Abstract
Background:
Obesity is a risk factor for many chronic diseases, and its prevalence and trends vary among populations. Saudi Arabia shows a greater rise in prevalence than many other countries. We aimed to study the association between several chronic disorders, demographic, and lifestyle factors with increased body mass index (BMI) in the adult population of Jeddah.
Methods:
Data were obtained from a door-to-door cross sectional study. A three-stage stratified cluster sampling technique was adopted. Individuals in selected households agreeing to participate were interviewed to complete a predesigned questionnaire covering demographic and lifestyle variables, medical history, and family history of chronic diseases. This was followed by anthropometric and blood pressure measurements. A random capillary plasma glucose (RPG) was measured, followed by further testing using fasting plasma glucose and glycated hemoglobin (HbA1c) to verify whether participants were normal, diabetic, or prediabetic. Multiple logistic regression analyses were used to adjust for confounding factors.
Results:
A total of 1419 individuals were included in the study: 667 men and 752 women. The prevalence of overweight and obesity was 35.1 and 34.8%, respectively, in men, and 30.1% and 35.6%, respectively, in women. Both overweight and obesity increased in prevalence to 60 years of age, and decreased in the oldest age group in both sexes. After adjusting for age, risk of obesity in men was increased with having a postgraduate degree [odds ratio (OR), 95%CI = 2.48, 1.1–5.61] and decreased with increased physical activity (OR, 95%CI = 0.49, 0.26–0.91). Risk of prediabetes and diabetes was increased in obese women (OR, 95%CI = 2.94, 1.34–6.44, and 3.61, 1.58–8.26 respectively), that of hypertension in obese men (OR, 95%CI =2.62, 1.41–4.87), and that of dyslipidemia in both sexes (OR, 95%CI = 2.60, 1.40–4.83 in men, and 2.0, 1.01–3.85 in women). A family history of dyslipidemia was associated with reduced risk of obesity among women (OR, 95%CI = 0.33, 0.12–0.92), whereas, in people with above normal weight (BMI ⩾25), there was increased risks of prediabetes, diabetes, and dyslipidemia among women (OR, 95%CI = 2.50, 1.21–5.17; 3.20, 1.45–7.03, and 1.88, 1.02–3.49, respectively ), and of hypertension among men (OR, 95%CI = 1.80, 1.00–3.23).
Conclusions:
The prevalence of overweight and obesity in the Saudi population remain high, indicating ineffectiveness or lack of preventive measures. Risk of prediabetes, diabetes, dyslipidemia, and hypertension increased with increasing BMI, with some sex differences in these associations.
Keywords: demographic and lifestyle factors, diabetes, dyslipidemia, hypertension, obesity, overweight, prediabetes
Introduction
There has been an impending rise in the prevalence of obesity globally, with the Kingdom of Saudi Arabia (KSA) showing a rise that is greater than in many other countries.1–7 According to World Health Organization (WHO) data,7 the overall prevalence of obesity in KSA was estimated to be 35.4% compared with 31.7%, 30.4%, and 27% in the neighboring united Arab Emirates, Iraq, and Oman, respectively, 27.8% in Syria, and 8.6% in Sudan. Obesity is a risk factor for many chronic noncommunicable diseases (NCDs) including type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), osteoarthritis, and some cancers,8 all of which are also associated with a great economic burden on health care, and work productivity of the affected individuals.9,10 In a recent population survey conducted in Jeddah on the western coast of Saudi Arabia, obesity and, in particular, abdominal obesity was found to be, after age, the second most important predictor of both DM and prediabetes.11 Whilst aging is unavoidable, obesity is a modifiable risk factor, which has the potential to be reversed or prevented. The success of programmes designed to do this are dependent on characteristics of the target population. In Saudi Arabia, the Ministry of Health (MOH) has proposed several public health programs on NCDs focusing on awareness and behavioral change.12 The most recent national household survey of the MOH has indicated that the prevalence of obesity might be lower than previously reported,13–15 but could not determine whether this decline in prevalence was due to the success of campaigns or other factors. Although the MOH study was conducted on a national level and included a large population (>10,000 participants) to determine the frequency of obesity and associated risk factors and chronic conditions, it did not report region-specific data.13 The KSA extends over a very large geographical area of more than 2.1 million km2, about half the area of Europe. It was earlier divided into six provinces, but is now divided into 13 administrative regions. Each of the original provinces has its own characteristics, differing in ethnic composition, dietary, and lifestyle habits. The ‘Western Province’ includes both of the holy cities (Makkah and Medinah), in addition to the seaside city of Jeddah. The unique position of Jeddah makes it the gateway to the holy cities, thus attracting people from different parts of the Islamic world to settle, with all their own genetic characteristic, and of course their cosmopolitan diets. Hence, its inhabitants represent a mixture of ethnicities, in addition to the indigenous Arabian tribes. Being of such diverse backgrounds, its people embrace new ideas, including western type lifestyle and diets, introduced following the oil boom in the late 1970s. The adoption of a western lifestyle in many developing societies has been associated with an epidemiological transition marked by a shift in the leading causes of death from communicable diseases to NCDs.9,16
We aimed to study the association of demographic and lifestyle factors, previously shown to be associated with excess weight in other populations, and increased body mass index (BMI) in the adult population of Jeddah located in the western part of KSA. The association between BMI and several NCDs was also investigated.
Materials and methods
Data included in this study were obtained from a door-to-door survey conducted in the city of Jeddah during the summer months of 2011 and 2012. This study was approved by the Committee on the Ethics of Human Research at the Faculty of Medicine-King Abdulaziz University, Jeddah (Reference No. 338-10).
Sampling methodology
The sampling methodology has been fully explained earlier,11 and is summarized here as follows: a 3-stage stratified cluster sampling technique was adopted for the sample selection, utilizing the digital geo-referenced map for Jeddah Governorate using the Geographic Information System (GIS) and its analytical tool ArcGIS. The city map was divided into large clusters, and 36 large clusters were selected randomly to cover slum as well as organized areas in the first stage. The large clusters were then divided into smaller ones, and two small clusters were chosen randomly from each large cluster in the second stage, with the centroid of each small cluster being considered as the landmark for the selection of the included residence. An alternative location was chosen if the selected one was not a residential building housing families. Families were then selected from each location for inclusion into the study based on type of housing as outlined earlier,11 so that a standardized procedure was used to select families living in apartment buildings, while all residents in single occupancy residence were included in the sample. All adults ≧18 years of age derived from selected families were included in the current study
Data collection
The selected households were visited to explain the study, obtain written consent, and make an appointment for sample collection. During the visit, to avoid incomplete collection of the information required, all individuals agreeing to participate and signing a written informed consent were interviewed face-to-face to complete a predesigned questionnaire covering demographic, dietary, and lifestyle variables, as well as medical history, including subjective symptoms, diagnosed NCDs, and family history of these diseases. The diagnosis of dyslipidemia was based on this information. This was followed by anthropometric (height, weight) and blood pressure measurements using standardized techniques and equipment.11 Weight and height were used to calculate BMI using the equation [BMI = weight (kg)/ height2 (meters2)], and this was used to classify the participants into categories of underweight (BMI <18.5 kg/m2), normal weight (BMI 18.5 to <25 kg/m2), overweight (BMI 25 to <30 kg/m2), and obese (BMI ⩾30 kg/m2). Hypertension was diagnosed as detailed earlier.11 In addition, the time of last meal was recorded, and a random capillary plasma glucose (RPG) was measured using calibrated glucometers (ACCU- CHEK1- Model GC- Roche, Jeddah, KSA). Individuals taking no drug treatment for diabetes, and with RPG of > 100 mg/dl, and reporting fasting status (last meal before 8–10 h), and those reporting less than 8 h fasting, and having RPG of ⩾126 mg/dl were given an appointment for further testing to verify whether they were normal, diabetic, or prediabetic as described earlier.11 As a result, 19 individuals previously unaware of their condition were found to be diabetic, and 122 were found to be prediabetic.
Statistical analysis
Analyses were performed using the SPSS statistical package version 21 (Chicago, IL, USA). A Chi-square test was used to identify the association between overweight or obesity and the independent variables. Based on the hypothesis that factors associated with overweight and obesity may differ, the analyses of overweight people included those who were obese, but the analyses of the obese excluded those who were overweight. Multiple logistic regression analyses were used to adjust for confounding factors. Unadjusted and age adjusted odds ratio (OR) for both sexes with its 95% confidence interval (CI) for demographic and lifestyle, as well as clinical covariates associated with overweight and obesity were presented. Educational attainment, smoking, physical activity, diagnosis of hypertension, dyslipidemia, prediabetes, diabetes, CVD, and family history of DM, dyslipidemia, and CVD were included in the model as independent variables. A p < 0.05 was accepted to be statistically significant.
Results
A total of 1419 individuals, 667 men and 752 women, with a complete set of data, derived from 390 families, were included in the study, with the overall prevalence of overweight and obesity being 35.1 and 34.8% %, respectively, in men, and 30.1% and 35.6%, respectively, in women (Figure 1).
Figure 1.
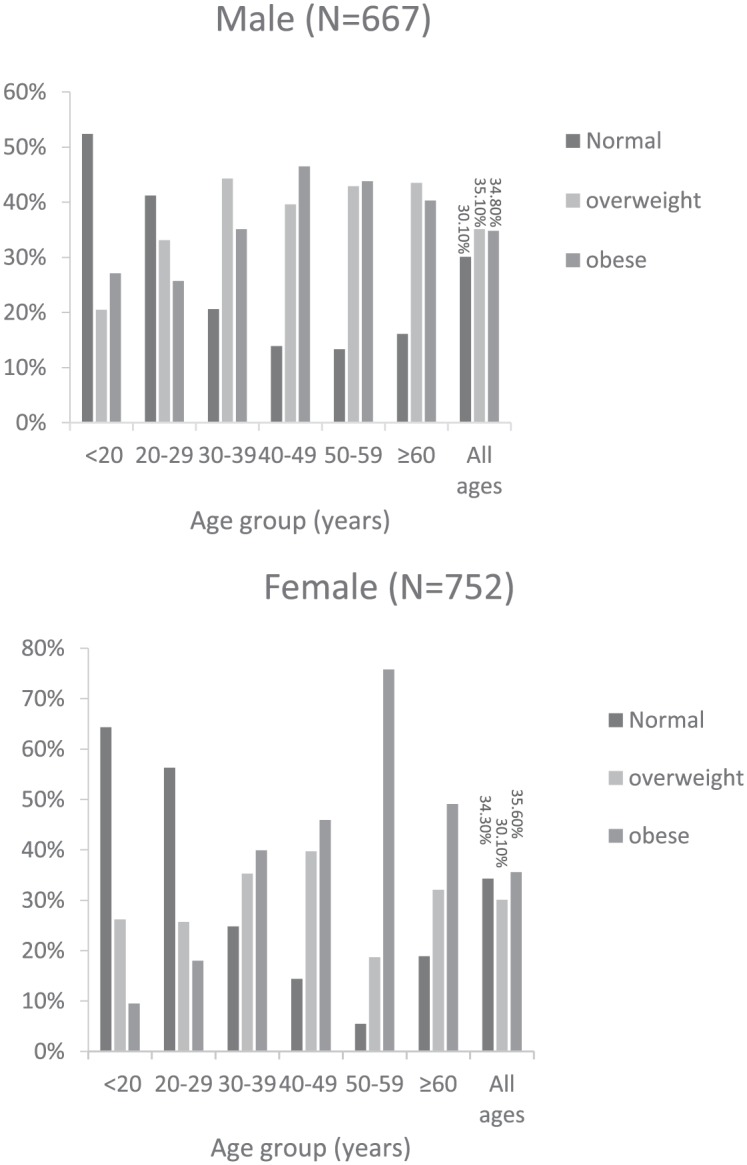
The prevalence of overweight and obesity according to age in (a) Males, (b) Females.
The prevalence of overweight and obesity differed by age in both sexes, but the pattern differed between men and women. The prevalence of overweight increased sharply in men between 20–29 years of age from 20.5% to 33.1%, and continued to increase to 44.3% in the age group 30–39, before stabilizing at around 43%, while in the case of obesity it increased after 30 years of age to 35.1%, with further increase after 40–46.5%, then decreasing slightly in the older age groups to 40.3%. A similar sharp increase in the prevalence of overweight from 25.7% to 35.3% was noted in women 30–39 years of age, followed by a smaller increase to 39.7% in the group aged 40–49 years, before decreasing in the next age group to 18.7%, and increasing again in women ⩾60 years of age to 32.1%. On the other hand, the prevalence of obesity in women was much lower, being 9.5% in the <20 years age group compared with that in men, but it almost doubled in the next age group, becoming 18%, then doubled again to 39.9%, continuing to increase in the next age groups, reaching a high of 75.8% in those aged 50–59 years, before decreasing markedly to 49.1% in the oldest age group.
Demographic and lifestyle characteristics of study participants according to BMI classification are shown in Table 1.
Table 1.
Demographic and lifestyle characteristics of participants according to the BMI category.
| Normal or underweight (BMI <25) (N = 459) | Overweight (BMI 25-29.9) (N = 460) | Obese (BMI 30+) (N = 500) | p value for differences in characteristics between BMI categories | |
|---|---|---|---|---|
|
Educational Level:
⩽ Primary school Intermediate school Secondary school and diplomas University degree Post graduate degree |
24.2% 29.4% 37.6% 30.5% 33.2% |
40.8% 38.6% 30.8% 33.1% 26.8% |
35.0% 32.0% 31.6% 36.4% 40.0% |
0.009 |
|
Family Income:
⩽3000 >3000- 5000 >5000-10000 >10000-20000 >20000 |
26.9% 31.9% 31.3% 33.3% 29.2% |
32.1% 36.3% 33.9% 30.7% 32.3% |
41.0% 31.9% 34.8% 35.9% 38.5% |
0.838 |
|
Ethnicity
Arabian tribes African tribes Mediterranean countriesa Indian continent Mid Asia South east Asia |
32.7% 27.4% 35.5% 32.9% 37.0% 16.0% |
31.8% 40.3% 33.3% 35.5% 30.4% 28.0% |
35.5% 32.3% 31.2% 31.6% 32.6% 56.0% |
0.534 |
|
Smoking status:
Non smoker Former smoker Smoker |
33.1% 22.6% 33.9% |
32.8% 34.5% 30.5% |
34.1% 42.9% 35.6% |
0.287 |
|
Physical activity: (moderate intensity)
< 60 minutes / week 60-<150 min/week ⩾150 min/week |
31.5% 35.0% 33.6% |
30.6% 40.0% 34.2% |
37.9% 25.0% 32.2% |
0.015 |
Mediterranean countries includes all Arab countries on the Mediterranean such as Syria, Lebanon, Palestine, Egypt, Tunisia, Algeria, Libya, and Morraco.
BMI, body mass index.
Family income, ethnicity, and smoking status did not differ between the different BMI classes, but educational attainment, and physical activity did. Participants with primary school or less education had the lowest percentage of normal or underweight subjects, while those holding a postgraduate degree showed a high percentage of obesity. Holders of secondary school certificates or diplomas had the highest percentage of normal or underweight subjects. As for physical activity, it was apparent that the majority of all groups were sedentary. A high percentage of obese individuals were sedentary, with a small percentage appearing to undergo some sort of exercise.
All demographic, lifestyle, and clinical variables were entered into a stepwise logistic regression analysis model (Tables 2 and 3). Obesity in men was found to be significantly associated with having a postgraduate degree after adjusting for age (Table 2). High physical activity was associated with a decreased risk of obesity in men after adjusting for age (Table 2), while demographic and lifestyle covariates were not associated significantly with overweight or obesity in women either before or following adjustment (Table 2).
Table 2.
OR for demographic and lifestyle covariates associated with obesity alone and with overweight and obesity combined.
|
Men
|
Women
|
|||
|---|---|---|---|---|
| Unadjusted OR (95% CI) | Age adjusted OR (95% CI) | Unadjusted OR (95% CI) | Age adjusted OR (95% CI) | |
| Educational Level: | ||||
| Intermediate schoola
Obesity Overweight and obesity combined |
0.88 (0.38–2.03) 0.63 (0.30–1.31) |
1.95 (0.77–4.91) 1.49 (0.67–3.34) |
0.66 (0.29–1.47) 1.04 (0.52–2.12) |
0.69 (0.27–1.8) 1.06 (0.48–2.31) |
| Secondary school and diplomasa
Obesity Overweight and obesity combined |
0.50 (0.26– 0.97) 0.37 (0.21–0.66) |
0.95 (0.46–1.98) 0.78 (0.41–1.47) |
0.66 (0.35–1.26) 0.82 (0.46–1.46) |
0.75 (0.36–1.58) 0.95 (0.50–1.80) |
| University degreea
Obesity Overweight and obesity combined |
0.55 (0.26–1.13) 0.47 (0.25–0.88) |
1.01 (0.46–2.22) 0.95 (0.48–1.87) |
1.14 (0.57–2.55) 1.21 (0.64–2.27) |
1.42 (0.65–3.11) 1.48 (0.74–2.96) |
| Post graduate degreea
Obesity Overweight and obesity combined |
1.36 (0.64–2.87) 0.75 (0.38–1.46) |
2.48 (1.1–5.61) 1.47 (0.71–3.03) |
0.57 (0.28– 1.15) 0.69 (0.37–1.30) |
0.60 (0.27–1.35) 0.85 (0.43–1.70) |
| Smoking status: | ||||
| Former smokerb
Obesity Overweight and obesity combined |
0.77 ( 0.48–1.22) 0.78 (0.52–1.16) |
0.75 (0.46–1.23) 0.88 (0.58–1.34) |
1.38 (0.90–2.12) 1.17 (0.80–1.72) |
1.60 (0.97–2.64) 1.20 (0.79–1.83) |
| Smokerb
Obesity Overweight and obesity combined |
0.91 (0.46–1.82) 0.70 (0.38–1.32) |
0.77 (0.37–1.60) 0.69 (0.36–1.34) |
1.44 (0.64–3.21) 1.30 (0.63–2.70) |
1.26 (0.48–3.28) 1.00 (0.44–2.28) |
| Physical activity: | ||||
| 60–<150 min/weekc
Obesity Overweight and obesity combined |
2.59 (0.27– 25.09) 0.73 (0.46–1.17) |
0.49 (0.26–0.91) 0.73 (0.44–1.20) |
0.75 (0.46–1.20) 0.97 (0.56–1.7) |
0.58 (0.26–1.31) 0.97 (0.53–1.77) |
| ⩾150 mins/weekc
Obesity Overweight and obesity combined |
0.65 (0.14–2.93) 0.90 (0.59–1.32) |
0.63 (0.38–1.10) 0.71 (0.46–1.09) |
1.10 (0.75–1.62) 0.91 (0.62–1.3) |
0.99 (0.60–1.63) 1.13 (0.75–1.70) |
Reference is ⩽ Primary school.
Reference is Nonsmoker.
Reference is <60 min/week.
CI, confidence interval; OR, odds ratio.
Table 3.
OR for clinical covariates associated with obesity alone and with overweight and obesity combined.
|
Covariates |
Men
|
Women
|
||
|---|---|---|---|---|
| Unadjusted OR (95% CI) | Age adjusted OR (95% CI) | Unadjusted OR (95% CI) | Age adjusted OR (95% CI) | |
|
Diagnosed prediabetes
Obesity Overweight and obesity combined |
2.50 (1.27–4.89) 1.60 (0.85–3.00) |
1.38 (0.67–2.85) 0.90 (0.46–1.78) |
5.48 (2.65–11.33) 3.93 (1.96–7.86) |
2.94 (1.34–6.44) 2.50 (1.21–5.17) |
|
Diagnosed diabetes (or treatment)
Obesity Overweight and obesity combined |
4.10 (2.24– 7.41) 3.12 (1.78–5.47) |
1.90 (0.97–3.73) 1.21 (0.64–2.28) |
12.78 (5.98–27.29) 9.20 (4.40–19.24) |
3.61 (1.58–8.26) 3.20 (1.45–7.03) |
|
Diagnosed Hypertension (140/90 or treatment)
Obesity Overweight and obesity combined |
4.70 (2.65–8.32) 3.51 (2.04–6.03) |
2.62 (1.41–4.87) 1.80 (1.00–3.23) |
3.60 (2.21–5.84) 2.55 (1.61–4.03) |
1.12 (0.62–2.02) 0.87 (0.51–1.48) |
|
Diagnosed Dyslipidemia
Obesity Overweight and obesity combined |
4.68 (2.65–8.30) 3.65 (2.13–6.26) |
2.60 (1.40–4.83) 1.76 (0.98–3.18) |
6.33 (3.52–11.37) 4.94 (2.82–8.67) |
2.0 (1.01–3.85) 1.88 (1.02–3.49) |
|
Diagnosed cardiovascular disease
Obesity Overweight and obesity combined |
3.56 (0.99–12.81) 3.23 (0.96–10.91) |
1.60 (0.42–6.10) 1.12 (0.31–4.05) |
2.13 (0.85–5.30) 1.91 (0.82–4.48) |
0.86 (0.28–2.66) 0.87 (0.33–2.29) |
|
Family history of diabetes
Obesity Overweight and obesity combined |
0.94 (0.63–1.41) 0.87 (0.61–1.24) |
1.14 (0.68–1.59) 0.93 (0.65–1.35) |
1.20 (0.74–1.72) 1.02 (0.74–1.39) |
1.32 (0.86–2.01) 0.99 (0.70–1.40) |
|
Family history of dyslipidemia
Obesity Overweight and obesity combined |
1.67 (0.66–4.22) 1.63 (0.73–3.64) |
1.50 (0.57–4.00) 1.42 (0.61–3.29) |
0.44 (0.8–1.10) 0.54 (0.23–1.25) |
0.33 (0.12–0.92) 0.44 (0.18–1.08) |
|
Family history of cardiovascular disease
Obesity Overweight and obesity combined |
1.26 (0.77–2.05) 1.26 (0.82–1.95) |
1.25 (0.75–2.10) 1.13 (0.72–1.79) |
1.69 (1.13–2.55) 1.41 (0.97–2.04) |
1.36 (0.85–2.17) 1.13 (0.76–1.71) |
CI, confidence interval; OR, odds ratio.
Prediabetes, diabetes, hypertension, and dyslipidemia were all associated with obesity in both sexes, but, after adjusting for age, prediabetes and diabetes were associated with obesity in women only, while dyslipidemia remained associated with obesity in both sexes (Table 3). In addition, family history of dyslipidemia became significantly associated with reduced risk of obesity among women.
When overweight was included together with obesity in the analysis, and adjusting for age (Table 3), significantly increased risk was noted for prediabetes, diabetes, dyslipidemia among women, and for hypertension among men.
Discussion
The obesity epidemic is a major global public health concern.17 Data from previous studies indicate an increasing trend for the prevalence of obesity in the KSA.1–7 Information regarding lifestyle practices and demographic characteristics associated with overweight and obesity among the adult population of different regions in the KSA is limited. Furthermore, studies of the impact of obesity and overweight on overall health status of our people is also lacking. Therefore, we conducted this study among the adult population of Jeddah, which is the largest city in the western region of the country, to investigate the association between demographic and lifestyle factors, and various chronic disorders with overweight and obesity, measured by BMI, as well as the relationship between increased BMI and various chronic disorders.
The overall prevalence of obesity was approximately 35% in both sexes. This is similar to previous reports conducted between 1985 and 2011,1–7,14,15 and higher than the most recent national survey conducted in 2013 for Saudi Arabia overall,13 indicating the lack of effect of obesity prevention programs in the western region of the Kingdom.
The prevalence of obesity and overweight increased with age, as has been reported in previous studies in the KSA,1,3,13 and other countries.18–22 Indeed, large population studies indicate that mean body weight and BMI increase gradually throughout adult life, reaching peak values at 50–59 years of age in both men and women, then decreasing after the age of 60 years.18–22 This was noted in our study, with a decrease in the percentage of obese men and women aged ⩾60 years, and an increase in the percentages of those with normal BMI. A possible explanation could be that appetite and food intake fall off at this age, or that BMI does not truly reflect adiposity, and that sarcopenia (reduction in muscle mass) is an issue. Also, selective mortality among obese people may contribute to a decrease in obesity prevalence in older people.23–25
Lifestyle habits have been linked to obesity in numerous studies26,27 Even though recommendations to improve lifestyle practices have been made in earlier national surveys,1 only one attempt was made to study associated factors in our society,13 and this was conducted on a national level, without specifying regional differences, a very important aspect in a large country like Saudi Arabia. This prompted us to re-examine data collected in an earlier survey between 2011 and 2012 in Jeddah to try and address this gap in knowledge, which is much needed to develop ‘Obesity prevention’ programmes. Saudi families strictly follow certain customs and traditions in their daily living; hence, dietary, and lifestyle practices have not changed in the last 10 years at least. Therefore, we believe that our collected data is still valid at this present date. Our first attempt was by using the data collected during 2011 to evaluate the association between general and abdominal obesity, and dietary and smoking habits.28 However, recognizing the importance of sociodemographic factors in the development of obesity, we re-examined the full data in this study, but without including dietary habits, and, in addition, investigated the association between BMI and several NCDs.
Age was adjusted for when studying association with various factors and disorders. Even though educational attainment and physical activity differed significantly between the different BMI classes for the studied population as a whole, when stratified for sex, none of the studied demographic and lifestyle covariates was found to be associated with overweight in either sex after adjustment. However, after adjustment obesity was found to be significantly increased in men with a postgraduate degree. This is in keeping with results from the most recent national study,13 which reported lower risk of obesity with increasing level of education among women but not men. In a review on obesity and educational attainment that examined 289 articles with reports on 410 populations in 91 countries,29 it was concluded that the relationship between educational attainment and obesity was modified by both gender and the country’s economic development level, with an inverse association being more common in studies of higher-income countries, and a direct association being more common in lower-income countries, with a stronger social patterning among women. However, the review found that only a few studies had controlled for a comprehensive set of potential confounding variables, or attempted to assess causality through the use of quasi-experimental designs.
Even though KSA is considered one of the higher income countries, wealth is not necessarily associated with educational level. Indeed the opposite might be true!! This might explain further the findings in our study. In addition, our findings can probably be explained by the expected lack of physical activity at work associated with higher or executive positions. This explanation is validated by finding a low OR in men carrying out physical activity, indicating the protective effect of exercise against excessive weight gain. Smoking has been reported to be associated with lower weight in some studies.30 However, this was not noted in our study, in agreement with the national survey results.13
Overweight and obesity were reported to be associated with increased risk of hypertension, dyslipidemia, T2DM, and CVD.31,32 Studying the unfavorable health effects accompanying overweight and obesity, differences between the sexes became more apparent. After adjustment for age, above normal weight (either overweight or obesity) was found to be associated with increased risk of hypertension in men, and prediabetes, diabetes, and dyslipidemia in women. However, obesity by itself was found to be associated with increased risk of dyslipidemia in addition to hypertension in men, as well as the same increased risk of prediabetes, diabetes and dyslipidemia in women. The lack of association between diabetes and obesity in men could be due to the fact that weight above normal is only one of the risk factors for T2DM. Age, ethnicity, and family history of diabetes are all recognize risk factors. In our study, a lower percentage of men aged ⩾50 years compared with women were obese. Furthermore, ethnicity and family history of diabetes could also be different between men and women in our study. Similar associations appeared in our earlier report using the same data,11 and the given explanation was that the commonly used cutoff values for BMI to define overweight and obesity were used in our study, which might not be the most suitable ones for the Saudi population, since the relationship between percentage body fat and BMI may be different among different ethnic populations.33 Another explanation may be abdominal fat, which has been shown to be more predictive of insulin resistance and related metabolic abnormalities than BMI.34–36 Therefore, using BMI as a sole measure of overweight and obesity in our study, we might have missed such associations seen with abdominal adiposity. Indeed, in our previous study,11 we found that abdominal obesity is the second most important predictor of both DM and prediabetes. The association between abdominal obesity and other chronic metabolic conditions in the Saudi population needs to be examined in more detail.
The noted strong association of overweight and obesity with risk factors for CVD raises concerns about the high prevalence of overweight and obesity throughout adult life, and even in people aged <30 years. In the WHO 2014 NCD country profile for the KSA,37 CVD was the most important cause of death, accounting for 46% of total deaths for all ages, and both sexes. These figures are expected to rise if well-constructed programmes to combat obesity and other cardiovascular are not initiated and followed diligently.
There are several limitations to our study, some of which are common in cross-sectional design studies. First of all, only willing subjects were included, hence representation of true population might be somewhat affected. Indeed, most of the approached households refusing to participate were from the high income sector. A second limitation is that physical activity and intensity were not evaluated in depth. A more detailed study might yield different results. Thirdly, cases of prediabetes and diabetes who have isolated high postchallenge glucose might have been missed due to the fact that we used only fasting blood glucose and HbA1c to identify them.11
In conclusion, our study indicates that, during 2011 and 2012, the prevalence of overweight and obesity among the population of Jeddah remain at least as high as earlier reported in previous surveys.1–7 Higher than normal weight was associated with hypertension in men, prediabetes, diabetes, and dyslipidemia in women. Obese men were likely to be less physically active, have a postgraduate degree, and to suffer from hypertension and dyslipidemia, while obese women were likely to be prediabetic, have a family history of dyslipidemia, and suffer from diabetes and dyslipidemia. Obviously, preventive measures are urgently needed to reduce overweight and obesity in the KSA. There are many societal issues that need to be addressed by collaboration between different governmental agencies and the private sector to alleviate the problem, such as providing reachable walking areas and sport centers in various districts within the city. Implementation and evaluation of evidence-based interventions is much encouraged. It will also be interesting to study the impact of the recent introduction of physical activity classes in schools for girls on the prevalence of overweight and obesity.
Supplemental Material
Supplemental material, Jeddah-obesity-supplementary_material_FV2 for The prevalence of obesity and overweight, associated demographic and lifestyle factors, and health status in the adult population of Jeddah, Saudi Arabia by Rajaa Al-Raddadi, Suhad M. Bahijri, Hanan A. Jambi, Gordon Ferns and Jaakko Tuomilehto in Therapeutic Advances in Chronic Disease
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and publication of this article: This research was funded by King Abdulaziz University Deanship of Scientific Research, grant number (01-33-RG), http://dsr.kau.edu.sa/Default.aspx?Site_ID=305&lng=AR.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Rajaa Al-Raddadi  https://orcid.org/0000-0002-8921-9628
https://orcid.org/0000-0002-8921-9628
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Rajaa Al-Raddadi, Department of Community Medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia Saudi Diabetes Study Research Group, King Fahd Medical Research Center, King Abdulaziz University, Jeddah, Saudi Arabia.
Suhad M. Bahijri, Saudi Diabetes Study Research Group, King Fahd Medical Research Center, King Abdulaziz University, Jeddah, Saudi Arabia Department of Clinical Biochemistry, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia.
Hanan A. Jambi, Saudi Diabetes Study Research Group, King Fahd Medical Research Center, King Abdulaziz University, Jeddah, Saudi Arabia Department of Food and Nutrition, Home Economics, King Abdulaziz University, Jeddah, Saudi Arabia.
Gordon Ferns, Saudi Diabetes Study Research Group, King Fahd Medical Research Center, King Abdulaziz University, Jeddah, Saudi Arabia; Division of Medical Education, Brighton and Sussex Medical School, Mayfield House, Falmer, Brighton, UK.
Jaakko Tuomilehto, Saudi Diabetes Study Research Group, King Fahd Medical Research Center, King Abdulaziz University, Jeddah, Saudi Arabia; Center for Vascular Prevention, Danube University Krems, Krems, Austria; Public Health Solutions, National Institute for Health and Welfare, Helsinki, Finland.
References
- 1. Al Othaimeen AI, Al Nozha M, Osman AK. Obesity: an emerging problem in Saudi Arabia. Analysis of data from the National Nutrition Survey. East Mediterr Health J 2007; 13: 441–448. [PubMed] [Google Scholar]
- 2. Warsy A, El Hazmi M. Diabetes mellitus, hypertension and obesity-common multifactorial disorders in Saudis. East Mediterr Health J 1999; 5: 825–829. [PubMed] [Google Scholar]
- 3. Al-Nozha MM, Al-Mazrou YY, Al-Maatouq MA, et al. Obesity in Saudi Arabia. Saudi Med J 2005; 26: 824–829. [PubMed] [Google Scholar]
- 4. DeNicola E, Aburizaiza OS, Siddique A, et al. Obesity and public health in the Kingdom of Saudi Arabia. Rev Environ Health 2015; 30: 191–205. [DOI] [PubMed] [Google Scholar]
- 5. Horaib GB, Al-Khashan HI, Mishriky AM, et al. Prevalence of obesity among military personnel in Saudi Arabia and associated risk factors. Saudi Med J 2013; 34: 401–407. [PubMed] [Google Scholar]
- 6. Al-Quwaidhi A, Pearce M, Critchley J, et al. Trends and future projections of the prevalence of adult obesity in Saudi Arabia, 1992–2022. East Mediterr Health J 2014; 20. [PubMed] [Google Scholar]
- 7. World Health Organization. Global Health Observatory (GHO) data. Overweight and obesity, https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adults/en/. (2016, accessed 15 May 2019).
- 8. Haslam DW, James WPT. Obesity. Lancet 2005; 366: 1197–1209. [DOI] [PubMed] [Google Scholar]
- 9. Boutayeb A, Boutayeb S. The burden of non communicable diseases in developing countries. Int J Equity Health 2005; 4: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Withrow D, Alter D. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev 2011; 12: 131–141. [DOI] [PubMed] [Google Scholar]
- 11. Bahijri SM, Jambi HA, Al Raddadi RM, et al. The prevalence of diabetes and prediabetes in the adult population of Jeddah, Saudi Arabia-a community-based survey. PLoS One 2016; 11: e0152559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. KSA Ministry of Health. National campaign against overweight and obesity 2012, 2012. [Google Scholar]
- 13. Memish ZA, El Bcheraoui C, Tuffaha M, et al. Peer reviewed: obesity and associated factors—Kingdom of Saudi Arabia, 2013. Prev Chronic Dis 2014; 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ministry of Health KoSA, in collaboration with World Health Organization, EMRO. WHO STEPwise approach to NCD surveillance, country-specific standard report, Saudi Arabia. 2005. [Google Scholar]
- 15. Badran M, Laher I. Obesity in Arabic-speaking countries. J Obes 2011; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Amuna P, Zotor FB. Epidemiological and nutrition transition in developing countries: impact on human health and development: The epidemiological and nutrition transition in developing countries: evolving trends and their impact in public health and human development. Proc Nutr Soc 2008; 67: 82–90. [DOI] [PubMed] [Google Scholar]
- 17. Van Vliet-Ostaptchouk JV, Nuotio M-L, Slagter SN, et al. The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: a collaborative analysis of ten large cohort studies. BMC Endocr Disord 2014; 14: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Han T, Tajar A, Lean M. Obesity and weight management in the elderly. Br Med Bull 2011; 97: 169–196. [DOI] [PubMed] [Google Scholar]
- 19. Popa S, Moţa M, Popa A, et al. Prevalence of overweight/obesity, abdominal obesity and metabolic syndrome and atypical cardiometabolic phenotypes in the adult Romanian population: PREDATORR study. J Endocrinol Invest 2016; 39: 1045–1053. [DOI] [PubMed] [Google Scholar]
- 20. Abarca-Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. Lancet 2017; 390: 2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kuskowska-Wolk A, Rössner S. Body mass distribution of a representative adult population in Sweden. Diabetes Res Clin Pract 1990; 10: S37–S41. [DOI] [PubMed] [Google Scholar]
- 22. Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002; 288: 1723–1727. [DOI] [PubMed] [Google Scholar]
- 23. Fontaine KR, Redden DT, Wang C, et al. Years of life lost due to obesity. JAMA 2003; 289: 187–193. [DOI] [PubMed] [Google Scholar]
- 24. Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med 2005; 352: 1138–1145. [DOI] [PubMed] [Google Scholar]
- 25. Monteverde M, Noronha K, Palloni A, et al. Obesity and excess mortality among the elderly in the United States and Mexico. Demography 2010; 47: 79–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jones BL, Fiese BH. Parent routines, child routines, and family demographics associated with obesity in parents and preschool-aged children. Front Psychol 2014; 5: 374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics 2015; 33: 673–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aljoudi SB, Kotbi ET, Alsomali FA, et al. Lifestyle factors and their relation to measures of obesity amongst adults living in Jeddah-Saudi Arabia: a cross-sectional study. Curr Res Nutr Food Sci J 2015; 3: 98–111. [Google Scholar]
- 29. Cohen AK, Rai M, Rehkopf DH, et al. Educational attainment and obesity: a systematic review. Obes Rev 2013; 14: 989–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mackay DF, Gray L, Pell JP. Impact of smoking and smoking cessation on overweight and obesity: Scotland-wide, cross-sectional study on 40,036 participants. BMC Pub Health 2013; 13: 348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003; 289: 76–79. [DOI] [PubMed] [Google Scholar]
- 32. Canoy D, Boekholdt SM, Wareham N, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation 2007; 116: 2933–2943. [DOI] [PubMed] [Google Scholar]
- 33. Deurenberg P, Yap M, Van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes 1998; 22: 1164–1171. [DOI] [PubMed] [Google Scholar]
- 34. Pouliot M-C, Després J-P, Nadeau A, et al. Visceral obesity in men: associations with glucose tolerance, plasma insulin, and lipoprotein levels. Diabetes 1992; 41: 826–834. [DOI] [PubMed] [Google Scholar]
- 35. Ross R, Aru J, Freeman J, et al. Abdominal adiposity and insulin resistance in obese men. Am J Physiol Endocrinol Metab 2002; 282: E657–E663. [DOI] [PubMed] [Google Scholar]
- 36. Lebovitz HE, Banerji MA. Point: visceral adiposity is causally related to insulin resistance. Diabetes Care 2005; 28: 2322–2325. [DOI] [PubMed] [Google Scholar]
- 37. World Health Organization. Noncommunicable diseases country profiles 2014. http://www.who.int/countries/sau/en/ (2014, accessed 2 May 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Jeddah-obesity-supplementary_material_FV2 for The prevalence of obesity and overweight, associated demographic and lifestyle factors, and health status in the adult population of Jeddah, Saudi Arabia by Rajaa Al-Raddadi, Suhad M. Bahijri, Hanan A. Jambi, Gordon Ferns and Jaakko Tuomilehto in Therapeutic Advances in Chronic Disease


