Abstract
Purpose:
Research by our group has shown that acupressure bands are efficacious in reducing chemotherapy-induced nausea (CIN) for breast cancer patients who expect nausea, and that their effectiveness in controlling CIN can largely be accounted for by patients’ expectations of efficacy, i.e., a placebo effect. The present research examined if the effectiveness of acupressure bands could be enhanced by boosting patients’ expectation of the bands’ efficacy.
Methods:
242 Chemotherapy-naïve patients with breast cancer who expected nausea were randomized. Arms 1 and 2 received acupressure bands, plus a relaxation MP3 and written handout that were either expectancy-enhancing (Arm 1) or expectancy-neutral (Arm 2). Arm 3 was the control without bands or MP3, and received standard care. All participants received guidelines specified antiemetics.
Results:
Peak CIN for Arms 1, 2, and 3 on a 1–7 scale was 3.52, 3.55, and 3.87, respectively (p=0.46). Because no differences were observed between Arms 1 and 2 (primary analysis), we combined these two arms (intervention) and compared them to controls for the following analyses. Significant interaction was found between intervention/control and receiving doxorubicin-based chemotherapy (yes/no) and pre-treatment anxiety (high/low). Intervention patients receiving doxorubicin had lower peak CIN than controls (3.62 vs. 4.38; p=0.02). Similarly, intervention patients with high pre-treatment anxiety had a lower peak CIN than controls (3.62 vs. 4.62; p=0.01).
Conclusions:
In breast cancer patients undergoing chemotherapy and having high CIN expectation, acupressure bands combined with a relaxation recording were effective in reducing CIN for patients who received doxorubicin or had high anxiety.
Keywords: Acupressure bands, Nausea, Anxiety, Chemotherapy, Doxorubicin, Breast Cancer
Introduction
Nausea is a prevalent side effect of chemotherapy experienced by breast cancer patients and is viewed as one of the most distressing and feared symptoms by patients, even more so than vomiting [1–3]. Because many patients do not achieve complete response with standard antiemetics, it is important to explore the additional role of non-pharmacologic interventions as an adjunct to antiemetics in the prevention and management of chemotherapy-induced nausea (CIN). Various behavioral interventions have been studied for this purpose, such as acupressure, expectation manipulation techniques, and relaxation therapy combined with guided imagery [4].
Acupressure bands apply light pressure on the skin over the P6 pressure point [5]. Although it is not clear how stimulation of the P6 pressure point reduces nausea, research done by our group and others provides evidence that acupressure bands are efficacious in reducing treatment-related nausea [5–10], and that acupressure bands are particularly effective for breast cancer patients who expect CIN [11]. Expectancy appears to play a dual role in the bands’ effectiveness, with research also showing that their effectiveness in controlling nausea can largely be accounted for by patients’ expectations of efficacy, i.e., a placebo effect [6,12,13]. In this regard, in addition to any intrinsic efficacy for relieving CIN they may have, the acupressure bands can be considered an inert device/remedy that facilitates a change in CIN expectancies. The interplay between patients’ expectation for developing CIN and their propensity to respond favorably to an intervention designed to increase positive expectations for CIN control leads to a logical question—can the effectiveness of acupressure bands in reducing CIN be enhanced by boosting patients’ expectation of the bands’ efficacy? Stated otherwise, can the placebo effect be maximized and utilized for enhanced CIN control?
This question was addressed by our group in a preliminary study examining the effects of an expectancy manipulation using acupressure bands on CIN in breast cancer patients [12]. This study showed that acupressure bands provided with expectancy-enhancing material resulted in significantly improved CIN control (Cohen’s d=0.78) in patients with high CIN expectancies, but not for patients with low CIN expectancies. Additionally, several studies have shown that CIN expectancies are important predictors for the development/and or severity of actual CIN above and beyond that from the emetogenicity of the chemotherapeutic agents as well as from other known predictors, such as age, gender, and anxiety [12,14–16]. For example, Roscoe et al. found that breast cancer patients, scheduled to receive doxorubicin-based chemotherapy, had 5-fold increase in severe CIN if they believed that they were “very likely” to experience severe CIN versus those who believed that they were “very unlikely” to do so [17].
The present study seeks to confirm and extend the findings from our preliminary study via a phase II, multicenter, three-arm, clinical trial of female breast cancer patients beginning chemotherapy and who expected to have CIN. The primary objective was to examine if acupressure bands with an expectancy-enhancing relaxation recording and a handout designed to enhance the expectation of acupressure bands’ efficacy will result in greater reduction of CIN than acupressure bands with an expectancy-neutral relaxation recording and handout. Secondary objectives were to determine potential moderators of the intervention and to assess the effectiveness of bands with relaxation recording as an adjunct to standard antiemetics in controlling CIN.
Methods
Patients
N=242 participants were recruited at four cancer clinics in three Northeastern U.S. cities between January 2013 and March 2017. Eligible participants were chemotherapy-naïve female breast cancer patients at least 18 years of age, scheduled to receive their first treatment with a chemotherapy regimen containing doxorubicin, or docetaxel with carboplatin, or docetaxel with cyclophosphamide, and who expected nausea (indicated by a response of >3 on a 5-point scale assessing expected nausea anchored at one end by 1 = “I am certain I WILL NOT have this,” and at the other end by 5 = “I am certain I WILL have this”). Patients receiving concurrent radiotherapy or interferon, or with clinical evidence of lymphedema, current bowel obstruction, or symptomatic brain metastases were excluded. The institutional review boards of the University of Rochester and each participating site approved the protocol, and subjects provided written informed consent. This trial is registered with ClinicalTrials.gov, number NCT01695993.
Study Design and Procedures
This study was a phase II, randomized, partially-blinded, placebo-controlled trial. Prior to first chemotherapy, patients were randomized to one of the three arms: 1) acupressure bands and expectancy-enhancing material (i.e., expectancy-enhancing handout concerning acupressure bands and expectancy-enhancing relaxation MP3 recording); 2) acupressure bands and expectancy-neutral material (i.e., expectancy-neutral handout concerning acupressure bands and expectancy-neutral relaxation MP3 recording); 3) control: only an expectancy-neutral handout without the mention of acupressure bands. Participants in all three groups received specified antiemetics that were in accordance with guidelines and were consistent across study sites. A computer-generated random numbers table with a randomized block size of 3 or 6 was used to assign patients to one of three arms. Randomization was stratified by recruitment site and whether patients received doxorubicin-based chemotherapy (yes/no). Researchers and treating physicians were not blinded regarding whether patients received the acupressure bands and MP3 recording. They were blinded, however, through the judicious use of sealed envelopes and earphones as to whether those patients who received the bands were assigned to the expectancy-enhancing vs. the expectancy-neutral condition.
Intervention
The complete intervention methods have been previously published [12]. Briefly, patients in Arms 1 and 2 were provided two acupressure bands (Sea-Band International, England) and were instructed to place them approximately 2 inches proximal to the distal skin crease of the wrist joint. Patients in Arms 1 and 2 were required to try the acupressure bands after randomization. They were, however, allowed to wear or remove the bands throughout the five intervention days at their own discretion.
The expectancy-enhancing handout provided to patients in Arm 1 included: 1) a one-page print-out of a bar graph with text that was printed on Cancer Center letterhead and signed by a medical oncologist (Fig. 1); and 2) a medical prescription, also signed by a medical oncologist, that instructed to “Wear Seabands for up to five days as needed to prevent or alleviate nausea.” Patients were instructed to use the acupressure bands in addition to their antiemetic regimen and not in place of it. The printout was intended to enhance the expected acupressure band efficacy, while the prescription was designed to enhance the credibility of the acupressure bands for nausea control.
Figure 1:
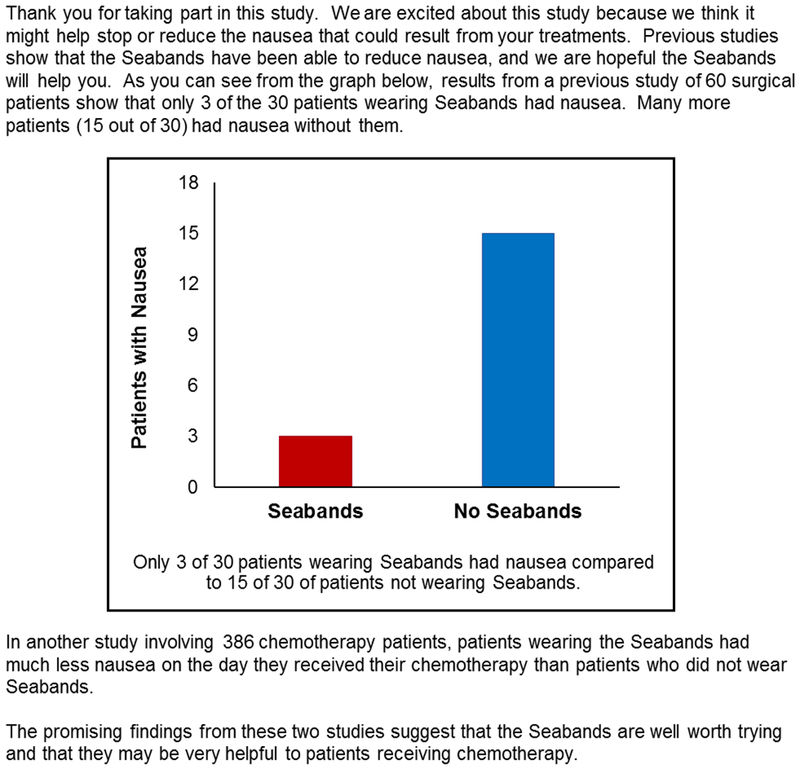
Expectancy-enhancing handout.
Figure 2:
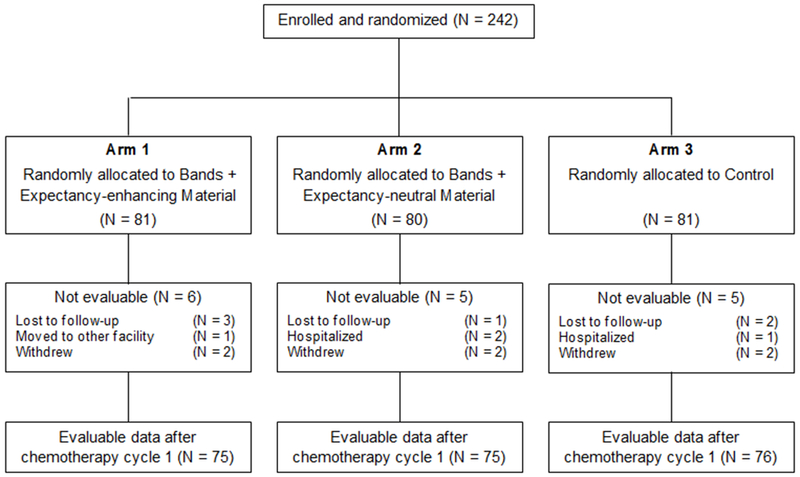
CONSORT diagram
The expectancy-neutral handout given to patients in Arm 2 was comprised of a thank you note for participating in the study and a non-prescription note that stated, “Use the acupressure bands in addition to your regular medication.” Patients in Arm 3 were given only a thank you note for participating in the study.
Both the expectancy-enhancing and expectancy-neutral relaxation music MP3 recordings were 12 minutes in length with a background of soothing flute music and relaxation instructions with guided imagery based on a published script [18,19]. Compared to the neutral version, the enhancing version had additional language inserted, less than one minute in length, concerning the efficacy of the acupressure bands and control of nausea. This was intended to strengthen patients’ beliefs that the acupressure bands would be effective by focusing patients’ attention on how effective the acupressure bands have been in reducing or eliminating nausea for other patients. Additionally, it was suggested that since the acupressure bands were helpful to others, “we think that they will be helpful to you as well.” Patients in Arms 1 and 2 were required to listen to the MP3 recording once during the randomization process and told they could listen to as much or as little as they desired throughout the study period.
Measures
On enrollment, participants provided demographic and clinical information and history of nausea from various causes. “Worst level of anxiety during the last 24 hours,” was also assessed on an 11-point scale ranging from 0–10, with higher scores indicating worst anxiety. From this, a dichotomous variable of anxiety high versus low was calculated (centered on the median value).
CIN was assessed by a self-report five-day diary [20,21] that has been used in previous large clinical trials [22,6,23]. Patients reported the severity of nausea four times each day (morning, afternoon, evening, and night) over a five-day period: starting on the day of chemotherapy and on the four following days. Nausea was rated on a 7-point scale ranging from 1 (= not at all nauseated) to 7 (= extremely nauseated). Peak CIN was defined as the highest nausea rating across the 20 nausea assessment points from the five-day diary. A score of ≥3 for peak CIN indicates moderate-severe level.
Expected worst level of CIN, assessed prior to randomization, was measured on a 5-point scale ranging from 1 (= none) to 5 (= intolerable). The expected band efficacy, assessed after randomization, was also measured on a 5-point scale ranging from 1 (= not at all effective) to 5 (= very effective). Whether patients’ expectation of band efficacy changed after the informational material was provided was also assessed on a 5-point scale ranging from 1 (= less likely to be effective) to 5 (= more likely to be effective).
A feedback questionnaire was completed by patients at the conclusion of the study period regarding the usefulness of the acupressure bands in managing CIN. The questionnaire also assessed if the bands and relaxation music reduced apprehension and whether participants would recommend them to other patients. All questions were assessed on a 5-point scale.
Statistical Analyses
In our previous study of antiemetic [22], the standard deviation for peak CIN pooled across the study arms was 1.89. Based on this number, we calculated that a sample size of 64 participants per arm would have 80% power at the 0.05 two-sided significance level to detect a peak CIN difference of 0.82 (analysis of covariance (ANCOVA), covariate-response correlation=0.5). Assuming an 11% dropout rate, we planned for 72 participants per arm.
The primary outcome variable was peak CIN after chemotherapy cycle 1. The analyses followed an intent-to-treat approach. Because 7% of the 242 patients did not provide CIN data after chemotherapy cycle 1, the analyses were conducted on data from 226 patients (completed cases). No data imputation was performed. Descriptive statistics were conducted. Percentages were calculated for categorical variables, and means and standard errors for continuous variables. To determine group differences, one-way analysis of variance (ANOVA) and independent t-tests were used for continuous variables and chi-squared tests for categorical variables.
ANCOVA was used for the primary analysis with: peak CIN as the response variable, Arm (1 or 2) as the fixed effect, expected band efficacy as the covariate, and adjusted for stratifying factors (recruitment site and doxorubicin (yes/no)). We also re-ran the model after controlling for covariates that were correlated with CIN. Spearman rank correlations were used to examine these correlations of CIN with covariates.
For the secondary analyses, the effect of acupressure bands was tested by creating two groups: bands + music (yes/no) i.e., patients who received acupressure bands with relaxation music (collapsing across Arms 1 and 2) versus who did not (control: Arm 3). To determine potential moderators of the bands’ effect on CIN, interactions with bands + music (yes/no) were tested. We found statistically significant interactions of bands + music (yes/no) with: doxorubicin (yes/no), anxiety (high/low), and doxorubicin times anxiety (all p’s≤0.03). Further analyses (ANOVA) were stratified by these moderators, with peak CIN as the response variable and bands + music (yes/no) as the fixed effect, and adjusted for recruitment site effect.
Two-sided p-value of ≤0.05 was considered statistically significant in all analysis. Analyses were performed using SPSS version 25 and SAS version 9.4 as appropriate.
Results
Patient characteristics
N=242 patients were consented and randomized; 226 patients (93% of 242 patients) completed the intervention and provided evaluable data after first chemotherapy on the primary outcome of peak CIN (Fig 2). Over the 5-day period, the average number of hours the patients used the acupressure bands was 56 (0–120) hours and the average number of times the patients listened to the relaxation music was 5 (0–31); there were no significant differences between Arms 1 and 2. No serious study-related adverse events were reported. Table 1 lists the baseline characteristics by the intervention arm. Mean age was 53 years, 88% were white, 97% were non-Hispanic or Latino, 72% were married or in a committed relationship, and 67% received doxorubicin. There were no significant differences between the groups at baseline.
Table 1:
Baseline characteristics of participants
| Characteristics | Total (N = 226) | Arm 1 (N = 75) | Arm 2 (N = 75) | Arm 3 (N = 76) | |
|---|---|---|---|---|---|
| Age | Mean (SE) | 53.0 (0.7) | 52.6 (1.2) | 53.2 (1.3) | 53.2 (1.3) |
| Range | 24–76 | 24–73 | 27–76 | 29–75 | |
| Race | White | 199 (88.1%) | 66 (88.0%) | 66 (88.0%) | 67 (88.2%) |
| Black/African American | 19 (8.4%) | 6 (8.0%) | 6 (8.0%) | 7 (9.2%) | |
| Asian | 4 (1.8%) | 1 (1.3%) | 1 (1.3%) | 2 (2.6%) | |
| Native American | 2 (0.9%) | 1 (1.3%) | 1 (1.3%) | — | |
| Unknown | 2 (0.9%) | 1 (1.3%) | 1 (1.3%) | — | |
| Ethnicity | Hispanic/Latino | 5 (2.2%) | 1 (1.3%) | 1 (1.3%) | 3 (3.9%) |
| Non-Hispanic/Latino | 220 (97.3%) | 73 (97.3%) | 74 (98.7%) | 73 (96.1%) | |
| Unknown | 1 (0.4%) | 1 (1.3%) | — | — | |
| Education | Bachelor’s or higher | 95 (42.0%) | 29 (38.7%) | 36 (48.0%) | 30 (39.5%) |
| Partial college training | 77 (34.1%) | 28 (37.3%) | 20 (26.7%) | 29 (38.2%) | |
| High school graduate or less | 54 (23.9%) | 18 (24.0%) | 19 (25.3%) | 17 (22.4%) | |
| Marital status | Married/committed relationship | 163 (72.1%) | 51 (68%) | 59 (78.7%) | 53 (69.7%) |
| Divorced/widowed/separated | 36 (15.9%) | 10 (13.3%) | 12 (16%) | 14 (18.4) | |
| Single | 27 (11.9%) | 14 (18.7%) | 4 (5.3%) | 9 (11.8%) | |
| Chemotherapy | Doxorubicin | 151 (66.8%) | 50 (66.7%) | 50 (66.7%) | 51 (67.1%) |
| Cyclophosphamide | 195 (86.3%) | 66 (88.0%) | 64 (85.3%) | 65 (85.5%) | |
| Docetaxel | 75 (33.2%) | 24 (32.0%) | 25 (33.3%) | 26 (34.2%) | |
| Carboplatin | 30 (13.3%) | 8 (10.7%) | 11 (14.7%) | 11 (14.5%) | |
| Herceptin | 31 (13.7%) | 9 (12.0%) | 11 (14.7%) | 11 (14.5%) | |
| Motion sickness | Yes | 139 (61.5%) | 45 (60.0%) | 43 (57.3%) | 51 (67.1%) |
| No | 86 (38.1%) | 30 (40.0%) | 32 (42.7%) | 24 (31.6%) | |
| Unknown | 1 (0.4%) | — | — | 1 (1.3%) | |
| Morning sickness during pregnancy | Yes | 142 (62.8%) | 50 (66.7%) | 49 (65.3%) | 43 (56.6%) |
| No | 49 (21.7%) | 13 (17.3%) | 18 (24.0%) | 18 (23.7%) | |
| Not applicable | 35 (15.5%) | 12 (16.0%) | 8 (10.7%) | 15 (19.7%) | |
| Pre-treatment anxiety | Mean (SE) | 4.4 (0.2) | 4.6 (0.3) | 4.1 (0.3) | 4.5 (0.4) |
| Pre-treatment nausea | Mean (SE) | 1.1 (0.2) | 1.4 (0.3) | 0.6 (0.2) | 1.2 (0.3) |
NOTE: Data might not add up to 100% because of rounding.
Abbreviations: SE, standard error; Arm 1, Acupressure bands + Expectancy-enhancing relaxation music and written handout; Arm 2, Acupressure bands + Expectancy-neutral relaxation music and written handout; Arm 3, Control.
Primary analyses on effects of the expectancy manipulation
As specified in the protocol, patients in Arm 1 were compared to patients in Arm 2 for the Primary Aim. N=150 of the 161 patients randomized to Arms 1 and 2 were included in the primary analysis (Fig 2). The unadjusted means for peak CIN (primary outcome) for Arms 1 and 2 were 3.52 (SE=0.20) and 3.55 (SE=0.23), respectively. Age, nausea susceptibility, motion sickness, morning sickness during pregnancy, and expected worst level of CIN were significantly associated with peak CIN (p≤0.03), while expected band efficacy was not (p=0.774).
No statistically significant group differences for peak CIN were observed between those receiving the expectancy-enhancing material and those receiving the expectancy-neutral material whether we did or did not control for above-mentioned variables that were correlated with peak CIN (both p’s>0.05; Table 2).
Table 2:
Comparison of peak chemotherapy-induced nausea by acupressure bands plus expectancy-enhancing or expectancy-neutral material
| Coefficient | Mean Difference | SE | P-value | 95% CI (Mean Difference) | ES | 95% CI (ES) |
|---|---|---|---|---|---|---|
| Arm (1 vs. 2) | ||||||
| Peak CIN | 0.002 | 0.31 | 0.996 | ‒0.61 to 0.62 | 0.001 | ‒0.32 to 0.32 |
| Peak CIN (after controlling for related covariates)a | ‒0.19 | 0.29 | 0.510 | ‒0.77 to 0.38 | ‒0.10 | ‒0.42 to 0.22 |
NOTE: Mean difference and associated statistics refer to adjusted differences between groups. Effect size (ES) is standardized mean difference (Cohen’s d). 95% CI is the lower and upper 95 % confidence limits.
Abbreviations: SE, standard error; CIN, chemotherapy-induced nausea; Arm 1, Acupressure bands + Expectancy-enhancing relaxation music and written handout; Arm 2, Acupressure bands + Expectancy-neutral relaxation music and written handout.
Covariates correlated with peak CIN for Arms 1 and 2: Age, nausea susceptibility, motion sickness, morning sickness during pregnancy, and expected worst level of CIN.
Mean expected band efficacy for Arms 1 and 2 was 3.45 (SE=0.09) and 3.25 (SE=0.10), respectively, with no significant group differences (p=0.144). We also assessed if expected band efficacy changed after patients received the expectancy-enhancing/neutral material during randomization. The means for Arms 1 and 2 were 3.95 (SE=0.09) and 3.73 (SE=0.10), respectively, with no significant group differences (p=0.122).
Secondary analyses on effects of the intervention collapsing across Arms 1 and 2
As stated in methods, because of significant interactions, these analyses are stratified. Of the 226 patients, a higher proportion of those on doxorubicin had moderate-severe levels of peak CIN than those not receiving doxorubicin (72% vs. 57%; p=0.025). Among patients receiving doxorubicin, acupressure bands with relaxation music significantly reduced peak CIN by 17% compared to controls (3.62 vs. 4.38; p=0.02). However, there was no beneficial effect of the intervention for patients not receiving doxorubicin (Table 3; Fig 3a).
Table 3:
Comparison of peak chemotherapy-induced nausea for doxorubicin and anxiety levels
| Coefficient | Mean Difference | SE | P-value | 95% CI (Mean Difference) | ES | 95% CI (ES) |
|---|---|---|---|---|---|---|
| Acupressure Bands + Relaxation Music (Yes vs. No) | ||||||
| Doxorubicin and non-doxorubicin groups | ||||||
| Peak CIN (doxorubicin group) | ‒0.76 | 0.33 | 0.020 | ‒1.41 to –0.12 | ‒0.40 | ‒0.74 to –0.06 |
| Peak CIN (non-doxorubicin group) | 0.51 | 0.46 | 0.278 | ‒0.42 to 1.43 | 0.27 | ‒0.22 to 0.75 |
| High and low pre-treatment anxiety groups | ||||||
| Peak CIN (high anxiety group) | ‒1.00 | 0.40 | 0.013 | ‒1.79 to –0.22 | ‒0.53 | ‒0.93 to –0.12 |
| Peak CIN (low anxiety group) | 0.21 | 0.36 | 0.556 | ‒0.50 to 0.93 | 0.11 | ‒0.27 to 0.50 |
| Doxorubicin with high anxiety (yes/no) | ||||||
| Peak CIN (doxorubicin with high anxiety = yes) | ‒1.38 | 0.51 | 0.008 | ‒2.39 to –0.37 | ‒0.72 | ‒1.21 to –0.22 |
| Peak CIN (doxorubicin with high anxiety = no) | 0.17 | 0.31 | 0.576 | ‒0.44 to 0.79 | 0.09 | ‒0.25 to 0.43 |
NOTE: Mean difference and associated statistics refer to adjusted differences between groups. Effect size (ES) is standardized mean difference (Cohen’s d). 95% CI is the lower and upper 95 % confidence limits.
Abbreviations: SE, standard error; CIN, chemotherapy-induced nausea.
Figure 3:
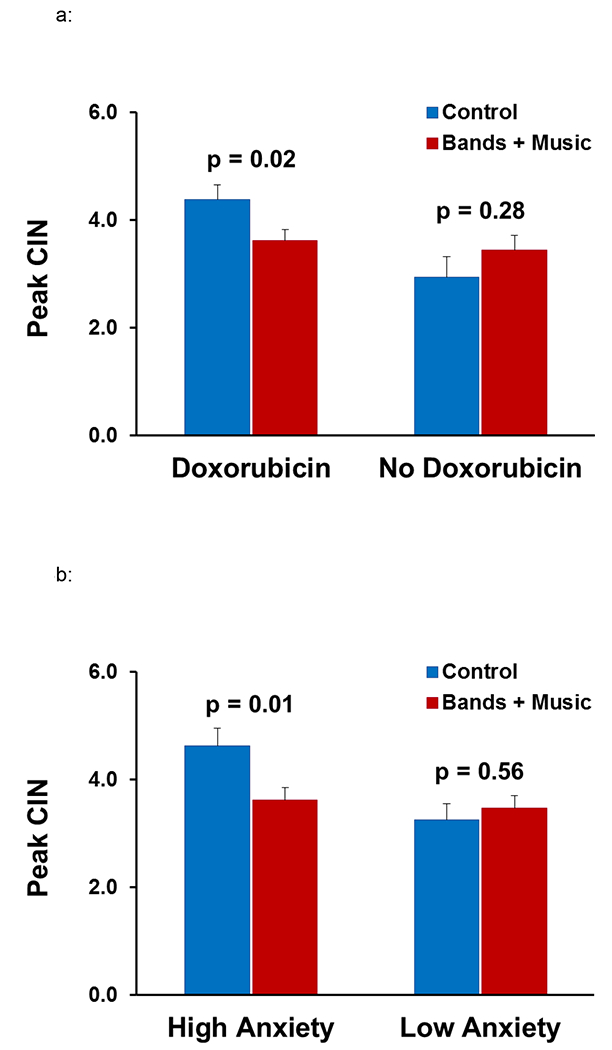
Adjusted means for peak CIN by intervention groups for (a) whether or not patients received doxorubicin-based chemotherapy, and (b) whether patients had high or low pre-treatment anxiety.
Among 226 patients, those with high pre-treatment anxiety had significantly higher peak CIN than patients with low anxiety (3.96 vs. 3.35; p=0.017). In patients with high anxiety, acupressure bands with relaxation music reduced peak CIN by 22% compared to controls (3.62 vs. 4.62; p=0.013). No positive effects of the intervention were seen for patients with low anxiety levels (Table 3; Fig 3b).
We also found that acupressure bands with relaxation music, compared to controls, reduced peak CIN by 28% for those patients who received doxorubicin and also had high pre-treatment anxiety (3.63 vs. 5.01; p=0.008; Table 3).
Satisfaction with Band
The overall satisfaction with acupressure bands and relaxation music, as assessed by the feedback question asking whether they would recommend them to other chemotherapy patients, was positive with mean responses of 3.92 and 3.59, respectively. Seventy percent of patients thought the bands were somewhat or very useful in managing CIN. Additionally, 89% said the bands reduced their apprehension of side effects, while 74% said the same for relaxation music.
Discussion
In this large, phase II RCT of female breast cancer patients with high CIN expectancies, we did not find significant difference between acupressure bands with expectancy-enhancing material designed to enhance the expectation of acupressure bands’ efficacy and acupressure bands with expectancy-neutral material, when used as an adjunct to standard antiemetics, for reducing CIN. This is contrary to the preliminary study from our group, in which manipulation of efficacy expectancies for acupressure bands resulted in improved control of CIN in patients with high CIN expectancies [12].
The failure of the study to support our primary hypothesis was likely due to the fact that our manipulation technique via relaxation music and written handout was not successful in changing these efficacy expectancies. We did not find significant group differences in expected band efficacy. Nor did we find group differences in changes in expected band efficacy after the expectancy material was provided. Additionally, we found no correlation between the expected band efficacy and CIN. This is in contrast to the generally accepted assumption that a positive expectancy is an essential element for placebo efficacy [24]. This may have occurred because the study selected for patients who expected CIN, and it is possible the magnitude of expected bands efficacy was not sufficient to affect CIN – a highly resistant symptom. Another possible explanation is that once generated, the placebo effect does not vary by dose. This possibility is supported by the findings of a study examining open-label placebo dose (one pill per day vs. four pills per day) on physical and psychological symptoms in 92 healthy undergraduates [25]. The authors found a placebo response, but did not find a dose-response on symptom improvement. They concluded that open-label placebo responses may not be dose-dependent. Their lack of a dose-response may be similar to what we found in our present study i.e., we most likely generated a placebo effect through the use of acupressure bands and relaxation MP3 recordings, but were unable to generate a dose-response effect by the additional use of written and verbal expectancy manipulations.
Interestingly, we found that acupressure bands and relaxation music, independent of the expectancy material, significantly improved CIN by 17% compared to controls for those patients who received a doxorubicin-based chemotherapy regimen, but not for patients who did not receive doxorubicin. Usually a 15−17% change in nausea is considered clinically significant improvement in many NCI-sponsored multicenter nausea trials [6,26]. A large proportion of our patients (67%) received doxorubicin, and they as a group had greater CIN than the other patients, who did not receive doxorubicin. Doxorubicin, an anthracycline, is a commonly used chemotherapeutic agent for breast cancer [27], and when used in combination with cyclophosphamide, as in 99% of our patient group, is considered highly emetogenic [28]. This is consistent with previous studies that have also shown a benefit of acupressure bands in improving CIN in patients receiving chemotherapy of moderate/high emetogenicity [5,7,8,11].
We do not truly know why the patients not receiving doxorubicin showed no benefit from the bands or music. We speculate that it may be related to a dynamic in the cancer clinic due to a general belief held by the clinic nurses that patients receiving doxorubicin will have greater CIN than other patients. We speculate that such expectancies are somehow transferred to patients, and that it is this type of transferred expectancy that increases both anxiety and CIN and is somewhat countered by the acupressure bands and relaxation music.
This speculation is supported by our finding that the acupressure bands combined with relaxation music, independent of the expectancy material, significantly reduced CIN by 22% compared to controls for those patients who had high anxiety, but not for those who had low anxiety. To the best of our knowledge, no previous study has examined the differential effects of acupressure bands and relaxation music on CIN based on patients’ level of anxiety. Anxiety is believed to contribute to CIN, partly through negative expectations, although the relationship between anxiety and negative expectations appear to be bi-directional [4]. In our overall study sample, we did find significant association of anxiety with both CIN expectancies and CIN. Previous research has also shown that acupressure is effective in decreasing anxiety in breast cancer patients [10]. Thus, indicating that for our study, the significant effect of acupressure in reducing CIN was probably through improvement in anxiety. We also found that those patients who received doxorubicin and had high anxiety saw even a greater reduction in CIN with acupressure bands and relaxation music compared to controls, further confirming the beneficial effects of the intervention in this high risk group.
The strengths of our study include the large sample size, being multicenter, and the randomized and blinded design. Nevertheless, the following limitations should be considered when interpreting the results from this study. First, the five-day diary measure of CIN is not a validated measure, although it has been previously utilized by many large nationwide clinical trials on CIN for over 20 years. Second, findings are limited to the population studied: female breast cancer patients receiving moderately or highly emetogenic chemotherapy, who expected CIN and who were predominantly white and non-Hispanic. The results of this study cannot be generalized to women with different racial and ethnic backgrounds, acupressure at acupoints other than P6, or to other methods of acupoint stimulation (e.g., electric acustimulation). Lastly, since the relaxation music was always included with the acupressure bands, we do not know the effects of the individual components. This study nonetheless has important clinical implications for an important subset of patients. That is for patients with breast cancer who expect CIN and either will receive doxorubicin and/or who have anxiety prior to treatment. For such patients, acupressure bands with relaxation music had significant beneficial effects on reducing CIN. Future research should evaluate the contributions independently from the bands and the relaxation music.
Conclusion
In breast cancer patients undergoing chemotherapy and having high expectation of CIN, an attempt to increase the efficacy of acupressure bands in controlling CIN through manipulation of expected efficacy was not successful. However, acupressure bands with relaxation music differentially impacted CIN based on patients’ type of chemotherapy regimen or level of anxiety and significantly reduced CIN for those who received anthracycline and/or had high anxiety. Considering that receiving doxorubicin and having anxiety are known predictors of CIN, it appears that our intervention had the serendipitous finding of working best for patients who needed it most. Our study provides support for the use of acupressure bands along with relaxation music as a safe and noninvasive adjunct to standard antiemetics for controlling CIN in breast cancer patients who receive anthracycline and/or have anxiety.
Acknowledgments
Funding
This study was supported by the National Cancer Institute grants R01 AT007474-01A1 and UG1 CA189961.
Footnotes
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Booth CM, Clemons M, Dranitsaris G, Joy A, Young S, Callaghan W, Trudeau M, Petrella T (2007) Chemotherapy-induced nausea and vomiting in breast cancer patients: a prospective observational study. J Support Oncol 5 (8):374–380 [PubMed] [Google Scholar]
- 2.Farrell C, Brearley SG, Pilling M, Molassiotis A (2013) The impact of chemotherapy-related nausea on patients’ nutritional status, psychological distress and quality of life. Support Care Cancer 21 (1):59–66. doi: 10.1007/s00520-012-1493-9 [DOI] [PubMed] [Google Scholar]
- 3.Russo S, Cinausero M, Gerratana L, Bozza C, Iacono D, Driol P, Deroma L, Sottile R, Fasola G, Puglisi F (2014) Factors affecting patient’s perception of anticancer treatments side-effects: an observational study. Expert Opin Drug Saf 13 (2):139–150. doi: 10.1517/14740338.2013.830710 [DOI] [PubMed] [Google Scholar]
- 4.Mustian KM, Devine K, Ryan JL, Janelsins MC, Sprod LK, Peppone LJ, Candelario GD, Mohile SG, Morrow GR (2011) Treatment of Nausea and Vomiting During Chemotherapy. US Oncol Hematol 7 (2):91–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee J, Dodd M, Dibble S, Abrams D (2008) Review of acupressure studies for chemotherapy-induced nausea and vomiting control. J Pain Symptom Manage 36 (5):529–544. doi: 10.1016/j.jpainsymman.2007.10.019 [DOI] [PubMed] [Google Scholar]
- 6.Roscoe JA, Morrow GR, Hickok JT, Bushunow P, Pierce HI, Flynn PJ, Kirshner JJ, Moore DF, Atkins JN (2003) The efficacy of acupressure and acustimulation wrist bands for the relief of chemotherapy-induced nausea and vomiting. A University of Rochester Cancer Center Community Clinical Oncology Program multicenter study. J Pain Symptom Manage 26 (2):731–742 [DOI] [PubMed] [Google Scholar]
- 7.Roscoe JA, Bushunow P, Jean-Pierre P, Heckler CE, Purnell JQ, Peppone LJ, Chen Y, Ling MN, Morrow GR (2009) Acupressure bands are effective in reducing radiation therapy-related nausea. J Pain Symptom Manage 38 (3):381–389. doi: 10.1016/j.jpainsymman.2008.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miao J, Liu X, Wu C, Kong H, Xie W, Liu K (2017) Effects of acupressure on chemotherapy-induced nausea and vomiting-a systematic review with meta-analyses and trial sequential analysis of randomized controlled trials. Int J Nurs Stud 70:27–37. doi: 10.1016/j.ijnurstu.2017.02.014 [DOI] [PubMed] [Google Scholar]
- 9.Molassiotis A, Helin AM, Dabbour R, Hummerston S (2007) The effects of P6 acupressure in the prophylaxis of chemotherapy-related nausea and vomiting in breast cancer patients. Complement Ther Med 15 (1):3–12. doi: 10.1016/j.ctim.2006.07.005 [DOI] [PubMed] [Google Scholar]
- 10.Genc F, Tan M (2015) The effect of acupressure application on chemotherapy-induced nausea, vomiting, and anxiety in patients with breast cancer. Palliat Support Care 13 (2):275–284. doi: 10.1017/S1478951514000248 [DOI] [PubMed] [Google Scholar]
- 11.Roscoe JA, Jean-Pierre P, Morrow GR, Hickok JT, Issell B, Wade JL, King DK (2006) Exploratory analysis of the usefulness of acupressure bands when severe chemotherapy-related nausea is expected. J Soc Integr Oncol 4 (1):16–20 [PubMed] [Google Scholar]
- 12.Roscoe JA, O’Neill M, Jean-Pierre P, Heckler CE, Kaptchuk TJ, Bushunow P, Shayne M, Huston A, Qazi R, Smith B (2010) An exploratory study on the effects of an expectancy manipulation on chemotherapy-related nausea. J Pain Symptom Manage 40 (3):379–390. doi: 10.1016/j.jpainsymman.2009.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alkaissi A, Stalnert M, Kalman S (1999) Effect and placebo effect of acupressure (P6) on nausea and vomiting after outpatient gynaecological surgery. Acta Anaesthesiol Scand 43 (3):270–274 [DOI] [PubMed] [Google Scholar]
- 14.Roscoe JA, Morrow GR, Colagiuri B, Heckler CE, Pudlo BD, Colman L, Hoelzer K, Jacobs A (2010) Insight in the prediction of chemotherapy-induced nausea. Support Care Cancer 18 (7):869–876. doi: 10.1007/s00520-009-0723-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colagiuri B, Roscoe JA, Morrow GR, Atkins JN, Giguere JK, Colman LK (2008) How do patient expectancies, quality of life, and postchemotherapy nausea interrelate? Cancer 113 (3):654–661. doi: 10.1002/cncr.23594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colagiuri B, Zachariae R (2010) Patient expectancy and post-chemotherapy nausea: a meta-analysis. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine 40 (1):3–14. doi: 10.1007/s12160-010-9186-4 [DOI] [PubMed] [Google Scholar]
- 17.Roscoe JA, Bushunow P, Morrow GR, Hickok JT, Kuebler PJ, Jacobs A, Banerjee TK (2004) Patient expectation is a strong predictor of severe nausea after chemotherapy: a University of Rochester Community Clinical Oncology Program study of patients with breast carcinoma. Cancer 101 (11):2701–2708. doi: 10.1002/cncr.20718 [DOI] [PubMed] [Google Scholar]
- 18.Montgomery GH, Weltz CR, Seltz M, Bovbjerg DH (2002) Brief presurgery hypnosis reduces distress and pain in excisional breast biopsy patients. Int J Clin Exp Hypn 50 (1):17–32. doi: 10.1080/00207140208410088 [DOI] [PubMed] [Google Scholar]
- 19.Rhue JW, Lynn SJ, Kirsch I (1993) Handbook of clinical hypnosis. American Psychological Association, Washington, DC [Google Scholar]
- 20.Burish TG, Carey MP, Krozely MG, Greco FA (1987) Conditioned side effects induced by cancer chemotherapy: prevention through behavioral treatment. Journal of consulting and clinical psychology 55 (1):42–48 [DOI] [PubMed] [Google Scholar]
- 21.Carey MP, Burish TG (1988) Etiology and treatment of the psychological side effects associated with cancer chemotherapy: a critical review and discussion. Psychol Bull 104 (3):307–325 [DOI] [PubMed] [Google Scholar]
- 22.Roscoe JA, Heckler CE, Morrow GR, Mohile SG, Dakhil SR, Wade JL, Kuebler JP (2012) Prevention of delayed nausea: a University of Rochester Cancer Center Community Clinical Oncology Program study of patients receiving chemotherapy. J Clin Oncol 30 (27):3389–3395. doi: 10.1200/JCO.2011.39.8123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryan JL, Heckler CE, Roscoe JA, Dakhil SR, Kirshner J, Flynn PJ, Hickok JT, Morrow GR (2012) Ginger (Zingiber officinale) reduces acute chemotherapy-induced nausea: a URCC CCOP study of 576 patients. Support Care Cancer 20 (7):1479–1489. doi: 10.1007/s00520-011-1236-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finniss DG, Kaptchuk TJ, Miller F, Benedetti F (2010) Biological, clinical, and ethical advances of placebo effects. Lancet 375 (9715):686–695. doi: 10.1016/S0140-6736(09)61706-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El Brihi J, Horne R, Faasse K (2019) Prescribing Placebos: An Experimental Examination of the Role of Dose, Expectancies, and Adherence in Open-Label Placebo Effects. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine 53 (1):16–28. doi: 10.1093/abm/kay011 [DOI] [PubMed] [Google Scholar]
- 26.Shelke AR, Roscoe JA, Morrow GR, Colman LK, Banerjee TK, Kirshner JJ (2008) Effect of a nausea expectancy manipulation on chemotherapy-induced nausea: a university of Rochester cancer center community clinical oncology program study. J Pain Symptom Manage 35 (4):381–387. doi: 10.1016/j.jpainsymman.2007.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NCCN Breast Cancer: National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology Breast Cancer, version 2, pp 1–202, 2016. [Google Scholar]
- 28.Herrstedt J, Roila F, Warr D, Celio L, Navari RM, Hesketh PJ, Chan A, Aapro MS (2017) 2016 Updated MASCC/ESMO Consensus Recommendations: Prevention of Nausea and Vomiting Following High Emetic Risk Chemotherapy. Support Care Cancer 25 (1):277–288. doi: 10.1007/s00520-016-3313-0 [DOI] [PubMed] [Google Scholar]


