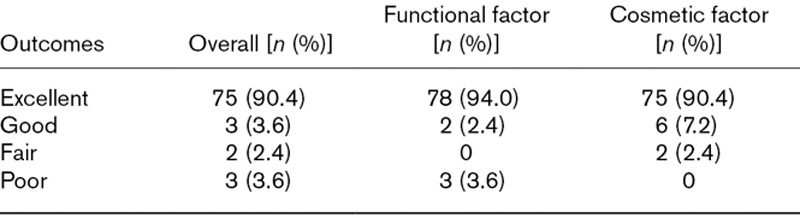
Many scoring systems have been used for elbow disorders. In this study, Flynn’s criteria were used to evaluate the functional and cosmetic results (Table 2). Although 78 (94.0%) patients achieved excellent results and two (2.4%) patients achieved good functional results, three (3.6%) were graded as unsatisfactory because of limited elbow motion. In the remaining three patients classified as having achieved unsatisfactory results, two had an extension deficit of 16° and one had a flexion deficit of 20°. None of the patients had a cubitus varus. Seventy-five (90.4%) patients achieved excellent results, six (7.2%) patients achieved good results and two (2.4%) patients achieved fair cosmetic results. The mean carrying angle measured 9.4° (1°–16°) compared with 10.8° on the contralateral side (5°–16°; Table 3). At the 1-year follow-up examination, none of the patients complained about any relevant pain symptoms. Five (6.0%) peripheral nerve lesions were observed in the first physical examination at admission and resolved spontaneously after an average of 15 weeks (range: 8–20 weeks). There was no case of iatrogenic ulnar nerve injury. Four (4.8%) superficial pin infections were found at follow-up and resolved by appropriate dressing with povidone iodine solution. No antibiotics were administered again.
Table 2.
Flynn’s criteria
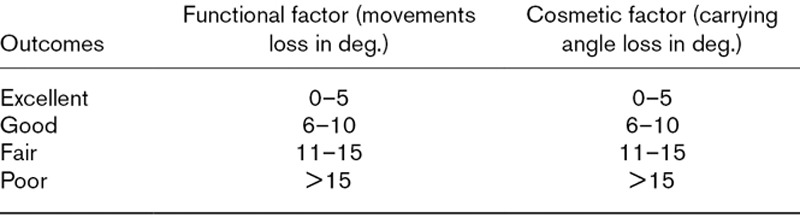
Table 3.
Outcomes according to Flynn’s criteria
Discussion
Supracondylar humerus fracture is one of the most common injuries in children, accounting for 50–80% of all paediatric elbow fractures [15]. During the past 5 years, more than 600 patients were treated for supracondylar humerus fracture in our department. About 12% of the patients were children older than 10 years of age. The main goals in paediatric supracondylar fracture treatment are as follows: achievement of normal cosmetic view of elbow, full recovery of elbow movements and protecting the patient from neurovascular complications that may occur. A common complication of paediatric supracondylar fractures is cubitus varus [2]. Biomechanical tests have shown that stress and strain of the medial part of the distal humerus are greater than the lateral part under the axial load. Internal rotation of the distal fragment is the major predisposing factor to varus deformity and is necessary for coronal varus tilt [7]. Stable reduction and fixation are important to prevent displacement of the distal fragment and postoperative deformity [16]. The appropriate strength of fixation was different because the stress of the fracture varies with age and type. Several studies have shown higher incidence of displacement of supracondylar humerus fractures in older children [3]. Satisfactory results can be achieved in Gartland type I and II fractures through closed reduction and immobilization by plaster or percutaneous pinning, which is not feasible in Gartland type III fractures as the fracture is usually associated with extremely swelling in the elbow region. Closed reduction may fail in situations such as delayed presentation and shortage of imaging facility. Soft tissue injuries and stripping of the periosteum resulting from repeated manual reduction were similar to those with open reduction. Percutaneous pinning may be dangerous as surface marking of bony landmarks is difficult. Royce et al. [17] treated 143 children with percutaneous crossed K-wires and described three ulnar secondary nerve palsies. Therefore, open reduction and internal fixation have been accepted for these widely displaced fractures with severe swelling not allowing acceptable closed reduction and primary neural disruption.
Four different surgical approaches have been described and every approach has its own advantages [9–11,18]. Anterior incision offers the advantage of a smaller scar and easy access to structures that might be injured between the fractured fragments. Ersan and colleagues reported that all 46 patients achieved satisfactory results on comparison of the anterior and lateral approach in the treatment of extension-type supracondylar humerus fractures in children. However, it is more technically demanding and excessive retraction of the wound can injure the ulnar nerve. The posterior approach is better than the other approaches in manipulation of fracture fragments, but it leads to poor functional results because of soft tissue injuries and fibrous surgical scars [11]. Medial and lateral open reduction approaches lead to similar cosmetic outcomes and functional results. However, Weiland et al. [19] reported a higher incidence of cubitus varus with the use of the lateral approach, which does not allow complete visualization of the medial column communication and tilt. The medial approach provides good visualization, ensuring the restoration of the medial column, and it is a method that induces the least incision scar. At the same time, the influence on the elbow appearance is minimal because the medial approach is hidden.
In our study, three patients showed poor functional results, whereas none of the patients showed poor cosmetic results. We believe that more follow-up and physical training under the guidance of rehabilitation doctors may be needed to improve the range of motion in the elbow. Several studies have reported that iatrogenic ulnar nerve injuries are encountered in about 6% of patients with supracondylar fractures during percutaneous pinning, including direct penetration or laceration of the nerve or tacking down the nerve sheet in a nonanatomical position [20]. The medial approach allows fracture reduction under visual guidance, which limits the risk of ulnar nerve injury, and has been recommended by several authors [21]. The middle finger of the surgeon touches the broken end of the fracture through the medial incision to assist reduction. Anatomical reduction can always be achieved under the assistance of the finger. In our study, we did not encounter any iatrogenic ulnar nerve palsy. This finding was in agreement with many studies.
In the management of Gartland type III fractures, different pin configurations are used. Yaokreh et al. [22] reported that the postoperative secondary displacement rates were 10.4% in a case-series of cross-wire fixation. Flynn et al. [14] described three 72 (4.2%) patients with a cosmetically unsatisfactory result because of loss in the carrying angle. Shim and Lee [23] reported one patient with a cubitus varus deformity in their series of 63 (1.6%) patients treated by cross-fixation with three K-wires. Crossing of the pins in the fracture site is associated with secondary displacement. Skaggs et al. [24] recommended using three diverging lateral epicondylar pins when concerns arose about the stability of the fixation. The internal fixation should be more stable for older children. Several studies have shown that cross pinning provides more stable fixation than lateral diverge or parallel pinning, and reduces the incidence of cubitus varus because of the displacement of the distal part of the fracture [9,10]. In our study, fractures were fixed with three crossed K-wires (two inserted from the lateral side, followed by one from the medial side). Keeping the lateral K-wires apart and the cross points of these three K-wires proximal to the fracture line can lead to more stable fixation. No loss of reduction was found in our series. However, the carrying angle of the injuried elbow reduced 10°–15° compared with the contralateral side in two patients. It may be because the medial cortical compression remained when the lateral cortical continuity was restored. Considering the cosmetic factor, we should compare the injured side with the normal side to ensure that the carrying angle of elbows is similar.
In terms of our method of treatment, none of these patients had a significant cubitus varus or iatrogenic ulnar nerve injury. Also, no Volkmann ischaemic contractures or compartment syndromes were observed. All patients were followed up from 12 to 15 months, which may be considered adequate for screening possible complications. One limitation of this study was the lack of a control group for comparison.
Conclusion
Open reduction by the medial approach and cross-fixation with three kirschner wires for severely displaced Gartland type III fractures is a safe and effective method with a low incidence of complications for older children.
Acknowledgements
All authors have participated sufficiently in this work concerning conception and design of this study, drafting the article, critical revision for important intellectual content, and final approval.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: a study of 3350 children. J Orthop Trauma. 1993;; 7:15–22 [DOI] [PubMed] [Google Scholar]
- 2.Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;; 109:145–154 [PubMed] [Google Scholar]
- 3.Reisoglu A, Kazimoglu C, Hanay E, Agus H. Is pin configuration the only factor causing loss of reduction in the management of pediatric type III supracondylar fractures? Acta Orthop Traumatol Turc. 2017;; 51:34–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mulpuri K, Tritt BL. Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J Orthop Trauma. 2006;; 20:234. [DOI] [PubMed] [Google Scholar]
- 5.Sharma A, Kahal K, Sharma S. Transolecranon and lateral Kirschner wire fixation for displaced supracondylar humeral fracture in children. J Orthop Surg (Hong Kong). 2015;; 23:319–322 [DOI] [PubMed] [Google Scholar]
- 6.Krusche-Mandl I, Aldrian S, Kottstorfer J, Seis A, Thalhammer G, Egkher A. Crossed pinning in paediatric supracondylar humerus fractures: a retrospective cohort analysis. Int Orthop. 2012;; 36:1893–1898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tellisi N, Abusetta G, Day M, Hamid A, Ashammakhi N, Wahab KH. Management of Gartland’s type III supracondylar fractures of the humerus in children: the role audit and practice guidelines. Injury. 2004;; 35:1167–1171 [DOI] [PubMed] [Google Scholar]
- 8.Lyons JP, Ashley E, Hoffer MM. Ulnar nerve palsies after percutaneous cross-pinning of supracondylar fractures in children’s elbows. J Pediatr Orthop. 1998;; 18:43–45 [PubMed] [Google Scholar]
- 9.Hussain S, Dhar S, Qayoom A. Open reduction and internal fixation of displaced supracondylar fractures of humerus with crossed k-wires via medial approach. Malays Orthop J. 2014;; 8:29–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pretell-Mazzini J, Rodriguez-Martin J, Aunon-Martin I, Zafra-Jimenez JA. Controversial topics in the management of displaced supracondylar humerus fractures in children. Strategies Trauma Limb Reconstr. 2011;; 6:43–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pretell Mazzini J, Rodriguez Martin J, Andres Esteban EM. Surgical approaches for open reduction and pinning in severely displaced supracondylar humerus fractures in children: a systematic review. J Child Orthop. 2010;; 4:143–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pennock AT, Charles M, Moor M, Bastrom TP, Newton PO. Potential causes of loss of reduction in supracondylar humerus fractures. J Pediatr Orthop. 2014;; 34:691–697 [DOI] [PubMed] [Google Scholar]
- 13.Sankar WN, Hebela NM, Skaggs DL, Flynn JM. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg Am. 2007;; 89:713–717 [DOI] [PubMed] [Google Scholar]
- 14.Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. 1974;; 56:263–272 [PubMed] [Google Scholar]
- 15.Houshian S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci. 2001;; 6:312–315 [DOI] [PubMed] [Google Scholar]
- 16.Eren A, Guven M, Erol B, Akman B, Ozkan K. Correlation between posteromedial or posterolateral displacement and cubitus varus deformity in supracondylar humerus fractures in children. J Child Orthop. 2008;; 2:85–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Royce RO, Dutkowsky JP, Kasser JR, Rand FR. Neurologic complications after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop. 1991;; 11:191–194 [DOI] [PubMed] [Google Scholar]
- 18.Ersan O, Gonen E, Arik A, Dasar U, Ates Y. Treatment of supracondylar fractures of the humerus in children through an anterior approach is a safe and effective method. Int Orthop. 2009;; 33:1371–1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiland AJ, Meyer S, Tolo VT, Berg HL, Mueller J. Surgical treatment of displaced supracondylar fractures of the humerus in children. Analysis of fifty-two cases followed for five to fifteen years. J Bone Joint Surg Am. 1978;; 60:657–661 [PubMed] [Google Scholar]
- 20.Ozkoc G, Gonc U, Kayaalp A, Teker K, Peker TT. Displaced supracondylar humeral fractures in children: open reduction vs. closed reduction and pinning. Arch Orthop Trauma Surg. 2004;; 124:547–551 [DOI] [PubMed] [Google Scholar]
- 21.Kumar R, Kiran EK, Malhotra R, Bhan S. Surgical management of the severely displaced supracondylar fracture of the humerus in children. Injury. 2002;; 33:517–522 [DOI] [PubMed] [Google Scholar]
- 22.Yaokreh JB, Gicquel P, Schneider L, Stanchina C, Karger C, Saliba E, et al. Compared outcomes after percutaneous pinning versus open reduction in paediatric supracondylar elbow fractures. Orthop Traumatol Surg Res. 2012;; 98:645–651 [DOI] [PubMed] [Google Scholar]
- 23.Shim JS, Lee YS. Treatment of completely displaced supracondylar fracture of the humerus in children by cross-fixation with three Kirschner wires. J Pediatr Orthop. 2002;; 22:12–16 [PubMed] [Google Scholar]
- 24.Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001;; 83-a:735–740 [PubMed] [Google Scholar]


