Abstract
Black and Latina transgender women (BLTW) are disproportionately impacted by HIV but remain underrepresented in HIV and health services research. Between March 2016 and May 2017, BLTW (N=201) were recruited in Baltimore, Maryland and Washington, D.C. through convenience sampling for a survey assessing multilevel determinants of HIV risk and treatment outcomes. Interviews concluded with a rapid oral HIV test. Bivariate and multivariable logistic regression modeling was performed to identify gender affirmation-related correlates of self-reported HIV treatment interruptions (HIVTIs) among BLTW living with HIV who had initiated antiretroviral therapy (ART) (n=96). Among them, 57.3% (n=55) reported at least one HIVTI. Unmet surgical needs (aOR=1.6), past-year marijuana use (aOR=14.6), and no current hormone use (aOR=24.9) were significantly (p<0.05) associated with HIVTIs in multivariable analysis. Unmet need for gender affirmation may inhibit ART adherence, highlighting opportunities to mitigate care interruptions in alignment with community needs and goals.
Keywords: HIV treatment interruptions, gender affirmation, transgender, medication adherence, antiretroviral therapy
Resumen
Las mujeres transgéneras negras y latinas (MTNL) son afectadas de manera desproporcionada por el VIH, pero están insuficientemente representadas en las investigaciones sobre el VIH y los servicios de salud. Entre marzo del 2016 y mayo del 2017, reclutamos MTNL (N = 201) en Baltimore, Maryland, y Washington, D.C., a través de un muestreo de conveniencia para una encuesta que evaluó los determinantes de niveles múltiples del riesgo de VIH y del tratamiento del VIH. Las entrevistas concluyeron con una prueba oral rápida de VIH. Realizamos una regresión logística bivariada y multivariada para identificar los correlatos relacionados con la afirmación de género de las interrupciones del tratamiento del VIH (ITVIH) entre las MTNL que viven con el VIH que habían iniciado la terapia antirretroviral (TAR) (n = 96). Entre ellas, 57,3% (n = 55) reportaron al menos una ITVIH. Las necesidades quirúrgicas que no fueron satisfechas (aOR = 1.6), el uso de marihuana durante el año anterior (aOR = 14.6), y la falta del uso de hormonas para afirmación de género (aOR = 24.9) están significativamente asociadas (p<0.05) con las ITVIH en el análisis multivariada. La necesidad insatisfecha de afirmación de género puede inhibir la adherencia al TAR, destacando oportunidades para mitigar las ITVIH en concordancia con las necesidades y objetivos de la comunidad transgénera.
Introduction
Transgender women (TW) are highly impacted by HIV and experience suboptimal outcomes along the continuum of HIV prevention, care, and treatment [1–3]. HIV prevalence estimates among TW worldwide highlight the disproportionate burden of HIV infection, with pooled estimates ranging from 19.1% [1] to 25% [2]. Identity-based victimization [4–14], psychological trauma [2,5,8,12,14–19], and unequal power dynamics in sexual relationships [16,20–22] have been cited as drivers of sexual risk behaviors and HIV acquisition among TW globally. Additionally, diminished access to supportive, gender affirming healthcare undermines TW’s capacity and willingness to engage with HIV care and treatment services [8–10,12,16,23–30].
In the United States (U.S.), Black and Latina TW shoulder a disproportionate burden of HIV infections. A recent systematic review estimated an HIV prevalence of 14.1% (95% CI: 8.7–21.2%) among TW; this prevalence estimate increased to 44.2% (95% CI: 23.2–67.5%) among Black TW and 25.8% (95% CI: 11.7–47.7%) among Latina TW [31]. Thus, Black and Latina transgender women (BLTW) are a key-affected group in the U.S. HIV epidemic and a priority population for HIV services.
Diagnosing and appropriately linking persons living with HIV to treatment and supportive services is critical for facilitating improved outcomes along the HIV care continuum. While treatment adherence is associated with durable viral suppression [32], a growing body of research has documented low rates of HIV diagnosis [3,23], antiretroviral therapy (ART) adherence challenges [9,17,29,33], and suboptimal viral suppression [3,9,23,34,35] among TW. BLTW may be especially vulnerable to poor HIV outcomes, as their heightened exposure to overlapping sources of instability, from housing insecurity [34] to social and financial exclusion from health services [8,29], threatens their ability to access health services. A recent study of 422 Black TW sampled across six U.S. cities documented suboptimal viral suppression (24.5%) [3], suggesting that existing strategies for increasing knowledge of HIV serostatus and promoting ART adherence may be insufficient for BLTW.
Despite emerging evidence of disparate vulnerabilities for BLTW specifically, the available literature offers insufficient insight into appropriate interventions to improve HIV outcomes for BLTW. HIV treatment interruptions (HIVTIs) are critical indicators of challenges within the HIV care continuum and highlight barriers to healthcare as well as ART adherence. In order to improve HIV disparities, a deeper understanding of factors influencing HIVTIs among BLTW is needed.
The Gender Affirmation Framework
Using data derived from qualitative interviews, Sevelius developed a multilevel framework for contextualizing HIV risk behaviors among BLTW in the U.S. [22]. The Gender Affirmation Framework (GAF) highlights pathways through which stigma, resulting in social oppression and psychological distress, increases the need for gender affirmation among BLTW and simultaneously decreases access to social, medical, and legal sources of gender affirmation. The GAF situates these co-occurring sources of adversity in four principal domains: (1) social oppression (e.g., transphobia, poverty) and (2) psychological distress (e.g., depression, body shame) that lead to (3) identity threat (e.g., need for gender affirmation exceeds access to gender affirmation), and ultimately (4) high-risk contexts (e.g., engagement in sex work, sex under the influence of substances) that result in HIV risk behaviors (e.g., condomless receptive anal intercourse, unsafe injection practices).
While the original GAF outcomes are proximal risk factors for HIV acquisition, we posit that the framework could also be used to describe risk for suboptimal engagement along the HIV care continuum among BLTW. In this study, we investigate how experiences articulated in the GAF may affect HIV treatment adherence and interruptions. Specifically, we apply this framework to measure the effect of gender affirmation-related, multilevel factors on HIVTIs in a sample of BLTW living with HIV in two U.S. cities.
Methods
Participants and Procedures
From March 2016 to May 2017, 201 BLTW participated in the STROBE (Supporting Transgender Research and Opportunities in the Baltimore and D.C. Environments) study. This study aimed to assess structural, social, and individual determinants of HIV vulnerability and treatment outcomes among urban BLTW in order to inform tailored HIV prevention and care services.
TW – individuals who were assigned male sex-at-birth (SAB) and identified as female, woman, or transgender [36] – were eligible for enrollment if they (1) were 15 years of age or older, (2) currently resided in the Baltimore or Washington, D.C. metropolitan areas, (3) self-identified as Black/African-American, Latina/Hispanic, or Mixed Race, (4) agreed to complete a rapid oral HIV test, and (5) spoke English or Spanish.
The STROBE study launched in Baltimore, M.D., in March 2016 and expanded to Washington, D.C., in February 2017 in response to recruitment challenges. The survey was translated from English to Spanish to improve accessibility to Latina TW. Terminology related to gender experiences were reviewed closely by community members to ensure translations were appropriate and affirming for Latina TW. Study methods have been described in detail elsewhere [37].
BLTW were reached through convenience sampling approaches: recruitment at local HIV and and/or transgender community events and activities; study promotion through social and client networks of local community-based organizations, including local health and social services providers for TW; and word-of-mouth.
Participants completed an interviewer-administered, tablet-based quantitative survey in English or Spanish, followed by a rapid oral HIV test (OraQuick Rapid HIV=1/2 test). Participants were not required to stay receive their HIV test results. All participants who tested positive for HIV and received their test results were offered linkage to confirmatory testing at local clinics. Interviewers used local resource guides to facilitate referral to health and social resources when requested. Interviews lasted between 60–90 minutes and were administered in private rooms at community-based organizations and community health centers. Participants received a $50 Visa gift card for participation.
Ethics
Verbal informed consent was obtained from all individual participants included in the study. The study protocol was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB00006279).
Measures
The primary outcome measure, lifetime HIVTIs, was measured using a single item asked of participants self-reporting HIV-positive status and initiating ART, “Have you ever stopped or experienced interruptions while taking your HIV medication?” Responses to this question were dichotomized as having experienced an HIVTI or not.
We selected potential covariates corresponding with sources of social and structural oppression identified in the GAF. Operationalization of selected covariates by their corresponding GAF domain is described below.
Social Oppression
Measures of social oppression capture consequences of transphobia, racism, stigma, and rejection, as articulated in the GAF. In the present study, these measures included socio-economic (e.g., unemployment, poverty), healthcare-related (e.g., transportation, misgendering in health facilities), and violent (e.g., sexual or physical violence) manifestations of social oppression. Current unemployment was defined as reporting no full- or part-time employment. Personal monthly income was dichotomized as above or below the federal poverty line (FPL) [38]. Ten items elicited participants’ barriers to healthcare access, ranging from social (e.g., previous poor experiences seeking services) to structural (e.g., transportation). Responses were dichotomized, comparing participants who reported experiencing one or more access barriers to participants who reported experiencing none. Lifetime experiences with physical, sexual, and psychological violence were assessed using a modified version of the Revised Conflict Tactics Scale (CTS-2) [39]. We expanded the CTS-2 to include violence by perpetrators other than intimate partners. CTS-2 data were used to create binary variables indicating presence or absence of recent (past 12 months) experience of physical, sexual, and psychological violence.
Psychological Distress
Indicators of psychological distress assess manifestations of duress, induced by oppressive experiences unique to BLTW (e.g., dually enacted racism and transphobia). In the GAF, these indicators include internalized transphobia, depression, post-traumatic stress disorder (PTSD), and suicidality. Internalized transphobia was measured using a validated sub-scale of the Gender Minority Stress and Resilience Measure [40]. Participants evaluated their level of agreement on a three-point Likert scale (0–2) with eight statements (e.g., “I sometimes resent my transgender identity”). Summary scores ranged from 0 to 24, with higher scores reflecting greater internalized transphobia.
Depression was assessed using the two-item Patient Health Questionnaire-2 (PHQ-2), a widely used screener for current depressive symptomology [41]. Participants were asked how often, over the past two weeks, they had: 1) “little interest or pleasure in doing things” and 2) “feeling down or depressed or hopeless.” PHQ-2 sum scores (range: 0–6) were dichotomized, with a pre-established threshold score of three or higher categorized as experiencing recent depressive symptomology [41]. Lifetime suicidality was determined using responses to a single dichotomous measure (i.e., “Did you ever have thoughts about killing yourself?”). PTSD symptomology was established using the 4-item Primary Care PTSD Screener (PC-PTSD) [42]. Participants either affirmed or denied experiencing four symptoms consistent with PTSD in the past 30 days (e.g., “Have you had nightmares about a traumatic event or thought about it when you did not want to?”). PC-PTSD sum scores (range: 0–4) were dichotomized, with a pre-established threshold score of three or higher categorized as experiencing recent PTSD symptomology [42].
Identity Threat
Identity threat was operationalized using variables representing access to and/or uptake of gender affirming interventions, including hormones, surgery, and gender marker changes on legal documents [22]. We interpreted reduced access to gender affirming interventions as experiencing heightened degrees of identity threat.
Current hormone use was assessed using a single item and dichotomized to compare participants who reported current hormone use to those who were not currently taking or never took hormones for gender transition. To assess unmet surgical need, participants were asked about desire for and access to 13 gender affirming medical procedures (e.g., breast augmentation, facial feminization). Response options included: “do not want it,” “not sure if I want it,” “want it,” or “have had it.” All “want it” responses were aggregated, with higher scores (range: 0–13) corresponding to greater unmet need for surgical gender affirmation. Legal gender affirmation was determined by asking participants about the extent to which their identification documents (IDs) list their desired name and gender marker. Responses indicating neither names nor gender markers had been changed on any legal document (e.g., birth certificate, passport, driver’s license) were categorized as not having accessed legal gender affirmation, versus some or all names and/or gender markers having been changed.
High-Risk Contexts
In the GAF, several social and structural contexts serve as mediating factors in the causal pathway from social oppression and psychological distress to sexual risk behaviors among BLTW. These high-risk contexts include substance use to cope with intersecting sources of discrimination (e.g., racism and transphobia) and other hardships as well as engagement in sex work for income to mitigate housing and food insecurity. We therefore assessed the association between these high-risk contexts and HIVTIs.
Recent drug use was assessed by asking participants to indicate which substances they had used in the past 12 months from an itemized list of non-injection drugs. Responses were collapsed into a categorical variable of no drug use (reference group), marijuana use only, or use of other illicit drugs (irrespective of marijuana use). We measured heavy drinking and/or alcohol abuse or dependence using the Alcohol Use Disorders (AUD) Identification Test for Consumption (AUDIT-C), a 3-item screener [43]. Scores of three or higher on the AUDIT-C were considered consistent with AUD.
Participants met criteria for lifetime sex exchange if they reported ever trading sex for money, shelter, food, drugs, or other material goods, including payment for gender affirming services (i.e., hormones, silicone, surgery). Participants reporting any inconsistent or unstable housing in the past 12 months from a provided list of 12 unstable housing circumstances (e.g., “stayed in a shelter,” “denied a house or apartment,” “moved to escape violence”) were classified as unstably housed.
Data Analysis
Data were analyzed using Stata 14.2 (College Station, TX, USA). Descriptive frequencies were calculated for relevant sociodemographic characteristics and other GAF-related measures. Binomial logistic regression was performed to identify associations between the outcome measure, lifetime HIVTIs, and independent covariates nested within the GAF domains. Independent variables meeting or exceeding a significance threshold of p<0.1 in bivariate analysis were introduced into multivariable logistic regression models, adjusted for select sociodemographic factors including age (as a continuous variable), race, ethnicity, study location, and living above or below the FPL. Due to the quantity of independent variables introduced into regression analysis, scores for model-specific Akaike Information Criteria (AIC) and Bayesian Information Criteria (BIC) were calculated and appraised in selecting the appropriate multivariable model. AIC and BIC measure the comparative quality of regression models using covariate parsimony as a primary assessment criterion, with variable-saturated models corresponding to higher AIC and BIC scores and, subsequently, poorer quality models [44]. A Hoesmer-Lemeshow goodness-of-fit test [45] was run on the selected multivariable model to verify that each covariate included in the final model contributed to variability in the primary outcome, HIVTI.
Results
Figure 1 presents key indicators for HIV-related clinical outcomes among 112 (55.7%) BLTW living with HIV in the study sample (N=201). The majority of participants (86.6%) reported knowing their HIV status prior to the HIV test administered during the study. Participants were highly engaged in care; all participants with prior knowledge of their serostatus had seen a healthcare provider for HIV-related care. Almost all (94.8%) reported current ART use with an average duration of 12.1 years (SD: ±9.6 years) on ART, however, HIVTIs were common. Among BLTW who had initiated ART (n=96), 57.3% (n=55) reported at least one HIVTI since beginning treatment.
Figure 1.
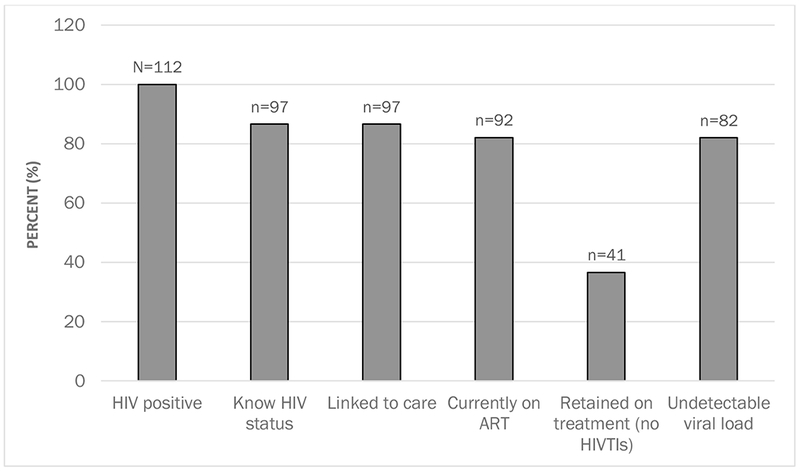
HIV care continuum among a sample of Black and Latina transgender women (n=112)
Table I summarizes sociodemographic and GAF-related characteristics among the sub-sample of HIV-positive BLTW who had initiated ART. The mean age was 41.1 years (SD: ±11.5 years), with most (76.0%) recruited from Washington, DC. A majority of participants (71.9%) identified as Black/African American, with 16.7% identifying as Hispanic/Latina. Most reported having at least high school-level education (74.7%).
Table 1.
Descriptive statistics of sociodemographic factors, HIV clinical indicators, and hypothesized covariates among a sample of Black and Latina Transgender Women living with HIV in Baltimore, MD, and Washington, DC (n=96).
| n/N (mean) | % (SD) | |
|---|---|---|
| Sociodemographic Factors | ||
| Age, in years | (41.1) | (11.5) |
| Race | ||
| Black/African American | 69/96 | 71.9 |
| American Indian, Alaska Native, Indigenous | 7/96 | 7.3 |
| Other | 5/96 | 5.2 |
| More than one race | 15/96 | 15.6 |
| Ethnicity: Hispanic/Latina | 16/96 | 16.7 |
| Education: completed high school or higher education | 71/95 | 74.7 |
| Location | ||
| Washington, DC | 73/96 | 76.0 |
| Baltimore, MD | 23/96 | 24.0 |
| HIV Clinical Indicators | ||
| Currently on ART | 91/96 | 94.8 |
| Duration on ART, in years | (12.1) | (9.6) |
| Ever experienced an interruption to HIV treatment | 55/96 | 57.3 |
| Social Oppression | ||
| Income below the U.S. federal poverty line, past 30 days | 73/92 | 79.4 |
| Housing instability, past 12 months | 52/96 | 54.2 |
| Currently unemployed | 43/96 | 44.8 |
| 1 or more barriers to accessing healthcare | 79/96 | 82.3 |
| Physical violence, past 12 months | 28/96 | 29.2 |
| Sexual violence, past 12 months | 13/96 | 13.5 |
| Psychological violence, past 12 months | 38/96 | 39.6 |
| Psychological Distress | ||
| Internalized transphobia | (2.9) | (3.8) |
| Depression symptom criteria, past two weeks | 24/95 | 25.3 |
| PTSD symptom criteria, past 30 days | 38/96 | 39.6 |
| Lifetime suicidal ideation | 47/96 | 49.0 |
| Identity Threat | ||
| Not currently taking hormones for gender affirmation | 15/94 | 16.0 |
| Unmet surgical need | (3.7) | (2.3) |
| No name and/or gender marker change on legal documents | 25/96 | 26.0 |
| High-Risk Contexts | ||
| Drug use, past 12 months | ||
| No drug use | 43/96 | 44.8 |
| Marijuana only | 20/96 | 20.8 |
| Any Illicit substance (with or excluding marijuana) | 33/96 | 34.4 |
| Alcohol use disorder, AUDIT-C | 37/96 | 38.5 |
| Lifetime sex exchange | 77/96 | 80.2 |
ART: antiretroviral therapy; AUDIT-C: Alcohol Use Disorder Identification Test—Consumption; PTSD: Post-Traumatic Stress Disorder; SD: standard deviation.
BLTW participants experienced high degrees of social oppression, manifesting through high unemployment, poverty, and exposure to violence. While more than half of BLTW participants were employed at the time of the survey (55.2%), over three-fourths (79.4%) reported monthly personal incomes below the FPL. Nearly half (54.2%) of participants reported housing instability in the past year. Recent experiences with violence were notably high, with a substantial number reporting experiences with physical (29.2%), sexual (13.5%), and psychological (39.6%) violence, in the past year.
Barriers to healthcare access were common, as illustrated in Figure 2. A majority (82.3%) of participants reported one or more barriers to general healthcare access, from transportation (53.1%) to previous mistreatment by providers and/or other patients in healthcare settings (9.4%). Compared to those without any interruptions to their HIV treatment, BLTW with lifetime HIVTIs were twice as likely to report perceived provider discomfort with caring for transgender patients as a barrier to accessing health services (29.1% vs. 12.2%, p<0.05).
Figure 2.
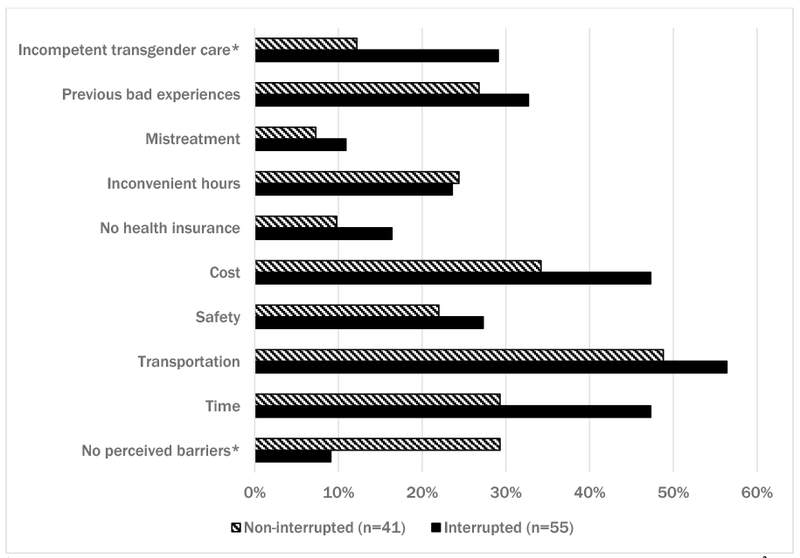
Distribution of barriers to healthcare access (%) among Black and Latina transgender women, stratified by HIV treatment interruption status (n=96).
Given the high burden of social oppression reported by participants, the high prevalence of psychological distress and HIV-risk behaviors were unsurprising. Recent depressive symptoms (25.3%) and PTSD (39.6%) accompanied noteworthy levels of suicidal ideation (49.0%) among BLTW. Over half (52.2%) of participants used some type of non-injection drugs (including marijuana) in the past year, and over one-third (38.5%) reported alcohol consumption behaviors consistent with AUD. The vast majority of participants (80.2%) reported ever trading sex in exchange for money or other goods.
Despite experiences with social and structural adversity, many participants reported accessing legal and medical gender affirming services. Seventy-four percent of participants reported at least one type of legal gender transition (i.e., desired name or gender marker on identification). Eighty-four percent reported currently taking hormones for gender affirmation. However, unmet needs for surgical gender affirmation were considerably high: of the 91.7% of participants who sought gender affirming surgical interventions, only 27.3% successfully obtained them, with an average of 3.9 (SD: ±2.3) surgical procedures desired but not obtained.
Table II presents associations identified between HIVTIs and GAF-related covariates using bivariate and multivariable logistic regression. In multivariable analysis, current hormone use was negatively associated with HIVTIs, while unmet surgical needs and past-year marijuana use were positively associated with HIVTIs. BLTW who reported not taking hormones exhibited 25 times the odds of HIVTIs (adjusted Odds Ratio [aOR]=24.9, 95% Confidence Interval [CI]: 3.3–118.9, p=0.002) compared to BLTW reporting current hormone use. Conversely, for each additional gender affirming surgical procedure desired but not obtained, the odds of HIVTIs increased by over 50% (aOR=1.6, 95% CI: 1.2–2.1, p=0.004). Finally, BLTW reporting past-year marijuana use were 10 times more likely (aOR=10.5, 95% CI: 2.1–53.7, p=0.005) to report an HIVTI than participants reporting no drug use in the past 12 months. Significant associations identified in bivariate analysis between HIVTIs and other GAF-related covariates, namely history of suicidal ideation (OR=2.4, 95% CI: 1.1–5.5, p=0.038) and one or more barriers to healthcare access (OR=4.1, 95% CI: 1.3–12.9, p=0.015), were attenuated after adjustment for sociodemographic factors and other gender affirmation-related covariates in multivariable analysis.
Table 2.
Bivariate and multivariable relationships between hypothesized covariates and lifetime self-reported HIV treatment interruptions among a sample of Black and Latina Transgender Women in Baltimore, MD, and Washington, DC (n=96).a
| Bivariate Models | Multivariable Modelb | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | p-value | AOR (95% CI) | p-value |
| Age, in years | 1.0 (0.9-1.0) | 0.540 | 1.0 (0.9-1.0) | 0.698 |
| Race | ||||
| Black/African American | 1 | Reference | 1 | Reference |
| American Indian, Alaska Native, Indigenous | 0.5 (0.1-2.2) | 0.325 | 0.1 (0.0-1.1) | 0.055 |
| Other | 0.2 (0.1-1.4) | 0.099 | 0.1 (0.0-1.2) | 0.068 |
| More than one race | 0.7 (0.2-2.1) | 0.520 | 0.2 (0.1-1.1) | 0.063 |
| Ethnicity: Hispanic/Latina | 0.7 (0.2-2.1) | 0.520 | ||
| Education: completed high school or higher education (n=95) | 0.8 (0.3-2.0) | 0.598 | ||
| Location | ||||
| Washington, DC | 1 | Reference | 1 | Reference |
| Baltimore, MD | 1.0 (0.4-2.2) | 0.933 | 0.6 (0.2-2.5) | 0.487 |
| Duration on ART, in years | 1.0 (0.9-1.0) | 0.497 | ||
| Social Oppression | ||||
| Income below the U.S. federal poverty line, past 30 days | 1.0 (0.4-2.7) | 0.977 | ||
| Housing instability, past 12 months | 1.2 (0.6-2.8) | 0.617 | ||
| Currently unemployed | 1.5 (0.7-3.4) | 0.327 | ||
| 1 or more barriers to accessing healthcare | 4.1 (1.3-12.9) | 0.015 | 2.5 (0.6-11.4) | 0.228 |
| Physical violence, past 12 months | 1.5 (0.6-3.7) | 0.375 | ||
| Sexual violence, past 12 months | 1.2 (0.4-4.1) | 0.739 | ||
| Psychological violence, past 12 months | 2.2 (0.9-5.1) | 0.077 | 1.0 (0.3-3.5) | 0.972 |
| Psychological Distress | ||||
| Internalized transphobia | 1.1 (1.0-1.2) | 0.126 | ||
| Depression symptom criteria, past two weeks (n=95) | 1.3 (0.5-3.3) | 0.598 | ||
| PTSD symptom criteria, past 30 days | 1.5 (0.7-3.5) | 0.348 | ||
| Lifetime suicidal ideation | 2.4 (1.1-5.5) | 0.038 | 2.0 (0.6-6.2) | 0.253 |
| Identity Threat | ||||
| Not currently taking hormones for gender affirmation (n=94) | 6.0 (1.3-28.5) | 0.023 | 24.9 (3.3-118.9) | 0.002 |
| Unmet surgical need | 1.3 (1.1-1.5) | 0.017 | 1.6 (1.2-2.1) | 0.004 |
| No name and/or gender marker change on legal documents | 2.4 (0.9-6.4) | 0.089 | 1.5 (0.4-6.3) | 0.602 |
| High-Risk Contexts | ||||
| Drug use, past 12 months | ||||
| No drug use | 1 | Reference | 1 | Reference |
| Marijuana only | 3.8 (1.2-12.3) | 0.027 | 10.5 (2.1-53.7) | 0.005 |
| Any Illicit substance (with or excluding marijuana) | 2.2 (0.9-5.6) | 0.095 | 1.7 (0.5-5.7) | 0.338 |
| Alcohol use disorder, AUDIT-C | 1.0 (0.4-2.2) | 0.933 | ||
| Lifetime sex exchange | 1.3 (0.5-3.5) | 0.647 | ||
AOR: adjusted odds ratio; ART: antiretroviral therapy; AUDIT-C: Alcohol Use Disorder Identification Test of Consumption; OR: odds ratio; PTSD: Post-Traumatic Stress Disorder; 95% CI: 95% confidence interval.
Bolded values represent statistically significant (p<0.05) associations between the covariate and HIV treatment interruption.
Model adjusted for all covariates presented in the “Multivariable Model” column of the table.
Figure 3 depicts multivariable associations between covariates that correspond to the GAF domains and lifetime HIVTIs. This figure adapts the original GAF by using HIVTIs as the outcome and quantifying the magnitude of association between HIVTIs and covariates nested within each of the GAF conceptual domains. Factors situated in the more proximal domains (i.e., Identity Threat, High-Risk Contexts) to the framework’s outcome emerged as significant correlates of HIVTIs in multivariable analysis more frequently than did covariates positioned more distally from the outcome (i.e., Social Oppression, Psychological Distress).
Figure 3.
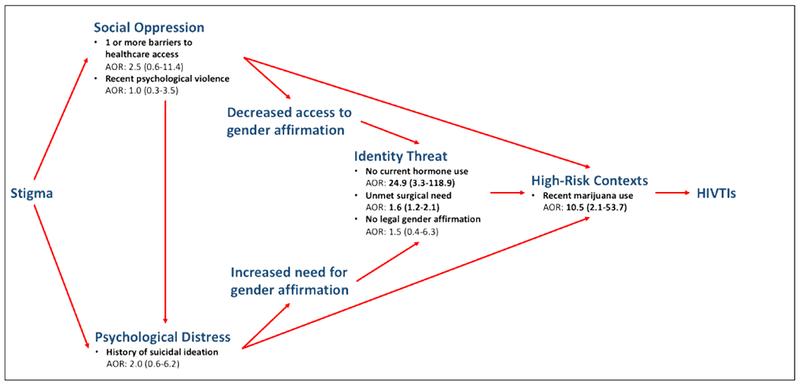
Modified Gender Affirmation Framework (GAF) with domain-specific covariates and their corresponding adjusted odds ratios (AOR) and 95% confidence intervals in relation to HIV treatment interruptions, adapted from Sevelius JM (2013). Sex roles, 68(11-12), 675-689.
Discussion
Findings from this analysis of 96 BLTW living with HIV who initiated ART highlight the concurrent, multilevel sources of adversity affecting engagement in HIV care and treatment in this population. Our study is one of the first to examine social and structural drivers of HIVTIs among BLTW living with HIV, an experience that can have important implications for treatment as prevention, which is an essential component of evidence-informed combination HIV prevention [46]. We found that barriers to gender affirmation, including lack of hormone use and surgical procedures, were significantly associated with treatment interruptions. Our assessment of these barriers was informed by the GAF, an important framework for examining HIV outcomes for BLTW. Our results suggest that in order to improve treatment disparities for BLTW, comprehensive, gender affirming care should be integrated into HIV services for BLTW.
While the majority of BLTW reported current hormone use and name/gender marker changes on identity documents, this access to medical and legal gender affirmation was tempered by existing unmet needs for gender affirming surgical interventions, including breast augmentation and vaginoplasty. Unmet surgical needs were accompanied by co-occurring barriers to health service access, including previous mistreatment in healthcare settings and transportation challenges. While the effect size of healthcare inaccessibility on HIVTIs was attenuated in multivariable analysis, the high frequency of self-reported barriers, and their independent associations with interrupted HIV treatment, demonstrate need for interventions to improve access to and quality of healthcare for BLTW. These interventions include improving provider competency in caring for transgender patients and subsidizing costs incurred during care-seeking (e.g., transportation costs) for financially unstable patients.
The observed association between HIVTIs and current hormone use among BLTW in this study offers supplemental evidence to the role of gender affirmation in the health and wellbeing of TW. Participants’ duration on ART and reported barriers to healthcare access, two such factors with a documented impact on HIV treatment outcomes, did not influence HIVTIs in bivariate and multivariable analysis, respectively, though inference is somewhat limited by the modest sample size.
Our findings contribute to a sparse, albeit growing, body of research exploring the relationship between hormone use and HIV-related outcomes in transgender populations. Braun et al. identified poor adherence to both ART and hormone therapy among TW concerned about harmful drug-drug interactions [47]. Reisner et al. additionally identified inverse associations between medical gender affirmation (hormone use and/or surgery) and maintaining HIV care appointments as well as viral suppression among 181 transgender youth aged 16–24 years (n=105 BLTW) [33]. In a study of HIV care continuum indicators, Sevelius and colleagues observed an association between sustained hormone therapy and ART adherence but not viral suppression [14]. Similar findings emerged in Bukowski et al.’s study of 422 Black TW in six U.S. cities, where current hormone use was negatively associated with viral suppression [3]. Concerns about drug-drug interactions between gender-affirming hormones and HIV medication pose additional barriers to ART initiation and adherence [47]. This study’s findings strengthen the available evidence that integrating HIV treatment with gender affirming care offers opportunities to address access, stigma, and other healthcare-related challenges unique to BLTW [16,48,49].
Previous research has identified associations between measures of resilience and HIV-related outcomes in transgender populations [14,17,34,50]. Resilience is conceptualized as the capacity to cope with stress and hardship (including avoidance of psychological challenges in response to hardship), and thus corresponds to the relationships between stigma and social oppression, in addition to psychological distress, within the GAF [51]. The role of medical gender affirmation in promoting resilience among BLTW is not well understood. A study of Black TW by Crosby et al. identified no significant associations between medical gender affirmation (6-item scored index) and resilience measures (personal competence and acceptance of self and life); however, social gender affirmation (5-item scored index, e.g., legal name change, currently in an intimate relationship) was significantly associated with resilience [52]. Conversely, a study by Glynn et al. with BLTW (N=573) documented a positively predictive relationship between social, psychological, and medical gender affirmation (hormone use and/or surgery) and improved mental health status (lower depression and higher self-esteem), which is often treated as an indicator of resilience [7]. Supported by our study findings, resilience-building activities among BLTW may present opportunities for reducing disparities along the continuum of HIV prevention, care, and treatment that employ a strengths-oriented approach, rather than deficit-based frameworks common within HIV research.
Drug use emerged as a significant correlate of HIVTIs among study participants. Drug use could function as a coping strategy for other stressors or as a source of adversity highlighted in the study (e.g., violence, internalized transphobia, housing instability), described elsewhere in the literature as mitigating factors of treatment adherence and engagement among TW [3,15,34]. However, due to the small sample size and the imprecision of the multivariable odds ratio (as demonstrated by the wide confidence interval), we cannot be certain of the effect. Drug use, for example, may have a mediating effect on distal indicators presented in the GAF, namely healthcare access barriers and suicidality, which were significantly associated with HIVTIs in our analysis. Future research with longitudinal data and a larger sample size could better assess the relationships between drug use, coping strategies, and HIVTIs for BLTW.
As demonstrated in Figure 3, variables nested in the domains most proximal to health outcomes in the GAF (i.e., identity threats, high-risk contexts) had a more statistically predictive effect on HIVTIs compared to covariates housed in more distal GAF domains (i.e., social oppression, psychological distress). Potential associations between indicators situated in the more distal GAF domains, specifically barriers to healthcare access and suicidal ideation, and HIVTIs may have been attenuated by the presence of other mediating factors not included in this analysis. Nonetheless, the proximity of covariates significant in multivariable analysis to health behaviors in the GAF may underscore the significant mediating influence of gender affirmation and high-risk contexts (i.e., substance use) on HIVTIs, offering theoretical extensions to the specific risk pathways originally presented in the GAF. Future studies with larger samples and longitudinal designs are needed to ascertain the effects of these distal indicators on HIVTIs.
Results from this study suggest the overlapping, multilevel sources of adversity experienced by BLTW, conceptualized in the GAF, may have consequences for the HIV care continuum. Our study’s focus on HIVTIs demonstrated that factors nested within all the GAF’s primary domains were significantly associated with HIVTIs for BLTW. Our analysis identifies opportunities for intervening in the proximal (i.e., medical gender affirmation) and distal factors associated with HIVTIs, particularly drivers of psychological distress (i.e., suicidality) and risk behaviors (i.e., substance use), and underscores a need to build and test interventions tailored for this population.
Limitations
There are several limitations to this study. First, the outcome of HIVTIs was reported over a participant’s lifetime and, thus, cannot be temporally situated in a participant’s gender trajectory. Nonetheless, the analysis provides a useful footing into, and demonstrates a need for, identifying temporal relationships between gender affirmation and HIV outcomes in this population. Second, the study’s recruitment of some participants from clinical settings may have resulted in an oversampling of BLTW with greater healthcare access or treatment-seeking behaviors, thereby potentially underestimating the HIVTI burden and unmet need for gender affirming services in this population. The cross-sectional design also precludes establishment of causal relationships between covariates and the outcome. Lastly, the overarching use of the GAF may have restricted our inclusion of other variables with potentially significant effects on HIVTIs. Our analysis, nonetheless, included and adjusted for potentially confounding factors of HIVTIs described in the literature.
Recognizing these limitations, this study makes a unique contribution to the literature on HIV and other health burdens in this underserved, highly impacted group. The theory-driven analysis, involving the purposive selection of variables using a prescribed theoretical model unique to BLTW, offers quantitative support for an existing conceptual framework derived from qualitative inquiry. Building from BLTW community needs and goals, these findings also importantly build evidence for the positive influence of gender affirmation (social, legal, and medical) on health service-seeking and sustained adherence to and engagement with HIV care.
Conclusions
This analysis provides support for the central role of gender affirmation in caring for transgender people, and highlights the coupled clinical and community value in integrating HIV care and access to gender affirming healthcare. Reducing barriers to gender affirming medical interventions, including hormone use and surgery, could cultivate a more stable environment for HIV care engagement and treatment adherence. A patient-centered care delivery model for BLTW should include a focus on gender affirmation goals.
Acknowledgements
We are grateful to Jean-Michel Brevelle, Falina Laron, Deborah Dunn, Ruby Corado, Alexa Rodriguez, Paty Hernandez, and Wendy Aly Escobar for their support with piloting the survey, study recruitment, and data dissemination. We are also thankful for the generous collaborative partnerships offered by the leadership and staff of Casa Ruby, Whitman Walker Health, and the DC Center. We would like to thank the people living with HIV who have generously shared their time, experiences, and bodies for the purposes of this research. Funding support was provided by the Johns Hopkins University Center for AIDS Research (P30AI094189) and the District of Columbia Center for AIDS Research (AI117970), NIH funded programs, supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, FIC, NIGMS, NIDDK, and OAR. This research was also supported in part by a National Institutes of Health/National Institute for Allergy and Infectious Diseases supplement to T. Poteat (P30AI094189-01A1). Support for this research also comes from the ADELANTE grant (AI050409) from the Centers for AIDS Research program at the National Institutes of Health to T. Yamanis. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding
This publication resulted from research supported by the Johns Hopkins University Center for AIDS Research (P30AI094189) and the District of Columbia Center for AIDS Research (AI117970), NIH funded programs, supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, FIC, NIGMS, NIDDK, and OAR. This research was also supported in part by a National Institutes of Health/National Institute for Allergy and Infectious Diseases supplement to T. Poteat (P30AI094189-01A1). Support for this research also comes from the ADELANTE grant (AI050409) from the Centers for AIDS Research program at the National Institutes of Health to T. Yamanis. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest: The authors declare they have no conflict of interest.
References
- 1.Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013. March;13(3):214–22. [DOI] [PubMed] [Google Scholar]
- 2.Poteat T, Ackerman B, Diouf D, Ceesay N, Mothopeng T, Odette K- Z, et al. HIV prevalence and behavioral and psychosocial factors among transgender women and cisgender men who have sex with men in 8 African countries: A cross-sectional analysis. PLoS Med. 2017. Nov;14(11):e1002422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bukowski LA, Chandler CJ, Creasy SL, Matthews DD, Friedman MR, Stall RD. Characterizing the HIV Care Continuum and Identifying Barriers and Facilitators to HIV Diagnosis and Viral Suppression Among Black Transgender Women in the United States. J Acquir Immune Defic Syndr 1999. 2018. December 1;79(4):413–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anand T, Nitpolprasert C, Kerr SJ, Muessig KE, Promthong S, Chomchey N, et al. A qualitative study of Thai HIV-positive young men who have sex with men and transgender women demonstrates the need for eHealth interventions to optimize the HIV care continuum. AIDS Care. 2017;29(7):870–5. [DOI] [PubMed] [Google Scholar]
- 5.Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, Mental Health, and Resilience in an Online Sample of the US Transgender Population. Am J Public Health. 2013. May;103(5):943–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chakrapani V, Newman PA, Shunmugam M, Dubrow R. Barriers to free antiretroviral treatment access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care. 2011. December;23(12):1687–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glynn TR, Gamarel KE, Kahler CW, Iwamoto M, Operario D, Nemoto T. The role of gender affirmation in psychological well-being among transgender women. Psychol Sex Orientat Gend Divers. 2016. Sep;3(3):336–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008. January;12(1):1–17. [DOI] [PubMed] [Google Scholar]
- 9.Kalichman SC, Hernandez D, Finneran S, Price D, Driver R. Transgender women and HIV-related health disparities: falling off the HIV treatment cascade. Sex Health. 2017. September 5; [DOI] [PubMed] [Google Scholar]
- 10.Logie CH, James L, Tharao W, Loutfy MR. “We don’t exist”: a qualitative study of marginalization experienced by HIV-positive lesbian, bisexual, queer and transgender women in Toronto, Canada. J Int AIDS Soc. 2012. September 7;15(2):17392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poteat T, Malik M, Scheim A, Elliott A. HIV Prevention Among Transgender Populations: Knowledge Gaps and Evidence for Action. Curr HIV/AIDS Rep. 2017. July 27; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Remien RH, Bauman LJ, Mantell JE, Tsoi B, Lopez-Rios J, Chhabra R, et al. Barriers and facilitators to engagement of vulnerable populations in HIV primary care in New York City. J Acquir Immune Defic Syndr 1999. 2015. May 1;69 Suppl 1:S16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salas-Espinoza KJ, Menchaca-Diaz R, Patterson TL, Urada LA, Smith D, Strathdee SA, et al. HIV Prevalence and Risk Behaviors in Male to Female (MTF) Transgender Persons in Tijuana, Mexico. AIDS Behav. 2017. October 14; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sevelius JM, Saberi P, Johnson MO. Correlates of antiretroviral adherence and viral load among transgender women living with HIV. AIDS Care. 2014;26(8):976–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dowshen N, Matone M, Luan X, Lee S, Belzer M, Fernandez MI, et al. Behavioral and Health Outcomes for HIV+ Young Transgender Women (YTW) Linked To and Engaged in Medical Care. LGBT Health. 2016. April;3(2):162–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dowshen N, Lee S, Franklin J, Castillo M, Barg F. Access to Medical and Mental Health Services Across the HIV Care Continuum Among Young Transgender Women: A Qualitative Study. Transgender Health. 2017;2(1):81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Machtinger EL, Haberer JE, Wilson TC, Weiss DS. Recent trauma is associated with antiretroviral failure and HIV transmission risk behavior among HIV-positive women and female-identified transgenders. AIDS Behav. 2012. November;16(8):2160–70. [DOI] [PubMed] [Google Scholar]
- 18.Mizuno Y, Beer L, Huang P, Frazier EL. Factors Associated with Antiretroviral Therapy Adherence Among Transgender Women Receiving HIV Medical Care in the United States. LGBT Health. 2017. Jun;4(3):181–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zeluf G, Dhejne C, Orre C, Mannheimer LN, Deogan C, Höijer J, et al. Targeted Victimization and Suicidality Among Trans People: A Web-Based Survey. LGBT Health. 2018. Apr;5(3):180–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Magno L, Dourado I, Silva LAV da, Brignol S, Amorim L, MacCarthy S. Gender-based discrimination and unprotected receptive anal intercourse among transgender women in Brazil: A mixed methods study. PloS One. 2018;13(4):e0194306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel VV, Masyukova M, Sutton D, Horvath KJ. Social Media Use and HIV-Related Risk Behaviors in Young Black and Latino Gay and Bi Men and Transgender Individuals in New York City: Implications for Online Interventions. J Urban Health Bull N Y Acad Med. 2016. April;93(2):388–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sevelius JM. Gender Affirmation: A Framework for Conceptualizing Risk Behavior among Transgender Women of Color. Sex Roles. 2013. June 1;68(11–12):675–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chow JY, Konda KA, Borquez A, Caballero P, Silva-Santisteban A, Klausner JD, et al. Peru’s HIV care continuum among men who have sex with men and transgender women: opportunities to optimize treatment and prevention. Int J STD AIDS. 2016. October;27(12):1039–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Melendez RM, Pinto RM. HIV prevention and primary care for transgender women in a community-based clinic. J Assoc Nurses AIDS Care JANAC. 2009. October;20(5):387–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med 1982. 2013. May;84:22–9. [DOI] [PubMed] [Google Scholar]
- 26.Prabawanti C, Dijkstra A, Riono P, Hartana G. A survey on HIV-related health-seeking behaviors among transgender individuals in Jakarta, based on the theory of planned behavior. BMC Public Health. 2015. November 16;15:1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reisner SL, Perez-Brumer AG, McLean SA, Lama JR, Silva-Santisteban A, Huerta L, et al. Perceived Barriers and Facilitators to Integrating HIV Prevention and Treatment with Cross-Sex Hormone Therapy for Transgender Women in Lima, Peru. AIDS Behav. 2017. April 18; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. Am J Public Health. 2009. April;99(4):713–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sevelius JM, Carrico A, Johnson MO. Antiretroviral therapy adherence among transgender women living with HIV. J Assoc Nurses AIDS Care JANAC. 2010. June;21(3):256–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sevelius JM, Patouhas E, Keatley JG, Johnson MO. Barriers and facilitators to engagement and retention in care among transgender women living with human immunodeficiency virus. Ann Behav Med Publ Soc Behav Med. 2014. February;47(1):5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the Prevalence of HIV and Sexual Behaviors Among the US Transgender Population: A Systematic Review and Meta-Analysis, 2006–2017. Am J Public Health. 2018. November 29;e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baguso GN, Gay CL, Lee KA. Medication adherence among transgender women living with HIV. AIDS Care. 2016. August;28(8):976–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reisner SL, Jadwin-Cakmak L, White Hughto JM, Martinez M, Salomon L, Harper GW. Characterizing the HIV Prevention and Care Continua in a Sample of Transgender Youth in the U.S. AIDS Behav. 2017. November 14; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jalil EM, Wilson EC, Luz PM, Velasque L, Moreira RI, Castro CV, et al. HIV testing and the care continuum among transgender women: population estimates from Rio de Janeiro, Brazil. J Int AIDS Soc. 2017. 19;20(1):21873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Santos G- M, Wilson EC, Rapues J, Macias O, Packer T, Raymond HF. HIV treatment cascade among transgender women in a San Francisco respondent driven sampling study. Sex Transm Infect. 2014. August;90(5):430–3. [DOI] [PubMed] [Google Scholar]
- 36.Reisner SL, Biello K, Rosenberger JG, Austin SB, Haneuse S, Perez-Brumer A, et al. Using a Two-Step Method to Measure Transgender Identity in Latin America/the Caribbean, Portugal, and Spain. Arch Sex Behav. 2014. November;43(8):1503–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yamanis T, Malik M, Del Río-González AM, Wirtz AL, Cooney E, Lujan M, et al. Legal Immigration Status is Associated with Depressive Symptoms among Latina Transgender Women in Washington, DC. Int J Environ Res Public Health. 2018. 12;15(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Federal Poverty Level (FPL) - HealthCare.gov Glossary [Internet]. HealthCare.gov. [cited 2018 Dec 13]. Available from: https://www.healthcare.gov/glossary/federal-poverty-level-fpl/
- 39.STRAUS MA, HAMBY SL, BONEY-McCOY S, SUGARMAN DB. The Revised Conflict Tactics Scales (CTS2): Development and Preliminary Psychometric Data. J Fam Issues. 1996. May 1;17(3):283–316. [Google Scholar]
- 40.Testa RJ, Habarth J, Peta J, Balsam K, Bockting W. Development of the Gender Minority Stress and Resilience Measure. Psychol Sex Orientat Gend Divers. 2015;2(1):65–77. [Google Scholar]
- 41.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003. November;41(11):1284–92. [DOI] [PubMed] [Google Scholar]
- 42.Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, et al. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Prim Care Psychiatry. 2003;9(1):9–14. [Google Scholar]
- 43.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998. September 14;158(16):1789–95. [DOI] [PubMed] [Google Scholar]
- 44.Akaike H Information Theory and an Extension of the Maximum Likelihood Principle In: Parzen E, Tanabe K, Kitagawa G, editors. Selected Papers of Hirotugu Akaike [Internet]. New York, NY: Springer New York; 1998; [cited 2018 Aug 28]. p. 199–213. (Springer Series in Statistics). Available from: 10.1007/978-1-4612-1694-0_15 [DOI] [Google Scholar]
- 45.Jr DWH, Lemeshow S, Sturdivant RX. Applied Logistic Regression. John Wiley & Sons; 2013. 528 p. [Google Scholar]
- 46.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011. August 11;365(6):493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Braun HM, Candelario J, Hanlon CL, Segura ER, Clark JL, Currier JS, et al. Transgender Women Living with HIV Frequently Take Antiretroviral Therapy and/or Feminizing Hormone Therapy Differently Than Prescribed Due to Drug-Drug Interaction Concerns. LGBT Health. 2017. October;4(5):371–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Munro L, Marshall Z, Bauer G, Hammond R, Nault C, Travers R. (Dis)integrated Care: Barriers to Health Care Utilization for Trans Women Living With HIV. J Assoc Nurses AIDS Care. 2017. September 1;28(5):708–22. [DOI] [PubMed] [Google Scholar]
- 49.Reisner SL, Bradford J, Hopwood R, Gonzalez A, Makadon H, Todisco D, et al. Comprehensive Transgender Healthcare: The Gender Affirming Clinical and Public Health Model of Fenway Health. J Urban Health. 2015. June 1;92(3):584–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crosby RA, Salazar LF, Hill BJ. Correlates of Not Using Antiretroviral Therapy Among Transwomen Living with HIV: The Unique Role of Personal Competence. Transgender Health. 2018;3(1):141–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grossman AH, D’augelli AR, Frank JA. Aspects of Psychological Resilience among Transgender Youth. J LGBT Youth. 2011. March 29;8(2):103–15. [Google Scholar]
- 52.Crosby RA, Salazar LF, Hill BJ. Gender Affirmation and Resiliency Among Black Transgender Women With and Without HIV Infection. Transgender Health. 2016;1(1):86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]


