Abstract
Purpose
The optimal method for intracorporeal esophagojejunostomy remains unclear because a purse-string suture for fixing the anvil into the esophagus is difficult to perform with a laparoscopic approach. Therefore, this study aimed to evaluate our novel technique to fix the anvil into the esophagus.
Materials and Methods
This retrospective study included 202 patients who were treated at our institution with an intracorporeal circular esophagojejunostomy in a laparoscopy-assisted total gastrectomy with a Roux-en-Y reconstruction (166 cases) or a laparoscopy-assisted proximal gastrectomy with jejunal interposition (36 cases). After incising 3/4 of the esophageal wall, a hand-sewn purse-string suture was placed on the esophagus. Next, the anvil head of a circular stapler was introduced into the esophagus. Finally, the circular esophagojejunostomy was performed laparoscopically. The clinical characteristics and surgical outcomes were evaluated and compared with those of other methods.
Results
The average operation time was 200.3 minutes. The average hand-sewn purse-string suturing time was 6.4 minutes. The overall incidence of postoperative complications (Clavien–Dindo classification grade ≥II) was 26%. The number of patients with an anastomotic leakage and stenosis at the esophagojejunostomy site were 4 (2.0%) and 12 (6.0%), respectively. All patients with stenosis were successfully treated by endoscopic balloon dilatation. There was no mortality. Regarding the materials and devices for anvil fixation, only 1 absorbable thread was needed.
Conclusions
Our procedure for hand-sewn purse-string suturing with the double ligation method is simple and safe.
Keywords: Laparoscopy, Gastrectomy, Anastomosis, Postoperative complications
INTRODUCTION
The laparoscopy-assisted distal gastrectomy is widely used for the treatment of early gastric cancer because of its safety, minimal invasiveness, and acceptable long-term outcomes [1,2,3]. In contrast, a laparoscopy-assisted total gastrectomy (LATG) is less commonly performed due to technical difficulties associated with the reconstruction procedure and concerns about anastomotic complications such as leakage and stricture [4].
In conventional open total gastrectomy, the most commonly performed technique is the standard circular esophagojejunostomy [5]. However, intracorporeal circular esophagojejunostomy remains technically demanding because of difficulties in inserting the anvil in the esophagus. Although several authors have developed alternative procedures to simplify this technique [4,6,7,8,9,10], they are complicated and have not been widely accepted.
We performed a laparoscopic hand-sewn purse-string suture and ligation to fix the anvil. First, 3/4 of the esophageal wall was incised and a hand-sewn purse-string suture was laparoscopically paced. Next, the anvil was fixed by ligation and the ligated thread was turned through the remnant of the posterior wall of the esophagus. Finally, the turned thread was ligated again to confirm reinforcement of the fixation.
The present study aimed to introduce our novel procedure and evaluate surgical outcomes. Additionally, we compared the outcomes of our technique with those by other methods.
MATERIALS AND METHODS
This was a single-center, retrospective study. From April 2011 to May 2018, we recruited 202 consecutive patients with carcinoma or benign disease who underwent intracorporeal circular esophagojejunostomy in laparoscopy-assisted total gastrectomy with Roux-en-Y reconstruction (LATG-RY: 166 cases) or laparoscopy-assisted proximal gastrectomy with jejunal interposition (LAPG-JI: 36 cases) at the Ogaki Municipal Hospital, Gifu, Japan. This study was approved by the Ethics Review Board of Ogaki Municipal Hospital. The subjects gave informed consent, and patient anonymity was preserved.
All the laparoscopy-assisted gastrectomies were performed in patients <80 years with an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. The study excluded patients with unstable angina or myocardial infarction, severe respiratory disease, and a history of previous upper abdominal surgery. An LATG was indicated for tumors with cT1, cN0 (or recently, due to the improved skill, cT1, 2, or 3 without esophageal invasion and lymph node metastasis confined to the perigastric nodes), according to the Japanese Classification of Gastric Carcinoma, 3rd English edition [11]. As previously described [12], an LAPG was indicated for tumors with cT1, cN0 if the distal half of the stomach could be preserved. If the distal half of the stomach could not be preserved, an LATG was performed.
The data on patient characteristics, operative details, postoperative course, and pathological parameters were extracted from the medical records. The tumors were classified according to the Japanese Classification of Gastric Carcinoma, 3rd English edition [11]. The postoperative complications, including all major and minor complications, were graded according to the Clavien–Dindo classification [13].
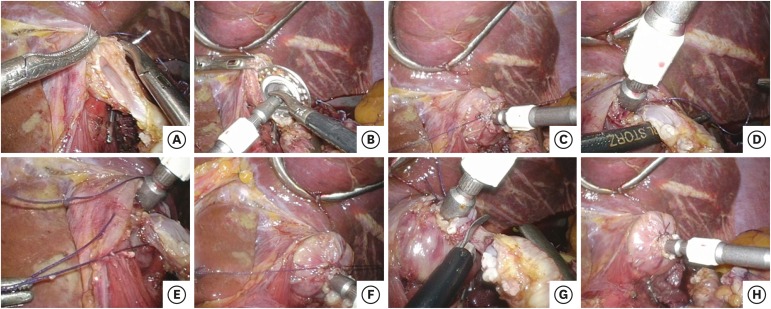
Operative procedure
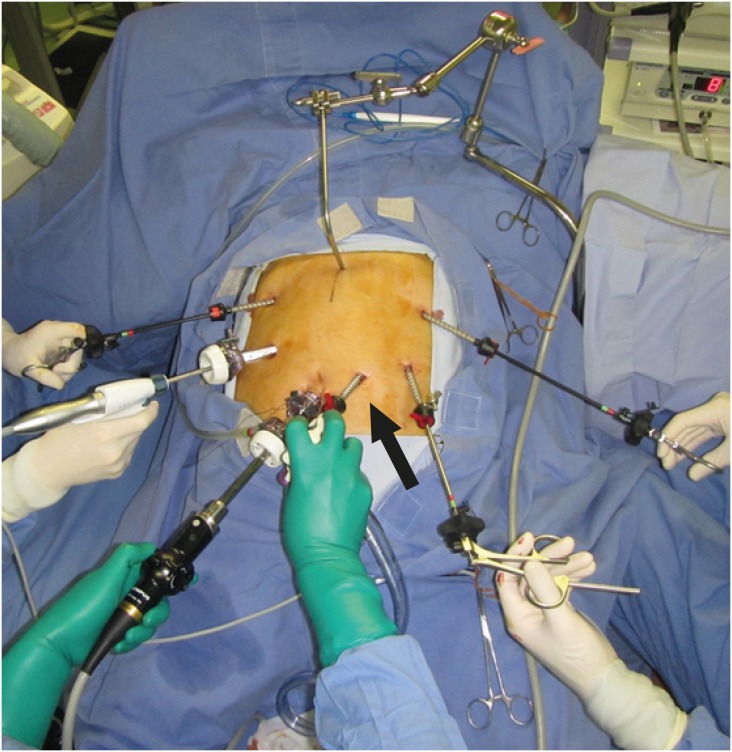
First, the patient was placed in a modified lithotomy position, and using the open method, a flexible laparoscope (Olympus Medical Systems Corp., Tokyo, Japan) was inserted below an umbilical incision. Next, 5 ports were created and a Nathanson liver retractor for liver lift was inserted under laparoscopic vision (Fig. 1) as previously described [14]. After complete exposure of the abdominal esophagus, the anvil of a 25 mm (diameter) circular stapler (Premium Plus CEEA; Medtronic, Cincinnati, OH, USA) was introduced into the abdominal cavity below the umbilical incision. The tip of the anvil was tied with a 2-0 silk thread and a detachable bowel clamp (Endo intestinal clip; Aesculap, Tuttlingen, Germany) was placed at the esophagogastric junction. The esophageal wall was then incised from the right side with a laparoscopic ultrasonic coagulating shear (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA) but was not severed completely; one-fourth of the posterior wall was left intact. A needle holder and Kelly forceps were introduced into the abdominal cavity through bilateral subcostal ports. A hand-sewn purse-string suture was placed using a 20 cm, 3-0 VICRYL (Ethicon; Johnson & Johnson, New Brunswick, NJ, USA) along the cut end of the esophagus with a full-thickness stitch, from the outside-in and inside-out (Fig. 2A). The suture was placed in a counterclockwise direction starting from the left of the esophageal stump to encircle it. Normally, the purse-string suture required approximately 4 stitches. After the purse-string suture was complete, the anterior wall of the esophagus was grasped by bowel forceps held by the operator in his left hand, and the anvil rim was grasped by a second bowel forceps, held by the laparoscopist in his right hand. Then, the anvil rim was introduced into the esophageal lumen by sliding it along the posterior wall of the esophagus (Fig. 2B); the direction of the anvil was changed by towing the thread at the tip of the anvil by the Kelly forceps held with the operator's right hand. After the anvil was positioned correctly, the suture was ligated and the anvil was fixed in its proper position (Fig. 2C). Then, the ligated thread was turned through the remnant posterior wall of the esophagus (Fig. 2D and E). The turned thread was ligated again to confirm the reinforcement of the fixation (Fig. 2F). Finally, the remnant esophageal wall was incised (Fig. 2G), and the fixation of the anvil was completed (Fig. 2H).
Fig. 1. Trocar placement. Infra-umbilical incision sites (12 mm) for the scope; right upper port (5 mm) for the instruments in the left hand of the operator; left upper port (5 mm) for the instruments in the right hand of the assistant; right lower port (12 mm) for the instruments in the right hand of the operator; and left lower port (5 mm) for the instruments in the left hand of the assistant. An aspiration tube was introduced through the 5 mm port on the right side of the umbilical port (5 mm) (arrow) for the aspirating tube in the right hand of the scopist.
Fig. 2. Anvil fixation technique. (A) After incising 3/4 of the esophageal wall, a laparoscopic hand-sewn purse-string suturing was performed. (B) An anvil rim was introduced into the esophageal lumen by sliding on the posterior wall of the esophagus. (C) The purse-string suturing was ligated. (D) Kelly forceps were passed through the posterior wall of the esophagus to grasp the ligated thread. (E) The ligated thread was turned through the posterior wall of the esophagus. (F) The turned thread was ligated again. (G) The remnant esophageal wall was incised. (H) The anvil fixation was completed.
A Nelaton catheter (Terumo Medical Products, Hangzhou, China) was inserted through the jejunum approximately 20 cm distal to the Treitz ligament to be delivered in an antecolic or retrocolic fashion, and a 4 cm longitudinal minilaparotomy incision was made between the epigastrium and umbilicus. When it was difficult to perform extracorporeal procedures safely in obese patients, the minilaparotomy incision was sometimes enlarged. The minilaparotomy wound was retracted and protected using a laparotomy wound retractor (Alexis Wound Retractor; Applied Medical, CA, USA), and the stomach was delivered through the minilaparotomy. In an LAPG-JI, the stomach was transected along the planned resection line using a linear stapler (100 mm; Covidien, Mansfield, MA, USA).
The jejunum put through by a Nelaton catheter was brought out through the laparotomy. To extend the jejunal pedicle, the mesentery was divided along the intestine under direct vision, and the jejunum was sacrificed. In all the cases, we checked to ensure that the jejunal Roux limb had appropriate circulation. A circular stapler was inserted into the jejunal limb, and the jejunum was tied to the instrument with a rubber band to prevent slipping of the jejunum from the circular stapler during the intracorporeal procedure. Next, the body of the circular stapler was introduced into the abdominal cavity, and the pneumoperitoneum was established by a sealing-off minilaparotomy employing a surgical glove attached to the circular stapler. A flexible laparoscope was introduced via the right lower abdominal port to obtain a good operating view for the intracorporeal anastomosis. The circular stapler was combined with the anvil under laparoscopic vision, and after the anastomosis, the circular stapler was withdrawn. Finally, the jejunal stump was closed with a 60 mm endoscopic linear stapler (Ethicon Endo-Surgery Inc.). The anastomosis was checked, and the esophagojejunostomy site was reinforced it was macroscopically brittle under laparoscopy or if the formation of resected rings after circular esophagojejunostomy was incomplete (Supplementary Video 1).
In an LATG-RY, the esophagojejunostomy was performed after the jejunojejunostomy. The jejunojejunostomy was performed via a minilaparotomy in a side-to-end fashion using the hand-sewn Gambee method to create a 45 cm-long Roux limb.
In an LAPG-JI, the esophagojejunostomy was performed before the other anastomoses. The jejunogastrostomy was performed via a minilaparotomy in a side-to-end fashion, using the hand-sewn Gambee method, 15 cm from the esophagojejunostomy site. The anal side of the jejunal interposition was closed using an endoscopic linear stapler 2 cm from the jejunogastrostomy site, and the mesentery was divided along the intestine, sacrificing a 10-cm length of jejunum. The jejunojejunostomy was performed via a minilaparotomy in an end-to-end fashion using the hand-sewn Gambee method.
A silicon drainage tube was placed around the esophagojejunal anastomosis.
In each patient, the esophagojejunostomy was performed by either an expert in laparoscopy surgery (Y.K., A.M., or Y.T.) or a trainee familiar with intracorporeal suturing and operating under the supervision of an expert.
RESULTS
Table 1 lists the characteristics of the patients and tumors. All the patients who underwent an LATG had carcinoma, except for 2 who had benign tumors. One patient aged >81 years was included in this study. Although the inclusion criteria in our institution were patients less than 80 years old, this patient had hoped strongly that she could undergo laparoscopic surgery. The surgical outcomes are summarized in Table 2. Esophageal injury during the anastomotic procedures occurred in 2 patients during LATG. We needed to convert the operation to open surgery because the esophageal wall was withdrawn into the mediastinum, and the hand-sewn purse-string suturing was impossible laparoscopically. The purse-string suture time (from the insertion of 3-0 VICRYL into the esophageal wall to completion) was 6.4 min, and 63 patients needed additional reinforcement at the esophagojejunostomy site.
Table 1. Characteristics of patients and tumors.
| Characteristics | Total (n=202) | LATG (n=166) | LAPG (n=36) | |
|---|---|---|---|---|
| Age (yr) | 65.4 (33–81) | 65.0 (33–81) | 67.6 (41–80) | |
| Sex (male/female) | 145/57 | 118/48 | 27/9 | |
| BMI (kg/m2) | 23.0 (16.5–36.9) | 23.0 (16.5–36.9) | 23.0 (18.6–29.5) | |
| Comorbidity | 118 (58) | 97 (58) | 21 (58) | |
| Disease (cancer/others) | 200/2 | 166/0 | 34/2 | |
| pT | ||||
| T1 | 111 (56) | 83 (50) | 28 (82) | |
| T2 | 34 (17) | 30 (18) | 4 (12) | |
| T3 | 25 (13) | 24 (14) | 1 (2.9) | |
| T4 | 30 (15) | 29 (17) | 1 (2.9) | |
| pN | ||||
| N0 | 133 (67) | 103 (62) | 30 (88) | |
| N1 | 30 (15) | 28 (17) | 2 (5.9) | |
| N2 | 17 (8.5) | 15 (9.0) | 2 (5.9) | |
| N3 | 20 (10) | 20 (12) | 0 | |
| Stage | ||||
| IA | 101 (51) | 74 (45) | 27 (79) | |
| IB | 23 (12) | 21 (13) | 2 (5.9) | |
| IIA | 20 (10) | 18 (11) | 2 (5.9) | |
| IIB | 19 (9.5) | 16 (9.7) | 3 (8.8) | |
| IIIA | 15 (7.5) | 15 (9.0) | 0 | |
| IIIB | 11 (5.5) | 11 (6.6) | 0 | |
| IIIC | 11 (5.5) | 11 (6.6) | 0 | |
Data are shown as number of patients (%) or mean (range).
LATG = laparoscopy assisted total gastrectomy; LAPG = laparoscopy assisted proximal gastrectomy; BMI = body mass index.
Table 2. Surgical outcomes.
| Outcomes | Total (n=202) | ||
|---|---|---|---|
| Operation time (min) | 200.3 (117–377) | ||
| Blood loss (mL) | 53.2 (1–500) | ||
| No. of harvested lymph nodes | 30.8 (4–107) | ||
| Purse-string suture time (min) | 6.4 (2–37) | ||
| Conversion to open surgery | 2 (1.0) | ||
| Overall complications* | 52 (25.7) | ||
| Grade II | 7 | ||
| Grade IIIa | 24 | ||
| Grade IIIb | 20 | ||
| Grade IV | 1 | ||
| Complications at esophagojejunostomy site* | 16 (7.9) | ||
| Anastomotic leakage | 4 (2.0) | ||
| Grade IIIa | 3 | ||
| Grade IVa | 1 | ||
| Anastomotic stricture | 12 (5.9) | ||
| Grade IIIa | 12 | ||
| Mortality | 0 (0) | ||
| Postoperative hospital stays (day) | 15.6 (10–104) | ||
| Observational period (mo) | 16.7 (1–85.0) | ||
Data are shown as number of patients (%) or mean (range).
*Complications grade II and higher according to the Clavien–Dindo classification.
The overall incidence of postoperative complications (≥grade II) was 26%, and the incidence of anastomotic complications at the esophagojejunostomy site was 8.0%. Anastomotic leakage at the esophagojejunostomy site occurred in 4 patients (2.0%). Among them, 1 patient developed a grade IIIa pancreatic fistula followed by a secondary anastomotic leakage, and 1 patient required additional surgical procedures. Anastomotic strictures at the esophagojejunostomy site occurred in 12 patients (6.0%). All of them were successfully treated by endoscopic balloon dilatation. No anastomotic bleeding occurred. The most frequent complications, excluding the anastomotic complications at the esophagojejunostomy sites, were bowel obstruction (5.5%), followed by pancreatic fistula (6%), and intra-abdominal abscess (2%). Reoperations were required in 11 patients (5.5%). The causes of reoperation were pancreatic fistula (1 patient), mediastinitis due to anastomotic leakage (1 patient), and bowel obstruction (9 patients). There was no mortality.
With respect to the materials and devices for anvil fixation, we needed only 1 absorbable thread and did not need specialized devices.
DISCUSSION
A circular stapler allows an esophagojejunostomy to be executed in a stable and safe manner during a conventional open procedure. However, such a procedure under laparoscopic vision is considered to be extremely difficult or impossible because of technical difficulties, especially with anvil insertion into the esophagus and proper placement of the purse-string sutures at the esophageal stump. To overcome this problem, methods for fixation of the anvil into the esophagus that eliminates the purse-string suture [4,6,8,15,16,17,18] were developed, and a specialized device for purse-string suturing, such as the Endostitch semiautomatic suturing device (Covidien Ltd., Dublin, Ireland) [19] or the Endo-PSI(II) [7] have been used. These procedures still appear to be complicated and have not been widely accepted. The transorally placed anvil technique using the OrVil (Covidien Ltd.) system [4] carries the possible risk of pharyngeal or esophageal injury at the level of the tracheal bifurcation resulting from the passage of the anvil head. Additionally, the efficacy of using linear staplers to construct esophagojejunostomies has increasingly been recognized in the field of laparoscopic surgery [9,10]. Linear staplers are easy to use and can be handled through 12 mm trocars. However, they need longer than usual margins of delaminated esophageal areas towards the mediastinum to secure the distance for anastomosis. This manipulation carries the potential risk of subsequent mediastinitis if leakage occurs.
We performed a laparoscopic hand-sewn purse-string suturing to fix the anvil followed meticulously by circular esophagojejunostomy. This method did not require the use of specialized devices to perform the anastomosis and was very similar to the technique used in conventional open surgery. In our procedures, a good operative field around the esophagus and moderate tension were provided by towing of the stomach by the assistant because the esophagus was not incised to the entire circumference. This technique also avoided the retreat of the esophageal stump into the mediastinum. This surgical field expansion enabled us to perform the laparoscopic hand-sewn purse-string sutures more easily. After the anvil was first fixed by ligation, the ligated thread was turned through the remnant posterior wall of the esophagus. The turned thread was ligated again for anvil fixation. Even if the first ligation seemed insufficient for anvil fixation, an additional ligation, including the remnant posterior wall, could be placed for reinforcement, which effectively secured the ligation. We believe that this ligation plays the same role as an Endoloop ligature (Ethicon Endo-Surgery Inc., Cornelia, GA, USA) [20].
Herein, we summarize the surgical outcomes of various methods for anvil fixation for circular esophagojejunostomy, including more than 30 cases (Table 3) [15,16,17,18,19,21,22,23,24,25,26]. To date, our study is the largest on this subject (n=200). Wada et al. [19] performed the hand-sewn purse-string suturing using the Endostitch and used an Endoloop for reinforcement. Lee et al. [21] and Liu et al. [22] used the Endo-PSI(II). For the hand-sewn purse-string suturing method, we summarized 4 reports, including our study [24,25]. The purse-string suturing time was 6.4 minutes in our study and 8.9 minutes in a study by Kim et al. [24]. Although the reconstruction approach and surgical method following resection were somewhat different, our mean operation time was 200.3 minutes, which was less than that for the other reports. The decrease in operation time might be partially due to the port setting; an aspirating tube was introduced through the 5 mm port on the left side of the umbilicus and manipulated by the right hand of the scopist to generate an auxiliary expanded field of view and to conduct lavage and aspiration to control the bleeding. Postoperatively, anastomotic leakage at the esophagojejunostomy site occurred in 4 patients (2.0%). This incidence seems relatively low when compared with other reports. With regard to anastomotic stenosis at the esophagojejunostomy site, our incidence (6%) seems relatively high when compared with other reports. A review by Umemura et al. [26] which compared esophagojejunostomy procedures found that the use of circular staplers was significantly associated with higher incidences of stenosis (8.3%) when compared with the use of linear staplers (1.8%). However, the first study to use the propensity score-matching, by Kyogoku et al. [27], compared the complication rates of esophagojejunostomies performed using a linear and circular stapler; the rate of stenosis did not differ (9% vs. 8%, P=0.753, respectively). The cause of anastomotic stenosis when using circular staplers is unknown; however, some authors have reported that the risk factors associated with this complication include using circular staplers with a diameter of 21 mm, female patients, double-staple technique anastomosis, and long-term postoperative fasting [27,28]. In our method, we used a 25 mm diameter circular stapler and the circular esophagojejunostomy was generally completed by a single-stapling technique. Kosuga et al. [29] reported that the use of a single staple technique for intracorporeal circular esophagojejunostomy could reduce anastomotic stenosis after laparoscopic total gastrectomy. However, the rate of stenosis was 6.2%, which was similar to that in the present study (6.0%). Katai et al. [30] reported that the tension in the jejunum may cause stenosis. It is more difficult to feel the degree of traction when pulling the stump of the esophagus to dock an anvil and circular stapler in laparoscopic surgery than in an open surgery. We also assumed that this can be a problem if too much tension is inadvertently applied. In the early phase of our method, there was strong tension at the esophagojejunostomy site. To relieve the tension of the esophagojejunostomy, the jejunum sacrificed was longer than that removed previously (20→30 cm), and we noted the extension of the jejunal pedicle. The frequency of anastomotic strictures decreased (unpublished data). Our results indicate that although hand-sewn purse-string suturing is considered difficult to perform, it is not very challenging and has become widely used in many procedures.
Table 3. Literature review of anvil fixation technique for circular esophagojejunostomy.
| Author | Year | No. | Method | Operation time (min) | Blood loss (mL) | Leakage (%) | Stenosis (%) | Observation period (mo) |
|---|---|---|---|---|---|---|---|---|
| Wada et al. [19] | 2014 | 100 | Endostich (Endoloop) | 249 | 182 | 5.0 | - | - |
| Lee et al. [21] | 2013 | 99 | Endo-PSI | 250 | 215 | 4.2 | 2.5 | 38.2 |
| Liu et al. [22] | 2017 | 41 | Endo-PSI | 245 | - | 0 | 0 | - |
| Kunisaki et al. [15] | 2011 | 30 | OrVil (LS) | 209.8 | 111 | 3.3 | - | - |
| Ito et al. [17] | 2014 | 117 | OrVil (LS) | 243 | 79 | 1.7 | 1.7 | - |
| Kawamura et al. [18] | 2017 | 49 | OrVil (LS) | 259.3 | 53.3 | 4.1 | 4.1 | - |
| Sugiyama et al. [23] | 2017 | 68 | Various methods* | 380.2 | 163.6 | 9.0 | - | - |
| Nunobe et al. [16] | 2011 | 41 | Modified lift-up method (LS) | 298.6 | 85.9 | 4.9 | 7.3 | - |
| Kim et al. [24] | 2013 | 36 | Handsewn (purse-string, 6 stiches) | 227.1 | 77.1 | 0 | - | 13.2 |
| Du et al. [25] | 2014 | 52 | Handsewn (over and over) | 297.1 | 291.5 | 0 | 0 | 17 |
| Kosuga et al. [29] | 2015 | 65 | Handsewn | 307.4 | 111.1 | 3.1 | 6.2 | - |
| Present study | 2018 | 200 | Handsewn (purse-string, 4 stitches) | 200.3 | 53.2 | 2.0 | 6.0 | 36 |
LS = linear stapler.
*OrVil (LS), modified lift-up method (LS), or Handsewn purse-string.
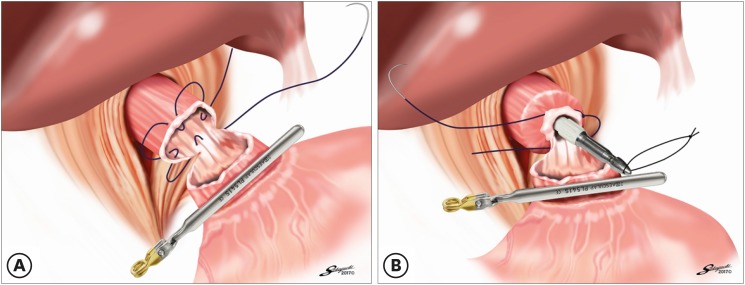
We believe that 4 factors that contribute to the success of an anastomosis. First, a good operative field around the esophagus is secured by towing the stomach. Second, the thread was near the stump of the esophagus so the excessive tissues did not remain around the ligated portion. Third, to reduce the spreading of the esophageal wall after the first ligation, the stitch width inside the esophagus was small and that on the outside was large. If the inner stitch width was large and that on the outside was small, the esophageal wall may spread out of the ligature (Supplementary Fig. 1). Fourth, after ligation, the ligated thread is turned through the remnant posterior wall of the esophagus, and the thread is ligated again to confirm reinforcement of the fixation (Fig. 3).
Fig. 3. The schema of purse-string suturing for anvil fixation into the esophagus. (A) After incising 3/4 of the esophageal wall, a hand-sewn purse-string suturing was performed. (B) After ligation, the ligated thread was turned through the remnant posterior wall of the esophagus.
This study had some limitations. First, patients >81 years of age or those with severe comorbidities were excluded from this procedure. These patients were expected to exhibit brittleness throughout the body, including the esophagus. Second, the influence of the learning level or technical maturation of the surgeons could not be excluded. Although most laparoscopy surgeons with basic skills in laparoscopy suturing could perform this procedure under expert supervision, the operation time, including the hand-sewn purse-string suturing time, and morbidity could vary depending on the surgeon. Third, this was a retrospective study at a single institution. However, this study had the largest sample size (n=200) for reports on surgical outcomes of circular esophagojejunostomy.
In conclusion, our method presented in this study is simple and safe. Additionally, our procedure did not require specialized materials or devices. This method might help LATG-RY and LAPG-JI become standard surgical options for the treatment of patients with gastric cancer.
Footnotes
- Conceptualization: T.Y.
- Data curation: M.A., F.Y., T.T., U.M.
- Formal analysis: K.Y., M.A., F.Y., T.T., U.M.
- Investigation: K.Y., M.A., F.Y., T.T., U.M.
- Writing - original draft: T.Y.
- Writing - review & editing: K.Y., M.A., F.Y., T.T., U.M.
Conflict of Interest: No potential conflict of interest relevant to this article was reported. Patient anonymity was preserved.
SUPPLEMENTARY MATERIALS
The schema of knack & pitfalls for hand-sewn purse-string suturing.
Hand-Sewn Purse-String Suturing by Double Ligation Method, followed by Intracorporeal Circular Esophagojejunostomy
References
- 1.Katai H, Sasako M, Fukuda H, Nakamura K, Hiki N, Saka M, et al. Safety and feasibility of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG 0703) Gastric Cancer. 2010;13:238–244. doi: 10.1007/s10120-010-0565-0. [DOI] [PubMed] [Google Scholar]
- 2.Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007;245:68–72. doi: 10.1097/01.sla.0000225364.03133.f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fukunaga T, Hiki N, Kubota T, Nunobe S, Tokunaga M, Nohara K, et al. Oncologic outcomes of laparoscopy-assisted distal gastrectomy for gastric cancer. Ann Surg Oncol. 2013;20:2676–2682. doi: 10.1245/s10434-013-2930-9. [DOI] [PubMed] [Google Scholar]
- 4.Jeong O, Park YK. Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc. 2009;23:2624–2630. doi: 10.1007/s00464-009-0461-z. [DOI] [PubMed] [Google Scholar]
- 5.Fujimoto S, Takahashi M, Endoh F, Takai M, Kobayashi K, Kiuchi S, et al. Stapled or manual suturing in esophagojejunostomy after total gastrectomy: a comparison of outcome in 379 patients. Am J Surg. 1991;162:256–259. doi: 10.1016/0002-9610(91)90081-n. [DOI] [PubMed] [Google Scholar]
- 6.Hiki N, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, Ohyama S, et al. Laparoscopic esophagogastric circular stapled anastomosis: a modified technique to protect the esophagus. Gastric Cancer. 2007;10:181–186. doi: 10.1007/s10120-007-0433-8. [DOI] [PubMed] [Google Scholar]
- 7.Usui S, Nagai K, Hiranuma S, Takiguchi N, Matsumoto A, Sanada K. Laparoscopy-assisted esophagoenteral anastomosis using endoscopic purse-string suture instrument “Endo-PSI (II)” and circular stapler. Gastric Cancer. 2008;11:233–237. doi: 10.1007/s10120-008-0481-8. [DOI] [PubMed] [Google Scholar]
- 8.Omori T, Oyama T, Mizutani S, Tori M, Nakajima K, Akamatsu H, et al. A simple and safe technique for esophagojejunostomy using the hemidouble stapling technique in laparoscopy-assisted total gastrectomy. Am J Surg. 2009;197:e13–e17. doi: 10.1016/j.amjsurg.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 9.Okabe H, Obama K, Tanaka E, Nomura A, Kawamura J, Nagayama S, et al. Intracorporeal esophagojejunal anastomosis after laparoscopic total gastrectomy for patients with gastric cancer. Surg Endosc. 2009;23:2167–2171. doi: 10.1007/s00464-008-9987-8. [DOI] [PubMed] [Google Scholar]
- 10.Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, et al. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg. 2010;211:e25–e29. doi: 10.1016/j.jamcollsurg.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 12.Takayama Y, Kaneoka Y, Maeda A, Fukami Y, Onoe S. Comparison of outcomes of laparoscopy-assisted and open proximal gastrectomy with jejunal interposition for early gastric cancer in the upper third of the stomach: a retrospective observational study. Asian J Endosc Surg. 2018;11:329–336. doi: 10.1111/ases.12469. [DOI] [PubMed] [Google Scholar]
- 13.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takayama Y, Kaneoka Y, Maeda A, Fukami Y, Onoe S. Extracorporeal hand-sewn anastomosis through a minilaparotomy in laparoscopic distal gastrectomy. J Laparoendosc Adv Surg Tech A. 2017;27:726–732. doi: 10.1089/lap.2016.0133. [DOI] [PubMed] [Google Scholar]
- 15.Kunisaki C, Makino H, Oshima T, Fujii S, Kimura J, Takagawa R, et al. Application of the transorally inserted anvil (OrVil) after laparoscopy-assisted total gastrectomy. Surg Endosc. 2011;25:1300–1305. doi: 10.1007/s00464-010-1367-5. [DOI] [PubMed] [Google Scholar]
- 16.Nunobe S, Hiki N, Tanimura S, Kubota T, Kumagai K, Sano T, et al. Three-step esophagojejunal anastomosis with atraumatic anvil insertion technique after laparoscopic total gastrectomy. J Gastrointest Surg. 2011;15:1520–1525. doi: 10.1007/s11605-011-1489-7. [DOI] [PubMed] [Google Scholar]
- 17.Ito H, Inoue H, Odaka N, Satodate H, Onimaru M, Ikeda H, et al. Evaluation of the safety and efficacy of esophagojejunostomy after totally laparoscopic total gastrectomy using a trans-orally inserted anvil: a single-center comparative study. Surg Endosc. 2014;28:1929–1935. doi: 10.1007/s00464-014-3417-x. [DOI] [PubMed] [Google Scholar]
- 18.Kawamura H, Ohno Y, Ichikawa N, Yoshida T, Homma S, Takahashi M, et al. Anastomotic complications after laparoscopic total gastrectomy with esophagojejunostomy constructed by circular stapler (OrVil™) versus linear stapler (overlap method) Surg Endosc. 2017;31:5175–5182. doi: 10.1007/s00464-017-5584-z. [DOI] [PubMed] [Google Scholar]
- 19.Wada N, Kurokawa Y, Takiguchi S, Takahashi T, Yamasaki M, Miyata H, et al. Feasibility of laparoscopy-assisted total gastrectomy in patients with clinical stage I gastric cancer. Gastric Cancer. 2014;17:137–140. doi: 10.1007/s10120-013-0235-0. [DOI] [PubMed] [Google Scholar]
- 20.Kinoshita T, Oshiro T, Ito K, Shibasaki H, Okazumi S, Katoh R. Intracorporeal circular-stapled esophagojejunostomy using hand-sewn purse-string suture after laparoscopic total gastrectomy. Surg Endosc. 2010;24:2908–2912. doi: 10.1007/s00464-010-1041-y. [DOI] [PubMed] [Google Scholar]
- 21.Lee MS, Lee JH, Park DJ, Lee HJ, Kim HH, Yang HK. Comparison of short- and long-term outcomes of laparoscopic-assisted total gastrectomy and open total gastrectomy in gastric cancer patients. Surg Endosc. 2013;27:2598–2605. doi: 10.1007/s00464-013-2796-8. [DOI] [PubMed] [Google Scholar]
- 22.Liu W, Guo Y, Qiu Z, Niu D, Zhang J. Intracorporeal circular stapled esophagojejunostomy using conventional purse-string suture instrument after laparoscopic total gastrectomy. J Laparoendosc Adv Surg Tech A. 2017;27:1299–1304. doi: 10.1089/lap.2016.0675. [DOI] [PubMed] [Google Scholar]
- 23.Sugiyama M, Oki E, Ogaki K, Morita M, Sakaguchi Y, Koga S, et al. Clinical outcomes of esophagojejunostomy in totally laparoscopic total gastrectomy: a multicenter study. Surg Laparosc Endosc Percutan Tech. 2017;27:e87–e91. doi: 10.1097/SLE.0000000000000435. [DOI] [PubMed] [Google Scholar]
- 24.Kim HI, Cho I, Jang DS, Hyung WJ. Intracorporeal esophagojejunostomy using a circular stapler with a new purse-string suture technique during laparoscopic total gastrectomy. J Am Coll Surg. 2013;216:e11–e16. doi: 10.1016/j.jamcollsurg.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 25.Du J, Shuang J, Li J, Li J, Hua J. Intracorporeal circular-stapled esophagojejunostomy after laparoscopic total gastrectomy: a novel self-pulling and holding purse-string suture technique. J Am Coll Surg. 2014;218:e67–e72. doi: 10.1016/j.jamcollsurg.2013.11.023. [DOI] [PubMed] [Google Scholar]
- 26.Umemura A, Koeda K, Sasaki A, Fujiwara H, Kimura Y, Iwaya T, et al. Totally laparoscopic total gastrectomy for gastric cancer: literature review and comparison of the procedure of esophagojejunostomy. Asian J Surg. 2015;38:102–112. doi: 10.1016/j.asjsur.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Kyogoku N, Ebihara Y, Shichinohe T, Nakamura F, Murakawa K, Morita T, et al. Circular versus linear stapling in esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer: a propensity score-matched study. Langenbecks Arch Surg. 2018;403:463–471. doi: 10.1007/s00423-018-1678-x. [DOI] [PubMed] [Google Scholar]
- 28.Zuiki T, Hosoya Y, Kaneda Y, Kurashina K, Saito S, Ui T, et al. Stenosis after use of the double-stapling technique for reconstruction after laparoscopy-assisted total gastrectomy. Surg Endosc. 2013;27:3683–3689. doi: 10.1007/s00464-013-2945-0. [DOI] [PubMed] [Google Scholar]
- 29.Kosuga T, Hiki N, Nunobe S, Ohashi M, Kubota T, Kamiya S, et al. Does the single-stapling technique for circular-stapled esophagojejunostomy reduce anastomotic complications after laparoscopic total gastrectomy? Ann Surg Oncol. 2015;22:3606–3612. doi: 10.1245/s10434-015-4417-3. [DOI] [PubMed] [Google Scholar]
- 30.Katai H, Morita S, Saka M, Taniguchi H, Fukagawa T. Long-term outcome after proximal gastrectomy with jejunal interposition for suspected early cancer in the upper third of the stomach. Br J Surg. 2010;97:558–562. doi: 10.1002/bjs.6944. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The schema of knack & pitfalls for hand-sewn purse-string suturing.
Hand-Sewn Purse-String Suturing by Double Ligation Method, followed by Intracorporeal Circular Esophagojejunostomy