Abstract
Federal food and nutrition programs implemented by the Administration on Aging and funded by the Older Americans Act (OAA) seek to enable older adults to remain in their homes and communities through a comprehensive, coordinated, and cost-effective array of services. We hypothesized that expenditures devoted to nutrition programs for home and community-based nutrition services were inversely related to changes in state-level rates of institutionalization for older adults from one year to the next, such that states that spend more money per capita on community-based nutrition programs would have smaller increases or greater decreases in rates of institutionalization, controlling f1or expenditures on other home and community based services (HCBS). We found, however, that there was not an effect of OAA Nutrition Services on the change in rates of nursing home residency. We noted, though, that states which direct a greater proportion of their long-term care expenditures to home and community based services appear to have more reduction in their rates of nursing home residency. Further longitudinal work at the state and individual levels is warranted.
Keywords: Public Policy, Older Americans Act, Aging in Place, Community-based Nutrition
INTRODUCTION
An increasing number of long-term care policies and programs in the United States are being targeted at supporting the ability and desire of older adults with functional impairments to maintain independence in the community. These services may be medical or social in nature and are aimed at persons with disabilities or chronic care needs. Among those long-term care services that have been frequently considered to be both popular and successful are home and community based services (HCBS) offered under a range of programs including Medicare and Medicaid. Additionally, the Aging Services Network created under the Older Americans Act (OAA) of 1965 offers HCBS. (1–3) Among the services authorized by this program are personal care, adult day care, nutrition, and transportation services that are provided in non-institutional settings and intended to help both healthy and functionally impaired older persons to remain living in the community. (4) Availability of these long-term care services vary according to the financial commitment of the states and area agencies on aging, and this research is one attempt to assess how that variation in services impacts outcomes, particularly related to aging in place vs. nursing home admission.
The Administration on Aging and the Older Americans Act
The OAA established the Administration on Aging (AoA) as a subdivision of the Department of Health and Human Service and as part of the larger National Aging Network including federal, state, tribal, and local partnerships. The explicit mission of the AoA is “to develop a comprehensive, coordinated and cost-effective system of long-term care that helps (older) individuals to maintain their dignity in their homes and communities.”(5) The OAA and the services it provides were established during the 1960’s and 1970’s when it was widely accepted that the responsibility of the federal government was to address social problems. (6) During times of scarce economic resources, however, it is useful to consider whether programs are effective in meeting their goals. While all of the services provided through the OAA as well as other agencies are important, we aim to assess the impact of the nutrition services program because the role of adequate and appropriate food intake is crucial for older adults’ overall independence and health while accounting for those other home and community-based services.
This paper examines two questions. First, are state-level expenditures on nutrition-related HCBS associated with rates of change in nursing home residency of older adults. Second, are expenditures on nutrition-related HCBS, when other HCBS services are accounted for, associated with rates of change in nursing home residency among older adults. The theme of these questions is centered on the effectiveness of OAA programs in meeting their goals—namely, do they help older adults remain in their homes in the community.
Nutrition Services of the Older Americans Act.
Nutrition programs that are supported by Title IIIC of the OAA include congregate and home-delivered meals. Congregate meal (CM) services are offered in group settings such as community centers, churches, and adult day centers; while home delivered meal (HDM) services, commonly called Meals-on-Wheels, are delivered to homebound older adults. Additionally, and to a much lesser extent, the Title III services include nutrition screening, assessment, education, and counseling as well as general health promotion and referrals to other services. The nutrition services programs are administered by states who must meet federal nutrition standards. Generally, programs provide meals five days per week, usually one meal per day, to recipients. Each meal is to provide one-third of the Dietary Reference Intakes (DRI) and meet the current requirements of the Dietary Guidelines for Americans, provide meals appealing to older adults, and meet state and local food service laws. The explicit purpose of these nutrition services is to: “reduce hunger and food insecurity, promote socialization of older individuals, and promote the health and well-being of older individuals and delay adverse health conditions through access to nutrition and other disease prevention and health promotion services.” (7) Services are available to individuals ≥60 years and to a limited number of people <60 years old with disabilities who are living with an older adult. The programs target those with low incomes, minorities, residents of rural areas, those with limited ability to speak English, and those at greatest risk for institutionalization.
Funding for Title IIIC Nutrition services comes primarily from the AoA by funds that are appropriated by the United States Congress and then allocated to states and territories based on the proportion of the population ≥60 years. Additionally, funding for congregate and home delivered meal services may be supplemented by “other federal funds, state and local funds, participant contributions, and private funding.” (8) The sources of additional funds vary by state.
It is estimated that OAA nutrition programs reach only 6–7% of older adults who need these services. (9) AoA data show participation in congregate meal services was down from 1.67 million people being served 94.8 million meals in 2007 to 1.66 million persons being served 94.2 million meals in 2008. The expenditures for the congregate meals program in 2008 were over $636 million, for an average of $384.12 per person and $6.75 per meal. The home delivered meals program reached nearly one million people with 146.9 million meals in 2008. The expenditures for this program were over $750 million, at an average of $830.02 per person, and $5.14 per meal. (10) Overall, total appropriations for the OAA Nutrition Program has declined significantly in the past two decades from $942 million in FY1990 to $820 million in FY2010; correspondingly total meals declined by almost 4 million. (11)
Evaluation of Home and Community Based Services
The reauthorization of the OAA in 2006 required that the Institute of Medicine conduct an evidence-based evaluation of the program, but Congress failed to authorize the funds necessary to carry out the evaluation, therefore it has not been done. (2, 11) The goal of the evaluation that was mandated in 2006 was “to document overall program results, find ways for program improvement, aid the program planning process, show the programs’ contributions to elder independence, and assess best practices including those programs demonstrating the most effective cost-benefit outcomes and impacts.” (12) While previous research findings have pointed to the efficacy of OAA’s programs on individual-level health outcomes, (13) current and expanded evaluation is warranted to specifically examine the role of nutrition services in the context of the larger HCBS programs. The AoA began conducting assessment of their nutrition programs annually, starting in 2005, using limited funds that they had that were earmarked for program evaluation. The focus of the evaluation was on program efficiency and effectiveness and client outcomes, assessed in consumer satisfaction surveys. The results suggested that clients participating in either congregate or home delivered meal programs believed that the programs enabled them to eat balanced meals and to continue living in their homes. (7) Caregivers also reported that these services helped them to continue caring for the older adults in their homes. A recent research brief prepared by Mathematica Policy Research, Inc. (14) found that Title III Nutrition Programs seemed to be reaching those older adults who were targeted for participation, namely those who were older, living in poverty, not married, and those with higher levels of disability and comorbidity.
Work done by Kaye, LaPlante and Harrington (15) shows that growth in HCBS programs may come with significant increased initial cost, but that they are associated with cost savings over the future. They demonstrate that states which invest in HCBS programs, at a minimum, are not put at a financial disadvantage for doing so, effectively saying that the “worst” case scenario is that states break-even on costs.
Whether provision of specific AoA nutritional services and other HCBS programs enable older adults to remain in their communities in a cost-effective manner has not been adequately studied and is the focus of our work. One way of measuring if older adults are remaining in their communities is to assess if states are incurring an increase or decrease in nursing home admission. Answers to questions such as this are increasingly important as the federal budget is constantly under scrutiny. In fact, the issue of delivering nutrition services in the community is regarded as such an important issue that the Institute of Medicine held a workshop in October 2011 entitled Nutrition and Healthy Aging in the Community. The question is further compelling because of the rising costs associated with providing high quality long-term care to a growing aging population combined with state budgetary constraints; wherein the evidence is increasingly mixed regarding whether providing long-term care in the community vis a vis within institutions, as has long been suggested, actually saves money. (16)
Because it is still unclear what the association between expenditures on home and community-based services, particularly nutrition-related services, and nursing home admissions is, we seek to examine one aspect of this relationship. We propose a model examining the effects of these expenditures on rates of change in nursing home admissions.
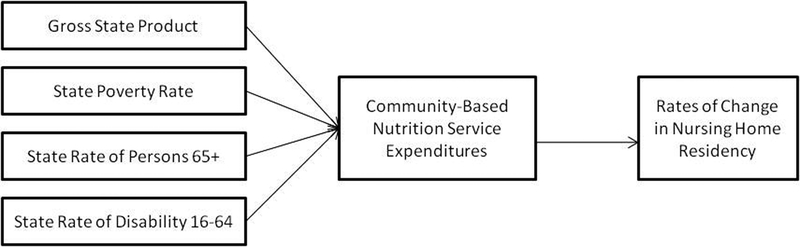
Conceptual Model
The present study was informed by a conceptual model that takes into account not only expenditures on community-based nutrition services but also other HCBS expenditures as well as socio-demographic and economic factors that may impact, directly or indirectly, the rates of change in nursing home residency between states. Socio-demographic factors include the poverty level of states, size of states’ older adult population, and size of the states’ disabled population. Economic factors include size of the states’ economies as measured by gross state product. Also, while there are many individual-level factors (e.g., functional status, comorbidity, social support, etc.) that may be associated with nursing home admissions, because this study is an ecological one that relies upon aggregate data at the state level, these individual factors that may influence nursing home residency rates may not be assessed in this model.
Socio-demographic factors.
States with higher levels of poverty may respond to welfare differently from other states. (17) This may be especially the case when poverty is spread across different age groups and states must make decisions to allocate resources according to poverty levels within those groups. Therefore, in addition to poverty level of the state, we take into account the proportion of older adults residing in those states. We might expect that states such as Florida and Arizona with high concentrations of older adults to respond differently to the needs of the older adult population than states with lower concentrations of older adults. Additionally, both of these factors impact levels of funding from the federal government which could affect states’ rates of delivery or use of these services, as well as states’ contributions of funding. Finally, in addition to poverty and residents 65 and older, we examine the effects of state level percentage of residents with a disability because of some home and community based services are made available to disabled persons. This is simply considered as a covariate because of the possible association with overall total long-term care expenditures and HCBS expenditures other than OAA programs, because OAA programs are not available to the general disabled population.
Economic factors.
Gross state product (GSP) is a sum of production and income generated by state during a given year (18) and has been shown to effectively control for economic differences across time and region. (19 & 20) GSP is also a reliable indicator of the size of the state’s economy which can influence their ability to contribute to welfare programs that include older adults’ nutrition programs.
Additionally, because we recognize that nutrition services are only one component of an array of publicly financed programs for older persons residing in the community, we also consider more comprehensively the total expenditures states devote to community based services. Previous research on this topic has shown that, particularly for older adults who do not have children, states commitment to HCBS reduces risk of nursing home placement. (4)
Hypothesis.
The purpose of this paper is to examine the impact of total state-level expenditures on OAA Title III Nutrition Services, namely home delivered and congregate meals, on rates of change in rates of nursing home residency of older adults. We hypothesize that expenditures devoted to nutrition programs for these home and community-based nutrition services are inversely related to changes in state-level rates of institutionalization for older adults from one year to the next, such that states that spend more money per capita on community-based nutrition programs will have smaller increases in rates of institutionalization.
METHODS
We used data collected from the Administration on Aging, Medicare Minimum Data Set, the United States Census Bureau, and multiple sources that report state-level spending on LTC to evaluate whether state-level expenditures on Title IIIC Nutrition Services was associated with rates of nursing home residency at the state level. While the ecological method precludes any deductions about individual-level associations, it does allow researchers to examine relationships at an aggregate level, in this case, the state level. The ecological approach to research is considered an effective methodology for examining the sorts of relationships we are interested in studying and for generating hypotheses for future research. (21) This study was reviewed by the University of Alabama at Birmingham Institutional Review Board and deemed to be not human subjects research.
Databases
Several databases were linked together for the purpose of these analyses. They are described here.
AGID.
The AGing Integrated Database (AGID) is an on-line database created by the AoA that allows users to query the system to obtain customized tables of AoA-related data files, including information on clients served, providers of services, and expenditures for particular programs. Additionally, the AGID includes population characteristics obtained from the the most recent (2007–2008) American Community Survey (ACS). (22) AGID data obtained for this study includes State Program Reports for the years 2007 and 2008.
Minimum Data Set.
The Minimum Data Set (MDS), a federally mandated data collection form for clinical assessment of all residents in Medicare or Medicaid certified nursing homes, was used to estimate rates of institutionalization. (23 & 24) MDS information is transmitted electronically by nursing homes to the MDS database in their respective states. MDS information from the state databases is captured in the national MDS database at the Centers for Medicare and Medicaid Services. The MDS is highly reliable and frequently used for research purposes. Data used in this study include quarterly reports on the number of all individuals in nursing homes receiving Medicaid and Medicare reimbursements for 2007 and 2008.
Home and Community Based Services and Long-term Care Expenditures.
Data used to analyze HCBS and LTC expenditures were obtained from multiple sources, following the method used by Muramatsu and colleagues. (4) This method is described below in our description of variables. Medicaid expenditures included monies spent on home health, personal care, nursing homes, and HCBS waivers. These data were obtained from Thomson Reuters’ annual report on “Medicaid LTC expenditures in FY 2007.” (25) Additional expenditures on HCBS from the AoA were compiled from AGiD. (22) Monies spent on the Social Services Block Grant were obtained from the US Department of Health and Human Services. (26) Additionally, state governments’ spending on HCBS was included. These data were obtained from the AARP’s annual report on “State-funded home and community-based services programs for older adults.” (27) The variables included accounted for state level commitment to HCBS and are a valid representation of the long-term care context in the states. (4) In order to examine if the nutrition services component independently impacts nursing home admission, both overall spending on HCBS (less nutrition services) and spending on nutrition services was included.
Variables
Dependent Variable.
The dependent variable is the state-level rate of change in nursing home residency from 2007–2008. This variable was used to evaluate the possible effects of expenditures on change in rates from year to year because rates in 2008 are not independent of the previous year. To create this variable, we first determined the proportions of persons ≥65 who were in a nursing home in 2007 (t1) and 2008 (t2). The formula was: number of persons in a nursing home (obtained from MDS Data) divided by the number of persons ≥65 (based upon Census Bureau Data). Next, we calculated rate of change in rate of nursing residency using the formula: [(t2-t1)/t1]*100. Nursing home residency was assessed by averaging the quarterly reports across 2007 and the reports across 2008 for persons 65+. The MDS captures resident counts for all persons in Medicare or Medicaid nursing home facilities.
Independent Variables.
The primary independent variables were state-level expenditures on home delivered and congregate meals per non-institutionalized older adult (obtained from the AGID Database). The percentage of older adults using these services are very small, potentially indicating the need for more advertisement and promotion of their availability. Furthermore, state-level spending on all LTC and specifically on HCBS was entered into the models as well. Socio-demographic and economic control variables that might affect rate of change in nursing home entry were included in our analyses.
Home-delivered and congregate meal expenditures per non-institutionalized older adult.
Home delivered and congregate meal expenditures (including total federal, state, and other sources of funding for Title IIIC) was divided by the population of older adults ≥65 years older for a total expenditure per non-institutionalized older adult (separately for home delivered and congregate meals).
Home and Community Based Services Expenditures Per Capita.
This variable was calculated by adding all sources of LTC expenditures except home delivered and congregate meal expenditures and nursing home expenditures. This figure was then divided by the number of non-institutionalized persons 65 and older.
Percent of Long-term Care Expenditures Spent on Home and Community Based Services.
This variable was calculated by dividing HCBS expenditures by total LTC expenditures.
Socio-demographic variables.
The socio-demographic control variables included in our analyses are 1) percent of the state population below poverty, 2) percent of the state population over 65 years of age, and 3) percent of persons in the state age 16–64 who are disabled.
Economic variable.
Gross state product (GSP) was also controlled for in our models. GSP is a sum of production and income generated by each state during a given year (Bureau of Economic Analysis, 2009).
Weighting Variable.
Total population, defined as the number of persons residing in the state in 2007 based on the ACS, is used as the weight in the weighted least squares analysis, in order to correct for our small sample size and variation among states.
Analysis
Analyses were conducted using Stata version 11.1. Descriptive statistics were generated to characterize state-level differences. Weighted least squares (WLS) regression was used to evaluate our hypothesis. This approach closely approximates ordinary least squares regression, however it allows for the correction of heteroscedasticity with the use of analytic weights, which was a problem in this sample because of small sample size and substantial variation in the size of the individual states. (28)
Five models were fit. First, only control variables were included in Model 1. In Model 2, congregate meals expenditures were included, followed by home delivered meal expenditures in Model 3. In Model 4, per capita HCBS expenditures were added, and finally, in Model 5, percent of LTC expenditures devoted to HCBS were included. Fitting five models allowed us to examine iterative changes in model fit when the two primary variables of interest, congregate and home delivered meal expenditures, were added sequentially. Then, we were able to examine changes with the addition of overall HCBS expenditures variables.
RESULTS
Sample Description
Initial analysis included all 50 States, however in the final analysis Alaska was excluded because it was an extreme outlier and influential case, especially in regard to state expenditures. Tables 1 and 2 present state-level descriptive statistics (including Alaska). Rates of nursing home residency per 1,000 individuals ≥65 varied widely among states with a low of 11.81 in Arizona in 2008 to a high of 57.50 in North Dakota in 2007. Rates of change in nursing home residency rates from 2007 to 2008 also varied largely with Delaware demonstrating an increase in rates of nursing home residency of 1.61% and Arizona having a decrease of 9.92%. States also varied widely on per capita expenditures for home delivered and congregate meals, with Arizona spending the least on home delivered meals ($7.30) and Wyoming spending the most on home delivered meals ($72.44) and Mississippi spending the least on congregate meals ($3.80) and Wyoming spending the most ($119.45).
Table 1.
State Level Population Data for Older Adults
| 2007 | 2008 | 2007–2008 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| State | Total Population | Population 65 and older | Ratea Instit. 65 and older | Total Population | Population 65 and older | Ratea Instit. 65 and older | Change in Rate of Instit.* | Rate of Change in Instit.** | ||
| Alabama | 4,627,851 | 625,756 | 31.61 | 4,661,900 | 641,667 | 30.62 | −.99 | −3.13% | ||
| Alaska | 683,478 | 47,935 | 9.00 | 686,293 | 50,277 | 8.74 | −.26 | −2.86% | ||
| Arizona | 6,338,755 | 820,391 | 11.81 | 6,500,180 | 862,573 | 10.64 | −1.17 | −9.92% | ||
| Arkansas | 2,834,797 | 397,108 | 40.53 | 2,855,390 | 407,205 | 38.67 | −1.86 | −4.60% | ||
| California | 36,553,215 | 4,003,593 | 20.34 | 36,756,666 | 4,114,496 | 19.52 | −.83 | −4.06% | ||
| Colorado | 4,861,515 | 492,685 | 28.09 | 4,939,456 | 511,094 | 26.33 | −1.76 | −6.26% | ||
| Connecticut | 3,502,309 | 472,284 | 49.91 | 3,501,252 | 478,007 | 47.98 | −1.93 | −3.86% | ||
| Delaware | 864,764 | 117,678 | 29.41 | 873,092 | 121,688 | 29.88 | .47 | 1.61% | ||
| Florida | 18,251,243 | 3,098,364 | 19.38 | 18,328,340 | 3,187,797 | 18.59 | −.79 | −4.07% | ||
| Georgia | 9,544,750 | 942,832 | 31.14 | 9,685,744 | 981,024 | 29.48 | −1.66 | −5.33% | ||
| Hawaii | 1,283,388 | 183,994 | 18.60 | 1,288,198 | 190,067 | 17.95 | −.65 | −3.50% | ||
| Idaho | 1,499,402 | 174,946 | 22.00 | 1,523,816 | 182,150 | 20.98 | −1.02 | −4.61% | ||
| Illinois | 12,852,548 | 1,548,781 | 37.56 | 12,901,563 | 1,575,308 | 35.82 | −1.74 | −4.63% | ||
| Indiana | 6,345,289 | 795,441 | 43.26 | 6,376,792 | 813,839 | 41.41 | −1.85 | −4.27% | ||
| Iowa | 2,988,046 | 438,448 | 54.11 | 3,002,555 | 444,554 | 52.21 | −1.90 | −3.51% | ||
| Kansas | 2,775,997 | 360,216 | 47.15 | 2,802,134 | 366,706 | 44.74 | −2.41 | −5.11% | ||
| Kentucky | 4,241,474 | 549,504 | 36.43 | 4,269,245 | 565,867 | 35.08 | −1.34 | −3.69% | ||
| Louisiana | 4,293,204 | 522,334 | 39.70 | 4,410,796 | 540,314 | 37.28 | −2.41 | −6.08% | ||
| Maine | 1,317,207 | 194,986 | 29.49 | 1,316,456 | 199,187 | 28.39 | −1.11 | −3.75% | ||
| Maryland | 5,618,344 | 661,809 | 31.37 | 5,633,597 | 679,565 | 29.82 | −1.54 | −4.92% | ||
| Massachusetts | 6,449,755 | 858,939 | 44.12 | 6,497,967 | 871,098 | 42.57 | −1.55 | −3.51% | ||
| Michigan | 10,071,822 | 1,280,152 | 27.65 | 10,003,422 | 1,304,322 | 26.93 | −.72 | −2.60% | ||
| Minnesota | 5,197,621 | 636,216 | 43.56 | 5,220,393 | 650,519 | 41.18 | −2.38 | −5.46% | ||
| Mississippi | 2,918,785 | 364,614 | 36.79 | 2,938,618 | 371,598 | 36.13 | −.66 | −1.80% | ||
| Missouri | 5,878,415 | 788,371 | 40.12 | 5,911,605 | 805,235 | 38.78 | −1.33 | −3.33% | ||
| Montana | 957,861 | 133,578 | 33.64 | 967,440 | 137,312 | 32.18 | −1.46 | −4.34% | ||
| Nebraska | 1,774,571 | 236,648 | 48.09 | 1,783,432 | 240,847 | 45.34 | −2.75 | −5.71% | ||
| Nevada | 2,565,382 | 285,654 | 13.11 | 2,600,167 | 296,717 | 12.58 | −.54 | −4.09% | ||
| New Hampshire | 1,315,828 | 165,742 | 37.31 | 1,315,809 | 169,978 | 36.27 | −1.04 | −2.79% | ||
| New Jersey | 8,685,920 | 1,134,636 | 32.96 | 8,682,661 | 1,150,941 | 32.31 | −.65 | −1.98% | ||
| New Mexico | 1,969,915 | 250,235 | 20.91 | 1,984,356 | 260,051 | 19.03 | −1.87 | −8.96% | ||
| New York | 19,297,729 | 2,546,405 | 36.37 | 19,490,297 | 2,607,672 | 35.56 | −.80 | −2.20% | ||
| North Carolina | 9,061,032 | 1,103,413 | 29.67 | 9,222,414 | 1,139,052 | 28.28 | −1.39 | −4.67% | ||
| North Dakota | 639,715 | 93,285 | 57.50 | 641,481 | 94,276 | 56.08 | −1.42 | −2.47% | ||
| Ohio | 11,466,917 | 1,545,085 | 41.80 | 11,485,910 | 1,570,837 | 40.27 | −1.53 | −3.65% | ||
| Oklahoma | 3,617,316 | 480,140 | 33.63 | 3,642,361 | 490,637 | 32.41 | −1.21 | −3.61% | ||
| Oregon | 3,747,455 | 488,936 | 13.76 | 3,790,060 | 503,998 | 12.46 | −.99 | −9.42% | ||
| Pennsylvania | 12,432,792 | 1,889,660 | 36.67 | 12,448,279 | 1,910,571 | 35.87 | −1.30 | −2.17% | ||
| Rhode Island | 1,057,832 | 146,847 | 49.68 | 1,050,788 | 147,646 | 47.87 | −.79 | −3.64% | ||
| South Carolina | 4,407,709 | 573,098 | 25.76 | 4,479,800 | 596,295 | 24.89 | −1.81 | −3.35% | ||
| South Dakota | 796,214 | 113,555 | 51.57 | 804,194 | 116,100 | 49.97 | −.86 | −3.10% | ||
| Tennessee | 6,156,719 | 793,117 | 35.08 | 6,214,888 | 819,626 | 33.40 | −1.60 | −4.79% | ||
| Texas | 23,904,380 | 2,394,157 | 33.21 | 24,326,974 | 2,472,223 | 32.20 | −1.68 | −3.03% | ||
| Utah | 2,645,330 | 233,982 | 18.09 | 2,736,424 | 246,202 | 16.57 | −1.01 | −8.40% | ||
| Vermont | 621,254 | 84,425 | 31.35 | 621,270 | 86,649 | 31.57 | −1.52 | 0.70% | ||
| Virginia | 7,712,091 | 909,522 | 26.32 | 7,769,089 | 940,577 | 25.23 | .22 | −4.17% | ||
| Washington | 6,468,424 | 757,852 | 20.73 | 6,549,224 | 783,877 | 19.44 | −1.10 | −6.19% | ||
| West Virginia | 1,812,035 | 280,666 | 30.09 | 1,814,468 | 285,067 | 29.40 | −1.28 | −2.29% | ||
| Wisconsin | 5,601,640 | 736,301 | 39.59 | 5,627,967 | 750,146 | 38.24 | −.69 | −3.42% | ||
| Wyoming | 522,830 | 63,901 | 33.38 | 532,668 | 65,614 | 32.89 | −1.35 | −1.45% | ||
Rates are per 1,000 individuals.
Instit: Institutionalization
Change in Rate of Inst. = Rate of institutionalized persons 65 (2008) - Rate of institutionalized persons 65 (2007)
Rate of Change in Inst. = Change in Rate of Inst. / Rate of institutionalized persons 65 (2007)
Table 2.
State Baseline Characteristics: 2007
| State | Gross State Producta | Population 65+ (%) | Population in Poverty (%) | Population with Disability (%) | Expenditures on Home delivered meals($)b | Expenditures on Congregate meals ($)b | Pct of LTC Exp on HCBS | HCBS less HDM & CM ($)b |
|---|---|---|---|---|---|---|---|---|
| Alabama | 158,566 | 13.39 | 13.30 | 17.88 | 14.57 | 17.80 | 29.47 | 581.17 |
| Alaska | 43,117 | 6.81 | 16.60 | 13.63 | 100.86 | 99.34 | 63.32 | 4538.67 |
| Arizona | 237,397 | 12.82 | 10.90 | 11.46 | 7.30 | 5.72 | 80.47 | 65.11 |
| Arkansas | 90,864 | 13.89 | 14.20 | 18.09 | 29.11 | 21.46 | 35.99 | 765.63 |
| California | 1,742,172 | 10.78 | 17.30 | 10.22 | 17.28 | 19.11 | 59.28 | 1329.41 |
| Colorado | 226,266 | 10.04 | 13.10 | 10.22 | 15.11 | 16.41 | 52.66 | 1166.96 |
| Connecticut | 204,964 | 13.42 | 11.60 | 9.89 | 17.73 | 16.06 | 41.17 | 1828.24 |
| Delaware | 59,589 | 13.42 | 8.30 | 11.60 | 35.17 | 28.42 | 39.75 | 912.76 |
| Florida | 716,505 | 16.79 | 10.70 | 11.59 | 10.72 | 10.64 | 37.86 | 470.47 |
| Georgia | 376,410 | 9.75 | 12.60 | 12.07 | 16.88 | 12.41 | 44.08 | 686.80 |
| Hawaii | 58,676 | 13.95 | 14.80 | 9.89 | 19.38 | 11.49 | 44.13 | 923.40 |
| Idaho | 48,441 | 11.54 | 9.40 | 11.93 | 21.43 | 29.61 | 53.71 | 966.78 |
| Illinois | 583,990 | 11.96 | 12.80 | 9.89 | 22.29 | 13.94 | 42.73 | 652.71 |
| Indiana | 238,693 | 12.42 | 12.30 | 12.93 | 11.78 | 10.88 | 47.43 | 900.01 |
| Iowa | 121,945 | 14.61 | 12.50 | 11.58 | 22.65 | 24.31 | 52.28 | 1119.28 |
| Kansas | 110,645 | 12.94 | 11.00 | 11.68 | 25.10 | 22.62 | 58.60 | 1368.71 |
| Kentucky | 146,415 | 12.77 | 12.20 | 18.64 | 16.18 | 12.33 | 34.80 | 736.89 |
| Louisiana | 203,167 | 12.21 | 17.00 | 15.41 | 27.50 | 13.69 | 50.48 | 975.23 |
| Maine | 46,340 | 14.58 | 19.40 | 16.50 | 20.50 | 12.00 | 58.68 | 1747.20 |
| Maryland | 257,577 | 11.58 | 12.70 | 10.47 | 8.56 | 16.77 | 43.47 | 1106.40 |
| Massachusetts | 335,313 | 13.30 | 8.00 | 11.15 | 44.89 | 10.85 | 41.83 | 1346.25 |
| Michigan | 375,759 | 12.49 | 10.00 | 13.60 | 27.74 | 12.97 | 38.94 | 738.58 |
| Minnesota | 242,095 | 12.14 | 13.50 | 9.94 | 11.90 | 24.36 | 67.71 | 2752.31 |
| Mississippi | 84,586 | 12.44 | 9.70 | 18.36 | 15.19 | 3.80 | 21.71 | 527.89 |
| Missouri | 220,092 | 13.33 | 20.90 | 14.37 | 27.67 | 17.22 | 48.55 | 907.90 |
| Montana | 31,994 | 13.82 | 13.80 | 13.29 | 28.44 | 40.02 | 49.16 | 1075.60 |
| Nebraska | 75,290 | 13.27 | 14.40 | 10.97 | 23.71 | 43.17 | 42.37 | 1019.83 |
| Nevada | 123,054 | 11.10 | 11.30 | 10.62 | 31.21 | 11.33 | 49.90 | 540.66 |
| New Hampshire | 56,073 | 12.37 | 10.50 | 10.97 | 59.55 | 18.96 | 40.62 | 1312.54 |
| New Jersey | 448,426 | 12.93 | 8.00 | 8.95 | 19.01 | 16.83 | 37.12 | 925.81 |
| New Mexico | 72,161 | 12.41 | 8.70 | 13.56 | 36.19 | 29.71 | 76.06 | 2204.07 |
| New York | 1,028,320 | 13.07 | 18.30 | 11.03 | 30.53 | 36.03 | 56.12 | 3358.32 |
| North Carolina | 380,932 | 12.16 | 14.20 | 13.98 | 11.95 | 10.24 | 54.55 | 1224.47 |
| North Dakota | 25,851 | 14.61 | 14.60 | 9.54 | 36.10 | 52.05 | 34.60 | 954.77 |
| Ohio | 451,600 | 13.35 | 11.70 | 13.43 | 22.51 | 9.84 | 35.85 | 954.36 |
| Oklahoma | 130,094 | 13.23 | 13.20 | 16.36 | 15.58 | 25.42 | 48.75 | 1001.93 |
| Oregon | 150,984 | 12.92 | 16.70 | 13.51 | 14.58 | 11.97 | 72.31 | 1561.50 |
| Pennsylvania | 508,769 | 15.15 | 13.40 | 13.02 | 19.44 | 15.66 | 33.57 | 1034.24 |
| Rhode Island | 45,733 | 13.86 | 12.00 | 13.14 | 16.06 | 21.26 | 47.10 | 1817.69 |
| South Carolina | 146,211 | 12.81 | 11.50 | 14.32 | 18.97 | 11.25 | 41.79 | 613.49 |
| South Dakota | 32,008 | 14.22 | 15.70 | 11.22 | 22.65 | 52.11 | 45.41 | 991.29 |
| Tennessee | 235,753 | 12.74 | 13.60 | 15.88 | 13.88 | 8.60 | 36.44 | 854.33 |
| Texas | 1,068,119 | 9.93 | 16.10 | 11.50 | 14.85 | 12.13 | 48.54 | 743.55 |
| Utah | 97,963 | 8.84 | 16.90 | 9.95 | 26.62 | 22.20 | 47.10 | 615.16 |
| Vermont | 23,628 | 13.30 | 10.70 | 13.35 | 44.02 | 27.81 | 15.69 | 243.07 |
| Virginia | 368,604 | 11.62 | 10.20 | 10.83 | 13.10 | 9.03 | 47.67 | 720.89 |
| Washington | 291,298 | 11.54 | 9.60 | 13.44 | 7.49 | 10.97 | 66.23 | 1539.73 |
| West Virginia | 56,016 | 15.33 | 11.80 | 21.26 | 23.35 | 23.43 | 45.42 | 1246.92 |
| Wisconsin | 223,394 | 13.03 | 17.60 | 11.02 | 24.19 | 27.55 | 49.73 | 1329.55 |
| Wyoming | 29,904 | 12.18 | 10.90 | 12.89 | 72.44 | 119.45 | 63.15 | 1819.77 |
GSP is in millions of dollars.
Per capita expenditures are in dollars per non-institutionalized older adult(NIOA).
LTC: long term care
HCBS: home and community-based services
HDM: home delivered meals
CM: congregate meals
Weighted Least Squares Analysis
Results of the WLS models are presented in Table 3.
Table 3.
Unstandardized Regression Coefficients for Rates of Change in Rates of Institutionalized Older Adults from 2007–2008, Weighted by Total Population (N=49)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||
|---|---|---|---|---|---|---|
| Gross state product (millions of dollars) | −1.26E-06* | −1.49E-06* | −1.61E-6** | −1.6E-06** | −1.42E-06*** | |
| (.000) | (.000) | (.000) | (.000) | (.000) | ||
| Percent of state below poverty | −0.019 | −0.107 | −0.090 | −0.090 | −0.032 | |
| (.091) | (.098) | (.095) | (.099) | (.066) | ||
| Percent of state over age 65 | 0.264 | 0.206 | 0.213 | 0.214 | −0.008 | |
| (.143) | (.141) | (.136) | (.138) | (.097) | ||
| Percent of state disabled (age 16–64) | 0.104 | 0.169 | 0.162 | 0.162 | 0.051 | |
| (.119) | (.120) | (.115) | (.117) | (.080) | ||
| Congregate meal expenditures per NIOA | 0.056* | 0.022 | 0.022 | 0.031 | ||
| (.028) | (.031) | (.036) | (.024) | |||
| Home delivered meal expenditures per NIOA | 0.065* | 0.065* | 0.018 | |||
| (.030) | (.031) | (.022) | ||||
| HCBS expenditures per NIOA | −3.21E-06 | 0.001* | ||||
| (.000) | (.000) | |||||
| Percent LTC expenditures on HCBS | −0.122*** | |||||
| (.017) | ||||||
| Intercept | −9.082*** | −9.012*** | −10.030*** | −10.032*** | −0.814 | |
| Adjusted R2 | 0.06 | 0.12 | 0.19 | 0.17 | 0.63 | |
| F-Change Statistic | 1.83 | 3.88 | 4.53* | 0 | 51.81*** | |
Notes: Standard error is reported in parenthesis under the slope coefficient.
p<. 05;
p<. 01;
p<.0 01 (two-tailed tests).
NIOA: non-institutionalized older adults
LTC: long term care
HCBS: home and community-based services
In Model 1 that included only the socio-demographic and economic variables of the states, only GSP was significant (b= −1.22E-06, p≤.05). The overall model was not significant. When adding congregate meals expenditures into Model 2, GSP was significant (b=−1.49E-06, p≤.05), with a negligible effect. Also, the variable measuring congregate meal expenditures per non-institutionalized older adults was associated with change in nursing home residency (b=.056, p<.05). The F-change statistic was not significant, indicating that the addition of congregate meal expenditures did not improve model fit.
When home delivered meal expenditures were added in Model 3, GSP (b=−1.6E-06, p≤.01), and home delivered meal expenditures (b=.065, p≤.05) were significant. The F-change value was significant (F=4.53, p<. 05), indicating that the addition of home delivered meal expenditures significantly improved model fit. However, the direction of the home delivered meal variable was positive. This score indicates that for every addition dollar spent per non-institutionalized older adult (NIOA), rates of change in nursing home residency increase by .06.
In Model 4, the variable per capita home and community based services (HCBS) expenditures was added to the model but was not significant. GSP remained significant (b=−1.6E-06, p≤.01), as did expenditures on home delivered meals (b=.065, p≤.05). However, the F-change statistic was not significant indicating that the additional variable did not contribute in a statistically meaningful way to the model.
In the final model, Model 5, the variable percent of LTC expenditures on HCBS was added. GSP remained significant (b=−1.42E-06, p≤.001). In this model, states’ attention to HCBS, as measured by per capita HCBS expenditures (b=.001, p≤.05) and percent of LTC expenditures on HCBS (b=−.122, p≤.01), were significant. This indicates that for every additional percentage point of HCBS on long-term care, there is a decrease in the rate of change of nursing home residency of .122. The F-change statistic for this model indicates that addition of HCBS expenditures/LTC contributes significant additional value to his model (F=51.81, p<.001). This full model has an adjusted R2 of .63, indicating that 63% of the variance in rate of change in nursing home residency can be accounted for by the variables in this model.
DISCUSSION
Many states are actively engaged in rebalancing efforts that shift monies spent on nursing homes to community based services in order to enable older adults with functional impairments to remain in the community for as long as possible. In this study, we attempted to isolate the role of nutrition programs, within the context of other long-term care services targeted at older adults, on decreased rates of nursing home residence. This research expounds on the work of Kaye, LaPlante and Harrington (15) who demonstrate long-term cost savings as an effect of community-based interventions and Muramastu et al. (4) who demonstrate the importance of home and community based services.
The results presented in Models 2 and 3 suggest that expenditures on home delivered meal services may be related to the rates of change in nursing home residency status among older adults at the state level in the positive direction, which was not hypothesized. These findings may indicate that states with older populations who are at risk of nursing home admission connect their residents to services more effectively than other states.
Older adults at nutritional risk, many of whom have limited social networks and resources available to help them meet basic nutritional needs, may be at increased risk of both hospitalization and nursing home placement. (29) OAA nutrition programs are intended to support precisely these at-risk adults maintain independence in the community. Recent research, however, indicates that older adults who are especially vulnerable for both nutritional risk and nursing home placement, namely those who are recently discharged from hospitals may be underserved by OAA nutrition programs. (30 & 31)
In Models 4 and 5, which account for comprehensive HCBS expenditures at the state level, expenditures on home delivered and congregate meals did not remain significant. It should be noted that the percentage of older adults using these services is small, with an estimate of 5.1% of eligible persons actually receiving services in 2007. (32) This small number may influence the results. However, variables representative of states’ commitment to HCBS were associated with change in nursing home residency. It is possible and likely that some of the state-level spending was devoted to nutritional programs, but we are not able to detect this in our data. HCBS spending per capita was significant in the hypothesized direction, indicating that additional dollars spent on HCBS per person yielded a decrease in the rate of institutionalization among OAs. Though this variable was significant, its effect size was marginal. In the final model, for every dollar spent on HCBS, rate of change in nursing home residency decreased by approximately 0.122. Percentage of LTC expenditures on HCBS were significant in the opposite direction hypothesized. This may be because states with high concentrations of older adults are also places where expenditures in the community and in institutions are both high, masking the true positive effects of HCBS.
In conclusion, we find that home and community based services are associated with decreased rates of nursing home residency. While we believe that our findings are important for generally highlighting the importance of home and community-based services, we believe that further work is needed to more completely understand the relationship between state-level commitment to these services and particularly to nutrition-services, for older adults’ ability to remain in the community and avoid nursing home admission. We turn now to a discussion of the limitations of this particular study and look to how future work might provide more clarity on the relationships discussed herein.
Limitations
There are several limitations to our work. First, the state-level data used in our analyses are subject to the ecological fallacy wherein the implications of our findings at the state level may not extend to individuals within those states. Second, while weighted least squares regression is a robust method, our analyses includes only 49 cases and limited the number of variables which could be considered. Third, our analysis represents a cross-section of data from two years, rather than from a longer period of time. Fourth, data are not available on institutionalization of individuals in the age category 60–64. Thus, expenditure and participation data for the non-institutionalized population 60 and older were regressed on the rates of change in institutionalization rates 65 and older. Fifth, we are unable to control for the effects of privately-funded programs such as local, church-based meals on wheels programs. Sixth, the variables we selected for inclusion in our conceptual model do not comprehensively measure all factors that impact either nutrition services expenditures or rates of change in nursing home rates. Our decision for inclusion of particular variables was guided by what we believed was most important based on a review of the literature and given the data that was available and our small sample size. Additionally, we were unable to account for the number of persons in either 2007 or 2008 who were admitted to the nursing home for short-stay rehabilitative purposes. While this would be helpful information since this population would probably not be impacted by nutrition services, we do not anticipate that the proportion of persons in this category changed drastically from 2007 to 2008 because there were no major policy shifts between the years.
There are many and varied complex factors that contribute to nursing home placement. These range from the individual and family level to the state and federal policy levels. Teasing out all of these interrelated factors is difficult and impossible in a single study. Our work represents a first step in our efforts to evaluate the potential role that nutrition programs may play in contributing to older adults’ ability to remain in the community.
The ecological design of this study precludes us from being able to speak about individual level outcomes, but it is useful in generating hypotheses to test at that level. Additionally, our work emphasizes that additional monies ought to be targeted at comprehensive evaluation of these programs, as well, particularly at the individual level. Comparisons between older adults who receive OAA nutrition services and those who do not is absent from the literature.
Future Directions
Future research is warranted that includes individual level data, utilizing larger sample sizes, with longitudinal waves of data collection, and a broader range of ages. Additionally, an examination of the effect of rates of participation on rates of nursing home residency lagged by years greater than one will require more sophisticated methods but may give more clear insight into relationships that exist.
Additionally, a comparison between matched older adults who receive nutrition services with those who do not is warranted. Use of large datasets, such as the National Health and Nutrition Examination Survey (NHANES) or the National Longitudinal Study of Aging might be particularly well-suited to evaluate more comprehensively the effects of the Title III Nutrition Services on nursing home entry, as well as other relevant health outcomes. Our research team, as well as AoA plans to use both NHANES data linked with Medicare claims data, for individual-level comparisons between participants and non-participants on health outcomes.
Figure 1.
Conceptual Model of Factors Predicting Rates of Change in Nursing Home Residency.
TAKE-AWAY POINTS.
Expenditures on home delivered meal services are associated with growth in nursing home residency among older adults at the state level. This was not expected and may be a function of states with larger older populations who are at risk of nursing home admission connecting their residents to services more effectively than other states.
HCBS spending per capita appears to be marginally associated with the rate of institutionalization among OAs, but the effects of home delivered and congregate meals are not significant. States that spend more of their long-term care dollars on home and community-based services have a significant decrease in rate of institutionalized older adults.
Future research is warranted to examine the association between home and community based services, particularly nutrition services, for the purpose of program improvement and for justifying expenditures on these important services. This work should utilize individual data and employ longitudinal methods to examine effects of these services over time.
BIBLIOGRAPHY
- 1.Kamp BJ, Wellman NS, Russell C. Position of the American Dietetic Association, American Society for Nutrition, and Society for Nutrition Education: Food and Nutrition Programs for Community-Residing Older Adults. Journal of Nutrition Education and Behavior 2000;42(2):72. [DOI] [PubMed] [Google Scholar]
- 2.O’Shaughnessy C The aging services network: accomplishments and challenges in serving a growing elderly population. Washington D.C.: National Health Policy Forum; 2008. [Google Scholar]
- 3.Kuczmarski MF, Weddle DO. Position paper of the American Dietetic Association: Nutrition across the spectrum of aging. Journal of the American Dietetic Association 2005;105(4):616–633. [DOI] [PubMed] [Google Scholar]
- 4.Muramatsu N, Yin H, Campbell RT, Hoyem RL, Jacob MA, Ross CO. Risk of Nursing Home Admission Among Older Americans: Does States’ Spending on Home- and Community-Based Services Matter? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 2007;62(3):S169–S178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Welcome {The Administration on Aging Home Page}. Accessed at http://www.aoa.gov/about/over/over_mission.Aspx on 15 October 2010.
- 6.Binstock RH. Title III of the Older Americans Act: An Analysis and Proposal for the 1987 Reauthorization. The Gerontologist 1987;27(3):259–265. [DOI] [PubMed] [Google Scholar]
- 7.Unofficial compilation of the Older Americans Act of 1965 as amended in 2006 (public law 109–365). Accessed at http://www.aoa.gov/aoaroot/aoa_programs/oaa/oaa_full.asp#_Toc153957692 on 15 October 2010.
- 8.Nutrition. Accessed at http://www.aoa.gov/AoAroot/Program_Results/Nutrition_Report/er_vol1ch5b.aspx on 15 October 2010.
- 9.Wellman NS, Rosenzweig LY, Lloyd JL. Thirty years of the Older Americans Nutrition Program. Journal of the American Dietetic Association 2002;102(3):348. [DOI] [PubMed] [Google Scholar]
- 10.FY 2008 U. S. profile of OAA programs. Accessed at http://aoa.gov/AoARoot/Program_Results/SPR/2008/Profiles/us.Xls on 28 September 2010.
- 11.Colello KJ. Older Americans Act: Title III Nutrition Services Program. In: Service CR, editor. Retrieved from http://aging.senate.gov/crs/nutrition1.pdf. 2010. [Google Scholar]
- 12.Evaluation of Title III-C nutrition services and Title VI Native American nutrition, supportive and family caregiver services programs—begun summer 2005. Accessed at www.aoa.gov/about/results/III-C-VI%20Evaluation%20status%20report on 28 September 2010.
- 13.Millen BE, Ohls JC, Ponza M, McCool AC. The Elderly Nutrition Program: An effective national framework for preventive nutrition interventions. Journal of the American Dietetic Association 2002;102(2):234. [DOI] [PubMed] [Google Scholar]
- 14.Evaluation of the federal elderly nutrition program. Mathematic Policy esearch,Inc Accessed at http://www.mathematica-mpr.com/nutrition/enp.asp. on October 3, 2010.
- 15.Kaye HS, LaPlante MP, Harrington C. Do Noninstitutional Long-Term Care Services Reduce Medicaid Spending? Health Affairs 2009;28(1):262–272. [DOI] [PubMed] [Google Scholar]
- 16.Weiner J Long-term care: Options in an era of health reform. Accessed at http://www.pioneernetwork.net/Data/Documents/AllianceLTCPaper.pdf on 10 October 2010.
- 17.Besley T, Case A. Political Institutions and Policy Choices: Evidence from the United States. Journal of Economic Literature 2003;41(1):7. [Google Scholar]
- 18.Gross domestic product by state. Accessed at http://www.bea.gov/regional/gsp/ on 12 October 2010.
- 19.Alamar B, Glantz SA. Effect of Smoke-Free Laws on Bar Value and Profits. American Journal of Public Health 2007;97(8):1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alamar BC, Glantz SA. Smoke-free Ordinances Increase Restaurant Profit and Value. Contemporary Economic Policy 2004;22(4):520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rothman KJ, Greenland S, Lash T,L Modern Epidemiology. 3rd ed Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 22.Welcome AGID {Aging Integrated Database}. Accessed at http://198.136.163.234/default.Asp on 10 September 2009.
- 23.Minimum data set overview. Accessed at http://www.cms.hhs.gov/MinimumDataSets20 on 10 September 2009.
- 24.Minimum data sets 2.0 overview. Accessed at http://www.cms.gov/MinimumDataSets20/ on 10 September 2009.
- 25.Burwell B Sredl K & Eiken S Medicaid LTC expenditures in FY 2007. Eagan (MN): Thomson Reuters: Medstat. Accessed at www.hcbs.org/moreInfo.php/doc/2374 on 12 October 2009. [Google Scholar]
- 26.U.S. Department of Health and Human Services, Administration on Children and Families, Office of Community Services. Social services block grant program annual report 2007.Washington D.C.: U.S. Government Printing Office; Accessed at: http://www.acf.hhs.gov/programs/ocs/ssbg/reports/2007/index.html on 12 October 2009. [Google Scholar]
- 27.Mollica RL, Simms-Kastelein K, and Kassner E. State-funded home and community-based services programs for older adults. Washington (DC): AARP Public Policy Institute and National Academy for State Health Policy; Accessed at http://assets.aarp.org/rgcenter/il/2009_06_hcbs.pdf on 12 December 2009. [Google Scholar]
- 28.Gill J Generalized Linear Models: A Unified Approach. Thousand Oaks, CA: Sage: Sage; 2001. [Google Scholar]
- 29.Yang Y, Brown CJ, Burgio KL, Kilgore ML, Ritchie CS, Roth DL, et al. Undernutrition at baseline and health services utilization and mortality over a 1-year period in older adults receiving Medicare home health services. Journal of the American Medical Directors Association 2011;12(4):287–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sahyoun NR, Anyanwu UO, Sharkey JR, Netterville L. Recently Hospital-Discharged Older Adults Are Vulnerable and May Be Underserved by the Older Americans Act Nutrition Program. Journal of Nutrition For the Elderly 2008; 29(2):227. [DOI] [PubMed] [Google Scholar]
- 31.Locher JL, Wellman NS. Never the Twain Shall Meet: Dual Systems Exacerbate Malnutrition in Older Adults Recently Discharged from Hospitals. Journal of Nutrition in Gerontology and Geriatrics 2011;30(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kamp BJ, Wellman NS, Russell C. Position of the American Dietetic Association, American Society for Nutrition, and Society for Nutrition Education: Food and Nutrition Programs for Community-Residing Older Adults. Journal of Nutrition Education and Behavior. 2010;42(2):72–82. [DOI] [PubMed] [Google Scholar]