Abstract
Anal canal duplication (ACD) is a rare congenital malformation, usually detected early in life. We report a case of a 67-year-old female with symptomatic ACD associated with a presacral cyst. Physical examination revealed an accessory opening located in the midline, posterior to the true anus. Imaging examinations, including fistulography, endoanal ultrasonography, and magnetic resonance imaging, revealed a blind-ending fistulous tract without connecting with the rectum and a presacral cyst posterior to the rectum. Complete surgical excision of the tract with cyst was performed through a posterior sagittal approach. Histologic examination revealed squamous epithelium lining and smooth muscle bundles, thereby confirming ACD. The postoperative course was uneventful, and the patient was doing well; no recurrence was observed 4 years after surgery. ACD can present for the first time in infants, children, and adults. Imaging examinations are useful for the diagnosis and preoperative assessment of ACD. Therefore, ACD should be considered in the differential diagnosis, even in adults, when a posterior perineal orifice is encountered, particularly in female patients. Once ACD is suspected, intense imaging inspection is recommended to visualize the ACD and associated anomalies, and surgical removal is warranted to prevent inflammatory complications or malignant changes.
Keywords: anal canal duplication, presacral cyst, endoanal ultrasonography, fistulography, magnetic resonance imaging
Introduction
Anal canal duplication (ACD) is a rare congenital malformation, with only 66 cases reported in the English-language literature since 19701-6). ACD is defined as second anal orifice, located posterior to the true anus. Most ACDs end blindly, without connecting with the rectum, and contain histologic features of a true anal canal, including squamous epithelium at the distal end and smooth muscle cells and anal glands in the canal wall7). Other diseases, such as fistula-in-ano or anorectal abscess, need to be differentiated from ACD using anatomical or pathological examination. ACDs are usually detected early in life2,3), and only a few cases remain undiagnosed until adulthood5,8). Here, we report a rare case of an adult female with ACD, review the clinical and diagnostic features, and discuss the current standard treatment for this condition.
Case Report
A 67-year-old female was referred to our hospital for the evaluation of anal pain. She was normal at birth and underwent a surgery for a perianal abscess at the age of 20 years. She began to experience intermittent anal pain 3 years prior to the presentation; however, she did not notice two anal holes. Physical examination revealed a small accessory opening, appearing as a secondary anus. The orifice was located at midline, approximately 1 cm posterior to the true anus (Figure 1a). Fistulography revealed a 2-cm-long narrow canal without connection with the rectum (Figure 1b). Endoanal ultrasonography (EAUS) with hydrogen peroxide injection revealed a brightly hyperechoic, blind-ending fistulous tract and a hypoechoic cystic mass in the superior retrorectal area (Figure 1c). Magnetic resonance imaging (MRI) revealed a multiloculated presacral cyst posterior to the rectum (Figure 1d). The clinical and radiologic features were consistent with an ACD associated with a presacral cyst.
Figure 1.
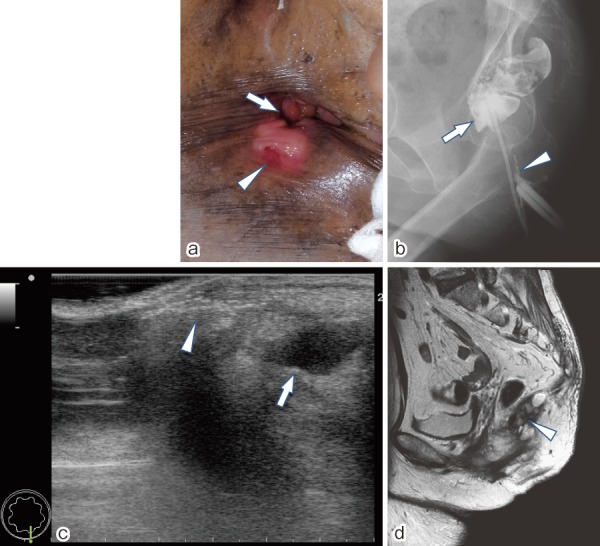
Physical and radiologic images.
(a) Physical examination shows a small, accessory opening (arrow head), located at midline, approximately 1 cm posterior to the true anus (arrow).
(b) Fistulography shows a 2-cm canal (arrow head) without connecting with the rectum (arrow).
(c) Endoanal ultrasonography shows a brightly hyperechoic blind-ending fistulous tract (arrow head) and a hypoechoic cystic mass (arrow) in the superior retrorectal area.
(d) Magnetic resonance imaging shows a multiloculated presacral cyst (arrow head) posterior to the rectum.
The patient underwent surgical excision under spinal anesthesia in the prone position through a posterior sagittal approach. The lesion circumscribing the second anal orifice was removed with incision, and the fistulous tract was separated carefully from the external anal sphincter and part of the striated muscle complex (Figure 2a). The fistulous tract was tubular, 2-cm long, and connected to the superior presacral cyst (Figure 2b). The anal opening and canal were removed in continuity with the cyst, which was adjacent to but separate from the rectum.
Figure 2.
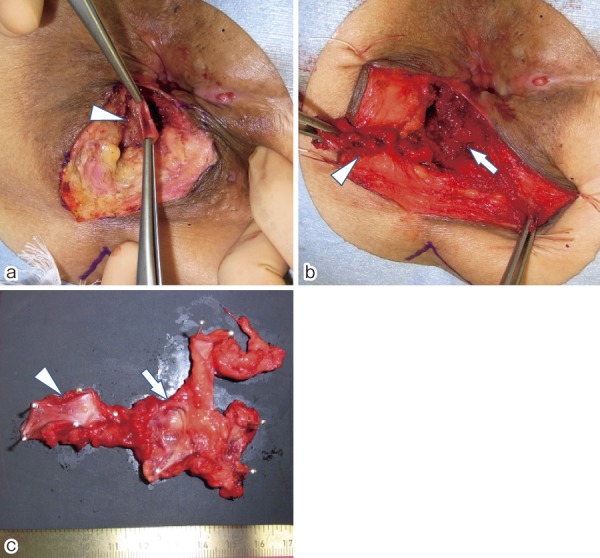
Intraoperative images.
(a) The lesion circumscribing the second anal orifice (arrow head) was removed with incision, and the fistulous tract was carefully separated from the external anal sphincter.
(b) The fistulous tract was found to be tubular, 2-cm long (arrow head), and connected with the superior presacral cyst (arrow).
(c) The resected specimen shows the distal portion is a 2.0-cm-long duct (arrow head) and is superiorly connected, via the firm restiform tissue, with a 5.0×5.0×2.0-cm cyst (arrow), filled with sebaceous material.
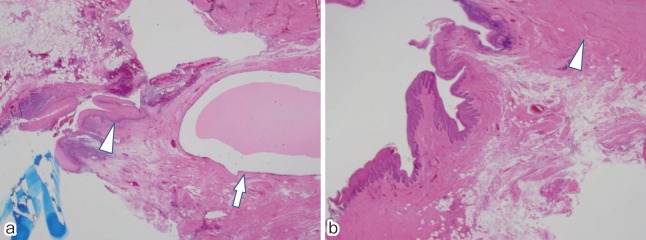
The resected specimen showed a distal, 2.0-cm-long duct superiorly connected via firm restiform tissue with a 5.0 × 5.0 × 2.0-cm cyst filled with sebaceous material (Figure 2c). Histologic examination revealed that the duct was predominantly lined by squamous epithelium and that the cyst was lined by squamous, columnar, and transitional epithelia (Figure 3a). Smooth muscle bundles were present throughout the duct wall (Figure 3b). Pathology confirmed a final diagnosis of ACD. The postoperative course was without complication, and the patient was doing well; no sign of recurrence was observed 4 years after the surgery.
Figure 3.
(a) The duct is predominantly lined by squamous epithelium (arrow head) and the cyst is lined by squamous, columnar, and transitional epithelia (arrow). (hematoxylin-eosin stain, 40×).
(b) Smooth muscle bundles are present in the wall of the duct (arrow head). (hematoxylin-eosin stain, 40×).
Discussion
Treating this case required two important clinical determinations. First, although ACD is a very rare congenital malformation that is usually detected early in infants or children, it can present for the first time in adults. Second, imaging examinations, including fistulography, EAUS, and MRI, are useful for the diagnosis and preoperative assessment of ACD in adults.
In the literature pertaining to ACD, approximately half of patients (47%) are reported to be asymptomatic. They are discovered incidentally or during the careful inspection of the perineum during the neonatal period4). In two-thirds of patients, diagnosis is made during the first year of life. In the English-language medical literature, there are no more than nine documented cases of patients older than 15 years of age, who were diagnosed with ACD2,5,8,9). Mild symptoms, such as diarrhea, constipation, anal pain, or mucous discharge, occur in 33% of patients, and more severe symptoms, such as recurrent fistulas, skin abscess, or sepsis, occur in 20% of patients. The severity of symptoms appears to increase with increase in age at presentation. Most ACDs are tubular (87%) although they occasionally contain a cystic component (13%), as observed in our patient. Approximately 36% cases are associated with other anomalies, such as teratomas, meningocele, cleft palate, and urogenital malformations. Females represent 89% of all cases; however, the reason for this predominance is unclear.
The diagnosis of ACD requires a strong clinical suspicion followed by radiological and histological confirmation. ACD should be differentiated from fistula-in-ano or anorectal abscess. Imaging modalities, such as fistulography, ultrasound, and MRI, are used to confirm the diagnosis2). Fistulography allows the evaluation of the ACD configuration (cystic or tubular), length, and connection with the anal canal3). Pelvic and abdominal ultrasound examinations are useful for evaluating the presence of associated anomalies in neonates, and MRI should be routinely used in older children and young adults because ultrasounds do not adequately visualize the intraspinal and presacral space in patients belonging to these age groups. EAUS is a reliable technique for the assessment of fistula-in-ano and is useful for distinguishing this condition from other inflammatory or tumorous conditions that affect the region around the anal canal10,11). In this study, EAUS with hydrogen peroxide injection revealed a brightly hyperechoic blind-ending fistulous tract without connection with the anal canal. Furthermore, EAUS revealed a hypoechoic cystic mass in the superior retrorectal area. Therefore, EAUS was useful for distinguishing ACD from fistula-in-ano and for visualizing associated presacral anomalies.
The main complications documented in the literature include infection risk arising from the accessary anal glands and the possibility for malignant progression6,12). Therefore, complete surgical excision through a perineal or posterior sagittal approach is considered the gold standard treatment for ACD3). Care must be taken to not excise the normal gut during complete ACD excision and to not injure the anal sphincter, which may potentially disrupt normal bowel function. After complete excision, the prognosis is excellent and the morbidity is minimal.
In conclusion, although ACD is a very rare condition, it can present for the first time not only in infants and children but also in adults. Imaging examinations, including fistulography, EAUS, and MRI, are useful for the diagnosis and preoperative assessment of ACD. When we encounter a posterior perineal orifice, particularly in female patients, ACD should be considered in the differential diagnosis, even in adults. Once ACD is suspected, intense imaging inspection should be performed to visualize the ACD and associated anomalies, and surgical removal is warranted to prevent inflammatory complications or malignant changes.
Conflicts of Interest
There are no conflicts of interest.
Source of Funding
No funding was provided for this case series.
References
- 1.Aaronson I. Anterior sacral meningocele, anal canal duplication cyst and covered anus occurring in one family. J Pediatr Surg. 1970 Oct; 5(5): 559-63. [DOI] [PubMed] [Google Scholar]
- 2.Kratz JR, Deshpande V, Ryan DP, et al. Anal canal duplication associated with presacral cyst. J Pediatr Surg. 2008 Sep; 43(9): 1749-52. [DOI] [PubMed] [Google Scholar]
- 3.Koga H, Okazaki T, Kato Y, et al. Anal canal duplication: experience at a single institution and literature review. Pediatr Surg Int. 2010 Oct; 26(10): 985-8. [DOI] [PubMed] [Google Scholar]
- 4.Van Biervliet S, Maris E, Vande Velde S, et al. Anal canal duplication in an 11-year-old-child. Case Rep Gastrointest Med. 2013 Sep; 2013: 503691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mirzaei R, Mahjubi B, Alvandipoor M, et al. Late presentation of anal canal duplication in adults: a series of four rare cases. Ann Coloproctol. 2015 Feb; 31(1): 34-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Honda S, Minato M, Miyagi H, et al. Anal canal duplication presenting with abscess formation. Pediatr Int. 2017 Apr; 59(4): 500-1. [DOI] [PubMed] [Google Scholar]
- 7.Ochiai K, Umeda T, Murahashi O, et al. Anal-canal duplication in a 6-year-old child. Pediatr Surg Int. 2002 Mar; 18(2-3): 195-7. [DOI] [PubMed] [Google Scholar]
- 8.Sinnya S, Curtis K, Walsh M, et al. Late presentation of anal canal duplication in an adolescent female--a rare diagnosis. Int J Colorectal Dis. 2013 Aug; 28(8): 1175-6. [DOI] [PubMed] [Google Scholar]
- 9.Tagart RE. Congenital anal duplication: a cause of para-anal sinus. Br J Surg. 1977 Jul; 64(7): 525-8. [DOI] [PubMed] [Google Scholar]
- 10.Engin G. Endosonographic imaging of anorectal diseases. J Ultrasound Med. 2006 Jan; 25(1): 57-73. [DOI] [PubMed] [Google Scholar]
- 11.Toyonaga T, Tanaka Y, Song JF, et al. Comparison of accuracy of physical examination and endoanal ultrasonography for preoperative assessment in patients with acute and chronic anal fistula. Tech Coloproctol. 2008 Sep; 12(3): 217-23. [DOI] [PubMed] [Google Scholar]
- 12.Dukes CE, Galvin C. Colloid Carcinoma arising within Fistulae in the Ano-Rectal Region. Ann R Coll Surg Engl. 1956 Apr; 18(4): 246-61. [PMC free article] [PubMed] [Google Scholar]