Abstract
Background
Inadvertent perioperative hypothermia (a drop in core temperature to below 36°C) occurs because of interference with normal temperature regulation by anaesthetic drugs, exposure of skin for prolonged periods and receipt of large volumes of intravenous and irrigation fluids. If the temperature of these fluids is below core body temperature, they can cause significant heat loss. Warming intravenous and irrigation fluids to core body temperature or above might prevent some of this heat loss and subsequent hypothermia.
Objectives
To estimate the effectiveness of preoperative or intraoperative warming, or both, of intravenous and irrigation fluids in preventing perioperative hypothermia and its complications during surgery in adults.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (2014, Issue 2), MEDLINE Ovid SP (1956 to 4 February 2014), EMBASE Ovid SP (1982 to 4 February 2014), the Institute for Scientific Information (ISI) Web of Science (1950 to 4 February 2014), Cumulative Index to Nursing and Allied Health Literature (CINAHL) EBSCOhost (1980 to 4 February 2014) and reference lists of identified articles. We also searched the Current Controlled Trials website and ClinicalTrials.gov.
Selection criteria
We included randomized controlled trials or quasi‐randomized controlled trials comparing fluid warming methods versus standard care or versus other warming methods used to maintain normothermia.
Data collection and analysis
Two review authors independently extracted data from eligible trials and settled disputes with a third review author. We contacted study authors to ask for additional details when needed. We collected data on adverse events only if they were reported in the trials.
Main results
We included in this review 24 studies with a total of 1250 participants. The trials included various numbers and types of participants. Investigators used a range of methods to warm fluids to temperatures between 37°C and 41°C. We found that evidence was of moderate quality because descriptions of trial design were often unclear, resulting in high or unclear risk of bias due to inappropriate or unclear randomization and blinding procedures. These factors may have influenced results in some way. Our protocol specified the risk of hypothermia as the primary outcome; as no trials reported this, we decided to include data related to mean core temperature. The only secondary outcome reported in the trials that provided useable data was shivering. Evidence was unclear regarding the effects of fluid warming on bleeding. No data were reported on our other specified outcomes of cardiovascular complications, infection, pressure ulcers, bleeding, mortality, length of stay, unplanned intensive care admission and adverse events.
Researchers found that warmed intravenous fluids kept the core temperature of study participants about half a degree warmer than that of participants given room temperature intravenous fluids at 30, 60, 90 and 120 minutes, and at the end of surgery. Warmed intravenous fluids also further reduced the risk of shivering compared with room temperature intravenous fluids
Investigators reported no statistically significant differences in core body temperature or shivering between individuals given warmed and room temperature irrigation fluids.
Authors' conclusions
Warm intravenous fluids appear to keep patients warmer during surgery than room temperature fluids. It is unclear whether the actual differences in temperature are clinically meaningful, or if other benefits or harms are associated with the use of warmed fluids. It is also unclear if using fluid warming in addition to other warming methods confers any benefit, as a ceiling effect is likely when multiple methods of warming are used.
Keywords: Humans; Body Temperature; Administration, Intravenous; Anesthesia; Anesthesia/adverse effects; Hot Temperature; Hypothermia; Hypothermia/etiology; Hypothermia/prevention & control; Infusions, Intravenous; Infusions, Intravenous/methods; Randomized Controlled Trials as Topic; Shivering; Therapeutic Irrigation; Therapeutic Irrigation/methods
Plain language summary
Warmed fluids for preventing hypothermia during operations
During surgical operations, patients may become cold as the result of a combination of factors including the action of anaesthetic drugs, the presence of uncovered skin and the administration of cold fluids into the veins or to parts of the body where surgery is taking place to wash them. Becoming cold during surgery can be unpleasant and can cause excessive shivering after the operation. It can also cause heart problems and bleeding problems and can contribute to problems with pressure sores and wound healing and longer hospital stay. This review seeks to find out whether warming the fluids given into veins or used to wash parts of the body may prevent patients from becoming cold.
We searched medical databases up until February 2014 to find studies comparing warmed fluids with unwarmed fluids and other methods of warming the patient. We found 24 relevant trials with 1250 adult patients undergoing all types of surgery. We did not include studies for which it was intended that the patient would become cold (such as to facilitate heart bypass surgery). We had intended to collect data on which patients became hypothermic (when their body temperature dropped to below 36 degrees Celsius), but no trials reported this, so we collected data on patient temperatures at various time points throughout surgery.
We found evidence of moderate quality showing that if patients had the fluids they were given into their veins warmed up, they were about half a degree Celsius warmer and shivered less than those who received unwarmed fluids; however, we were unable to show a significant difference in patients who received warmed fluids to wash out parts of their bodies.
We have demonstrated that warming fluids does keep adult patients warmer; however it is unclear whether this alone can make a difference in the severe complications that becoming cold may cause.
Summary of findings
Summary of findings for the main comparison. Warmed intravenous fluids for preventing inadvertent perioperative hypothermia.
| Warmed intravenous fluids for preventing inadvertent perioperative hypothermia | |||||
| Patient or population: patients with inadvertent perioperative hypothermia Settings: any Intervention: warmed IV fluids | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Control | Warmed IV fluids | ||||
| Core temperature at 30 minutes after induction degrees Celsius | Mean temperature at 30 minutes in the control groups was 36.0°C | Mean temperature at 30 minutes in the intervention groups was 0.41 higher (0.24 to 0.57 higher) | ‐ | 374 (9 studies) | ⊕⊕⊕⊝ Moderatea |
| Core temperature at 60 minutes after induction degrees Celsius | Mean temperature at 60 minutes in the control groups was 35.9°C | Mean temperature at 60 minutes in the intervention groups was 0.51 higher (0.33 to 0.69 higher) | ‐ | 312 (8 studies) | ⊕⊕⊕⊝ Moderatea |
| Core temperature at 90 minutes after induction degrees Celsius | Mean temperature at 90 minutes in the control groups was 35.9°C | Mean temperature at 90 minutes in the intervention groups was 0.54 higher (0.04 to 1.04 higher) | ‐ | 109 (3 studies) | ⊕⊕⊕⊝ Moderatea |
| Core temperature at 120 minutes after induction degrees Celsius | Mean temperature at 120 minutes in the control groups was 35.8°C | Mean temperature at 120 minutes in the intervention groups was 0.74 higher (0.31 to 1.17 higher) | ‐ | 149 (4 studies) | ⊕⊕⊕⊝ Moderatea |
| Core temperature at end of procedure/arrival to PACU ‐ simple design degrees Celsius | Mean temperature at end of procedure/arrival to PACU ‐ simple design in the control groups ‐ was 35.7°C | Mean temperature at end of procedure/arrival to PACU ‐ simple design in the intervention groups was 0.63 higher (0.28 to 0.98 higher) | ‐ | 682 (11 studies) | ⊕⊕⊕⊝ Moderatea |
| Patient‐reported outcome: shivering various tools | Study population | RR 0.39 (0.23 to 0.67) | 428 (9 studies) | ⊕⊕⊕⊝ Moderatea | |
| 370 per 1000 | 144 per 1000 (85 to 248) | ||||
| Median | |||||
| 440 per 1000 | 172 per 1000 (101 to 295) | ||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | |||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
aMost trials had unclear risk of bias with some likelihood of selection bias.
Summary of findings 2. Warmed irrigation fluids for preventing inadvertent perioperative hypothermia.
| Warmed irrigation fluids for preventing inadvertent perioperative hypothermia | |||||
| Patient or population: patients with inadvertent perioperative hypothermia Settings: any Intervention: warmed irrigation fluids | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Control | Warmed irrigation fluids | ||||
| Temperature at end of procedure /arrival in PACU | Mean temperature at end of procedure/arrival to PACU ‐ simple design in the control groups was 36.2°C | Mean temperature at end of procedure/arrival to PACU in the intervention groups was 0.24 higher (‐0.06 to 0.55 higher) | 310 (5 studies) | ⊕⊕⊕⊝ Moderatea | |
| Event rate of shivering various tools | Mean control group risk from studies | RR 0.09 (0.01 to 1.55) | 102 (2 studies) | ⊕⊕⊕⊝ Lowa,b | |
| 100 per 1000 | 9 per 1000 (1 to 155) | ||||
| Control group risk from study with events | |||||
| 217 per 1000 | 20 per 1000 (2 to 336) | ||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | |||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
aMost trials had unclear risk of bias, with some concern that selection bias may result.
bQuality of data has been downgraded further as the result of imprecision.
Background
Inadvertent perioperative hypothermia occurs because of interference with normal temperature regulation by anaesthetic drugs and exposure of skin for prolonged periods. Several interventions have been proposed to maintain body temperature by reducing heat loss or causing active warming, or both.
Description of the condition
Regulation of temperature
Body temperature is usually maintained between 36ºC and 37.5ºC by balancing the body's heat losses and gains. Heat is gained as a product of metabolism, including that associated with muscular activity. Heat is lost through convection, conduction and radiation from the skin, by evaporation through sweating and, to a lesser extent, through the respiratory tract. To maintain this balance, information from temperature sensors in deep tissues and in the skin is processed in the brain. Heat loss is increased mainly through sweating and increased blood flow through the skin. Heat loss is reduced by reducing blood flow through the skin and by increasing heat production, mainly by inducing muscular activity (shivering) and increasing the basal metabolic rate (the background rate of energy used by a person at rest).
A useful concept involving heat regulation is that the body has a central compartment comprising the major organs, where temperature is tightly regulated, and a peripheral compartment, where temperature varies widely. Typically the periphery may be 2ºC to 4ºC cooler than the core compartment.
Effects of perioperative care and anaesthesia on thermal regulation
Exposure of the skin during the perioperative period can increase heat loss. Furthermore, cool intravenous and irrigation fluids and possibly inspired or insufflated (blown into body cavities) gases may directly cool patients. During exposure to cold, blood vessels are vasoconstricted (narrowed). Sedatives and anaesthetic agents inhibit the normal response to cold, effectively resulting in improved blood flow to the peripheries and increased heat loss. During the early part of anaesthesia, these effects are seen as a rapid decrease in core temperature caused by redistribution of heat from the central to the peripheral compartment. This early decrease is followed by a more gradual decline, reflecting ongoing heat loss. With epidural or spinal analgesia, peripheral blockade of vasoconstriction (narrowing of blood vessels) below the level of the nerve block results in vasodilatation (widening of blood vessels) and therefore greater ongoing heat loss and reduced heat production due to anaesthesia.
Risk of inadvertent perioperative hypothermia varies widely, for example, reports from audits describe a risk of 1.5% (Al‐Qahtani 2011) to 20% (Harper 2008). Individuals who are most susceptible to heat loss include the elderly, patients with greater anaesthetic risk (American Society of Anesthesiologists (ASA) grade III to IV), people with cachexia (loss of body mass due to increased metabolic rate associated with cancer and other chronic conditions), burn victims, patients with hypothyroidism and those affected by corticoadrenal insufficiency.
Perioperative hypothermia complications
By altering various systems and functions, hypothermia may result in increased morbidity. Patients often comment on subsequent shivering upon awakening from anaesthesia as one of the most uncomfortable immediate postoperative experiences. Shivering originates as a response to cold and is the result of involuntary muscular activity with the objective of increasing metabolic heat (Sessler 2001).
Cardiac complications are the principal causes of morbidity during the postoperative phase. Prolonged ischaemia (reduced blood flow) is usually associated with cellular damage; for this reason, it seems likely that treating factors that can lead to such complications, like body temperature, is important. Hypothermia stimulates the release of noradrenaline, causing peripheral vasoconstriction and hypertension (Sessler 1991; Sessler 2001) ‐ factors that favour or increase the chances of myocardial ischaemia (with reduced blood supply to the heart muscle). It appears that the increased risk of cardiac complications can be reversed by maintenance of normothermia (Frank 1997).
Some studies have shown that intraoperative hypothermia accompanied by vasoconstriction constitutes an independent factor that slows wound healing and increases the risk of surgical wound infection (Kurz 1996; Melling 2001).
Even moderate hypothermia (35ºC) can alter physiological coagulation mechanisms by affecting platelet function and modifying enzymatic reactions. Decreased platelet activity results in increased bleeding and a greater need for transfusion (Rajagopalan 2008). Moderate hypothermia can also reduce the metabolic rate, manifesting as a prolonged effect of certain drugs that are used during anaesthesia and some uncertainty about their effects. This is particularly significant for elderly patients (Heier 1991; Heier 2006; Leslie 1995).
For the above reasons, inadvertent non‐therapeutic hypothermia is considered an adverse effect of general and regional anaesthesia (Bush 1995; Putzu 2007; Sessler 1991). Body temperature is therefore frequently monitored to assist maintenance of normothermia during surgery and timely detection of the appearance of unintended hypothermia.
Description of the intervention
The objective of preserving patients' body heat during anaesthesia and surgery is to minimize heat loss by reducing radiation and convection from the skin, evaporation from exposed surgical areas and cooling caused by the introduction of cold intravenous fluids, irrigation fluids or cold gases for respiration or insufflation of body cavities.
During surgery, patients may receive large volumes of intravenous and irrigation fluids. If these fluids are cold or are provided at room temperature, they can cause significant heat loss. Warming these fluids to body temperature or slightly above by using prewarmed fluids or in‐line warming can prevent some of this heat loss and subsequent hypothermia. These fluids may be warmed by a number of different mechanisms. Warming is part of a series of interventions provided to minimize heat loss that can be classified as follows:
Interventions to decrease redistribution of heat and subsequent heat loss (i.e. preoperative pharmacological vasodilatation and prewarming of the skin before anaesthesia).
Passive warming systems aimed at reducing heat loss and thus preventing hypothermia, including changes in environmental temperature, passive insulation by covering exposed body surfaces and closed or semi closed anaesthesia circuits with low flows.
Active warming systems aimed at transferring heat to the patient. The effectiveness of these systems might depend on various factors such as the design of the machine, the type of heat transfer performed, placement of the system over the patient and total body area covered in the heat exchange. The following systems are used for active warming: infrared lights, electric blankets, mattresses or blankets with warm water circulation, forced air warming or convective air warming transfer, warming of intravenous and irrigation fluids, warming and humidifying of anaesthetic air and warming of carbon dioxide (CO2) in laparoscopic surgery.Intravenous nutrients have been proposed as a way of inducing increased metabolism and thus energy production.
Why it is important to do this review
The clinical effectiveness of the different types of patient warming devices that can be used has been assessed in a very extensive guideline commissioned by the National Institute for Health and Care Excellence (NICE) in the UK (NICE 2008). The report concludes that evidence of clinical effectiveness and cost‐effectiveness is sufficient for recommendations to be made on the use of forced air warming to prevent and treat perioperative hypothermia. Nevertheless, most of the data have been derived from intermediate outcomes such as temperature. The search for evidence covered studies reported to the year 2007 and so needs updating.
This review is one of several reviews conducted to explore this topic (Alderson 2014; Campbell 2012a; Warttig 2012). Cochrane reviews have covered warming of gases used in minimally invasive abdominal surgery (Birch 2011) and use of warmed and humidified inspired gases in ventilated adults (Kelly 2010); a review on active warming is in planning stages (Urrútia 2011). Remaining areas to be covered include the following.
Preoperative or intraoperative thermal insulation, or both.
Preoperative or intraoperative warming, or both, of intravenous and irrigation fluids.
Preoperative or intraoperative pharmacological interventions, or both, including intravenous nutrients.
Postoperative treatment for inadvertent hypothermia.
Objectives
To estimate the effectiveness of preoperative or intraoperative warming, or both, of intravenous and irrigation fluids in preventing perioperative hypothermia and its complications during surgery in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) or quasi‐randomized controlled trials (such as allocation by alternation) of interventions used in the preoperative period (one hour before induction of anaesthesia), the intraoperative period (total anaesthesia time) or both.
Types of participants
We included adults (over 18 years of age) undergoing elective or emergency surgery (including surgery for trauma) under general or regional (central neuraxial block) anaesthesia, or both.
The following groups were not covered.
Patients who had been treated with therapeutic hypothermia (e.g. use of cardiopulmonary bypass).
Patients undergoing operative procedures under local anaesthesia.
Patients with isolated severe head injury resulting in impaired temperature control.
Patients with burns who are undergoing surgery (e.g. for skin grafting).
Types of interventions
For the purposes of this review, 'warmed intravenous fluids' includes all methods of warming fluids before administration to the patient. 'Warmed irrigation fluids' includes any irrigation fluids administered to a body cavity that is warmed by any method, such as in‐line fluid warmers or a warming cabinet. We included studies in which intravenous fluid warming was commenced up to one hour before anaesthesia was commenced. We expected use of irrigation fluids to be exclusive to the intraoperative period.
Comparisons of interest include warmed intravenous fluids and irrigation fluids versus the following.
Other warmed fluid interventions.
Standard care: cotton sheets or blankets, wool blankets, other non‐reflective textiles.
Thermal insulation or passive warming: reflective and non‐reflective blankets, suits and head covering.
Active warming: forced air warmers, electric mattresses and blankets, radiant heaters, warm water mattresses or blankets.
Preoperative or intraoperative warming, or both, of inspired and insufflated gases.
Preoperative and intraoperative pharmacological interventions including ketamine, calcium channel blockers, intravenous nutrients and opiates.
We excluded studies that provided multiple interventions such as fluid warming and reflective blanket versus no fluid warming and no reflective blanket. We included studies in which the difference between groups consisted of only one intervention, such as fluid warming and reflective blanket versus no fluid warming and reflective blanket. Intravenous fluids and irrigation fluids were regarded as two separate interventions.
Types of outcome measures
Primary outcomes
Risk of hypothermia at any point during surgery and temperature at the end of surgery or on admission to postanaesthesia care (mild, core temperature 35.0ºC to 35.9ºC; moderate, 34.0 ºC to 34.9 ºC; severe, < 34.0ºC) measured at the direct tympanic membrane, bladder, oesophagus, pulmonary artery, nasopharynx or rectum. As no data were found on rates of hypothermia, we made a post hoc decision to use data reporting mean core temperatures at various time points during and after surgery.
Major cardiovascular complications (cardiovascular death, non‐fatal myocardial infarction, non‐fatal stroke and non‐fatal cardiac arrest).
Secondary outcomes
Infection and complications of the surgical wound (wound healing and dehiscence), as defined by study authors.
Pressure ulcers, as defined by study authors.
Bleeding complications (blood loss, transfusions, coagulopathy).
Other cardiovascular complications (bradycardia, new arrhythmias).
Patient‐reported outcomes (i.e. shivering, anxiety, comfort in postsurgical wake‐up, etc.).
All‐cause mortality at the end of the study.
Length of stay (in postanaesthesia care unit, hospital).
Unplanned high dependency or intensive care admission.
Adverse effects including temperature greater than 37.5ºC, burns or feeling too hot.
Search methods for identification of studies
We conducted a single search across the suite of reviews on this topic (thermal insulation, warmed fluids and treatment of inadvertent perioperative hypothermia) with the following strategy, which was refined following a cross‐check with studies included in the UK National Institute for Health and Care Excellence (NICE) guidelines on this topic (NICE 2008).
Electronic searches
To identify eligible randomized clinical trials, we searched the following electronic databases in June 2011, June 2012, February 2013, November 2013 and February 2014: the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (February 2014; see Appendix 1); MEDLINE Ovid SP (1956 to February 2014; see Appendix 2); EMBASE Ovid SP (1982 to February 2014; see Appendix 3); the Institute for Scientific Information (ISI) Web of Science (1950 to February 2014; see Appendix 4); and the Cumulative Index to Nursing and Allied Health Literature (CINAHL EBSCOhost) (1980 to February 2014; see Appendix 5). In searching the databases, we used both subject headings and free text terms with no language or date restrictions. We adapted our MEDLINE search strategy for searching all other databases.
Searching other resources
To identify additional published, unpublished and ongoing studies, we searched the Science Citation Index and checked the references of relevant studies and reviews. We also searched the databases of ongoing trials, such as:
Current Controlled Trials; and
Clinicaltrials.gov.
Data collection and analysis
Selection of studies
For new searches, we (PA, GC and SW) independently sifted results of the literature searches to identify relevant studies such that each record was reviewed by two people. This was done once for all interventions, and the interventions were recorded on a data extraction form (see Appendix 6). If an article could not be excluded by review of the title and abstract, we retrieved a full copy of the article. We recorded reasons for exclusion and resolved disagreements about inclusion or exclusion by discussion involving another review author (AS) if necessary.
Data extraction and management
We (PA, GC and SW) independently extracted relevant data onto a data extraction form and resolved disagreements by discussion or by consultation with a clinical expert (AS).
One review author (GC) entered data into RevMan, and SW and PA checked for transcription errors.
We extracted the following data.
General information, such as title, study authors, contact address, publication source, publication year and country.
Methodological characteristics and study design.
Clinical and demographic characteristics of study participants.
Descriptions of the intervention and the control, including information on type of surgery, duration, surgical team experience and prophylactic antibiotic administration, when available.
Outcome measures, as noted above.
Results for each study group.
Assessment of risk of bias in included studies
We (PA, GC and SW) independently assessed risk of bias for each study (those included in the NICE guideline and newly identified studies) using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion or by involving a third assessor (AS).
We considered trials as having low risk of bias if all of the following criteria were assessed as adequate. We considered trials as having high risk of bias if one or more of the following criteria were not assessed as adequate.
Random sequence generation (checking for possible selection bias). We described for each included study the method used to generate the allocation sequence when reported in sufficient detail to allow an assessment of whether it should produce comparable groups. We assessed the methods as adequate (any truly random process, e.g. random number table, computer random number generator); inadequate (any non‐random process, e.g. odd or even date of birth, hospital or clinic record number); or unclear.
Allocation concealment (checking for possible selection bias). We described for each included study the method used to conceal the allocation sequence when reported in sufficient detail and determined whether intervention allocation could have been foreseen in advance of or during recruitment, or changed after assignment. We assessed the methods as adequate (e.g. telephone or central randomization, consecutively numbered sealed opaque envelopes); inadequate (open random allocation, unsealed or non‐opaque envelopes, alternation, date of birth); or unclear.
Blinding of participants and personnel (checking for possible performance bias). We described for each included study the methods used, if any, to blind participants and personnel from knowledge of which intervention a participant received. We also provided information on whether the intended blinding was effective. When blinding was not possible, we assessed whether lack of blinding was likely to have introduced bias. Blinding was assessed separately for different outcomes or classes of outcomes. We assessed the methods as adequate; inadequate; or unclear.
Blinding of outcome assessment (checking for possible detection bias). We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We also provided information on whether the intended blinding was effective. Blinding was assessed separately for different outcomes or classes of outcomes. We assessed the methods as adequate; inadequate; or unclear.
Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts and protocol deviations). We described for each included study and for each outcome the completeness of data, including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total number of randomly assigned participants), reasons for attrition or exclusion when reported and whether missing data were balanced across groups or were related to outcomes. When sufficient information was reported or supplied by the trial authors, we planned to include missing data in the analyses. We considered intention‐to‐treat (ITT) analysis as adequate if all dropouts or withdrawals were accounted for, and as inadequate if the number of dropouts or withdrawals was not stated, or if reasons for dropouts or withdrawals were not stated.
Selective reporting. We reported for each included study which outcomes of interest were and were not reported. We did not search for trial protocols.
Other bias. We described for each included study any important concerns that we have about other possible sources of bias. We assessed whether each study was free of other problems that could put it at risk of bias: yes; no; or unclear.
With reference to (1) to (7) above, we considered the likely magnitude and direction of bias when study findings are interpreted. We planned to explore the impact of the level of bias by undertaking sensitivity analyses (see Sensitivity analysis).
The quality of data for each outcome was assessed according to GRADE (Grades of Recommendation, Assessment, Development and Evaluation) principles and was ranked as high, moderate, low or very low. To make this assessment, we considered risk of bias, imprecision, inconsistency, indirectness and publication bias. Quality of the evidence was downgraded from high if flaws were identified in any of these domains.
Measures of treatment effect
We analysed dichotomous data using risk ratios (RRs) and continuous data using mean differences (MDs). For both, we used 95% confidence intervals (CIs) around the point estimate.
Unit of analysis issues
All trials were randomized by individual, and outcome data were reported for participants.
Dealing with missing data
We analysed available data on an ITT basis.
Assessment of heterogeneity
Before obtaining pooled estimates of relative effects, we carried out a statistical heterogeneity analysis by assessing the value of the I2 statistic, thereby estimating the percentage of total variance across studies that is due to heterogeneity rather than to chance (Higgins 2002). We considered a value greater than 30% as a sign of important heterogeneity, and if present, we sought an obvious explanation for the heterogeneity by considering the design of the trials. We also considered heterogeneity in terms of the clinical importance of variations in temperature and the overall pattern of direction of effect.
Assessment of reporting biases
We recorded the number of included studies that reported each outcome but did not use statistical techniques to try to identify the presence of publication bias. We planned that if we identified more than 10 studies for a comparison, we would generate a funnel plot and analyse it by visual inspection.
Data synthesis
We used DerSimonian and Laird random‐effects model meta‐analyses of risk ratios in RevMan 5.3 for dichotomous data and mean differences for continuous data. Pooled estimates had a 95% confidence interval
Subgroup analysis and investigation of heterogeneity
We performed subgroup analysis for pregnant women. Data were insufficient to allow additional subgroup analyses (such as type/duration of anaesthesia, timing of application of the intervention, participant age, American Society of Anesthesiologists (ASA) score, urgency of surgery, type of surgery, prewarmed versus in‐line warmed fluids and temperature of the fluid).
Sensitivity analysis
We planned to carry out sensitivity analysis according to study methodological quality (for trials with low risk of bias) but did not complete this because of lack of variation in study quality.
Summary of findings tables
We constructed a 'Summary of findings' table by choosing seven of the 10 outcomes for which we found the most clinically useful data, but including the two primary outcomes, irrespective of whether we found any useful data.
Results
Description of studies
Results of the search
We carried out the search for this review as part of a single search for three related reviews on prevention and treatment of perioperative hypothermia (Alderson 2014; Campbell 2012a; Warttig 2012). Figure 1 summarizes the search results, combined for searches conducted in June 2011, June 2012, February 2013, November 2013 and February 2014. These searches identified a total of 4094 hits. For this review, we retrieved 46 papers for consideration and included 24 studies in the review, 21 of which provided some quantitative data.
1.
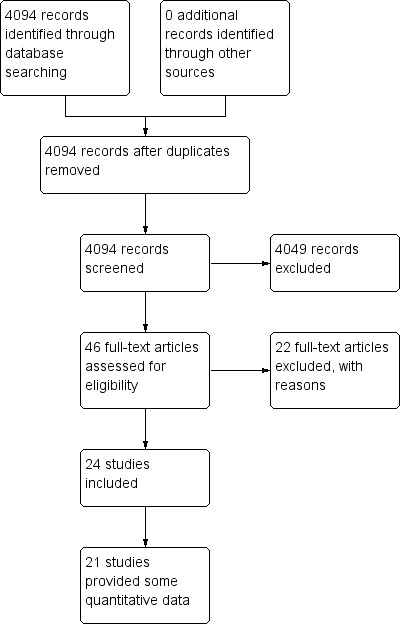
Study flow diagram.
We tried to contact the authors of three studies (Andrzejowski 2010; Demir 2002; Moore 1997) to clarify details but were unable to contact them or found that they were not able to provide further information.
Included studies
A total of 24 studies with 1250 participants are included in this review, but only 21 of these contributed useable quantitative outcome data to the analyses (1150 participants). The other three studies presented data as inadequately labelled graphs, percentage changes in temperature or differences between baseline and minimum temperature. We have listed the excluded studies in the Excluded studies section. A total of 1190 participants were involved in the studies included in the analyses. Nine studies (Camus 1996; Demir 2002; Kelly 2000; Moore 1997; Shao 2012; Smith 1998b; Xu 2010; Yamakage 2004; Yokoyama 2009) had 20 or fewer participants in each arm. Two studies were conducted in the UK, five in the USA, two in Japan, three in Korea, two in China, two in Iran and one in each of France, Brazil, Turkey, Denmark, Canada, Germany and Nigeria. All surgeries were elective and were provided for patients classified as ASA I to III. A mix of general and regional anaesthesia was reported. Surgeries were both major and minor and included abdominal, gynaecological, urological and orthopaedic. One study (Jeong 2008) included participants who underwent off‐pump cardiac surgery. Most studies excluded patients with medical morbidity, such as thyroid disease, acute illness and central causes for abnormal temperature regulation.
Seventeen studies contributed data on comparisons of warmed and unwarmed intravenous fluids (Andrzejowski 2010; Camus 1996; Chung 2012; De Mattia 2013; Hasankhani 2007; Jeong 2008; Jorgenson 2000; McCarroll 1986; Muth 1996; Oshvandi 2011; Shao 2012; Smith 1998a; Smith 1998b; Woolnough 2009; Xu 2010; Yamakage 2004, Yokoyama 2009). Six of these included 372 women (Chung 2012; Jorgenson 2000; McCarroll 1986; Oshvandi 2011; Woolnough 2009; Yokoyama 2009) undergoing elective caesarean section and formed a separate subgroup. Yamakage 2004 was the only study that looked at hydroxyethyl starch solutions as well as haemodilutional autotransfusion. We included these data in the meta‐analysis, but it is worth noting that starch solutions have been withdrawn from use in the UK.
Five studies compared warmed and unwarmed irrigation fluids for a variety of operations ‐ arthroscopic knee surgery (Kelly 2000), arthroscopic shoulder surgery (Kim 2009), gynaecological laparoscopy (Moore 1997) and transurethral resection of the prostate (Jaffe 2001). One trial of 160 participants undergoing elective abdominal procedures (Shao 2012) had a complex design, with 32 treatment groups, each receiving some combination of five different interventions. From this, we pooled results in which intravenous fluid or warmed irrigation fluid was the only difference. Eligible studies were insufficient to allow any subgroup analysis in the warmed irrigation comparison.
For one trial (Woolnough 2009), we pooled two groups with warmed fluid ‐ one with pre‐warmed fluid and the other with in‐line fluid warming. This was also the case for Andrzejowski 2010, although those data were unsuitable for meta‐analysis.
A major issue was that a wide range of co‐interventions were used in the studies, such as active warming or warmed inspired gases, but we included only studies for which warmed fluid was found to be the only difference between the two groups. A wide range of methods of warming included prewarmed fluids and various devices for in‐line warming; fluids were warmed to a range of temperatures between 37°C and 41°C. All methods of warming and temperatures were considered as a single group. (See Characteristics of included studies for details of studies.)
Excluded studies
We excluded 22 studies largely because reading of full text revealed that the comparison was not included in the review. (See Characteristics of excluded studies for details of studies.)
Ongoing studies
We identified no ongoing studies.
Studies awaiting classification
We identified no studies awaiting classification.
Risk of bias in included studies
We have presented summaries of the judgements for risk of bias in Figure 2 and Figure 3. We have provided details of included studies in the Characteristics of included studies section.
2.
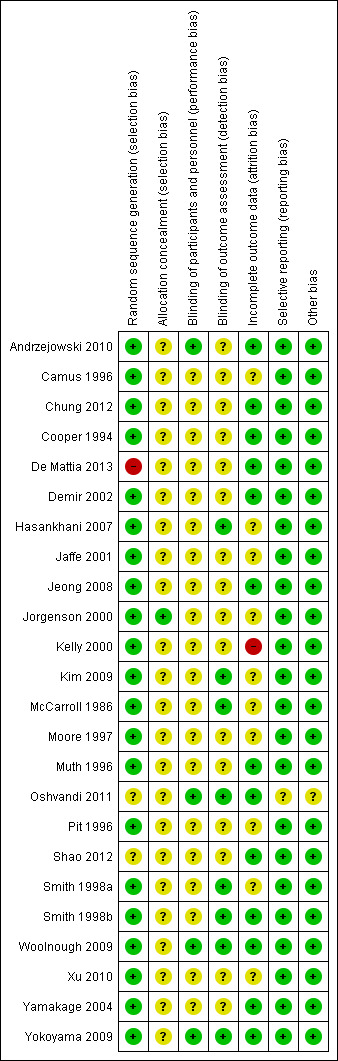
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
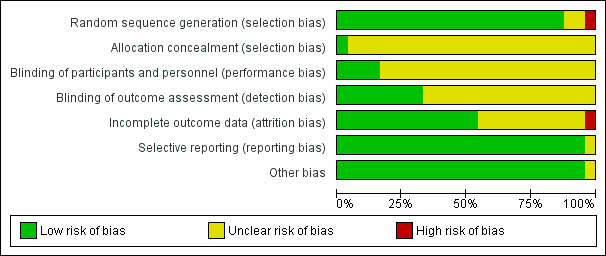
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Reporting of allocation concealment was largely unclear, making it difficult for review authors to come to an overall view of the likelihood of selection bias. No obvious imbalances in the groups can be seen in the tables of demographic data, but this does not rule out selection bias.
Blinding
We made an overall judgement about performance and detection bias, as no clear indication suggested that blinding was different for different outcomes. Most trials did not report blinding, perhaps because it is difficult to blind participants (particularly under regional analgesia only) and clinicians to the intervention used.
Incomplete outcome data
The trials were of fairly short duration and were conducted in highly controlled environments; attrition did not occur to any serious extent. Risk of bias due to attrition was therefore low.
Selective reporting
We found no definitive evidence of selective reporting but did not seek out trial protocols. Few of the outcomes that we hoped to find were reported, but we are unclear whether the data were collected.
Other potential sources of bias
We identified no other definitive sources of potential bias.
Effects of interventions
Warmed intravenous fluids versus room temperature intravenous fluids
Primary outcomes
Risk of hypothermia
This outcome was not reported by any of the included trials. We made a post hoc decision to use mean core temperature as our primary outcome (Differences between protocol and review).
Major cardiovascular outcomes
This outcome was not reported by any of the included trials.
Core temperature
Our protocol specified risk of hypothermia as the primary outcome. As no trials reported this, we decided to include data related to mean core temperature instead, as this was reported by most of the included studies. We decided to summarize data by presenting weighted mean difference at 30, 60, 90 and 120 minutes after induction of anaesthesia and at the end of surgery/admission to the postanaesthesia care unit (PACU).
Important heterogeneity was present in most of the analyses (ranging from I² = 58% to 94%), but we decided to continue with pooling of results, as the absolute differences in individual trial results were relatively small and were in the same direction of effect. We also performed sensitivity analysis by removing outlying studies and found that inclusion or exclusion of outliers did not change the conclusions we would draw. Thus all included studies remained in all analyses.
30 minutes after induction
Nine trials (Camus 1996; McCarroll 1986; Oshvandi 2011; Smith 1998a; Smith 1998b; Woolnough 2009; Xu 2010; Yamakage 2004; Yokoyama 2009) (n = 374) compared warmed intravenous fluids versus room temperature intravenous fluids at 30 minutes after induction of anaesthesia (Analysis 1.1). Overall, among people undergoing all types of surgery, those receiving warmed intravenous fluids had a higher core temperature at 30 minutes than those receiving room temperature intravenous fluids, but this difference was less than half a degree (MD = 0.41°C, 95% CI 0.24 to 0.57; moderate‐quality evidence). Important heterogeneity was present in the analysis (I² = 88%, P value < 0.001).
1.1. Analysis.
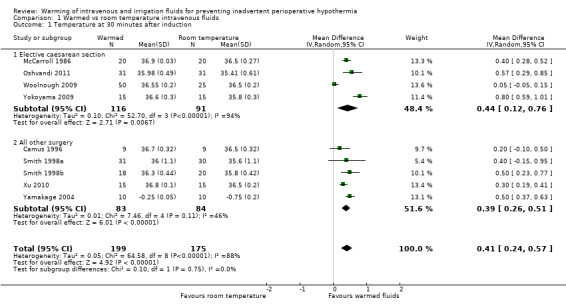
Comparison 1 Warmed vs room temperature intravenous fluids, Outcome 1 Temperature at 30 minutes after induction.
It was possible to perform planned subgroup analyses for this time point, but lack of data meant that this was possible only for the subgroup of women undergoing elective caesarean section, not for men and women undergoing all other types of surgery. Tests of subgroup differences showed no significant differences between the two subgroups (P value = 0.75).
60 minutes after induction
Eight trials (Camus 1996; Jeong 2008; Smith 1998a; Smith 1998b; Woolnough 2009; Xu 2010; Yamakage 2004; Yokoyama 2009) (n = 312) compared warmed intravenous fluids versus room temperature intravenous fluids at 60 minutes after induction of anaesthesia (Analysis 1.2). Overall, among people undergoing all types of surgery, those receiving warmed intravenous fluids were about half a degree warmer at 60 minutes than those receiving room temperature intravenous fluids (MD = 0.51°C, 95% CI 0.33 to 0.69; moderate‐quality evidence). Again, important heterogeneity was present in the analysis (I² = 83%, P value < 0.001).
1.2. Analysis.
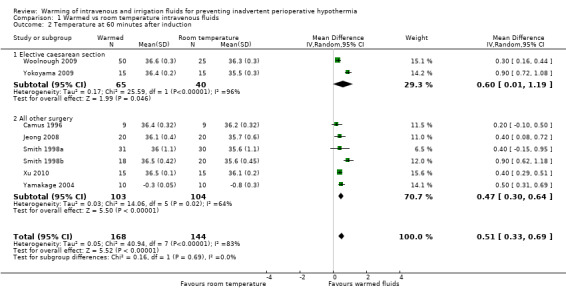
Comparison 1 Warmed vs room temperature intravenous fluids, Outcome 2 Temperature at 60 minutes after induction.
It was possible to perform planned subgroup analyses, but lack of data meant that this was possible only for a subgroup of women undergoing elective caesarean section, not for men and women undergoing all other types of surgery. Tests of subgroup differences showed no statistically significant differences between the two subgroups (P value = 0.69).
Demir 2002 also reported core temperature at 60 minutes after induction of anaesthesia for the warmed intravenous fluids group (n = 9, mean = 35.4°C) compared with the room temperature intravenous fluids group (n = 9, mean 35°C) but did not report measures of dispersion to enable inclusion in the meta‐analysis.
90 minutes after induction
Three trials (Camus 1996; Smith 1998a; Xu 2004) (n = 109) compared warmed intravenous fluids versus room temperature intravenous fluids at 90 minutes after induction of anaesthesia (Analysis 1.3). A statistically significant difference in core temperature was noted, with participants in the warmed intravenous fluids group about half a degree warmer than those in the room temperature group (MD = 0.54°C, 95% CI 0.04 to 1.04; moderate‐quality evidence).
1.3. Analysis.
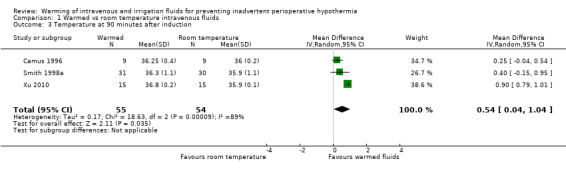
Comparison 1 Warmed vs room temperature intravenous fluids, Outcome 3 Temperature at 90 minutes after induction.
Demir 2002 also reported core temperature at 90 minutes after induction of anaesthesia for the warmed intravenous fluids group (n = 9, mean = 35.4°C) compared with the room temperature intravenous fluids group (n = 9, mean 34.8°C) but did not report measures of dispersion to enable inclusion in the meta‐analysis.
120 minutes after induction
Four trials (Camus 1996; Jeong 2008; Smith 1998a; Xu 2004) (n = 149) compared warmed intravenous fluids versus room temperature intravenous fluids at 120 minutes after induction of anaesthesia (Analysis 1.4). A statistically significant difference in core temperature was noted between the two groups, with participants in the warmed intravenous fluids group over half a degree warmer than those in the room temperature group (MD = 0.74°C, 95% CI 0.31 to 1.17; moderate‐quality evidence). Important heterogeneity was present in the analysis (I² = 79%, P value < 0.001).
1.4. Analysis.

Comparison 1 Warmed vs room temperature intravenous fluids, Outcome 4 Temperature at 120 minutes after induction.
Demir 2002 also reported core temperature at 120 minutes after induction of anaesthesia for the warmed intravenous fluids group (n = 9, mean = 35.3°C) compared with the room temperature intravenous fluids group (n = 9, mean 34.6°C) but did not report measures of dispersion to enable inclusion in the meta‐analysis.
End of surgery/arrival to post anaesthesia care unit (PACU)
A total of 11 trials (Camus 1996; De Mattia 2013; Hasankhani 2007; Jorgenson 2000; Muth 1996; Oshvandi 2011; Shao 2012; Smith 1998a; Smith 1998b; Xu 2010; Yokoyama 2009) (n = 682) compared warmed intravenous fluids versus room temperature intravenous fluids at end of surgery/arrival to the PACU (Analysis 1.5). A statistically significant difference in core temperature was noted between the two groups, with those in the warmed intravenous fluids group over half a degree warmer than those in the room temperature group (MD = 0.63°C, 95% CI 0.28 to 0.98; moderate‐quality evidence). Important heterogeneity was evident in the result (I² = 96%, P value < 0.001).
1.5. Analysis.
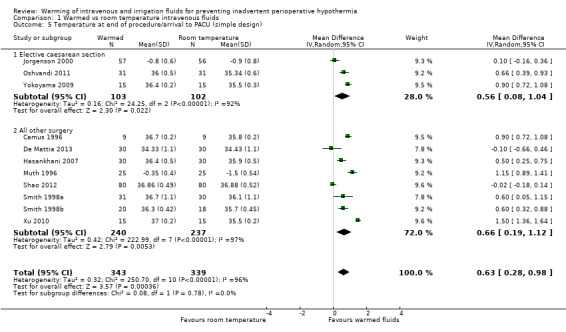
Comparison 1 Warmed vs room temperature intravenous fluids, Outcome 5 Temperature at end of procedure/arrival to PACU (simple design).
Subgroup analysis was possible for women undergoing elective caesarean section compared with men and women undergoing all other types of surgery. Tests of subgroup differences showed no significant differences between the two subgroups (P value = 0.78).
Andrzejowski 2010 reported the core temperature difference at the end of surgery/arrival to PACU for intravenous fluids at room temperature (n = 25, median = 35.7°C), warmed by an in‐line warmer (n = 25, median = 35.9°C), and warmed by a warming cabinet (n = 26, 36.1°C). Insufficient data were provided by the study to enable pooling of data in the main meta‐analysis, but the study authors reported no significant differences in core temperature between groups (P value = 0.073).
Secondary outcomes
Bleeding complications
Four trials (Jeong 2008; Smith 1998a; Smith 1998b; Yamakage 2004) reported mean blood loss (Analysis 1.7). We did not pool these results because of the wide range of estimated mean differences and the high heterogeneity.
1.7. Analysis.
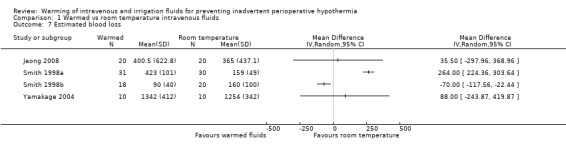
Comparison 1 Warmed vs room temperature intravenous fluids, Outcome 7 Estimated blood loss.
Woolnough 2009 reported blood loss in the room temperature group (n = 25, median = 0.5 L, range = 0.3 to 1.0), the cabinet‐warmed group (n = 25, median = 0.5 L, range = 0.3 to 1.5) and the hotline‐warmed group (n = 25, median = 0.5 L, range = 0.4 to 2.6).
Muth 1996 reported red cells transfused via cell saver in the warmed intravenous fluids group (n = 25) and in the group that received intravenous fluids delivered at room temperature (n = 25). No statistically significant differences were found between the two groups (MD = ‐38 mL, 95% CI ‐357.61 to 281.61).
Yokoyama 2009 reported combined blood/amniotic fluid loss in the warmed fluid group (n = 15) compared with the room temperature intravenous fluids group (n = 15) and found no statistically significant differences between the two groups (MD = ‐176 mL, 95% CI ‐470.29 to 118.29).
Shivering
Nine trials (Andrzejowski 2010; Camus 1996; Chung 2012; Hasankhani 2007; McCarroll 1986; Smith 1998a; Smith 1998b; Woolnough 2009; Xu 2004) (n = 428) comparing warmed intravenous fluids versus room temperature intravenous fluids reported shivering (Analysis 1.6). A statistically significant difference was noted between groups, with people in the warmed fluids group having lower risk of shivering than those in the room temperature group (RR 0.39, 95% CI 0.23 to 0.67; moderate‐quality evidence). Heterogeneity was not statistically significant but reached our prespecified threshold (I² = 36%, P value = 0.13).
1.6. Analysis.
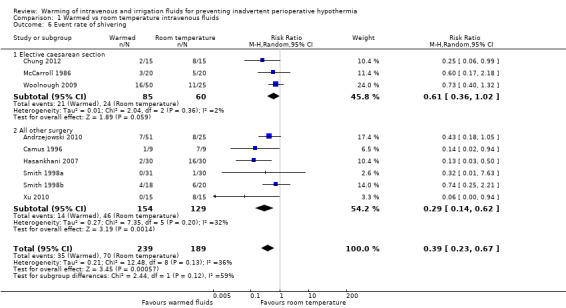
Comparison 1 Warmed vs room temperature intravenous fluids, Outcome 6 Event rate of shivering.
Subgroup analysis was possible for women undergoing elective caesarean section compared with men and women undergoing all other types of surgery. Tests of subgroup differences showed a reduction in shivering in the warmed fluids group, but this finding was not statistically significant (P value = 0.06).
Other secondary outcomes
No data were available on the following outcomes: infections and complications of the wound; pressure ulcers; other cardiovascular complications; all‐cause mortality; length of stay; unplanned high dependency or intensive care admission; and adverse effects.
Warmed irrigation fluids versus room temperature irrigation fluids
Primary outcomes
Risk of hypothermia
This outcome was not reported by any of the included trials. We made a post hoc decision to use mean core temperature as our primary outcome. (See Differences between protocol and review.)
Major cardiovascular complications
This outcome was not reported by any of the included trials.
Core temperature
Our protocol specified risk of hypothermia as the primary outcome. As no trials reported this, we decided to include data related to mean core temperature instead.
Moore 1997 reported core temperature at various time points, but insufficient information on group size at the different time points was available, preventing meaningful analysis of these data.
60 minutes after induction
Kim 2009 reported mean core temperature for warmed irrigation fluid in comparison with room temperature irrigation at 60 minutes after induction of anaesthesia. A statistically significant difference in favour of warmed irrigation fluid was found (MD = 0.45°C, 95% CI 0.25 to 0.65; moderate‐quality evidence).
Mean core temperature at end of surgery/arrival to PACU
Five trials (Jaffe 2001; Kelly 2000; Kim 2009; Moore 1997; Shao 2012) (n = 310) compared warmed irrigation fluids versus room temperature irrigation fluids (Analysis 2.1) and showed no statistically significant differences in core body temperature. Important heterogeneity was present (I² = 94%, P value < 0.001), but we decided to continue with pooling of results, as the absolute differences in individual trial results were relatively small and were generally in the same direction of effect. Inclusion or exclusion of an outlier did not change the conclusions that we would draw. Thus all included studies remained in the final analysis.
2.1. Analysis.

Comparison 2 Warmed vs room temperature irrigation fluids, Outcome 1 Temperature at end of procedure/arrival to PACU (simple design).
Secondary outcomes
Bleeding complications
Kim 2009 reported a mean decrease in haemoglobin for warmed irrigation fluid (n = 23) in comparison with room temperature irrigation fluid (n = 23). No statistically significant differences were found (MD ‐0.30 g/dL, 95% CI ‐0.68 to 0.08).
Patient‐reported outcome: shivering
Two trials (Jaffe 2001; Kim 2009) compared warmed irrigation fluids versus room temperature irrigation fluids for rates of shivering (Analysis 2.2). No significant difference was noted between groups.
2.2. Analysis.
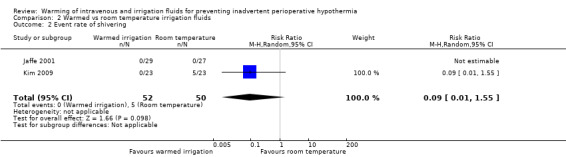
Comparison 2 Warmed vs room temperature irrigation fluids, Outcome 2 Event rate of shivering.
Secondary outcomes not reported
None of the included trials reported the following outcomes: infection and complications of the surgical wound; pressure ulcers; other cardiovascular complications; all‐cause mortality; length of stay; unplanned high dependency or intensive care admission; and adverse effects.
Warmed fluids versus active warming
Primary outcomes
Rate of hypothermia
None of the included trials reported this outcome.
Major cardiovascular outcomes
None of the included trials reported this outcome.
Core temperature
Only one trial (Shao 2012) reported this outcome in relation to core temperature at end of surgery. In this trial, 80 participants were exposed to warm intravenous fluids, warm irrigation fluids or active warming (with or without additional interventions). We pooled the results for participants randomly assigned to any warm intravenous or irrigation fluids and compared them with those for participants randomly assigned to active warming. Overall, a statistically significant difference was noted between warmed fluids and active warming, favouring active warming. Participants in the warmed fluids group were about half a degree colder than those in the active warming group (MD ‐0.49, 95% CI ‐0.70 to ‐0.28).
Secondary outcomes
Shivering
Chung 2012 compared preoperative warming versus warmed intravenous fluids or versus a forced air warmer. The incidence of shivering was 2/15 in the warmed intravenous fluids group and 3/15 in the forced air warmer group. No difference was observed between the two groups in the number of people shivering.
Bleeding complications
Chung 2012 compared the effects of preoperative warming versus warmed intravenous fluids (n = 15) or versus a forced air warmer (n = 15) on mean blood loss. No statistically significant differences in blood loss were noted between the two groups (MD ‐80 mL, 95% CI ‐180.20 to 20.20).
Discussion
Key data are summarized in Table 1 and Table 2.
Summary of main results
No evidence was available on our two primary outcomes: 'risk of hypothermia' and 'major cardiovascular complications'. As a result of this, we made a post hoc decision to include evidence related to mean core temperature at different time points during surgery.
Warmed intravenous fluids
We found that warmed intravenous fluids kept people significantly warmer than room temperature intravenous fluids at 30, 60, 90 and 120 minutes after induction of anaesthesia, and at end of surgery/arrival to the postanaesthesia care unit (PACU). Data quality was ranked as moderate largely as the result of incomplete reporting of trial design and resultant unclear risk of bias. A subgroup analysis was performed on participants undergoing caesarean section who showed a reduction in core temperature similar to the non‐caesarean section group and a non‐statistically significant reduction (P value = 0.06) in shivering in the warmed fluid group. Both pregnancy itself and rapid infusion of fluids may have affected these results.
The degree of warming produced by warming fluids may be related to both the volume infused and the rate at which it is delivered. Volume infused and duration of surgery are noted in the Description of studies. Generally, participants undergoing caesarean section had greater fluid turnover (approximately 2600 mL/h) than was seen in non‐caesarean section participants, whose fluid turnovers ranged from 600 mL/h to 1000 mL/h, with only Muth 1996 reporting higher rates of infusion, at around 1200 mL/h. Subgroup analysis on fluid turnover alone was not possible; however, the subgroup of participants who underwent caesarean section did tend to have greater turnover of fluid during a relatively short procedure but did not show a statistically significant difference in core temperature or rates of shivering.
The magnitude of temperature difference at the end of surgery was only 0.6°C, and the difference did not reach 0.5°C until the 60‐minute time point. This difference is small and may have only limited clinical significance. Core temperatures do drop into the mild hypothermic range at 60 minutes (35.9°C) and to 35.7°C at the end of surgery, so even such a small increase in temperature does render the patient normothermic. Significant heterogeneity was noted between the studies, but variations in absolute temperature differences were small and the direction of effect was largely consistent. Variation in the background interventions used in these studies is a possible cause of the heterogeneity, but we were unable to explore this because of the relatively small number of studies identified.
Shivering is a clinically significant problem ‐ it is uncomfortable for the patient, and the increase in metabolic demand may cause cardiovascular complications. We were able to demonstrate a significant reduction in shivering; however, we were unable to make any judgement on the severity of shivering, as no two studies used the same scale to assess shivering. We considered the data as indicating presence or absence of shivering, even though some studies used more complex rating scales; for this reason, the quality of data is rated as moderate.
The effect of warmed fluids on bleeding complications was unclear, as this outcome was not reported by all studies. Individual trials reporting this outcome used different measures of bleeding complications and were highly heterogeneous, which prevented meaningful analysis and interpretation.
Warmed irrigation fluids
No statistically significant difference in body temperature was noted between warmed and room temperature fluid groups. The body cavity that is irrigated, along with temperature, volume and duration of irrigation, is likely to affect the core temperature; however we had insufficient data to perform a meaningful analysis that would address these factors.
Summary
Overall, these results suggest that warmed intravenous fluids do keep patients significantly warmer than room temperature fluids, but the actual difference in temperature conferred by these methods is only about a half degree Celsius, and so the clinical significance of such a small difference is unclear. A 'ceiling' effect may occur when multiple methods are used to keep patients warm, for example, the use of three warming methods may not result in patients being three times as warm as with a single warming intervention. This 'ceiling' effect may mean that the addition of warmed fluids to one or more other warming methods may not actually have a meaningful impact on core temperature. We are unable to comment further on combinations of warming methods, as we included studies that used several different background warming methods but analysed groups for which the only difference between groups was warming of fluids. We excluded from our analyses many studies that compared multiple warming interventions.
Similar results were found for risk of shivering and for core temperature. Participants in the room temperature fluids groups had greater risk of shivering than those in the warmed fluids groups, although this finding was not statistically significant.
Warmed fluids given at around body temperature have very few clinically relevant side effects, and none were reported. Overwarming and thermal discomfort are potential problems but were not reported, so no further analyses could be performed.
Overall completeness and applicability of evidence
Participant populations were fairly representative of people undergoing a range of elective surgical procedures with various anaesthetic techniques and co‐interventions aimed at reducing hypothermia. Thus the evidence does seem directly applicable to current practice. However, we could not use several trials (Cooper 1994; Demir 2002; Pit 1996), as they did not report relevant outcomes, and no data were available on any of our prespecified primary outcomes or on most of our secondary outcomes.
Quality of the evidence
Reporting of trial design was largely incomplete, leading to difficulty in interpreting the risk of bias. It would be difficult to blind participants and practitioners to the intervention used, but it is not clear how great an effect this may have had on temperature readings made by healthcare professionals. Attrition was generally low, as would be expected in short‐term studies. As we were unable to then make a clear assessment of risk of bias, the quality of data was considered moderate for all core temperature outcomes.
Reporting of shivering varied, and several different shivering scales were used, so even though we analysed shivering as present or absent, we ranked data quality as moderate or low. Bleeding complications were inconsistently reported, and heterogeneity was significant, so the quality of the data was considered very low and results were not pooled.
Potential biases in the review process
After the data were reviewed, several decisions were made regarding handling of the data and investigation of heterogeneity, and this may introduce bias. As no data were reported in the trials, we changed our primary outcome to mean core temperature (Differences between protocol and review). Therefore we have been cautious about interpretation of the data.
Agreements and disagreements with other studies or reviews
The National Institute for Health and Care Excellence (NICE) guideline on perioperative hypothermia recommends fluid warming for volumes greater than 500 mL and for surgery durations longer than 30 minutes, but the preferred method of warming and the temperature to which fluid should be warmed are not stated (NICE 2008). Our findings do not contradict this. The NICE guideline was based on modelling of the effects of temperature differences on patient‐important outcomes and on an economic analysis, and we have not attempted to replicate this.
Authors' conclusions
Implications for practice.
Warm intravenous and/or irrigation fluids have a beneficial effect on the patient's core temperature during surgery, but it is unclear whether the benefit offered is clinically important. When warmed fluids are used in addition to other methods of patient warming, the additional benefit conferred by warm fluid is unclear.
Implications for research.
Any further trials in this area should be conducted at a high level of quality and should collect outcome data that easily translate into important patient‐relevant outcomes. As several other competing interventions are available, the design of further trials should be based on an overview of all relevant comparisons.
Acknowledgements
This review builds on the work undertaken as part of the NICE clinical guideline on inadvertent perioperative hypothermia, and we would like to acknowledge the work of the NICE group.
We would like to thank Anna Lee (content editor); Cathal Walsh (statistical editor protocol); Nathan Pace (statistical editor review); Oliver Kimberger, Janneke Horn and Rainer Lenhardt (peer reviewers); and Anne Lyddiatt (consumer, protocol) for their help and editorial advice.
Appendices
Appendix 1. Search strategy for CENTRAL
#1 MeSH descriptor Rewarming explode all trees #2 (intervention* adj3 treat*):ti,ab or vasodilatat* or infrared light* or intravenous nutrient* or warming system* or ((Mattress* or blanket*) near (warm water or Electric)) or (warm* near (air or CO2 or fluid* or an?esthetic* or IV or gas* or device* or patient* or passive* or active* or skin or surg*)) or (warming or blanket*):ti,ab or pharmacological agent* or thermal insulat* or pre?warm* or re?warm* #3 (#1 OR #2) #4 MeSH descriptor Hypothermia explode all trees #5 MeSH descriptor Body Temperature Regulation explode all trees #6 MeSH descriptor Shivering explode all trees #7 hypo?therm* or normo?therm* or thermo?regulat* or shiver* or ((thermal or temperature) near (regulat* or manage* or maintain*)) or (low* near temperature*) or thermo?genesis or ((reduc* or prevent*) and temperature and (decrease or decline)) or (heat near (preserv* or loss or retention or retain* or balance)) or (core near (thermal or temperature*)) #8 (#4 OR #5 OR #6 OR #7) #9 (#3 AND #8)
Appendix 2. Search strategy for MEDLINE (Ovid SP)
1. Rewarming/ or (intervention* adj3 treat*).ti,ab. or vasodilatat*.mp. or infrared light*.mp. or intravenous nutrient*.mp. or warming system*.mp. or ((Mattress* or blanket*) adj3 (warm water or Electric)).mp. or (warm* adj3 (air or CO2 or fluid* or an?esthetic* or IV or gas* or device* or patient* or passive* or active* or skin or surg*)).mp. or (warming or blanket*).ti,ab. or pharmacological agent*.mp. or thermal insulat*.mp. or (pre?warm* or re?warm*).mp. 2. exp Hypothermia/ or exp body temperature regulation/ or exp piloerection/ or exp shivering/ or hypo?therm*.af. or normo?therm*.mp. or thermo?regulat*.mp. or shiver*.mp. or ((thermal or temperature) adj2 (regulat* or manage* or maintain*)).mp. or (low* adj2 temperature*).mp. or thermo?genesis.mp. or ((reduc* or prevent*).af. and (temperature adj3 (decrease or decline)).mp.) or (heat adj2 (preserv* or loss or retention or retain* or balance)).mp. or (core adj2 (thermal or temperature*)).mp. 3. 1 and 2 4. ((randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or placebo.ab. or drug therapy.fs. or randomly.ab. or trial.ab. or groups.ab.) not (animals not (humans and animals)).sh. 5. 3 and 4
Appendix 3. Search strategy for EMBASE (Ovid SP)
1. warming/ or (intervention* adj3 treat*).ti,ab. or vasodilatat*.mp. or infrared light*.mp. or intravenous nutrient*.mp. or warming system*.mp. or ((Mattress* or blanket*) adj3 (warm water or Electric)).mp. or (warm* adj3 (air or CO2 or fluid* or an?esthetic* or IV or gas* or device* or patient* or passive* or active* or skin or surg*)).mp. or (warming or blanket*).ti,ab. or pharmacological agent*.mp. or thermal insulat*.mp. or (pre?warm* or re?warm*).mp. 2. exp HYPOTHERMIA/ or exp thermoregulation/ or reflex/ or exp SHIVERING/ or hypo?therm*.af. or normo?therm*.mp. or thermo?regulat*.mp. or shiver*.mp. or ((thermal or temperature) adj2 (regulat* or manage* or maintain*)).mp. or (low* adj2 temperature*).mp. or thermo?genesis.mp. or ((reduc* or prevent*).af. and (temperature adj3 (decrease or decline)).mp.) or (heat adj2 (preserv* or loss or retention or retain* or balance)).mp. or (core adj2 (thermal or temperature*)).mp. 3. 1 and 2 4. (placebo.sh. or controlled study.ab. or random*.ti,ab. or trial*.ti,ab.) not (animals not (humans and animals)).sh. 5. 3 and 4
Appendix 4. Search strategy for ISI Web of Science
#1 TS=((hypo?therm* or normo?therm* or thermo?regulat* or shiver*) or ((thermal or temperature) SAME (regulat* or manage* or maintain*)) or (low* SAME temperature*) or thermo?genesis or ((reduc* or prevent*) and temperature and (decrease or decline)) or (heat SAME (preserv* or loss or retention or retain* or balance)) or (core SAME (thermal or temperature*))) #2 TS=((intervention* SAME treat*) or (vasodilatat* or infrared light* or intravenous nutrient* or warming system*) or ((Mattress* or blanket*) SAME (warm water or Electric)) or (warm* and (air or CO2 or fluid* or an?esthetic* or IV or gas* or device* or patient* or passive* or active* or skin or surg*))) or TI=(warming or blanket*) or TI=(pharmacological agent* or thermal insulat* or pre?warm* or re?warm*) #3 #1 and #2 #4 TS=(random* or (trial* SAME (control* or clinical*)) or placebo* or multicenter* or prospective* or ((blind* or mask*) SAME (single or double or triple or treble))) #5 #3 and #4
Appendix 5. Search strategy for CINAHL (EBSCOhost)
S1 (MM "Warming Techniques") S2 vasodilatat* or infrared light* or intravenous nutrient* or warming system* S3 intervention* N3 treat* S4 ((Mattress* or blanket*) and (warm water or Electric)) S5 (warm* and (air or CO2 or fluid* or an?esthetic* or IV or gas* or device* or patient* or passive* or active* or skin or surg*)) S6 AB warming or blanket* S7 AB pharmacological agent* S8 TI thermal insulat* or AB (pre?warm* or re?warm*) S9 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 S10 (MM "Hypothermia") OR (MM "Body Temperature Regulation") OR (MM "Shivering") S11 hypo?therm* or normo?therm* or thermo?regulat* or shiver* S12 AB ((thermal or temperature) and (regulat* or manage* or maintain*)) S13 low* N3 temperature* S14 ( reduc* or prevent* ) and temperature and ( decrease or decline ) S15 thermogenesis S16 heat N3 (preserv* or loss or retention or retain* or balance) S17 core N3 (thermal or temperature*) S18 S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 S19 S9 and S18
Appendix 6. Data extraction form
| Cochrane Anaesthesia Review Group Study selection, quality assessment & data extraction form Warming of IV and irrigation fluids for preventing inadvertent perioperative hypothermia |
Code of paper: |
|
| Reviewer initials: | Date: | |
| First author | Journal/Conference proceedings, etc. | Year |
| |
Study eligibility
| RCT/Quasi/CCT (delete as appropriate) | Relevant participants | Relevant interventions | Relevant outcomes |
| Yes/No/Unclear |
Yes/No/Unclear |
Yes/No/Unclear |
Yes/No*/Unclear |
is
* Issue relates to selective reporting – when study authors may have taken measurements for particular outcomes without reporting these within the paper(s). Review authors should contact trialists for information on possible non‐reported outcomes and reasons for exclusion from publication. Study should be listed in ‘Studies awaiting assessment’ until clarified. If no clarification is received after three attempts, study should then be excluded.
| Do not proceed if any of the above answers is ‘No’. If study is to be included in the ‘Excluded studies’ section of the review, record below the information to be inserted into ‘Table of excluded studies’. |
| |
| Freehand space for comments on study design and treatment: |
Methodological quality
| Allocation of intervention | ||
| State here method used to generate allocation and reasons for grading (quote) | Grade (circle) | |
| Page number | Adequate (random) | |
| Inadequate (e.g. alternate) | ||
| Unclear | ||
|
Concealment of allocation Process used to prevent foreknowledge of group assignment in an RCT, which should be seen as distinct from blinding | ||
| State here method used to conceal allocation and reasons for grading (quote) | Grade (circle) | |
| Page number | Adequate | |
| Inadequate | ||
| Unclear | ||
| Blinding | Page number | |
| Person responsible for participant's care | Yes/No | |
| Participant | Yes/No | |
| Outcome assessor | Yes/No | |
| Other (please specify) | Yes/No | |
|
Intention‐to‐treat An intention‐to‐treat analysis is one in which all participants in a trial are analysed according to the intervention to which they were allocated, whether or not they received it | ||
| Number of participants entering the trial | ||
| Number excluded | ||
| % excluded (greater than or less than 15%) | ||
| Not analysed as ‘intention‐to‐treat’ | ||
| Unclear | ||
| Were withdrawals described? | Yes/No/Not clear | |
| Free text: | ||
Participants and trial characteristics
| Participant characteristics | ||
| Further details | Page number | |
| Age (mean, median, range, etc.) | ||
| Sex of participants (numbers/%, etc.) | ||
| Trial characteristics | ||
| Further details | Page number | |
| Single centre/Multi‐centre | ||
| Country/Countries | ||
| How was participant eligibility defined? | ||
| How many people were randomly assigned? | ||
| How many people were analysed? | ||
| Control group (size and details, e.g. 2 cotton blankets + fluid warmer + HME) | ||
| Intervention group 1 (size and details) | ||
| Intervention group 2 (size and details) | ||
| Intervention group 3 (size and details) | ||
| Time treatment applied (e.g. 30 minutes preoperatively) | ||
| Duration of treatment (mean + SD) | ||
| Total anaesthetic time | ||
| Duration of follow‐up | ||
| Time points when measurements were taken during the study | ||
| Time points reported in the study | ||
| Time points you are using in RevMan | ||
| Trial design (e.g. parallel/cross‐over*) | ||
| Other | ||
* If cross‐over design, please refer to the Cochrane Editorial Office for further advice on how to analyse these data.
| Relevant outcomes | ||
| Reported in paper (circle) | Page number | |
| Infection and complications of surgical wound | Yes/No | |
| Major CVS complications (CVS death, MI, CVA) | Yes/No | |
| Risk of hypothermia (core temperature) | Yes/No | |
| Pressure ulcers | Yes/No | |
| Bleeding complications | Yes/No | |
| Other CVS complications (arrhythmias, hypotension) | Yes/No | |
| Patient‐reported outcomes (shivering, discomfort) | Yes/No | |
| All‐cause mortality | Yes/No | |
| Adverse effects | Yes/No | |
| Relevant subgroups | Page number | |
| Age > 80 | Yes/No | |
| Pregnancy | Yes/No | |
| ASA scores | Yes/No | |
| Urgency | Yes/No | |
Subgroups
Number of participants
| Age > 80 | Pregnant | Elective | Urgent | ASA I or II | ASA III or IV | |
| Control | ||||||
| Intervention 1 | ||||||
| Intervention 2 | ||||||
| Intervention 3 | ||||||
| | ||||||
| Free text: | ||||||
| For continuous data | ||||||||||||||||
| Code of paper |
Outcomes |
Unit of measurement |
Control group | Intervention 1 (thermal insulation) | Intervention 2 | Intervention 3 | ||||||||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |||||||||
| Temperature at end of surgery | Degrees C | |||||||||||||||
| Temperature at ................. | Degrees C | |||||||||||||||
| Temperature at ................. | Degrees C | |||||||||||||||
| Number of units of red cells transfused | Units | |||||||||||||||
| For dichotomous data (n = number of participants) | ||||||||||||||||
| Code of paper |
Outcomes |
Control group | Intervention 1 (thermal insulation) | Intervention 2 | Intervention 3 | Free text | ||||||||||
| n | n | n | n | |||||||||||||
| Wound complications | ||||||||||||||||
| Major CVS complications (CVS death, non‐fatal MI, non‐fatal CVA and non‐fatal arrest) | ||||||||||||||||
| Bleeding complications (coagulopathy) | ||||||||||||||||
| Pressure ulcers | ||||||||||||||||
| Other CVS complications (hypotension, bradycardia, hypotension) | ||||||||||||||||
|
Other information that you feel is relevant to the results: Indicate if any data were obtained from the primary author; if results were estimated from graphs, etc.; or if results were calculated by you using a formula (this should be stated and the formula given). In general if results not reported in paper(s) are obtained, this should be made clear here to be cited in the review. |
| |
| Freehand space for writing actions such as contact with study authors and changes |
References to trial
Check other references identified in searches. If further references describe this trial, link the papers now and list below. All references to a trial should be linked under one Study ID in RevMan.
| Code each paper | Study author(s) | Journal/Conference proceedings, etc. | Year |
References to other trials
| Did this report include any references to published reports of potentially eligible trials not already identified for this review? | ||
| First author | Journal/Conference | Year of publication |
| Did this report include any references to unpublished data from potentially eligible trials not already identified for this review? If yes, list contact names and details | ||
| | ||
Data and analyses
Comparison 1. Warmed vs room temperature intravenous fluids.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Temperature at 30 minutes after induction | 9 | 374 | Mean Difference (IV, Random, 95% CI) | 0.41 [0.24, 0.57] |
| 1.1 Elective caesarean section | 4 | 207 | Mean Difference (IV, Random, 95% CI) | 0.44 [0.12, 0.76] |
| 1.2 All other surgery | 5 | 167 | Mean Difference (IV, Random, 95% CI) | 0.39 [0.26, 0.51] |
| 2 Temperature at 60 minutes after induction | 8 | 312 | Mean Difference (IV, Random, 95% CI) | 0.51 [0.33, 0.69] |
| 2.1 Elective caesarean section | 2 | 105 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.01, 1.19] |
| 2.2 All other surgery | 6 | 207 | Mean Difference (IV, Random, 95% CI) | 0.47 [0.30, 0.64] |
| 3 Temperature at 90 minutes after induction | 3 | 109 | Mean Difference (IV, Random, 95% CI) | 0.54 [0.04, 1.04] |
| 4 Temperature at 120 minutes after induction | 4 | 149 | Mean Difference (IV, Random, 95% CI) | 0.74 [0.31, 1.17] |
| 5 Temperature at end of procedure/arrival to PACU (simple design) | 11 | 682 | Mean Difference (IV, Random, 95% CI) | 0.63 [0.28, 0.98] |
| 5.1 Elective caesarean section | 3 | 205 | Mean Difference (IV, Random, 95% CI) | 0.56 [0.08, 1.04] |
| 5.2 All other surgery | 8 | 477 | Mean Difference (IV, Random, 95% CI) | 0.66 [0.19, 1.12] |
| 6 Event rate of shivering | 9 | 428 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.23, 0.67] |
| 6.1 Elective caesarean section | 3 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.36, 1.02] |
| 6.2 All other surgery | 6 | 283 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.14, 0.62] |
| 7 Estimated blood loss | 4 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 2. Warmed vs room temperature irrigation fluids.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Temperature at end of procedure/arrival to PACU (simple design) | 5 | 310 | Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.06, 0.55] |
| 2 Event rate of shivering | 2 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 0.09 [0.01, 1.55] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andrzejowski 2010.
| Methods | Single‐centre study from the UK | |
| Participants | 82 patients randomly assigned (6 later excluded) undergoing general anaesthesia for day case surgery anticipated to last < 30 minutes; approx 34% male; mean age approx 40 years Exclusion criteria: laparoscopic surgery, surgery with irrigation fluids, estimated blood loss > 200 mL, use of ACE inhibitors or calcium channel antagonists |
|
| Interventions | Room temperature IV fluids (n = 25) In‐line warming (n = 25) Warming cabinet IV fluids (n = 26) |
|
| Outcomes | Oesophageal temperature recorded every 10 minutes | |
| Notes | For analysis, in‐line warming and prewarmed fluids were combined. After enrolment, 2 participants were excluded as the result of surgical cancellation, 2 as they were given regional anaesthesia and 2 as data sheets were missing Each participant received 1 litre of fluids, and mean anaesthetic duration for the room temp group was 31 minutes, for the in‐line warming group 37 minutes and for the warming cabinet group 35 minutes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly assigned by a computer' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Single‐blind study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 participants excluded |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Camus 1996.
| Methods | Single‐centre study in France | |
| Participants | ASA I or II individuals undergoing major abdominal surgery lasting at least 3 hours under general anaesthesia; 18 patients | |
| Interventions | Room temperature IV fluids (n = 9) Warmed IV fluids using hotline to 37°C (n = 9) Both groups also had an electric warming blanket |
|
| Outcomes | Core temperature (location measured is not stated) measured every 30 minutes for the first 2 hours, then hourly thereafter; shivering measured by a clinical observer as present or absent | |
| Notes | Volume of fluid infused: control group 3.5 ± 0.3 litres over 380 ± 3 minutes, warmed group 3.6 ± 0.3 litres over 340 ± 24 minutes None were obese or febrile or had a history of endocrine disease |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly assigned' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Chung 2012.
| Methods | Single‐centre study from Korea | |
| Participants | 45 healthy pregnant ladies undergoing elective caesarean section at between 38 and 42 weeks of gestation | |
| Interventions | Group 1 received warmed intravenous fluids (n = 15), mean volume infused 1210 ± 120 mL Group 2 received forced air warming (n = 15), mean volume infused 1197 ± 215 mL Group 3 received usual care only (n = 15), mean volume infused 1140 ± 140 mL |
|
| Outcomes | Core temperature (tympanic) measured every 15 minutes but reported only at 45 minutes; shivering measured using a scale of 0 to 4 |
|
| Notes | Exclusions: gestational hypertension, weight < 50 kg, weight > 100 kg, fever, placenta praevia, multiple pregnancy, recent drugs/medication | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly assigned' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Cooper 1994.
| Methods | Single‐centre study from Australia | |
| Participants | 14 women aged 31 to 49 undergoing routine hysteroscopic surgery | |
| Interventions | Room temperature irrigation fluid (n = not stated) Body temperature irrigation fluid (n = not stated) |
|
| Outcomes | Oesophageal temperature measured intraoperatively every 10 minutes | |
| Notes | No exclusion criteria were described; the data were provided in the form of a graph, but what the error bars represented was not clear, so data were not useable Neither volumes irrigated nor surgical duration was stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Patients were randomized' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
De Mattia 2013.
| Methods | Single‐centre study in Brazil | |
| Participants | 60 ASA I to III adults undergoing elective abdominal surgery with anaesthetic duration longer than 1 hour, with body temperature 36°C to 37.1°C upon entry to the OR Patients with a predisposition to temperature changes were excluded, including those with thyroid and neurological disorders, extreme weight, ASA IV to VI and axillary body temperature under 36°C or over 37.1°C upon entry to the OR |
|
| Interventions | Warmed intravenous infusion (n = 30) Routine care (n = 30) |
|
| Outcomes | Temperature at time of exit from the OR | |
| Notes | All participants received passive warming via a cover sheet | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random sampling technique: 'A draw was held to determine the group of the first patient of the sample, whether it was the experimental group or the control group, who was selected for the experimental group, and from this, the second patient was selected for the control group, and so forth, successively intercalated until 30 patients were selected for each group' |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Demir 2002.
| Methods | Single‐centre study in Turkey | |
| Participants | 27 patients undergoing elective major abdominal surgery who did had no metastatic malignancy or secondary disease. All patients underwent a thoracic epidural | |
| Interventions | No extra warming other than routine anaesthetic care (n = 9); rate and volume not stated Mixed amino acid solution (n = 9), infused at 143 mL/h; duration not stated but recordings until 4 hours All IV fluids warmed to 37°C until the end of anaesthesia (n = 9) |
|
| Outcomes | Rectal temperature as measured every 30 minutes during surgery | |
| Notes | No useable data were provided: We tried to contact the study author but received no reply | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly assigned' |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Hasankhani 2007.
| Methods | Single‐centre study in Iran | |
| Participants | ASA I orthopaedic patients with surgeries lasting longer than 60 minutes Exclusion criteria: preoperative calcium channel antagonists, temperature > 38°C or < 35.5°C, endocrine disease, obesity, pregnancy, anaemia, age < 18 or > 55 years |
|
| Interventions | Room temperature intravenous fluids (n = 30): volume infused 918 ± 118 mL, duration of surgery 70 ± 4 minutes Warmed intravenous fluids (n = 30): volume infused 984 ± 173 mL, duration of surgery 73 ± 6 minutes |
|
| Outcomes | Oesophageal temperature as measured every 15 minutes intraoperatively; shivering; time spent in postanaesthesia care unit | |
| Notes | Shivering was measured using a 5‐point scale | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly assigned (by the toss of a coin)' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | 'Recording nurse was unaware of which patients were in which group' |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Jaffe 2001.
| Methods | Single‐centre study in USA | |
| Participants | 56 male patients (mean age 71.2 ± 8.2 years) undergoing transurethral resection of the prostate (TURP) | |
| Interventions | Room temperature irrigation fluids (n = 27): volume irrigated 17,333 ± 1226 mL, time in OR 102.2 ± 30.6 minutes Warmed irrigation fluids (n = 29): volume irrigated 17,596 +/‐ 1013 mL, time in OR 96.8 ± 27.9 minutes |
|
| Outcomes | Core (tympanic) body temperature at the beginning and at the conclusion of TURP; shivering | |
| Notes | Consecutive patients; no exclusion criteria were documented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly assigned' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Jeong 2008.
| Methods | Single‐centre study in Korea | |
| Participants | 40 patients undergoing off‐pump coronary artery bypass surgery; 29 male, 11 female, average age 62 years Exclusion criteria: patients requiring inotropes or intra‐aortic balloon pump, preoperative temperature < 36°C or > 37°C, anticipated need for cardiopulmonary bypass, skin disease, hypersensitivity to skin adhesives |
|
| Interventions | Intravenous fluids warmed to 41°C (n = 20): mean volume infused crystalloid 2301.5 ± 1006.7, blood 400.5 ± 622.8 mL, anaesthesia time 280 ± 59 minutes No warmed fluids (n = 20): mean volume infused crystalloid 2191.2 ± 622.3 mL, blood 365.0 ± 437.1 mL, anaesthesia time 278 ± 53 minutes Both groups lay on a warming water mattress, and operating room temperature was maintained at 25°C |
|
| Outcomes | Hourly bladder temperature recorded intraoperatively; temperature at 4 hours postoperatively; blood loss; length of ICU stay; length of hospital stay | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly allocated' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Jorgenson 2000.
| Methods | Study conducted in Denmark (presumed single centre) | |
| Participants | 120 healthy term parturients consenting to spinal anaesthesia for elective caesarean section; patients with pre‐eclampsia, arterial hypertension or multiple pregnancy were excluded | |
| Interventions | Warmed saline heated to 37°C (n = 57) Cold saline at 21°C (n = 56) Each participant was infused with 20 mL/kg 15 minutes before spinal, then 10 mL/kg in the 20 minutes after spinal injection |
|
| Outcomes | Decrease in core temperature (location measured not specified); discomfort; incidence of shivering; blood pressure; heart rate | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was achieved with computer‐generated codes |
| Allocation concealment (selection bias) | Low risk | Codes were placed in sealed envelopes, which were opened after the participant arrived to the theatre |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7 participants were withdrawn from the study: 1 because of violation of selection criteria, 2 because of failed spinal anaesthesia and 5 because of protocol violations |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Kelly 2000.
| Methods | Single‐centre study in USA | |
| Participants | 24 ASA I and II patients aged 18 to 65 years undergoing spinal anaesthesia for arthroscopic knee surgery; 17 male, 3 female Exclusion criteria: patients who could not have a spinal, co‐existing disease that may affect temperature, recent use of antipyretics 4 participants were excluded from the final analysis |
|
| Interventions | Room temperature irrigation fluids (n = 12): surgical duration 45.6 ± 20.1 minutes, volume irrigated 11.7 ± 10.7 litres Irrigation fluids warmed to 40°C (n = 12): surgical duration 44.3 ± 22.6 minutes, volume irrigated 11.8 ± 11.0 litres Both groups were covered with cloth sheets and drapes and were given room temperature intravenous fluids |
|
| Outcomes | Tympanic temperature as measured every 15 minutes intraoperatively and for 1 hour postoperatively | |
| Notes | Data were recorded as percentage change in temperature, so were not included in the analyses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Random numbers table' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1 participant in the treatment group and 1 in the control group were excluded from the final analysis, as they required warming. 2 additional participants in the treatment group were excluded as they required tourniquet inflation |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Kim 2009.
| Methods | Single‐centre study in Korea | |
| Participants | 50 patients undergoing elective arthroscopic shoulder surgery 4 patients were excluded because of incomplete data; no other exclusion criteria were described |
|
| Interventions | Room temperature irrigation fluid (n = 23): volume irrigated 10.3 ± 4.3 litres, surgical time 91.1 ± 32.4 minutes Warmed irrigation fluid to 37°C to 39°C (n = 23): volume irrigated 9.8 ± 3.2 litres, surgical time 94.5 ± 21.9 minutes |
|
| Outcomes | Core temperature (oesophageal) measured every 20 minutes; shivering; fall in haemoglobin | |
| Notes | No shivering score was used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Shivering detected by an independent observer |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 4 excluded because of incomplete data |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
McCarroll 1986.
| Methods | Single‐centre study in Canada | |
| Participants | 40 patients undergoing elective caesarean section | |
| Interventions | Room temperature intravenous fluids (n = 20) Warmed intravenous fluids (n = 20) Volumes infused and surgical duration not stated |
|
| Outcomes | Core (tympanic) temperature every 10 minutes | |
| Notes | No inclusion or exclusion criteria were described Shivering was scored as 0 to 3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Person who assessed shivering was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Moore 1997.
| Methods | Single‐centre study in USA | |
| Participants | N = 35; gynaecological laparoscopy (excluding laparoscopic hysterectomy); mean age 32 years Pregnant women and those weighing < 40 kg or > 100 kg were excluded |
|
| Interventions | Ambient temperature irrigation fluids (n = 16): mean irrigation volume 1481 ± 231 mL, surgery time 96 ± 8 minutes Irrigation fluids warmed to 39°C (n = 13): mean irrigation volume 1264 ± 231 mL, surgery time 90 ± 10 minutes Both groups were lying on a heating blanket at 37.8°C, and the upper body was covered with blankets |
|
| Outcomes | Oesophageal temperature as measured every 15 minutes | |
| Notes | 6 were excluded post randomization as they did not require irrigation; 1 was excluded as temperature was < 34°C | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Random numbers table' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding was attempted (nurses selected appropriate fluid temperature without the knowledge of the operating surgeon), but fluid temperature was obvious by the temperature of the handheld probe |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 6 women did not require irrigation and were analysed separately |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Muth 1996.
| Methods | Single‐centre study in Germany | |
| Participants | 50 patients of average age 65 years undergoing elective repair of abdominal aortic aneurysm Inclusion/exclusion criteria were not described |
|
| Interventions | No warmed intravenous fluids (n = 25): total volume fluid replacement 3449 ± 1380 mL, surgical duration 173 ± 8 minutes Intravenous fluids warmed via countercurrent‐like heat exchangers (hotline) (n = 25): total volume fluid replacement 3499 ± 1623 mL, surgical duration 171 ± 59 minutes |
|
| Outcomes | Oesophageal temperature at end of surgery | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Random allocation according to patients' day of surgery (odd or even numbers)' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Oshvandi 2011.
| Methods | Single‐centre study in Iran | |
| Participants | 62 women undergoing elective caesarean section under general anaesthesia at 37 to 42 weeks of gestation. Average maternal age about 28 years Exclusion criteria: steroids, sedatives, magnesium sulphate, antihypertensive drugs, endocrine or vascular disease, hypertension, fever, ruptured membranes, polyhydramnios or oligohydramnios |
|
| Interventions | IV fluid was Ringer's lactate at 25.5°C (n = 31) IV fluid was Ringer's lactate at 37°C (n = 31) |
|
| Outcomes | Tympanic temperature as measured by infrared thermometer, measured before anaesthesia and at 15‐minute intervals | |
| Notes | Appears to describe postrandomization exclusion criteria: surgery lasting longer than 1 hour, intraoperative hypotension requiring extra IV fluid, but it is not clear whether any participants were excluded on the basis of these criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The subjects were randomly assigned to study and control groups" |
| Allocation concealment (selection bias) | Unclear risk | "The subjects were randomly assigned to study and control groups" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | ".....the subjects were blinded to the study.." and, as the outcome was measured while participants were under general anaesthesia, it is unlikely that the measurement was affected. Personnel were probably aware of the group, but it seems unlikely that this would have introduced bias |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "...the research coworkers.......were blinded to the study..."; seems to suggest adequate blinding, although it is not explicit that these staff members were measuring the temperature |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No clear evidence that other outcomes were collected |
| Other bias | Unclear risk | No evidence |
Pit 1996.
| Methods | Single‐centre Dutch study | |
| Participants | 59 men (mean age 72 years) undergoing transurethral resection of the prostate under spinal anaesthesia | |
| Interventions | Room temperature irrigation fluid (n = 31): resection time 30 minutes Isothermic irrigation fluid (n = 28): resection time 28 minutes |
|
| Outcomes | Rectal temperature, preoperative and postoperative haemoglobin concentrations and subjective participant assessment | |
| Notes | No exclusion criteria were described. The data were not useable, as differences between lowest temperature and starting temperature were recorded rather than serial temperature measurements, postoperative haemoglobin rather than estimated blood loss and subjective feeling of cold rather than shivering Volumes irrigated were not stated As a result of the proximity of the rectum and prostate, core temperature measurements at the rectum may be inaccurate |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomized selection' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | 'The patient was not aware of the temperature treatment he had received until the second post‐operative day'; it was not described whether the investigator was blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Shao 2012.
| Methods | Single‐centre RCT in China | |
| Participants | 160 ASA I or II patients aged 18 to 60 years, scheduled for elective abdominal surgery Exclusions: abnormal temperature, systemic metabolic disease, infection, interruption of surgery for frozen section |
|
| Interventions | A total of 32 intervention groups were described, each with 5 patients who had a unique combination of the following 5 interventions:
|
|
| Outcomes | Nasopharyngeal and rectal temperature at end of surgery | |
| Notes | Data provided for each of the 32 groups. We combined these to compare groups when the only difference was warmed intravenous fluids or surgical rinse | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | 'Double blind was carried out by having one researcher seal each envelope containing warming instructions and then have the envelope opened by a second researcher, with the operation and warming method conducted according to the instructions' |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Smith 1998a.
| Methods | Single‐centre study in USA | |
| Participants | 61 patients: 15 male, 41 female; ASA I to III; major gynaecological, orthopaedic or general surgery scheduled to last longer than 90 minutes under general anaesthesia Exclusion criteria: emergency surgery, preoperative calcium channel blockers |
|
| Interventions | Room temperature intravenous fluids (n = 30): fluid replacement crystalloid 1773 ± 253 mL, colloid 1000 ± 500 mL, red cells 2 units; anaesthesia time 162 ± 16 minutes Warmed intravenous fluids (hotline) (n = 31): fluid replacement crystalloid 2973 ± 307 mL, colloid 594 ± 131 mL, red cells 1.5 ± 0.5 units; anaesthesia time 243 ± 23 minutes |
|
| Outcomes | Oesophageal temperature; estimated blood loss; length of stay in recovery; shivering requiring meperidine; extra warming required in recovery; hypoxia (oxygen saturations < 91%); incidences of mild and moderate hypothermia | |
| Notes | Both groups received forced air warming | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Random numbers table' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | 'A nurse who was unaware of patient group' |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Smith 1998b.
| Methods | Single‐centre study in the USA | |
| Participants | 38 female patients undergoing general anaesthesia for elective gynaecological surgery; mean age 33 years Exclusion criteria: head injury, otitis, preoperative temperature > 38°C or < 35.5°C, patients taking calcium channel blockers |
|
| Interventions | Room temperature intravenous fluids (n = 20): mean volume infused 1390 ± 220 mL, anaesthesia time 112 ± 16 minutes Intravenous fluids warmed to 38°C to 39°C using hotline set to 42°C, with 8 cm extension flowing at 13 to 25 mL/min (n = 18): mean volume infused 1270 ± 100 mL, total anaesthesia time 100 ± 16 minutes Both groups were covered with 2 cotton blankets |
|
| Outcomes | Tympanic temperature was recorded every 15 minutes intraoperatively and at 30 and 60 minutes after arrival to the PACU; shivering; pain requiring opioids; use of radiant heat lamps; hypoxia (sats < 91%) | |
| Notes | Shivering was measured as none, mild or severe | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomized' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Postoperative data were recorded by a PACU nurse who was unaware of study groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Woolnough 2009.
| Methods | Single‐centre study from UK | |
| Participants | 75 female patients undergoing elective caesarean section for a singleton pregnancy greater than 37 weeks of gestation under combined spinal‐epidural anaesthesia Exclusion criteria: pyrexia, pre‐eclampsia, drug therapy other than antacids or vitamins, patients at increased risk of intraoperative bleeding |
|
| Interventions | Group 1 (n = 25) room temperature intravenous fluids: 2.0 ± 0.4 litres infused Group 2 (n = 25) prewarmed intravenous fluids: 2.1 ± 0.4 litres infused Group 3 (n = 23) in‐line warming: 2.4 ± 1.4 litres infused |
|
| Outcomes | Tympanic temperature measured every 15 minutes; blood loss; shivering; subjective feelings of hot or cold Shivering assessed using a 3‐point scale: 0 = no shivering; 1 = mild, intermittent shivering; 2 = intense, continuous shivering |
|
| Notes | Both groups of warmed fluids combined for analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Computer generated random numbers and sealed envelopes' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | To maintain blinding, all groups had fluids delivered via a hotline fluid warmer, which was switched on only for group 3. The investigator was not allowed to touch any fluid bags or to give any IV drugs |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A blinded investigator recorded temperature and assessed the degree of shivering |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Xu 2010.
| Methods | Single‐centre study from China | |
| Participants | ASA I or II adult patients requiring general anaesthesia for abdominal surgery; 30 patients aged 18 to 65, 19 female, 11 male Exclusion criteria: thyroid disease, dysautonomia, malignant hyperthermia |
|
| Interventions | Room temperature intravenous fluids (n = 15): volume infused 2.1 ± 0.4 litres over 174 ± 14 minutes Intravenous fluids warmed to 37°C with hotline (n = 15): volume infused 2.0 ± 0.3 litres over 164 ± 11 minutes Both groups had unwarmed cotton blankets; operating temperature was maintained at 24°C and humidity at 30% |
|
| Outcomes | Tympanic temperature was recorded every 30 minutes, as was the incidence of shivering | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Random digits table' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Observer evaluating shivering was blinded to the study; low risk for shivering, unclear for temperature |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Yamakage 2004.
| Methods | Single‐centre study in Japan | |
| Participants | 20 patients (3 female, 17 male), ASA I or II undergoing urological surgery under general anaesthesia plus epidural Exclusion criteria: thyroid disease, dysautonomia, Raynaud's disease, malignant hyperthermia |
|
| Interventions | Unwarmed intravenous HES 1000 mL (n = 10) Prewarmed HES 1000 mL (n = 10) |
|
| Outcomes | Temperature measured every 5 minutes up to 60 minutes | |
| Notes | All participants received 10 mL/kg unwarmed Ringer's lactate before removal of 800 to 1200 mL blood for haemodilution autotransfusion; subsequent 1000 mL hydroxy ethyl starch (HES) was then given at room temperature or prewarmed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomly allocated by an envelope technique' |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
Yokoyama 2009.
| Methods | Single‐centre study in Japan | |
| Participants | 30 female patients undergoing elective caesarean section under combined spinal‐epidural block | |
| Interventions | Warmed intravenous fluids (n = 15): volume infused 1980 ± 400 mL Room temperature fluids (n = 15): volume infused 1800 ± 240 mL |
|
| Outcomes | Core temperature (tympanic) at key points in the procedure and at the end of the procedure, use of vasopressors, blood loss, fetal pH, Apgar scores | |
| Notes | Estimation of blood loss was not used, as the value also includes the volume of amniotic fluid Surgical duration approximately 45 minutes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | 'Double blinded study'; administration of Iv fluids was started by nurses who were not involved in the investigation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Temperature and blood loss were measured by nurses who were not involved in the investigation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No evidence of this |
| Other bias | Low risk | None |
ACE inhibitor = angiotensin‐converting enzyme inhibitor.
ASA = American Society of Anesthesiologists.
C = Celsius.
HES = hydroxy ethyl starch.
ICU = intensive care unit.
IV = intravenous.
N = numbers.
OR = operating room.
PACU = postanaesthesia care unit.
RCT = randomized controlled trial.
TURP = transurethral resection of the prostate.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Board 2008 | Not randomized ‐ first 12 patients were control group followed by next 12 assigned to warmed irrigation fluids |
| Carli 1986 | Several interventions vs none |
| Carli 1989 | Multiple interventions |
| Cavallini 2005 | Multiple interventions ‐ control group with standard surgical drapes vs fluid warming and forced air warming concurrently |
| Chan 1989 | Multi‐intervention |
| Dai 2010 | Multiple interventions |
| Dyer 1986 | Sublingual temperature, not core temperature |
| Ellis‐Stoll 1996 | Compared 2 methods of warming fluids ‐ prewarmed vs in‐line warming |
| Evans 1994 | Multiple interventions |
| Gerig 1979 | No information on formation of comparison groups |
| Heathcote1986 | Not randomized |
| Kiessling 2006 | Active warming vs warmed fluids and thermal insulation |
| Monga 1996 | Oral temperature, not central |
| Neoh 1989 | Axilliary temperature, not core temperature |
| Okeke 2007 | Oral temperature, not central |
| Park 2007 | Not an RCT, before‐and‐after study |
| Park 2009 | Retrospective study |
| Patel 1996 | Compares 2 different fluid warming methods |
| Patel 1997 | Multiple interventions ‐ control group with reflective blankets and warmed fluids vs forced air warming with room temperature fluids |
| Szlyk‐Augustyn 2002 | Multiple interventions |
| Xu 2004 | Multiple interventions |
| Yamauchi 1998 | All patients were on cardiopulmonary bypass |
RCT = randomized controlled trial.
Differences between protocol and review
Differences between Campbell 2012b and review
We had wanted to analyse the outcome of hypothermia as a dichotomous one, but the data were not presented in this way. Outcomes for analysis were chosen after review of study data. As no data on hypothermia were available, we made the decision to analyse mean core temperatures at different time points during surgery.
For assessment of heterogeneity, we had set a threshold of I2 > 30% as indicating important heterogeneity. We found high levels of I2 in almost all analyses, but the absolute differences in temperature were very small and the direction of effect largely consistent. No obvious explanation was found for the heterogeneity, and so we decided to proceed with a meta‐analysis.
Contributions of authors
Gillian Campbell (GC), Phil Alderson (PA), Andrew F Smith (AS), Sheryl Warttig (SW).
Conceiving the review: PA.
Co‐ordinating the review: GC.
Undertaking manual searches: not applicable.
Screening search results: GC, PA, SW.
Organizing retrieval of papers: GC.
Screening retrieved papers against inclusion criteria: GC, PA, SW.
Appraising quality of papers: GC, PA, SW.
Abstracting data from papers: GC, PA, SW.
Writing to authors of papers for additional information: GC.
Providing additional data about papers: none.
Obtaining and screening data on unpublished studies: none.
Managing data for the review: GC, SW.
Entering data into Review Manager (RevMan 5.3): GC, SW, PA.
Analysing RevMan statistical data: CG, SW.
Performing other statistical analysis not using RevMan: none.
Interpreting data: GC, SW.
Making statistical inferences: GC, SW.
Writing the review: GC, SW.
Securing funding for the review: none.
Performing previous work that provided a foundation for the present study: none.
Serving as guarantor for the review (one author): AS
Taking responsibility for reading and checking the review before submission: GC, SW, PA, AS.
Sources of support
Internal sources
-
Morecambe Bay University Hospital Trust, UK.
GC is employed by MBUHT
External sources
-
National Institute for Health Research, UK.
Provided a grant for preparation of Cochrane reviews on perioperative care that has supported this work
Declarations of interest
Gillian Campbell ‐ none known.
Phil Alderson ‐ none known.
Andrew F Smith ‐ none known.
Sheryl Warttig ‐ none known.
New
References
References to studies included in this review
Andrzejowski 2010 {published data only}
- Andrzejowski JC, Turnbull D, Nandakumar A, Gowthaman S, Eapen G. A randomised single blinded study of the administration of pre‐warmed fluid vs active fluid warming on the incidence of peri‐operative hypothermia in short surgical procedures. Anaesthesia 2010;65(9):942‐5. [PUBMED: 20649896] [DOI] [PubMed] [Google Scholar]
Camus 1996 {published data only}
- Camus Y, Delva E, Cohen S, Lienhart A. The effects of warming intravenous fluids on intraoperative hypothermia and postoperative shivering during prolonged abdominal surgery. Acta Anaesthesiologica Scandinavica 1996;40(7):779‐82. [PUBMED: 8874562] [DOI] [PubMed] [Google Scholar]
- Camus, Y, Cohen S, Delva E, Ollivier M, Lienhart A. Effect of warming i.v. fluids on intraoperative hypothermia and postoperative shivering. British Journal of Anaesthesia 1995;74(Suppl):116. [Google Scholar]
Chung 2012 {published data only}
- Chung S, Lee B, Yang H, Kweon K, Kim H, Song J, et al. Effect of preoperative warming during cesarean section under spinal anaesthesia. Korean Journal of Anesthesiology 2012;62(5):454‐60. [PUBMED: 22679543] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 1994 {published data only}
- Cooper MJ, Molnar BG, Broadbent JA, Richardson R, Magos LA. Hypothermia associated with extensive hysteroscopic surgery. Australian and New Zealand Journal of Obstetrics and Gynaecology 1994;34(1):88‐9. [PUBMED: 8053885] [DOI] [PubMed] [Google Scholar]
De Mattia 2013 {published data only}
- Mattia AL, Barbosa MH, Freitas Filho JP, Rocha Ade M, Pereira NH. Warmed intravenous infusion for controlling intraoperative hypothermia. Revista Latino‐Americana de Enfermagem 2013;21(3):803‐10. [23918028] [DOI] [PubMed] [Google Scholar]
Demir 2002 {published data only}
- Demir A, Lyican D, Muslu B, Durak P, Erdemli O. Maintaining body temperature, a comparative study. Acta Anaesthesiologica Italica 2002;53(3):177‐86. [Google Scholar]
Hasankhani 2007 {published data only}
- Hasankhani H, Mohammadi E, Moazzami F, Mokhtari M, Naghgizadh MM. The effects of intravenous fluid temperature on perioperative hemodynamic situation, post‐operative shivering, and recovery in orthopaedic surgery . Canadian Operating Room Nursing Journal 2007;25(1):20. [PUBMED: 17472154] [PubMed] [Google Scholar]
- Hasankhani H, Mohammadi E, Moazzami F, Mokhtari M, Naghizadeh MM. The effects of warming intravenous fluids on perioperative haemodynamic situation, postoperative shivering and recovery in orthopaedic surgery. British Journal of Anaesthetic & Recovery Nursing 2005;6(1):7‐11. [PUBMED: 17472154] 17472154 [Google Scholar]
Jaffe 2001 {published data only}
- Jaffe JS, McCullough TC, Harkaway RC, Ginsberg PC. Effects of irrigation fluid temperature on core body temperature during transurethral resection of the prostate. Urology 2001;57(6):1078‐81. [PUBMED: 11377310 ] [DOI] [PubMed] [Google Scholar]
Jeong 2008 {published data only}
- Jeong SM, Hahm KD, Jeong YB, Yang HS, Choi IC. Warming of intravenous fluids prevents hypothermia during off‐pump coronary artery bypass graft surgery. Journal of Cardiothoracic and Vascular Anesthesia 2008;22(1):67‐70. [PUBMED: 18249333] [DOI] [PubMed] [Google Scholar]
Jorgenson 2000 {published data only}
- Jorgensen HS, Bach LF, Helbo‐Hansen HS, Nielsen PA. Warm or cold saline for volume preload before spinal anaesthesia for caesarean section? . International Journal of Obstetric Anesthesia 2000;9(1):20‐5. [PUBMED: 15321106] [DOI] [PubMed] [Google Scholar]
Kelly 2000 {published data only}
- Kelly JA, Doughty JK, Hasselbeck AN, Vacchiano CA. The effect of arthroscopic irrigation fluid warming on body temperature. Journal of PeriAnesthesia Nursing 2000;15(4):245‐52. [PUBMED: 11235460] [DOI] [PubMed] [Google Scholar]
Kim 2009 {published data only}
- Kim YS, Lee JY, Yang SC, Song JH, Koh HS, Park WK. Comparative study of the influence of room‐temperature and warmed fluid irrigation on body temperature in arthroscopic shoulder surgery. Arthroscopy 2009;25(1):24‐9. [PUBMED: 19111215] [DOI] [PubMed] [Google Scholar]
McCarroll 1986 {published data only}
- McCarroll SM, Cartwright P, Weeks SK, Donati F. Warming intravenous fluids and the incidence of shivering during caesarean sections under epidural anaesthesia. Canadian Anaesthetists Society Journal 1986;33:72‐3. [Google Scholar]
Moore 1997 {published data only}
- Moore SS, Green CR, Wang FL, Pandit SK, Hurd WW. The role of irrigation in the development of hypothermia during laparoscopic surgery. American Journal of Obstetrics and Gynecology 1997;176(3):598‐602. [PUBMED: 9077613] [DOI] [PubMed] [Google Scholar]
Muth 1996 {published data only}
- Muth CM, Mainzer B, Peters J. The use of countercurrent heat exchangers diminishes accidental hypothermia during abdominal aortic aneurysm surgery. Acta Anaesthesiologica Scandinavica 1996;40(10):1197‐202. [PUBMED: 8986182] [DOI] [PubMed] [Google Scholar]
Oshvandi 2011 {published data only}
- Oshvandi K, Shiri FH, Fazel MR, Safari M, Ravari A. The effect of pre‐warmed intravenous fluids on prevention of intraoperative hypothermia in Caesarian section. Iranian Journal of Nursing and Midwifery Research 2014;19(1):64‐9. [PUBMED: 24554962] [PMC free article] [PubMed] [Google Scholar]
- Oshvandi K, Shiri FH, Safari M, Fazel MR. Effect of pre‐warmed intravenous fluid therapy on prevention of postoperative shivering after caesarean section. Hayat 2011;17:1‐11. [Google Scholar]
Pit 1996 {published data only}
- Pit MJ, Tegelaar RJ, Venema PL. Isothermic irrigation during transurethral resection of the prostate: effects on peri‐operative hypothermia, blood loss, resection time and patient satisfaction. British Journal of Urology 1996;78(1):99‐103. [PUBMED: 8795409] [DOI] [PubMed] [Google Scholar]
Shao 2012 {published data only}
- Shao L, Zheng H, Wang H, Liu L, Sun Q, An M, et al. Methods of patient warming during abdominal surgery. PLoS ONE 2012;7(7):e39622. [PUBMED: 22808045] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 1998a {published data only}
- Smith CE, Desai R, Glorioso V, Cooper A, Pinchak AC, Hagen KF. Preventing hypothermia: convective and intravenous fluid warming versus convective warming alone. Journal of Clinical Anesthesia 1998;10(5):380‐5. [PUBMED: 9702617] [DOI] [PubMed] [Google Scholar]
Smith 1998b {published data only}
- Smith CE, Gerdes E, Sweda S, Myles C, Punjabi A, Pinchak AC, et al. Warming intravenous fluids reduces perioperative hypothermia in women undergoing ambulatory gynecological surgery. Anesthesia and Analgesia 1998;87(1):37‐41. [PUBMED: 9661542] [DOI] [PubMed] [Google Scholar]
Woolnough 2009 {published data only}
- Woolnough M, Allam J, Hemingway C, Cox M, Yentis SM. Intra‐operative fluid warming in elective caesarean section: a blinded randomised controlled trial. International Journal of Obstetric Anesthesia 2009;18(4):346‐51. [PUBMED: 19665366] [DOI] [PubMed] [Google Scholar]
Xu 2010 {published data only}
- Xu HX, You ZJ, Zhang H, Li Z. Prevention of hypothermia by infusion of warm fluid during abdominal surgery. Journal of PeriAnesthesia Nursing 2010;25(6):366‐70. [PUBMED: 21126666] [DOI] [PubMed] [Google Scholar]
Yamakage 2004 {published data only}
- Yamakage M, Sasaki H, Jeong SW, Iwasaki S, Namiki A. Safety and beneficial effect on body core temperature of a prewarmed plasma substitute ‐ hydroxyethyl starch ‐ during anesthesia. Journal of Anesthesia 2004;18(3):166‐71. [PUBMED: 15290413] [DOI] [PubMed] [Google Scholar]
Yokoyama 2009 {published data only}
- Yokoyama K, Suzuki M, Shimada Y, Matsushima T, Bito H, Sakamoto A. Effect of administration of pre‐warmed intravenous fluids on the frequency of hypothermia following spinal anesthesia for Cesarean delivery. Journal of Clinical Anesthesia 2009;21(4):242‐8. [PUBMED: 19502035] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Board 2008 {published data only}
- Board TN, Srinivasan MS. The effect of irrigation fluid temperature on core body temperature in arthroscopic shoulder surgery. Archives of Orthopaedic and Trauma Surgery 2008;128(5):531‐3. [DOI] [PubMed] [Google Scholar]
Carli 1986 {published data only}
- Carli F, Itiaba K. Effect of heat conservation during and after major abdominal surgery on muscle protein breakdown in elderly patients. British Journal of Anaesthesia 1986;58(5):502‐7. [DOI] [PubMed] [Google Scholar]
Carli 1989 {published data only}
- Carli F, Emery PW, Freemantle CA. Effect of peroperative normothermia on postoperative protein metabolism in elderly patients undergoing hip arthroplasty. British Journal of Anaesthesia 1989;63(3):276‐82. [DOI] [PubMed] [Google Scholar]
Cavallini 2005 {published data only}
- Cavallini M, Baruffaldi Preis FW, Casati A. Effects of mild hypothermia on blood coagulation in patients undergoing elective plastic surgery . Plastic and Reconstructive Surgery 2005;116(1):316‐23. [DOI] [PubMed] [Google Scholar]
Chan 1989 {published data only}
- Chan VW, Morley‐Forster PK, Vosu HA. Temperature changes and shivering after epidural anesthesia for cesarean section. Regional Anesthesia 1989;14(1):48‐52. [PubMed] [Google Scholar]
Dai 2010 {published data only}
- Dai Y, Wang J, Zhang M. Influence of applying warm fluids during operation on postoperative shivering and myocardial oxygen consumption of patients accepting bilateral artificial joints replacement [Chinese]. Chinese Nursing Research 2010;24(3A):577‐80. [Google Scholar]
Dyer 1986 {published data only}
- Dyer PM, Heathcote PS. Reduction of heat loss during transurethral resection of the prostate. Anaesthesia and Intensive Care 1986;14(1):12‐6. [DOI] [PubMed] [Google Scholar]
Ellis‐Stoll 1996 {published data only}
- Ellis‐Stoll CC, Anderson C, Cantu LG, Englert SJ, Carlile WE. Effect of continuously warmed i.v. fluids on intraoperative hypothermia. AORN Journal 1996;63(3):599‐606. [DOI] [PubMed] [Google Scholar]
Evans 1994 {published data only}
- Evans JW, Singer M, Coppinger SW, Macartney N, Walker JM, Milroy EJ. Cardiovascular performance and core temperature during transurethral prostatectomy. The Journal of Urology 1994;152(6):2025‐9. [DOI] [PubMed] [Google Scholar]
Gerig 1979 {published data only}
- Gerig HJ. Methods influencing intraoperative heat balance in the sterile enclosure [Beeinflussung des intraoperativen Wärmehaushaltes bei Operationen in der Sterilboxe]. Der Anaesthesist 1979;28(4):171‐6. [PubMed] [Google Scholar]
Heathcote1986 {published data only}
- Heathcote PS, Dyer PM. The effect of warm irrigation on blood loss during transurethral prostatectomy under spinal anaesthesia. British Journal of Urology 1986;58(6):669‐71. [DOI] [PubMed] [Google Scholar]
Kiessling 2006 {published data only}
- Kiessling AH, Isgro F, Lehmann A, Piper S, Blome M, Saggau W. Evaluating a new method for maintaining body temperature during OPCAB and robotic procedures. Medical Science Monitor 2006;12(7):MT39‐42. [PubMed] [Google Scholar]
Monga 1996 {published data only}
- Monga M, Comeaux B, Roberts JA. Effect of irrigating fluid on perioperative temperature regulation during transurethral prostatectomy. European Urology 1996;29(1):26‐8. [PUBMED: 8821686] [DOI] [PubMed] [Google Scholar]
Neoh 1989 {published data only}
- Neoh CA, Jawan B, Fung S, Lee JH. The effect of warm irrigating fluids on the incidence of shivering during transurethral resection of the prostate (TURP). Ma Zui Xue Za Zhi = Anaesthesiologica Sinica 1989;27(3):265‐8. [PubMed] [Google Scholar]
Okeke 2007 {published data only}
- Okeke LI. Effect of warm intravenous and irrigating fluids on body temperature during transurethral resection of the prostate gland. BMC Urology 2007;18(7):15. [PUBMED: 17877827] [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2007 {published data only}
- Park H, Yoon H. A comparison of the effects of intravenous fluid warming and skin surface warming on peri‐operative body temperature and acid base balance of elderly patients with abdominal surgery. Daehan Ganho Haghoeji 2007;37(7):1061‐72. [DOI] [PubMed] [Google Scholar]
Park 2009 {published data only}
- Park JK, Lee SK, Han SH, Kim SD, Choi KS, Kim MK. Is warm temperature necessary to prevent urethral stricture in combined transurethral resection and vaporization of prostate? . Urology 2009;74(1):125‐9. [DOI] [PubMed] [Google Scholar]
Patel 1996 {published data only}
- Patel N, Smith CE, Pinchak AC, Hagen JF. Prospective, randomized comparison of the Flotem Iie and Hotline fluid warmers in anesthetized adults. Journal of Clinical Anesthesia 1996;8(4):307‐16. [DOI] [PubMed] [Google Scholar]
Patel 1997 {published data only}
- Patel N, Smith CE, Knapke D, Pinchak AC, Hagen JF. Heat conservation vs convective warming in adults undergoing elective surgery. Canadian Journal of Anaesthesia 1997;44(6):669‐73. [DOI] [PubMed] [Google Scholar]
Szlyk‐Augustyn 2002 {published data only}
- Szlyk‐Augustyn M, Wujtewicz M, Steffek M, Suchorzewska J, Tomaszewski D, Kurowski K. [Perioperative assessment of body temperature in elderly patients during thoracic surgery]. [Polish]. Przeglad Lekarski 2002;59(4‐5):249‐51. [PubMed] [Google Scholar]
Xu 2004 {published data only}
- Xu L, Zhao J, Huang YG, Luo AL. The effect of intraoperative warming on patient core temperature. Zhonghua Wai Ke Za Zhi 2004;42(16):1010‐3. [PubMed] [Google Scholar]
Yamauchi 1998 {published data only}
- Yamauchi M, Nakayama Y, Yamakage M, Tsuchida H, Iwasaki H, Namiki A. [Preventive effect of fluid warmer system on hypothermia induced by rapid intravenous infusion]. [Japanese]. Masui ‐ Japanese Journal of Anesthesiology 1998;47(5):606‐10. [PubMed] [Google Scholar]
Additional references
Al‐Qahtani 2011
- Al‐Quatani AS, Messahel FM. Benchmarking inadvertent perioperative hypothermia guidelines with the National Institute for Health and Clinical Excellence. Saudi Medical Journal 2011;32(1):27‐31. [PUBMED: 21212912] [PubMed] [Google Scholar]
Alderson 2014
- Alderson P, Campbell G, Smith AF, Warttig S, Nicholson A, Lewis SR. Thermal insulation for preventing inadvertent perioperative hypothermia. Cochrane Database of Systematic Reviews 2014, Issue 6. [DOI: 10.1002/14651858.CD009908.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Birch 2011
- Birch DW, Manouchehri N, Shi X, Hadi G, Karmali S. Heated CO2 with or without humidification for minimally invasive abdominal surgery. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD007821.pub2] [DOI] [PubMed] [Google Scholar]
Bush 1995
- Bush HJ, Fischer E, Fantini G, Silane M, Barie P. Hypothermia during elective abdominal aortic aneurysm repair: the price of avoidable morbidity. Journal of Vascular Surgery 1995;21(3):392‐400. [DOI] [PubMed] [Google Scholar]
Campbell 2012a
- Campbell G, Alderson P, Smith AF, Warttig S. Interventions for treating inadvertent postoperative hypothermia. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD009892] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frank 1997
- Frank SM, Fleisher LA, Breslow MJ, Higgins MS, Olson KF, Kelly S, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA 1997;277(14):1127‐34. [PUBMED: 9087467] [PubMed] [Google Scholar]
Harper 2008
- Harper CM, Andrzejowski JC, Alexander R. NICE and warm. British Journal of Anaesthesia 2008;101(3):293‐5. [DOI: 10.1093/bja/aen233] [DOI] [PubMed] [Google Scholar]
Heier 1991
- Heier T, Caldwell J, Sessler D, Miller R. Mild intraoperative hypothermia increases duration of action and spontaneous recovery from vecuronium blockade during nitrous oxide‐isoflurane anesthesia in humans. Anesthesiology 1991;74:815‐9. [DOI] [PubMed] [Google Scholar]
Heier 2006
- Heier T, Caldwell J. Impact of hypothermia on the response to neuromuscular blocking drugs. Anesthesiology 2006;104(5):1070‐80. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins J, Thompson S. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21:1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Kelly 2010
- Kelly M, Gillies D, Todd DA, Lockwood C. Heated humidification versus heat and moisture exchangers for ventilated adults and children. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD004711.pub2] [DOI] [PubMed] [Google Scholar]
Kurz 1996
- Kurz A, Sessler DI, Lenhardt RA. Perioperative normothermia to reduce the incidence of surgical wound infection and shorten hospitalization. Study of wound infections and temperature group. The New England Journal of Medicine 1996;334:1209‐15. [DOI] [PubMed] [Google Scholar]
Leslie 1995
- Leslie K, Sessler D, Bjorksten A, Moayeri A. Mild hypothermia alters propofol pharmacokinetics and increases the duration of action of atracurium. Anesthesia and Analgesia 1995;80(5):1007‐14. [DOI] [PubMed] [Google Scholar]
Melling 2001
- Melling A, Ali B, Scott E, Leaper J. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. Lancet 2001;358:876‐80. [DOI] [PubMed] [Google Scholar]
NICE 2008
- The management of inadvertent perioperative hypothermia in adults: clinical guideline 65. National Institute for Health and Clinical Excellence, http://www.nice.org.uk/guidance/cg65/resources/guidance‐inadvertent‐perioperative‐hypothermia‐pdf (accessed March 2015), 2008.
Putzu 2007
- Putzu M, Casati A, Berti M, Pagliarini G, Fanelli G. Clinical complications, monitoring and management of perioperative mild hypothermia: anesthesiological features. Acta Biomedica 2007;78(3):163‐9. [PubMed] [Google Scholar]
Rajagopalan 2008
- Rajagopalan S, Mascha E, Na J, Sessler D. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology 2008;108(1):71‐7. [DOI] [PubMed] [Google Scholar]
Sessler 1991
- Sessler D, Rubinstein E, Moayeri A. Physiologic responses to mild perianaesthetic hypothermia in humans. Anesthesiology 1991;75:594‐610. [DOI] [PubMed] [Google Scholar]
Sessler 2001
- Sessler D. Complications and treatment of mild hypothermia. Anesthesiology 2001;95:531‐43. [DOI] [PubMed] [Google Scholar]
Urrútia 2011
- Urrútia G, Roqué i Figuls M, Campos JM, Paniagua P, Cibrian Sánchez S, Maestre L, et al. Active warming systems for preventing inadvertent perioperative hypothermia in adults. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD009016] [DOI] [PMC free article] [PubMed] [Google Scholar]
Warttig 2012
- Warttig S, Alderson P, Lewis SR, Smith AF. Intravenous nutrients for preventing inadvertent perioperative hypothermia. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD009906] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Campbell 2012b
- Campbell G, Alderson P, Smith AF, Warttig S. Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD009891] [DOI] [PMC free article] [PubMed] [Google Scholar]


