To the Editor—We thank Gérardin and colleagues [1] for their comments on our article and for reexamining pediatric data [2] from the 2005–2006 chikungunya epidemic on La Réunion Island. Upon splitting the original dataset to reflect the 2 epidemic waves of chikungunya virus (CHIKV) transmission on La Réunion, the authors found, among other results, an inverse relationship between the probability of CHIKV infection in an initially naive population (ie, seroprevalence, what they call the attack rate) and the probability of an inapparent outcome given infection, the latter a probabilistic expression of the symptomatic-to-inapparent (S:I) ratio. Our studies of the chikungunya epidemics experienced by a pediatric cohort [3] in Managua, Nicaragua, showed this association with both epidemiological risks and rates [4, 5]. Research from a community-based cohort study in the Philippines also documented this relationship with risks and rates [6, 7]. More broadly, this inverse association was first put forward in the chikungunya field by Manimunda et al [8], and it has since been remarked upon by others [9].
Here, we present evidence in favor of Manimunda et al’s hypothesis that we collected from the literature. Following PRISMA guidelines [10], we conducted a systematic review of the chikungunya literature in the PubMed database, without any restrictions. Our only search term was “chikungunya,” and we screened 3480 articles. We extracted data for studies reporting the ratio of symptomatic and inapparent infections among serologically confirmed CHIKV infections in initially naive populations who experienced a chikungunya epidemic. We corresponded with study authors when questions arose regarding their data or study design to ensure consistency and accuracy. The results are presented in Figure 1 and Supplementary Table 1.
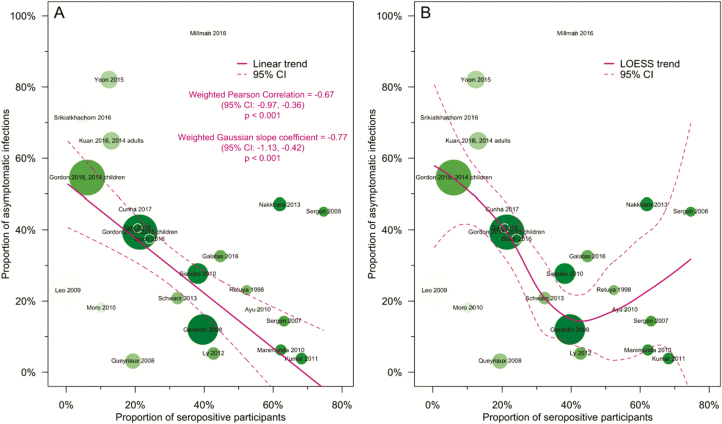
Figure 1.
Risk of chikungunya virus (CHIKV) infection and asymptomatic presentation in the published literature. Scatterplot elements correspond to data in Supplementary Table 1 and references in Supplementary Materials. The radius of each study’s data point is scaled to the sample size and shaded to the size of the CHIKV-infected population. A, Data summarized with a Gaussian model. B, Data summarized with a LOESS model. Abbreviation: CI, confidence interval.
Assuming a Gaussian model, the overall correlation between the probability of CHIKV infection and asymptomatic infection, after weighting by the sample size and the size of the CHIKV-infected population, is −0.67 (95% confidence interval, −0.98, −0.36; P < .001; Figure 1A). This weighted Pearson correlation is robust to exclusion of any one study population. A sensitivity analysis based on iterative jackknife [11] estimates of the weighted Pearson correlation estimator shows that the correlation estimates range from a maximum value of −0.55 (P < .01) with the removal of our 2014 Nicaraguan pediatric data [5] to a minimum value of −0.76 (P < .0001) with the removal of Nakkhara et al’s data [12]. Figure 1B summarizes the same data with a flexible LOESS model [13], which more accurately reflects the variability of the association of interest in the published literature. The inverse association holds reliably for studies that report at most a 40% CHIKV seroprevalence in initially naive populations that have experienced a recent CHIKV epidemic. At higher seroprevalence levels, the variance of the association is large, owing to small sample sizes and variable percentages of asymptomatic infection at high seroprevalence levels.
As indicated in our original article, such a relationship between force of infection and the S:I ratio has been observed with other infectious diseases, including dengue and malaria [14, 15]. Thus, this inverse association may represent a broader phenomenon observed across multiple infectious diseases, which has yet to be fully explained.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Note
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Gérardin P, Freitas ARR, Sissoko D, Teixeira MG. Transmission dynamics and disease severity in children infected with East Central South African or ECSA-derived clades of chikungunya virus. Clin Infect Dis. 2019; 68:171–2. [DOI] [PubMed] [Google Scholar]
- 2. Gérardin P, Guernier V, Perrau J, et al. . Estimating chikungunya prevalence in La Réunion Island outbreak by serosurveys: two methods for two critical times of the epidemic. BMC Infect Dis 2008; 8:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kuan G, Gordon A, Avilés W, et al. . The Nicaraguan pediatric dengue cohort study: study design, methods, use of information technology, and extension to other infectious diseases. Am J Epidemiol 2009; 170:120–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kuan G, Ramirez S, Gresh L, Ojeda S, et al. . Seroprevalence of anti-chikungunya virus antibodies in children and adults in Managua, Nicaragua, after the first chikungunya epidemic, 2014–2015. Bingham A, ed. PLoS Negl Trop Dis 2016; 10:e0004773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gordon A, Gresh L, Ojeda S, et al. . Differences in transmission and disease severity between two successive waves of chikungunya. Clin Infect Dis 2018; 68:170–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yoon I-K, Alera MT, Lago CB, et al. . High rate of subclinical chikungunya virus infection and association of neutralizing antibody with protection in a prospective cohort in the Philippines. Powers AM, ed. PLoS Negl Trop Dis 2015; 9:e0003764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Srikiatkhachorn A, Alera MT, Lago CB, et al. . Resolution of a chikungunya outbreak in a prospective cohort, Cebu, Philippines, 2012-2014. Emerg Infect Dis 2016; 22:1852–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Manimunda SP, Sugunan AP, Rai SK, et al. . Outbreak of chikungunya fever, Dakshina Kannada district, South India, 2008. Am J Trop Med Hyg 2010; 83:751–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gay N, Rousset D, Huc P, et al. . Seroprevalence of Asian lineage chikungunya virus infection on Saint Martin Island, 7 months after the 2013 emergence. Am J Trop Med Hyg 2016; 94:393–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Efron B, Tibshirani R.. An introduction to the bootstrap. London, UK: Chapman & Hall, 1994:436. [Google Scholar]
- 12. Nakkhara P, Chongsuvivatwong V, Thammapalo S. Risk factors for symptomatic and asymptomatic chikungunya infection. Trans R Soc Trop Med Hyg 2013; 107:789–96. [DOI] [PubMed] [Google Scholar]
- 13. R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2017. [Google Scholar]
- 14. Endy TP, Anderson KB, Nisalak A, et al. . Determinants of inapparent and symptomatic dengue infection in a prospective study of primary school children in Kamphaeng Phet, Thailand. Harris E, ed. PLoS Negl Trop Dis. 2011; 5:e975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Greenwood BM. The epidemiology of malaria. Ann Trop Med Parasitol 1997; 91:763–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.