Abstract
Background
Stress reaction in bone, which may proceed to a fracture, is a significant problem in military recruits and in athletes, particularly long distance runners.
Objectives
To evaluate the evidence from randomised controlled trials of interventions for prevention or management of lower‐limb stress fractures and stress reactions of bone in active young adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (April 2004), the Cochrane Central Register of Controlled Trials (The Cochrane Library Issue 1, 2004), MEDLINE (1966 to September week 1, 2004), EMBASE, CINAHL, Index to UK Theses, reference lists of relevant articles and contacted trialists.
Selection criteria
Any randomised or quasi‐randomised trials evaluating interventions for preventing or treating lower limb stress reactions of bone or stress fractures in active young adults.
Data collection and analysis
We independently selected trials for inclusion, assessed trial quality and extracted data. Only limited data pooling was undertaken.
Main results
We included 16 trials. All 13 prevention trials involved military recruits undergoing training. Participants of two of the three treatment trials were military personnel. Ten prevention trials tested the effects of various foot inserts and other footwear modifications. While pooling of data was not possible, the four trials evaluating the use of "shock‐absorbing" boot inserts versus control found fewer stress injuries of the bone in their intervention groups. However, the only trial showing a significant benefit lacked important information about trial design. A key issue in several trials was the acceptability, in terms of practicality and comfort, of the boot inserts. Two cluster‐randomised prevention trials found no significant effect of leg muscle stretching during warm up before exercise.
Pooled data from three small but very different trials testing the use of pneumatic braces in the rehabilitation of tibial stress fractures showed a significant reduction in the time to recommencing full activity (weighted mean difference ‐33.39 days, 95% confidence interval ‐44.18 to ‐22.59 days). These results were highly heterogeneous (I squared = 90%), which is likely to reflect the underlying differences of the trials, including differences in the control group interventions and definitions of outcomes.
Authors' conclusions
The use of shock absorbing inserts in footwear probably reduces the incidence of stress fractures in military personnel. There is insufficient evidence to determine the best design of such inserts but comfort and tolerability should be considered.
Rehabilitation after tibial stress fracture may be aided by the use of pneumatic bracing but more evidence is required to confirm this.
Plain language summary
Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults
Stress fractures are a type of overuse injury. They can be very painful and debilitating. Lower limb stress fractures are common in people undergoing military training and in athletes, particularly long distance runners. Measures to prevent stress fractures include modifications to footwear and changes to training schedules. We found some evidence that shock absorbing boot inserts help prevent stress fractures during military training. It is not clear what is the best design to use. Treatment of stress fractures generally involves a long period of activity restriction. We found some evidence that pneumatic braces may speed recovery of tibial stress fracture.
Background
Spontaneous activity‐associated lower‐limb pain, particularly in the region of the tibia, is a significant problem in military recruits and in athletes, particularly long distance runners. In both groups considerable personal and economic costs are involved.
A number of pathological exercise induced conditions can give rise to pain syndromes in this population; these include soft tissue injuries to muscle, tendon, and ligaments, and disturbances in bone remodelling leading to stress reactions and stress fractures of bone. In normal activity, bone is exposed to repetitive loading at low intensity which appears to act as a stimulus for bone remodelling, but which may also result in damage at a microstructural level. Both the mechanical properties of bone and the activity of muscles in creating and attenuating load are important variables determining the level of bone remodelling activity. In normal conditions, skeletal integrity is maintained by a balance between fatigue damage accumulation and remodelling activity. High levels of stress may lead to accelerated remodelling and fatigue damage of bone. Any young active individual with activity‐induced lower extremity pain may have a stress reaction in bone, which may proceed to a fracture.
As the underlying pathophysiological process takes place over time, available imaging techniques show a range of appearances (Anderson 1996). Early changes in bone at the stage of "stress reaction" are identified by scintigraphy and by magnetic resonance imaging (MRI), but not by conventional radiography, which only shows evidence of stress fracture at a later stage. Thus, the apparent incidence of stress fracture depends on the imaging algorithm used to confirm diagnosis. Studies which accept positive scintigraphy without confirmatory radiologic changes will report a higher incidence.
In the elderly in whom involutional osteoporosis has weakened the skeleton, many fractures of the spine and hip are also attributable to fatigue damage accumulation. The prevention and management of fractures in the elderly are dealt with in other reviews. In addition, prevention of pelvic stress fractures are not covered in this review. This review concentrates on lower‐limb stress fractures in active young adults.
This is a substantive update of a review originally published in 1999 (Gillespie 1999), which had been prompted by a earlier project funded by the Ministry of Defence, UK, aimed at systematically reviewing the effectiveness of interventions used to prevent or treat musculoskeletal injuries in soldiers. Stress or fatigue fractures are a significant problem in military training, both in their frequency and consequences. However, this review extended the focus to the general population of active young adults participating in intensive physical activities who are also at risk of overuse injuries such as stress fractures.
Objectives
The objective of the review was to evaluate the evidence from randomised or quasi‐randomised controlled trials of treatments and programmes for prevention or management of lower‐limb stress fractures and stress reactions of bone in active young adults.
We set out to test the following null hypotheses.
(1) There is no difference in outcome, primarily the incidence of lower‐limb stress reactions of bone and stress fractures, between any intervention aimed at preventing lower‐limb stress fractures and stress reactions of bone in active young adults and no intervention, or any other intervention of similar aims.
(2) There is no difference in outcome between any intervention used for treating lower‐limb stress fractures and/or stress reactions of bone in active young adults and no intervention, or any other intervention of similar aims.
Methods
Criteria for considering studies for this review
Types of studies
Any randomised or quasi‐randomised trial meeting the specifications for participants, intervention or outcomes listed below was eligible for inclusion.
Types of participants
Physically active individuals of either gender from adolescence into middle age, in particular those undergoing athletic or military training. Reports which focused on elderly people with reduced bone density and children were excluded. An explicit diagnosis of lower‐limb stress fracture or stress reactions of bone was required for trials testing treatment interventions. In particular, trials involving the treatment of shin splints or medial tibial stress syndrome were excluded.
Types of interventions
Any intervention (single or as multi‐component) which had been applied to prevent or treat lower‐limb stress fractures. Preventive interventions include treatments or programmes designed to minimize the impact of risk factors (e.g. pre‐exercise stretching, rest, graduated or reduced training schedules), protective devices worn in footwear (e.g. shock‐absorbing insoles, foot orthotic devices), and calcium supplementation. Treatment interventions include rest, activity restriction and early mobilisation with bracing.
Types of outcome measures
We sought the following outcomes.
Evaluation of prevention
Occurrence and location of stress fracture, stratified by diagnostic method. (Shin splints, especially where there is no indication of serious incapacity, are treated as a separate entity and not as precursors or indicators of stress fracture.)
Incidence of other lower‐limb injuries.
Complications/adverse effects: e.g. fitness deficit, skin abrasions, other injuries.
Measures of service utilisation or resource use: e.g. costs, health care worker contacts, orthotic appliances, diagnostic procedures.
Compliance including serious discomfort and performance inhibition.
Evaluation of management
Return to training schedule.
Return to normal physical activity.
Quality of life measures.
Measures of service utilisation or resource use e.g. costs, health care worker contacts, orthotic appliances, diagnostic procedures or therapeutic procedures, length of hospital stay and degree of dependency.
Adverse effects.
Compliance.
Search methods for identification of studies
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (April 2004), the Cochrane Central Register of Controlled Trials (The Cochrane Library Issue 1, 2004), MEDLINE (1966 to September week 1 2004), EMBASE (1988 to 2004 week 36), CINAHL (1982 to September week 1 2004), Index to Theses (1990 to 2004) and Dissertation Abstracts (1990 to 2004). We also searched Current Controlled Trials at http://www.controlled‐trials.com (accessed June week 1, 2004) and the UK National Research Register at http://www.update‐software.com/national/ (up to Issue 1, 2004) for ongoing and recently completed trials. We checked Current Contents (to week 1, September 2004) and hand searched the following podiatric journals for relevant trials: British Journal of Podiatry, International Journal of Podiatric Biomechanics, Physiotherapy, Australasian Journal of Podiatric Medicine. We searched reference lists of articles, including those identified by the above searches, and related Cochrane reviews. A search for unpublished or unlisted studies was made by contacting the Medical Departments of Defence Forces in Europe and North America; initially through the assistance of the Ministry of Defence (Army) in the United Kingdom. No language restrictions were applied. In MEDLINE (OVID‐Web) subject specific terms were combined with the optimal trial search strategy (Alderson 2004a) (seeAppendix 1). Similar searches were conducted for EMBASE and CINAHL. All three databases were checked on a weekly basis.
The search for the first version of this review was conducted up to December 1997. The previous search strategy for MEDLINE (SilverPlatter) is reported in Appendix 2.
Data collection and analysis
Selection of studies
One author (KR) screened abstracts of candidate studies identified for the update and obtained full copies of potentially relevant studies to put forward for consideration. Another author (HH) performed some subsidiary searches including putting forward for consideration trials identified from other Cochrane reviews aimed at prevention of lower‐limb injuries. All three authors independently selected newly identified trials for inclusion. In addition, we checked to see if we considered the 12 trials included in the first version of the review met the inclusion criteria. As in the original version, we aimed to include all randomised or quasi‐randomised controlled trials evaluating an intervention or strategy to reduce the incidence of stress fractures in young adults undergoing athletic or military training. Thus, reports in which participants were not allocated at enrolment in a randomised or quasi‐randomised fashion into treatment or control groups were excluded.We checked the list of previously excluded studies and only listed those that appeared to meet the inclusion criteria but were excluded upon closer inspection (Alderson 2004b).
Data extraction and management
At least two authors independently extracted the trial information and data of the newly included trials using a standard pre‐designed form. One author (HH) cross checked the results presented in the original version of the review with the associated trial reports. Any discrepancies and data for newly included outcomes were checked by another author (KR). Disagreement was resolved through discussion.
Assessment of risk of bias in included studies
In this review, risk of bias is implicitly assessed in terms of methodological quality.
We independently assessed methodological quality of all the included trials using the criteria described in Table 13. Our quality scoring scheme differed from that used in the original version of the review in several ways. Firstly, the scores for the individual items A to F were altered from 1, 2, 3 to 0, 1, 2. Secondly, trials failing to provide any description of the method of randomisation were given a score of one (Cochrane code B) instead of zero for item A. Thirdly, those trials were intention‐to‐treat analysis was clearly not done, such as the omission from the analysis of the results of non‐compliers, scored zero for item B. Fourthly, additional criteria were added to inform the scoring for item D (comparability of baseline data). Lastly, some guidance was given for scoring of item G (outcome assessment) for treatment trials. Disagreement was resolved through discussion, aided by the use of a discrepancies form.
1. Methodological quality assessment scoring scheme.
| Items | Scores | Notes |
| A. Was the assigned treatment adequately concealed prior to allocation? | 2 = method did not allow disclosure of assignment. 1 = small but real chance of disclosure of assignment or unclear (states random but gives no description (individual randomisation)). 0 = quasi‐randomised or open list/tables; or cluster randomisation with no description of randomisation. | Cochrane code (see Handbook): Clearly Yes = A; Not sure = B; Clearly No = C. |
| B. Were the outcomes of participants who withdrew described and included in the analysis (intention to treat)? | 2 = withdrawals well described and accounted for in analysis: primary analysis based on all cases as randomised. 1 = states numbers and reasons for withdrawal, but analysis unmodified/possible. 0 = not mentioned or intention to treat analysis clearly not done. | |
| C. Assessment of outcome. Were assessors of outcome blinded to treatment status? | 2 = action taken to blind assessors, or outcomes such that bias is unlikely. 1 = small or moderate chance of unblinding of assessors, or some blinding of outcomes attempted. 0 = not done or not mentioned. | |
| D. Comparability of treatment and control groups at entry. | 2 = unconfounded; good comparability of groups or confounding adjusted for. 1 = confounding small, mentioned but not adjusted for, or comparability reported in text without confirmatory data. Inclusion criteria (e.g. all male participants) indicate comparability for the main confounders 0 = large potential for confounding, or not discussed. | The principal confounders considered for prevention trials were sex, age, previous overuse lower‐limb injury and prior physical activity profile. The principal confounders considered for treatment trials were sex, age, and duration, location and severity of stress fracture. |
| E. If feasible, was a placebo treatment assigned as part of the randomisation? | 2 = Yes. 1 = Not feasible. 0 = No. | |
| F. Were inclusion and exclusion criteria clearly defined? | 2 = clearly/well defined. 1 = poorly/inadequately defined. 0 = not defined. | |
| G. Methods of assessment of outcome. | Prevention trials, for stress fracture: 3 = pain, discrete bone scan changes, confirmatory discrete radiological changes. 2 = pain, bone scan changes at one or more sites in the lower limb. 1 = pain compatible with stress fracture or other exercise associated lower limb pain; clinical decision. 0 = not stated. Treatment trials: 3 = optimal (comprehensive, well defined, active and sufficiently long follow‐up) 2 = active and adequate but not optimal 1 = active but inadequate 0 = not defined, inadequate and passive |
Data synthesis
For the studies randomised by individuals, relative risks (RR) with 95% confidence intervals (CI) were calculated for dichotomous outcomes and mean differences with 95% confidence intervals were calculated for continuous outcomes. Some changes to the results presented for the trials included in the first version of the review reflect the use of relative risks instead of Peto odds ratios. Very limited data pooling was undertaken: in both instances, weighted mean differences (WMD) with 95% confidence intervals were calculated. Heterogeneity was tested using chi squared and I squared statistics. We choose the random‐effects model because of high heterogeneity.
Some of the included trials used cluster randomisation. When allocation is by a group of participants, such as training platoon, unit of analysis errors are likely to result from the presentation of outcome by the individual participants. The risk of injury of such individuals cannot be considered independent of the cluster unit (team/platoon). Using statistical methods that assume, for example, that all participants' chances of injury are independent ignores the possible similarity between outcomes for participants within the same platoon. This may underestimate standard errors and give misleadingly and inappropriately narrow confidence intervals, leading to the possibility of spurious positive findings (Bland 1997). Whilst we have presented the overall results of these trials where available, we have indicated these as cluster‐randomised trials and suggest cautious interpretation. Clustered studies were not pooled.
Results
Description of studies
Of 24 additional studies identified for this review update, eight (Allen 2004; Bensel 1986; Finestone 1999; Finestone 2004a; Finestone 2004b; Mundermann 2001; Pope 1998; Pope 2000) were included, 13 (Amako 2003; Callison 2002; Clark 1989; Ekenman 2002; Gray 2003; Hartig 1999; Larsen 2002; Popovich 2000; Sherman 1996; Thompson 2004; Tokki 2002; Van Mechelen 1993; Wedderkopp 1999) were excluded, one (Owen 2004) was listed as an ongoing study and two (London 2005; Wang 2001) were placed in 'Studies awaiting assessment' pending further information.
Of the 12 trials included in the original review, we excluded four (Giladi 1985; Nissen 1994; Scully 1982; Smith 1985). For each of the three prevention trials (Giladi 1985; Scully 1982; Smith 1985), we considered that there was no/insufficient indication of the use of random or quasi‐random methods for allocation of groups of individuals to the interventions under test. We excluded Nissen 1994 because it investigated the effect of low‐energy laser treatment of medial tibial stress syndrome and not tibial stress fractures. We also considered a further two studies (Schwellnus 1990; Schwellnus 1992) as candidates for exclusion. The previous version of this review (Gillespie 1999) drew attention to these two trials, noting that they "were reported separately without any clear indication in the text of linkage, but it is evident from the data that the same control group has been used in each study." Gillespie 1999 considered that Schwellnus 1992, included "as the only comparative study we have found which evaluates calcium supplements in the prevention of stress fractures and reactions", "is a non‐randomised controlled clinical trial" and noted "the possibility that the control and experimental populations may not have been sampled at the same time". We consider the same could apply to Schwellnus 1990. However, given a concurrent trial involving all three groups is also a possibility, we have retained both trials for now. Repeated requests for clarification have been sent to the lead author.
In all, 16 trials were included. Thirteen trials reported outcomes of interventions to prevent stress reactions of bone or stress fractures. Three trials reported the evaluations of treatments for stress reactions or stress fractures. The details of each of these studies are reported in the 'Characteristics of included studies' table. The 'Characteristics of excluded studies' table gives the reasons for excluding 21 studies. We removed five previously excluded studies from the review: three were cohort studies, one was a before and after study, and one was a study involving the same population as that of an already included trial (Milgrom 1985).
Preventive strategies All the studies identified in this category had been carried out in military recruits, in five countries. Four studies (Andrish 1974; Milgrom 1985; Mundermann 2001; Schwellnus 1990) compared the effect of training in boots/shoes into which "shock absorbing" insoles/orthoses had been inserted with training in boots/shoes alone. Bensel 1986 compared two types of cushioning inserts/insoles (urethane foam with fibre backing versus moulded grid‐like network with a smooth cover) with standard inserts in standard US army boots. Gardner 1988 compared an insole made of a visco‐elastic polymer with a nylon mesh insole. Finestone 1999 compared semi‐rigid versus soft custom‐made biomechanical foot orthoses versus standard insoles worn inside modified infantry boots. Finestone 2004a and Finestone 2004b, which were reported in the same article, used the same study design but tested different comparisons and were conducted at different army bases. Finestone 2004a compared custom‐made versus prefabricated soft foot orthoses for standard army boots. Finestone 2004b compared custom‐made mechanical semi‐rigid foot orthoses versus prefabricated semi‐rigid foot orthoses for standard army boots. Table 14 summarises the characteristics of the foot orthoses used in the above trials. Milgrom 1992 reported training in modified baseball 'high top' shoes rather than in military boots. A graduated running programme with reduced running in the first two weeks of training was also tested in Andrish 1974. Two studies reported on the effect of pre‐exercise stretching (Pope 1998; Pope 2000). One study (Schwellnus 1992) reported an evaluation of the impact of calcium supplements.
2. Characteristics of foot orthotics (FOs) or insoles tested in the included trials.
| Study ID | Intervention | Material | Subtalar neutral? | Custom‐made? |
| Andrish 1974 | (a) Use of 1.3 cm thick foam rubber heel pad | Foam rubber | No | Probably no |
| Bensel 1986 | (a) Urethane foam backed with fibre‐board boot insert | Urethane foam with fibre board backing | No | Probably yes |
| (b) "Moulded network of lever‐like projections attached at their back to material in the form of a grid." Smooth grid surface of boot insert closest to the foot | Not stated | No | Probably yes | |
| (c) Standard ventilating boot insert (control) | Multi‐layered plastic mesh with nylon cover | No | Probably no | |
| Finestone 1999 | (a) Custom‐made semi‐rigid foot orthoses | Polypropylene with neutral rearfoot posts | Yes | Yes |
| (b) Custom‐made soft foot orthoses | 3 layers of polyurethane (80, 60, 80 densities) | Yes | Yes | |
| (c) Simple insoles | Cross‐linked polyortholene foam | No | No | |
| Finestone 2004a | (a) Custom‐made soft foot orthoses | Close‐cell polyethylene foam | Yes | Yes |
| (b) Prefabricated soft foot orthoses | Closed‐cell cross‐linked polyethylene foam | No | No | |
| Finestone 2004b | (a) Custom‐made semi‐rigid foot orthoses | Ortholene with acrylic rearfoot posts. Top cover: EVA | Yes | Yes |
| (b) Prefabricated semi‐rigid foot orthoses | Ortholene with acrylic rearfoot posts. Top cover: EVA | No | No | |
| Gardner 1988 | (a) Shock‐absorbent polymer insoles | Closed cell polyurethane foam | No | No |
| (b) Standard mesh insoles (control group) | Not stated | No | No | |
| Milgrom 1985 | (a) "Military stress orthotic" insole | Polyofelin shell; 30‐styrene butadiene rubber rearfoot post. Top cover: open cell polyurethane foam | Probably yes | No |
| Mundermann 2001 | (a) Choice of 6 shoe inserts | Not stated | Probably no | Probably yes |
| Schwellnus 1990 | (a) Neoprene ("shock absorbing") insoles | Neoprene‐impregnated nitrogen bubbles. Top cover of nylon | No | Probably no |
Treatment programmes All three studies, two (Allen 2004; Slatyer 1995) involving military recruits and the other (Swenson 1997) involving athletes, investigated a planned return to activity with the symptomatic limb supported by a pneumatic ankle foot orthosis (Aircast Brace).
Risk of bias in included studies
The methodological quality of these studies, as reported, was generally poor. The scores for each category for each study are listed in the 'Characteristics of included studies' table. The scores for the 13 prevention trials are summarised in Table 15; those of the three treatment trials are summarised in Table 16. Comments on various aspects of trial quality are given below.
3. Quality assessment scores for prevention studies.
| Study id | Item A | Item B | Item C | Item D | Item E | Item F | Item G |
| Andrish 1974 | 1 | 0 | 0 | 1 | 1 | 1 | 3 |
| Bensel 1986 | 1 | 1 | 0 | 1 | 0 | 1 | 0 |
| Finestone 1999 | 1 | 0 | 0 | 1 | 2 | 1 | 2 |
| Finestone 2004a | 1 | 1 | 0 | 1 | 2 | 1 | 0 |
| Finestone 2004b | 1 | 1 | 0 | 1 | 2 | 1 | 0 |
| Gardner 1988 | 0 | 2 | 2 | 1 | 0 | 1 | 3 |
| Milgrom 1985 | 1 | 0 | 0 | 1 | 1 | 1 | 2 |
| Milgrom 1992 | 1 | 2 | 0 | 1 | 1 | 1 | 2 |
| Mundermann 2001 | 1 | 1 | 0 | 1 | 0 | 1 | 0 |
| Pope 1998 | 0 | 2 | 0 | 1 | 2 | 2 | 2 |
| Pope 2000 | 0 | 2 | 1 | 1 | 0 | 2 | 2 |
| Schwellnus 1990 | 1 | 1 | 0 | 1 | 1 | 1 | 3 |
| Schwellnus 1992 | 1 | 1 | 2 | 1 | 0 | 2 | 3 |
4. Quality assessment scores for treatment studies.
| Study ID | Item A | Item B | Item C | Item D | Item E | Item F | Item G |
| Allen 2004 | 1 | 1 | 2 | 2 | 1 | 2 | 2 |
| Slatyer 1995 | 2 | 2 | 0 | 1 | 1 | 2 | 2 |
| Swenson 1997 | 1 | 1 | 0 | 0 | 1 | 2 | 2 |
Prevention trials In no study was the assigned treatment clearly and adequately concealed prior to allocation (item A). In three trials (Gardner 1988; Pope 1998; Pope 2000), the experimental and control interventions were clearly allocated by cluster randomisation (by the training platoon to which the recruit had been assigned). Again, we draw attention to the shared control group of Schwellnus 1990 and Schwellnus 1992 and the lack of clarification on study design in these two trials.
Serious intention‐to‐treat problems (item B) were found in Andrish 1974, where the results of platoons found not to be carrying out the allocated prophylactic regimens were transferred to the control group. Intention‐to‐treat analysis was not carried out in Finestone 1999 or Milgrom 1985. Full results in Finestone 1999 were only provided for completers, including those that wore orthotics throughout. Milgrom 1985 excluded the results of 30 participants who discontinued use of their orthotics. Though not scored, the very high losses to follow up and/or analyses in several trials (Finestone 1999: 51%; Mundermann 2001: 62%) are likely to be a source of serious bias.
In two studies (Gardner 1988; Schwellnus 1992) the outcome assessors were clearly blinded to participant status; secure blinding was not confirmed in Pope 2000. In the majority of studies, some comparability of treatment and control groups at entry (item D) was assumed based on the similarity evident from the shared characteristics of the study population: for example, male recruits who had passed a fitness test establishing suitability for military training. The method of diagnosis of stress fracture (item G) was not described in two trials (Finestone 2004a; Finestone 2004b), and was based on clinical examination only in Bensel 1986 and self‐reported questionnaires in Mundermann 2001. Radiological confirmation of the presence of stress fracture or stress reaction in cortical bone was required in four trials (Andrish 1974; Gardner 1988; Schwellnus 1990; Schwellnus 1992) and was an option in three other trials (Milgrom 1985; Pope 1998; Pope 2000). Scintigraphic (bone scan) changes at one or more sites in the lower limb were measured in five trials (Finestone 1999; Milgrom 1985; Milgrom 1992; Pope 1998; Pope 2000). Thus, the term "stress fracture" in these papers was assumed to also include stress reactions of bone without fracture.
Treatment trials Allocation (item A) was adequately concealed in one of the three treatment studies (Slatyer 1995). The other two trials (Allen 2004; Swenson 1997) provided insufficient information to judge if this was achieved. Just over one third of participants (35%) were excluded from Allen 2004. Though the high loss to follow up is likely to be a source of serious bias in this trial, Allen 2004 claimed that the available data on the drop outs showed similarity with that of those completing the trial. There was assessor blinding (item C) in Allen 2004.
Effects of interventions
The three trials (Gardner 1988; Pope 1998; Pope 2000) that used cluster randomisation presented results, as if randomised by individuals rather than groups, that did not account for the effect of clustering. Exploratory analyses have been presented in the graphs, but the confidence intervals shown are an underestimate and thus narrower than they should be. We have thus not pooled data from these trials.
Prevention Insoles/orthotics or other footwear modifications Insoles/orthotics versus control Thirty of the 143 recruits who were allocated orthotics in Milgrom 1985 discontinued using these within 14 days because they could not "accommodate" to them.Injury data for these recruits were not provided in the report nor were the exact numbers of participants in the two groups who had sustained a stress fracture. There was no specific report on compliance in Andrish 1974, Mundermann 2001 or Schwellnus 1990. However, the results of platoons found not to comply with using heel pads (or the other prophylactic regimens) in Andrish 1974 were transferred to the control group. Random inspections to ensure compliance were carried out in Schwellnus 1990 and a questionnaire on wear and comfort sent to 143 of the 237 participants (60%) of the insoles group. This found that three trainees had worn their insoles for less than three days per week; that five found their insoles uncomfortable and that 32 considered their insoles needed replacing after nine weeks of training.
Andrish 1974 reported two tibial stress fractures (radiographically confirmed), both which occurred in the control group (heel pads: 0/807 versus no heel pads: 2/1753). The results of this trial are not pooled due to the potential for serious bias resulting from a failure to conduct intention‐to‐treat analysis. Based on an assumption of it being a trial involving random allocation to individual recruits, the stress fracture results of Schwellnus 1990 comparing the use of an insole in military training footwear are presented graphically (see Graph 01.01: relative risk (RR) 0.17, 95% confidence interval (CI) 0.1 to 2.79). Graph 01.02, which includes data from Milgrom 1985 and Mundermann 2001, shows a generally lower incidence of stress injury of the bone in the tibia and foot bones in those allocated insoles. Overall, there were significantly fewer people with injuries, including overuse injuries, in the insoles group in Schwellnus 1990 (see Graph 01.03). Comparisons of different insoles Five studies (Bensel 1986; Finestone 1999; Finestone 2004a; Finestone 2004b; Gardner 1988) compared different types of insole.
Cushioning/shock absorbing insoles/orthotics versus standard mesh insoles (see Graphs 02.01 to 02.05) Two types of cushioning insoles (inserts) were compared with standard insoles in regulation US army boots in one study (Bensel 1986). There were no statistically significant differences in the numbers with tibial, calcaneal or metatarsal stress reactions in those participants wearing cushioned insoles compared with those wearing standard insoles (e.g. calcaneal stress reactions: RR 1.15, 95% CI 0.61 to 2.19). Separate data were provided for 29 other types of lower‐limb injury or complaint. An overall impression of the injuries sustained is provided by the numbers attending a medical facility over the training period, the numbers with activity restriction and the numbers discharged for medical reasons. The combined results of the cushioned insoles groups compared with the standard insoles group revealed no statistically significant differences in those attending a medical facility (RR 0.95, 95% CI 0.77 to 1.17), with activity restriction (RR 0.91, 95% CI 0.67 to 1.23), nor in those discharged for medical reasons relating to lower‐limb complaints (RR 3.12, 95% CI 0.94 to 10.31). Similar numbers (around 70%) of participants in the three groups reported having always worn the insoles in their boots. There was no statistically significant difference between those wearing cushioned insoles and those wearing standard insoles who rated their insoles as uncomfortable Gardner 1988 showed no significant difference between visco‐elastic insoles and mesh insoles in stress fracture rates (see Graph 03.01: RR 1.16, 95% CI 0.62 to 2.20) in the number of stress fractures when analysed on the assumption of individual randomisation. Similar numbers sustained other serious lower extremity injuries in the two groups (101/1557 versus 97/1468) in Gardner 1988.
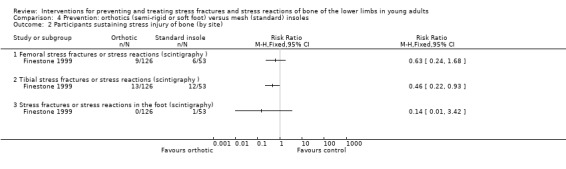
The reduction in the stress fracture rates between participants of Finestone 1999 completing the trial who used custom‐made semi‐rigid or soft‐foot orthoses and those who had standard insoles reached borderline statistical significance (see Graph 04.01: RR 0.52, 95% CI 0.27 to 1.00 ); the reduction in tibial stress fracture in the orthotics groups was statistically significant (see Graph 04.02). Similar proportions of the two groups found the orthotics or insoles intolerable (see Graph 04.03); 61 versus 30 trial participants, assigned orthotics or insoles respectively, were excluded from the preceding stress fracture analyses. There were no data for other injuries or costs.
Urethane versus special grid‐like mesh insoles (see Graphs 05.01 to 05.05) This comparison was tested by one study (Bensel 1986). There were no statistically significant differences in the numbers with tibial, calcaneal or metatarsal stress reactions in those participants wearing cushioned insoles compared with those wearing standard insoles (for example, calcaneal stress reactions: RR 0.67, 95% CI 0.34 to 1.35). There were no statistically significant differences between the two groups in those attending a medical facility (RR 1.12, 95% CI 0.88 to 1.42) or with activity restriction (RR 1.16, 95% CI 0.82 to 1.64). However, significantly more participants wearing urethane insoles were discharged for medical reasons (RR 2.66, 95% CI 1.05 to 6.71). Similar numbers (around 70%) of participants in the two groups reported having always worn the insoles in their boots. There was no statistically significant difference between the two group in the number of participants who found their insoles uncomfortable.
Semi‐rigid versus soft‐foot orthoses (see Graphs 06.01 to 06.03) Finestone 1999 showed no statistically significant difference in the stress fracture rates between participants completing the trial who wore custom‐made semi‐rigid orthoses and those who wore soft biomechanical foot orthoses (RR 1.47, 95% CI 0.59 to 3.66). However, four times as many people assigned semi‐rigid orthoses found these intolerable (RR 3.96, 95% CI 2.21 to 7.09); 49 versus 12 trial participants, assigned semi‐rigid versus soft orthoses respectively, were excluded from the preceding stress fracture analyses. There were no data for other injuries or costs. Custom‐made versus prefabricated soft foot orthoses for standard army boots Finestone 2004a showed no statistically significant difference in the rates of stress fracture of the foot between participants with complete clinical follow up who were provided with custom‐made soft foot orthoses for their infantry boots versus those provided with prefabricated soft foot orthoses (RR 1.04, 95% CI 0.57 to 1.91). Similarly, there were no statistically significant differences between the two groups in recruits sustaining foot problems or ankle sprains (see Graph 07.02). However, significantly fewer participants gave up wearing their orthoses in the custom‐made orthosis group (RR 0.66, 95% CI 0.51 to 0.85). The cost ratio of the custom‐made to the prefabricated orthoses, which were from the same manufacturer, was reported as approximately four to three.
Custom‐made mechanical semi‐rigid orthoses versus prefabricated semi‐rigid foot orthoses for standard army boots Finestone 2004b showed no statistically significant difference in the rates of stress fracture of the foot between participants with complete clinical follow up who were provided with custom‐made mechanical semi‐rigid foot orthoses for their infantry boots versus those provided with prefabricated semi‐rigid foot orthoses (RR 1.30, 95% CI 0.67 to 2.50). Similarly, there were no statistically significant differences between the two groups in recruits sustaining foot problems or ankle sprains (see Graph 08.02). More participants gave up wearing their orthoses in the custom‐made orthosis group but the difference between the two groups was not statistically significant (RR 1.41, 95% CI 0.97 to 2.05). The cost of the custom‐made mechanical semi‐rigid orthoses, which was from the same manufacturer as the prefabricated orthoses, was approximately twice that of the prefabricated orthoses (and four times that of the prefabricated soft foot orthoses in Finestone 2004a).
Basketball shoes versus military boots A comparison between training in modified basketball shoes and normal military boots (Milgrom 1992) was inconclusive in respect of the total number of stress fractures and reactions (see Graph 09.01: RR 1.21, 95% CI 0.85 to 1.72: ) and overall overuse injuries of the lower limb (RR 1.00, 95% CI 0.93 to 1.06). However, there were no participants wearing basketball shoes with stress fractures in the foot (see Graph 09.02: 0/187 versus 7/203) and training in basketball shoes was associated with a significant reduction in the incidence of other foot overuse injuries (RR 0.64, 95% CI 0.42 to 0.97). Similar proportions of recruits responding to a questionnaire indicated a preference to train in the same footwear as allocated in the trial (104/170 versus 103/176). However, the basketball shoes were less durable (61% allocated basketball shoes required at least one change of shoes during the training period) and tended to absorb water (31% of questionnaires for this group indicated ground wetness was a problem).
Reduction in the frequency and intensity of running Andrish 1974 tested the effects of a graduated running programme featuring a reduced running schedule in the first two weeks of military training. However, the results of platoons found not to comply with the prophylactic regimens tested in this trial were transferred to the control group. Andrish 1974 reported no stress fractures in the modified running schedule group and one tibial stress fractures (radiographically confirmed) in the control group (intervention group: 0/217 versus control group: 1/1453). However, these results are not presented graphically since there is a potential for serious bias resulting from a failure to conduct intention‐to‐treat analysis in this trial.
Pre‐exercise leg muscle stretching Calf muscle stretching was compared with arm muscle stretching during warm up in Pope 1998, and complex stretching (six leg muscles including the calf muscles) was compared with control (no stretching) during warm up in Pope 2000. Since both trials involved cluster randomisation, their power to detect differences was reduced and thus caution in interpretation is advised. However, irrespective of the trial design, there were no statistically significant differences between the stretching and control groups in the overall numbers of stress fractures sustained in either the calf stretching trial (8/549 versus 8/544; RR 0.99, 95% CI 0.37 to 2.62) or the six leg muscle stretching trial (47/735 versus 42/803; RR 1.22, 95% CI 0.82 to 1.83). A breakdown by site of stress fracture is presented in Graph 10.02. There were also no statistically significant differences in overall numbers of lower‐limb injuries recorded in the two trials (see Graph 10.03). It should be noted that the method used to record injury ‐ primary injury only noted ‐ meant that some stress fractures may not have been counted in those with multiple injuries. Oral calcium supplements Based on an assumption of it being a trial involving random allocation to individual recruits, the stress fracture results of Schwellnus 1992, which evaluated the administration of calcium supplements, showed no statistically significant difference between the two groups (see Graph 11.01: RR 0.33, 95% CI 0.04 to 2.52). The sole stress fracture in the calcium group was a tibial fracture (see Graph 11.02). Overall, there were significantly fewer people with injuries, including overuse injuries, in the calcium group in Schwellnus 1992 (see Graph 11.03).
Treatment Rehabilitation in pneumatic brace The context and control group interventions of the three trials (Allen 2004; Slatyer 1995; Swenson 1997) testing the effects of rehabilitation of tibial stress fractures using a pneumatic brace were markedly different. The participants of Allen 2004 were active duty US soldiers; those of Slatyer 1995 were Australian military recruits undergoing training; and those of Swenson 1997 were competitive and recreational athletes in the USA. Control group participants of Allen 2004 were prescribed the same activity profile and rehabilitation programme as those in the brace group; the only difference being that they did not wear the brace during daily activities and rehabilitation. Control group participants in Slatyer 1995 were given six weeks convalescent leave with guidelines for a non‐impact exercise programme, whereas those of Swenson 1997 were prescribed non‐impact activities and began a gradual return to activity after three pain‐free days. Allen 2004 found no significant difference between the two groups in the mean time to starting functional progression (see Graph 12.01: mean difference 1.10 days, 95% CI ‐6.24 to 8.44 days); whereas Swenson 1997 reported a significantly earlier return to light activity in the brace group (see Graph 12.01: mean difference ‐23.00 days, 95% CI ‐42.26 to ‐3.74 days). As shown in Graph 12.01, these results are significantly heterogeneous (I squared = 81%). It is noteworthy that, in contrast to Swenson 1997, several participants of Allen 2004 were able to start functional progression from the start (day 0). Pooled data from all three trials showed a significant reduction in the mean number of days to recommencing full activity (see Graph 12.02: weighted mean difference ‐33.39 days, 95% CI ‐44.18 to ‐22.59 days). These results were highly heterogeneous (I squared = 90%), which is likely to reflect the underlying differences, including definitions of outcomes. In particular, the results of Slatyer 1995 reflect a context‐specific threshold for returning to training. The results of Slatyer 1995 were confounded by the greater demotivation experienced by the recruits assigned to the control group: ultimately this could have contributed to the significantly greater numbers of recruits in the control group being discharged from the army on medical grounds (see Graph 12.03: RR 0.53, 95% CI 0.31 to 0.93). While there was probably full/good compliance with brace use and rehabilitation in the brace group of Slatyer 1995, there were clear indications that compliance with rehabilitation was less good in the control group, who were unsupervised whilst on convalescent leave. Slatyer 1995 estimated that the mean cost of managing an established tibial stress fracture in the context of the Australian army was $920 per person in the brace group and $1962 in the control group; the component contributing the main difference was rehabilitation costs. Despite the adjustment made after a pilot study, various side effects of brace use were reported (e.g. fitting problems: 11 recruits; local pain: 12; chafing: 30; cutting into skin: 23; skin rashes: common problem, also reported in control group). Swenson 1997 reported that none of the brace group athletes considered their brace impeded performance. In contrast, Allen 2004 noted, but did not quantify, that brace group participants "frequently complained" that they found the brace cumbersome and uncomfortable for extended wear and cosmetically displeasing. Allen 2004 referred to reports of low compliance with brace use outside the weekly evaluations.
Discussion
One key issue in this review is the methods of randomisation used in the trials. Especially prior to initiatives such as those behind the CONSORT statement (Begg 1996; Moher 2001), description of the method of allocation of trial interventions is frequently incomplete or absent in trial reports. It is often hard to judge whether randomisation (or quasi randomisation) actually occurred, let alone whether concealment of allocation was achieved. Cluster‐randomised controlled trials present an additional level of complexity. In some cases, while trial participants were effectively or actually randomly placed in different units/clusters, the key information on the mode of allocation of treatment interventions, whether to groups or individuals, is missing. We judged that three previously included studies (Giladi 1985; Scully 1982; Smith 1985) were not randomised studies: this was based on obtaining further information in Giladi 1985 and on a stricter application of the review inclusion criteria for the other two trials. The consequences of excluding these trials are minimal in terms of the amount of reliable evidence lost. For instance, just one stress fracture was reported in Smith 1985, which examined the effects of insoles. We remain concerned about the inclusion and interpretation of Schwellnus 1990 and Schwellnus 1992, which, as explained above, share the same control group. If these two trials report on a study involving concurrent intervention groups, a further question is whether the allocation was at a cluster or individual level. The favourable results of Schwellnus 1990 for insoles would be unlikely to remain statistically significant should this be a cluster‐randomised controlled trial.
Key issues also arise pertaining to the external applicability of the review. One aspect is the diagnosis and definition of stress fractures and stress responses of bone. In this review update, we made explicit that shin splints would be considered as a separate entity. This reflected the underlying and continuing difficulties in the diagnosis of tibial stress injuries. Some specific reflections on the diagnosis of stress fractures in the prevention and treatment trials in this review are given below but a general comment is the important need for effective and specific diagnosis of stress fractures/stress reactions of bone in these trials. Another key aspect is that all 13 prevention trials and two of the three treatment trials involved military personnel. The special circumstances of military training are likely to restrict the generalisability of the results to other people at risk of overuse injuries and stress fractures such as athletes and other people involved in high intensity and repetitive physical training/activity. Factors such as the use of heavy army boots, the inflexibility and standardisation of intensive training in large groups, the often considerable change in the level of activity at the start with the objective of achieving a very high of physical fitness within a very few weeks, and training with heavy loads all contribute to the very high risk environment for overuse injuries. The balance of risk factors is likely to be different for many categories of athletes, who will generally have more flexible training schedules that can be more readily adapted on an individual basis upon early signs of overuse injury.
Prevention The methodological quality, as reported, of the 13 prevention trials was generally poor. Serious bias in the findings of these trials could have arisen from the failure to conceal allocation of trial interventions, to conduct intention‐to‐treat analysis and/or perform, where possible, blinded outcome assessment. The high losses to follow up in Finestone 1999 (51%) and Mundermann 2001 (62%) give particular cause for concern. As well as questions on the reliability of trial findings, some questions arise regarding their applicability. Related to this, some discussion on the description, basis of action and variety of the orthotics used in nine trials is given below. As indicated in the 'Background' of this review and above, the diagnosis of stress fractures is problematic. We found large variation in, and reporting of, the methods used to detect stress fractures in these trials. The methods used ranged from self report, as in Mundermann 2001, or clinical evaluation only, as in Bensel 1986, to radiological confirmation of clinically suspected stress fractures. In those trials using inadequate methods of detection, some misdiagnosis should be considered likely. For those relying on radiological confirmation, the possible overlooking of early stress fractures is also likely. There was a great variety of foot orthoses/footwear inserts used in the included trials (Table 14). For instance, the materials used ranged from foam rubber material to complex thermoplastic polymers such as polypropylene. The rationale for the choice of specific orthoses used in individual trials was often unclear; this is not helped by the variation and imprecision in the terms used to describe orthoses. For instance, some trials (Finestone 1999; Finestone 2004a; Finestone 2004b; Milgrom 1985) referred to soft and semi‐rigid foot orthoses, whereas other trials referred to shock absorbing insoles, which perhaps suggests the use of softer materials. The choice of orthotics may often have been influenced by what was available. For instance, the materials selected for Bensel 1986 may reflect what was available for military boots at that time in the USA. We suggest that the biomechanical rationale for the six inserts ‐ employing the construction of metatarsal bars, or domes made from soft, hard, elastic and spherical materials ‐ used in Mundermann 2001 remains unclear in terms of preventing tibial stress fractures. However, there is some scientific basis for the use of mechanical controlled foot orthoses, based upon the principles of controlling the foot in a sub‐talar neutral position, as employed in four trials (Finestone 1999; Finestone 2004a; Finestone 2004b; Milgrom 1985).
Overall, there is insufficient evidence from randomised trials of preventive interventions to draw firm conclusions. However, there is limited evidence from randomised trials suggesting that the provision of "shock absorbing" insoles in the boots of military recruits reduces the overall incidence of stress fractures and stress reactions of bone. There is, however, insufficient evidence to determine the best design of such inserts or other footwear modifications but comfort and tolerability should be considered. There is some evidence indicating a lack of protection from leg muscle stretching during warm up before exercise.
The evidence for the use of foot orthoses in military boots suggests that the provision of "shock absorbing" insoles in the boots of military recruits reduces the overall incidence of stress fractures and stress reactions of bone. However, pooling of results was either not possible, such as the lack of data for the overall numbers of people sustaining a stress fracture in Milgrom 1985, or not appropriate as in the lack of clarification on the study design of Schwellnus 1990. In consequence, the results of Schwellnus 1990 must be viewed with caution. There is also insufficient evidence to determine the best design of such inserts or other footwear modifications. From a clinician's perspective, a common encounter with the prescription of foot orthoses is non‐compliance: this was common too in these trials. Many military recruits using foot orthoses found them intolerable or did not wear them throughout the trial period. Practical aspects also need to taken into consideration. For instance, while participants of Milgrom 1992 reported they preferred training in basketball shoes, the latter were less durable and fared worse on wet ground than military boots. Consistent with that given for other overuse injuries, the standard advice to avoid stress fractures is that people embarking on a physical training programme should build up their capacity, such as running distance, gradually and stop the activity if there are signs and symptoms of a bony stress response/fracture. Though the pre‐training level of fitness in military recruits will vary, for the majority of recruits there is a considerable increase in the level of physical activity on starting a military training regime. Such sudden jumps in physical activity levels predispose military recruits to stress fractures as does the need to sustain high levels of activity in order to achieve a high level of fitness within a set time period. The evidence available from the only randomised trial testing a modification in military training regime that specifically reported on stress fracture (Andrish 1974) is insufficient to inform this issue.
Both intervention and control groups in the two trials (Pope 1998; Pope 2000) testing the effects of stretching before exercise on the risk of injury also performed gentle warm‐up exercises. Both trials found no significant difference between the two groups in stress fractures or overall lower‐limb injury. These two trials were also included in a systematic review of stretching before and after exercising on the risk of injury (Herbert 2002). This reported that additional analyses undertaken to account for possible clustering of outcomes by platoon yielded "essentially identical" results. It is noteworthy that 94 participants in the control group of Pope 2000 withdrew because they wished to perform lower‐limb stretch exercises; thus underlining a common perception, not supported by the results of either Pope 1998 or Pope 2000, that stretching is required before exercise.
The rationale for calcium supplementation in young athletes remains unclear. We have already made clear our reservations on the study design of Schwellnus 1992, which anyway did not yield a significant difference in the incidence of stress fracture between those taking calcium supplements and those in the control group.
Treatment The issues surrounding diagnosis and definition of stress fractures are highly relevant to treatment. We excluded one previously included trial (Nissen 1994) through applying stricter criteria that excluded trials of treatment interventions for shin splints or medial tibial stress syndrome. We considered that for inclusion in this review a trial should have a specific diagnosis of stress fracture or stress reactions of bone. Confirmatory radiographic evidence was not required for any of the three treatment trials, all of which used bone scans to detect tibial stress fractures. Though two trials (Allen 2004; Swenson 1997) both focussed on the treatment of stress fractures in the distal two thirds of the tibia, the duration and definition of symptoms differed and the two trial populations are likely to have differed in the stage and severity of the condition at trial entry. This is illustrated in part by the readiness of several of the participants in Allen 2004 to start functional progression immediately.
There was some evidence from three small treatment trials that support of the injured leg in a pneumatic brace appears to allow a return to training activity and thus a quicker rehabilitation. The heterogeneity of the trials, in terms of diagnosis, control group intervention, adherence to the allocated intervention (brace use appears to have been very poor in Allen 2004), rehabilitation programmes and outcome definition, was considerable as was the statistical heterogeneity in the pooled results. This and the potential for other aspects of the study designs (such as other major differences in the interventions (Slatyer 1995); and the high loss to follow up in Allen 2004) to influence the trial results means this promising result needs further confirmatory evidence.
Authors' conclusions
Implications for practice.
There is insufficient evidence from randomised trials of preventive interventions to draw firm conclusions. However, there is limited evidence from randomised trials suggesting that the provision of "shock absorbing" insoles in the boots of military recruits reduces the overall incidence of stress fractures and stress reactions of bone. There is, however, insufficient evidence to determine the best design of such inserts or other footwear modifications but comfort and tolerability should be considered. There is some evidence indicating a lack of protection from leg muscle stretching during warm up before exercise.
There is limited evidence that following diagnosis of a tibial stress fracture, early mobilisation with the support of a pneumatic brace may accelerate a return to training activity.
Implications for research.
Lower‐limb stress fractures are serious injuries that can result in prolonged activity restriction and major changes in occupation and leisure activity. Further research to identify effective methods of prevention and treatment of these injuries is justified. People planning future trials of preventive or treatment measures for lower‐limb stress injuries of bone should take note of the messages arising from this review.
These include the following.
1) The need to establish, potentially via a consensus process, a generally accepted framework for the diagnosis of stress fractures and stress reactions of bone, which can inform the conduct, reporting and interpretation of future trials and studies.
2) The need for careful choice and justification for selection of interventions, such as foot orthoses, for evaluation.
3) Attention to methodological issues (randomisation techniques ensuring allocation concealment, analysis by intention to treat, blinding, and clearly defined outcome criteria) and adequate reporting of study design, the study population, interventions and results (Moher 2001). Trials using cluster randomisation should perform appropriate analyses and include sufficient information in trial reports to aid interpretation by readers and users of such trials (Campbell 2004).
4) The need for comprehensive and systematic outcome assessment, which includes acceptability of the intervention to trial participants and economic evaluation.
We suggest that, in particular, additional evidence from randomised trials is required to confirm that the use of a pneumatic brace enables quicker rehabilitation for tibial stress fracture. As well as attending to the methodological and other issues listed above, such trials should ensure that the intervention and control groups differ only in the use of the pneumatic brace and also have sufficiently long‐term follow up to establish adverse effects, including re‐injury, or additional benefits.
What's new
| Date | Event | Description |
|---|---|---|
| 22 October 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 2, 1996 Review first published: Issue 4, 1999
| Date | Event | Description |
|---|---|---|
| 14 January 2005 | New citation required and conclusions have changed | The main changes in this substantive update, published in Issue 2, 2005, are: (1) change of review authorship; (2) update of the literature search to September 2004; (3) the identification of 24 new studies, eight of which are included; (4) the exclusion of four previously included trials; (5) modifications to the quality assessment tool, addition of other outcome measures, such as other lower limb injuries, and other updating of methods including the use of relative risks rather than odds ratios; (6) revisions resulting from review by the new authors of previously included materials and obtaining further information from trialists; (7) addition of a 'Synopsis', and revised text through out. |
Acknowledgements
This review update takes forward the work of the two authors, Prof William Gillespie and Ms Inga Grant, of the first version of the review. These authors acknowledged the help of the following colleagues and members of the Cochrane Bone, Joint and Muscle Trauma Group: Dr Helen Handoll, Ms Kathryn Quinn, Dr Jennifer Browning. The work on the first version was supported by the Chief Scientist Office, Department of Health, The Scottish Office, UK.
We thank Mrs Lesley Gillespie for her support and feedback, and her great help with the search and retrieval of trials. We thank Mrs Lesley Gillespie, Prof William Gillespie, Mr Iain Annan, Mr Peter Herbison and Dr Janet Wale for helpful feedback at editorial and external review.
We thank Captain Christopher Allen, Dr Charles Milgrom, Gethin Owen and Captain Kerry Thompson for providing further information on their trials.
Appendices
Appendix 1. Search strategy for MEDLINE (OVID‐WEB)
| MEDLINE |
| 1. Fractures, Stress/ 2. stress fractur$.tw. 3. shin splint$.tw. 4. (bone adj3 stress adj3 reaction$).tw. 5. ((fract$ or injur$) adj3 (insufficiency or fatigue or overuse)).tw. 6. or/2‐5 7. Athletic Injuries/ 8. Cumulative Trauma Disorders/ 9. Military Personnel/ 10. exp Running/ or Walking/ or Dancing/ 11. or/7‐10 12. and/6,11 13. or/1,12 14. randomized controlled trial.pt. 15. controlled clinical trial.pt. 16. Randomized Controlled Trials/ 17. Random Allocation/ 18. Double‐Blind Method/ 19. Single‐Blind Method/ 20. or/14‐19 21. Animal/ not Human/ 22. 20 not 21 23. clinical trial.pt. 24. exp Clinical Trials/ 25. (clinic$ adj25 trial$).tw. 26. ((singl$ or doubl$ or trebl$ or tripl$) adj (mask$ or blind$)).tw. 27. Placebos/ 28. placebo$.tw. 29. random$.tw. 30. Research Design/ 31. (latin adj square).tw. 32. or/23‐31 33. 32 not 21 34. 33 not 22 35. Comparative Study/ 36. exp Evaluation Studies/ 37. Follow‐Up Studies/ 38. Prospective Studies/ 39. (control$ or prospectiv$ or volunteer$).tw. 40. Cross‐Over Studies/ 41. or/35‐40 42. 41 not 21 43. 42 not (22 or 34) 44. or/22,34,43 45. and/13,22 46. and/13,34 47. and/13,43 |
Appendix 2. Former search strategy for MEDLINE (Silverplatter)
| MEDLINE |
| The optimum search strategy for randomised trials described by Dickersin et al (Dickersin 1994*) was used with the following specific search terms: 1. Fractures, stress/ all subheadings (MESH) 2. Athletic injuries/all subheadings (MESH) 3. Repetition strain injury/all subheadings (MESH) 4. #1 or #2 or #3 5. fractur* 6. (insufficiency or fatigue or overuse or athletic) near #5 7. #4 or #6 8. explode Arm injuries/all subheadings (MESH) 9.#7 not #8 10. Risk factors/all subheadings (MESH) 11. Military personnel/all subheadings (MESH) 12. #9 and #10 13. #9 and #11 14. #9 and Cochrane optimal strategy. The output of the search was #12 to #14. * (Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. BMJ 1994;309:1286‐91.) |
Data and analyses
Comparison 1. Prevention: insoles/orthotics versus control (no insole).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress injury of bone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Diagnosed by clinical signs with confirmatory radiology | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants sustaining stress injury of bone (by site) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Femoral stress fractures (radiological confirmation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Femoral stress fractures or stress reactions (scintigraphy ) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Tibial stress fractures (radiological confirmation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Tibial stress fractures or stress reactions (scintigraphy) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Stress fractures in the foot (radiological confirmation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Stress fractures or stress reactions in the foot (scintigraphy) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.7 Stress fractures or pain in the foot (self report) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Participants sustaining an injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Any injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Overuse injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.

Comparison 1 Prevention: insoles/orthotics versus control (no insole), Outcome 1 Participants sustaining stress injury of bone.
1.2. Analysis.

Comparison 1 Prevention: insoles/orthotics versus control (no insole), Outcome 2 Participants sustaining stress injury of bone (by site).
1.3. Analysis.

Comparison 1 Prevention: insoles/orthotics versus control (no insole), Outcome 3 Participants sustaining an injury.
Comparison 2. Prevention: cushioned (urethrane or special grid‐like mesh) versus standard insoles.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress reaction of bone (by site) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Tibial stress reactions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Calcaneal stress reactions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Metatarsal stress reactions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants attending medical facility for lower‐limb disorder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Participants with activity restriction due to lower‐limb disorder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Medical discharge due to lower‐limb disorder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Participants rating their insoles as uncomfortable | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
2.1. Analysis.
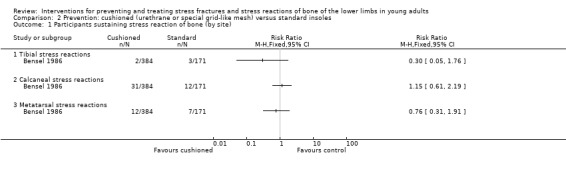
Comparison 2 Prevention: cushioned (urethrane or special grid‐like mesh) versus standard insoles, Outcome 1 Participants sustaining stress reaction of bone (by site).
2.2. Analysis.

Comparison 2 Prevention: cushioned (urethrane or special grid‐like mesh) versus standard insoles, Outcome 2 Participants attending medical facility for lower‐limb disorder.
2.3. Analysis.

Comparison 2 Prevention: cushioned (urethrane or special grid‐like mesh) versus standard insoles, Outcome 3 Participants with activity restriction due to lower‐limb disorder.
2.4. Analysis.

Comparison 2 Prevention: cushioned (urethrane or special grid‐like mesh) versus standard insoles, Outcome 4 Medical discharge due to lower‐limb disorder.
2.5. Analysis.

Comparison 2 Prevention: cushioned (urethrane or special grid‐like mesh) versus standard insoles, Outcome 5 Participants rating their insoles as uncomfortable.
Comparison 3. Prevention: visco‐elastic polymer versus mesh (standard) insoles (exploratory analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress injury of bone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Diagnosed by clinical signs with confirmatory radiology | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants sustaining stress injury of bone in the foot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Diagnosed by clinical signs with confirmatory radiology | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.

Comparison 3 Prevention: visco‐elastic polymer versus mesh (standard) insoles (exploratory analysis), Outcome 1 Participants sustaining stress injury of bone.
3.2. Analysis.

Comparison 3 Prevention: visco‐elastic polymer versus mesh (standard) insoles (exploratory analysis), Outcome 2 Participants sustaining stress injury of bone in the foot.
Comparison 4. Prevention: orthotics (semi‐rigid or soft foot) versus mesh (standard) insoles.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress injury of bone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Diagnosed by clinical signs or scintigraphy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants sustaining stress injury of bone (by site) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Femoral stress fractures or stress reactions (scintigraphy ) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Tibial stress fractures or stress reactions (scintigraphy ) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Stress fractures or stress reactions in the foot (scintigraphy) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Early dissatisfaction with orthotic/insole (reason for drop out) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
4.1. Analysis.

Comparison 4 Prevention: orthotics (semi‐rigid or soft foot) versus mesh (standard) insoles, Outcome 1 Participants sustaining stress injury of bone.
4.2. Analysis.
Comparison 4 Prevention: orthotics (semi‐rigid or soft foot) versus mesh (standard) insoles, Outcome 2 Participants sustaining stress injury of bone (by site).
4.3. Analysis.

Comparison 4 Prevention: orthotics (semi‐rigid or soft foot) versus mesh (standard) insoles, Outcome 3 Early dissatisfaction with orthotic/insole (reason for drop out).
Comparison 5. Prevention: urethrane versus special grid‐like mesh insoles.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress reaction of bone (by site) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Tibial stress reactions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Calcaneal stress reactions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Metatarsal stress reactions | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants attending medical facility for lower‐limb disorder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Participants with activity restriction due to lower‐limb disorder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Medical discharge due to lower‐limb disorder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Participants rating their insoles as uncomfortable | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
5.1. Analysis.
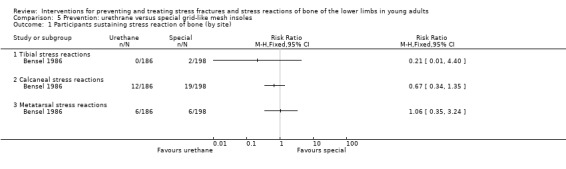
Comparison 5 Prevention: urethrane versus special grid‐like mesh insoles, Outcome 1 Participants sustaining stress reaction of bone (by site).
5.2. Analysis.

Comparison 5 Prevention: urethrane versus special grid‐like mesh insoles, Outcome 2 Participants attending medical facility for lower‐limb disorder.
5.3. Analysis.

Comparison 5 Prevention: urethrane versus special grid‐like mesh insoles, Outcome 3 Participants with activity restriction due to lower‐limb disorder.
5.4. Analysis.

Comparison 5 Prevention: urethrane versus special grid‐like mesh insoles, Outcome 4 Medical discharge due to lower‐limb disorder.
5.5. Analysis.

Comparison 5 Prevention: urethrane versus special grid‐like mesh insoles, Outcome 5 Participants rating their insoles as uncomfortable.
Comparison 6. Prevention: semi‐rigid versus soft foot orthotics.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress injury of bone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Diagnosed by clinical signs or scintigraphy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants sustaining stress injury of bone (by site) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Femoral stress fractures or stress reactions (scintigraphy ) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Tibial stress fractures or stress reactions (scintigraphy ) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Stress fractures or stress reactions in the foot (scintigraphy) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Early dissatisfaction with orthotic (reason for drop out) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
6.1. Analysis.
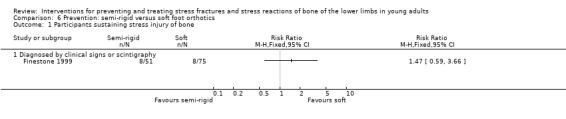
Comparison 6 Prevention: semi‐rigid versus soft foot orthotics, Outcome 1 Participants sustaining stress injury of bone.
6.2. Analysis.

Comparison 6 Prevention: semi‐rigid versus soft foot orthotics, Outcome 2 Participants sustaining stress injury of bone (by site).
6.3. Analysis.

Comparison 6 Prevention: semi‐rigid versus soft foot orthotics, Outcome 3 Early dissatisfaction with orthotic (reason for drop out).
Comparison 7. Prevention: custom‐made versus prefabricated soft foot orthoses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress injury of bone in the foot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Diagnostic method not reported | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants sustaining foot overuse injuries | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Foot problem | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Ankle sprain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Participants failing to complete training in allocated insoles | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
7.1. Analysis.
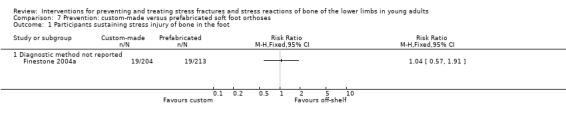
Comparison 7 Prevention: custom‐made versus prefabricated soft foot orthoses, Outcome 1 Participants sustaining stress injury of bone in the foot.
7.2. Analysis.

Comparison 7 Prevention: custom‐made versus prefabricated soft foot orthoses, Outcome 2 Participants sustaining foot overuse injuries.
7.3. Analysis.

Comparison 7 Prevention: custom‐made versus prefabricated soft foot orthoses, Outcome 3 Participants failing to complete training in allocated insoles.
Comparison 8. Prevention: custom‐made mechanical versus prefabricated semi‐rigid foot orthoses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress injury of bone in the foot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Diagnostic method not reported | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants sustaining foot overuse injuries | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Foot problem | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Ankle sprain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Participants failing to complete training in allocated insoles | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
8.1. Analysis.
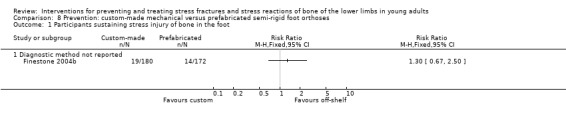
Comparison 8 Prevention: custom‐made mechanical versus prefabricated semi‐rigid foot orthoses, Outcome 1 Participants sustaining stress injury of bone in the foot.
8.2. Analysis.
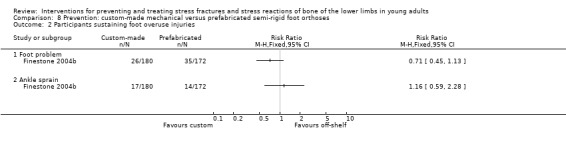
Comparison 8 Prevention: custom‐made mechanical versus prefabricated semi‐rigid foot orthoses, Outcome 2 Participants sustaining foot overuse injuries.
8.3. Analysis.

Comparison 8 Prevention: custom‐made mechanical versus prefabricated semi‐rigid foot orthoses, Outcome 3 Participants failing to complete training in allocated insoles.
Comparison 9. Prevention: modified basketball shoe versus standard infantry boot.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress injury of bone | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Diagnosed by clinical signs and scintigraphy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants sustaining stress injury of bone (by site) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Femoral stress fractures or stress reactions (scintigraphy ) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Tibial stress fractures or stress reactions (scintigraphy ) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Stress fractures or stress reactions in the foot (scintigraphy) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Participants sustaining overuse injuries | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Other foot injury: metatarsalagia, heel or arch pain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Any lower limb overuse injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
9.1. Analysis.

Comparison 9 Prevention: modified basketball shoe versus standard infantry boot, Outcome 1 Participants sustaining stress injury of bone.
9.2. Analysis.

Comparison 9 Prevention: modified basketball shoe versus standard infantry boot, Outcome 2 Participants sustaining stress injury of bone (by site).
9.3. Analysis.

Comparison 9 Prevention: modified basketball shoe versus standard infantry boot, Outcome 3 Participants sustaining overuse injuries.
Comparison 10. Prevention: pre‐exercise stretching (exploratory analysis).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 All stress fractures | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Calf muscles stretching versus arm muscles stretching | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Leg muscles stretching versus control | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Stress fractures (by site) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Femur | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Tibia | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Fibula | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Foot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Ilium | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Pubic rami | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 All lower limb injuries | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Calf muscles stretching versus arm muscles stretching | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Leg muscles stretching versus control | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
10.1. Analysis.
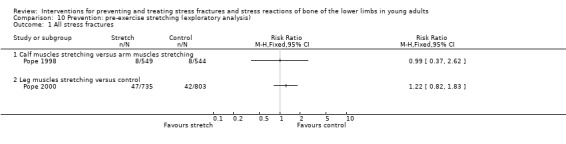
Comparison 10 Prevention: pre‐exercise stretching (exploratory analysis), Outcome 1 All stress fractures.
10.2. Analysis.
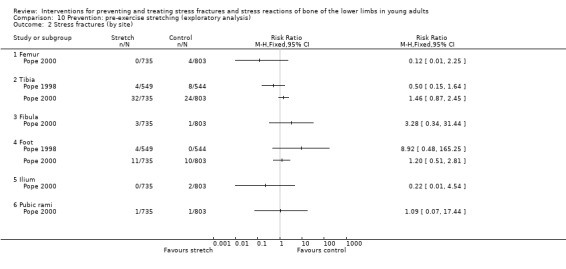
Comparison 10 Prevention: pre‐exercise stretching (exploratory analysis), Outcome 2 Stress fractures (by site).
10.3. Analysis.

Comparison 10 Prevention: pre‐exercise stretching (exploratory analysis), Outcome 3 All lower limb injuries.
Comparison 11. Prevention: calcium supplementation versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants sustaining stress fractures | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Participants sustaining stress fractures (by site) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Femoral stress fractures (radiological confirmation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Tibial stress fractures (radiological confirmation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Stress fractures in the foot (radiological confirmation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Participants sustaining an injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Any injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Overuse injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
11.1. Analysis.

Comparison 11 Prevention: calcium supplementation versus placebo, Outcome 1 Participants sustaining stress fractures.
11.2. Analysis.

Comparison 11 Prevention: calcium supplementation versus placebo, Outcome 2 Participants sustaining stress fractures (by site).
11.3. Analysis.

Comparison 11 Prevention: calcium supplementation versus placebo, Outcome 3 Participants sustaining an injury.
Comparison 12. Treatment: rehabilitation in a pneumatic air brace versus control (no brace).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to resuming light activity | 2 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐1.96 [‐8.81, 4.90] |
| 2 Time to return to full activity/training | 3 | 98 | Mean Difference (IV, Fixed, 95% CI) | ‐33.39 [‐44.18, ‐22.59] |
| 2.1 Return to full unrestricted activity (days) | 2 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐18.90 [‐32.31, ‐5.49] |
| 2.2 Lost training days | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐60.09 [‐78.29, ‐41.89] |
| 3 Medical discharge from army | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
12.1. Analysis.

Comparison 12 Treatment: rehabilitation in a pneumatic air brace versus control (no brace), Outcome 1 Time to resuming light activity.
12.2. Analysis.

Comparison 12 Treatment: rehabilitation in a pneumatic air brace versus control (no brace), Outcome 2 Time to return to full activity/training.
12.3. Analysis.

Comparison 12 Treatment: rehabilitation in a pneumatic air brace versus control (no brace), Outcome 3 Medical discharge from army.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allen 2004.
| Methods | RCT: use of a random number generator. Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 1 Blinding of outcome assessors: 2 Comparability of treatment groups at entry: 2 Use of placebo: 1 Definition of inclusion and exclusion criteria: 2 Methods of assessment of outcome: 2 Losses to follow up: 11 (35%). Six were reassigned to another location, 4 didn't attend weekly follow ups and 1 had a calcaneal stress fracture. | |
| Participants | Location: USA. US Army Community Hospital(s), Texas and Georgia (active duty soldiers) Recruitment period: 2000 31 active duty soldiers (6 male, 25 female) of mean age 22 years. Inclusion criteria: distal 2/3rd tibial shaft stress fracture, ascertained by clinical symptoms and confirmatory nuclear bone scan, diagnosed within 1 month of study. Exclusion criteria: stress fractures involving proximal 1/3rd of tibial shaft including tibial plateau; bone scan results consistent with medial tibial stress syndrome; stress fracture involving the anterior or anterolateral tibia with a partial or complete fracture line; under 3 weeks remaining at training installation; other injuries preventing participation. | |
| Interventions | (1) Use of Aircast leg brace on affected limb during daily activities except sleeping and bathing. (2) No brace and no immobilisation. All participants were given identical physical profiles limiting and specifying the amount and type of physical activities and duties during the study. When a participant was able to walk without pain for 2 days, a functional rehabilitation programme was initiated at the next weekly evaluation. Advance was on pain‐free completion of the previous level. | |
| Outcomes | Length of follow up: completion of functional rehabilitation (maximum 78 days) (1) Time to pain‐free hop (2) Start time for functional progression. (3) Completion and time to completion of functional rehabilitation programme (1 mile pain‐free run): return to unrestricted military duties. (4) Compliance and complaints (no data) with brace. | |
| Notes | Pre‐publication article provided by Chris Allen 14 October 2004. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Andrish 1974.
| Methods | RCT: method not stated (stratified by previously tested scholastic and athletic aptitude) Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 0 (see Notes) Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 1 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 3 Losses to follow up: None described | |
| Participants | Location: USA Naval Academy Recruitment period: 1972‐1973 2777 first year midshipmen. No exclusion criteria described. | |
| Interventions | (1) Use of 1.3 cm thick foam rubber heel pad inside tennis shoes for running. Normal running schedule. (2) Graduated running programme: one third distance run in the first week, two thirds in the second week compared with control group. (3) Control group: no heel pads and normal running schedule. | |
| Outcomes | Length of follow up: duration of summer training programme (1) Tibial stress fracture diagnosed by pain, localised tenderness, and confirmation by radiological examination. (2) Other episodes of leg pain ‐ specifically shin splints. | |
| Notes | Trial also tested heel cord stretching exercises: these have not been included in this review. Trial has serious intention‐to‐treat problems: "Spot checks of the individual platoons and physical education programs were made. As a result of these checks, those platoons found not to have carried out the prophylactic regimens were placed in the control group." The larger size of the control group probably indicates that this took place. There was a supplementary RCT comparing heel pad versus no heel pad involving the 97 midshipmen treated for shin splints resulting from first trial. This secondary prevention trial is not presented here: there were no stress fractures reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Bensel 1986.
| Methods | RCT: forms marked A, B or C, were randomly distributed to participants Adequacy of concealment of assigned allocation: B Intention to treat analysis: 1 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 0 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 0 Losses to follow up: medical discharge 24 (part of results) ‐ no mention of losses | |
| Participants | Location: USA. US Army training establishment, Fort Jackson (Army trainees) Recruitment period: not stated (1985?) 555 army recruits, all female, no age given, in 7 basic training companies, undergoing a 9 weeks training course. No exclusion criteria described. | |
| Interventions | (1) Urethane foam backed with fibre‐board boot insert. (2) "Molded network of lever‐like projections attached at their back to material in the form of a grid." Smooth grid surface of boot insert closest to the foot. (3) Standard ventilating boot insert (control). All inserts were sized to fit from heel to toe in black leather combat boots. After fitting, each participant was issued with two pairs of boots with two allocated inserts already in place. | |
| Outcomes | Length of follow up: 9 weeks. (1) Tibial, calcaneal and metatarsalgia stress reactions diagnosed by clinical examination and reason for sick‐call data. (2) Individual incidences of other lower limb injuries/complaints including: blister; foot/knee/lower leg or ankle/pes cavus/pes planus pain; lateral ankle sprain; swollen ankle; ingrown nail; dermatitis; numb feet/toes; peroneal tendonitis; Achilles tendonitis; shin splints; plantar fasciitis; subluxing patella; callous; bunion. (3) Medical discharge for lower limb disorder (4) Number attending any treatment facility; mean number of visits. (5) Any restriction of activity; also none/limited/other. Mean duration of restriction. (6) Compliance (inserts always worn) and comfort. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Finestone 1999.
| Methods | RCT: randomised by choosing a card from a shuffled deck of 420 cards Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 0 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 2 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 2 Losses to follow up: 207 (51%) | |
| Participants | Location: Israel (Army recruits) Recruitment period: unknown. 404 infantry (probably all male) recruits participated in 14 weeks of basic training. Aged 17‐27. No exclusion criteria described. | |
| Interventions | All recruits wore modified infantry boots with soles similar to basketball shoes (see Milgrom 1992) (1) Custom‐made semi‐rigid foot orthoses. (2) Custom‐made soft foot orthoses. (3) Simple insoles (impressions made of feet but not used). | |
| Outcomes | Length of follow up: 14 week training period. (1) Stress fracture diagnosed by clinical examination and scintigraphy. (2) Comfort and compliance. | |
| Notes | Stress fracture data were only presented for trial completers: those who wore assigned orthoses/insoles and who were available to follow up throughout basic training. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Finestone 2004a.
| Methods | RCT: randomised using a randomisation programme in Excel Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 1 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 2 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 0 Losses to follow up: 34 (8%) without full clinical follow up | |
| Participants | Location: Israel (Army recruits) Recruitment period: unknown. 451 male infantry recruits participated in 14 weeks of basic training. Mean age 19. No exclusion criteria described except informed consent required. | |
| Interventions | All recruits wore standard infantry boots. Foot impressions made for both groups, but used only in the custom‐made group (1) Custom‐made soft foot orthoses. (2) Prefabricated soft foot orthoses (impressions made of feet but not used). | |
| Outcomes | Length of follow up: 14 week training period. (1) Stress fracture: no details of method of diagnosis. (2) Ankle sprain. (3) All foot problems. (4) Comfort and compliance. | |
| Notes | Reported as the first part of a two part study. The second part, which used similar methods but was conducted at a different military base, is presented in Finestone 2004b. Injuries data were given as percentages in the trial report. Extrapolating the results for presenting in this review showed some small problems with the calculation of these in the report. Corrected data received from Dr Milgrom on 20/10/04. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Finestone 2004b.
| Methods | RCT: randomised using a randomisation programme in Excel Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 1 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 2 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 0 Losses to follow up: 71 (17%) without full clinical follow up | |
| Participants | Location: Israel (Army recruits) Recruitment period: unknown. 423 male infantry recruits participated in 14 weeks of basic training. Mean age 19. No exclusion criteria described except informed consent required. | |
| Interventions | All recruits wore standard infantry boots. Foot impressions made for both groups, but used only in the custom‐made group (1) Custom‐made semi‐rigid foot orthoses. (2) Prefabricated semi‐rigid foot orthoses (impressions made of feet but not used). | |
| Outcomes | Length of follow up: 14 week training period. (1) Stress fracture: no details of method of diagnosis. (2) Ankle sprain. (3) All foot problems. (4) Comfort and compliance. | |
| Notes | Reported as the second part of a two part study. The first part, which used similar methods but was conducted at a different military base, is presented in Finestone 2004a. Injuries data were given as percentages in the trial report. Extrapolating the results for presenting in this review showed some small problems with the calculation of these in the report. Corrected data received from Dr Milgrom on 20/10/04. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Gardner 1988.
| Methods | Quasi‐randomised cluster (46 or 47 platoons: approximately 65 in each platoon) comparison: allocation by odd and even numbered platoons Adequacy of concealment of assigned allocation: C Intention‐to‐treat analysis: 2 Blinding of outcome assessors: 2 Comparability of treatment groups at entry: 1 Use of placebo: 0 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 3 Losses to follow up: 17 (omitted from one analysis table) (0.6%) | |
| Participants | Location: USA (US Marine recruits) Recruitment period: 1985 3025 male marine recruits, aged 18‐41, undergoing 12 weeks training. No exclusion criteria described. | |
| Interventions | (1) Shock‐absorbent polymer insoles in standard marine boots. (2) Standard mesh insoles (control group). | |
| Outcomes | Length of follow up: 12 week training period (1) Stress fractures/stress reactions of bone in the lower limb (above the foot, and in the foot) diagnosed by clinical evaluation and confirmatory radiology (2) Other lower limb injuries | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Milgrom 1985.
| Methods | RCT: randomised by drawing cards from a deck of cards Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 0 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 1 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 2 Losses to follow up: 30 excluded from analysis (10%) | |
| Participants | Location: Israel (Army recruits) Recruitment period: 1983 295 male Israeli Army recruits undergoing a 14 week basic training programme. "All recruits had passed a rigorous physical endurance and strength test before beginning the training. All had volunteered from this specific training." (see Notes) Exclusion criteria: not clarified. | |
| Interventions | (1) "Military stress orthotic" insole in the army combat boot. (2) Boots without orthotic insoles. | |
| Outcomes | Length of follow up: 14 week training period. (1) Stress fracture in the femur, tibia, or foot diagnosed by clinical examination followed where indicated by bone scanning. Some also had X‐rays but the given data refer to bone scan diagnosis. (2) Compliance: discontinuation of use/non‐use. | |
| Notes | Results from 30 recruits who discontinued use of their orthotics in the first 2 weeks were not reported. Method of randomisation and further information on recruits received from Dr Milgrom on 03/09/04. Simkin et al (1989) presented the findings of the trial in the context of the arch structure of the foot of the recruits participating in this study. None of the data presented in this paper were used in this review. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Milgrom 1992.
| Methods | RCT: use of a computer generated randomisation programme Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 2 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 1 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 2 Losses to follow up: None | |
| Participants | Location: Israel (Army recruits) Recruitment period: 1988 390 male Israeli Army recruits beginning a 14 week basic training programme. Informed consent. Exclusion criteria not stated. | |
| Interventions | (1) Modified (including use of water repellent) 'high top' basketball shoes used throughout training in place of boots. (2) Standard army boots used throughout. | |
| Outcomes | Length of follow up: 14 week training period (plus 1 month if problems) (1) Stress fracture diagnosed by clinical examination and scintigraphy. (2) Lower limb overuse injuries. (3) Participant evaluation of footwear. | |
| Notes | Prior pilot study involving 22 recruits in 1987 randomised to 4 types of basketball shoes to assess comfort and durability. Method of randomisation and further information on recruits received from Dr Milgrom on 03/09/04. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mundermann 2001.
| Methods | RCT: method not stated Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 1 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 0 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 0 Losses to follow up: 127 (62%) | |
| Participants | Location: Canada (Army recruits) Recruitment period: not stated. 206 Canadian Army recruits (10 female), mean age 28.5 years, participating in a 4 month basic training programme. Exclusion criteria: no consent, current musculoskeletal or lower extremity disorder. | |
| Interventions | (1) Choice of 6 shoe inserts. (2) Controls given no shoe insert. | |
| Outcomes | Length of follow up: 4 months. (1) Self‐report of pain and injuries during training. (2) Exit questionnaire (noted by physician, kind of injury, location, duration and frequency). (3) Comfort score. | |
| Notes | Comfort score not split by randomised groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pope 1998.
| Methods | Two stage process with cluster randomisation. Masked quasi‐randomised assignment based on surnames of recruits to army training platoons. Random allocation, by pairs of platoons (26 platoons in all): method not stated. Adequacy of concealment of assigned allocation: C Intention‐to‐treat analysis: 2 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 2 Definition of inclusion and exclusion criteria: 2 Methods of assessment of outcome: 2 Losses to follow up: 210 (162 discharged or reassigned to a later platoon (back squadding) and 48 withdrew) (19%) | |
| Participants | Location: Australia (Army recruits) Recruitment period: 1992‐1993. 1093 male recruits aged 17‐35 undertaking a 12 week training programme. Exclusion criteria: significant pre‐existing injury or injury before arrival at training location. Non consent. | |
| Interventions | (1) Two 20 second stretches for each calf muscle (gastrocnemius and soleus) in both legs after 3 minutes warm‐up exercises. (2) Warm‐up exercises only, then stretches of wrist flexor and triceps muscles. | |
| Outcomes | Length of follow up: 12 week training period (1) Stress fracture of tibia and foot: diagnosis confirmed by positive bone scan or X‐rays. (2) Lateral ankle sprain. (3) Tibial periostitis (4) Achilles tendinitis (5) Anterior compartment syndrome (tibia). | |
| Notes | Once a recruit presented with a lower‐limb injury, his survival time was terminated. Thus only the first injury was counted. If a recruit presented with two or more lower‐limb injuries simultaneously, only the primary injury was recorded. Only injuries sustained up to the time when a recruit was prematurely discharged or back squadded or withdrew from the trial were registered. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Pope 2000.
| Methods | Two stage process with cluster randomisation. Masked quasi‐randomised assignment based on surnames of recruits to army training platoons. Random allocation, by pairs of platoons (39 platoons in all): method not stated. Adequacy of concealment of assigned allocation: C Intention‐to‐treat analysis: 2 Blinding of outcome assessors: 1 Comparability of treatment groups at entry: 1 Use of placebo: 0 Definition of inclusion and exclusion criteria: 2 Methods of assessment of outcome: 2 Losses to follow up: 170 discharged or transferred. (11%) (The 89 recruits who were reassigned to a later platoon (back squadding) and 94 who withdrew continued to be monitored). | |
| Participants | Location: Australia (Army recruit training establishment) Recruitment period: 1994 1538 male recruits aged 17‐35 undertaking a 12 week training programme. Exclusion criteria: psychologically unsuitable (assessed by pen and paper aptitude tests); history of significant injury. | |
| Interventions | (1) 20 second stretches of six lower limb muscles during warm‐up exercises (2) Warm‐up exercises only | |
| Outcomes | Length of follow up: 12 weeks training period All lower limb injuries: (1) Stress fracture (tibia, foot, femur, fibula, Ilium, pubic rami) diagnosis confirmed by radiographs, computed tomography or bone scan (2) Other bone injuries: acute fracture periostitis stress changes (3) Soft tissue injuries: ankle sprain other ligament sprains (knee and foot) muscle strain (3 locations) tendonitis (3 locations) knee meniscal injury compartment syndrome (shank) patellofemoral joint other (e.g. bursitis). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Schwellnus 1990.
| Methods | RCT: method not stated Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 1 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 1 Definition of inclusion and exclusion criteria: 1 Methods of assessment of outcome: 3 Losses to follow up: 123 were transferred to other units (8%) | |
| Participants | Location: South Africa (Army recruit training centre) Recruitment period: not described. 1511 male (inferred) military recruits (age of sample 17‐25) undergoing basic training. Exclusion criteria: gross biomechanical abnormality or history of previous major injury or illness. | |
| Interventions | (1) Neoprene ("shock absorbing") insoles in standard military footwear (2) No insoles | |
| Outcomes | Length of follow up: 9 week training period (1) Stress fractures of femur, tibia, or metatarsals, diagnosed by clinical evaluation and confirmatory radiology. (2) Other injuries including overuse and trauma. (3) Of sample of insoles group: comfort, compliance and wear. | |
| Notes | This trial and Schwellnus 1992 shared the same control group. Email (13/09/04) and letter (23/09/04) sent to Schwellnus requesting clarification on when the study took place and method of randomisation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Schwellnus 1992.
| Methods | RCT: method not stated Adequacy of concealment of assigned allocation: B Intention‐to‐treat analysis: 1 Blinding of outcome assessors: 2 Comparability of treatment groups at entry: 1 Use of placebo: 0 Definition of inclusion and exclusion criteria: 2 Methods of assessment of outcome: 3 Losses to follow up: 113 were transferred to other units (7.5%) | |
| Participants | Location: South Africa (Army recruit training centre) Recruitment period: Not described 1511 male military recruits, all under 25 years, undergoing basic training. Exclusion criteria: one or more "gross biochemical abnormalities", history of previous major injury or illness, documented hypercalcaemia or hypercalciuria, renal failure, sarcoidosis, or milk‐alkali syndrome. | |
| Interventions | (1) Calcium supplementation: Sandoz Forte 500 mg daily for 9 weeks (training period). (2) No intervention. All recruits wore standard military boots. | |
| Outcomes | Length of follow up: 9 week training period (1) Stress fractures of femur, tibia, or metatarsals, diagnosed by clinical evaluation and confirmatory radiology. (2) Other injuries including overuse and trauma. | |
| Notes | This trial and Schwellnus 1990 shared the same control group. Email (13/09/04) and letter (23/09/04) sent to Schwellnus requesting clarification on when the study took place and method of randomisation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Slatyer 1995.
| Methods | RCT: use of a computer‐based random number generator to construct randomisation schedule. Paper claimed there was no evidence of corruption of the randomisation process. Adequacy of concealment of assigned allocation: A Intention‐to‐treat analysis: 2 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 1 Use of placebo: 1 Definition of inclusion and exclusion criteria: 2 Methods of assessment of outcome: 2 Losses to follow up: None | |
| Participants | Location: Australia. Infantry Training Centre, New South Wales (Army recruits) Recruitment period: 1989‐90 60 infantry recruits (53 male, 7 female) aged 17 to 31 years. Inclusion criteria: Grade 1 or 2 tibial shaft stress fracture, ascertained by clinical symptoms and regional three‐phase bone scan, positive attitude to use of the experimental appliance. Exclusion criteria: stress fracture at other location | |
| Interventions | (1) Use of Aircast leg brace on affected limb until completion of training, continuing to undertake graded exercise rehabilitation programme in a rehabilitation platoon. (2) Hospital admission for assessment, advice for non‐impact exercise programme, 6 weeks convalescent leave. First week comprised rest with no physical activity. After convalescent period, participants entered into a formal rehabilitation programme (similar to that for the brace group). | |
| Outcomes | Length of follow up: 6 months, including 10 weeks assessment over study period (1) Training days lost (2) Completion of training in study period, medical discharge by 6 months (3) Pain on walking, running, activity and at night (4) Running distance (5) Coopersmith self esteem inventory score and desire to stay in the army (6) Compliance with rehabilitation programmes (7) Brace side effects (8) Costs of healthcare | |
| Notes | A preliminary pilot study identified problems associated with sustained brace use in a recruit training environment. Attempts were made to address these problems in order to minimise side effects. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Swenson 1997.
| Methods | RCT: method not stated Adequacy of concealment of assigned allocation: B Intention to treat analysis: 1 Blinding of outcome assessors: 0 Comparability of treatment groups at entry: 0 Use of placebo: 1 Definition of inclusion and exclusion criteria: 2 Methods of assessment of outcome: 2 Losses to follow up: 3 (14%). Two dropped out and one was excluded after developing unrelated symptoms preventing functional rehabilitation. | |
| Participants | Location: USA (athletes) Recruitment period: 1990‐93 21 competitive and recreational athletes between the ages of 15 and 45 years. Inclusion criteria: Localised pain and tenderness to palpation for less than 6 months in the distal two thirds of the tibia; positive bone scan at that site. Exclusion criteria: stress fracture with radiological evidence of significant bone resorption in the anterior or anterolateral tibia; stress fracture in the proximal one third of the tibia; diffuse linear isotope uptake consistent with medial tibial stress syndrome. | |
| Interventions | (1) Functional activity progression programme, weightbearing in long air‐stirrup leg brace (Aircast). (2) Functional activity progression programme; initially nonweightbearing ‐ weight relief with crutches if required. No bracing. Both groups began a gradual return to impact activities when they had been walking pain‐free for three days. | |
| Outcomes | Length of follow up: 12 weeks or until return to full activity (1) Time from treatment to beginning of light activity. (2) Time to ability to hop without pain. (3) Time to completion of functional progression (return to full activity). (4) Performance inhibition in brace | |
| Notes | Means and standard deviations were calculated from graphs presented in the trial report. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Amako 2003 | Not an RCT. A comparison in military recruits of static stretching before and after exercise versus no static stretching. Although the "new recruits were randomly assigned" to one of three companies in each year of the 3 years of the study, the allocation of the intervention appeared to be at the discretion of the company commander. |
| Bensel 1976 | Quasi‐randomised comparative study. Specific to the US Army, comparing two types of combat boots of the early 1970s, and was considered to be of historic rather than contemporary relevance. |
| Benson 1989 | RCT (placebo controlled) evaluating the effect of vitamin/mineral supplementation on the incidence, severity and nature of ballet injuries. No stress fracture data available. |
| Callison 2002 | RCT on the treatment for shin splints not stress fractures. |
| Clark 1989 | RCT examining use of viscoelastic shoe insoles in aerobic dancing. No specific injury including stress fracture data available. |
| Ekenman 2002 | Randomised controlled laboratory study involving in vivo strain measurements in nine members of the Swedish police during treadmill walking and running with or without biomechanical shoe orthosis in boots or running shoes. Laboratory study with surrogate outcomes only: no stress fracture data. |
| Giladi 1985 | Not an RCT. A comparison of two different infantry training programmes. One programme had a more gradual training programme than the other, but both were designed to reach the same level of training by the end. Soldiers were assigned to either of the two infantry units according to their preference and space availability. |
| Gray 2003 | RCT of conservative treatment for tuberosity fractures of the fifth metatarsal. These were 'avulsion' fractures rather than stress fractures. |
| Hartig 1999 | Not an RCT. Report on hamstring flexibility in military recruits on reducing overuse injuries that included stress fractures |
| Larsen 2002 | RCT. No stress fracture data. 147 Danish Army recruits beginning basic training programme were assigned to custom‐made biomechanic shoe orthoses versus no intervention. Self‐reported back and/or lower extremity problems included shin splints. Trialist did not respond to request for confirmation that there were no stress fractures. However, this seems very unlikely given that time off sick for any injury was rarely more than one day. |
| Nissen 1994 | RCT examining the use of laser treatment of shin splints (medial tibial stress syndrome) not stress fractures. |
| Pollock 1977 | RCT. No stress fracture data. The total number of training injuries was significantly lower if running training was limited to three runs per week of 30 minutes duration. Running longer distances or for longer periods, increased the incidence of injuries, without appearing to offer significant advantages in aerobic fitness. |
| Popovich 2000 | Not an RCT. There is no indication that there was random assignment of four variants of the training schedule (avoidance of running in the second, third to fourth week, increased running mileage) to four companies of army recruits, or of the standard training schedule to the other two companies. The study was described as "not fully controlled", which reflected the lack of consistency in the training schedules (above that resulting from the interventions) between the six companies. |
| Rudzki 1997 | RCT (cluster). Military recruits. Data given for all lower limb injuries and for a subset of stress fractures which resulted in discharge from the armed forces. No overall stress fracture data reported. |
| Scully 1982 | This was a controlled comparison, conducted in 1974, involving 880 USA army trainees testing the elimination of running, jumping and double timing during third week of training versus an uninterrupted programme of training. There was very little information on methods including a lack of information on whether the two groups were concurrent, or method of allocation to the intervention groups, and on the method for diagnosing stress fracture. |
| Sherman 1996 | In this comparative study, involving 1132 males, shock absorbing inserts were issued to every trainee in every other basic training unit as the units were filled by soldiers entering the US Army. The number of units were not stated but would have been small since each unit comprised several hundred trainees. At best this could be viewed as a quasi‐randomised cluster trial. However, the study was further and seriously compromised by the self purchase of inserts in over one third of the soldiers who had not been issued with inserts. |
| Smith 1985 | Not an RCT. A comparison of two shock absorbing insoles (cellular neoprene versus cellular polyurethane) with no insole (control). Though the sample was "randomly selected", there was no specific mention of randomisation nor any description of how the 90 recruits from the US Coast Guard Training Center were divided into three groups of 30. One, in the control group, of the 68 participants followed up was indicated as having a "tibial stress" injury. |
| Thompson 2004 | Not an RCT. Comparison of shock absorbing boots versus standard boots in female USA navy recruits. The first to arrive of each pair of divisions got the new boots and the other got the old boots. |
| Tokki 2002 | RCT of individually fitted sports shoes in Finnish newspaper carriers. No stress fractures. |
| Van Mechelen 1993 | RCT examining health education and exercises in male recreational runners. No report of stress fractures. |
| Wedderkopp 1999 | RCT (cluster) examining ankle disk and muscle training in young female handball players. No stress fractures. |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Owen 2004.
| Trial name or title | The effectiveness of a pneumatic brace in the rehabilitation of tibial stress fractures. |
| Methods | |
| Participants | 50 Army recruits (age 17‐28 years) with bone scan confirmed tibial stress fracture. |
| Interventions | Lower‐limb pneumatic brace group versus none (control). All participants followed a progressive active rehabilitation program supervised by a physical therapist. |
| Outcomes | Pain on palpation; single‐leg hops; a 1.5 mile run; time in rehabilitation. |
| Starting date | Not known |
| Contact information | David Gethin Owen Defence Medical Rehabilitation Centre Epsom UK Email: gethowen@dsca.mod.uk |
| Notes | Preliminary results presented at 51st annual meeting of the American College of Sports Medicine (2004) |
Contributions of authors
Keith Rome (KR) initiated and co‐ordinated the first update of the review. KR performed most of the literature searching. All three authors selected studies, assessed trial quality and, to varying extents, extracted data. KR and Helen Handoll (HH) contracted trialists for further information. HH compiled the review in RevMan, and with KR composed first drafts and rewrites of the text and tables. Robert Ashford critically reviewed the review at various stages. Keith Rome and Helen Handoll are guarantors of the review.
Sources of support
Internal sources
University of Teesside, Middlesbrough, UK.
University of Central England, Birmingham, UK.
External sources
No sources of support supplied
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
Allen 2004 {published and unpublished data}
- Allen CS, Flynn TW, Kardouni JR, Hemphill NH, Schneider CA, Pritchard AE, et al. The use of a pneumatic leg brace in soldiers with tibial stress fractures‐‐a randomized clinical trial. Military Medicine 2004; Vol. 169, issue 11:880‐4. [DOI] [PubMed]
- Allen CS, Hemphill NH, Kardouni JR, Schneider CA, Flynn TW, Pritchard AE, et al. A randomized controlled trial of a pneumatic leg brace versus traditional treatment in individuals with tibial stress fractures [abstract]. Journal of Orthopaedic & Sports Physical Therapy 2002;32(1):A3. [Google Scholar]
Andrish 1974 {published data only}
- Andrish JT, Bergfeld JA, Walheim J. A prospective study of the management of shin splints. Journal of Bone and Joint Surgery. American Volume 1974;56:1697‐700. [PubMed] [Google Scholar]
Bensel 1986 {unpublished data only}
- Bensel C, Kaplan DB. Wear test of boot inserts. Report No. STRNC‐ICH. Natrick (MA): US Army Natrick Research & Development Laboratories, 1986. [Google Scholar]
Finestone 1999 {published data only}
- Finestone A, Giladi M, Elad H, Salmon A, Mendelson S, Eldad A, et al. Prevention of stress fractures using custom biomechanical shoe orthoses. Clinical Orthopaedics & Related Research 1999;(360):182‐90. [DOI] [PubMed] [Google Scholar]
Finestone 2004a {published and unpublished data}
- Finestone A, Novack V, Farfel A, Berg A, Amir H, Milgrom C. A prospective study of the effect of foot orthoses composition and fabrication on comfort and the incidence of overuse injuries. Foot & Ankle International 2004;25(7):462‐6. [DOI] [PubMed] [Google Scholar]
- Milgrom C. personal communication October 20 2004.
Finestone 2004b {published and unpublished data}
- Finestone A, Novack V, Farfel A, Berg A, Amir H, Milgrom C. A prospective study of the effect of foot orthoses composition and fabrication on comfort and the incidence of overuse injuries. Foot & Ankle International 2004;25(7):462‐6. [DOI] [PubMed] [Google Scholar]
- Milgrom C. personal communication October 20 2004.
Gardner 1988 {published data only}
- Gardner LI, Dziados JE, Jones BH, Brundage JF, Harris JM, Sullivan R, et al. Prevention of lower extremity stress fractures: a controlled trial of shock absorbing insole. American Journal of Public Health 1988;78:1563‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffin MR 4th. On shock absorbent insoles to prevent bone fractures [letter; comment]. American Journal of Public Health 1989;79:1056‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Milgrom 1985 {published data only}
- Milgrom C, Giladi M, Kashtan H, Simkin A, Chisin R, Margulies J, et al. A prospective study of the effect of a shock absorbing orthotic device on the incidence of stress fractures in military recruits. Foot and Ankle 1985;6:101‐4. [DOI] [PubMed] [Google Scholar]
- Simkin A, Leichter I, Giladi M, Stein M, Milgrom C. Combined effect of foot arch structure and an orthotic device on stress fractures. Foot and Ankle 1989;10:25‐9. [DOI] [PubMed] [Google Scholar]
Milgrom 1992 {published data only}
- Milgrom C, Finestone A, Shlamkovitch N, Wosk J, Laor A, Voloshin A, et al. Prevention of overuse injuries of the foot by improved shoe shock attenuation. A randomized prospective study. Clinical Orthopaedics and Related Research 1992;(281):189‐92. [PubMed] [Google Scholar]
Mundermann 2001 {published data only}
- Mundermann A, Stefanyshyn DJ, Nigg BM. Relationship between footwear comfort of shoe inserts and anthropometric and sensory factors. Medicine & Science in Sports & Exercise 2001;33:1939‐45. [DOI] [PubMed] [Google Scholar]
Pope 1998 {published data only}
- Pope R, Herbert R, Kirwan J. Effects of ankle dorsiflexion range and pre‐exercise calf muscle stretching on injury risk in Army recruits. Australian Journal of Physiotherapy 1998;44(3):165‐72. [EMBASE AN: 1998321721] [DOI] [PubMed] [Google Scholar]
Pope 2000 {published data only}
- Pope RP, Herbert RD, Kirwan JD, Graham BJ. A randomized trial of preexercise stretching for prevention of lower‐limb injury. Medicine & Science in Sports & Exercise 2000;32(2):271‐7. [DOI] [PubMed] [Google Scholar]
Schwellnus 1990 {published data only}
- Schwellnus MP, Jordaan G, Noakes TD. Prevention of common overuse injuries by the use of shock absorbing insoles. American Journal of Sports Medicine 1990;18:636‐41. [DOI] [PubMed] [Google Scholar]
Schwellnus 1992 {published data only}
- Schwellnus MP, Jordaan G. Does calcium supplementation prevent bone stress injuries? A clinical trial. International Journal of Sport Nutrition 1992;2:165‐74. [DOI] [PubMed] [Google Scholar]
Slatyer 1995 {published data only}
- Slatyer M. Lower limb training injuries in an army recruit population [thesis]. Newcastle (NSW, Australia): Univ. of Newcastle, 1995. [Google Scholar]
Swenson 1997 {published data only}
- Swenson EJ, DeHaven KE, Sebastianelli WJ, Hanks G, Kalenak A, Lynch JM. The effect of a pneumatic leg brace on return to play in athletes with tibial stress fractures. American Journal of Sports Medicine 1997;25(3):322‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Amako 2003 {published data only}
- Amako M, Oda T, Masuoka K, Yokoi H, Campisi P. Effect of static stretching on prevention of injuries for military recruits. Military Medicine 2003;168(6):442‐6. [PubMed] [Google Scholar]
Bensel 1976 {published data only}
- Bensel CK. The effects of tropical and leather combat boots on lower extremity disorders among US Marine Corps recruits. Report No: TR 76‐49‐CEMEL. Massachusetts (MA): US Army, 1976. [Google Scholar]
Benson 1989 {published data only}
- Benson JE, Geiger CJ, Eiserman PA, Wardlaw GM. Relationship between nutrient intake, body mass index, menstrual function, and ballet injury. Journal of the American Dietetic Association 1989;89:58‐63. [PubMed] [Google Scholar]
Callison 2002 {published data only}
- Callison M Callison M. Clinical study: Acupuncture & tibial stress syndrome (Shin splints). Journal of Chinese Medicine 2002;70:24‐7. [Google Scholar]
Clark 1989 {published data only}
- Clark JE, Scott SG, Mingle M. Viscoelastic shoe insoles: Their use in aerobic dancing. Archives of Physical Medicine and Rehabilitation 1989;70(1):37‐40. [PubMed] [Google Scholar]
Ekenman 2002 {published data only}
- Ekenman I, Milgrom C, Finestone A, Begin M, Olin C, Arndt T, et al. The role of biomechanical shoe orthoses in tibial stress fracture prevention. American Journal of Sports Medicine 2002;30:866‐70. [DOI] [PubMed] [Google Scholar]
Giladi 1985 {published data only}
- Giladi M, Milgrom C, Danon Y, Aharanson Z. The correlation between cumulative march training and stress fractures in soldiers. Military Medicine 1985;150:600‐1. [PubMed] [Google Scholar]
- Milgrom C. personal communication September 4 2004.
Gray 2003 {published and unpublished data}
- Gray A, Rooney B, Drake P, Ingram R. A prospective study of conservative treatment options for tuberosity fractures of the fifth metatarsal [abstract]. Journal of Bone and Joint Surgery. British Volume 2003;85 Suppl 1:156‐7. [Google Scholar]
- Gray AC. Conservative treatment of fifth metatarsal fractures: a prospective study. In: The National Research Register, Issue 3, 2003. Oxford: Update Software.
Hartig 1999 {published data only}
- Hartig DE, Henderson JM. Increasing hamstring flexibility decreases lower extremity overuse injuries in military basic trainees. American Journal of Sports Medicine 1999;27:173‐6. [DOI] [PubMed] [Google Scholar]
Larsen 2002 {published data only}
- Larsen K, Weidich F, Lebouef‐Yde C. Can custom‐made biomechanic shoe orthoses prevent problems in the back and lower extremities? A randomised, controlled intervention trial of 146 military conscripts. Journal of Manipulative & Physiological Therapeutics 2002;25(5):326‐31. [DOI] [PubMed] [Google Scholar]
Nissen 1994 {published data only}
- Nissen LR, Astvad K, Madsen L. Low energy laser treatment of shin splints [Lavenergi‐laserbehandling af medialt tibialt stress‐syndrom]. Ugeskrift for Laeger 1994;156:7329‐31. [PubMed] [Google Scholar]
Pollock 1977 {published data only}
- Pollock ML, Gettman LR, Milesis CA. Effects of frequency and duration of training on attrition and incidence of injury. Medicine and Science in Sports and Exercise 1977;9:31‐6. [PubMed] [Google Scholar]
Popovich 2000 {published data only}
- Popovich RM, Gardner JW, Potter R, Knapik JJ, Jones BH. Effect of rest from running on overuse injuries in army basic training. American Journal of Preventive Medicine 2000;18:147‐55. [DOI] [PubMed] [Google Scholar]
Rudzki 1997 {published data only}
- Rudzki SJ. Injuries in Australian Army recruits. Part I. Decreased incidence and severity of injury seen with reduced running distance. Military Medicine 1997;162:472‐6. [PubMed] [Google Scholar]
- Rudzki SJ. Injuries in Australian Army recruits. Part II: Location and cause of injuries seen in recruits. Military Medicine 1997;162:477‐80. [PubMed] [Google Scholar]
- Rudzki SJ. Injuries in Australian Army recruits. Part III: The accuracy of a pretraining orthopedic screen in predicting ultimate injury outcome. Military Medicine 1997;162:481‐3. [PubMed] [Google Scholar]
Scully 1982 {published data only}
- Scully TJ, Besterman G. Stress fractures ‐ a preventable training injury. Military Medicine 1982;147:285‐7. [PubMed] [Google Scholar]
Sherman 1996 {published data only}
- Sherman RA, Karstetter KW, May H, Woerman AL. Prevention of lower limb pain in soldiers using shock‐absorbing inserts. Journal of the American Podiatric Medical Association 1996;86:117‐22. [DOI] [PubMed] [Google Scholar]
Smith 1985 {published data only}
- Smith W, Walter J, Bailey M. Effect of insoles in coastguard basic training footwear. Journal of the American Podiatry Association 1985;45:644‐7. [DOI] [PubMed] [Google Scholar]
Thompson 2004 {published data only}
- Thompson K. personal communication September 3 2004.
- Thompson KR, McVey E. Efficacy of shock absorbing boots to reduce lower extremity injuries in female Navy recruits [abstract]. Poster presented at the 51st Annual Meeting of the American College of Sports Medicine 2004 June 2‐5; Indianapolis, Indiana (http://www.acsm.org/meetings/annualmeeting.htm accessed 01/07/2004).
Tokki 2002 {published data only}
- Torkki M, Malmivarra A, Reivonen N, Seitsalo S, Laippala P, Hoikka V. Individually fitted sports shoes for overuse injuries among newspaper carriers. Scandinavian Journal of Work, Environment & Health 2002;28(3):176‐83. [DOI] [PubMed] [Google Scholar]
Van Mechelen 1993 {published data only}
- Mechelen W, Hlobil H, Kemper HC, Voorn WJ, Jongh HR. Prevention of running injuries by warm‐up, cool‐down, and stretching exercises. American Journal of Sports Medicine 1993;21(5):711‐9. [DOI] [PubMed] [Google Scholar]
Wedderkopp 1999 {published data only}
- Wedderkopp N, Kaltoft M, Lundgaard B, Rosendahl M, Froberg K. Prevention of injuries in young female players in European team handball. A prospective intervention study. Scandinavian Journal of Medicine & Science in Sports 1999;9(1):41‐7. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
London 2005 {published data only}
- Etherington J. A randomised controlled trial of the effectiveness of Air‐cast brace and the active rehabilitation versus conventional treatment for the lower limb stress fractures. In: National Research Register, Issue 1, 2005. Oxford: Update Software. Available at: http://www.nrr.nhs.uk/ViewDocument.asp?ID=N0013101035. [N001310135]
Wang 2001 {published data only}
- Wang B, Xu D, Sun C. [Therapeutic trial on function bandage for military training injuries]. Chung‐Hua Liu Hsing Ping Hseuh Tsa Chih [Chinese Journal of Epidemiology] 2001;22(6):408‐10. [PubMed] [Google Scholar]
References to ongoing studies
Owen 2004 {published and unpublished data}
- Owen DG, Duncan S, Clauss R, Etherington J. The effectiveness of a pneumatic brace in the rehabilitation of a tibial stress fracture [abstract]. Poster presented at the 51st Annual Meeting of the American College of Sports Medicine 2004 June 2‐5; Indianapolis, Indiana (http://www.acsm.org/meetings/annualmeeting.htm accessed 01/07/2004).
Additional references
Alderson 2004a
- Alderson P, Green S, Higgins JPT, editors. MEDLINE highly sensitive search strategies for identifying reports of randomized controlled trials in MEDLINE. Cochrane Reviewers' Handbook 4.2.2 [updated March 2004]; Appendix 5b. In: The Cochrane Library, Issue 2, 2004. Chichester, UK: John Wiley & Sons, Ltd.
Alderson 2004b
- Alderson P, Green S, Higgins JPT, editors. Verification of study eligibility. Cochrane Reviewers' Handbook 4.2.2 [updated March 2004]; Section 7.4.2. In: The Cochrane Library, Issue 2, 2004. Chichester, UK: John Wiley & Sons, Ltd.
Anderson 1996
- Anderson MW, Greenspan A. Stress fractures. Radiology 1996;199:1‐12. [DOI] [PubMed] [Google Scholar]
Begg 1996
- Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA 1996;276:637‐9. [DOI] [PubMed] [Google Scholar]
Bland 1997
- Bland JM, Kerry SM. Statistics notes. Trials randomised in clusters. BMJ 1997;315(7108):600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2004
- Campbell MK, Elbourne DR, Altman DG, for the CONSORT group. CONSORT statement: extension to cluster randomised trials. BMJ 2004;328:702‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Herbert 2002
- Herbert RD, Gabriel M. Effects of stretching before and after exercising on muscle soreness and risk of injury: systematic review. BMJ 2002;325:468‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG, for the CONSORT group. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357:1191‐4. [PubMed] [Google Scholar]
References to other published versions of this review
Gillespie 1999
- Gillespie WJ, Grant I. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. The Cochrane Library 1999, Issue 4. [DOI] [PubMed] [Google Scholar]


