Abstract
The assistive equipment provision process is routinely carried out with patients to mitigate fall risk factors via the fitment of assistive equipment within the home. However, currently, over 50% of assistive equipment is abandoned by the patients due to poor fit between the patient and the assistive equipment. This paper explores clinician perceptions of an early stage three-dimensional measurement aid prototype, which provides enhanced assistive equipment provision process guidance to clinicians. Ten occupational therapists trialled the three-dimensional measurement aid prototype application; think-aloud and semi-structured interview data was collected. Usability was measured with the System Usability Scale. Participants scored three-dimensional measurement aid prototype as ‘excellent’ and agreed strongly with items relating to the usability and learnability of the application. The qualitative analysis identified opportunities for improving existing practice, including, improved interpretation/recording measurements; enhanced collaborative practice within the assistive equipment provision process. Future research is needed to determine the clinical utility of this application compared with two-dimensional counterpart paper-based guidance leaflets.
Keywords: assistive equipment, assistive technologies, falls prevention, health care, occupational therapy, three-dimensional visualisation technology
Background
Falls are a major health concern and pose a significant health challenge to an ageing world population. The number of falls and related injuries has risen in recent years, in part due to a growing population aged 80 years and over.1 Falls often cause debilitating injuries, which precipitate early hospital and long-term care admission and result in an increased burden on health-care services.2 The cost of falls to the National Health Service (NHS) in the United Kingdom is estimated at over £2.3 billion per year.3 Recent policy directives within the United Kingdom highlight the need for new and innovative technology-based applications utilising Information and Communication Technologies (ICTs) within the falls prevention domain. These are seen as having the potential to reduce health-care costs while also lessening the demands that an ageing population has on health-care services.4,5 Furthermore, there is recognition that ICTs have numerous additional benefits, such as the potential to deliver more effective, personalised, patient-centred interventions and improvements in levels of patient engagement and adherence; all of which are likely to enhance patient satisfaction and overall quality of life.4,6 Although in the context of occupational therapy, the assistive equipment provision process (AEPP) is routinely carried out to prevent falls, there are numerous other benefits that may be realised as a consequence of assistive equipment (AE) provision, including enabling ageing in place and independent living, improved facilitation of care, increased self-esteem, and overall improvement of quality of life.7 In the context of occupational therapy, falls prevention activities are carried out as part of the AEPP. This involves working closely with patients to assess intrinsic and extrinsic fall risk factors. Intrinsic fall risk factors focus on functional ability deficits presented by the patient and typically relate to balance and cognitive impairments. Extrinsic fall risk factors focus on risks that are apparent within the environment in which patients carry out occupations on a day-to-day basis, which include poor lighting, slippery surfaces, raised door thresholds, stairs and steps, clutter, and trip hazards.8 Extrinsic fall risk factors also include improper use of AE or the absence of AE such as stair handrails, toilet raisers, bath boards, and bathroom grab rails where these would be deemed necessary.
AEPP, measurement, and falls prevention
The goal of the AEPP is to identify and reduce barriers that impact patients’ ability to carry out the activities of daily living (ADLs) and mitigate the overall risk of falling. This is typically achieved by recommending minor and major adaptations to the home environment to accommodate functional changes, assist with ageing in place, and reduce the patient’s overall risk of falling.2 During the AEPP, clinicians assess whether AE is needed to help maintain independent living and/or to overcome potential fall hazards. A crucial part of the process involves clinicians measuring the dimensions of home furniture and specific parts of the patient’s body. These measurements are used to determine the nature and details of the adaptations that are necessary to reduce the overall risk of falling and to enable patients to successfully engage in their ADLs. The recorded measurements are used to determine the specific sizes of AE prescribed for fitment within the patient’s home environment. An appropriate fit between the equipment, an item of furniture, and/or the patient is only possible if measurements are taken from the correct locations on a person or item and are measured and recorded accurately. Adaptations to the home typically include occupational therapists (OTs) prescribing the installation of AE such as chair raisers, grab rails on stairs, bath boards, toilet raisers, and bathroom grab rails to help with transfers when bathing.9 Measurements are used to ascertain whether the height of furniture either facilitates or hinders functional independence. To recommend a chair raiser, for example, the OT measures the height of the patient’s leg (popliteal height) and the height of the chair. The OT calculates the difference between those two measurements, which provides the height that the chair must be raised. The customisation of measurements plays an important role in ensuring the successful fit of the AE to the patient.10 Clinicians may receive some training in relation to the provision of AE; however, there is currently no mechanism in place to ascertain whether they are prescribing safely.
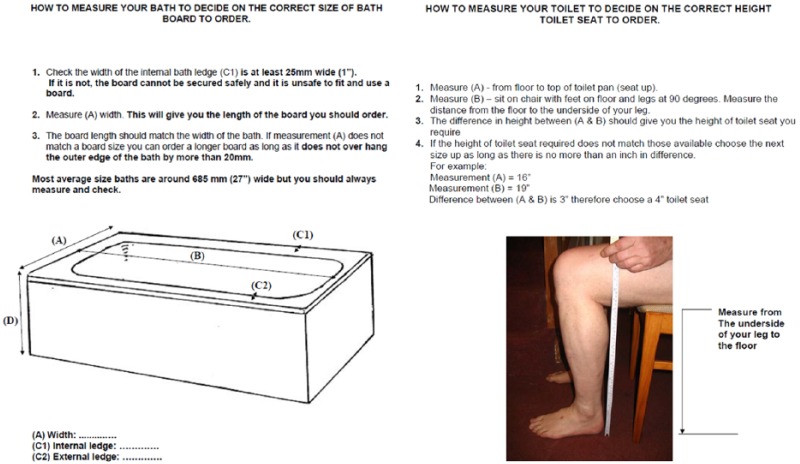
Current AEPP practice involves utilising paper-based forms designed to guide the clinician through the process and ensure that measurements are taken and recorded accurately, along with any necessary patient-related data. These paper-based forms often provide additional measurement guidance in the form of two-dimensional (2D) representations of home furniture and the patient. The key function of the 2D representations is to help the clinician to identify the precise points within three-dimensional (3D) space that must be measured, on each respective item of furniture/patient and make an unambiguous record of these measurements, with a view to accurately calculating and prescribing AE that will facilitate ADL and mitigate the risk of falling.11 Some existing AEPP paper-based forms are presented in Figure 1.
Figure 1.
Paper-based measurement guidance currently used in practice.12,13
The prescription and fitment of inappropriate AE results not only in a failure to provide necessary assistance where it is needed but also has the potential of compounding the very fall risks that they were installed to mitigate. Despite the widespread provision of paper-based 2D visual guidance which aims to minimise inappropriate prescription and fitment, approximately 50 per cent of AE prescribed by clinicians is reported to be abandoned by patients,14–16 in part as a consequence of ‘poor fit’ between the AE, the patient, and the furniture on which it is installed.17,18 The impact of such practice is, therefore, significant and widespread and includes a negative impact on patient health outcomes; accelerated functional decline; an overall increase in exposure to fall risks in the home; and, more generally, an unnecessary depletion of valuable health-care resources.19
Existing and future technologies for falls prevention
The key areas in which falls prevention research is undertaken correspond to four overarching categories/sub-domains: (1) exercise interventions, (2) fall risk assessments; (3) education interventions, and (4) home assessments/prescription of assistive technologies.20 However, when exploring the technology-based applications that have been presented across the falls prevention research landscape, it appears that certain of these sub-domains have received significantly more attention than others. For example, there are numerous exercise intervention–focused systems such as that of Mirelman et al.,21 who augment treadmill exercise training with virtual reality technology to improve functional ability and cognitive function. Fall risk assessment systems include those presented by Staranowicz et al.22 and Weiss et al.23 which use motion capture sensors to monitor gait in real time and predict fall risks, providing early intervention where necessary. Falls prevention education is presented by Bell et al.,24 who combine a Nintendo Wii game console with falls prevention education to enhance patient awareness of the importance of reducing clutter, arranging furniture in the living area, positioning of the rugs, flooring types, lighting, and staircase and bathroom safety. However, with regard to the home assessments/prescription of assistive technologies sub-domain, there do not appear to be any applications that attempt to assist in this falls prevention activity. A recent survey of ‘state-of-the art’ falls prevention technology supports this finding, concluding that there is an urgent need to develop new technology-based applications and highlighting the potential of applying 3D visualisation technologies to this particular area of fall prevention practice.20
The term ‘3D visualisation technologies’ refers to computer graphics software applications that capitalise on natural aspects of human perception by the visual simulation of three spatial dimensions in 2D space, enabling the user to visualise, interact with, and control a given object within a 3D scope. The value of 3D visualisation technologies to the falls prevention research domain has already been demonstrated in a number of existing falls prevention research studies, which often focus on the area of exercise intervention.25,26 One existing study explores the potential of exploiting 3D visualisation technologies to assist clinicians in identifying extrinsic fall hazards. Du et al.27 developed a robotic system to automatically model patients’ home environments in 3D space. A 3D visualisation of the environment is constructed to assist clinicians in identifying the precise location and nature of extrinsic fall hazards. The use of 3D visualisations has also shown promise in being able to overcome the challenges of existing 2D clinical tools by improving the visual quality necessary to conceptualise visual cues as part of a particular treatment and assessment.28 For example, Spyridonis et al.29 found that enabling patients to report the type and precise location of back pain using a 3D visualisation of the human body was more accurate and intuitive than the traditional paper-based 2D model of the human body typically used in practice. Other studies have found similar benefits to using 3D visualisation to communicate other forms of pain to clinicians. For example, Jang et al.30 enable patients to express and communicate their symptoms of pain by annotating specific regions on an on-screen 3D representation of the human body using free-hand drawing.
Clinician perceptions and acceptance of technology
Designing usable tools, applications, and functionality that is aligned with the needs of the user are as important as the innovation itself.31,32 Patients and practitioners are more likely to engage with and adopt new technologies in practice if they are usable and are perceived to be compatible with their needs.33,34 Therefore, when developing technology-based health-care applications, it is crucial that clinicians’ needs and perceptions are understood and incorporated into every stage of the design and development process.35 User-centred design methods31 and technology adoption theories, such as the technology acceptance model (TAM), provide a means of gaining valuable insights into the factors that must be considered to ensure users adopt, accept, and use new technologies, and that these are incorporated into the design of that technology.6 Until recently, TAM has been used predominantly in a quantitative context; however, increasingly, the high-level TAM constructs, such as perceived usefulness (PU) and perceived ease of use (PEOU), are informing deductive qualitative user-centred design research on the incremental design and development of technological health innovations.28
Considering the equipment abandonment issues faced by the current AEPP process, issues relating to inaccurate measurement of furniture, and the subsequent ‘lack of fit’ of AE to the environment and patient, there is a need explore the potential value of utilising 3D visualisation technologies to aid the process of carrying out key measurement tasks as part of the AEPP. It should be noted, however, that equipment abandonment does not only occur because of inaccurate measurement or poorly prescribed equipment. There are a range of complex personal reasons involved, including perceived poor fit between the equipment and lifestyle, lack of volition to engage with rehabilitative activities, or desire to retain an unadapted home environment.36 The aims of this study are twofold. First, to develop and present a bespoke 3D mobile application prototype that provides AEPP measurement guidance to OTs via the use of 3D visualisation technologies. Second, to explore OTs’ perceptions of the prototype application, particularly its usability and the feasibility, challenges, and opportunities of its utilisation to support the AEPP in practice. Section ‘Conceptual design and application walkthrough’ of this article presents the details of an initial concept design phase deployed with OTs and provides a detailed walkthrough of the 3D mobile measurement guidance application. Section ‘Methods’ presents the main study which was conducted with OTs to explore utilisation of the 3D mobile application within the AEPP in practice. Section ‘Results’ presents the results. Section ‘Discussion’ outlines and discusses the key findings and proposes future design considerations and implications for deployment of the application in practice. Conclusions are drawn and details of future work are provided in section ‘Conclusion’.
Conceptual design and application walkthrough
As a first step towards developing the 3D measurement aid prototype (3D-MAP) application, an initial user-centred conceptual design phase was undertaken to ensure that the design and functionality of the application was aligned to the needs of clinicians. Three interaction designers and eight OTs currently utilising the 2D paper-based guidance to support the AEPP took part in this phase. Figure 2 presents the protocol of the initial conceptual design phase.
Figure 2.
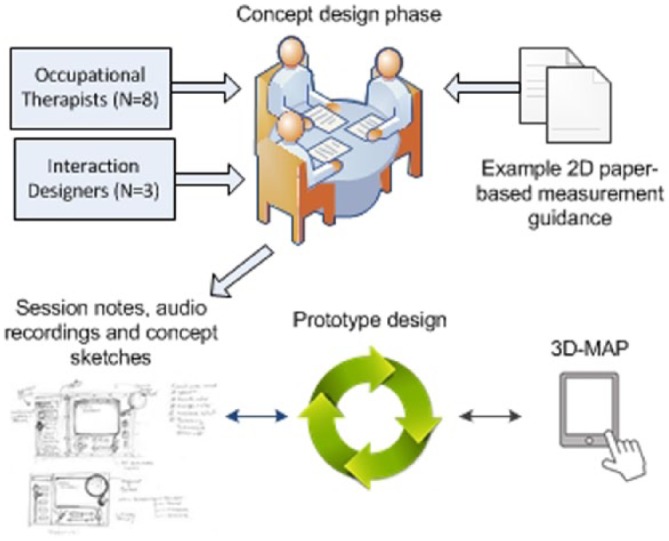
Overview of the protocol for the initial concept design phase.
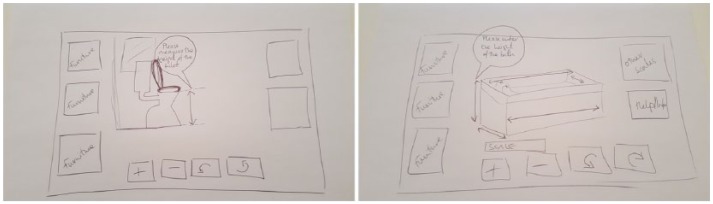
A sample of existing 2D paper-based measurement guidance leaflets was provided for participants to use as a point of reference during the conceptual design phase. OTs were asked to reflect on their experiences of using paper-based measurement guidance leaflets as part of their role. They were also shown a low fidelity prototype application which demonstrated how 2D representations of the patient and furniture could be presented using 3D visualisation technology, deployed on either a tablet, mobile phone, or laptop. Participants were asked to explore the idea of using a software application to assist in the AEPP and suggest the key features and functionality that they believed would be necessary if it was to replace paper-based leaflets. Furthermore, alongside the interaction designers, participants were encouraged to develop annotated concept sketches of a potential application interface and associated requirements and functionality. Figure 3 provides an example conceptual design sketch produced during a participatory design session.
Figure 3.
Concept sketches produced during the participatory design sessions.
Once all participatory design sessions were completed, notes and recordings of the sessions and the annotated concept sketches were perused and used to inform the design and development of the 3D-MAP application. Table 1 presents the key design requirements that emerged from these sessions.
Table 1.
Participatory design meeting user requirements.
| User and system requirements |
|---|
| UR1. Digitally record measurements on a 3D representation of the item |
| UR2. Clean and user-friendly UI |
| UR3. Rotate and zoom the 3D furniture models |
| UR4. Provide arrow prompts to input measurements |
| UR5. Generate assessment reports |
| UR6. Merge assessments and prescriptions with patient records |
| UR7. Implement on range of mobile platforms |
| UR8. Provide audio cues that instruct/guide users to measure effectively |
3D: three-dimensional; UI: user interface.
The 3D-MAP application
The 3D-MAP application used in this study has been developed taking into account the user requirements that emerged from initial conceptual design phase and in accordance with the 3D visualisation guidelines found in the literature.37,38 The system architecture and an application walkthrough is presented in this section.
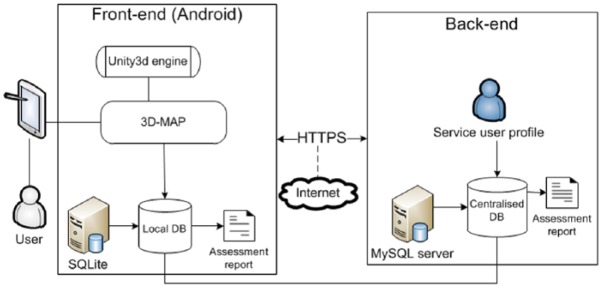
System architecture
The deployment platform chosen for the 3D-MAP is the Android operating system (OS). This is an open-source platform freely available for commercial and personal use. The application may be deployed on a range of devices, including mobile phones and tablets that are running an up-to-date version of Android OS. To support other required platform migrations in the future, the prototype was developed using a Unity3D game engine that allows multiplatform deployment, including Android, IOS, and Windows (UR7). The system architecture is presented in Figure 4.
Figure 4.
3D-MAP system architecture.
The key input mechanism/user interface used for the application is the standard touch screen interface provided by mobile Android devices. Users input measurements via the standard Android virtual touch screen keyboard. Measurement data are stored temporarily in a local database (DB) on the device in order to account for situations with limited wireless and/or mobile network connection. The stored data are then transmitted by hypertext transfer protocol (HTTPS) to a centralised MySQL DB, which is in an encrypted format and accessible only to authorised clinical users. Initially, the clinician sets up a service user profile before conducting their home assessments. All measurements are saved to a local DB and mirrored across to a centralised DB. The data collected include details of the service users’ functional ability, personal and furniture item measurements, their ability to transfer to and from furniture, as well as lying-to-stand transitions (UR6). Clinicians also have the option of generating an assessment report (UR5).
Application walkthrough
The 3D-MAP application integrates all the user requirements identified in the conceptual design sessions. A crucial feature of the 3D-MAP application is the visualisation of the measurement guidance, based on the paper-based leaflets currently in use.7,39–42 The prototype application did not include a facility to assist in taking measurements of the patient, but rather primarily focused on furniture measurement. The application displays 3D models of the five items most commonly measured as part of the AEPP (bed, bath, toilet, chair, and stairs) and are also known to be most frequently associated with falls in the home environment.43 Measurement guidance for each respective item is accessed via the main menu shown in Figure 5 (UR2).
Figure 5.

3D-MAP application’s main menu.
After selecting an item of furniture from the main menu, a representative 3D model of the chosen item is presented to the user, along with arrows that are superimposed onto the item which serve as prompts to indicate the discrete points on the furniture items that need to be measured (UR4). An example of the bath scene is presented in Figure 6.
Figure 6.
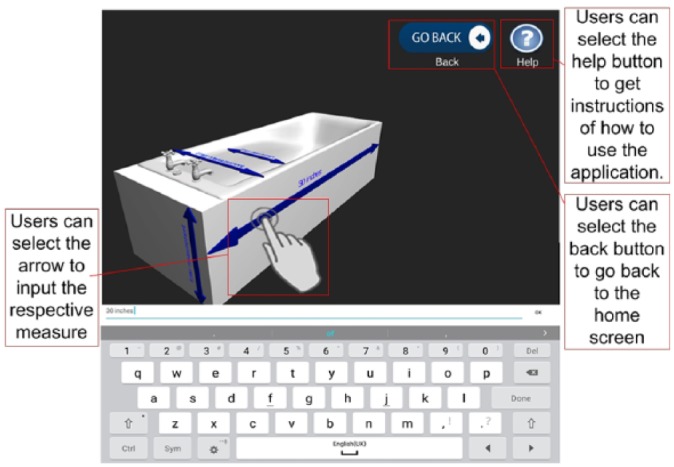
Bath measurement guidance interface.
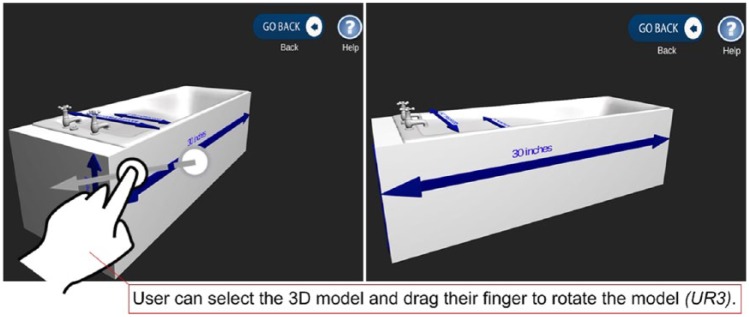
The measurement guidance is presented using two prompt features: 3D arrows, as mentioned above, and audio instructions which guide the user to provide the necessary measurements (UR8). Written instructions from the paper-based forms were taken and translated into audio files. Audio cues are activated when the arrows are touched, providing instructions on how and where to accurately measure specific parts of home furniture (UR8). Users can rotate the 3D furniture models to view discrete areas of interest in detail. To do so, the figure swipe gesture input was employed, which enabled rotation of the models (UR3). Figure 7 presents an example of rotating one of the models clockwise by swiping horizontally to the left.
Figure 7.
Rotation feature before rotation (left) and after rotation (right).
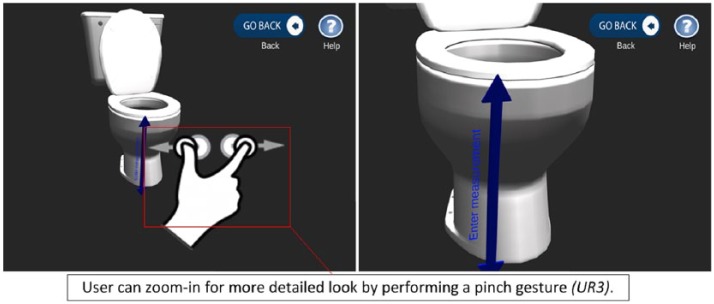
Another key component of the design is the zoom-in and zoom-out feature, which changes the viewpoint and perspective and provides for a more detailed look at the 3D furniture models. The ‘pinch gesture’ is used to achieve this (UR3). An example of this function is presented in Figure 8.
Figure 8.
Zoom in/out to facilitate better clinical guidance.
The application enables users to input home furniture measurements via the use of the arrow prompts augmented with sound instructions (UR1). The application is flexible in relation to the interface used and the visualisation capability, and audio cue options provided to clinicians are also optional for users who have grasped the use of the application, and no longer require audio assistance.
Methods
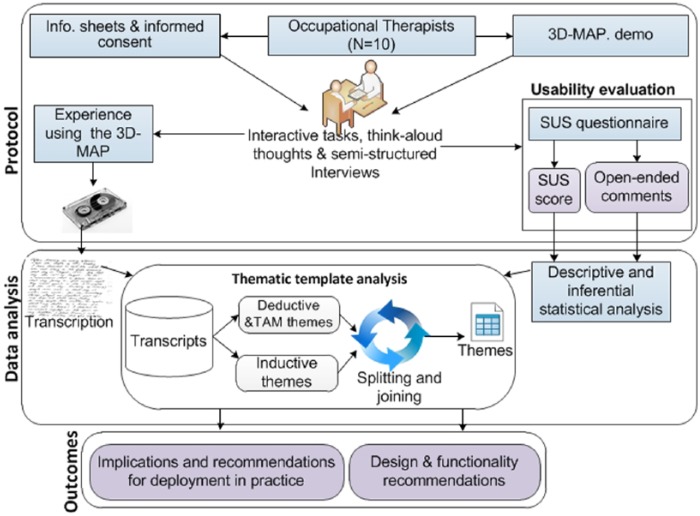
This section provides details of the data collection and analysis methods used to explore the perceptions of OTs regarding the use of the 3D-MAP application within the AEPP in practice. Figure 9 presents an overview of the study design.
Figure 9.
Overview study design.
Participants
A purposive sampling strategy was used for this study, which involved a total of 10 OTs. Participants were recruited via a range of sources, including online OT groups on social media networking websites (e.g. Facebook and LinkedIn), and by approaching local social service departments, NHS trusts, and specialist fall services. Candidates were initially sent an email invitation to take part in the study, with a £10 voucher offered as an incentive. The inclusion criteria were that participants were required to be practising OTs, had relevant clinical experience of carrying out home visit assessments, prescribed AE, and had familiarity with using a smartphone, tablet, or desktop computer. The sample size of 10 participants is in excess of the five-user assumption typically considered as a reliable guideline for carrying out usability and interaction design studies.44 All participants were female, which, to a large extent, reflects the female-dominated OT profession.45 Table 2 presents a summary of participant profiles.
Table 2.
Summary of participant profiles.
| Participant ID | Gender | Years of experience | Specialty |
|---|---|---|---|
| P1 | F | >31 | Adults of all ages |
| P2 | F | >10 | Social services |
| P3 | F | >5 | Surgical rehabilitation |
| P4 | F | >5 | Neurology therapy |
| P5 | F | >20 | Rehabilitation |
| P6 | F | >10 | Neurology |
| P7 | F | >1 | Neurology |
| P8 | F | >2 | Neurology |
| P9 | F | >5 | Re-ablement |
| P10 | F | >15 | Social services |
Protocol and instrumentation
Participant sessions were conducted on a one-to-one basis and were approximately 90 min in duration. Informed consent was obtained at the start of each session. Initially, participants were given a brief demonstration of the 3D-MAP application and were shown how to use the key functions of the application, record measurements, and generate assessment reports. Participants were then asked to use the application and were given written instructions outlining a series of interactive tasks to be carried out. Concurrently, the think-aloud technique was used to capture participant thoughts and preferences in real time while interacting with a software application.46 This involved encouraging participants to share their thoughts about the 3D-MAP application while interacting with it. We used prompts such as ‘what are you thinking?’ and ‘what are you doing now?’ if extended periods of silence were observed. The interactive task involved measuring home furniture items. Participants were asked to do the following.
On completion of the interactive task, participants were asked to complete a System Usability Scale (SUS) questionnaire,47 which was used to gain insight into the usability of the prototype application. The SUS is composed of 10 statements which users rate on a 5-point Likert-type scale ranging from 1 (‘strongly disagree’) to 5 (‘strongly agree’). After completion of the SUS instrument, each participant was asked to discuss the score they attributed to each SUS item. Semi-structured interviews were subsequently carried out with each participant at the end of the interactive sessions, which lasted approximately 20–25 min (mean = 22.4 min) each. Participants were encouraged to reflect on the experience of using the application, the functionality they found useful, challenging, or required improvement and to discuss the feasibility, challenges, and opportunities of using a 3D-MAP application as an assistive tool in practice. The interview questions were designed to enable participants to provide their feedback and experiences through open-ended discussion in order to investigate the AEPP in more depth and the potential ways that the application may be successfully integrated, in addition to identifying their particular needs for better visualisation of guidance. All interviews were recorded and transcribed verbatim.
Data analysis
Statistical analysis of SUS responses was carried out using IBM SPSS v 20.0.0. Initially, the approach presented by Bangor et al.48 was used to analyse and interpret the SUS scores. This involved calculating a SUS score from the completed questionnaires and generating a value on a 100-point scale which could then be mapped to descriptive adjectives (Worst Imaginable, Poor, OK, Good, Excellent, Best Imaginable), an acceptability range (Acceptable, Marginal, Not Acceptable), and a school grading scale (i.e. 90–100 = A, 80–89 = B, etc.). These baseline ranges and gradings are derived from a sample of over 3000 software applications, which provide the comparative baseline.48 Furthermore, Lewis and Sauro49 propose that SUS is composed of a two-factor structure in which two sub-scales – namely, Usability (SUS items S1, S2, S3, S5, S6, S7, S8, and S9) and Learnability (SUS items S4 and S10) – underpin the SUS instrument. Additional statistical analysis was performed using one-sample t-test to establish whether there were significant differences between the respective mean SUS scores and the mid-point value of three (of the 5-point Likert-type scale responses) for each individual SUS item and for the Usability and Learnability constructs.
Transcripts of audio recordings of the interactive task sessions and semi-structured interviews were subjected to thematic template analysis. This is a qualitative analysis method used for searching and identifying themes that occur within textual data sets.50 Using this method enabled patterns in the data set to be identified and categorised. Analysis of the semi-structured interview data was both inductive, as the development of the themes was data driven, and deductive, beginning with pre-defined (a priori) themes that are theory driven and linked to the analytical interest of researcher(s).51 The first stage involved creating a template which used the pre-defined codes specified by the TAM. Hence, analysis considered the participants’ perceptions of the 3D-MAP application in the context of the two high-level TAM themes, PU and PEOU, and themes that emerged in addition to these. The entire data set was then read, and comments were assigned iteratively through several stages of splicing, linking, deleting, and reassigning sub-themes within each pre-determined high-level theme.
Ethical considerations
The research study was reviewed and ethically approved by Brunel University Research Ethics Committee prior to any data collection. Informed consent was sought from each participant prior to taking part in the sessions. Each participant was guaranteed confidentiality and anonymity and was informed of their right to withdraw from the study at any time, both verbally and in written forms.
Results
This section presents the results of the analysis of the SUS, think-aloud, and semi-structured interview data.
SUS evaluation
The overall SUS score for the 3D-MAP application was 85 (85 out of 100; standard deviation (SD) = 5.6), which, according to the evaluation criteria for SUS,48 indicates that the application delivers ‘excellent’ (Descriptive adjective), ‘acceptable’ (Acceptability range), and ‘Grade B’ (School grading scale) levels of usability. An analysis of SUS Usability and Learnability revealed that both constructs achieved mean scores significantly above the neutral mid-point value of 3.00, 4.56 (p = 0.000) and 4.85 (p = 0.000), respectively. This indicates that users were positive about the Usability and Learnability of the application. Cronbach’s measure of consistency for both constructs was above the threshold of acceptable reliability of 0.6 for small sample studies;52 however, items S1, S5, and S8 were removed to reach the consistency threshold. The result of individual SUS items, compared against the mid-point, is presented in Table 3.
Table 3.
Mean SUS score and mid-point comparison.
| SUS item | Mid-point | 3D-MAP |
Gap score | df | t-value | p-value (two-tail) |
|---|---|---|---|---|---|---|
| Mean ± SD | ||||||
| S1: Use 3D-MAP frequently | 3.00 | 3.20 ± 1.14 | 0.20 | 9 | 0.55 | 0.591 |
| S2: Unnecessarily complexa | 3.00 | 4.60 ± 0.52 | 1.60 | 9 | 9.80 | 0.000* |
| S3: Easy to use | 3.00 | 4.60 ± 0.52 | 1.60 | 9 | 9.80 | 0.000* |
| S4: Support of a technical persona | 3.00 | 4.80 ± 0.42 | 1.80 | 9 | 13.50 | 0.000* |
| S5: The various functions were well integrated | 3.00 | 3.30 ± 0.95 | 0.30 | 9 | 1.00 | 0.343 |
| S6: Too much inconsistencya | 3.00 | 4.00 ± 0.94 | 1.00 | 9 | 3.35 | 0.008* |
| S7: Learn to use 3D-MAP very quickly | 3.00 | 4.60 ± 0.52 | 1.60 | 9 | 9.80 | 0.000* |
| S8: Cumbersome to usea | 3.00 | 4.30 ± 0.95 | 1.30 | 9 | 4.33 | 0.002* |
| S9: Confident using 3D-MAP | 3.00 | 4.60 ± 0.70 | 1.60 | 9 | 7.24 | 0.000* |
| S10: Learn a lot of things before using 3D-MAPa | 3.00 | 4.90 ± 0.32 | 1.90 | 9 | 19.00 | 0.000* |
SUS: System Usability Scale; SD: standard deviation.
Responses of negative items were reversed to align with positive items.
Statistically significant ≤0.05 confidence level.
All mean scores were above the mid-point, indicating that, overall, participants tended to be positive about the 3D application. In statistical terms, 8 of the 10 SUS items (S2–S4 and S6–S10) were significantly higher than the mid-point benchmark. Although items S1 and S5 were above the mid-point benchmark, there was no significant difference between the means and mid-point.
Item S1 asked participants to report how frequently they would like to use the application. While the mean score was higher than the mid-point benchmark, the difference was not significant (mean = 3.20, p = 0.591). There were mixed opinions about using the application frequently. Some OTs expressed an interest in its regular use provided that they had access to a tablet computer. Others suggested that the application required additional functionality before it could be fully incorporated into daily OT work activity, such as assisting in the task of recommending items of AE:
… if it’s around, I would use it, purely because you know I’ve not got scraps of paper …and also provided that we have a tablet, which we haven’t got. (P5)
As the application stands … I don’t think I would use it. If it was providing … a more visual impression to somebody in 3D … so I’m showing them a virtual drawing of what the rail is going to look like beside their bath … then possibly yes. (P1)
Results for S2 revealed that participants were positive about the application and tended to disagree that it was unnecessarily complex (mean = 4.60, p = 0.000). The application’s purpose appeared to be clear to participants; however, one participant working with patients with complex needs felt that additional functionality – such as a note-taking facility – would be a useful addition:
It’s not complex, what it’s lacking is the complexity. So as an OT, I’m looking into so many little details, so for example, I’m working in neurological ward at the moment, I need to consider so many abilities, disabilities of the patient, risks, that one, two, three measurements per furniture might not cover … I would have to write extra notes about that piece of equipment and extra take measurements because this wouldn’t give me enough information later on. (P6)
Responses to S3, relating to the application’s ease of use, were significantly higher than the mid-point (mean = 4.60, p = 0.000). Participants noted that the written instructions and audio cues provided by the application were basic but effective and that, overall, it was easy to use. Some expressed concerns about the alignment of measurement arrows for the chair item, which they felt provided ambiguous guidance:
Some of them I was doubting. What do you want me to measure, the width of the chair with the arms … or just the seat … it was somewhere in between, the arrow, so that wasn’t very clear, but otherwise using it … that’s very easy. (P5)
For S4, participants tended to disagree that there was a need for a technical person to be able to use the application (mean = 4.80, p = 0.000). One participant commented that it could even be used without a demonstration (P9). However, there was a feeling that technical support should be available if the application malfunctioned:
No, I’m OK with technology, so, and that was fairly easy, … but I think a normal person would be able to manage. (P9)
if it went wrong you … you’d like to know there was somebody on the end of the phone. (P6)
Mean scores for S5 were only marginally above the mid-point (mean = 3.30, p = 0.343). Explanatory comments relating to this statement revealed that while the application provided the necessary measurement guidance, it needed additional functionality such as the enabling the recording of additional information to supplement/contextualise the recorded measurements:
Yes, you’ve got the measurements for certain things but … I’d still need to have paper to write down all the additional information … it would be good to have it in one place. (P4)
Participants tended to disagree with (S6), the statement that there was too much inconsistency in the application (mean = 4.00, p = 0.008). However, some participants did suggest that the application would benefit from additional features, such as the ability to create bespoke measurement arrows.
Participants strongly agreed with S7, that people could learn to use the application very quickly (mean = 4.60, p = 0.000). However, one participant noted that some older adults might struggle if they were not familiar with touch screen devices:
… if you were asking … somebody older, it’s not true of all older generation but just some people who aren’t familiar with that type of technology might struggle a bit more with it. (P4)
Participants tended to disagree with S8, that is, the notion of the application being cumbersome to use (mean = 4.30, p = 0.002). The application interface tended to be perceived as simple in design with intuitive features and clear measurement instructions:
I think it’s quite simple in design. It’s quite clear what object you’re measuring … and easy to learn, easy to remember how to use it. (P8)
Participants tended to agree with statement S9 that they were confident about using the application (mean = 4.60, p = 0.000). The ability to change measurement values (as opposed to ‘cross-out’ paper-based values) was a factor that helped participants to have confidence when using the application.
The results for S10 indicate that users disagreed with the notion of having to learn a lot of things prior to using the application (mean = 4.90, p = 0.000). In particular, participants commented that the application was user-friendly; however, some emphasised that a basic understanding of touch screen technology was a prerequisite for using the application:
If they’ve got kind of a basic understanding of technology, are able to use it, then yeah, it’s very user-friendly. (P4)
Semi-structured interview results
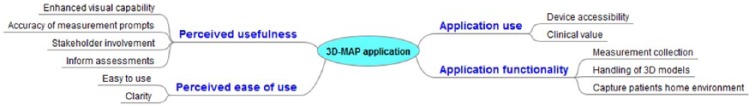
Four high-level themes and numerous sub-themes were identified as a result of the thematic analysis of the think-aloud interactive task data and semi-structured interview data. These are (1) PU, (2) PEOU, (3) application use, and (4) application functionality. Figure 10 presents a thematic mind map of the key themes and sub-themes.
Figure 10.
Thematic mind map of key themes and associated sub-themes.
PU
Participants reported that they were satisfied with the enhanced visual capability of the 3D application, compared with the equivalent 2D diagrams presented in paper-based measurement guidance leaflets. In particular, they highlighted that the 3D models seemed to offer a more realistic representation of the item they were measuring and aided them to better comprehend the precise measurement locations. Some participants believed that the visual clarity of the 3D visualisations could also help to improve patient’s understanding of measurements taken and how the process translated to fitment of AE in the home. However, the application in its current form does not show how AE fits onto items of home furniture, or, indeed, how these fit within the context of the home environment. This is a function which some participants felt would enhance its usefulness:
… it was useful looking at a 3D model, rather than just you know a flat model … as an OT you’re kind of used to doing it flat but … if service users are (going to look at it) it’s good to see it in 3D, it’s more easy to understand. (P5)
… so they can have a look and then look at the 3D dimensions, it might give people a better idea. (P9)
Some participants were of the opinion that while the look and feel of the 3D models were a significant improvement, the accuracy of measurement prompts was lacking in some respects, which could affect how the measurement guidance is interpreted and impact negatively on the reliability of the data collected:
… Some of the arrows were not working when pressed and I think it could have done with more aligning … you know, showing you exactly where you measure from. (P4)
Participants felt that the use of the application would support enhanced and wide-ranging stakeholder involvement in the AEPP. For example, it was considered that the application could be used by patients’ family members or carers, who may be able to take furniture measurements on behalf of the service user. The application was also seen as having potential educational value for OT students to practice and familiarise themselves with measurement tasks:
I would use it to give it to family members to measure things. (P7)
As the application is now, probably it would be useful for OT students, you know just like for practise, to get used to measuring and recording measurements. (P6)
It was also suggested that while the application may not necessarily make the act of carrying out measurements any easier, it would have value helping to inform assessments, that is, provide more effective prompts to ensure the relevant dimensions of items are measured and collected in accordance with existing guidelines:
It could serve as a prompt. I don’t know if it would make measurements … any easier, but I think it would help. (P7)
PEOU
Overall, participants felt that the 3D application was easy to use. However, one participant believed that the rotation of the 3D models was awkward, especially to get the model back to its original starting position. Consequently, it was suggested that a feature to reset the 3D model position was incorporated:
Yeah, fairly easy, just the rotation was a little tricky to kind of get it back to normal view. Maybe if you had a button to reset it back to what it was when you first moved it. (P5)
Participants noted that the clarity, look and feel of the application, and the instructions it provided were clear. In particular, the icons on the main menu clearly indicated what each section included (participant P4):
I think the simplicity … all you do is add a number basically (a measurement) and the visuals are very clear. (P4)
Application use
Benefits of using the application compared to paper-based approaches were also highlighted. Some participants expressed their intention to use the application but stressed the need for access to a tablet if they were to be able to use it in practice:
I thought it was easy to use and not more complicated certainly than a pad or a form that you would otherwise fill in by hand. So yeah, the simplicity of it I think is making it user-friendly. I would use it … is this only available on a tablet because we don’t have access to these. (P9)
It was also suggested that using the 3D-MAP application in practice could be of clinical value to collaborate with other clinicians and service users. More specifically, it was felt that the application would be useful for handing over a case to another OT. Value was also seen in integrating recorded measurements with other information such as assessment notes about service users, which would save time and effort:
I think if it incorporated more of the whole report thing, so you weren’t kind of having to go from paper to tablet, then definitely, it would be even better. (P7)
Sometimes, like if I want to order rails for instance, I’ll take a picture, go back, e-mail it to myself and then go on to paint and draw a rail on top of the picture and then send it to the equipment company. So … if I could just screen shot that rail on the bathroom, then that would make my life easier! (P8)
Application functionality
Participants felt that using the 3D-MAP application would provide clinical value and were enthusiastic with respect to measurement collection, which, with the help of the application, could be done in a more standardised and systematic fashion. Some additional application features were suggested, particularly with regard to enabling better control and handling of the 3D models within the application. Some participants expressed a need to include a function to photographically capture patients’ home environment, particularly the item being measured, so that there was a pictorial record as a point of reference alongside the annotated 3D model of the furniture item. It was felt that having photographic records of the item – ideally in its context within the home – would help shed light on issues that may later feed into the decision-making of selecting AE:
If there could be a photo, capturing more information, possibly that might be useful more than me asking them or writing and drawing on a piece of paper. (P6)
Discussion
This study presented a mobile application which uses 3D visualisation technology, designed to guide and assist OTs in the taking and recording of measurements as part of the AEPP. A total of 10 OTs used the 3D-MAP application to engage in a measurement task of home furniture known to be associated with falls and routinely measured as part of the AEPP. The analysis of the quantitative SUS data revealed that the sample attributed a score of 85/100 to its Usability, indicating that the application may be described as ‘excellent’, delivering ‘acceptable’, ‘Grade B’, levels of usability overall. In terms of the two SUS sub-scales, OTs also tended to strongly agree with statements related to the Usability and Learnability of the application. The SUS results highlighted a general consensus that the application was easy to use and that learning to use it was also straightforward. These are promising results, and it is likely that the early conceptual design phase and participatory design sessions conducted with a separate sample of OTs played an important role in ensuring that the 3D-MAP application was fit for purpose and able to generate a range of comments about the overall concept of using 3D visualisation technologies during the main trial, as opposed to being related to fundamental usability issues only. Analysis of the individual SUS items and associated open-ended comments, along with think-aloud and semi-structured interview data, provided detailed study outcomes on the perceived feasibility, usability, challenges, and opportunities of the application being deployed in practice. Table 4 presents a summary of the key study outcomes and categorises these in terms of implications for deployment in practice and design and functionality recommendations. Each of these outcomes are mapped to their respective sources, that is, individual SUS items (S1–S10) and/or the high-level inductive and deductive themes that emerged from the analysis of the semi-structured interviews (PU, PEOU, Actual Use [AU], and Application Functionality [AF]).
Table 4.
Study outcomes, implications, and recommendations.
| Areas of focus | Study outcomes | Source |
|---|---|---|
| Implications and recommendations for deployment in practice | Clear and usable application without the need for technical expertise/support | S2–S4,S6–S8 |
| Valuable tool to facilitate collaborative practice and inter-professional handover | AU | |
| Enhanced visual quality of home furniture measurement guidance | S1, PU | |
| Systematic, organised solution which instils confidence | S1, S9 | |
| Standardised furniture measurement guidance, clear instructions | PU, PEOU, S3 | |
| Explore use by alternative users including care givers and service users | S7, PU | |
| Include educational component regarding AE and measurement function | PU | |
| Access to tablets is necessary in order to use the 3D application | AU | |
| Design and functionality recommendations | Provide improved guidance to make assistive equipment recommendations | S1 |
| Provide a facility to record notes and assessment data | S2, S5 | |
| Clearer prompts to measure home furniture | S3 and PU | |
| Clear and more usable controls to rotate 3D models | PEOU | |
| Additional function to reset the 3D models to its original position | PEOU | |
| Capture images of the patients environment to provide context | AF, PU |
PU: perceived usefulness; PEOU: perceived ease of use; 3D: three-dimensional.
In terms of implications and recommendations for deployment in practice, OTs reported that they felt that the application could be used in practice without the need for technical support, assuming that there was no malfunction (S4). The interface was perceived as being clear (S2 and S8), consistent (S6), and easy to use (S3) and requiring minimal levels of effort to learn how to utilise key features and functionality (S7). Interestingly, it was suggested that even ‘a normal person would be able to manage with the app’ (S4) implying that there may be scope for non-OT engagement with application, such as by service users, care givers and other health-care professionals. It was also submitted that the use of such an application could help to enhance collaborative practice (AU) in a team of clinicians, for example, when handing over referrals or to enable patients to take measurements of their own, which, in turn, could be used to inform shared decision-making related to AE prescription.
The notion of empowering patients to take their own measurements has become an important emerging area of interest in the field of occupational therapy and within the AEPP, particularly given increasing constraints on health-care sector budgets.53 This finding, in particular, supports the personalisation agenda which advocates the delivery of home-based health-care services and the enablement of older patients to engage in self-assessment practice.54 While the personalisation agenda promises numerous health benefits to the patient, it is also seen as a strategy to reduce costs and lessen the burden on health-care systems. Specifically, in this respect, it should be noted that OTs make up 2 per cent of the health and social care sector, with 35 per cent of adult care service referrals having to be handled by them.55 Although further research is required to establish the extent to which this application is usable by other user types, its realisation would certainly complement the evident need to move away from the view of the patient as a passive recipient of care, to models where they are responsible for carrying out important aspects of their own care.56 The observation that the application provides a systematic, organised (S1, PU), and standardised (PU) solution that helps to instil confidence in the user, while recording accurate measurements is a positive implication for deployment in practice (S1, S9). The fact that measurements can be input and easily changed, if the initial entry was found to be inaccurate, was seen as a significant benefit over paper-based records. It was felt by most of the participants that the application provided clear prompts of where to measure, using the 3D arrows alongside audio instructions (PU, PEOU, S3).
Furthermore, use within a health education setting (S7, PU) was suggested, particularly to educate trainee/junior OTs on the practice of measurement. These findings are in line with a recent review that explored the value of 3D visualisation technology for educational health interventions to inform and shape clinical practice in a simulated environment, prior to implementing interventions in practice.57 This is a particularly important finding given that approximately 50 per cent of AE prescribed is abandoned14–16,43 partly due to the ‘poor fit’ as a result of misinterpretation of guidance and absence of standardised measurement practice.43,58 Due to the heterogeneous practice of the AEPP across UK NHS trusts, and the lack of consensus in terms of practice,59 the 3D application was seen as having potential to improve and standardise the measurement process (PU). The present findings are also supported by a recent study which concluded that there is a need to standardised measurement guidance, particularly for the provision of AE.60 Clinicians viewed the 3D-MAP application as a tool which improved the visual quality and detail/clarity of measurement guidance (S1, PU), constituting an alternative solution to the typical 2D diagrams currently in use across NHS trusts. This finding is consistent with those of past studies by Spyridonis et al.,29 which found that 3D visualisation technology improved the visual quality of 2D paper-based assessments currently in use, visualising and locating exact points on 3D models that are of clinical relevance and importance. Another study found that 3D visualisation enhanced visualisations of patients’ movements, highlighting discrete areas to target for rehabilitation exercise programmes.61 However, one key obstacle to an application such as 3D-MAP being adopted in practice is the availability of mobile touch screen devices. Some participants commented that they did not have access to such devices, and, consequently, although the deployment of the application may be desirable, it is not feasible in practice until such technologies are provided. Although this issue is not related directly to the usability/functionality of the application, it still poses a problem to realising the benefits that such applications may be capable of.62 A significant concern which continues to persist for clinicians is how to successfully integrate new technology in practice. While incorporating the needs and requirements of clinicians into the application was a key lesson learned, issues with using the application in practice (which would require a supporting infrastructure) and the impact of its adoption would need to be addressed and closely studied before its deployment in the field. This supported by previous findings, particularly as the maintenance and deployment of any new technology typically requires changes to the health organisation, delivery of care, and collaboration between clinicians and patients.32,63 More broadly, this research is aligned with the UK government’s encouragement for clinicians to adopt new technologies and develop associated strategies that respond to ongoing challenges in health-care delivery.4,64 Having technology that addresses issues with prescribing the right AE could have cost-saving implications for the health and social care system,19 providing that adequate training and support is available to stakeholders. While implications that relate to deploying the application in practice have been noted in this study, the application as a component is interoperable; hence, giving some flexibility to clinicians from different health services to develop their own ad hoc solutions via the support of the application and move away from a ‘one-size-fits-all’ approach.
There were numerous design and functionality recommendations that emerged from this study, which indicate how the application may be further developed to accommodate the needs of OTs who intend to use the application in practice (and, in doing so, possibly further enhance the application’s functionality). For example, the measurement guidance provided by the current version of the application requires further extension to help prescribe appropriate AE for the item of furniture that has been measured (S1). Several suggestions were made regarding the need for a facility to record notes in conjunction with the assessment data collected, as the clinical decision-making process for prescribing equipment includes clinicians’ observations of patients carrying out day-to-day activities (S2 and S5). Participants expressed the need for clearer visual prompts to measure home furniture items, as some of these appeared to be unclear and/or counterintuitive, which could impact the reliability of users interpreting the guidance for logging accurate measurements (S3, PU). This requirement is particularly important considering that the application was developed to enhance the visualisation of measurement guidance using 3D models and arrows to sufficiently locate end-to-end points on an arrow. Participants expressed that they had trouble rotating the 3D models. Consequently, it is concluded that the controls were counterintuitive and need further development, especially given that older patients may use this application (PEOU). Several further adaptations were suggested, in particular, to better handling for the 3D model by resetting its position, to help remedy the current counterintuitive rotation function (PEOU). There is a need to explore alternative controls that can be implemented to improve the current ones for manipulating the viewpoint/position of the 3D models and better support both patient and clinical users of the application. Furthermore, it should be noted that this prototype 3D-MAP application did not include a facility to assist in taking measurements of the patient, but rather focused on furniture measurement. Future work should include this additional function and explore how the application may be further developed to ensure an accurate fit between the patient and the prescribed equipment is achieved.
Enabling photographic capture of the patients’ home environment, particularly images of the home furniture items within their real-world context (AF), could provide important information that may be used when prescribing AE. Existing studies in the literature have explored the use of taking images of the patient’s home to provide a visual aid to support clinical decision-making/reasoning and serve as an adjunct to or substitute for the traditional home visit assessment.65 Interestingly, some participants mentioned using their smartphones to take photographs during home visits to help with their assessments and the decision-making process for recommendations. This particular feature has been reported in the literature as being a valuable technique within the provision of home visit assessments and AE to explore the feasibility of home modifications and to remotely inspect the home environment for extrinsic fall risk factors.65,66 As such, this shows the potential of a photographic feature may have value over and above the provision of detailed guidance for recording measurements.
Conclusion
This study investigated OTs’ perceptions regarding the feasibility, opportunities, and challenges of using the 3D-MAP application prototype as a measuring tool within the AEPP. OTs were positive about the application, in terms of its usability by them as part of AEPP practice and, potentially, other stakeholders such as care givers, trainee OTs, and patients. The study also showed that OTs considered that the 3D-MAP application has the potential to effectively augment existing 2D diagrams and deliver numerous benefits over these. For example, OTs believed that 3D-MAP enhanced the visual quality of measurement guidance via the use of browseable 3D models, more clearly articulated the discrete points of measurement, and introduced the opportunity for patients and clinicians to engage in greater collaborative practice and possible easing of the handover process. One of the key challenges to deploying such an application, however, is the lack of availability of mobile touch screen devices to practitioners. Further research is needed to establish whether such an application could feasibly be used by service users, family members, and care givers and to include the facility to assist in the measurement of the patient as well as the home environment. It is also necessary for more research to be conducted into the clinical utility of this application in terms of its efficiency, effectiveness, and the relative accuracy and reliability of measurements recorded by clinicians using the 3D-MAP application compared with 2D paper-based guidance leaflets.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was in part funded by the Royal Society grant Ref: RG130826.
Contributor Information
Arthur G Money, Brunel University London, UK.
Anita Atwal, London South Bank University, UK.
Gheorghita Ghinea, Brunel University London, UK.
References
- 1. Logan PA, Coupland CA, Gladman JR, et al. Community falls prevention for people who call an emergency ambulance after a fall: randomised controlled trial. BMJ 2010; 340: c2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006; 35(suppl. 2): ii37–ii41. [DOI] [PubMed] [Google Scholar]
- 3. Craig J, Murray A, Mitchell S, et al. The high cost to health and social care of managing falls in older adults living in the community in Scotland. Scott Med J 2013; 58(4): 198–203. [DOI] [PubMed] [Google Scholar]
- 4. Department of Health. Equity and excellence: liberating the NHS (white paper). London: The Stationery Office, 2010. [Google Scholar]
- 5. Money AG, Barnett J, Kuljis J, et al. Patient perceptions and expectations of an anticoagulation service: a quantitative comparison study of clinic-based testers and patient self-testers. Scand J Caring Sci 2015; 29(4): 662–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Atwal A, Money AG, Harvey M. Occupational therapists’ views on using a virtual reality interior design application within the pre-discharge home visit process. J Med Internet Res 2014; 16(12): e283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Southwark. OT specialist assessment form, 2017, http://www.proceduresonline.com/southwarkadults/user_controlled_lcms_area/uploaded_files/OT%20specialist%20assessment%20_V3%20.docx
- 8. College of Occupational Therapists. Occupational therapy in the prevention and management of falls in adults: practice guideline. London: College of Occupational Therapists Ltd, 2015, pp. 1–126. [Google Scholar]
- 9. Hoffmann T, McKenna K. A survey of assistive equipment use by older people following hospital discharge. Br J Occup Ther 2004; 67(2): 75–82. [Google Scholar]
- 10. Buning M, Hammel J, Angelo J, et al. Assistive technology within occupational therapy practice (2004). Am J Occup Ther 2004; 58(6): 678–680. [DOI] [PubMed] [Google Scholar]
- 11. Atwal A, Luke A, Plastow N. Evaluation of occupational therapy pre-discharge home visit information leaflets for older adults. Br J Occup Ther 2011; 74(8): 383–386. [Google Scholar]
- 12. Tool Oxfordshire Self Assessment (OsSA). How to measure your bath to decide on the correct size of bath board to order, 2016, https://www.oxfordshire.gov.uk/cms/sites/default/files/folders/documents/socialandhealthcare/adultsocialcare/livingathome/equipmentaidsadaptations/BathMeasure.pdf
- 13. Tool OsSA. How to measure your toilet to decide on the correct height toilet seat to order, 2016, https://www.oxfordshire.gov.uk/cms/content/home-assessment-equipment-aids-and-adaptations
- 14. Nygård L, Grahn U, Rudenhammar A, et al. Reflecting on practice: are home visits prior to discharge worthwhile in geriatric inpatient care? Scand J Caring Sci 2004; 18(2): 193–203. [DOI] [PubMed] [Google Scholar]
- 15. Martin JK, Martin LG, Stumbo NJ, et al. The impact of consumer involvement on satisfaction with and use of assistive technology. Disabil Rehabil Assist Technol 2011; 6(3): 225–242. [DOI] [PubMed] [Google Scholar]
- 16. Gitlin LN. Why older people accept or reject assistive technology. Generations 1995; 19(1): 41–46. [Google Scholar]
- 17. Federici S, Corradi F, Meloni F, et al. Successful assistive technology service delivery outcomes from applying a person-centered systematic assessment process: a case study. Life Span Disab 2015; 18(1): 41–74. [Google Scholar]
- 18. Federici S, Scherer MJ, Borsci S. An ideal model of an assistive technology assessment and delivery process. Technol Disabil 2014; 26(1): 27–38. [Google Scholar]
- 19. Goodacre K, McCreadie C, Flanagan S, et al. Enabling older people to stay at home: the costs of substituting and supplementing care with assistive technology. Br J Occup Ther 2008; 71(4): 130–140. [Google Scholar]
- 20. Hamm J, Money AG, Atwal A, et al. Fall prevention intervention technologies: a conceptual framework and survey of the state of the art. J Biomed Inform 2016; 59: 319–345. [DOI] [PubMed] [Google Scholar]
- 21. Mirelman A, Rochester L, Reelick M, et al. V-TIME: a treadmill training program augmented by virtual reality to decrease fall risk in older adults: study design of a randomized controlled trial. BMC Neurol 2013; 13(1): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Staranowicz A, Brown GR, Mariottini G-L. Evaluating the accuracy of a mobile Kinect-based gait-monitoring system for fall prediction. In: Proceedings of the 6th international conference on PErvasive technologies related to assistive environments, Rhodes, 29–31 May 2013 New York: ACM. [Google Scholar]
- 23. Weiss A, Brozgol M, Dorfman M, et al. Does the evaluation of gait quality during daily life provide insight into fall risk? A novel approach using 3-day accelerometer recordings. Neurorehabil Neural Repair 2013; 27(8): 742–752. [DOI] [PubMed] [Google Scholar]
- 24. Bell CS, Fain E, Daub J, et al. Effects of Nintendo Wii on quality of life, social relationships, and confidence to prevent falls. Phys Occup Ther Geriatr 2011; 29(3): 213–221. [Google Scholar]
- 25. Uzor S, Baillie L. Exploring & designing tools to enhance falls rehabilitation in the home. In: Proceedings of the SIGCHI conference on human factors in computing systems, Paris, 27 April–2 May 2013 New York: ACM. [Google Scholar]
- 26. Doyle J, Bailey C, Dromey B, et al. BASE – an interactive technology solution to deliver balance and strength exercises to older adults. In: Proceedings of the international conference on pervasive computing technologies for healthcare (PervasiveHealth) (ed J Doyle, C Bailey, B Dromey, et al. ), Munich, 22–25 March 2010 New York: IEEE. [Google Scholar]
- 27. Du R, Jagtap V, Long Y, et al. Robotics enabled in-home environment screening for fall risks. In: Proceedings of the 2014 workshop on mobile augmented reality and robotic technology-based systems, Bretton Woods, 16 June 2014 New York: ACM. [Google Scholar]
- 28. Money AG, Atwal A, Young KL, et al. Using the Technology Acceptance Model to explore community dwelling older adults’ perceptions of a 3D interior design application to facilitate pre-discharge home adaptations. BMC Med Inform Decis Mak 2015; 15(1): 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Spyridonis F, Gawronski J, Ghinea G, et al. An interactive 3-D application for pain management: results from a pilot study in spinal cord injury rehabilitation. Comput Methods Programs Biomed 2012; 108(1): 356–366. [DOI] [PubMed] [Google Scholar]
- 30. Jang A, MacLean DL, Heer J. BodyDiagrams: improving communication of pain symptoms through drawing. In: Proceedings of the 32nd annual ACM conference on Human factors in computing systems, Toronto, Canada, 26 April–1 May 2014 New York: ACM. [Google Scholar]
- 31. Money AG, Barnett J, Kuljis J, et al. The role of the user within the medical device design and development process: medical device manufacturers’ perspectives. BMC Med Inform Decis Mak 2011; 11: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Greenhalgh T, Procter R, Wherton J, et al. What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med 2015; 13(1): 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Calvin KL, Ben-Tzion K. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc 2009; 16(4): 550–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Barnett J, Harricharan M, Fletcher D, et al. myPace: an integrative health platform for supporting weight loss and maintenance behaviors. IEEE J Biomed Health Inform 2015; 19(1): 109–116. [DOI] [PubMed] [Google Scholar]
- 35. Atwal A, McIntyre A, Craik C, et al. Occupational therapists’ perceptions of predischarge home assessments with older adults in acute care. Br J Occup Ther 2008; 71(2): 52–58. [Google Scholar]
- 36. Lilja M, Bergh A, Johannson L, et al. Attitudes towards rehabilitation needs and support from assistive technology and the social environment among elderly people with disability. Occup Ther Int 2003; 10(1): 75–93. [DOI] [PubMed] [Google Scholar]
- 37. Vinson NG. Design guidelines for landmarks to support navigation in virtual environments. In: Proceedings of the SIGCHI conference on human factors in computing systems (ed Vinson NG.), Pittsburgh, PA, 15–20 May 1999 New York: ACM. [Google Scholar]
- 38. Burigat S, Chittaro L. Navigation in 3D virtual environments: effects of user experience and location-pointing navigation aids. Int J Hum-Comput St 2007; 65(11): 945–958. [Google Scholar]
- 39. Living made easy. Toilet height, 2017, http://www.livingmadeeasy.org.uk/scenario.php?csid=327
- 40. Assistireland. Choosing a chair and chair accessories, 2017, http://www.assistireland.ie/eng/Information/Information_Sheets/Choosing_a_Chair_and_Chair_Accessories.html
- 41. Robert Jones and Agnes Hunt Orthopaedic Hospital. Patient home information form, 2017, https://www.rjah.nhs.uk/RJAHNHS/files/56/56787067-d87f-4623-a883-df774a0590fd.pdf
- 42. DLF. Choosing equipment to get up and down stairs, 2017, http://www.dlf.org.uk/factsheets/stairs
- 43. Williamson JD, Fried LP. Characterization of older adults who attribute functional decrements to ‘old age’. J Am Geriatr Soc 1996; 44: 1429–1434. [DOI] [PubMed] [Google Scholar]
- 44. Borsci S, Macredie RD, Barnett J, et al. Reviewing and extending the five-user assumption: a grounded procedure for interaction evaluation. ACM T Comput: Hum Int 2013; 20(5): 29. [Google Scholar]
- 45. Brown T, Williams B, Jolliffe L. Leadership style preference of undergraduate occupational therapy students in Australia. Hong Kong J Occup Th 2014; 24(1): 35–42. [Google Scholar]
- 46. Van Den Haak M, De Jong M, Jan Schellens P. Retrospective vs. concurrent think-aloud protocols: testing the usability of an online library catalogue. Behav Inf Technol 2003; 22(5): 339–351. [Google Scholar]
- 47. Brooke J. SUS: a quick and dirty usability scale. In: Jordan PW, Thomas B, McClelland IL. (eds) Usability evaluation in industry. Boca Raton, FL: CRC Press, 1996, pp. 189–194. [Google Scholar]
- 48. Bangor A, Kortum P, Miller J. Determining what individual SUS scores mean: adding an adjective rating scale. J Usability Stud 2009; 4(3): 114–123. [Google Scholar]
- 49. Lewis JR, Sauro J. The factor structure of the system usability scale. In: Proceedings of the 1st international conference on human centered design (HCD 2009), San Diego, CA, 19–24 July 2009, pp. 94–103. Berlin: Springer. [Google Scholar]
- 50. Joffe H, Yardley L. Content and thematic analysis. In: Marks DF, Yardley L. (eds) Research methods for clinical and health psychology. London: SAGE, 2004, pp. 56–68. [Google Scholar]
- 51. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3(2): 77–101. [Google Scholar]
- 52. Hair JF, Black WC, Babin BJ, et al. Multivariate data analysis. Upper Saddle River, NJ: Pearson Prentice Hall, 2006. [Google Scholar]
- 53. Isaacson M. Best practices by occupational and physical therapists performing seating and mobility evaluations. Assist Technol 2011; 23(1): 13–21. [Google Scholar]
- 54. Tucker S, Brand C, O’Shea S, et al. An evaluation of the use of self-assessment for the provision of community equipment and adaptations in English local authorities. Br J Occup Ther 2011; 74(3): 119–128. [Google Scholar]
- 55. Boniface G, Mason M, Macintyre J, et al. The effectiveness of local authority social services’ occupational therapy for older people in Great Britain: a critical literature review. Br J Occup Ther 2013; 76(12): 538–547. [Google Scholar]
- 56. Department of Health. Liberating the NHS: no decision about me without me. London: The Stationery Office, 2012, pp. 1–41. [Google Scholar]
- 57. Saxena N, Kyaw BM, Vseteckova J, et al. Virtual reality environments for health professional education. The Cochrane Library, 2016, http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD012090/full [Google Scholar]
- 58. Wielandt T, Strong J. Compliance with prescribed adaptive equipment: a literature review. Br J Occup Ther 2000; 63(2): 65–75. [Google Scholar]
- 59. Atwal A, Paraskevopoulos I, Spiliotopoulou G, et al. How are service users instructed to measure home furniture for provision of minor assistive devices? Disabil Rehabil Assist Technol 2015; 12(2): 153–159. [DOI] [PubMed] [Google Scholar]
- 60. Spiliotopoulou G, Atwal A. Embedding the personalization agenda in service users’ self-assessment for provision of assistive devices. Br J Occup Ther 2014; 77(10): 483. [Google Scholar]
- 61. Loudon D, Macdonald AS, Carse B, et al. Developing visualisation software for rehabilitation: investigating the requirements of patients, therapists and the rehabilitation process. Health Informatics J 2012; 18(3): 171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Erickson K. Evidence considerations for mobile devices in the occupational therapy process. Open J Occup Ther 2015; 3(2): 7. [Google Scholar]
- 63. Mort M, Roberts C, Pols J, et al. Ethical implications of home telecare for older people: a framework derived from a multisited participative study. Health Expect 2015; 18(3): 438–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Darzi A. (ed.). High quality care for all NHS next stage review final report. London: Department of Health, 2008. [Google Scholar]
- 65. Daniela H, Oesch P, Stuckd AE, et al. Evaluation of a novel photography-based home assessment protocol for identification of environmental risk factors for falls in elderly persons. Swiss Med Wkly 2013; 143: w13884. [DOI] [PubMed] [Google Scholar]
- 66. Ritchey KC, Meyer D, Ice GH. Non-therapist identification of falling hazards in older adult homes using digital photography. Prev Med Rep 2015; 2: 794–797. [DOI] [PMC free article] [PubMed] [Google Scholar]