Abstract
OBJECTIVES:
Addressing procedure‐related anxiety should improve adherence to colorectal cancer screening programs and diagnostic colonoscopy. We performed a systematic review to assess anxiety among individuals undergoing colonoscopy or flexible sigmoidoscopy (FS).
METHODS:
We searched multiple electronic databases for studies evaluating anxiety associated with colonoscopy or FS published from 2005 to 2017. Two reviewers independently identified studies, extracted data, and assessed study quality. The main outcomes were the magnitude of pre‐procedure anxiety, types of concerns, predictors of anxiety, and effectiveness of anxiety‐lowering interventions in individuals undergoing lower endoscopy. The protocol was prospectively registered in PROSPERO.
RESULTS:
Fifty‐eight studies (24,490 patients) met the inclusion criteria. Patients undergoing colonoscopy had a higher mean level of anxiety than that previously reported in the general population, with some studies reporting more than 50% of patients having moderate‐to‐severe anxiety. Areas of anxiety‐related concern included bowel preparation, difficulties with the procedure (embarrassment, pain, possible complications, and sedation), and concerns about diagnosis; including fear of being diagnosed with cancer. Female gender, higher baseline anxiety, functional abdominal pain, lower education, and lower income were associated with greater anxiety prior to colonoscopy. Providing higher‐quality information before colonoscopy, particularly with a video, shows promise as a way of reducing pre‐procedure anxiety but the studies to date are of low quality.
CONCLUSIONS:
A large proportion of patients undergoing colonoscopy report anxiety before the procedure. Improvement in pre‐procedure information delivery and evaluation of approaches to reduce anxiety is required, especially for those with predictors of pre‐procedure anxiety.
BACKGROUND
In North America, colorectal cancer (CRC) remains the second most common cause of cancer‐related deaths, after lung cancer [1, 2]. However, CRC mortality rates have declined in many developed countries [3, 4], and it is believed that screening has had a large role in this trend [5,6,7,8]. A model by Edwards et al. [5] estimated that screening accounted for 53% of the CRC mortality reduction for the period 1975‐2000 in the United States. Screening can reduce CRC mortality by detecting early‐stage CRC and by detecting and removing precancerous lesions [9]. In North America, the CRC screening rate among people of 50‐74 years of age is only 55‐58% [10]. This indicates that CRC screening is still underutilized in a substantial portion of the population. There are many barriers associated with this low uptake at the patient, provider, and system levels [11]. Numerous studies have looked for ways to address these barriers in order to improve uptake of screening [12].
Tests such as the fecal occult blood test are often used as a first step in CRC screening. Colonoscopy and flexible sigmoidoscopy (FS) are also essential first or intermediate tests for CRC screening and are also used widely for other diagnostic purposes. Among all the barriers to acceptance of a recommendation for CRC screening, anxiety associated with colonoscopy or FS is a commonly cited factor [13,14,15,16,17,18,19,20,21,22]. A better understanding of anxiety concerning these procedures may help in development of measures to reduce preprocedure anxiety and improve acceptance.
The term anxiety covers a wide range of topics. For this review, we use a health anxiety perspective [23]. Health is one of the most important sources of security in life. Health anxiety focuses on the range of anxiety concerning one's health. We consider health anxiety to be a dimensional rather than a categorical construct. Categorical measures are used in some studies in this area, and when they are used, we describe the strengths and weaknesses of these measures. Health anxiety may cause people to increase their use of health services (to be vigilant for possible health problems) or to reduce their use of health services (for fear of finding health problems that are alarming).
The relationship between anxiety and screening adherence is complex and Consedine et al. proposed that it is the result of the interplay of several variables, including the source of anxiety and the degree of anxiety [24]. For example, specific anxiety toward procedural pain or embarrassment will deter screening, while a generalized anxiety of cancer may promote screening [24]. Furthermore, patients with either minimal or extreme anxiety of cancer may be less likely to pursue screening compared with those with “moderate” anxiety [24]. Therefore, an improved understanding of the degree and types of anxiety patients have is necessary for developing interventions aimed to improve screening adherence. Moreover, reduction in anxiety would be beneficial to patients, whether or not this causes an increase in adherence to recommendations for colonoscopy.
To the best of our knowledge, there are no systematic reviews synthesizing information on pre‐procedure anxiety concerning colonoscopy or FS.
The objectives of this systematic review were to assess the magnitude of anxiety, types of concerns, predictors of anxiety, and anxiety‐lowering interventions in patients undergoing colonoscopy or FS.
METHODS
Protocol and registration
We conducted this systematic review in accordance to the Methodological Expectations of Cochrane Intervention Reviews (MECIR) guidelines and reported as per the Preferred Reporting Items for Systematic Reviews and Meta‐analysis (PRISMA) guidelines for systematic review and meta‐analysis [25, 26]. An a priori protocol was published in PROSPERO according to the aforementioned guidelines (CRD42017069365).
Search strategy
The electronic databases MEDLINE, EMBASE, CINAHL, PsychInfo, Web of Science, Cochrane Library, and Scopus were searched for relevant studies from 2005 to 2017 and published in English or French. We limited the searches to articles published in or after 2005, as we were interested in studies most relevant to the current practices: patient education and clinical practices (e.g., sedation and indications of procedures) have changed over time. The search strategies were designed specific to each database by a librarian with expertise in a systematic review search methodology, with input from the review team. The search strategies were peer‐reviewed by a second librarian with expertise in a systematic review search methodology. The search strategy used for MEDLINE (Ovid) database is provided in Supplementary Appendix 1.
Study selection
The clinical questions for this review were (1) what is the magnitude of pre‐procedure anxiety in patients undergoing colonoscopy or FS?; (2) what are the concerns related to the anxiety of undergoing colonoscopy or FS?; (3) what are the predictors of this anxiety?; and (4) which interventions are effective in lowering this anxiety? We included observational and experimental studies in adults (aged ≥ 16) being considered or undergoing colonoscopy or FS. For the fourth question, we only included randomized controlled trials.
Two reviewers (C.Y. and V.S.) independently screened the title and abstracts of references retrieved from the database search, and categorized them as either “include,” “exclude,” or “unsure.” Then, the full texts of references marked as “include” and “unsure” were further reviewed independently by these two reviewers for eligibility, and eventually categorized as “included” or “excluded.” The reasons for studies excluded at the full text screening stage are provided. Disagreements were resolved by mutual discussion or consultation with a third reviewer (H.S.).
Data collection process and data items
We developed a data extraction form of predefined items, pilottested it, and revised it accordingly. One reviewer (C.Y.) extracted the data from included studies and a second reviewer (V.S.) verified the extracted data to avoid transcription errors. Only published studies were included in this analysis. The following data items were extracted from each included study when available: study information (country, study design, number of centers, funding sources, indications for colonoscopy/FS, open‐access endoscopy vs. consultation, inclusion, and exclusion criteria), study participants (sample size, age, percent of males, withdrawals or loss to follow‐up, and history of previous colonoscopy/FS), outcome measure (anxiety measure), timing of anxiety assessment relative to endoscopy, magnitude of anxiety, patient‐reported concerns related to anxiety, predictors of anxiety, and anxiety‐lowering interventions (type, adherence, timing of intervention relative to endoscopy, and degree of anxiety reduction).
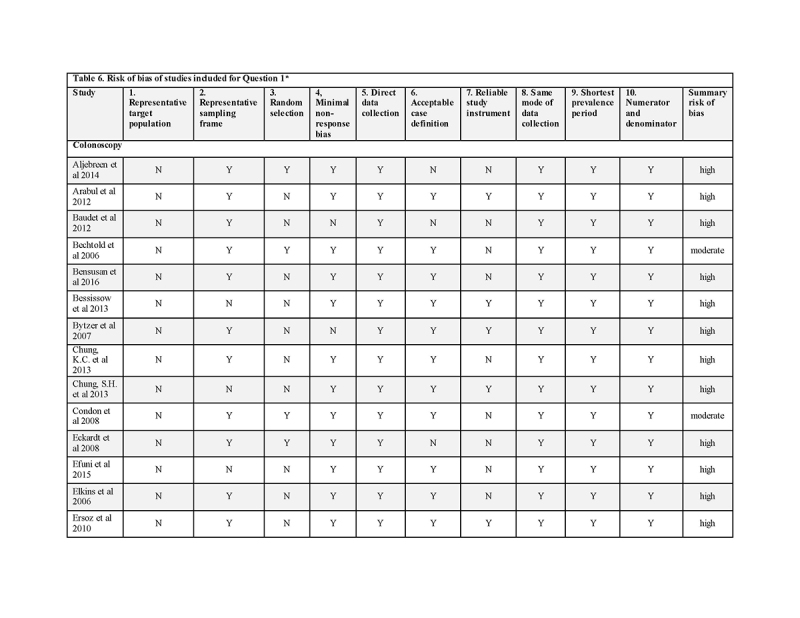
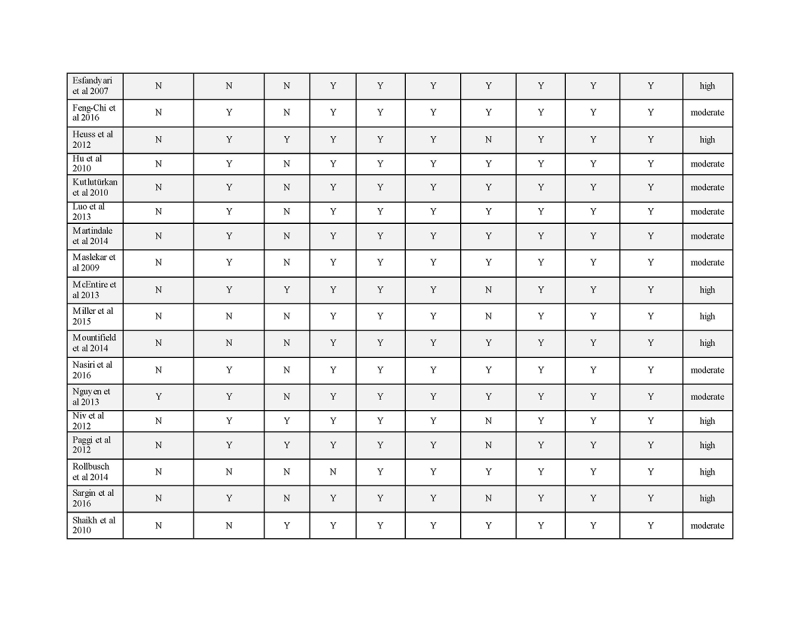
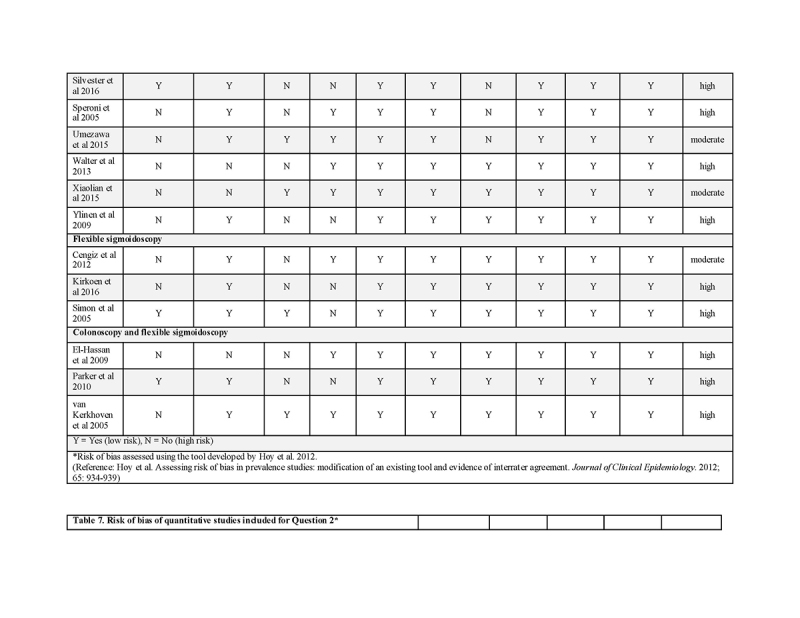
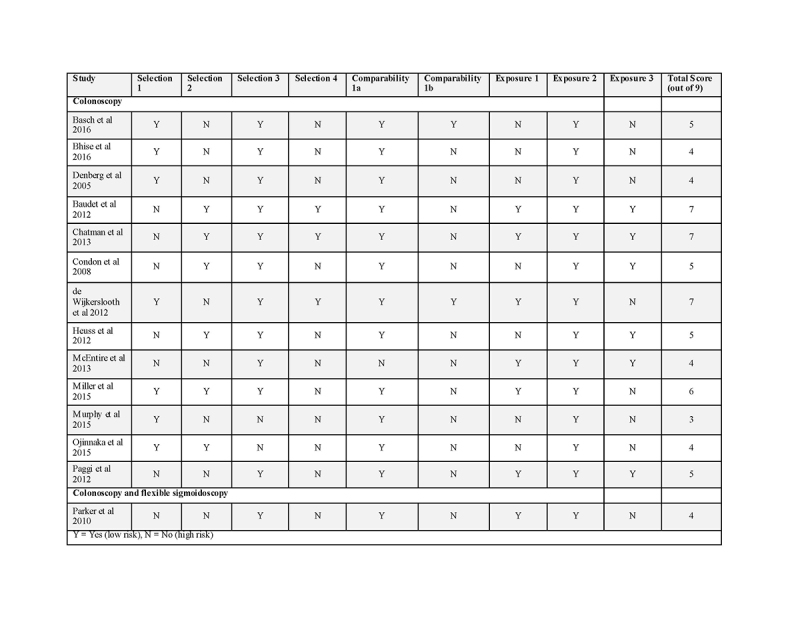
Quality assessment
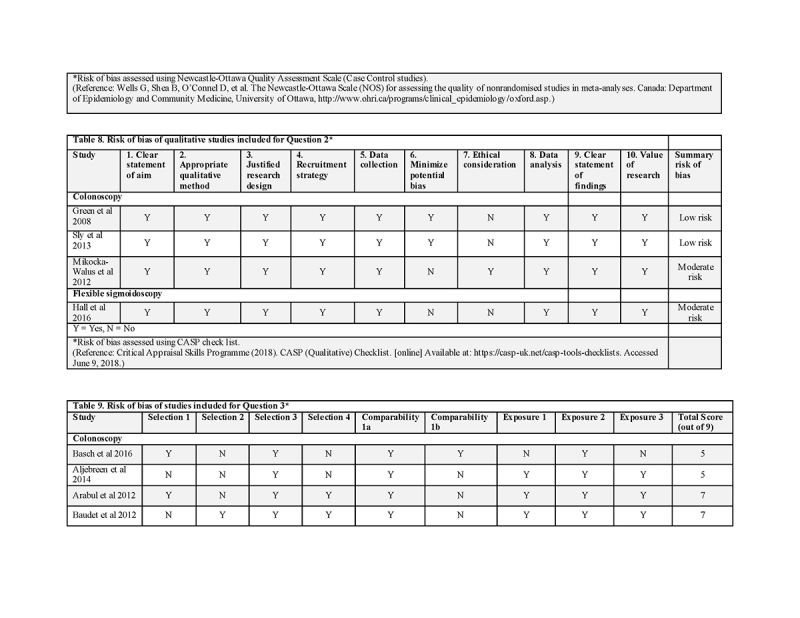
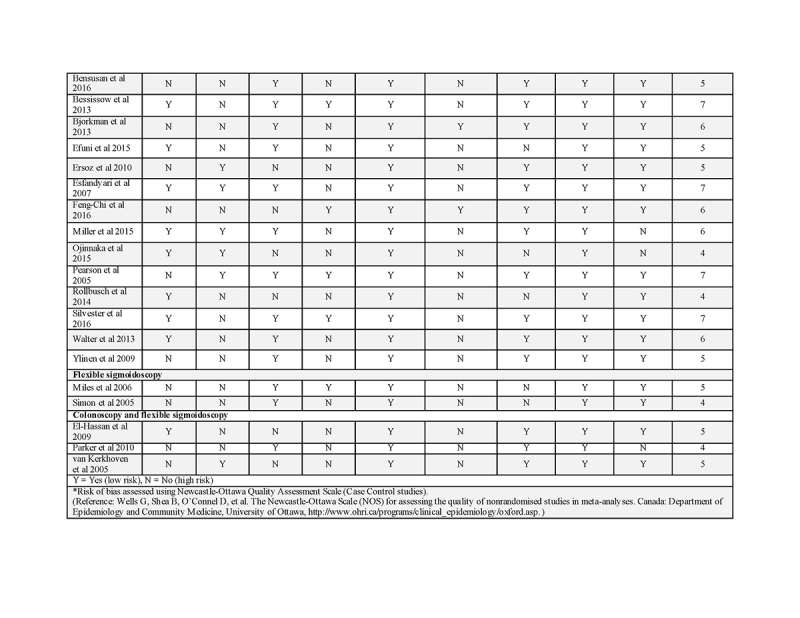
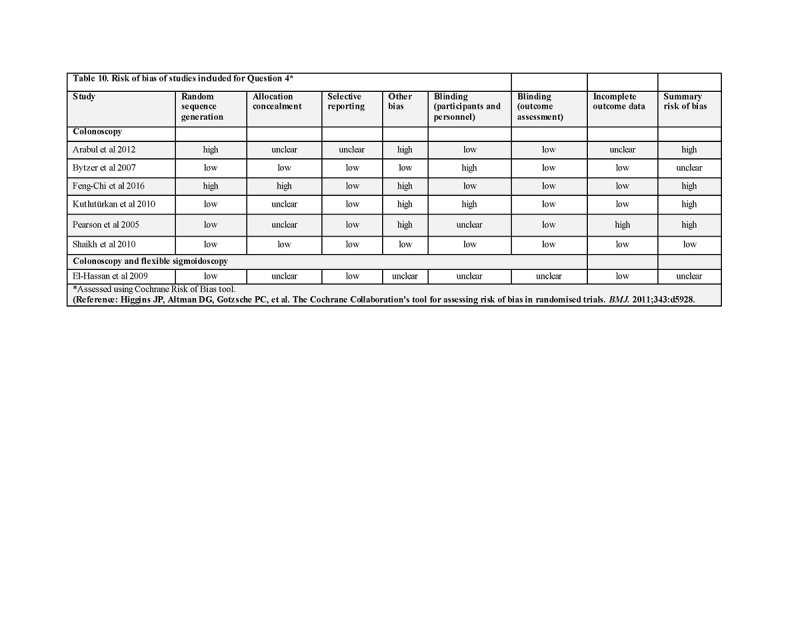
Risk of bias assessments were performed separately for studies included under each of the four clinical questions. Prevalence studies included for question 1 were assessed using the tool developed by Hoy et al. [27]. Quantitative studies addressing question 2 and 3 were assessed using the Newcastle‐Ottawa Scale (NOS) for case‐control studies [28]. Each trial was judged on selection of the study groups, comparability of the groups, and ascertainment of exposure or outcome of interest. Qualitative studies for question 2 and 3 were assessed using the CASP (Qualitative) Checklist [29]. The randomized trials of question 4 were assessed using the Cochrane Risk of Bias tool [30]. This tool assesses seven domains: random sequence generation, allocation concealment, selective reporting, other sources of bias, blinding of participants and personnel, blinding of outcome assessors, and incomplete outcome data. The overall risk of bias is based on responses to these individual domains and is rated as “high risk,” “low risk,” or “unclear risk”.
Outcome measures
The outcome measures of interest were the magnitude of anxiety, patient‐reported concerns related to anxiety, predictors of anxiety, and effectiveness of anxiety‐lowering interventions in patients undergoing colonoscopy or FS.
Evidence summary
The results of included studies were summarized with respect to the four key questions they addressed and were stratified for colonoscopy and FS. Due to the significant heterogeneity of the studies included with regard to study design, patient populations, and outcome data, a quantitative pooling (e.g., meta‐analysis) was not performed. Instead, the data were analyzed using a qualitative approach and presented in a narrative format. Cohen's d [31] was calculated to estimate effect size wherever possible if enough data (i.e., mean and standard deviation) were provided by the study. Cohen's d is defined as the difference between two means divided by a standard deviation for the data, for example, the pooled standard deviation. Cohen suggested that d = 0.2 be considered a “small” effect size, 0.5 represents a “medium” effect size, and 0.8 a “large” effect size (see http://rpsychologist.com/d3/cohend) [32].
A post hoc sensitivity analysis was performed in response to peer review comments to identify potential influence of several factors on the outcome measures (i.e., magnitude of anxiety), including patient demographics (age and sex), country of origin, year of study, study design, indication of endoscopy, and time assessed prior to endoscopy. Any patterns that emerged were presented in a narrative format.
RESULTS
Study selection
The search of the databases yielded a total of 292 records, of which 58 studies (24,490 participants) met the inclusion criteria and were included in the final review (Fig. 1).
Fig. 1.
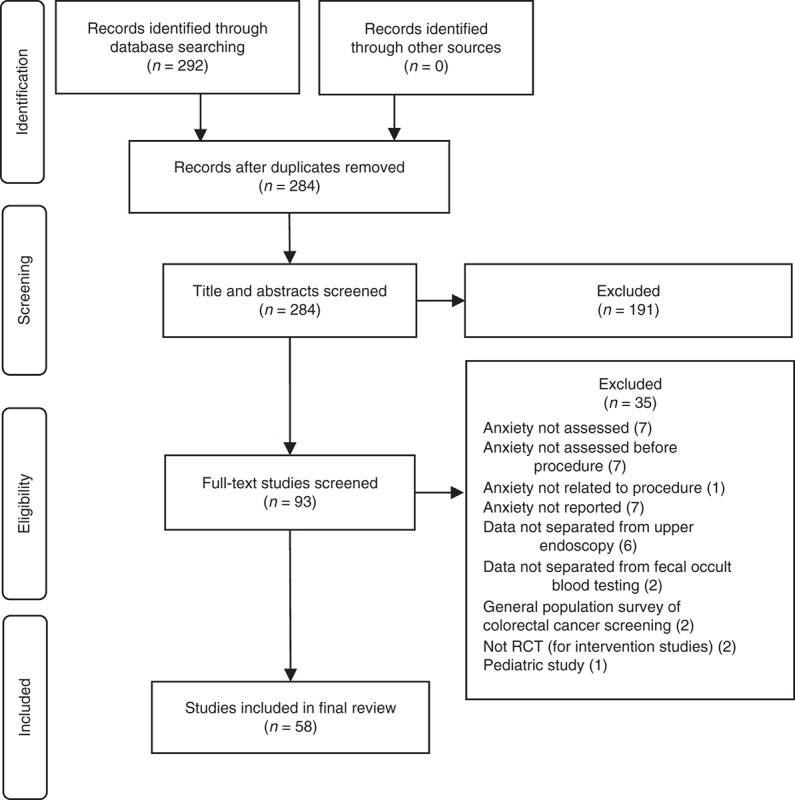
Study selection flow diagram
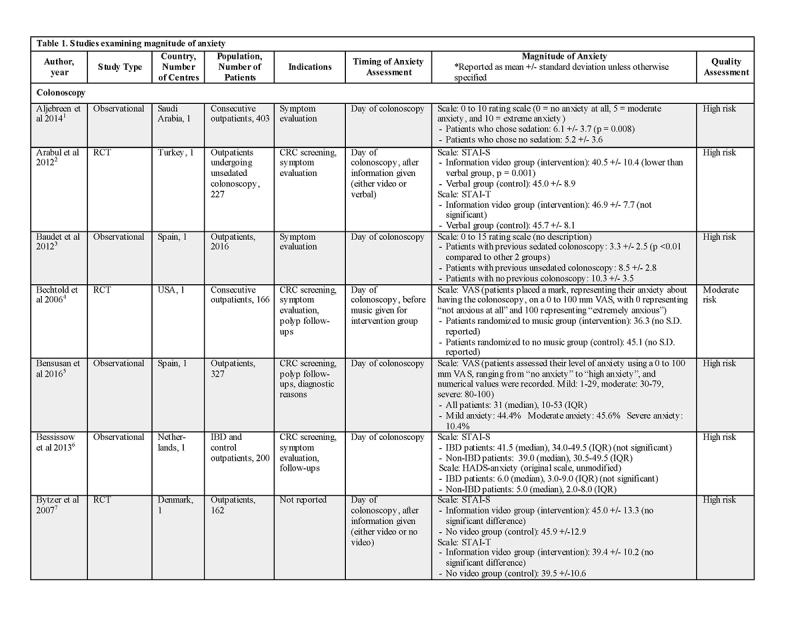
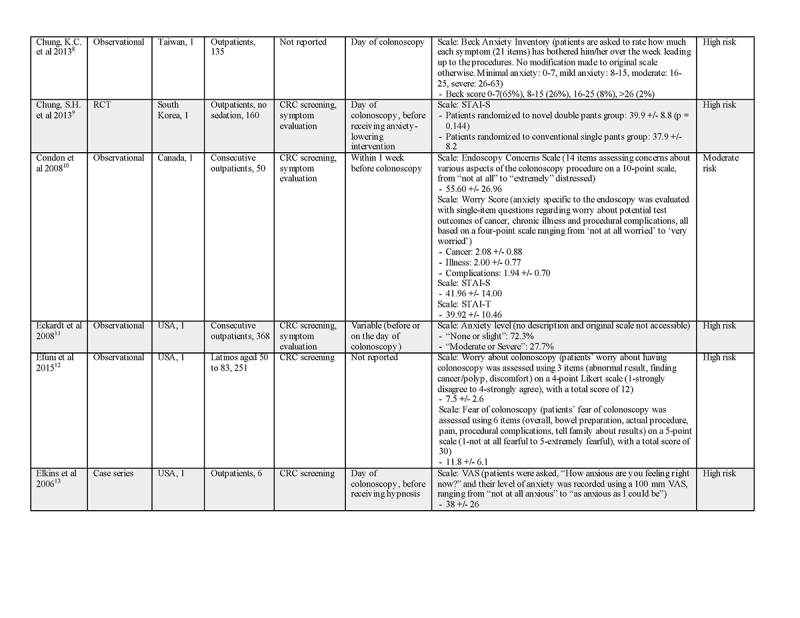
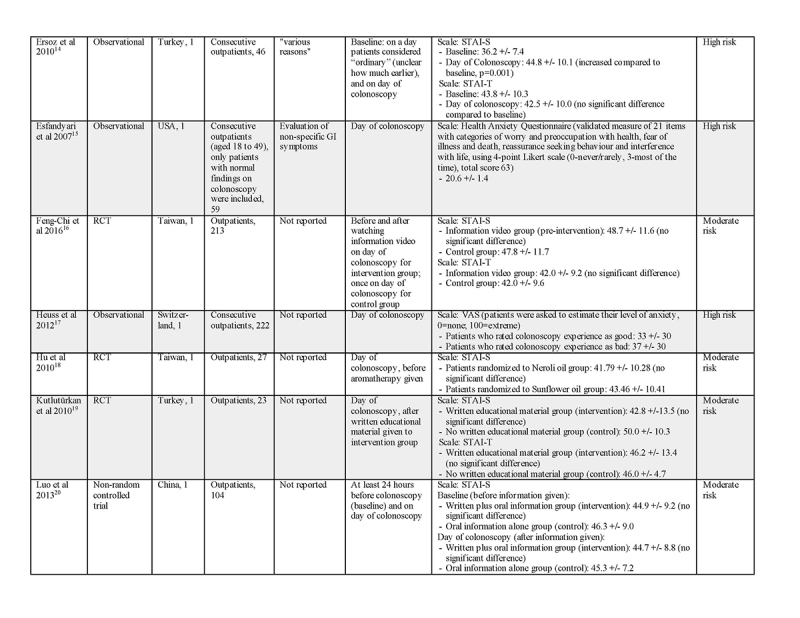
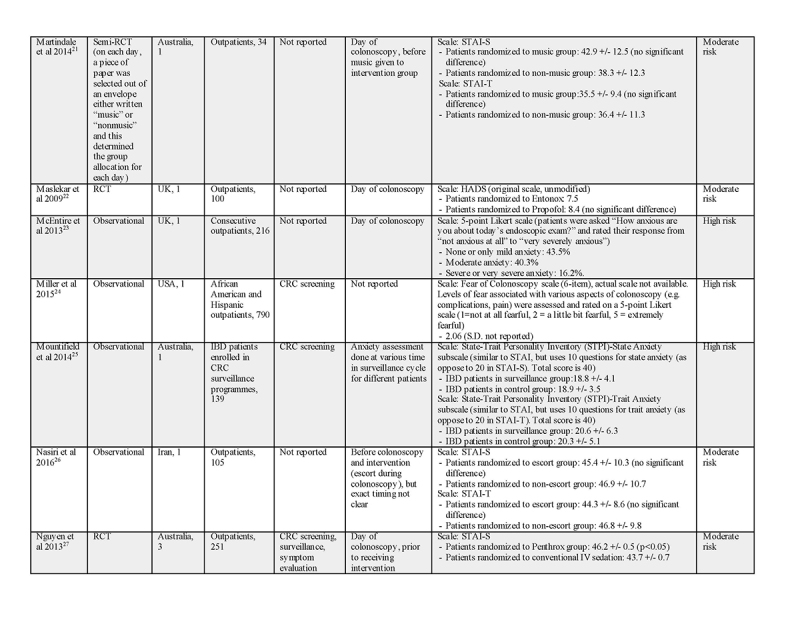
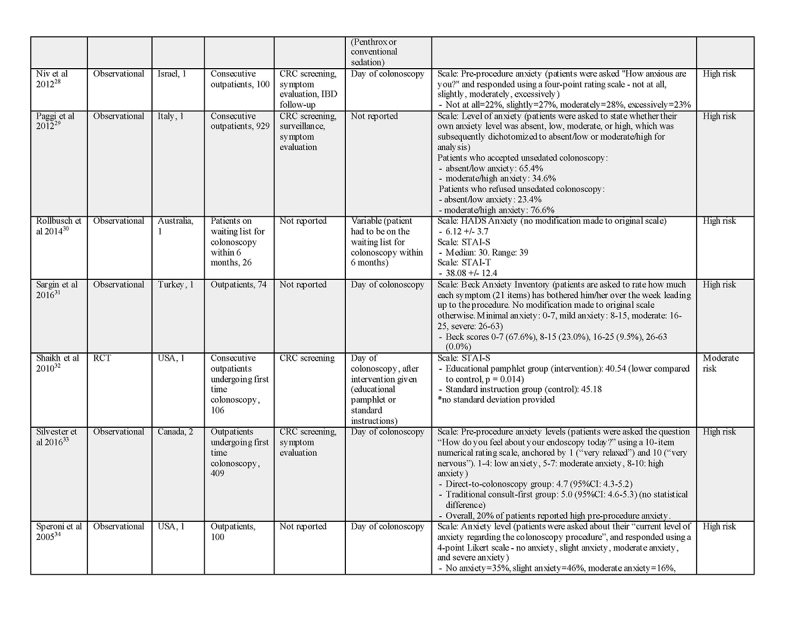
Study characteristics
The characteristics of the included studies are summarized in Supplementary Tables 1 to 4. The majority of the included studies were observational in nature; we did include 17 randomized trials and one case series. The study designs were heterogeneous, mainly with regard to the timing of anxiety assessment relative to the procedure and the type of anxiety measure used. CRC screening was the most common indication for colonoscopy or FS in tertiary care centers, but evaluation for symptoms and surveillance of polyps or inflammatory bowel disease were also common. Most studies did not limit the indication for endoscopy. Most studies assessed patients' anxiety on the day of the endoscopic procedure, while a few assessed their anxiety in weeks before the procedure.
The most common anxiety measure used was Spielberger State‐Trait Anxiety Inventory (STAI) [33]. The state version asks how the person is feeling “right now, at this moment.” The trait version asks people to describe “how I generally feel.” Other anxiety measures used include the Visual Analog Scale [34], the Beck Anxiety Inventory [35], and the Hospital Anxiety and Depression Scale‐Anxiety (HADS‐A) [36]. For the latter two measures, the instructions for the measure would have to be modified to assess situational anxiety as the standard instructions cover longer time periods—the last month for the Beck Anxiety Inventory and the last week for the HADS‐A scale. The wording of the rating scales used in the HADS‐A does not seem well suited to use for assessing situational anxiety. Many studies also used anxiety measures developed for the specific study. Some of these measures provide the advantage of giving a clear indication of the participant's opinion about their anxiety regarding colonoscopy/FS.
Quality of included studies
The risk of bias assessment per domain per study is provided in Supplementary Tables 6 to 10. The majority of the observational studies were of low‐to‐moderate quality. Only one randomized trial was considered to be at low risk of bias.
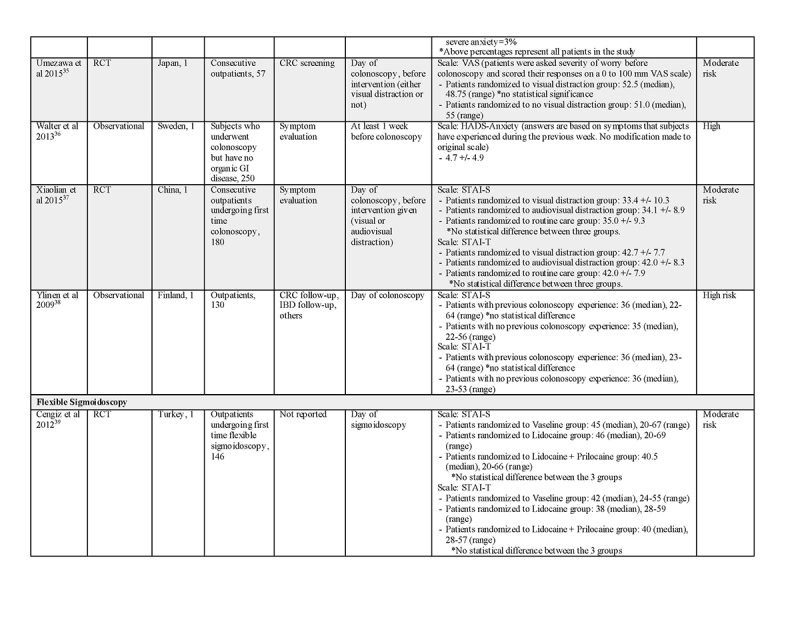
Magnitude of anxiety concerning colonoscopy
Anxiety was measured by diverse methods and therefore challenging to compare the levels across the studies. Fourteen studies used STAI‐state (STAI‐S) scale on the day of colonoscopy; they reported mean scores in the range between 33.4 and 50.0 out of a total score of 80 (Supplementary Table 1). The mean scores of STAI‐trait (STAI‐T) on the day of colonoscopy ranged from 35.5 to 46.9 out of 80. The two studies that collected data both before and on the day of colonoscopy found that patients' anxiety as measured by STAI‐S increased significantly on the day of colonoscopy compared with that measured earlier (36.2‐44.8, p = 0.001; 29.1‐32.5, p = 0.03) [37, 38].
Studies that used Visual Analog Scale usually reported median rather than mean, with median scores ranging from 31 to 52.5 (out of 100) [39, 40]. Most of the studies reported values in the 30‐40 range.
Two studies [41, 42] assessed anxiety using Beck Anxiety Inventory, and reported that 65‐68% of patients had minimal anxiety, 23‐26% had mild anxiety, 8‐10% had moderate anxiety, and 0‐2% had severe anxiety. As noted above, this scale may not lend itself well to assessing anxiety associated with a procedure because of the time frame covered by the instructions and the item rating scale.
A number of studies used rating scales developed by the authors. These measures generally have not been validated and instructions have not been standardized, but the simple wording on some of the scales may give us a helpful view of patients' opinions concerning their own anxiety. For example, the study by McEntire et al. [43] used a five‐point Likert scale. Among 216 respondents having a colonoscopy, 43.5% reported no or mild anxiety, 40.3% moderate anxiety, and 16.2% severe or very severe anxiety [43]. Another study with 100 patients [44] used a simple four‐point rating scale with the question: “How anxious are you?”. The responses were “not at all” (22%), “slightly” (27%), “moderately” (28%), and “excessively” (23%). A third study [45] also used a four‐point rating scale and found that 35% of patients reported no anxiety, 46% slight anxiety, 16% moderate anxiety, and 3% severe anxiety.
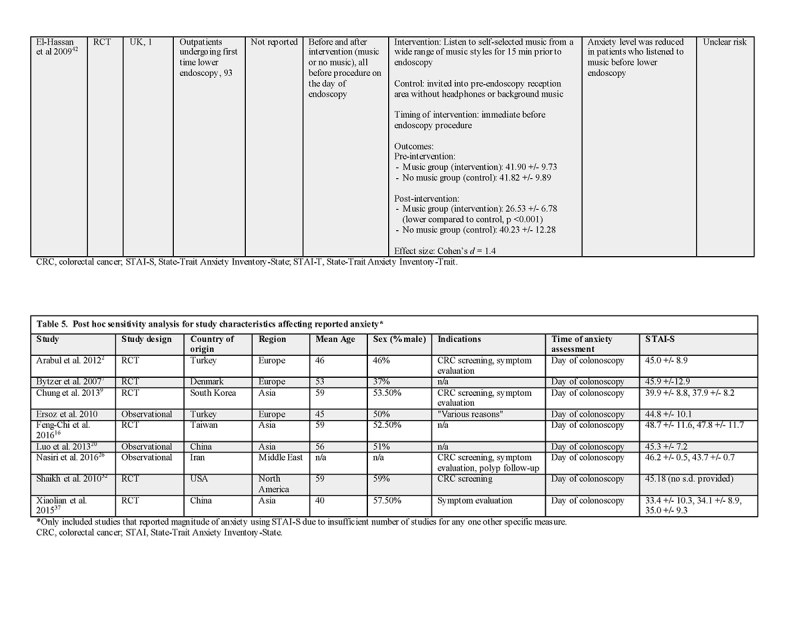
A post hoc sensitivity analysis was performed on studies that reported the magnitude of anxiety using mean STAI‐S (Supplementary Table 5). Studies that used other anxiety measures could not be compared due to a limited number of studies for any one other specific measure. Three studies were excluded for having a very small sample size. Two studies were excluded for reporting STAI‐S as median. In the remaining nine studies, no clear pattern emerged for the influence of age, sex, year of study, or study design on the magnitude of anxiety in patients undergoing colonoscopy. When these studies were examined based on country of origin or region (i.e., Europe and Asia), no clear pattern was identified either. With respect to indications of colonoscopy, many studies did not specify this information and the remaining studies nearly always performed colonoscopy for both CRC screening and symptom evaluation. All these studies assessed anxiety on the day of colonoscopy, so the effect of timing of assessment could not be evaluated.
Magnitude of anxiety concerning flexible sigmoidoscopy
Only three studies [46,47,48], using different measures, assessed anxiety in patients undergoing FS. Cengiz et al. [46] reported a similar STAI‐S score for FS as those reported for colonoscopy.
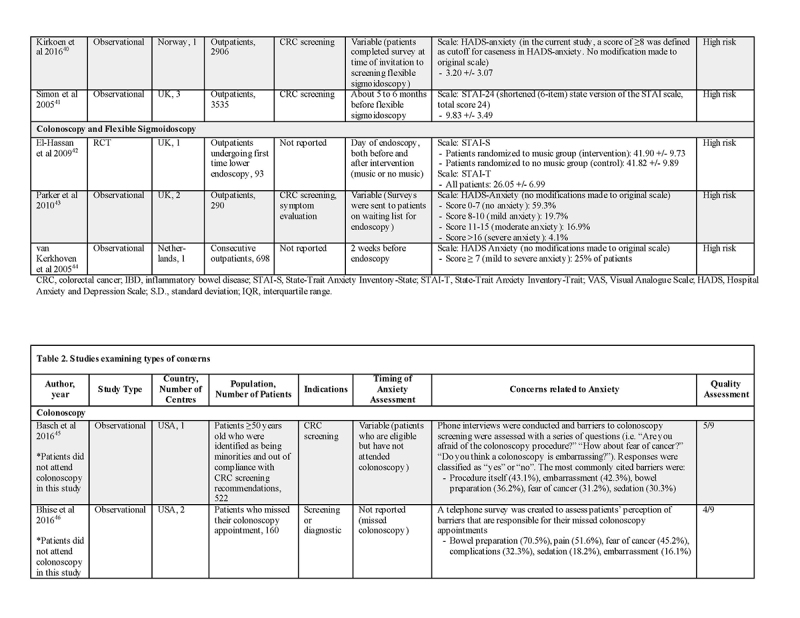
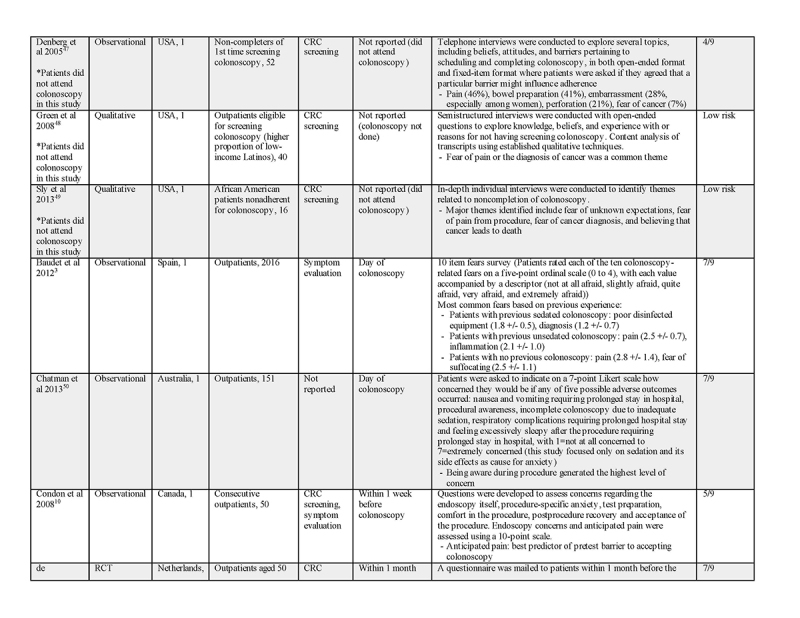
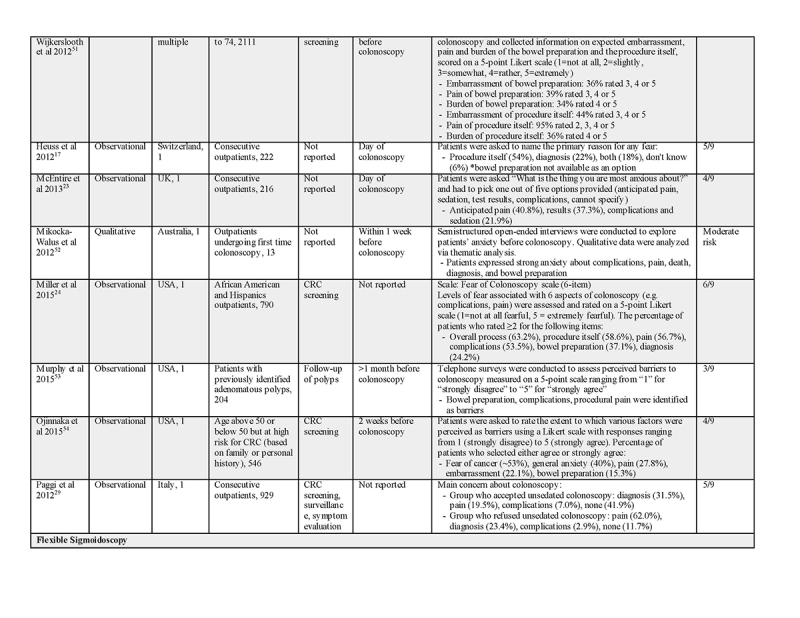
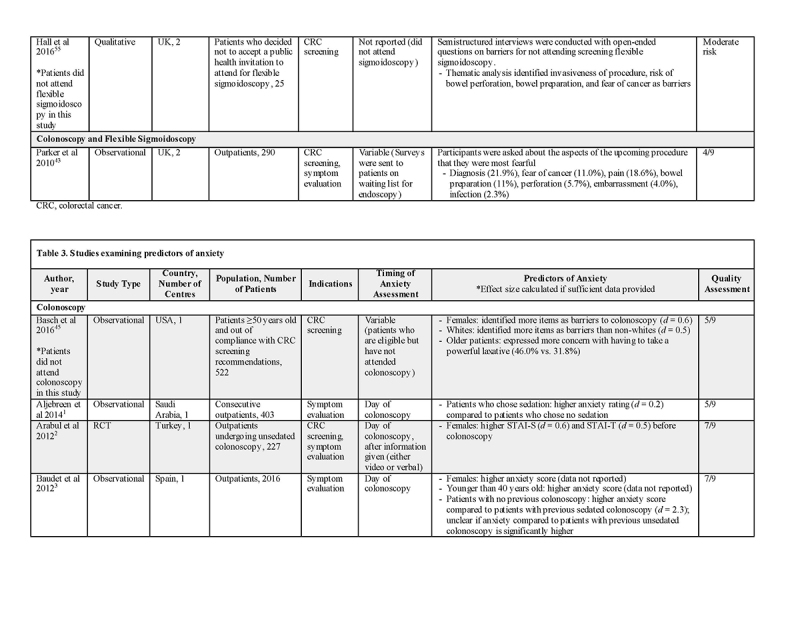
Areas of anxiety concerns
Some studies identified considered the concerns of patients undergoing colonoscopy. A smaller number of studies considered patients who had missed appointments for colonoscopy or those who had not followed up on invitations or recommendations for colonoscopy as a part of a cancer screening program [13,49,50,51,52]. The latter studies are especially interesting because they may provide helpful information concerning patients not taking advantage of recommendations for colonoscopy. The concerns revealed depend on the number of possible concerns addressed in the questions. Concerns related to colonoscopy or FS can be divided into those related to the bowel preparation process, the procedure itself, or diagnosis (Supplementary Table 2). Among studies evaluating patients who missed or did not attend colonoscopy, 36‐71% were anxious about the bowel preparation process; 46‐52% were anxious about anticipated pain from colonoscopy; 16‐42% were anxious about being embarrassed; 18.2‐30.3% of the patients had anxiety about undergoing sedation for colonoscopy; and 21‐32% were anxious about suffering complications. As many as 45% patients in one study had fears about the diagnosis of cancer [49].
Among studies evaluating patients undergoing colonoscopy, between 15 and 37% felt anxious about bowel preparation, when asked weeks to months before the colonoscopy. Both the embarrassment and pain of taking a powerful laxative have been reported as important contributors to anxiety. The colonoscopy procedure itself can generate anxiety in several ways. Around 53% of the patients were anxious about having complications from the colonoscopy procedure. Anticipated pain from colonoscopy was reported by 28‐95% of the patients. Baudet et al. [53] found that pain was a bigger concern among patients with no previous colonoscopy experience or patients who had no sedation with their previous procedure. Patients (22‐44%) also expected to be embarrassed during their colonoscopy, more so among women. Last, the fear of diagnosis, especially cancer, also generated a high level of anxiety, anywhere from 22 to 55% in some studies.
Only one study with a very small sample size assessed the concerns of patients undergoing FS, and simply reported factors such as invasiveness of the procedure, bowel preparation, and fear of cancer as contributors of anxiety [54].
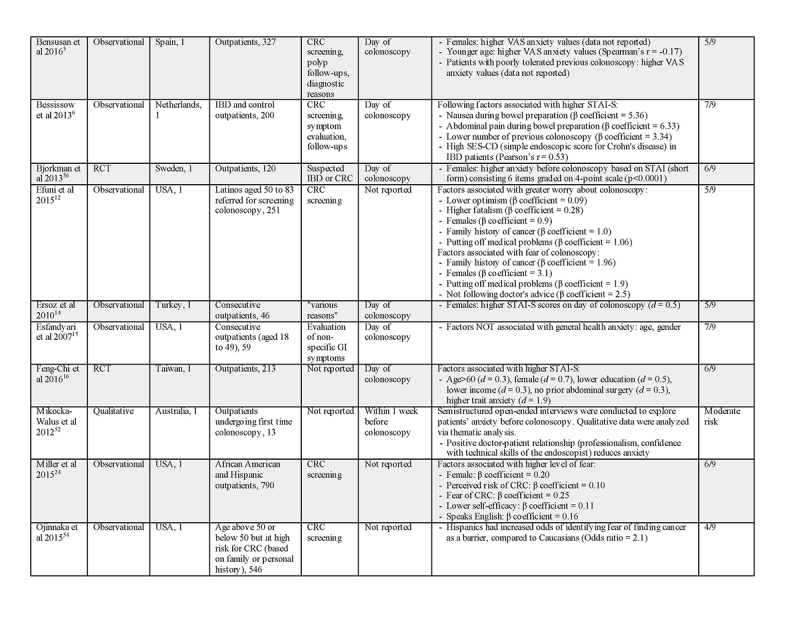
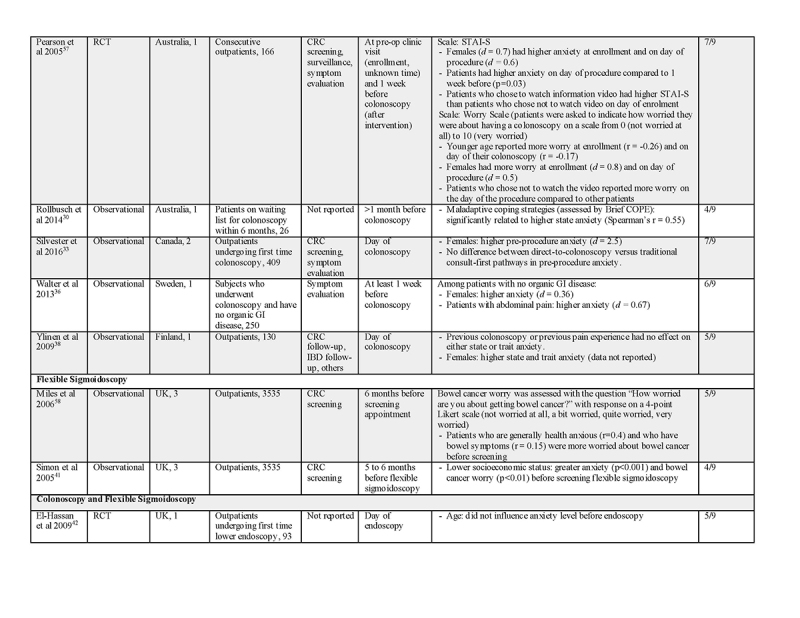
Predictors of anxiety
Several predictors have been identified that correlated with greater anxiety in patients undergoing colonoscopy (Supplementary Table 3): female gender (Cohen's d: 0.5‐2.5), functional abdominal pain (Cohen's d: 0.67), higher baseline anxiety as measured by STAI‐T (Cohen's d: 1.9), lower education (Cohen's d: 0.5), lower income (Cohen's d: 0.3), and no prior abdominal surgery (Cohen's d: 0.3). Other predictors include poorly tolerated previous colonoscopy, no previous colonoscopy, family history of cancer, poor doctor‐patient relationship, undergoing colonoscopy for symptoms (as opposed to for CRC screening), and use of maladaptive coping strategies.
It appeared that younger patients were more likely to experience anxiety before colonoscopy, although the results were not definitive. Three studies showed that younger patients experienced greater anxiety before colonoscopy [38, 39, 53]. Feng‐Chi et al. [55], on the other hand, found older patients to have greater anxiety. Efuni et al. [56] did not find age to be a factor in anxiety before colonoscopy.
The study by Silvester et al. [57] was the only one that compared open access versus prior consultation among patients undergoing colonoscopy and found no difference in anxiety.
Among patients undergoing FS, the factors associated with higher anxiety were being generally health anxious, the presence of bowel symptoms, and lower socioeconomic status [48, 58].
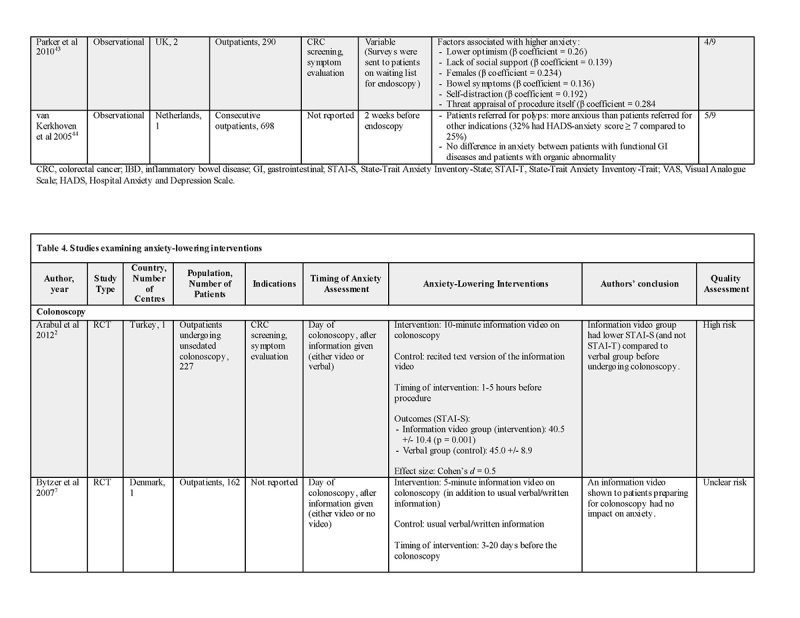
Anxiety‐lowering interventions
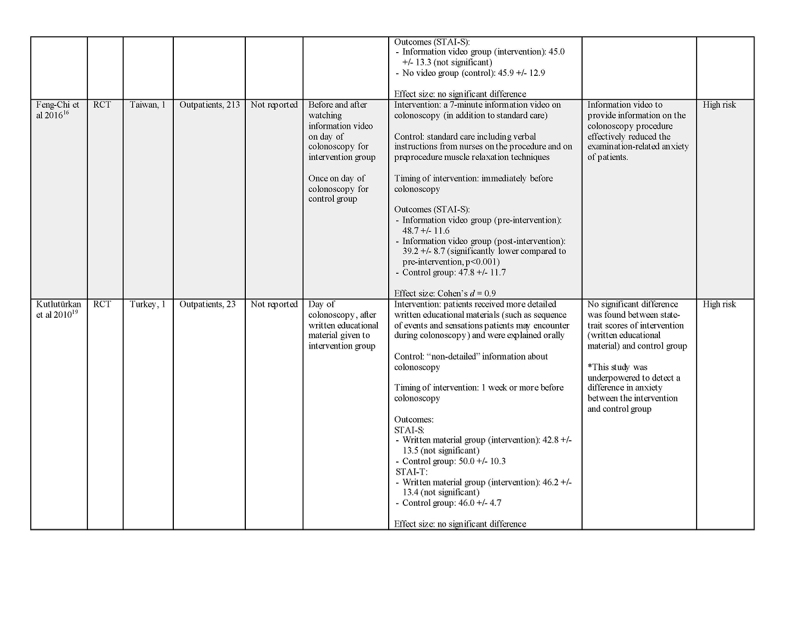
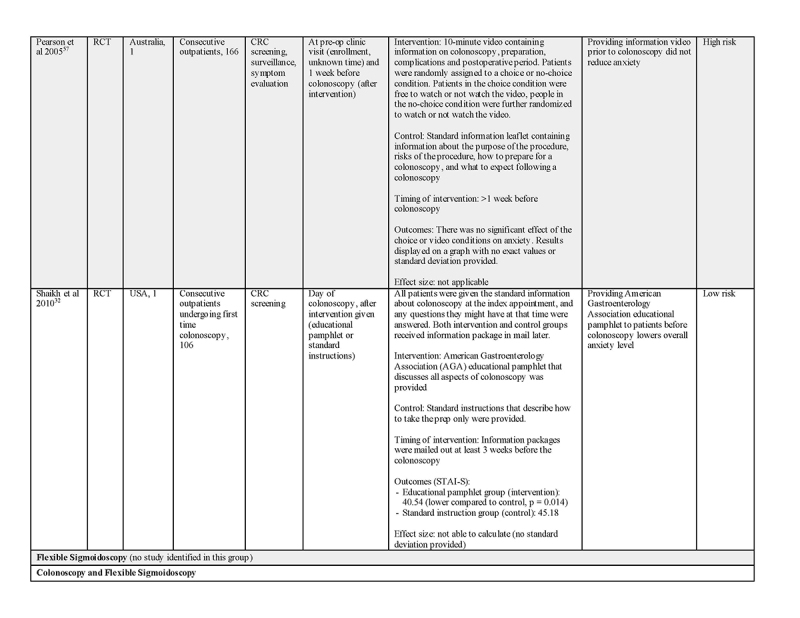
Three types of pre‐procedure interventions were evaluated by seven randomized trials for their effect on reducing anxiety in patients undergoing colonoscopy or FS (Supplementary Table 4). Four trials considered improved information with video content, two considered improved written educational materials, and one considered music immediately prior to colonoscopy. Most of the interventions focused on better informing patients about colonoscopy. None of them described any aspect of the intervention that was specifically intended to deal with anxiety concerns—although improving information may be a factor in lowering anxiety.
Some of the studies provided the intervention on the day of the colonoscopy, while others provided in advance of the colonoscopy at a pre‐procedure visit. All of the studies evaluated anxiety shortly before the procedure. In most of these studies, the intervention was compared to the standard process in place before the study was carried out. Often, a limited amount of information was provided about the content of the video material, but the focus was most often in informing patients about bowel preparation and the procedure.
Arabul et al. [59] and Feng‐Chi et al. [55] reported that showing an information video to patients on the day of their colonoscopy reduced their anxiety with an effect size (Cohen's d) of 0.5 and 0.9, respectively. In the Arabul study [59], patients received either the video (intervention) or the same information orally and with illustrations (according to a script) presented by a physician not performing the colonoscopy (control). In the Feng‐Chi study [55], patients in the control group received the information verbally from a nurse. In contrast, Bytzer et al. [60] and Pearson et al. [38] reported no benefit of an information video in improving patients' anxiety before colonoscopy; interestingly, the information video was shown to patients days to weeks before their colonoscopy procedure in both of these studies. For the Bytzer study [60], the video lasted for 5 min and focused on bowel preparation and technical aspects of the procedure, sedation, and possible results.
In a study by Shaikh et al. [61], providing an educational pamphlet to patients was found to reduce their anxiety before colonoscopy. The intervention was an American Gastroenterology Association educational pamphlet for patients; the control was a standard instruction sheet about bowel preparation [61]. Even so, Kutlutürkan et al. [62] found no difference between patients who received written educational materials and those who did not, although this had a much smaller sample size. Both groups received “nonspecific” information about the procedure orally from a nurse at a clinic visit a week or more before the procedure. The written information group received much more detailed information about the procedure which they read and was also explained orally.
We did not identify any studies that looked at anxiety‐lowering interventions for patients undergoing FS specifically. A randomized trial by El‐Hassan et al. [63] considered patients having either colonoscopy or FS, and found that listening to music of the person's choice for 15 min reduced anxiety with an effect size (Cohen's d) of 1.4.
DISCUSSION
Most of the included studies using the STAI‐S reported similar scores to a previous systematic review on preoperative surgical patients [64]. Thus, the process of undergoing colonoscopy seems to generate a similar degree of anxiety in patients as undergoing surgery. Our findings also suggest that the mean anxiety level among individuals having a colonoscopy is higher than that in the general population. Crawford et al. [65] reported a mean STAI‐S of 33.2 (standard deviation = 11.7) in a healthy adult population. Mean STAI‐S among older adult population has been reported to be in the range of 30‐33 [66]. Most studies in our review reported a higher mean STAI‐S score among patients undergoing colonoscopy. Some studies reported up to 51‐56% of patients having moderate‐to‐severe anxiety [43, 44].
Consedine et al. explained in their conceptual framework that health professionals need to identify the source of a patient's anxiety in order to provide effective interventions [24]. Concerns about pain and embarrassment during the procedure were common in the studies included in this review, as was concern about sedation and the possibility of complications. Addressing these concerns when making a recommendation of colonoscopy or FS may help improve its acceptance. As expected, the fear of being diagnosed with cancer is a major anxiety concern among many patients. Diagnosis of cancer and complications are rare and hence providing the actual numbers experiencing these events may alleviate some of the anxiety.
Our review identified several predictors associated with increased anxiety. Using these predictors will help clinicians identify those patients more at risk for developing significant anxiety. There are other factors not adequately explored by the studies included in this systematic review. For example, whether referral by an open‐access system versus consultation with an endoscopist play a role in patients' anxiety cannot be assessed because only one observational study reported this information. Anesthesia involvement to provide deep sedation may be another important contributor to pre‐procedural anxiety. Baudet et al. [53] found that patients who were sedated during their previous colonoscopy had lower anxiety and higher acceptance when undergoing a repeat colonoscopy.
In addition to being a barrier to acceptance, pre‐procedural anxiety also has other implications. For example, Feng‐Chi et al. [55] found that a key predictor of pain during colonoscopy was a patient's pre‐procedural anxiety level as measured by STAI‐S. This can affect sedation requirements, length of the colonoscopy procedure, and patient satisfaction.
Our review examined the effects of interventions aimed at lowering anxiety in patients having colonoscopy or FS. Among the interventions focused on improving patients' knowledge, if the previous process was well designed to inform the patient, it would be more difficult to show an improvement, while if the previous process was quite limited, it would be easier to show a change. This may explain some of the variable findings among the studies. It appears that showing patients an information video on the day of their colonoscopy procedures may reduce anxiety based on two randomized trials with high risk of bias [55, 59]. Unfortunately, this would have no effect on improving acceptance of colonoscopy, given that it was limited to those patients about to have the procedure. Providing a well‐designed information pamphlet to patients in the weeks prior to having a colonoscopy was found to reduce anxiety on the day of the procedure in one randomized trial with low risk of bias [67]. Some studies have found that patients have reduced anxiety when they receive information about the sensations they are likely to experience during endoscopy, as opposed to information about the technical aspects of the procedure alone [68, 69]. This was explored further in a study by Morgan et al. [70], where patients were divided based on their coping styles (“information seekers” and “information avoiders”), and it was found that patients who were given information congruent with their coping style experienced less anxiety before their colonoscopy. This suggests that patients vary in the type and amount of pre‐procedural information they prefer to receive.
Interventions designed to increase the quality and amount of information patients receive before the colonoscopy are promising. Information may be presented to patients in various formats including discussion with a health care provider, a written brochure, audio content, and video content. Previous research on communication with patients indicates that different patients prefer different types of information and there is not one type of information that is superior for all patients [71]. High‐quality information is information that is more easily understood by patients, information that may be discussed with family and friends, and information that describes the experiences of patients as they have a procedure. Better quality information is often available when patients participate in the production of the material. With a wide access to the Internet in recent years, the Internet may be a convenient way to get high‐quality information to people, at low cost, well in advance of the colonoscopy appointment. Concerns about embarrassment, pain, and possible sedation could be addressed by information or recorded video testimonials from other patients who have experienced colonoscopy.
Anxiety concerning colonoscopy or FS is one of the barriers for some patients considering CRC screening [13, 72, 73]. While demographic factors are also important determinants of the uptake of screening, anxiety related to the procedure or the diagnosis of cancer is more amenable to change by targeted interventions. However, the effect of anxiety on screening adherence is complex as it may act as either a barrier or facilitator. As suggested by Consedine et al., the source of anxiety is an important factor in screening behavior; patients with more specific anxiety toward the medical establishment, pain, or embarrassment of the procedure seek to alleviate their anxiety by avoiding screening, whereas patients with more generalized anxiety about “getting cancer” tend to reduce anxiety by undergoing screening [24]. In addition, the degree of anxiety may also play a role. Too little anxiety may lead to apathy and too much anxiety promotes avoidance; a “moderate” level of anxiety may provide the most impetus for screening adherence [24]. Last, ethnicity may be a modifier concerning the relationship between anxiety and screening adherence [74]. For example, breast cancer literature supports the notion that African‐American women are more likely to avoid screening mammography because of fear of cancer diagnosis compared to Whites [75]. All these factors can influence how a patient's procedure or cancer‐related anxiety affects their screening adherence. Knowledge of these factors helps guide the development of effective interventions in the appropriate patient population.
Our review highlights several limitations to the available literature on anxiety for colonoscopy. The studies included in the analysis were very heterogeneous, precluding the data from being quantitatively pooled. This makes it difficult to conclude the overall magnitude of anxiety in patients undergoing colonoscopy. Future systematic reviews may consider conducting a meta‐analysis as more data from homogeneous study designs become available. Our post hoc sensitivity analysis did not identify any subgroup effects between the nine studies that reported STAI‐S but was limited by the small number of studies. In addition, the majority of studies in our review were of moderate‐to‐low quality based on our methodological assessment. The quality of evidence for anxiety‐lowering interventions is poor, given the limited number of randomized trials in this area and the high risk of bias in most of them. For all types of outcomes, studies on FS were very limited and few conclusions could be made specific for FS. Most studies in our review assessed anxiety on the day of the endoscopic procedure; this did not capture any patients who could have canceled their appointments due to severe anxiety.
Our review did not examine several other barriers to the uptake of screening colonoscopy or FS, such as perceived utility of these procedures, lack of time, arranging transportation, and inadequate knowledge about cancer.
CONCLUSION
Our systematic review found that the mean anxiety level among patients undergoing colonoscopy was higher than that reported for the general population. In addition, anxiety level was increased on the day of the colonoscopy compared to earlier. A high proportion of the patients experience anxiety due to concerns related to different aspects of having a colonoscopy. Certain patient characteristics, such as female sex, higher baseline anxiety, functional abdominal pain, low education, and low‐income level can help identify those more likely to experience anxiety and may benefit from targeted interventions. Providing an information video may alleviate anxiety in some patients having a colonoscopy, but additional high‐quality studies are needed to confirm this effect. We anticipate that the findings of this study will be useful in improving the information provided to patients considering colonoscopy and FS.
CONFLICT OF INTEREST
Guarantor of the article: Harminder Singh, MD, MPH.
Specific author contributions: Study concept and design (C.Y., A.M.A.S., W.P., J.W., and H.S.); analysis and interpretation of the data (all authors); drafting of the paper (C.Y. and H.S.); critical revision of the paper for important intellectual content; and final approval (all authors). All authors had access to the study data and reviewed and approved the final paper.
Financial support: This study was funded in part by the Health Sciences Center Medical Staff Fellowship Fund Research Award and Research Manitoba. These entities did not have any role in study design, collection, analysis, or interpretation of the data.
Potential competing interests: H.S. has served on the advisory board for Pendopharm and Ferring Canada and received funding for an investigator‐initiated study from Merck Canada. These entities did not have any role in study design, collection, analysis, or interpretation of the data. None of the authors disclose any conflict that could affect the design or analysis of this systematic review.
Study Highlights
WHAT IS CURRENT KNOWLEDGE
✓ There are no systematic reviews synthesizing information on pre‐procedure anxiety concerning colonoscopy or flexible sigmoidoscopy.
WHAT IS NEW HERE
✓ Several reports indicate that the majority of patients are anxious about having a colonoscopy, with overall a similar degree of anxiety as those undergoing general surgery.
✓ Providing improved pre‐procedure information, such as that in the form of a video, may help reduce anxiety.
✓ Higher‐quality studies are needed to assess the magnitude of benefit of anxiety reducing interventions in different practice settings.
✓ This systematic review summarizes several concerns and several predictors associated with increased pre‐colonoscopy anxiety, which should be considered for targeted interventions.
✓ Knowledge of identified common concerns about colonoscopy can assist in the development of educational materials realistically addressing those concerns—such as specific information on numbers of patients experiencing adverse effects and being diagnosed with cancer.
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at https://doi.org/10.1038/s41395‐018‐0398‐8
Correspondence: H.S. (email: Harminder.singh@umanitoba.ca)
Published online 1 November 2018
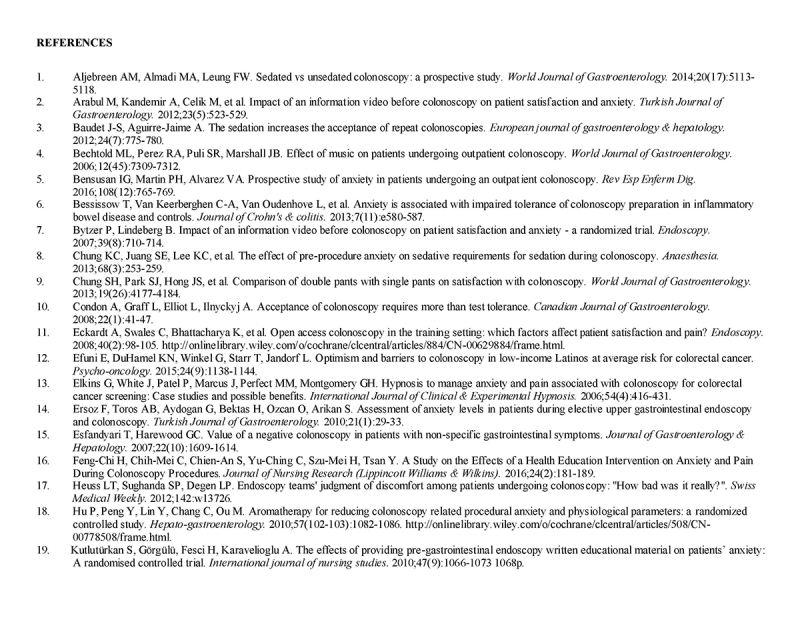
REFERENCES
- 1.Canadian Cancer Society's Advisory Committee on Cancer Statistics. Canadian Cancer Statistics. 2016. [Google Scholar]
- 2.Jemal A, Ward EM, Johnson CJ, et al. Annual report to the nation on the status of cancer, 1975-2014, Featuring Survival. J Natl Cancer Inst. 2017;109:djx030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center MM, Jemal A, Smith RA, Ward E. Worldwide variations in colorectal cancer. CA Cancer J Clin. 2009;59:366–78. [DOI] [PubMed] [Google Scholar]
- 4.Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67:177–93. [DOI] [PubMed] [Google Scholar]
- 5.Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosetti C, Levi F, Rosato V, et al. Recent trends in colorectal cancer mortality in Europe. Int J Cancer. 2011;129:180–91. [DOI] [PubMed] [Google Scholar]
- 7.Bosetti C, Bertuccio P, Malvezzi M, et al. Cancer mortality in Europe, 2005-2009, and an overview of trends since 1980. Ann Oncol. 2013;24:2657–71. [DOI] [PubMed] [Google Scholar]
- 8.Hewitson P, Glasziou P, Watson E, Towler B, Irwig L. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult): an update. Am J Gastroenterol. 2008;103:1541–9. [DOI] [PubMed] [Google Scholar]
- 9.Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends-an update. Cancer Epidemiol Biomark Prev. 2016;25:16–27. [DOI] [PubMed] [Google Scholar]
- 10.Singh H, Bernstein CN, Samadder JN, Ahmed R. Screening rates for colorectal cancer in Canada: a cross-sectional study. CMAJ Open. 2015;3:E149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pignone MP, Lewis CL. Using quality improvement techniques to increase colon cancer screening. Am J Med. 2009;122:419–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holden DJ, Jonas DE, Porterfield DS, Reuland D, Harris R. Systematic review: enhancing the use and quality of colorectal cancer screening. Ann Intern Med. 2010;152:668–76. [DOI] [PubMed] [Google Scholar]
- 13.Green AR, Peters-Lewis A, Percac-Lima S, et al. Barriers to screening colonoscopy for low-income Latino and white patients in an urban community health center. J Gen Intern Med. 2008;23:834–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greiner KA, Born W, Nollen N, Ahluwalia JS. Knowledge and perceptions of colorectal cancer screening among urban African Americans. J Gen Intern Med. 2005;20:977–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh JM, Kaplan CP, Nguyen B, Gildengorin G, McPhee SJ, Perez-Stable EJ. Barriers to colorectal cancer screening in Latino and Vietnamese Americans. Compared with non-Latino white Americans. J Gen Intern Med. 2004;19:156–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shokar NK, Vernon SW, Weller SC. Cancer and colorectal cancer: knowledge, beliefs, and screening preferences of a diverse patient population. Fam Med. 2005;37:341–7. [PubMed] [Google Scholar]
- 17.Khankari K, Eder M, Osborn CY, et al. Improving colorectal cancer screening among the medically underserved: a pilot study within a federally qualified health center. J Gen Intern Med. 2007;22:1410–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jandorf L, Ellison J, Villagra C, et al. Understanding the barriers and facilitators of colorectal cancer screening among low income immigrant hispanics. J Immigr & Minor Health. 2010;12:462–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janz NK, Wren PA, Schottenfeld D, Guire KE. Colorectal cancer screening attitudes and behavior: a population-based study. Prev Med. 2003;37 (6 Pt 1):627–34. [DOI] [PubMed] [Google Scholar]
- 20.Feeley TH, Cooper J, Foels T, Mahoney MC. Efficacy expectations for colorectal cancer screening in primary care: identifying barriers and facilitators for patients and clinicians. Health Commun. 2009;24:304–15. [DOI] [PubMed] [Google Scholar]
- 21.Berkowitz Z, Hawkins NA, Peipins LA, White MC, Nadel MR. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008;56:307–14. [DOI] [PubMed] [Google Scholar]
- 22.Geiger TM, Miedema BW, Geana MV, Thaler K, Rangnekar NJ, Cameron GT. Improving rates for screening colonoscopy: analysis of the health information national trends survey (HINTS I) data. Surg Endosc. 2008;22:527–33. [DOI] [PubMed] [Google Scholar]
- 23.Furer P, Walker J, Stein M. Treating Health Anxiety and Fear of Death: A Practitioner's Guide. New York: Springer; 2006. [Google Scholar]
- 24.Consedine NS, Magai C, Krivoshekova YS, Ryzewicz L, Neugut AI. Fear, anxiety, worry, and breast cancer screening behavior: a critical review. Cancer Epidemiol Biomark Prev. 2004;13:501–10. [PubMed] [Google Scholar]
- 25.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. [DOI] [PubMed] [Google Scholar]
- 26.Higgins JPT, Lasserson T, Chandler J, Tovey D, Churchill R. Standards for the conduct of new Cochrane Intervention Reviews. In: Higgins JPT, Lasserson T, Chandler J, Tovey D, Churchill R. Methodological Expectations of Cochrane Intervention Reviews. Cochrane: London, 2016. [Google Scholar]
- 27.Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9. [DOI] [PubMed] [Google Scholar]
- 28.Wells G, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Canada: Department of Epidemiology and Community Medicine. [Google Scholar]
- 29.CASP (Qualitative) Checklist. 2018. https://casp-uk.net/casp-tools-checklists.
- 30.Higgins JP, Altman DG, Gotzsche PC, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Magnusson K. Interpreting Cohen's d effect size. http://rpsychologist.com/d3/cohend/. Accessed May 23, 2018.
- 33.Spielberger C, Gorsuch R, Lushene P, Vagg P, Jacobs A. Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto: Consulting Psychologists Press, Inc; 1983. [Google Scholar]
- 34.Rossi V, Pourtois G. Transient state-dependent fluctuations in anxiety measured using STAI, POMS, PANAS or VAS: a comparative review. Anxiety Stress Coping. 2012;25:603–45. [DOI] [PubMed] [Google Scholar]
- 35.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–7. [DOI] [PubMed] [Google Scholar]
- 36.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52:69–77. [DOI] [PubMed] [Google Scholar]
- 37.Ersoz F, Toros AB, Aydogan G, Bektas H, Ozcan O, Arikan S. Assessment of anxiety levels in patients during elective upper gastrointestinal endoscopy and colonoscopy. Turk J Gastroenterol. 2010;21:29–33. [DOI] [PubMed] [Google Scholar]
- 38.Pearson S, Maddern G, Hewett P. Interacting effects of preoperative information and patient choice in adaptation to colonoscopy. Dis Colon Rectum. 2005;48:2047–54. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/200/CN-00531200/frame.html [DOI] [PubMed] [Google Scholar]
- 39.Bensusan IG, Martin PH, Alvarez VA. Prospective study of anxiety in patients undergoing an outpatient colonoscopy. Rev Esp Enferm Dig. 2016;108:765–9. [DOI] [PubMed] [Google Scholar]
- 40.Umezawa S, Higurashi T, Uchiyama S, et al. Visual distraction alone for the improvement of colonoscopy-related pain and satisfaction. World J Gastroenterol. 2015;21:4707–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chung KC, Juang SE, Lee KC, et al. The effect of pre-procedure anxiety on sedative requirements for sedation during colonoscopy. Anaesthesia. 2013;68:253–9. [DOI] [PubMed] [Google Scholar]
- 42.Sargin M, Uluer MS, Aydogan E, et al. Anxiety levels in patients undergoing sedation for elective upper gastrointestinal endoscopy and colonoscopy. Med Arch. 2016;70:112–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McEntire J, Sahota J, Hydes T, Trebble TM. An evaluation of patient attitudes to colonoscopy and the importance of endoscopist interaction and the endoscopy environment to satisfaction and value. Scand J Gastroenterol. 2013;48:366–73. [DOI] [PubMed] [Google Scholar]
- 44.Niv Y, Bogolavski I, Ilani S, et al. Impact of colonoscopy on quality of life. Eur J Gastroenterol Hepatol. 2012;24:781–6. [DOI] [PubMed] [Google Scholar]
- 45.Speroni KG, Hannah J, Atherton M, Corriher J. Evaluation of demographic, behavioral, and procedural factors on pain perception by patients undergoing colonoscopy and moderate sedation. Gastroenterol Nurs. 2005;28:502-508507. [DOI] [PubMed] [Google Scholar]
- 46.Cengiz C, Pampal H, Ozdemir B, Boyacioglu S, Kuzu M. No effect of perianal application of topical anaesthetic on patient comfort during nonsedated flexible sigmoidoscopy: a randomized, placebo-controlled clinical trial. Colorectal Dis: Off J Assoc Coloproctology Gt Br Irel. 2012;14:872–5. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/266/CN-00839266/frame.html [DOI] [PubMed] [Google Scholar]
- 47.Kirkoen B, Berstad P, Botteri E, et al. Do no harm: no psychological harm from colorectal cancer screening. Br J Cancer. 2016;114:497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Simon AE, Steptoe A, Wardle J. Socioeconomic status differences in coping with a stressful medical procedure. Psychosom Med. 2005;67:270–6. [DOI] [PubMed] [Google Scholar]
- 49.Bhise V, Modi V, Kalavar A, et al. Patient-reported attributions for missed colonoscopy appointments in two large healthcare systems. Dig Dis Sci. 2016;61:1853–61. [DOI] [PubMed] [Google Scholar]
- 50.Denberg TD, Melhado TV, Coombes JM, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20:989–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sly JR, Edwards T, Shelton RC, Jandorf L. Identifying barriers to colonoscopy screening for nonadherent African American participants in a patient navigation intervention. Health Educ & Behav. 2013;40:449–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Basch CH, Basch CE, Zybert P, Wolf RL. Fear as a barrier to asymptomatic colonoscopy screening in an urban minority population with health insurance. J Community Health. 2016;41:818–24. [DOI] [PubMed] [Google Scholar]
- 53.Baudet J-S, Aguirre-Jaime A. The sedation increases the acceptance of repeat colonoscopies. Eur J Gastroenterol Hepatol. 2012;24:775–80. [DOI] [PubMed] [Google Scholar]
- 54.Hall N, Birt L, Rees CJ, et al. Concerns, perceived need and competing priorities: a qualitative exploration of decision-making and non-participation in a population-based flexible sigmoidoscopy screening programme to prevent colorectal cancer. BMJ Open. 2016;6:e012304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Feng-Chi H, Chih-Mei C, Chien-An S, Yu-Ching C, Szu-Mei H, Tsan Y. A study on the effects of a health education intervention on anxiety and pain during colonoscopy procedures. J Nurs Res (Lippincott Williams & Wilkins). 2016;24:181–9. [DOI] [PubMed] [Google Scholar]
- 56.Efuni E, DuHamel KN, Winkel G, Starr T, Jandorf L. Optimism and barriers to colonoscopy in low-income Latinos at average risk for colorectal cancer. Psychooncology. 2015;24:1138–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silvester JA, Kalkat H, Graff LA, Walker JR, Singh H, Duerksen DR. Information seeking and anxiety among colonoscopy-naive adults: Direct-to-colonoscopy vs traditional consult-first pathways. World J Gastrointest Endosc. 2016;8:701–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Miles A, Wardle J. Adverse psychological outcomes in colorectal cancer screening: does health anxiety play a role? Behav Res Ther. 2006;44:1117–27. [DOI] [PubMed] [Google Scholar]
- 59.Arabul M, Kandemir A, Celik M, et al. Impact of an information video before colonoscopy on patient satisfaction and anxiety. Turk J Gastroenterol. 2012;23:523–9. [DOI] [PubMed] [Google Scholar]
- 60.Bytzer P, Lindeberg B. Impact of an information video before colonoscopy on patient satisfaction and anxiety - a randomized trial. Endoscopy. 2007;39:710–4. [DOI] [PubMed] [Google Scholar]
- 61.Shaikh A, Hussain S, Rahn S, Desilets D. Effect of an educational pamphlet on colon cancer screening: a randomized, prospective trial. Eur J Gastroenterol Hepatol. 2010;22:444–9. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/040/CN-00749040/frame.html. [DOI] [PubMed] [Google Scholar]
- 62.Görgülü, Kutlutürkan S, Fesci H, Karavelioglu A. The effects of providing pre-gastrointestinal endoscopy written educational material on patients' anxiety: A randomised controlled trial. Int J Nurs Stud. 2010;47:1066-10731068. [DOI] [PubMed] [Google Scholar]
- 63.El-Hassan H, McKeown K, Muller A. Clinical trial: music reduces anxiety levels in patients attending for endoscopy. Aliment Pharmacol Ther. 2009;30:718–24. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/592/CN-00732592/frame.html. [DOI] [PubMed] [Google Scholar]
- 64.Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database of Systematic Reviews 2013, Issue 6. Art. No.: CD006908. 10.1002/14651858.CD006908.pub2. [DOI] [PMC free article] [PubMed]
- 65.Crawford J, Cayley C, Lovibond PF, Wilson PH, Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Aust Psychol. 2011;46:3–14. [Google Scholar]
- 66.Knight RG, Waal-Manning HJ, Spears GF. Some norms and reliability data for the state-trait anxiety inventory and the zung self-rating depression scale. Br J Clin Psychol. 1983;22(Pt 4):245–9. [DOI] [PubMed] [Google Scholar]
- 67.Shaikh AA, Hussain SM, Rahn S, Desilets DJ. Effect of an educational pamphlet on colon cancer screening: a randomized, prospective trial. Eur J Gastroenterol Hepatol. 2010;22:444–9. [DOI] [PubMed] [Google Scholar]
- 68.Shipley RH, Butt JH, Farbry JE, Horwitz B. Psychological preparation for endoscopy. Physiological and behavioral changes in patients with differing coping styles for stress. Gastrointest Endosc. 1977;24:9–13. [DOI] [PubMed] [Google Scholar]
- 69.Johnson JE, Morrisey JF, Levanthal H. Psychological preparation for an endoscopic examination. Gastrointest Endosc. 1973;19:180–2. [DOI] [PubMed] [Google Scholar]
- 70.Morgan J, Roufeil L, Kaushik S, Bassett M. Influence of coping style and precolonoscopy information on pain and anxiety of colonoscopy. Gastrointest Endosc. 1998;48:119–27. [DOI] [PubMed] [Google Scholar]
- 71.Cunningham CE, Walker JR, Eastwood JD, et al. Modeling mental health information preferences during the early adult years: a discrete choice conjoint experiment. J Health Commun. 2014;. 19:413–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cai S-R, Zhang S-Z, Zhu H-H, Zheng S. Barriers to colorectal cancer screening: a case-control study. World J Gastroenterol. 2009;15:2531–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Good K, Niziolek J, Yoshida C, Rowlands A. Insights into barriers that prevent African Americans from seeking colorectal screenings: a qualitative study. Gastroenterol Nurs. 2010;33:204–8. [DOI] [PubMed] [Google Scholar]
- 74.Bromley EG, May FP, Federer L, Spiegel BMR, van Oijen MGH. Explaining persistent under-use of colonoscopic cancer screening in African Americans: a systematic review. Prev Med. 2015;71:40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Peek ME, Sayad JV, Markwardt R. Fear, fatalism and breast cancer screening in low-income African-American women: the role of clinicians and the health care system. J Gen Intern Med. 2008;23: 1847–53. [DOI] [PMC free article] [PubMed] [Google Scholar]