Abstract
Background:
Bipolar Disorder (BD) is a recurrent illness associated with high morbidity and mortality. The frequency of mood episode recurrence in BD is highly heterogeneous and significantly impacts the person’s psychosocial functioning and well-being. understanding the factors associated with mood recurrences could inform the prognosis and treatment. The objective of this review is to summarize the literature on factors, present during childhood, that influence recurrence.
Methodology:
A systematic review of PubMed (1946–2017) and PsycINFO (1884–2017) databases was conducted to identify candidate studies. Search terms included bipolar disorder, episodes, predictors, recurrences, and course. Study characteristics, risk for bias, and factors associated with recurrence were coded by two raters according to predetermined criteria.
Results:
Twenty child studies and 28 adult studies that retrospectively evaluated childhood variables associated with mood recurrences were included. Early age of onset, low socioeconomic status, comorbid disorders, inter-episode subsyndromal mood symptoms, BD-I/II subtypes, presence of stressors, and family history of BD were associated with higher number of recurrences.
Limitations:
Risk factors and mood recurrences were assessed and defined in different ways, limiting generalizability.
Conclusion:
Multiple factors are associated with increased risk of mood episode recurrence in BD. Interventions targeting modifiable factors could reduce the impact of BD. For example, treatment of comorbid disorders and subsyndromal mood symptoms, coupled with appropriate cognitive behavioral and family-focused therapies could ameliorate risk related to many clinical factors. When coupled with social services to address environmental factors, the number of episodes could be reduced and the course of BD significantly improved.
Keywords: bipolar disorder, recurrence, risk factors, review
BACKGROUND
Bipolar Disorder (BD), an illness characterized by recurrent mood episodes, significantly affects psychosocial functioning and increases the risk for other psychiatric disorders (e.g., substance abuse) and suicidality (1). The course of BD, and frequency of mood episode recurrence, is highly variable, therefore the study of the factors associated with the risk for recurrence could aid in better prognostication and inform treatment (2, 3). The identification of factors, particularly those amenable for modification, could provide an opportunity to avoid or attenuate them if their impact on the course of the disorder is negative or, conversely, could lead to efforts to promote those factors that are associated with a positive outcome. Relatedly, the recognition of factors that increase the risk for recurrences, might inform a more aggressive treatment approach.
The aim of this article is to review the extant literature regarding factors associated with mood recurrences in BD. To do this, we selected longitudinal and cross-sectional studies of BD that evaluated the influence of factors that were present in childhood, on the frequency of mood episode recurrence. We chose to focus on factors present during childhood because the presence of risk or protective factors early in the illness has substantial influence on the course of BD across the lifespan (4); consequently, identifying and targeting these factors could have a greater impact on illness trajectory than factors present only in adulthood. There are undoubtedly factors that influence mood episode recurrence later in life (e.g., substance use, stressful or traumatic events), but as the effects of the illness accumulate, it becomes harder to distinguish independent risk from those factors that share a bidirectional relation with mood symptoms. Our goal is to better understand childhood factors that influence mood recurrence in order to inform strategies to promote mood stability. To our knowledge, this is the first systematic review of the influence of multiple childhood factors on mood episode recurrence in BD.
METHODOLOGY
The systematic review was carried out following the recommendations of PRISMA guide (Preferred Reporting Items for Systematic reviews and Meta-Analyses). The present review protocol was recorded in PROSPERO (CRD42018086583) (5).
Eligibility criteria for studies
Studies of both youth and adults with BD were eligible. Studies carried out in adults had to include data about factors that were present during childhood. Additionally, all included studies had to report on the association between the childhood factors and the onset of recurrent mood episodes. Studies that had a dimensional outcome (e.g., manic symptoms) were excluded because the presence of some symptoms does not necessarily constitute an episode and we were specifically interested in the relation between childhood factors and mood episode recurrence. Studies that reported only on treatment as the factor related to recurrence were also excluded, as there is a large literature on the effectiveness of different treatments in preventing recurrence, which falls outside the scope of the present paper. Finally, we evaluated the impact of sex in child studies only; following puberty, the inclusion of sex carries with it multiple additional factors that might affect recurrence such as hormonal cycles, pregnancy, puerperium (also possible in adolescents), and menopause. Although important, these factors are beyond the scope of this child-focused review.
Study selection
The bibliographic search was conducted through PubMed (1946–2017) and PsycINFO (1884–2017) databases from September to November 2017 combining the following keywords: bipolar disorder AND episodes, bipolar disorder AND predictors, bipolar disorder AND recurrences, bipolar disorder AND course.
The search yielded 25,695 potential articles, 28 articles were added using other resources (bibliographic references of the selected articles and specialized books on the subject). The eligibility determination of the articles, data coding and quality assessment were carried out independently by two of the authors (X.E.P. & E.C.R.). A third author (S.B.V.) was consulted when agreement between both raters could not be reached. The initial screening was done by reading the title and summary of each article. Once the initial screening, based on the eligibility criteria described below, and elimination of duplications were made, 156 articles were selected (81 pediatric and 73 adult samples). Of these, 154 full text articles were obtained, the other two were not publicly available and requests to the authors were not answered (Figure 1). Cohen’s kappa coefficient was good for the article selection process (K = 0.74).
Figure 1.
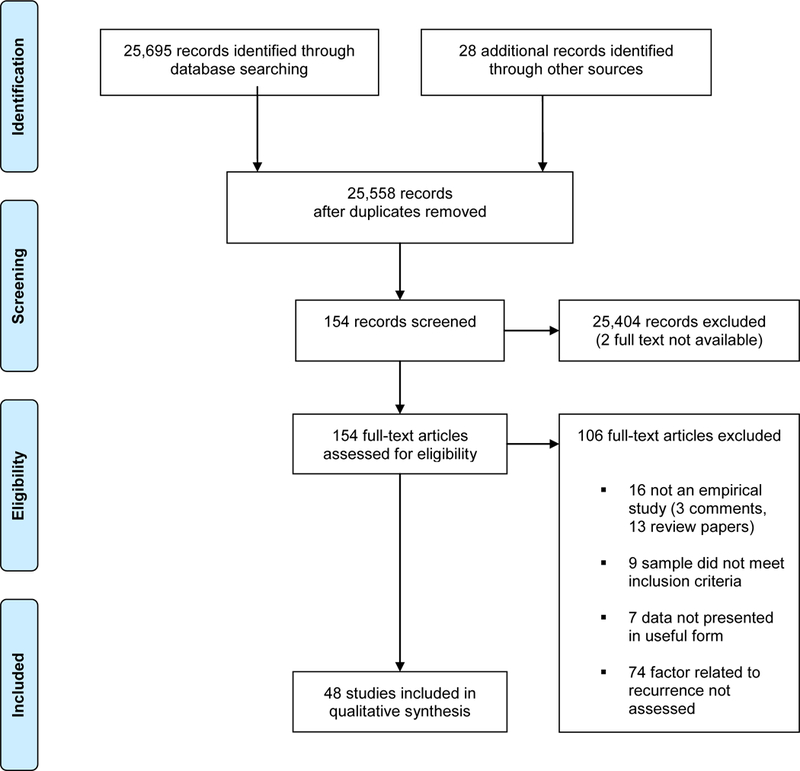
Study selection
Data coding
The following information was extracted from each article: (1) author, year, and country; (2) financing; (3) type of study (longitudinal or cross-sectional, although information about factors in adult studies was always retrospective); (4) follow-up (duration, number of interviews and interview frequency); (5) the study’s inclusion/exclusion criteria; (6) whether follow-up assessments were blind to baseline diagnosis; (7) characteristics of the comparison group(s) (if included); (8) sample demographic characteristics (recruitment, total sample, age at onset, average age, socio-economical status (SES), percentage of females (child studies only), and race; (9) sample clinical characteristics (number of participants diagnosed with BD, BD I %, illness duration, type of course (e.g., predominant polarity, rapid cycling), polarity of the first episode, number of manic, hypomanic, mixed, depressive and total episodes, subsyndromal mood symptoms, comorbid disorders, suicide attempts, and psychotic symptoms); (10) environmental characteristics (living with both natural parents and stressors); (11) family history of BD; (12) assessment tools (e.g., how were diagnosis, mood recurrence, and factors measured); (13) outcome or recurrence (definition of recurrence, polarity of episode); and (14) whether the type of factor influence increases risk, decreases risk, or was not described.
Risk of bias was assessed using the Newcastle-Ottawa Quality Assessment Scale (NOQAS) (Supplement 1). The NOQAS is recommended by the Cochrane Collaboration to assess risk of bias for case control and cohort studies (6, 7). The NOQAS assesses eight criteria with a maximum score of nine. Scores below five points represent high risk of bias (8).
Each article was coded by two authors (X.E.P. & E.C.P.). Cohen’s kappa coefficients were good for coding factors of influence (K = 0.87) and mood recurrence (K = 0.90). Cohen’s kappa coefficient was moderate (K = 0.58) for the risk of bias assessment between the two review authors (X.E.P. & E.C.P.). Disagreements were resolved by discussion between the two review authors and by contacting the authors of the original studies, as necessary. When the study author could not be reached for clarification (one third of those contacted responded), a third author (S.B.V) was consulted.
Studies varied widely in the way they assessed and defined risk factors and recurrences (Table 1 and Table 2). Studies that clearly defined the outcome as “new episode” or “recurrence” were preferable. However, the specific nature of the recurrence was often ill-defined (e.g., the polarity of episode or whether the episode was a relapse or a recurrence were not stated and the distinction between first episodes versus recurrent episodes was not clear); consequently, we included all studies that evaluated the association between childhood factors and risk for a future mood episode, but the lack of consistency in how both the risk factors and outcomes were described is a limitation.
Table 1:
Child studies
| Author | Original Sample | Diagnostic criteria / Semi-structured Interview used | Recurrence definition | Recurrence assessment | Factor assessed | Risk or Protective factor | Factor assessment | Prospective or cross-sectional | Case control or cohort |
|---|---|---|---|---|---|---|---|---|---|
| Yen et al., 2016 | COBY | DSM-IV / KSADS-PL | Depressive or manic episode, was defined as having followed a period of recovery, and as having again met full diagnostic criteria (PSR score of 5 or 6) for a minimum duration of 1 week for mania and 2 weeks for depression. | A-LIFE; PSR | Comorbidity (Anxiety, ADHD, Disruptive Behavior Disorders, Substance Abuse) | Risk | KSADS-PL | Prospective | Case-control |
| Hirneth et al., 2015 (91) | The Bipolar Program | DSM-IV-TR / WASH-U-KSADS | Episodes were defined as a period of active symptoms ( ≥ 4 or ‘moderate’ on WASH-U-KSADS items; ≥ 3 or ‘mild’ for hypomania) demarcated at each end by a period of nil or minimal mood and behavioral symptoms consistent with the person’s baseline level of functioning; that is, ratings of 1 (nil) or 2 (slight) on WASH-U-KSADS. items. |
WASH-U-KSADS | Bipolar subtype I (vs. II and NOS) | Risk | WASH-U-KSADS | Cross-sectional | Cohort |
| Birmaher et al., 2014 | Age at onset (higher) | Protective | KSADS-PL | ||||||
| Lifetime family history of bipolar and substance use disorders (less) | Protective | FHS | |||||||
| History at baseline of severe depression or manic or hypomanic symptoms (less) | Protective | KSADS-PL | |||||||
| KSADS M | |||||||||
| COBY | DSM-IV / KSADS-PL | A recurrence (new episode) required a PSR ≥5, with duration of 1-week for mania/hypomania and 2-weeks for depression. | A-LIFE; PSR | KSADS D | Prospective | Case-control | |||
| Protective | KSADS-PL | ||||||||
| Subsyndromal episodes (fewer) | KSADS M | ||||||||
| KSADS D | |||||||||
| Sexual abuse (less) | Protective | CBQ | |||||||
| FACES-II | |||||||||
| Socioeconomic status (higher) | Protective | HS | |||||||
| Sala et al., 2014 | COBY | DSM-IV / KSADS-PL | A recurrence (new episode) required a PSR ≥5, with duration of 1-week for mania/hypomania and 2-weeks for depression. | A-LIFE; PSR | Comorbidity (anxiety) | Risk | KSADS-PL | Prospective | Cohort |
| Wozniak et al., 2013 | Massachusetts | DSM-IV / KSADS-E | To gauge a distinct episode, our interviewers asked for ‘a distinct period (of at least 1 week) of extreme and persistently elevated, expansive or irritable mood’ and further required that the irritability endorsed in this module is ‘super’ and ‘extreme.’ | KSADS-E | Sex (male) | Risk | KSADS-E | Cross-sectional | Cohort |
| Sala et al., 2012 | COBY | DSM-IV / KSADS-PL | A recurrence (new episode) required a PSR ≥5, with duration of 1-week for mania/hypomania and 2-weeks for depression. | A-LIFE; PSR | Comorbidity (anxiety) | Risk | KSADS-PL | Prospective | Cohort |
| Hua et al., 2011 | Massachusetts | DSM-IV/ KSADS-E | Lifetime BPD episodes were classified as the number of distinct and separate BPD episodes that met either full or subthreshold DSM-IV criteria for Mania. | KSADS-E | Comorbidity (psychosis) | Risk | KSADS-E | Cross-sectional | Cohort |
| Ratheesh et al., 2011 | NIMHANS | DSM-IV / KSADS-PL | Not defined | KSADS-PL | Comorbidity (anxiety) | Risk | KSADS-PL | Cross-sectional | Cohort |
| Wozniak et al., 2011 | Massachusetts | DSM-IV / KSADS-E | To gauge a distinct episode our interviewers asked for a distinct period (of at least one week) of extreme and persistently elevated, expansive or irritable mood and further required that the irritability endorsed in this module was ‘super’ and ‘extreme.’ To meet for a subthreshold diagnosis of mania, a child must have met criterion A for a period of four days or longer, and/or have at least two (three if the mood is irritable only) of the seven criterion B symptoms, and associated impairment. | KSADS-E; SCID |
Symptomatic group (vs. subsyndromal) |
Risk | KSADS-E/ SCID | Prospective | Cohort |
| Birmaher et al., 2009 | COBY | DSM-IV / KSADS-PL | A recurrence (new episode) required a PSR ≥ 5, with duration of 1-week for mania/hypomania and 2-weeks for depression. | A-LIFE; PSR | Bipolar subtype I and II (vs. NOS) | Risk | KSADS-PL | Prospective | Cohort |
| Geller et al., 2008 | PCPBD | DSM-IV / WASH-U- KSADS | Relapse after recovery was defined as 2 consecutive weeks of meeting DSM-IV criteria for mania with a CGAS score of 60 or lower, indicating significant clinical impairment. | WASH-U-KSADS | Maternal warmth (low) | Risk | PSSAC-R | Prospective | Cohort |
| DelBello et al., 2007 | DSM-IV / WASH-U- KSADS | Syndromic recurrence was defined by 1 week (2 weeks for depression) with a LIFE overall score of ≥5 anytime after syndromic recovery. Time to each type of recovery included the 8 consecutive weeks that the patient met criteria for that type of recovery. | YMRS; HAM-D; SAPS | Risk | WASH-U-KSADS | Prospective | Cohort | ||
| CCHMC | Comorbidity (alcohol use disorder) | ||||||||
| Birmaher et al., 2006 | A recurrence (new episode) required a PSR score of 5 or more, with durations of 1 week for mania/hypomania and 2 weeks for depression. | Bipolar subtype I | Risk | KSADS-PL | Prospective | Cohort | |||
| (vs. II and NOS) | |||||||||
| COBY | DSM-IV / KSADS-PL | A-LIFE; PSR | Socioeconomic status (lower) | Risk | HS | ||||
| Comorbidity (psychosis) | Risk | KSADS-PL | |||||||
| Sex (female) | Risk | KSADS-PL | |||||||
| Wals et al., 2005 | Netherlands offspring | DSM-IV / KSADS-PL | Not defined | KSADS-PL | Stressful life events | Risk Not Found | LEDS | Prospective | Cohort |
| Jairam et al., 2004 | NIMHANS | DSM-III-R / DICA-R | Relapse is defined as a new affective episode satisfying DSM-IV criteria for the disorder occurring after the period of recovery or without any intervening period of recovery if there was a clear change in polarity along with a clinically significant impairment with the CGAS score < 60. | MAGIC |
Depressive episodes CGAS follow-up (lower) |
Risk Risk |
DICA-R CGAS |
Prospective | Case-control |
| YMRS | Prior episodes | Risk Not Found | DICA-R | ||||||
| GAS | First episode polarity | Risk Not Found | DICA-R | ||||||
| Sex | Risk Not Found | DICA-R | |||||||
| Age at onset | Risk Not Found | DICA-R | |||||||
| Comorbidity (psychosis included) | Risk Not Found | DICA-R | |||||||
| Subsyndromal symptoms | Risk Not Found | DICA-R | |||||||
| Lifetime family history of affective illness | Risk Not Found | DICA-R | |||||||
| Lewinsohn et al., 2000 (92) | Western Oregon | DSM-IIIR / KSADS | Not defined | LIFE | Syndromal group | Risk | KSADS | Prospective | Cohort |
| (vs. Bipolar subtype NOS) | |||||||||
| Srinath et al., 1998 | NIMHANS | DSM-IIIR / ISCA | Relapse was defined as a new episode of illness satisfying DSM-IIIR criteria for the disorder. | FISA | Age at onset | Risk Not Found | ISCA; ISAAC | Prospective | Cohort |
| ISCA | Sex | Risk Not Found | ISCA; ISAAC | ||||||
| Other resources | Prior episodes | Risk Not Found | ISCA; ISAAC | ||||||
| First episode polarity | Risk Not Found | ISCA; ISAAC | |||||||
| Comorbidity (psychosis) | Risk Not Found | ISCA; ISAAC | |||||||
| Lifetime family history of affective and psychotic illness | Risk Not Found | FH-RDC | |||||||
| Kovacs et al., 1995 | University of Pittsburgh | DSM-III / ISCA | If the subject recovered from an episode, but upon follow-up was found to have become symptomatic again in 2 months or less of the tentative “offset” date, he or she was designated as still in the previous episode of the illness. | ISCA | Comorbidity (conduct disorder) | Risk Not Found | ISCA | Prospective | Cohort |
| Strober et al., 1995 | UCLA | DSM-III / KSADS | Relapse was defined as a new episode of illness satisfying RDC for mania or major depression. | Sex | Risk Not Found | KSADS | Prospective | Cohort | |
| Comorbidity (psychosis) | Risk Not Found | KSADS | |||||||
| LIFE | Lifetime family history of bipolar illness | Risk Not Found | KSADS | ||||||
| Prior episodes | Risk Not Found | KSADS | |||||||
| Polarity episode intake | Risk Not Found | KSADS | |||||||
| Bashir et al., 1987 | Rivendell | DSM-III / no interview | Not defined | Check-Lists | Age at onset | Risk Not Found | Clinical interview | Prospective | Cohort |
NOQAS: Newcastle-Ottawa Quality Assessment Scale; COBY: Course and Outcome of Bipolar Youth; DSM: Diagnostic and Statistical Manual of Mental Disorders; KSADS-PL: Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime version; PSR: Psychiatric Status Rating; A-LIFE: Adolescent-Longitudinal Interval Follow-up Evaluation; ADHD: attention deficit hyperactivity disorder; WASH-U-KSADS: Washington University at St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia version; Bipolar subtype NOS: Bipolar subtype no otherwise specified; FHS: Family History Screen; KSADS M: Kiddie Mania Rating Scale; KSADS D: Kiddie Depression Rating Scale; CBQ: Conflict Behavior Questionnaire; FACES-II: Family Adaptation and Cohesion Scale-II; HS: Hollingshead 4-Factor Scale; KSADS-E: Kiddie Schedule for Affective Disorders and Schizophrenia Epidemiological version; BPD: Bipolar Disorder; NIMHANS: National Institute of Mental Health and Neurosciences; SCID: Structured Clinical Interview for DSM; PCPBD: Phenomenology and Course of Pediatric Bipolar Disorders; CGAS: Children’s Global Assessment Scale; PSSAC-R: Psychosocial Schedule for School-Age Children-Revised; CCHMC: Cincinnati Children’s Hospital Medical Center; YMRS: Young Maria Rating Scale; HAM-D: Hamilton Depression rating Scale; SAPS: Scale for the Assessment of Positive Symptoms; LEDS: The Bedfort College Life Event and Difficulties Schedule; DICA-R: Diagnostic Interview for Children and Adolescents-Revised; MAGIC: Missouri Assessment for Genetic Interview in Children; GAS: Global Assessment Scale; LIFE: Longitudinal Interval Follow-up Evaluation; ISCA: Interview Schedule for Children and Adolescents; FISA: Follow-up Interview Schedule for Young Adults; ISAAC: Intake Sheet for Adolescents: Cross-Cultural Study; FH-RDC: Family History-Research Diagnostic Criteria; UCLA: University of California, Los Angeles; RDC: Research Diagnostic Criteria.
Table 2:
Adult studies
| Author | Original Sample | Diagnostic criteria / Semi-structured Interview used | Recurrence definition | Recurrence assessment | Factor assessed | Risk or Protective factor | Factor assessment | Prospective or cross-sectional | Case control or cohort |
|---|---|---|---|---|---|---|---|---|---|
| Serra et al., 2017 |
Lucio Bini Mood Disorder Center |
DSM-IV TR/ SCID-I | Not defined |
Semi-structured Interview (no more data) |
Anxiety disorders |
Risk |
Semi-structured Interview (no more data) |
Prospective | Cohort |
|
Gilman et al., 2015 |
NESARC |
DSM-IV/ NESARC |
Not defined |
NESARC | Child abuse | Risk | Check-List |
Prospective |
Cohort |
| Karthick et al., 2015 |
Tertiary-care Hospital | DSM-IV TR/ SCID-I | Not defined | NIMH-LCM | Age at onset | Risk Not Found | SCID-I | Cross-sectional | Cohort |
| YMRS | |||||||||
| HDRS | |||||||||
| Erten et al., 2014 |
Bakirkoy Hospital | DSM-IV/ No data | Not defined | YMRS | Child abuse | Risk | CANQ |
Cross-sectional |
Cohort |
| HDRS | |||||||||
| Li et al., 2014 |
Beijing Anding Hospital |
DSM-IV/ SCID |
Not defined |
SCID | Child abuse | Risk Not Found | CTQ-SF |
Cross-sectional |
Cohort |
| CECA.Q | |||||||||
| Post et al., 2014a |
Stanley Foundation Bipolar Network | Not defined/ Not defined | Not defined | Self-reports | Child abuse | Risk | Cross-sectional | Case-control | |
| Poor social support | Risk | Self-reports | |||||||
| Employment difficulties | Risk | ||||||||
| Comorbidity | Risk | SCID | |||||||
| (anxiety and substance abuse) | |||||||||
| Post et al., 2014b (93) |
Stanley Foundation Bipolar Network | Not defined/ SCID | Not defined | NIMH-LCM | Living USA | Risk | SCID | Prospective | Cohort |
| YMRS | |||||||||
| IDS | |||||||||
|
Coryell et al., 2013 |
CDS | RDC/ SADS | Any week with a PSR of ‘3’ or more for major, intermittent or schizoaffective depressive disorder indicated the current presence of a depressive episode. Likewise, a manic episode was considered present for all weeks with a PSR of ‘3’ or more for hypomania, mania, or schizoaffective mania. | LIFE-II | Age at onset | Risk | SADS | Prospective | Cohort |
| SLICE | |||||||||
| PSR | |||||||||
| Comorbidity (anxiety) | Risk | ||||||||
| Etain et al., 2013 |
France and TOP Study | DSM-IV/ DIGS & SCID-I | Not defined | DIGS/ SCID-I | Emotional abuse | Risk | CTQ | Cross-sectional | Cohort |
| Larsson et al., 2013 |
TOP Study | DSM-IV/ SCID-I | Not defined | SCID-I | Emotional abuse | Risk | CTQ-short version | Cross-sectional | Cohort |
| Baldessarini et al., 2012 | International Consortium for Bipolar Research | DSM-IV/ SCID-P |
Not defined | SCID-P | Age at onset | Risk | SCID-P | Prospective | Cohort |
| BPRS | |||||||||
| YMRS | |||||||||
| HDRS | |||||||||
| Post et al., 2010 (94) |
Stanley Foundation Bipolar Network | DSM-IV/ SCID | Not defined | NIMH-LCM | Age at onset | Risk | SCID | Prospective | Cohort |
| Perlis et al., 2009 |
STEP-BD | DSM-IV/ ADE & MINI | Recurrence was defined as meeting full DSM-IV criteria for a manic, hypomanic, mixed, or depressive episode on any one follow-up visit. | CMF | Age at onset | Risk | ADE | Prospective | Cohort |
| MADRS | MINI | ||||||||
| YMRS | |||||||||
| Ryden et al., 2009 |
Tertiary-care Hospital | DSM-IV/ ADE & MINI | Not defined | ADE | Comorbidity (ADHD) | Risk | WURS-25/ | Cross-sectional | Cohort |
| MINI | A-TAC | ||||||||
| NIMH-LCM | |||||||||
| Yatham et al., 2009 |
STOP-EM | DSM-IV TR/ MINI | Relapse and recurrence, defined as mood symptoms occurring within 8 weeks of syndromal recovery and occurring after remission, respectively. Recurrence was considered if manic or depressive symptoms fulfilled DSM-IV-TR for a mood episode. | BPRS | Age at onset | Risk | MINI | Prospective | Cohort |
| YMRS | |||||||||
| HDRS | |||||||||
| MADRS | |||||||||
|
McIntyre et al., 2008 |
MDPU | DSM-IV-TR/ Not used | Not defined | Chart Review | Child abuse | Risk Not Found | Chart Review | Cross-sectional | Cohort |
| Tamam et al., 2008 |
Cukurova University Medical School Hospital | DSM-IV TR/ SCID-I | Not defined | SCID-I | Comorbidity (ADHD) | Risk | KSADS-PL | Cross-sectional | Cohort |
| WURS-25 | |||||||||
| Leverich et al., 2007 |
Stanley Foundation Bipolar Network | DSM-IV/ SCID | Not defined | NIMH-LCM | Age at onset | Risk | SCID | Prospective | Cohort |
| Bromet et al., 2005 |
Suffolk County Mental Health Project | DSM-IIIR/ SCID | The date of the first relapse was defined as the start of a new episode meeting DSM-IV symptom and duration criteria. | SCID | Age at onset | Risk | SCID | Prospective | Cohort |
| Child abuse | Risk | Not defined | |||||||
| Comorbidity (anxiety) | Risk | SCID | |||||||
| Garno et al., 2005 |
New York Presbyterian Hospital | DSM-IV/ SCID-IV | Not defined | SCID-IV | Child abuse | Risk | CTQ |
Cross-sectional |
Cohort |
| Nolen et al., 2004 |
Stanley Foundation Bipolar Network | DSM-IV/ SCID | Not defined | NIMH-LCM | Child abuse | Risk | Not defined | Prospective | Cohort |
| Perlis et al., 2004 (95) |
STEP-BD | DSM-IV & ICD-10/ | Not defined | ADE | Age at onset | Risk | ADE | Cross-sectional | Cohort |
| ADE & MINI | MINI | MINI | |||||||
| Suppes et al., 2001 |
Stanley Foundation Bipolar Network | DSM-IV/ SCID-P | Not defined | SCID-P | Age at onset | Risk | SCID-P | Cross-sectional | Cohort |
| Carlson et al., 2000 |
Suffolk County Mental Health Project | DSM-IIIR/ SCID | Not defined | SCID | Age at onset | Risk | SCID | Prospective | Cohort |
| BPRS | |||||||||
| HDRS | |||||||||
| mania scale | |||||||||
| Schurhoff et al., 2000 |
Pitie-Salpetriere and Robert Depre Hospitals | DSM-IV & RDC/ DIGS | Not defined | DIGS | Age at onset | Risk Not Found | DIGS | Cross-sectional | Cohort |
| Lish et al., 1994 |
DMDA | Not defined/ Not used | Not defined | Self-report | Age at onset | Risk | Self-report | Cross-sectional | Cohort |
| Winokur et al., 1989 (96) |
University of Iowa Psychiatric Hospital | Not defined/ Not used | Not defined | Chart Review | Age at onset | Risk Not Found | Clinical Interview | Prospective | Case-control |
| Carlson et al., 1977 |
NIMH Affective Disorder Study | Not defined/ Not used | Not defined | Clinical Interview | Age at onset | Risk Not Found | Clinical Interview | Cross-sectional | Cohort |
NOQAS: Newcastle-Ottawa Quality Assessment Scale; DSM: Diagnostic and Statistical Manual of Mental Disorders; KSADS-PL: Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime version; LIFE-II: Longitudinal Interval Follow-up Evaluation; ADHD: attention deficit hyperactivity disorder; SADS: Schedule for Affective Disorders and Schizophrenia version; SCID: Structured Clinical Interview for DSM; YMRS: Young Maria Rating Scale; RDC: Research Diagnostic Criteria; NESARC: National Epidemiologic Survey on Alcohol and Related Conditions; CDS: National Institute of Mental Health Collaborative Depression Study; TOP Study: Thematically Organized Psychosis [TOP] Study; STEP-BD: Systematic Treatment Enhancement Program for Bipolar Disorder; STOP-EM: Systematic Treatment Optimization Program for Early Mania; MDPU: Mood Disorders Psychopharmacology Unit; DMDA: National Depres- sive and Manic-Depressive Association; CTQ: Childhood Trauma Questionnaire; WURS-25: Wender Utah rating scale; A-TAC: Autism-Tics, ADHD, and other comorbidities; CECA.Q: Collaborative Pro- gram on the Psychobiology of Depression and the NIMH Epidemiologic Catchment Area Questionnaires; CANQ: Abuse and Neglect Questionnaire; SCID: Structured Clinical Interview for DSM; DIGS: Diagnostic Interview for Genetic Studies; ADE: Affective Disorders Evaluation; MINI: Mini International Neuropsychiatric Interview; ICD-10: International Statistical Classification of Diseases and Related Health Problems; NIMH-LCM: National Institute Mental Health-life chart method; HDRS: Hamilton Depression Rating Scale; IDS: inventory for depressive symptoms; SLICE: Streamlined Longitudinal Interval Continuation Evaluation; PSR: Psychiatric Symptom Ratings; BPRS: Brief Psychiatric Rating Scale; CMF: Clinical Monitoring Form; MADRS: Montgomery-Asberg Depression Rating Scale.
Prospective studies with a case control design, comparing people with BD who were exposed to a specific factor to those who were not, provide the most valuable information about how factors influence recurrence. However, due to the small number of prospective case control studies available, cross-sectional and cohort studies were also included.
Articles written in English, French, Italian, Portuguese or Spanish were included. Review articles were read in order to ensure that the studies they reported on were included; but were not considered as part of the data synthesis.
To explore variability in study results (heterogeneity) we specified the following hypotheses before conducting the analysis: we expected that factors that are associated with a more severe presentation of BD would also be associated with a greater number of mood recurrences (9, 10, 11, 12, 13, 14), including earlier age at onset, lower SES, BD I and II subtypes, type of course (rapid cycling), suicide attempts, psychotic symptoms, subsyndromal mood symptoms, comorbid disorders, family history of BD, and exposure to stressors defined as childhood abuse (emotional or sexual abuse), low maternal warmth, and stressful life events. We expected to find similar results in studies conducted in youth and adult samples.
RESULTS
Of the 48 studies included in this review, 41.6% (k = 20) were carried out in pediatric populations; all were published in English; the most recent study was published in 2017 and the oldest in 1977; 64.6% were conducted in the United States, 12.5% in Europe, and 22.9% in other countries. Two studies were funded by industry, one partially (15) and the other entirely (16), 35 studies received a grant, and funding sources for 11 of the studies were not reported.
The studies included a total of 3,356 children and adolescents with BD recruited from 11 samples and 13,521 adults with BD recruited from 22 samples. Both inpatient and outpatient samples were represented in the youth and adult literatures; additional details on sample characteristics and study design are presented in Table 1 and 2.
For the purposes of this paper, we have organized the factors into four categories – demographic (sex and age at onset), clinical (bipolar subtype, comorbidity, and subsyndromal mood symptoms), environmental (low SES and stressors), and family history of BD.
Factors associated with recurrence:
Among youth studies, the reported factors related to recurrence were: demographic characteristics (sex, k = 5 and age at onset, k = 4), clinical factors (bipolar subtype, k = 4; comorbidity with other psychiatric disorders, k = 11; subsyndromal mood symptoms, k = 3), environmental factors (low SES, k = 2; stressors, k = 3), and family history of BD (k = 4). Among adult studies, reported factors were: demographic characteristics (age at onset, k = 4), clinical factors (comorbidity with other psychiatric disorders, k = 6), environmental factors (low SES, k = 1; stressors, k = 10). The strength association between specific factors and recurrence is shown in Table 3.
Table 3:
Risk of recurrence, mood polarity, and strength association (when possible) of each assessed factor
|
Demographic Factors | ||||||
|---|---|---|---|---|---|---|
|
Sex | ||||||
| Author | Adult/Child Study | Risk of recurrence | ||||
| Birmaher et al., 2006 | Child | more mood episodes in female sex (t = 1.99, p= 0.05) | ||||
| Jairam et al., 2004 | Child | no statistically significant difference (ND) | ||||
| Srinath et al., 1998 | Child | no statistically significant difference (ND) | ||||
| Strober et al., 1995 | Child | no statistically significant difference (ND) | ||||
| Wozniak et al., 2013 | Child | more depressive episodes in males (M= 10.7, SD= 23.3 vs. M= 10.2, SD= 16.8, t=7.2, p<0.001) | ||||
|
Age at onset | ||||||
| Author | Adult/Child Study | Risk of recurrence | ||||
| Baldessarini et al., 2012 | Adult | more mood episodes in earlier onset group (F=3.92, p=0.02) | ||||
| Bashir et al., 1987 | Child | no statistically significant difference (ND) | ||||
| Birmaher et al., 2014 | Child | less mood episodes in later onset of mood symptoms group (χ2= 25.57, p= 0.001) | ||||
| Bromet et al., 2005 | Adult | shorter time to relapse in earlier onset group (HR=0.51; 95% CI=0.31–0.84, p˂ 0.01) | ||||
| Carlson et al., 1977 | Adult | no statistically significant difference (0.38 vs. 0.42 mean episode frequency/year) | ||||
| Carlson et al., 2000 | Adult | more manic and mixed episodes in earlier onset group (64.7% vs. 12.5% and 26.1% vs. 3.3% OR=10.23; 95% CI=1.13–92.37) and less depressive episodes in earlier onset group (17.6% vs. 62.5) | ||||
| Coryell et al., 2013 | Adult | more depressive episodes in earlier onset group (M= 39.9, SD= 32.3 vs. M= 35.1, SD= 31.3, p= 0.015) | ||||
| Jairam et al., 2004 | Child | no statistically significant difference (ND) | ||||
| Karthick et al., 2015 | Adult | no statistically significant difference (ND) | ||||
| Leverich et al., 2007 | Adult | more mood episodes in earlier onset group (20 episodes before entry study: 50 childhood, 105 adolescents and 30 adulthood. Number episodes in first year follow-up: M= 5.4, SD= 3.72 childhood; M= 4.1, SD= 3.43 adolescents; M= 2.8, SD= 3.34 adult) | ||||
| Lish et al., 1994 | Adult | more mood episodes in earlier onset group (51% vs 34%, χ2 = 9.3, p= 0.002) | ||||
| Perlis et al., 2004 | Adult | more mood episodes in earlier onset group (χ2 = 13.82, p= 0.001) | ||||
| Perlis et al., 2009 | Adult | earliest recurrence in childhood onset group (log-rank χ2 = 14.98, p= 0.0001) and adolescent onset group (χ2 = 6.87, p= 0.01) vs. adult onset. Risk not found between child- and adolescent-onset groups (χ2 = 1.79, p= 0.18). Median days to recurrence were 308, 418, and 542 for the child-, adolescent- , and adult-onset age groups, respectively | ||||
| Post et al., 2010 | Adult | more mood episodes in earlier onset group (effect size not reported) | ||||
| Schurhoff et al., 2000 | Adult | risk not found (M= 0.25, SD= 0.05 vs. M= 0.23, SD= 0.07 mania/year and M= 0.33, SD= 0.06 vs. M= 0.45, SD= 0.31 depression/year) | ||||
| Srinath et al., 1998 | Child | no statistically significant difference (ND) | ||||
| Suppes et al., 2001 | Adult | more mood episodes in earlier onset group (64 vs. 57, p= 0.0002 in depression and 53 vs. 46, p= 0.005 in mania). | ||||
| Winokur et al., 1989 | Adult | more mood episodes in earlier onset group (42% polyepisodic group and 25% oligoepisodic group, p= 0.005) | ||||
| Yatham et al., 2009 | Adult | more mood episodes in earlier onset group (small increase in survival time HR (β = 1.119; p= 0.02) with later age of onset) | ||||
| Clinical Factors | ||||||
|
Comorbidity | ||||||
| Author | Adult/Child Study |
Comorbidity type |
Risk of recurrence | |||
| Birmaher et al., 2006 | Child | Psychosis | more mood episodes in psychotic group (t = 2.78 [p= .006]) | |||
| Bromet et al., 2005 | Adult | ANX | more mood episodes in ADHD group (M= 6.0, SD= 3.5 vs. M= 3.9, SD= 3.2, p˂ 0.0001) | |||
| Coryell et al., 2013 | Adult | ANX | more mood episodes in SUD group (OR = 1.57; 95% CI, 0.96–2.58; p= 0.07) | |||
| DelBello et al., 2007 | Child | SUD (alcohol) | more mood episodes in SUD group (HR= 4.3, 95% CI= 3.3 to 5.3, p= 0.005) | |||
| Hua et al., 2011 | Child | Psychosis | more mood episodes in psychotic group (63.39±126.33 vs. 19.92±34.48) | |||
| Jairam et al., 2004 | Child | Psychosis | no statistically significant difference (ND) | |||
| Kovacs et al., 1995 | Child | DBD | no statistically significant difference. No more mood episodes in DBD groups (4.8 (1–12) vs. 6.9 (1–17)) | |||
| Post et al., 2014a | Adult | ANX | more mood episodes in ANX group (OR = 1.36; 95% CI, 0.82–2.27; p= 0.23) | |||
| SUD | more mood episodes in psychotic group (63.39±126.33 vs. 19.92±34.48) | |||||
| Ratheesh et al., 2011 | Child | ANX | more mood episodes in ANX group (3 (1–4) vs. 2 (1–14)) | |||
| Ryden et al., 2009 | Adult | ADHD | more depressive episodes in ANX group (effect size not reported) | |||
| Sala et al., 2012 | Child | ANX | less follow-up time spent euthymic (OR = 0.97; 95% CI, 0.96–0.99; p= 0.0004) | |||
| Sala et al., 2014 | Child | ANX | ↑ risk any mood recurrences (76% vs. 56.4%, χ2= 15.12, p= 0.0001) and depression recurrences specifically (64.9% vs. 49.4%, F= 5.33, p= 0.02) | |||
| Serra et al., 2017 | Adult | ANX | more time in mood episodes in ANX group (%) (5.49±8.94 vs 3.12±6.17, p= 0.04) more time in depressive episodes in ANX group (%) (26.0±22.9 vs. 17.9±22.9, p= 0.009). |
|||
| Srinath et al., 1998 | Child | Psychosis | no statistically significant difference (ND) | |||
| Strober et al., 1995 | Child | Psychosis | no statistically significant difference (ND) | |||
| Tamam et al., 2008 | Adult | ADHD | more mixed episodes in ADHD group (M= 5.6, SD= 9.2 vs. M= 0.81, SD= 3.4, p˂ 0.001) | |||
|
Yen et al., 2016 |
Child | ANX | 1 point ↑ ANX PSR= ↑ risk depressive recurrence 43% (HR= 1.43, 95% CI [1.24–1.65] 1 point ↑ ANX PSR= ↑ risk mania recurrence 43% (HR= 1.43, 95% CI [1.16–1.75] |
|||
| ADHD | 1 point ↑ ADHD PSR= ↑ risk depressive recurrence 53% (HR= 1.53, 95% CI [1.25–1.85]) 1 point ↑ ADHD PSR= ↑ risk mania recurrence 72% (HR= 1.72, 95% CI [1.21–2.44] |
|||||
| DBD | 1 point ↑ DBD PSR= ↑ risk depressive recurrence 22% (HR= 1.22, 95% CI [1.04–1.44]) 1 point ↑ DBD PSR= ↑ risk mania recurrence 67% (HR= 1.67, 95% CI [1.29–2.16] |
|||||
| SUD | 1 point ↑ SUD PSR= ↑ risk depressive recurrence 21% (HR= 1.21, 95% CI [1.01–1.44]) 1 point ↑ SUD PSR= ↑ risk mania recurrence 46% (HR= 1.46, 95% CI [1.09–1.96] |
|||||
|
Subsyndromal mood symptoms | ||||||
| Author | Adult/Child Study | Risk of recurrence | ||||
| Birmaher et al., 2014 | Child | less mood episodes in fewer subsyndromal episodes group (χ2= 10.36, p= 0.02) | ||||
| Jairam et al., 2004 | Child | no statistically significant difference (ND) | ||||
| Wozniak et al., 2011 | Child | Persistent BD-I group had significantly higher one-year prevalence of major depressive disorder compared to the Non-Persistent BD-I group (effect size not reported) | ||||
|
Bipolar subtype | ||||||
| Author | Adult/Child Study | Risk of recurrence | ||||
| Birmaher et al., 2006 | Child | BD-I group was 1.7 times (95% CI, 1.06–2.67) and BD-II group was 2.7 times (95% CI, 1.35–5.31) more likely to have a recurrence than those with BD-NOS | ||||
| Birmaher et al., 2009 | Child | higher rates of mood episodes in BD-I group (65.2%) and BD-II (81.0%) compared to BD-NOS group (53.7%). Recurrence was associated with BD-I and BD-II (vs. BD-NOS, HR:1.37, 95% CI:1.01–1.88) | ||||
| Hirneth et al., 2015 | Child | higher rates of previous mood episodes in BD-I group (45.8% vs. 7.7% BD-II, Fisher’s exact test, p= 0.027; and 19.6% BD-NOS, Fisher’s exact test, p= 0.027) | ||||
| Lewinsohn et al., 2000 | Child | ↑ risk mood episode in symptomatic group (27.3% vs. 2.1%; OR=17.3; 95% CI=1.6–189.6) | ||||
| Environmental Factors | ||||||
| Low SES | ||||||
| Author | Adult/Child Study | Risk of recurrence | ||||
| Birmaher et al., 2006 | Child | with every unit of decrease in SES 20% higher likelihood of recurrence (95% CI, 0.67–0.95) | ||||
| Birmaher et al., 2014 | Child | less mood episodes (χ2= 7.17, p= 0.07) in higher SES group | ||||
|
Post et al., 2014a |
Adult | more mood episodes in poor social support group (OR= 1.18; 95% CI, 0.71–1.97; p= 0.53) and more mood episodes in employment difficulties group (OR= 1.32; 95% CI, 0.79–2.21; p= 0.3) | ||||
| Stressors | ||||||
| Author | Adult/Child Study | Stressor type | Risk of recurrence | |||
| Birmaher et al., 2014 | Child | Sexual abuse | less mood episodes (χ2= 8.16, p= 0.04) in less sexual abused group | |||
| Bromet et al., 2005 | Adult | Child abuse | shorter time to relapse in child abused group (effect size not reported) | |||
| Erten et al., 2014 | Adult | Child abuse | more depressive episodes (t= −2.38, p= 0.019) and total episodes (t= −2.25, p= 0.026) in negative live event group | |||
| Etain et al., 2013 | Adult | Emotional abuse | more number of depressive episodes in emotional abused group (7.07±6.96 vs. 4.72±5.44, r2 = 0.03, P = .002) just in females (no in males) | |||
| Garno et al., 2005 | Adult | Child abuse | more depressive episodes in child abused group (M= 30.4, SD= 50.4 vs. M= 12.0, SD= 24.3, p= 0.026) | |||
| Geller et al., 2008 | Child | Low maternal warmth | more mood episodes in low maternal warmth group (HR= 2.9 (95% CI, 1.5–5.4) | |||
| Gilman et al., 2015 | Adult | Child abuse | more mood episodes in negative live event group (abuse and maltreatment; OR=1.55 and 1.60, respectively) | |||
| Larsson et al., 2013 | Adult | Emotional abuse | more incidence of (hypo)manic episodes (df = 8.3, p < 0.001) in emotional abused group | |||
| Li et al., 2014 | Adult | Child abuse | no statistically significant difference (r= −0.012, p ˃ .05) | |||
| McIntyre et al., 2008 | Adult | Child abuse | no statistically significant difference (ND) | |||
| Nolen et al., 2004 | Adult | Child abuse | more mood episodes in child abused group (r= 0.23, p ˂ .05) | |||
|
Post et al., 2014a |
Adult | Child abuse | more mood episodes in negative live event group (OR= 1.11; 95% CI, 0.63–1.96; p= 0.71) | |||
| Wals et al., 2005 | Child | Stressful life events | no statistically significant difference (OR=2.1, CI=0.2–21.9, p=0.521) | |||
| Family history of bipolar disorder | ||||||
| Author | Adult/Child Study | Risk of recurrence | ||||
| Birmaher et al., 2014 | Child | less mood episodes in less family history of bipolarity group (χ2= 13.02, p= 0.005) | ||||
| Jairam et al., 2004 | Child | no statistically significant difference (ND) | ||||
| Srinath et al., 1998 | Child | no statistically significant difference (ND) | ||||
| Strober et al., 1995 | Child | no statistically significant difference (ND) | ||||
ANX: anxiety; ADHD: attention deficit hyperactivity disorder; DBD: disruptive behavioral disorders; SUD: substance use disorders; SES: socio-economic status; BD-I: bipolar disorder I; BD-II: bipolar disorder II; BD-NOS: bipolar disorder not otherwise specified; mood episode: mood polarity not specified; ND: numerical data not reported; PSR: psychiatric status rating; HR: hazard ratio; CI: coefficient interval; OR: odds ratio; M: median; SD: standard deviation.
Demographic characteristics
Sex.
Five child studies evaluated the effect of sex on recurrence (we did not include adult studies in this category for reasons described above). Results were heterogeneous; one study reported higher frequency of recurrence in males (17), another found more recurrence in females (18) while others did not find any difference in recurrences between the sexes (19, 20, 21).
Age at onset.
Nineteen studies evaluated age at onset. One pediatric study reported fewer mood episodes among those with later onset of the illness (3). The other three child studies (19, 20, 22) reported no association between age at onset and mood recurrence. Studies conducted in adult populations were largely consistent in finding that earlier illness onset was associated with a higher number of recurrences; only three of 15 adult studies found no association between age at onset and mood recurrence (23, 24, 25). Most of the studies in adult populations adjusted for the number of recurrences and the age at onset of the first mood symptom when evaluating this relationship; both prospective and retrospective designs yielded the same results (16, 26, 27, 28, 29, 30, 31).
Clinical factors
Bipolar subtype.
Four studies evaluated whether BD subtype was associated with the number of recurrences. All four found that BD I or BD II subtypes had more recurrences than BD Not Otherwise Specified (NOS) subtype.
Comorbidity.
The effect of comorbidity on recurrences was evaluated in 17 studies. Comorbid mental health disorders were consistently associated with more frequent recurrence, including anxiety disorders (32, 33, 34, 35, 36, 37), attention deficit/hyperactivity disorder (ADHD) (32, 38, 39) and substance use disorders (SUD) (32, 37, 40). The influence of disruptive behavior disorders (DBD) and psychosis was less consistent. The effect of DBD on recurrences was evaluated in two articles, one reported a higher risk (32) while the other reported no effect (41). Presence of psychosis was evaluated in five studies; three of these reported no influence on recurrence while two studies reported increased risk (18, 42).
Subsyndromal mood symptoms.
Three studies evaluated whether the presence of subclinical, inter-episode mood symptoms during childhood were associated with recurrence; one study (19) found no difference in the number of recurrences, while the other two reported higher rates of recurrence among those who experienced subclinical mood symptoms between episodes (3, 43).
Environmental factors
Low SES.
Low SES was related to mood episode recurrence in all studies (k = 3). Of the two child studies that reported on this association, one reported fewer mood episodes among youth with higher SES (3), the other reported 20% higher likelihood of recurrence with every unit of decrease in SES (18). The adult study found that unemployment was associated with more mood episodes (37).
Stressors.
All but two (44, 45) of eleven studies that reported on the association between child abuse and recurrence reported increased risk for mood episodes among those with a history of abuse. Low maternal warmth was also associated with an increase of recurrence in the one study that reported on this relation (46). Stressful life events were associated with depressive episode recurrence in one study, but this association was no longer significant after adjusting for demographic and baseline clinical characteristics (47).
Family history of BD.
Four child studies evaluated family history of BD. One study reported a higher number of recurrences in youth with a family history of BD (3), the other three studies did not find an association between family history of BD and recurrence (19, 20, 21).
DISCUSSION
The goal of this review was to evaluate the influence of childhood risk factors on mood episode recurrence in people with bipolar disorder. Although we sought to characterize all factors associated with recurrence or lack thereof, there was surprisingly little variability in the focus of the majority of studies, and some factors for which we expected to find an association (e.g., suicide attempt, rapid cycling) were not represented in any published report. Additionally, there was almost no information about protective factors. Consequently, there are likely gaps in our knowledge about important influences on illness course. Among the factors that were described, they tended to fall into four broad categories – demographic characteristics, clinical factors, environmental factors, and family history of BD. Studies of children and adults tended to focus on somewhat different risk factors, but across studies results were fairly consistent; earlier age of onset, BD I and BD II subtypes, comorbidity with other psychiatric disorders, subsyndromal mood symptoms, low SES, and stressors were associated with more mood episode recurrence.
Demographic characteristics
The findings related to sex and mood recurrence were inconsistent; the study that found higher risk of depressive episodes in males, described other differences between the sexes (e.g., males had longer duration and earlier onset illness, plus a higher rate of comorbid panic disorder; 17) that may have influenced the higher rate of recurrence in boys. Additionally, both boys and girls in this study (17) were younger, on average, than the youth in the study in which mood episodes were more prevalent in females (18) (average age 10.7 ± 3.0 vs. 13.2 ± 3 respectively). This result is consistent with other research suggesting that females are at higher risk for mood (especially depressive) episodes in adolescence due to both psychosocial and biological risk factors (48). Relatedly, it is important to note that we evaluated the effect of sex only in those studies carried out in pediatric populations. However, the studies we included focused on ranged in age from 10 to 18, which introduces possible bias associated with sex.
The results related to the association between an earlier age at onset and recurrence varied depending on whether the data were collected in child- or adulthood. This may be a meaningful difference; among the youth studies, there was little variance in terms of age of onset because all the participants were children when their BD developed, which could obscure the relationship. In contrast, adult studies include participants with a wider range of onset ages, which could highlight this association. Differences in how age of onset is defined could also impact the association; youth studies are more likely to report an average, whereas many adult studies stratify it, grouping people by the developmental period during which they became symptomatic (e.g., 12–18 years, 19–25, 25–31, etc…), which makes it easier to observe age-related differences. It could also be that the effect of early onset is not yet be evident in youth samples; the kindling theory posits that with each mood recurrence, the likelihood of another mood episode grows (11); based on this model, the impact of early onset would grow over the years. This finding that the influence of age of onset on recurrence changes over the lifespan, emphasizes the importance of longitudinal designs to fully understand the developmental processes that interact with risk factors to influence the course of BD. Additionally, because collecting accurate data on the timing of specific events (including age of onset) becomes more difficult as time passes, due to recall biases, prospective designs are necessary to collecting accurate information on the associations between risk factors and mood recurrence.
Clinical factors
All four studies carried out in pediatric populations found that youth with BD NOS had fewer recurrences than those with BD I or BD II. This is in contrast with some adult studies, which tend to show that individuals with BD I have the fewest recurrences (49, 50). However, it is important to note, in the case of the comparison between BD I or II and BD NOS, that once a youth has a manic episode, s/he is no longer in the NOS group, so this comparison can become somewhat tautological.
The majority of youth with BD meet criteria for at least one additional mental illness (32), which, according to the results of this review, puts them at higher risk for a mood episode recurrence. There are a number of reasons that comorbidity may be associated with higher risk of recurrences. First, youth with more severe presentations of BD, characterized by a predominantly ill course, tend to have more comorbid disorders, in addition to greater impairment and poorer treatment response (3). Additionally, comorbidity has been associated with lower family cohesion, early-onset academic and behavior problems, and worse functioning (42). These factors are likely to contribute to a more chaotic home environment, which could increase stress and the likelihood of mood recurrences (51, 52, 53, 54, 55, 56, 57). Additionally, worse course, greater impairment and trouble in other domains (e.g,. home, school, peers) might make it harder for families to prioritize treatment compliance – both for BD and for comorbid disorders (13), or the comorbid condition could obscure the BD and reduce the likelihood of appropriate treatment. It is also possible that greater overall illness burden could increase the risk of environmental factors (e.g., stressful events) that are a risk factor both for the development of other childhood disorders and for mood recurrence itself (33, 58). It is also possible that comorbid conditions increase risk for mood episodes through other pathways; for example, frequent criticism of a child’s hyperactive and impulsive behavior may lead to depressed mood (59). The genetic link between some disorders (anxiety with depression for example) may also confer a higher risk for mood episodes (60). Medications for comorbid conditions may also increase the risk for recurrences (e.g., SSRIs, stimulants; 3, 61), interfere with mood treatment efficacy (62).
We hypothesized that psychotic symptoms, which tend to be associated with more severe presentations of BD in youths (1), would be related to a greater number of recurrences. This hypothesis was only partly supported; psychotic symptoms were associated with heterogeneous results regarding appearance of new episodes. We think that this result should be carefully interpreted; the samples in which no association was found (19, 20, 21) were smaller, were collected in the 1990s, and were unusual in that the rates of comorbidity were very low. Additionally, two of three studies reporting no association between psychotic symptoms and mood recurrences obtained a 5 point NOQAS scoring (19, 21), indicating higher risk of bias than the studies reporting increased risk (18, 42). In contrast, the two studies that did find an association between psychotic symptoms and mood recurrence were much larger, had more heterogeneous participants, and were conducted more recently (18, 42). If there is an association between psychotic symptoms and greater mood recurrence, it seems likely that there are other factors involved; youth who have BD with psychotic symptoms typically have more comorbidity, lower psychosocial functioning, lower family cohesion, lower cognitive functioning and more family history of psychosis than bipolar youths without psychotic symptoms (42). These factors contribute greater severity to the illness course and could result in poorer treatment response or adherence, which could explain the higher number of mood recurrences among those with psychosis.
Higher rates of recurrence among youth who continued to experience subclinical mood symptoms between episodes suggests that those who do not respond well to treatment or have inadequate treatment and, consequently, do not achieve remission, are at higher risk for recurrence (or relapse). Similar findings have been reported in longitudinal studies of adults with BD (2, 63, 64) and in youths (48) and adults with unipolar depression (65). This is not surprising, but it emphasizes the importance of research to develop a more personalized approach to BD treatment; in acute treatment trials, rates of remission in youth with BD range from 14% to 100% (40), but we know little about the main factors that determine who gets well. Related, there are no randomized controlled maintenance studies in youths with BD to provide information about the best strategies to prevent recurrence.
Environmental factors
The association between low SES and a greater number of mood recurrences was consistent with our hypothesis; recurrence and more severe psychopathology are consistently associated with low SES (3, 14, 40). This association may be indirect; a lower SES could increase familial stress and make it more difficult to follow to treatment recommendations, which could lead to a worse course of illness.
Stressors were evaluated in 13 studies and the results were generally consistent with our hypothesis that stress would lead to more recurrences (66). However, the nature of the stressors varied (stressful life events (47), childhood abuse (sexual and emotional; 3, 10, 27, 37, 44, 45, 67, 68, 69, 70, 71), and low maternal warmth (46), which presumably would lead to different levels of impact. Additionally, barely half of the studies were prospective (three youth and three adult studies), which limits the conclusions that can be drawn in terms of the temporal relation between the stressor and mood recurrence. Prospective collection of data regarding life events is ideal, in order to limit the influence of recall bias, but even when this is not possible, there are methods for acertaining more reliable accounts (e.g., using a semi-structured interview such as the Bedford College Life Events Difficulties Schedule, 72). The majority of the studies in this review relied on less robust methods, such as checklists, which may impact the reliability of the findings. Additionally, there are other factors, such as the severity and chronicity of the stressor (73, 74, 75), the age and sex of the child (76, 77), and whether it involves interpersonal violence, that further influence the impact of a stressor. Without more detail, it is impossible to draw clear conclusions about the ways stressful childhood events are likely to impact the course of BD.
Another important consideration is whether stressors – which vary significantly in chronicity and severity, among other factors – are risk factors for recurrence, or whether they, in fact, trigger the new episode directly. The distinction is important, as it could indicate different mechanisms by which the stress of the event impacts the pathophysiology of BD (78). The relation between stressors and mood episodes has been studied from different perspectives, including as a gene-environment interaction (76, 79) or psychosocial disruption (80). Greater specificity, in terms of the stressor itself, the developmental period in which it occurred, and its temporal relationship with the mood episode, will help to build our understanding of the impact of these events on people with BD.
Family history of BD
Only one of four studies that evaluated the relation between family history of BD and mood recurrences, found an association. However, the study that did find an association had longer follow-up and a larger, more representative sample, which may have given it better power for detecting an effect (3). There are three primary reasons to predict that family history of BD would be associated with more recurrence; first, family history is the most robust risk factor for the onset of the disorder (81). Second, in addition to genetic risk, having a close family member with BD is likely to increase stress and chaos, which could then trigger a new mood episode in other family members (51, 82). A chaotic environment may also disrupt circadian rhythms (e.g., sleep) in youths, which in turn, may increase the risk for recurrences (80, 83, 84). Moreover, adults with BD often meet criteria for comorbid disorders as well, increasing the overall psychiatric burden (85), which could contribute to worse family functioning (including negative attachment style) and environmental factors (stressors) that are associated with increased risk of recurrence (55, 57). Family history of psychopathology other than BD is also likely to contribute risk for recurrence through environmental influences. However, none of the child-focused papers included in this review reported on the influence of non-BD familial psychopathology
Implications
Consistent with our hypotheses, factors that are generally associated with a more severe BD presentation also tend to be associated with a greater number of mood recurrences. Paying attention to these factors will inform prognostication and, when the burden of risk is high, should impact treatment decisions. We know that treatment reduces recurrences (81), and that when treatment is initiated early, the potential for positive outcomes is greater (4, 81, 86, 87). Notably, although we sought to investigate both risk and protective factors, the majority of papers focused on the risk factors associated with an increase in recurrence. An important next step in understanding how to mitigate the risk of frequent recurrences and a worse illness trajectory over time will be to study how treatment can moderate the impact of the risk factors identified here. This is particularly true for risk factors, such as stressors and family function, that may be unavoidable, but for which the psychological impact could be ameliorated with psychosocial interventions (e.g., changes in cognition, emotional and behavioral regulation, coping skills, and circadian cycles). Family-focused therapies for bipolar offspring and for children and adolescents with BD to help reduce stress and improve functioning may be particularly beneficial (84, 88, 89, 90). Social services (e.g., linkage to mental health providers, programs to facilitate treatment adherence, support from employment and educational institutions) could also help by reducing stressors and their associated impact on both mood symptoms and risk factors for recurrence. Finally, an early diagnosis together with effective treatment of comorbid disorders and subsyndromal mood symptoms could be an important component of reducing the burden associated with BD and improving patient outcomes.
Limitations
The systematic review reported here combines data across studies in order to better understand factors associated mood recurrences with more precision than is possible in a single study. This review has several limitations. The first is that both the definitions and methods for assessing risk factors and recurrences vary widely across studies. This prevented the evaluation of the data using meta analysis and limits the generalizability of the findings. Related, the studies varied significantly in terms of what they reported, with some giving details about the polarity of mood episode recurrences and others saying only that there was a relapse. Likewise, most studies included little-to-no detail about how much time passed before the recurrence or about the frequency of recurrence, and the retrospective nature of most of the reports precludes a detailed understanding of the temporal relations between risk factors and recurrence. Prospective studies offer the clearest evidence of a causal relationship between factors associated with risk for recurrences and course, and the 30 prospective studies included in the review are a strength. Importantly, similar patterns of risk emerged in both prospective and retrospective designs. It is also possible that publication bias impacted our results, the quality of the studies varied (as indicated by the NOQAS scores), but this risk should be low due to the fact that the risk factors we were interested in are not things about which authors would be expected to have a conflict of interest. Finally, two of the risk factors we had hypothesized would be related to mood recurrence – suicide attempt and rapid cycling – were not reported in any of the papers included in this review.
As we expected, youth and adult studies showed similar results, but there were differences in focus across pediatric and adult studies that limit our ability to generalize across the lifespan. For example, the effects of family history of BD or BD subtype on recurrences were more often assessed and reported in pediatric studies, whereas child abuse was more often the focus in adult studies. It is possible that these factors actually vary in their impact across the lifespan (e.g., the measurable effects of abuse on illness course may not be apparent until later in its course), but this is not possible to determine given how many studies are conducted (cross-sectional with retrospective report) and how the data are reported (with minimal detail).
CONCLUSIONS
Early identification and treatment of modifiable risk factors such as the presence of comorbid disorders and subsyndromal mood symptoms, coupled with appropriate cognitive behavioral therapies and family-focused therapies could reduce the number of episodes and potentially improve the course of BD. Furthermore, social programs designed to reduce exposure stressors, including poverty and abuse, would benefit young people with BD, among others.
Taking a lifespan approach, whether through longitudinal studies that span multiple developmental periods or through coordination between research groups to ensure consistency in the measurement of hypothesized risk and resilience factors across developmental periods is likely to yield knowledge helpful for the development of interventions that can improve outcomes among people with BD. Embracing standard definitions and measurement tools would allow for the conduct of meta analytic studies, which can clarify the associations between risk and protective factors and mood recurrence, enabling a more proactive approach to managing the course of BD. In spite of the limitations of this literature, the progress we have made in understanding BD is helping to inform future studies that will further build our knowledge about its mechanisms, enabling more accurate diagnosis and prognostication and more effective treatment adminstration. It is clear that there are factors that influence the recurrence of mood episodes and, as we gain more precise knowledge of these factors, our ability to reduce recurrence and improve quality of life for those affected will grow.
Supplementary Material
ACKNOWLEDGEMENTS
Funding support: Xavier Estrada-Prat received support from an Alicia Koplowitz Foundation grant. The sponsor played no role in study design, collection, analysis, interpretation of data, writing of the report, or in the decision to submit the paper for publication.
Fundings: Funding for this study was provided by the National Institute of Mental Health (NIMH) grants MH59929 (B. B.), MH59977 (M. A. S.), and MH59691 (M. B. K.). Xavier Estrada-Prat received support from a grant from the Alicia Koplowitz Foundation.
Fundings: Funding for this study was provided by the National Institute of Mental Health (NIMH) grants MH59929 (B. B.), MH59977 (M. A. S.), and MH59691 (M. B. K.). Dr. Estrada received support from a grant from the Alicia Koplowitz Foundation.
Professor Birmaher receives funds for research from the National Institute of Mental Health. He receives royalties for publications from: Random House, Inc., Lippincott Williams & Wilkins, APA Press, and UpToDate.
Footnotes
Systematic review registration number (PROSPERO): CRD42018086583.
Conflict of interest statement:
The authors Anna R. Van Meter, Ester Camprodon-Rosanas, Santiago Batlle-Vila, and Benjamin I. Goldstein have nothing to disclose. All the authors declare no financial interests or potential conflicts of interest related directly or indirectly to this work.
REFERENCES
- 1.Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, Yen S, Hower H, Esposito-Smythers C, Goldstein T, Ryan N, Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. Am J Psychiatry 2009; 166(7), 795–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, Leon AC, Rice JA, Keller MB. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002; 59(6), 530–537. [DOI] [PubMed] [Google Scholar]
- 3.Birmaher B, Gill MK, Axelson DA, Goldstein BI, Goldstein TR, Yu H, Liao F, Iyengar S, Diler RS, Strober M, Hower H, Yen S, Hunt J, Merranko JA, Ryan ND, Keller MB. Longitudinal trajectories and associated baseline predictors in youths with bipolar spectrum disorders. Am J Psychiatry 2014; 171(9), 990–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, Gao K, Miskowiak KW, Grande I. Bipolar disorders. Nat Rev Dis Primers 2018; 4, 18008. [DOI] [PubMed] [Google Scholar]
- 5.University of York. Centre for Reviews and Dissemination. PROSPERO International prospective register of systematic reviews URL: http://www.crd.york.ac.uk. Registration number: CRD42018086583 [0½9/2018]
- 6.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos P, Tugwell P (2001). Nonrandomised studies, including case-control and cohort studies Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed in February, 2018.
- 7.Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. Edited by Higgins JPT, Green S. [http://www.cochrane-handbook.org].
- 8.Veronese N, Cereda E, Solmi M, Fowler SA, Manzato E, Maggi S, Manu P, Abe E, Hayashi K, Allard JP, Arendt BM, Beck A, Chan M, Audrey YJ, Lin WY, Hsu HS, Lin CC, Diekmann R, Kimyagarov S, Miller M, Cameron ID, Pitkälä KH, Lee J, Woo J, Nakamura K, Smiley D, Umpierrez G, Rondanelli M, Sund-Levander M, Valentini L, Schindler K, Törmä J, Volpato S, Zuliani G, Wong M, Lok K, Kane JM, Sergi G, Correll CU. Inverse relationship between body mass index and mortality in older nursing home residents: a meta-analysis of 19,538 elderly subjects. Obes Rev 2015; 16: 1001–1015. [DOI] [PubMed] [Google Scholar]
- 9.Gershon A, Eidelman P. Inter-episode affective intensity and instability: predictors of depression and functional impairment in bipolar disorder. J Behav Ther Exp Psychiatry 2015; 46, 14–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gilman SE, Ni MY, Dunn EC, Breslau J, McLaughlin KA, Smoller JW, Perlis RH. Contributions of the social environment to first-onset and recurrent mania. Mol Psychiatry 2015; 20(3), 329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev 2007; 31(6), 858–873. [DOI] [PubMed] [Google Scholar]
- 12.Starling J, Williams LM, Hainsworth C, Harris AW. The presentation of early-onset psychotic disorders. Aust N Z J Psychiatry 2013; 47(1), 43–50. [DOI] [PubMed] [Google Scholar]
- 13.Suppes T, Dennehy EB, Gibbons EW. The longitudinal course of bipolar disorder. J Clin Psychiatry 2000; 61 Suppl 9, 23–30. [PubMed] [Google Scholar]
- 14.Suppes T, Leverich GS, Keck PE, Nolen WA, Denicoff KD, Altshuler LL, McElroy SL, Rush AJ, Kupka R, Frye MA, Bickel M, Post RM. The Stanley Foundation Bipolar Treatment Outcome Network. II. Demographics and illness characteristics of the first 261 patients. J Affect Disord 2001; 67(1–3), 45–59. [DOI] [PubMed] [Google Scholar]
- 15.Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994; 31(4), 281–294. [DOI] [PubMed] [Google Scholar]
- 16.Yatham LN, Kauer-Sant’Anna M, Bond DJ, Lam RW, Torres I. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Program For Early Mania project. Can J Psychiatry 2009; 54(2), 105–112. [DOI] [PubMed] [Google Scholar]
- 17.Wozniak J, Biederman J, Martelon MK, Hernandez M, Woodworth KY, Faraone SV. Does sex moderate the clinical correlates of pediatric bipolar-I disorder? Results from a large controlled family-genetic study. J Affect Disord 2013; 149(1–3), 269–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry 2006; 63(2), 175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jairam R, Srinath S, Girimaji SC, Seshadri SP. A prospective 4–5 year follow-up of juvenile onset bipolar disorder. Bipolar Disord 2004; 6(5), 386–394. [DOI] [PubMed] [Google Scholar]
- 20.Srinath S, Janardhan Reddy YC, Girimaji SR, Seshadri SP, Subbakrishna DK. A prospective study of bipolar disorder in children and adolescents from India. Acta Psychiatr Scand 1998; 98(6), 437–442. [DOI] [PubMed] [Google Scholar]
- 21.Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995; 34(6), 724–731. [DOI] [PubMed] [Google Scholar]
- 22.Bashir M, Russell J, Johnson G. Bipolar affective disorder in adolescence: a 10-year study. Aust N Z J Psychiatry 1987; 21(1), 36–43. [DOI] [PubMed] [Google Scholar]
- 23.Karthick S, Kattimani S, Rajkumar RP, Bharadwaj B, Sarkar S. Long term course of bipolar I disorder in India: using retrospective life chart method. J Affect Disord 2015; 173, 255–260. [DOI] [PubMed] [Google Scholar]
- 24.Schurhoff F, Bellivier F, Jouvent R, Mouren-Simeoni MC, Bouvard M, Allilaire JF, Leboyer M. Early and late onset bipolar disorders: two different forms of manic-depressive illness? J Affect Disord 2000; 58(3), 215–221. [DOI] [PubMed] [Google Scholar]
- 25.Carlson GA, Davenport YB, Jamison K. A comparison of outcome in adolescent- and later-onset bipolar manic-depressive illness. Am J Psychiatry 1977; 134(8), 919–922. [DOI] [PubMed] [Google Scholar]
- 26.Baldessarini RJ, Tondo L, Vazquez GH, Undurraga J, Bolzani L, Yildiz A, Khalsa HM, Lai M, Lepri B, Lolich M, Maffei PM, Salvatore P, Faedda GL, Vieta E, Tohen M. Age at onset versus family history and clinical outcomes in 1,665 international bipolar-I disorder patients. World Psychiatry 2012; 11(1), 40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bromet EJ, Finch SJ, Carlson GA, Fochtmann L, Mojtabai R, Craig TJ, Kang S, Ye Q. Time to remission and relapse after the first hospital admission in severe bipolar disorder. Soc Psychiatry Psychiatr Epidemiol 2005; 40(2), 106–113. [DOI] [PubMed] [Google Scholar]
- 28.Carlson GA, Bromet EJ, Sievers S. Phenomenology and outcome of subjects with early- and adult-onset psychotic mania. Am J Psychiatry 2000; 157(2), 213–219. [DOI] [PubMed] [Google Scholar]
- 29.Coryell W, Fiedorowicz J, Leon AC, Endicott J, Keller MB. Age of onset and the prospectively observed course of illness in bipolar disorder. J Affect Disord 2013; 146(1), 34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leverich GS, Post RM, Keck PE Jr., Altshuler LL, Frye MA, Kupka RW, Nolen WA, Suppes T, McElroy SL, Grunze H, Denicoff K, Moravec MK, Luckenbaugh D. The poor prognosis of childhood-onset bipolar disorder. J Pediatr 2007; 150(5), 485–490. [DOI] [PubMed] [Google Scholar]
- 31.Perlis RH, Dennehy EB, Miklowitz DJ, Delbello MP, Ostacher M, Calabrese JR, Ametrano RM, Wisniewski SR, Bowden CL, Thase ME, Nierenberg AA, Sachs G. Retrospective age at onset of bipolar disorder and outcome during two-year follow-up: results from the STEP-BD study. Bipolar Disord 2009; 11(4), 391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yen S, Stout R, Hower H, Killam MA, Weinstock LM, Topor DR, Dickstein DP, Hunt JI, Gill MK, Goldstein TR, Goldstein BI, Ryan ND, Strober M, Sala R, Axelson DA, Birmaher B, Keller MB. The influence of comorbid disorders on the episodicity of bipolar disorder in youth. Acta Psychiatr Scand 2016; 133(4), 324–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sala R, Axelson DA, Castro-Fornieles J, Goldstein TR, Goldstein BI, Ha W, Liao F, Gill MK, Iyengar S, Strober MA, Yen S, Hower H, Hunt JI, Dickstein DP, Ryan ND, Keller MB, Birmaher B. Factors associated with the persistence and onset of new anxiety disorders in youth with bipolar spectrum disorders. J Clin Psychiatry 2012; 73(1), 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sala R, Strober MA, Axelson DA, Gill MK, Castro-Fornieles J, Goldstein TR, Goldstein BI, Ha W, Liao F, Iyengar S, Yen S, Hower H, Hunt J, Dickstein DP, Ryan ND, Keller MB, Birmaher B. Effects of comorbid anxiety disorders on the longitudinal course of pediatric bipolar disorders. J Am Acad Child Adolesc Psychiatry 2014; 53(1), 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ratheesh A, Srinath S, Reddy YC, Girimaji SC, Seshadri SP, Thennarasu K, Hutin Y. Are anxiety disorders associated with a more severe form of bipolar disorder in adolescents? Indian J Psychiatry 2011; 53(4), 312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Serra G, Koukopoulos A, De Chiara L, Koukopoulos AE, Sani G, Tondo L, Girardi P, Reginaldi D, Baldessarini RJ. Early clinical predictors and correlates of long-term morbidity in bipolar disorder. Eur Psychiatry 2017; 43, 35–43. [DOI] [PubMed] [Google Scholar]
- 37.Post RM, Altshuler LL, Leverich GS, Nolen WA, Kupka R, Grunze H, Frye MA, Suppes T, McElroy SL, Keck PE Jr., Rowe M. Illness progression as a function of independent and accumulating poor prognosis factors in outpatients with bipolar disorder in the United States. Prim Care Companion CNS Disord 2014; 16(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ryden E, Thase ME, Straht D, Aberg-Wistedt A, Bejerot S, Landen M. A history of childhood attention-deficit hyperactivity disorder (ADHD) impacts clinical outcome in adult bipolar patients regardless of current ADHD. Acta Psychiatr Scand 2009; 120(3), 239–246. [DOI] [PubMed] [Google Scholar]
- 39.Tamam L, Karakus G, Ozpoyraz N. Comorbidity of adult attention-deficit hyperactivity disorder and bipolar disorder: prevalence and clinical correlates. Eur Arch Psychiatry Clin Neurosci 2008; 258(7), 385–393. [DOI] [PubMed] [Google Scholar]
- 40.DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry 2007; 164(4), 582–590. [DOI] [PubMed] [Google Scholar]
- 41.Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry 1995; 34(6), 715–723. [DOI] [PubMed] [Google Scholar]
- 42.Hua LL, Wilens TE, Martelon M, Wong P, Wozniak J, Biederman J. Psychosocial functioning, familiality, and psychiatric comorbidity in bipolar youth with and without psychotic features. J Clin Psychiatry 2011; 72(3), 397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wozniak J, Petty CR, Schreck M, Moses A, Faraone SV, Biederman J. High level of persistence of pediatric bipolar-I disorder from childhood onto adolescent years: a four year prospective longitudinal follow-up study. J Psychiatr Res 2011; 45(10), 1273–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McIntyre RS, Soczynska JK, Mancini D, Lam C, Woldeyohannes HO, Moon S, Konarski JZ, Kennedy SH. The relationship between childhood abuse and suicidality in adult bipolar disorder. Violence Vict 2008; 23(3), 361–372. [DOI] [PubMed] [Google Scholar]
- 45.Li XB, Liu JT, Zhu XZ, Zhang L, Tang YL, Wang CY. Childhood trauma associates with clinical features of bipolar disorder in a sample of Chinese patients. J Affect Disord 2014; 168, 58–63. [DOI] [PubMed] [Google Scholar]
- 46.Geller B, Tillman R, Bolhofner K, Zimerman B. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry 2008; 65(10), 1125–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wals M, Hillegers MH, Reichart CG, Verhulst FC, Nolen WA, Ormel J. Stressful life events and onset of mood disorders in children of bipolar parents during 14-month follow-up. J Affect Disord 2005; 87(2–3), 253–263. [DOI] [PubMed] [Google Scholar]
- 48.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet 2012; 379(9820), 1056–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, Leon AC, Rice JA, Keller MB. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry, 2002; 59(6), 530–537. [DOI] [PubMed] [Google Scholar]
- 50.Suppes T, Leverich GS, Keck PE, Nolen WA, Denicoff KD, Altshuler LL, McElroy SL, Rush AJ, Kupka R, Frye MA, Bickel M, Post RM. The Stanley Foundation Bipolar Treatment Outcome Network. II. Demographics and illness characteristics of the first 261 patients. J Affect Disord, 2001; 67(1–3), 45–59. [DOI] [PubMed] [Google Scholar]
- 51.Johnson SL, Miller I. Negative life events and time to recovery from episodes of bipolar disorder. J Abnorm Psychol 1997; 106(3), 449–457. [DOI] [PubMed] [Google Scholar]
- 52.Miklowitz DJ, Johnson SL. Social and Familial Factors in the Course of Bipolar Disorder: Basic Processes and Relevant Interventions. Clin Psychol (New York) 2009; 16(2), 281–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sullivan AE, Judd CM, Axelson DA, Miklowitz DJ. Family functioning and the course of adolescent bipolar disorder. Behav Ther 2012; 43(4), 837–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cohen AN, Hammen C, Henry RM, Daley SE. Effects of stress and social support on recurrence in bipolar disorder. J Affect Disord, 2004; 82(1), 143–147. [DOI] [PubMed] [Google Scholar]
- 55.Hammen C Adolescent Depression: Stressful Interpersonal Contexts and Risk for Recurrence. Curr Dir Psychol Sci, 2009; 18(4), 200–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hammen C, Brennan PA, Keenan-Miller D, Hazel NA, Najman JM. Chronic and acute stress, gender, and serotonin transporter gene-environment interactions predicting depression symptoms in youth. J Child Psychol Psychiatry, 2010; 51(2), 180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ostiguy CS, Ellenbogen MA, Linnen AM, Walker EF, Hammen C, Hodgins S Chronic stress and stressful life events in the offspring of parents with bipolar disorder. J Affect Disord, 2009; 114(1–3), 74–84. [DOI] [PubMed] [Google Scholar]
- 58.Bohacek J, Mansuy IM. Epigenetic inheritance of disease and disease risk. Neuropsychopharmacology 2013; 38(1), 220–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Majumder PP, Moss HB, Murrelle L. Familial and nonfamilial factors in the prediction of disruptive behaviors in boys at risk for substance abuse. J Child Psychol Psychiatry 1998; 39(2), 203–213. [PubMed] [Google Scholar]
- 60.Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychol Med 2007; 37(3), 453–462. [DOI] [PubMed] [Google Scholar]
- 61.Goldsmith M, Singh M, Chang K. Antidepressants and psychostimulants in pediatric populations: is there an association with mania? Paediatr Drugs 2011; 13(4), 225–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pettinati HM, O’Brien CP, Dundon WD. Current status of co-occurring mood and substance use disorders: a new therapeutic target. Am J Psychiatry 2013; 170(1), 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Angst J, Sellaro R. Historical perspectives and natural history of bipolar disorder. Biol Psychiatry 2000; 48(6), 445–457. [DOI] [PubMed] [Google Scholar]
- 64.Tohen M, Waternaux CM, Tsuang MT. Outcome in Mania. A 4-year prospective follow-up of 75 patients utilizing survival analysis. Arch Gen Psychiatry 1990; 47(12), 1106–1111. [DOI] [PubMed] [Google Scholar]
- 65.Goldberg JF, Harrow M. Consistency of remission and outcome in bipolar and unipolar mood disorders: a 10-year prospective follow-up. J Affect Disord 2004; 81(2), 123–131. [DOI] [PubMed] [Google Scholar]
- 66.Grandin LD, Alloy LB, Abramson LY. Childhood stressful life events and bipolar spectrum disorders. Journal of social and clinical psychology 2017; 26, 460–478. [Google Scholar]
- 67.Erten E, Funda Uney A, Saatcioglu O, Ozdemir A, Fistikci N, Cakmak D. Effects of childhood trauma and clinical features on determining quality of life in patients with bipolar I disorder. J Affect Disord 2014; 162, 107–113. [DOI] [PubMed] [Google Scholar]
- 68.Etain B, Aas M, Andreassen OA, Lorentzen S, Dieset I, Gard S, Kahn JP, Bellivier F, Leboyer M, Melle I, Henry C. Childhood trauma is associated with severe clinical characteristics of bipolar disorders. J Clin Psychiatry 2013; 74(10), 991–998. [DOI] [PubMed] [Google Scholar]
- 69.Larsson S, Aas M, Klungsoyr O, Agartz I, Mork E, Steen NE, Barrett EA, Lagerberg TV, Rossberg JI, Melle I, Andreassen OA, Lorentzen S. Patterns of childhood adverse events are associated with clinical characteristics of bipolar disorder. BMC Psychiatry 2013; 13, 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Garno JL, Goldberg JF, Ramirez PM, Ritzler BA. Impact of childhood abuse on the clinical course of bipolar disorder. Br J Psychiatry 2005; 186, 121–125. [DOI] [PubMed] [Google Scholar]
- 71.Nolen WA, Luckenbaugh DA, Altshuler LL, Suppes T, McElroy SL, Frye MA, Kupka RW, Keck PE Jr., Leverich GS, Post RM. Correlates of 1-year prospective outcome in bipolar disorder: results from the Stanley Foundation Bipolar Network. Am J Psychiatry 2004; 161(8), 1447–1454. [DOI] [PubMed] [Google Scholar]
- 72.Brown GW, Harris T. Social origins of depression: A study of psychiatric disorder in women London: Tavistock Publications; 1978. [Google Scholar]
- 73.Bottonari KA, Roberts JE, Kelly MA, Kashdan TB, & Ciesla JA (2007). A prospective investigation of the impact of attachment style on stress generation among clinically depressed individuals. Behav Res Ther, 45(1), 179–188. doi: 10.1016/j.brat.2006.01.003 [DOI] [PubMed] [Google Scholar]
- 74.Farmer AE, and McGuffin P Humiliation, loss and other types of life events and difficulties: a comparison of depressed subjects, healthy controls and their siblings. Psychol Med, 2003; 33(7), 1169–1175. [DOI] [PubMed] [Google Scholar]
- 75.Frank E, Anderson B, Reynolds CF 3rd, Ritenour A, Kupfer DJ. Life events and the research diagnostic criteria endogenous subtype. A confirmation of the distinction using the Bedford College methods. Arch Gen Psychiatry, 1994; 51(7), 519–524. [DOI] [PubMed] [Google Scholar]
- 76.Alameda L, Ferrari C, Baumann PS, Gholam-Rezaee M, Do KQ, Conus P Childhood sexual and physical abuse: age at exposure modulates impact on functional outcome in early psychosis patients. Psychol Med, 2015; 45(13), 2727–2736. [DOI] [PubMed] [Google Scholar]
- 77.Harkness KL, Alavi N, Monroe SM, Slavich GM, Gotlib IH, Bagby RM. Gender differences in life events prior to onset of major depressive disorder: the moderating effect of age. J Abnorm Psychol, 2010; 119(4), 791–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Agnew-Blais J, Danese A. Childhood maltreatment and unfavourable clinical outcomes in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry 2016; 3(4), 342–349. [DOI] [PubMed] [Google Scholar]
- 79.Strickland PL, Deakin JF, Percival C, Dixon J, Gater RA, Goldberg DP. Bio-social origins of depression in the community. Interactions between social adversity, cortisol and serotonin neurotransmission. Br J Psychiatry, 2002; 180, 168–173. [DOI] [PubMed] [Google Scholar]
- 80.Malkoff-Schwartz S, Frank E, Anderson BP, Hlastala SA, Luther JF, Sherrill JT, Houck PR, Kupfer DJ. Social rhythm disruption and stressful life events in the onset of bipolar and unipolar episodes. Psychol Med, 2000; 30(5), 1005–1016. [DOI] [PubMed] [Google Scholar]
- 81.Goldstein BI, Birmaher B, Carlson GA, DelBello MP, Findling RL, Fristad M, Kowatch RA, Miklowitz DJ, Nery FG, Perez-Algorta G. The International Society for Bipolar Disorders Task Force report on pediatric bipolar disorder: Knowledge to date and directions for future research 2017; 19(7), 524–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Algorta GP, Van Meter A, Youngstrom E. The Apple and the Tree. In Yildiz A, Ruiz P, & Nemeroff CB (Eds.), The Bipolar Book: History, Neurobiology, and Treatment New York: Oxford University Press, 2015: 171–180. [Google Scholar]
- 83.Leibenluft E, Suppes T. Treating bipolar illness: focus on treatment algorithms and management of the sleep-wake cycle. Am J Psychiatry 1999; 156(12), 1976–1981. [DOI] [PubMed] [Google Scholar]
- 84.Frank E. Interpersonal and social rhythm therapy: a means of improving depression and preventing relapse in bipolar disorder. J Clin Psychol 2007; 63(5), 463–473. [DOI] [PubMed] [Google Scholar]
- 85.Birmaher B, Axelson D, Goldstein B, Monk K, Kalas C, Obreja M, Hickey MB, Iyengar S, Brent D, Shamseddeen W, Diler R, Kupfer D. Psychiatric disorders in preschool offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring Study (BIOS). Am J Psychiatry 2010; 167(3), 321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Joyce K, Thompson A, Marwaha S. Is treatment for bipolar disorder more effective earlier in illness course? A comprehensive literature review. Int J Bipolar Disord 2016; 4(1), 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Miklowitz DJ, Schneck CD, Walshaw PD, Garrett AS, Singh MK, Sugar CA, Chang KD. Early intervention for youth at high risk for bipolar disorder: A multisite randomized trial of family-focused treatment. Early Interv Psychiatry 2017; August 4. [DOI] [PMC free article] [PubMed]
- 88.Goldstein TR, Axelson DA, Birmaher B, Brent DA. Dialectical behavior therapy for adolescents with bipolar disorder: a 1-year open trial. J Am Acad Child Adolesc Psychiatry 2007; 46(7), 820–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Miklowitz DJ, George EL, Axelson DA, Kim EY, Birmaher B, Schneck C, Beresford C, Craighead WE, Brent DA. Family-focused treatment for adolescents with bipolar disorder. J Affect Disord 2004; 82 Suppl 1, S113–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.West AE, Weinstein SM, Peters AT, Katz AC, Henry DB, Cruz RA, Pavuluri MN. Child- and family-focused cognitive-behavioral therapy for pediatric bipolar disorder: a randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2014; 53(11), 1168–1178, 1178.e1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hirneth SJ, Hazell PL, Hanstock TL, Lewin TJ. Bipolar disorder subtypes in children and adolescents: demographic and clinical characteristics from an Australian sample. J Affect Disord 2015; 175, 98–107. [DOI] [PubMed] [Google Scholar]
- 92.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord 2000; 2(3 Pt 2), 281–293. [DOI] [PubMed] [Google Scholar]
- 93.Post RM, Altshuler L, Kupka R, McElroy S, Frye MA, Rowe M, Leverich GS, Grunze H, Suppes T, Keck PE Jr., Nolen WA. More pernicious course of bipolar disorder in the United States than in many European countries: implications for policy and treatment. J Affect Disord 2014; 160, 27–33. [DOI] [PubMed] [Google Scholar]
- 94.Post RM, Leverich GS, Kupka RW, Keck PE Jr., McElroy SL, Altshuler LL, Frye MA, Luckenbaugh DA, Rowe M, Grunze H, Suppes T, Nolen WA. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry 2010; 71(7), 864–872. [DOI] [PubMed] [Google Scholar]
- 95.Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, Bowden CL, Sachs GS, Nierenberg AA. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry 2004; 55(9), 875–881. [DOI] [PubMed] [Google Scholar]
- 96.Winokur G, Kadrmas A. A polyepisodic course in bipolar illness: possible clinical relationships. Compr Psychiatry 1989; 30(2), 121–127. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


