Abstract
Inflammation can be a causative factor for carcinogenesis or can result from a consequence of cancer progression. Moreover, cancer therapeutic interventions can also induce an inflammatory response. Various inflammatory parameters are used to assess the inflammatory status during cancer treatment. It is important to select the most optimal biomarker among these parameters. Additionally, suitable biomarkers must be examined if there are no known parameters. We briefly reviewed the published literature for the use of inflammatory parameters in the treatment of patients with cancer. Most studies on inflammation evaluated the correlation between host characteristics, effect of interventions, and clinical outcomes. Additionally, the levels of C-reactive protein, albumin, lymphocytes, and platelets were the most commonly used laboratory parameters, either independently or in combination with other laboratory parameters and clinical characteristics. Furthermore, the immune parameters are classically examined using flow cytometry, immunohistochemical staining, and enzyme-linked immunosorbent assay techniques. However, gene expression profiling can aid in assessing the overall peri-interventional immune status. The checklists of guidelines, such as STAndards for Reporting of Diagnostic accuracy and REporting recommendations for tumor MARKer prognostic studies should be considered when designing studies to investigate the inflammatory parameters. Finally, the data should be interpreted after adjusting for clinically important variables, such as age and cancer stage.
Keywords: Inflammation, Cancer, Biomarkers, Immune system, Outcome assessment
INTRODUCTION
Inflammatory response, which promotes the healing of injured tissues, is a physiological defense mechanism against foreign substances. Inflammation can be a causative factor in cancer development or can result from a consequence of cancer progression. Additionally, inflammation can be induced by cancer interventions and/or by the cancer-associated complications and subsequently affect the tumor recurrence, progression, and metastasis [1]. It is important to determine the molecular players involved in the inflammatory response against cancer cells to assess the inflammation status and to devise the best therapeutic strategy [2].
Surgery is an invasive intervention for cancer treatment. Clinicians gather routine clinical and laboratory information perioperatively to predict the surgical outcomes. However, the clinical and laboratory information is sometimes insufficient to assess the inflammation status in patients. Hence, novel parameters must be investigated for a more reliable prediction of surgical outcomes. Currently, various inflammatory and nutritional parameters as well as the body weight-related data are used to evaluate the inflammatory response associated with therapeutic interventions. In a recent study, we compared multiple parameters and demonstrated that simple biomarkers, such as albumin level, body mass index (BMI), and neutrophil count were more effective in predicting surgical outcomes than sophisticated biomarkers, such as the prognostic nutritional index (PNI), nutritional risk index (NRI), and neutrophil-to-lymphocyte ratio (NLR) [3]. The results of the study suggested that low albumin level, high BMI, high neutrophil count are predictors of major complications, operative mortality and unfavorable recurrence-free survival, and unfavorable overall and recurrence-free survival, respectively. These observations indicated that we must reconsider the parameters currently used for determining the surgical outcome of patients. We reviewed the published literature for parameters used to determine inflammatory response in patients with cancer. Further, the parameters were classified to guide researchers to systematically evaluate the inflammatory response in patients.
FACTORS ASSOCIATED WITH INFLAMMATION IN PATIENTS WITH CANCER
We grouped the published studies into three groups (Table 1) [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81]. The first group included studies that identified the characteristics of hosts exhibiting inflammation, the second group included studies that measured the effect of treatment interventions, and the third group included studies that predicted the outcomes of interventions.
Table 1. Studies on inflammatory response parameters in cancer.
| Host | Intervention | Outcomes | ||||
|---|---|---|---|---|---|---|
| Inherence | Behavior | Disease | Surgical | Medical | Prediction | Prognosis |
| Sex [4,5,6] | Immunosuppressive medication [12] | Chronic disease [16] | Open surgery vs MIS [21,22,23,24] | Anesthesia, analgesia [30,31,32] | Morbidity and mortality [56,57,58,59,60,61,62,63] | Recurrence [68,69,70,71,72] |
| Age [7,8] | Nutritional status [13] | Cancer progression [17] | Major vs minor surgery [1,25] | Fast track protocol [33,34,35] | Infection [64,65] | Survival [12,26,73,74,75,76,77,78,79,80,81] |
| Obesity [3,9,10,11] | Smoking [14] | Psychiatric disease [18] | Emergency surgery [26,27] | Transfusion [36,37] | Prediction of neoadjuvant response [66,67] | |
| Exercise [15] | Ischemia [19] | Surgical stress [28,29] | Nutritional support* [38,39,40,41,42,43,44] | |||
| Sepsis [20] | Steroid and other immune modulators [25,45,46,47,48,49,50] | |||||
| Adjuvant/neoadjuvant treatment [51,52,53] | ||||||
| NSAID [54] | ||||||
| Statin [55] | ||||||
MIS = minimally invasive surgery; NSAID = non-steroid anti-inflammatory drug.
*Includes enteral, parenteral, and immune-enhancing nutrition.
Host factors
Among the various factors that affect inflammatory response, the inherent factors, such as sex, age, and obesity are well-known and are the most important host factors. Men and women exhibit differential immune response due to the difference in the number of X chromosomes and variations in sex hormones [4]. Estrogen promotes T helper cell type 2 (Th2) and suppresses T helper cell type 1 (Th1) immune responses, whereas testosterone suppresses the Th2 immune response [5]. The Th1 immune responses are cell-mediated responses that target the intracellular pathogen, whereas Th2 responses are antibody-mediated responses that target the extra-cellular pathogen. The analysis of differential immune response between the genders revealed that women have a lower risk of microbial infections and higher prevalence of autoimmune disease, whereas men have a higher susceptibility to systemic inflammatory response syndrome or infectious complications after surgery [6]. Age is also an important clinical parameter. The body's ability to distinguish between self and non-self cells decreases with age. Hence, decreased number of immune cells and weakened immune function associated with aging increase the susceptibility to malignancies and reactivation of chronic infections among aged individuals. Thus, several studies have evaluated the postoperative outcomes for elderly patients [7,8]. Obesity, which is generally measured by BMI, is associated with impaired immune function [9], inflammation [10], and complications following treatment interventions [11].
Other factors that may affect the inflammatory response and clinical outcomes include behavior- and disease-related characteristics, such as immunosuppressive medication usage [12], nutritional status [13], smoking status [14], exercise habits [15], presence of chronic disease [16], cancer stage [17], psychiatric condition [18], and presence of ischemia [19] or sepsis [20].
Intervention factors
Among the various therapeutic interventions, surgery is the most invasive intervention. The incision size or resection extent is directly correlated with the degree of surgical trauma. Hence, several studies are focused on developing novel surgical techniques that are associated with less surgical trauma and exhibit similar therapeutic efficacy. In the last few decades, comparative efficacy of open and laparoscopic surgery has been well studied [21]. The advantages of laparoscopic surgery include decreased surgical trauma and attenuated inflammatory response. The Th1/Th2 ratio is modulated to favor a decreased inflammatory response and decreased concentration of acute phase markers [22,23]. Recently, minimally invasive surgical procedures, such as reduced port laparoscopy and robotic surgery have been used to reduce the inflammatory response associated with open surgery [23,24].
The inflammatory response resulting from surgical intervention correlates with surgical trauma and is easy to predict. However, inflammatory responses resulting from other medical interventions are diverse and difficult to predict. Anesthetic techniques affect not only postoperative recovery but can also potentially impair the survival outcomes due to the suppression of inflammation [30,82,83]. Regional or epidural anesthesia is reported to be a factor that mitigates surgery-induced immunosuppression [31,32]. Moreover, peri-operative management [33,34,35], transfusion strategy [36,37], and pain management [32] are reported to considerably influence the inflammatory response.
Nutritional supplements, such as glutamine and arginine are used to enhance the immune response (referred to as immunonutrition) [38,39], while probiotics are used for perioperative modulation of the gut microbiome [40,41]. Nutrional supplements and probiotics have been extensively studied to determine their effect on the immune response and clinical outcomes. However, it is difficult to evaluate the effect of nutritional interventions on well-nourished patients. The nutritional interventions are most effective in patients exhibiting malnourishment [84,85].
Finally, steroids are one of the most well studied drugs that are used to attenuate the immune response. Preoperative steroid administration is reported to markedly decrease systemic inflammatory cytokine release and improve the postoperative clinical course of patients, without adverse effects on immunity [45,46]. The immune modulators, such as dendritic cell-activated cytokine-induced killer cells [47], interleukin (IL)-2 [48], neutrophil elastase inhibitors [49], protease inhibitors [50], and recombinant human granulocyte colony-stimulating factor [25] have been studied to determine their effectiveness during the peri-intervention period.
Outcomes
The most classical clinical outcomes measured following therapeutic interventions, such as surgery, chemotherapy, or radiotherapy are complication rates and recovery time in short-term [61], and survival without unfavorable events in long-term [71]. Additionally, some inflammation parameters including tumor-infiltrating lymphocytes or composite scores can be used for predicting the inflammation response following neoadjuvant chemo-radiation therapy [64,65] or for anticipating an infection [66] following an intervention.
APPROACHES FOR EVALUATING INFLAMMATORY PARAMETERS
Laboratory parameters
Historically, laboratory values are used to assess the inflammatory status of the patients (Table 2) [3,17,23,26,34,35,38,39,42,44,50,59,62,66,69,71,73,74,75,76,77,78,79,84,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106]. Laboratory parameters are economical to evaluate, easily measurable, repeatable, and ready to use in daily clinical practice. Among the various laboratory parameters, acute phase protein levels are the most relevant to determine the inflammatory status of patients. The levels of positive acute phase proteins increase, whereas those of negative acute phase proteins decrease during inflammation [107]. C-reactive protein (CRP) and albumin are the most commonly used positive and negative acute phase proteins, respectively. CRP is secreted from the liver and the CRP levels increase upon secretion of IL-6 by macrophages and T-cells. Although meta-analyses have revealed limited diagnostic value of CRP for diagnosing postoperative complications [108,109], CRP level is useful during follow-up as it has a short half-life.
Table 2. Laboratory parameters.
| Parameters | ||
|---|---|---|
| Single value | Combined values | |
| Positive APPs | ||
| CRP [34,39,71,86] | NRS-2002 [3,44,84] | |
| High sensitivity CRP [87,88] | MUST [3] | |
| Erythrocyte sedimentation rate [89] | Skeletal muscle index [90] | |
| Alpha 1-acid glycoprotein levels [91] | NRI [3] | |
| Serum amyloid A levels [92,93] | SIRS criteria [50,94] | |
| Alpha-1-antitrypsin levels [95] | CRP/Albumin ratio [17,75] | |
| Procalcitonin levels [23,62,96] | GPS, modified GPS, hepatic GPS [17,26,66,79] | |
| Fibrinogen levels [88,97] | PNI [69,98] | |
| Complement-C3 and C4 levels [35,44] | Prognostic index [98] | |
| APRI [99] | ||
| Negative APPs | CONUT [78] | |
| Albumin levels [3,100] | Naples prognostic score [73] | |
| Prealbumin levels [38,42] | Canton score [101] | |
| Retinol-binding protein levels [38,95] | PLR [74,102] | |
| Transferrin levels [39,95] | NLR [59,74,77,102] | |
| COP-NLR [76] | ||
| NMLR [103] | ||
| GLR [104] | ||
| LMR [105] | ||
| SII [106] | ||
APP = acute phase protein; CRP = C-reactive protein; NRS = nutritional risk screening; MUST = malnutrition universal screening tool; NRI = nutritional risk index; SIRS = systemic inflammatory response syndrome; GPS = Glasgow prognostic score; PNI = prognostic nutritional index; APRI = aspartate aminotransferase/platelet count ratio index; CONUT = controlling nutritional status; PLR = platelet-to-lymphocyte ratio; NLR = neutrophil-to-lymphocyte ratio; COP-NLR = combination of platelet count and neutrophil-to-lymphocyte ratio; NMLR = neutrophil-monocyte-to-lymphocyte ratio; GLR = granulocyte-to-lymphocyte ratio; LMR = lymphocyte-to-monocyte ratio; SII = systemic immune-inflammation index.
The predominant protein in the blood serum is albumin. Albumin carries water-insoluble molecules necessary for various metabolic processes. Although albumin is reported to be a negative acute phase protein, hypoalbuminemia does not represent an increased inflammatory status in patients [110]. Hence, albumin level is used independently or in combination with other laboratory values to assess the nutritional status in patients [100].
The combination of CRP and albumin has been extensively studied for the prediction of survival [106,111], tumor recurrence [70,71], peri-operative mortality [58], and specific outcomes, such as central venous catheter-related bloodstream infection [66]. The predictive value of CRP and albumin combination is not conclusive due to the heterogeneity in results reported by different studies. However, the CRP and albumin levels are the most sensitive and reliable biomarkers among the various inflammation-based scores [98,111,112,113].
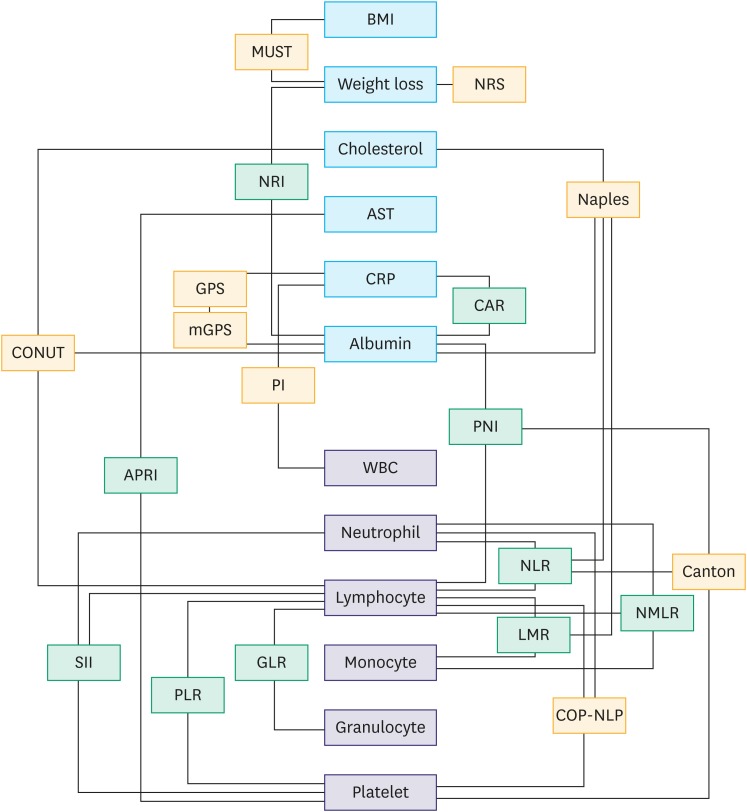
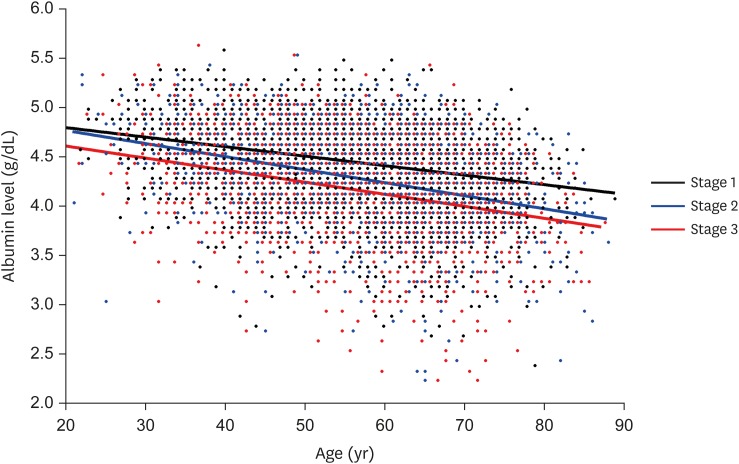
Currently, CRP, albumin, lymphocytes, or platelets are used in combination to predict the surgical outcomes. Fig. 1 shows the relationship among these parameters. However, the use of combinations of these four parameters without accounting for the clinical parameters can be misleading as these 4 parameters are not independent but associated with patient characteristics, such as age and cancer stage. Thus, combined parameters based on albumin may lose their predictive value after adjustment with patient characteristics [3,114]. As shown in Fig. 2, there is a correlation between albumin level, age, and cancer stage [115].
Fig. 1. Relationship among parameters. Parameters with continuous values (Green boxes) and with categorical values (Orange boxes). Detail of values are presented in Appendix 1.
BMI = body mass index; MUST = malnutrition universal screening tool; NRS = nutritional risk screening; NRI = nutritional risk index; AST = aspartate transaminase; CRP = C-reactive protein; GPS = Glasgow prognostic score; CAR = C-reactive protein-to-albumin ratio; CONUT = controlling nutritional status; PI = prognostic index; PNI = prognostic nutritional index; WBC = white blood cell; APRI = aspartate aminotransferase/platelet count ratio index; NLR = neutrophil-to-lymphocyte ratio; NMLR = neutrophil-monocyte-to-lymphocyte ratio; LMR = lymphocyte-to-monocyte ratio; SII = systemic immune-inflammation index; GLR = granulocyte-to-lymphocyte ratio; PLR = platelet-to-lymphocyte ratio; COP-NLR = combination of platelet count and neutrophil-to-lymphocyte ratio.
Fig. 2. Relationship of albumin level with age according to stage. Each point represents age and albumin level of a patient. Linear regression of each stage group shows that mean albumin level at same age decrease as the disease progresses. Dataset from Lee et al. [115].
Immune parameters
Immune cells
Assessment of immune cells and cytokines is necessary to evaluate the immune response in patients (Table 3) [1,3,13,14,18,20,22,25,27,29,30,31,34,35,39,42,43,44,47,50,51,52,53,54,60,63,67,72,79,80,81,85,86,87,88,90,91,93,95,97,103,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132]. The innate immune response is rapid and does not require prior exposure to an antigen. This general, non-specific, and first-line defense system against foreign substances is mediated by the natural killer (NK) cells. In response to injury, macrophages and mast cells are the first host tissue cells that are activated, which subsequently coordinate the immune response. The adaptive immune cells mainly consist of B and T lymphocytes. The analysis of complete blood count (CBC) provides the crude numbers of neutrophils, granulocytes, lymphocytes, and platelets. However, evaluating the lymphocyte subpopulations of dendritic cells and T-cells is more complicated and requires flow cytometric analysis. The T-cells comprise cytotoxic T-cell and helper T-cell subpopulations, which can be further classified as Th1, Th2, Th17, and regulatory T cells. Cancer recurrence can be predicted by phenotyping and functional assay of lymphocytes from the peripheral blood and tumor lysate [68]. If fresh blood is not available, the immune status of tumor tissues can be evaluated by immunohistochemical staining. The advantage of using paraffin-embedded tissue blocks is that the long-term outcome of the treated patients is already known. The tumor microenvironment is assessed by evaluating the lymphocytes [133,134,135], tumor-associated macrophages [72], and myeloid-derived suppressor cells [136].
Table 3. Immune parameters.
| Parameter | ||
|---|---|---|
| Immune cells | Peripheral blood | |
| Lymphocyte counts [22,85] | ||
| Neutrophil counts [3,51,79,116] | ||
| Monocyte counts [103] | ||
| Dendritic cell counts [54,80] | ||
| NK cell counts [117,118] | ||
| T lymphocyte subpopulation counts [42,44,53,81] | ||
| B lymphocyte counts [53,117,118] | ||
| Tissue | ||
| Tumor-infiltrating lymphocyte levels [52,81] | ||
| Tumor-associated macrophage levels [72] | ||
| Mast cell density positive to tryptase [119] | ||
| Other fluid | ||
| Peritoneal fluid: Lymphocyte subsets and HLA-DR expression [120] | ||
| Cytokines | Peripheral blood | |
| TNF-α levels [22,39,50] | ||
| IFN-γ levels [22,53,54] | ||
| Th1/Th2 ratio [30,31,121,122] | ||
| IL-1 levels [1] | ||
| IL-2 levels [53,123] | ||
| IL-4 levels [1,53,123] | ||
| IL-5 levels [123] | ||
| IL-6 levels [22,34,43,50] | ||
| IL-8 levels [18,116] | ||
| IL-9 levels [124] | ||
| IL-10 levels [29,63] | ||
| IL-12 levels [20,63] | ||
| IL-13 levels [53] | ||
| IL-15 levels [27] | ||
| IL-17 levels [30,54] | ||
| IL-18 levels [13] | ||
| Levels of multiple cytokines [47,124] | ||
| TNF-R levels [25,125] | ||
| TNF-R inhibitor levels [125,126] | ||
| IL-2 receptor levels [42] | ||
| IL-1 receptor antagonist levels [25,60,95] | ||
| IL-6 soluble receptor levels [127] | ||
| Adipocytokine leptin levels [93] | ||
| Immunosuppressive acidic protein levels [127] | ||
| Neopterin levels [39] | ||
| Levels of globulins including IgG, IgA, and IgM [35,44,86] | ||
| Proapoptotic protein-soluble Fas levels [126] | ||
| MCP-1 levels [97] | ||
| Calprotectin levels [90] | ||
| Levels of DAMPs (HSP-S100A-HMGB) [128] | ||
| Neutrophil elastase levels [67,88,116] | ||
| Other fluid | ||
| Alveolar lavage: levels of multiple cytokines [129] | ||
| Peritoneal lavage: levels of multiple cytokines [120] | ||
| Gene expression | Peripheral blood | |
| HLA-DR expression on monocytes [1,25,29,34] | ||
| mRNA expression of TLR2-TLR4 [91] | ||
| Expression of histamine receptors [130] | ||
| Other fluid | ||
| Alveolar lavage: RT-PCR for proinflammatory cytokines [14] | ||
| Others | NK activity [13,15,36,43] | |
| Lymphocyte oxidative activity [131] | ||
| Lymphocyte proliferation [25,43] | ||
| Phagocytic capacity [132] | ||
| Skin-prick tests [130] | ||
| Oxidative stress-antioxidant capacity [87] | ||
NK = natural killer; HLA-DR = human leukocyte antigen-DR isotype; TNF = tumor necrosis factor; INF, interferon; Th = T helper; IL = interleukin; Ig = immunoglobulin; MCP-1 = monocyte chemoattractant protein-1; DAMP = damage-associated molecular patterns; TLR = Toll-like receptors; RT-PCR = real-time polymerase chain reaction.
Cytokines
The immune cells communicate with each other through signaling molecules or cell-to-cell communication, which involve toll-like receptors, B and T cell receptors and the complement system [137,138]. However, majority of the immune cells communicate through the secretion of cytokines. Cytokines are a category of cell-signaling proteins that regulate various immunological functions. Various proteins, such as lymphokines (produced by lymphocytes), monokines (produced by monocytes), chemokines (regulate chemotactic activities between cells), interferons (involved in the antiviral activity), and interleukins function as cytokines. Several cytokine classifications were proposed based on the Th1/2 axis [139,140]: receptor and cytokine structures [141], the position of cysteine residues [142], and pro-inflammatory or anti-inflammatory parameters [143].
Among these classifications, the functional classifications (Th1/2) and receptor structures is the most relevant grouping method (Table 4) [144]. The functional classification is widely used in clinical and experimental practice and categorize the cytokines based on their involvement in cellular immune responses (Th1) and antibody-mediated responses (Th2). The Th1 response is the principal immune mechanism underlying cellular immunity. Cell-mediated immune response includes activation of monocytes and cytotoxic T lymphocytes against virus-infected cells, intracellular parasites, intracellular bacteria, and tumors [145]. The critical cytokines involved in type I response are interferon-gamma (IFN-γ) and IL-12. The mechanism underlying humoral immunity involves type II response. Humoral immune response includes the activation of eosinophils, mast cells, and B lymphocyte proliferation and differentiation. The key cytokines involved in mediating type II response are IL-4 and IL-10. Type II response is immunosuppressive and is observed after extensive injury in patients with cancer undergoing surgery. IL-4 and IL-10 inhibit type I response, whereas IFN-γ inhibits type II response. As these 2 response mechanisms may inhibit each other, the ratio of the major molecular players involved in type I and type II responses (the ratio of IFN-γ or IL-12/IL-4 or IL-10) can be useful biomarkers [30,31,121,122,143,145].
Table 4. Representative cytokines of each classification.
| Representative cytokine | Th1/2 | Receptor structure | Example* |
|---|---|---|---|
| IL-2† | Th1 | Type 1, common r-chain† | IL-7,9,15,21 |
| IL-6 | Th1 | Type 1, IL-6 like cytokines | IL-11,30 |
| IL-12 | Th1 | Type 1, IL-12 subfamilies | IL-23, 27, 35 |
| IL-17 | Th1 | Type 1, IL-17R | |
| TNF-α | Th1 | Type 1, TNF | TNF-β |
| IFN-γ | Th1 | Type 2, IFN | |
| IL-8 | Th1 | Chemokine R | |
| IL-3 | Th1 & Th2 | Type 1, common-b-chain | IL-5, GM-CSF |
| IL-4† | Th2 | Type 1, common r-chain† | IL-13 |
| IL-1 | Th2 | Type 1, IG | IL-18, 33, 36, 37, 38 |
| IL-10 | Th2 | Type 2, IL-10 subfamily | IL-19, 20, 22, 24, 26 |
| MCP-1 | Th2 | Chemokine R | |
| TGF-β | Th2 | TGF receptor family |
IL = interleukin; Th = T helper; TNF = tumor necrosis factor-alpha; IFN, interferon; GM-CSF = granulocyte-macrophage colony-stimulating factor; MCP-1 = monocyte chemoattractant protein-1; TGF = transforming growth factor.
*Examples according to receptor structure; may not show the same Th1/2 balance as representative cytokines; †IL-2 and IL-4 share the same receptor structure but show opposite Th1/2 balance.
Gene expression
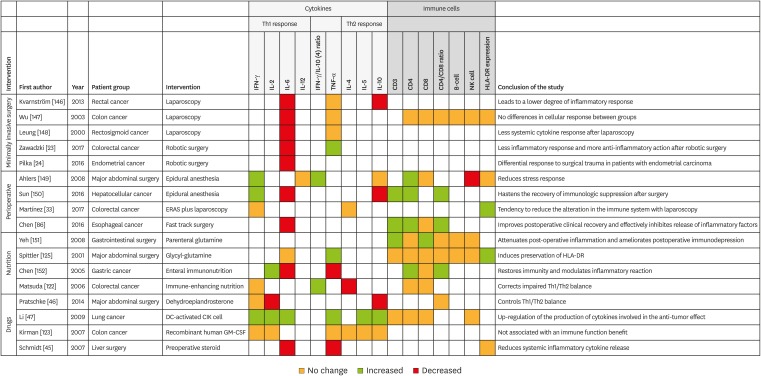
Flow cytometry and enzyme-linked immunosorbent assay are used for classical hypothesis-driven studies. These are confirmatory techniques that are specific for the selected parameters (Fig. 3) [23,24,33,45,46,47,86,122,123,125,146,147,148,149,150,151,152]. However, measuring only selected immune responses does not provide information on the global changes associated with complex immune response. The inflammatory response status can be evaluated using gene expression. A study on patients with colon cancer undergoing surgery demonstrated that the genes associated with antigen presentation, general T-cell receptor signaling, and granzyme-B encoding for NK and CD8+ T-cells are downregulated [153]. Additionally, the study revealed that the genes encoding cytokines (IL-1B, IL-6, tumor necrosis factor [TNF], and IL-10), CRP, growth factor, and matrix metalloproteinase were upregulated [153]. This indicated downregulation of T-cell receptor signaling, antigen presentation, and NK cell activity and promotion of metastases, growth, and angiogenesis. The strength of this high-throughput study enables us to assess the “genomic storm” of peri-operative changes in gene expression. The gene expression changes indicate not only immune system activation but also the inability to maintain homeostasis. Another study demonstrated the downregulation of differentiation/clonal expansion of T cytotoxic cell and T-cell surface markers and up-regulation of IL-18 and IL-10 signaling pathways [154].
Fig. 3. Associations of interventions with response patterns.
INF = interferon; IL = interleukin; TNF = tumor necrosis factor; NK = natural killer; HLA-DR = human leukocyte antigen-DR isotype; ERAS = enhanced recovery after surgery; Th = T helper; DC = dendritic cell; CIK = cytokine-induced killer; GM-CSF = granulocyte-macrophage colony-stimulating factor.
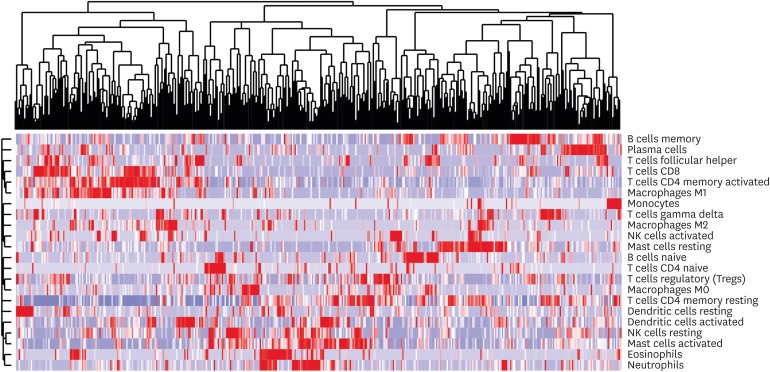
It is intriguing that transcriptomic data from a bulk tumor can be used to predict the status of immune cell infiltration. Fig. 4 illustrates a heatmap of 22 types of immune cell infiltration inferred from The Cancer Genome Atlas stomach adenocarcinoma gene expression cohort [155]. Cell-type identification by estimating relative subsets of RNA transcripts (CIBERSORT) is a deconvolution algorithm that uses a set of reference gene expression values to support the vector regression inference immune cell types in data from mixed cell types of bulk tumor samples [156].
Fig. 4. Unsupervised clustering of inferred immune fraction using leukocyte signature matrix in the cancer genome atlas stomach adenocarcinoma (TCGA-STAD) transcriptomic dataset (n=450). Integrative transcriptomic analysis enables the identification of distinct immune landscapes associated clinical phenotypes using the fraction of infiltrated immune subsets in each sample as well as the evaluation of oncogenic pathway specific to each sample.
Guidelines
Effective data collection is necessary to identify the relevant parameters associated with the inflammatory response. REporting recommendations for tumor MARKer prognostic studies (REMARK) and STAndards for Reporting of Diagnostic accuracy studies (STARD) provide suggested guidelines as checklists to supply relevant information necessary for the design and reporting of prognostic markers and diagnostic accuracy [157,158]. STARD guidelines are focused on the preciseness of a parameter compared to the gold-standard. The prediction of complications based on preoperative or immediate postoperative laboratory values provides a good example of STARD guidelines [108,159]. REMARK guidelines are used to predict the survival of patients undergoing a test or treatment. A preoperative neutrophil-to-lymphocyte ratio predicting long term survival would be an example of application of REMARK guidelines [77]. As REMARK guidelines are related to survival, it is important to assess time-to-event and associated clinical factors such as age, sex, and disease status. These two guidelines share the essential factors of describing a good study and defining other unique requirements. We compared the checklists of STARD and REMARK guidelines to guide good study design and data analysis (Table 5).
Table 5. Guidelines for biomarker studies.
| Structure | Common guidelines | STARD-specific guidelines | REMARK-specific guidelines |
|---|---|---|---|
| Introduction | Background, objective, and hypothesis | ||
| Methods | • Eligibility criteria | • Participant identification methods | • Description of biological material used |
| • Participants chosen for the study | • Rationale for reference standard | • Clinical endpoints examined | |
| • Detailed protocol sufficient to replicate | • List of all candidate variables initially examined | ||
| • Study performer, readers, or assessors blinded to identifying information | |||
| • Data collection methods (retrospective vs prospective) | |||
| • Sample size determination | |||
| • Missing data handling | |||
| • Rationale for cut-offs | |||
| Results | • Study flow | • Time interval between index test and reference standard | • Univariable analyses revealing the correlation between the marker and outcome |
| • Characteristics of patients | • Adverse events due to the index test or the reference standard | • Confidence intervals from an analysis in which the marker and standard prognostic variables are included | |
| • Relation of index test (marker) and reference standard (prognosis) | • Results of further investigations | ||
| • Estimation of accuracy and precision (STARD) or confidence intervals (REMARK) | |||
| Discussion | • Limitations, implications for practice, and future research | • Interpret the results in the context of the pre-specified hypotheses |
STARD = STAndards for Reporting of Diagnostic accuracy studies; REMARK = REporting recommendations for tumor MARKer prognostic studies.
Interpretation of data
A prerequisite for the identification of a novel biomarker is the valid interpretation of data. We suggest that three issues must be elaborated during the data interpretation. First, inherent characteristics of patients, such as age, sex, and disease status, should be adjusted using a multivariate analysis for assessing the value of inflammatory parameters. This is to prevent the misinterpretation of data. The level of albumin, which is required for calculation of PNI, is highly correlated with age and cancer stage, such that the diagnostic value of PNI decreases after adjustment [3,115]. Second, most of the inflammatory parameters exhibit continuous variation. For any regression analysis, it is always preferable to treat continuous parameters as continuous. However, these parameters are converted to categorical values to enter into regression models in most studies. An arbitrary decision for the cut-off values may result in a misinterpretation of data and hinders their routine use in clinical practice. Third, a value could be interpreted differently in the context of the inflammatory response. Skewing Th1/Th2 immune function, proportion of regulatory T-cells among helper T-cells, and a sequential change of parameters following surgery are good examples.
INFLAMMATION AND GASTRIC CANCER
Various aspects of the relationship between inflammation and gastric cancer treatment have also been studied. Microenvironment generated by unresolved inflammation is involved in the pathogenesis of non-cardia gastric cancer [160]. The host factors, such as age, obesity, and nutritional status are reported to be associated with the outcome of gastric cancer treatment [161,162]. Minimally invasive surgery has been widely used and several studies, including randomized trials have demonstrated the higher efficacy of laparoscopic and robot-assisted surgeries compared to open surgery [163,164]. Anesthesia techniques and perioperative nutritional support have enhanced postoperative recovery after the guidelines for gastric cancer surgery were published [165,166]. Laboratory and immune parameters are reported to be a predictor of outcomes in several studies, including our earlier studies [3,101,115].
Inflammation is the common condition that was evaluated in all these studies. The purpose of cancer research should not only include killing cancer cells but also patient care. However, there are limited studies that have comprehensively evaluated the correlation between high-quality clinical parameters, immune cells, and cytokines. We believe that sharing insights of inflammation during the disease process and biomedical literacy of clinicians in molecular, genetic, and immune mechanisms will change the way of providing care to patients with gastric cancer in the future [153,155].
CONCLUSIONS
There has been an increased interest in predicting short- and long-term treatment outcomes. To show a significant difference during the hypothesis test, study aim, selection of parameters, and interpretation of results should be carefully performed, as recommended in this review. Although not discussed here, issues associated with the sources of examined material (peripheral blood, tumor lysate, or tumor draining vein) and timing of examination (pre- or immediate post-interventional) are also important. Selection of when, how, and what to measure during the intervention may critically affect the decisions and clinical outcomes. Thus, peri-interventional inflammatory responses in patients with cancer require further exploration by a clinical oncologist.
Appendix 1
Parameters with continuous values (Green boxes in Fig. 1)
NRI (nutritional risk index): 15.19 × albumin level (g/dL) + 41.7 × (present weight/usual weight)
CAR (C-reactive protein [CRP]-to-albumin ratio): serum CRP level (mg/dL)/serum albumin level (g/dL)
PNI (prognostic nutritional index): 10 × albumin level (g/dL) + (0.005 × lymphocyte count [number/mm3])
SII (systemic immune-inflammation index): (platelet count × neutrophil count)/lymphocyte count
NLR (neutrophil-to-lymphocyte ratio): neutrophil count/lymphocyte count
PLR (platelet-to-lymphocyte ratio): platelet count/lymphocyte count
GLR (granulocyte-to-lymphocyte ratio): granulocyte count/lymphocyte count
LMR (lymphocyte-to-monocyte ratio): lymphocyte count/monocyte count
NMLR (neutrophil-monocyte-to-lymphocyte ratio): (neutrophil count × monocyte count)/lymphocyte count
APRI (aspartate aminotransferase-to-platelet count ratio): Aspartate aminotransferase level (units/L)/platelet count
Parameters with categorical values (Orange boxes in Fig. 1)
NRS (nutritional risk screening 2002):
Summation of points for (1) nutritional status (0, weight loss ≤5% in 3 months; 1, >5% in 3 months; 2, >5% in 2 months; 3, >5% in 1 month), (2) severity of disease (0, normal; 1, hip fracture; 2, major abdominal surgery; 3, head injury and APACHE score ≥10), and (3) age (0, <70 years; 1, ≥70 years)
MUST (malnutrition universal screening tool):
Summation of points for (1) body mass index (BMI) score (0, BMI ≥20 kg/m2; 1, BMI=18.5–20 kg/m2; 2, BMI ≤18.5 kg/m2), (2) weight loss in 3 months (0, ≥5%; 1, 5%–10%; 2, ≥10%), and (3) acute disease effect score (0, normal; 2: no nutritional intake >5 days)
COP-NLR (combination of platelet count and neutrophil-to-lymphocyte ratio): Composite score of platelet count and NLR (Score 0/1/2)
COP-NLR 0: normal platelet count (<300 × 103/mL) or a normal NLR (<3)
COP-NLR 1: elevated platelet count (>300 × 103/mL) or an elevated NLR (>3)
COP-NLR 2: elevated platelet count (>300 × 103/mL) and an elevated NLR (>3)
PI (prognostic index): Composite score of serum CRP and white blood cell (WBC) count (Score 0/1/2)
PI 0: normal CRP levels (<1.0 mg/dL) and normal WBC count (<11 × 109/L)
PI 1: elevated CRP levels (>1.0 mg/dL) or elevated WBC count (>11 × 109/L)
PI 2: elevated CRP levels (>1.0 mg/dL) and elevated WBC count (>11 × 109/L)
GPS (Glasgow prognostic score): Composite score of serum CRP and albumin levels (Score 0/1/2)
GPS 0: Normal albumin (>3.5 g/dL) and normal CRP (<1.0 mg/dL) levels
GPS 1: Low albumin (<3.5 g/dL) or elevated CRP (>1.0 mg/dL) levels
GPS 2: Both low albumin (<3.5 g/dL) and elevated CRP (>1.0 mg/dL) levels
mGPS (modified Glasgow prognostic score): Composite score of serum CRP and albumin levels (Score 0/1/2)
mGPS 0: Normal CRP levels (≤1.0 mg/dL) regardless of albumin levels
mGPS 1: Normal albumin (≥3.5 g/dL) and elevated CRP (>1.0 mg/dL) levels
mGPS 2: Low albumin (<3.5 g/dL) and elevated CRP (>1.0 mg/dL) levels
Canton score: Composite score of PNI, NLR, and platelet count (Score 0/1/2/3)
Canton 0: elevated PNI (≥48), low NLR (≤1.83), and normal platelet count (≤300 × 103/mL)
Canton 1: presence of one among the predictors of poor outcome: low PNI (<48), elevated NLR (>1.83), and elevated platelet count (>300 × 103/mL)
Canton 2: presence of two among the predictors of poor outcome: low PNI (<48), elevated NLR (>1.83), and elevated platelet count (>300 × 103/mL)
Canton 3: low PNI (< 48), elevated NLR (> 1.83), and elevated platelet count (> 300 × 103/mL)
Naples prognostic score: Composite score of the serum albumin level, total cholesterol level, NLR, and LMR (Score 0/1/2)
Summation of points for (1) serum albumin level (0, ≥4 g/dL; 1, <4 g/dL), (2) Total cholesterol level (0, >180 mg/dL; 1, ≤180 mg/dL), (3) NLR (0, ≤2.96; 1, >2.9), and (4) LMR (0, >4.44; 1, ≤4.44). The sum of all four points: 0, Naples group 0; 1 or 2, Naples group 1; 3 or 4, Naples group 2
CONUT (controlling nutritional status): Composite score of the serum albumin level, lymphocyte count, and total cholesterol value
Sum of the albumin score (scores 1, 2, 4, and 6 for 3.5–4.5, 3–3.49, 2.5–2.9, and < 2.5 g/dL, respectively), lymphocyte score (scores 0, 1, 2, and 3 for ≥ 1600, 1200–1599, 800–1199, and < 800/mm3, respectively), and total cholesterol score (scores 0, 1, 2, and 3 for >180, 140–180, 100–139, and < 100 mg/dL, respectively). The summation of all three scores: 0–1, Normal; 2–4, Light; 5–8, Moderate; 9–12, Severe
Footnotes
Funding: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No.2016R1A2B4014984) and a faculty research grant of Yonsei University College of Medicine (6-2016-0087).
- Conceptualization: G.A., K.H.I.
- Funding acquisition: K.H.I.
- Resources: G.A., K.H.I.
- Writing - original draft: G.A.
- Writing - review & editing: K.H.I.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Hensler T, Hecker H, Heeg K, Heidecke CD, Bartels H, Barthlen W, et al. Distinct mechanisms of immunosuppression as a consequence of major surgery. Infect Immun. 1997;65:2283–2291. doi: 10.1128/iai.65.6.2283-2291.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zeltsman M, Mayor M, Jones DR, Adusumilli PS. Surgical immune interventions for solid malignancies. Am J Surg. 2016;212:682–690.e5. doi: 10.1016/j.amjsurg.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guner A, Kim SY, Yu JE, Min IK, Roh YH, Roh C, et al. Parameters for predicting surgical outcomes for gastric cancer patients: simple is better than complex. Ann Surg Oncol. 2018;25:3239–3247. doi: 10.1245/s10434-018-6684-2. [DOI] [PubMed] [Google Scholar]
- 4.Pennell LM, Galligan CL, Fish EN. Sex affects immunity. J Autoimmun. 2012;38:J282–J291. doi: 10.1016/j.jaut.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Roved J, Westerdahl H, Hasselquist D. Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences. Horm Behav. 2017;88:95–105. doi: 10.1016/j.yhbeh.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 6.Ono S, Tsujimoto H, Hiraki S, Takahata R, Kinoshita M, Mochizuki H. Sex differences in cytokine production and surface antigen expression of peripheral blood mononuclear cells after surgery. Am J Surg. 2005;190:439–444. doi: 10.1016/j.amjsurg.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 7.Kosuga T, Ichikawa D, Okamoto K, Komatsu S, Konishi H, Takeshita H, et al. Impact of age on early surgical outcomes of laparoscopy-assisted gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer. Anticancer Res. 2015;35:2191–2198. [PubMed] [Google Scholar]
- 8.Kudoh A, Katagai H, Takazawa T, Matsuki A. Plasma proinflammatory cytokine response to surgical stress in elderly patients. Cytokine. 2001;15:270–273. doi: 10.1006/cyto.2001.0927. [DOI] [PubMed] [Google Scholar]
- 9.Milner JJ, Beck MA. The impact of obesity on the immune response to infection. Proc Nutr Soc. 2012;71:298–306. doi: 10.1017/S0029665112000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolb R, Sutterwala FS, Zhang W. Obesity and cancer: inflammation bridges the two. Curr Opin Pharmacol. 2016;29:77–89. doi: 10.1016/j.coph.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gunderson CC, Java J, Moore KN, Walker JL. The impact of obesity on surgical staging, complications, and survival with uterine cancer: a Gynecologic Oncology Group LAP2 ancillary data study. Gynecol Oncol. 2014;133:23–27. doi: 10.1016/j.ygyno.2014.01.041. [DOI] [PubMed] [Google Scholar]
- 12.Khoury W, Lavery IC, Kiran RP. Effects of chronic immunosuppression on long-term oncologic outcomes for colorectal cancer patients undergoing surgery. Ann Surg. 2011;253:323–327. doi: 10.1097/SLA.0b013e3181fc9d36. [DOI] [PubMed] [Google Scholar]
- 13.Moulin CM, Marguti I, Peron JP, Halpern A, Rizzo LV. Bariatric surgery reverses natural killer (NK) cell activity and NK-related cytokine synthesis impairment induced by morbid obesity. Obes Surg. 2011;21:112–118. doi: 10.1007/s11695-010-0250-8. [DOI] [PubMed] [Google Scholar]
- 14.Kotani N, Hashimoto H, Sessler DI, Yoshida H, Kimura N, Okawa H, et al. Smoking decreases alveolar macrophage function during anesthesia and surgery. Anesthesiology. 2000;92:1268–1277. doi: 10.1097/00000542-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Na YM, Kim MY, Kim YK, Ha YR, Yoon DS. Exercise therapy effect on natural killer cell cytotoxic activity in stomach cancer patients after curative surgery. Arch Phys Med Rehabil. 2000;81:777–779. doi: 10.1016/s0003-9993(00)90110-2. [DOI] [PubMed] [Google Scholar]
- 16.Ukkonen M, Karlsson S, Laukkarinen J, Rantanen T, Paajanen H Finnsepsis Study Group. Severe sepsis in elderly patients undergoing gastrointestinal surgery-a prospective multicenter follow-up study of Finnish Intensive Care Units. J Gastrointest Surg. 2016;20:1028–1033. doi: 10.1007/s11605-016-3076-4. [DOI] [PubMed] [Google Scholar]
- 17.Solaini L, Atmaja BT, Arumugam P, Hutchins RR, Abraham AT, Bhattacharya S, et al. The role of perioperative inflammatory-based prognostic systems in patients with colorectal liver metastases undergoing surgery. A cohort study. Int J Surg. 2016;36:8–12. doi: 10.1016/j.ijsu.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 18.Kudoh A, Katagai H, Takazawa T. Plasma inflammatory cytokine response to surgical trauma in chronic depressed patients. Cytokine. 2001;13:104–108. doi: 10.1006/cyto.2000.0802. [DOI] [PubMed] [Google Scholar]
- 19.Sutter PM, Spagnoli GC, Marx A, Gürke L, Troeger H, Fricker R, et al. Increased surface expression of CD18 and CD11b in leukocytes after tourniquet ischemia during elective hand surgery. World J Surg. 1997;21:179–184. doi: 10.1007/s002689900212. [DOI] [PubMed] [Google Scholar]
- 20.Weighardt H, Heidecke CD, Emmanuilidis K, Maier S, Bartels H, Siewert JR, et al. Sepsis after major visceral surgery is associated with sustained and interferon-gamma-resistant defects of monocyte cytokine production. Surgery. 2000;127:309–315. doi: 10.1067/msy.2000.104118. [DOI] [PubMed] [Google Scholar]
- 21.Sammour T, Kahokehr A, Chan S, Booth RJ, Hill AG. The humoral response after laparoscopic versus open colorectal surgery: a meta-analysis. J Surg Res. 2010;164:28–37. doi: 10.1016/j.jss.2010.05.046. [DOI] [PubMed] [Google Scholar]
- 22.Evans C, Galustian C, Kumar D, Hagger R, Melville DM, Bodman-Smith M, et al. Impact of surgery on immunologic function: comparison between minimally invasive techniques and conventional laparotomy for surgical resection of colorectal tumors. Am J Surg. 2009;197:238–245. doi: 10.1016/j.amjsurg.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Zawadzki M, Krzystek-Korpacka M, Gamian A, Witkiewicz W. Comparison of inflammatory responses following robotic and open colorectal surgery: a prospective study. Int J Colorectal Dis. 2017;32:399–407. doi: 10.1007/s00384-016-2697-0. [DOI] [PubMed] [Google Scholar]
- 24.Pilka R, Marek R, Adam T, Kudela M, Ondrová D, Neubert D, et al. Systemic inflammatory response after open, laparoscopic and robotic surgery in endometrial cancer patients. Anticancer Res. 2016;36:2909–2922. [PubMed] [Google Scholar]
- 25.Schneider C, von Aulock S, Zedler S, Schinkel C, Hartung T, Faist E. Perioperative recombinant human granulocyte colony-stimulating factor (Filgrastim) treatment prevents immunoinflammatory dysfunction associated with major surgery. Ann Surg. 2004;239:75–81. doi: 10.1097/01.sla.0000103062.21049.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crozier JE, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC. Relationship between emergency presentation, systemic inflammatory response, and cancer-specific survival in patients undergoing potentially curative surgery for colon cancer. Am J Surg. 2009;197:544–549. doi: 10.1016/j.amjsurg.2007.12.052. [DOI] [PubMed] [Google Scholar]
- 27.Kimura A, Ono S, Hiraki S, Takahata R, Tsujimoto H, Miyazaki H, et al. The postoperative serum interleukin-15 concentration correlates with organ dysfunction and the prognosis of septic patients following emergency gastrointestinal surgery. J Surg Res. 2012;175:e83–e88. doi: 10.1016/j.jss.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Aosasa S, Ono S, Mochizuki H, Tsujimoto H, Osada S, Takayama E, et al. Activation of monocytes and endothelial cells depends on the severity of surgical stress. World J Surg. 2000;24:10–16. doi: 10.1007/s002689910003. [DOI] [PubMed] [Google Scholar]
- 29.Flohé S, Lendemans S, Schade FU, Kreuzfelder E, Waydhas C. Influence of surgical intervention in the immune response of severely injured patients. Intensive Care Med. 2004;30:96–102. doi: 10.1007/s00134-003-2041-3. [DOI] [PubMed] [Google Scholar]
- 30.Gu CY, Zhang J, Qian YN, Tang QF. Effects of epidural anesthesia and postoperative epidural analgesia on immune function in esophageal carcinoma patients undergoing thoracic surgery. Mol Clin Oncol. 2015;3:190–196. doi: 10.3892/mco.2014.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen WK, Ren L, Wei Y, Zhu DX, Miao CH, Xu JM. General anesthesia combined with epidural anesthesia ameliorates the effect of fast-track surgery by mitigating immunosuppression and facilitating intestinal functional recovery in colon cancer patients. Int J Colorectal Dis. 2015;30:475–481. doi: 10.1007/s00384-014-2098-1. [DOI] [PubMed] [Google Scholar]
- 32.Sacerdote P, Bianchi M, Gaspani L, Manfredi B, Maucione A, Terno G, et al. The effects of tramadol and morphine on immune responses and pain after surgery in cancer patients. Anesth Analg. 2000;90:1411–1414. doi: 10.1097/00000539-200006000-00028. [DOI] [PubMed] [Google Scholar]
- 33.Martínez AB, Longás J, Ramírez JM. A model for lymphocyte activation in open versus laparoscopic surgery in colorectal cancer patients in enhanced recovery after surgery (ERAS) protocols. Int J Colorectal Dis. 2017;32:913–916. doi: 10.1007/s00384-016-2731-2. [DOI] [PubMed] [Google Scholar]
- 34.Veenhof AA, Vlug MS, van der Pas MH, Sietses C, van der Peet DL, de Lange-de Klerk ES, et al. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg. 2012;255:216–221. doi: 10.1097/SLA.0b013e31824336e2. [DOI] [PubMed] [Google Scholar]
- 35.Yang D, He W, Zhang S, Chen H, Zhang C, He Y. Fast-track surgery improves postoperative clinical recovery and immunity after elective surgery for colorectal carcinoma: randomized controlled clinical trial. World J Surg. 2012;36:1874–1880. doi: 10.1007/s00268-012-1606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heiss MM, Fasol-Merten K, Allgayer H, Ströhlein MA, Tarabichi A, Wallner S, et al. Influence of autologous blood transfusion on natural killer and lymphokine-activated killer cell activities in cancer surgery. Vox Sang. 1997;73:237–245. doi: 10.1046/j.1423-0410.1997.7340237.x. [DOI] [PubMed] [Google Scholar]
- 37.Theodoraki K, Markatou M, Rizos D, Fassoulaki A. The impact of two different transfusion strategies on patient immune response during major abdominal surgery: a preliminary report. J Immunol Res. 2014;2014:945829. doi: 10.1155/2014/945829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fukuda T, Seto Y, Yamada K, Hiki N, Fukunaga T, Oyama S, et al. Can immune-enhancing nutrients reduce postoperative complications in patients undergoing esophageal surgery? Dis Esophagus. 2008;21:708–711. doi: 10.1111/j.1442-2050.2008.00861.x. [DOI] [PubMed] [Google Scholar]
- 39.Giger U, Büchler M, Farhadi J, Berger D, Hüsler J, Schneider H, et al. Preoperative immunonutrition suppresses perioperative inflammatory response in patients with major abdominal surgery-a randomized controlled pilot study. Ann Surg Oncol. 2007;14:2798–2806. doi: 10.1245/s10434-007-9407-7. [DOI] [PubMed] [Google Scholar]
- 40.Arumugam S, Lau CS, Chamberlain RS. Probiotics and Synbiotics Decrease Postoperative Sepsis in Elective Gastrointestinal Surgical Patients: a Meta-Analysis. J Gastrointest Surg. 2016;20:1123–1131. doi: 10.1007/s11605-016-3142-y. [DOI] [PubMed] [Google Scholar]
- 41.Liu Z, Li C, Huang M, Tong C, Zhang X, Wang L, et al. Positive regulatory effects of perioperative probiotic treatment on postoperative liver complications after colorectal liver metastases surgery: a double-center and double-blind randomized clinical trial. BMC Gastroenterol. 2015;15:34. doi: 10.1186/s12876-015-0260-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Braga M, Gianotti L, Vignali A, Di Carlo V. Immunonutrition in gastric cancer surgical patients. Nutrition. 1998;14:831–835. doi: 10.1016/s0899-9007(98)00103-8. [DOI] [PubMed] [Google Scholar]
- 43.Furukawa K, Tashiro T, Yamamori H, Takagi K, Morishima Y, Sugiura T, et al. Effects of soybean oil emulsion and eicosapentaenoic acid on stress response and immune function after a severely stressful operation. Ann Surg. 1999;229:255–261. doi: 10.1097/00000658-199902000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang WP, Yan XL, Ni YF, Guo K, Ke CK, Cheng QS, et al. Effects of lipid emulsions in parenteral nutrition of esophageal cancer surgical patients receiving enteral nutrition: a comparative analysis. Nutrients. 2013;6:111–123. doi: 10.3390/nu6010111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schmidt SC, Hamann S, Langrehr JM, Höflich C, Mittler J, Jacob D, et al. Preoperative high-dose steroid administration attenuates the surgical stress response following liver resection: results of a prospective randomized study. J Hepatobiliary Pancreat Surg. 2007;14:484–492. doi: 10.1007/s00534-006-1200-7. [DOI] [PubMed] [Google Scholar]
- 46.Pratschke S, von Dossow-Hanfstingl V, Dietz J, Schneider CP, Tufman A, Albertsmeier M, et al. Dehydroepiandrosterone modulates T-cell response after major abdominal surgery. J Surg Res. 2014;189:117–125. doi: 10.1016/j.jss.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 47.Li H, Wang C, Yu J, Cao S, Wei F, Zhang W, et al. Dendritic cell-activated cytokine-induced killer cells enhance the anti-tumor effect of chemotherapy on non-small cell lung cancer in patients after surgery. Cytotherapy. 2009;11:1076–1083. doi: 10.3109/14653240903121252. [DOI] [PubMed] [Google Scholar]
- 48.Brivio F, Lissoni P, Gilardi R, Ferrante R, Vigore L, Curzi L, et al. Abrogation of surgery-induced decline in circulating dendritic cells by subcutaneous preoperative administration of IL-2 in operable cancer patients. J Biol Regul Homeost Agents. 2000;14:200–203. [PubMed] [Google Scholar]
- 49.Nishiyama J, Matsuda M, Ando S, Hirasawa M, Suzuki T, Makuuchi H. The effects of the early administration of sivelestat sodium, a selective neutrophil elastase inhibitor, on the postoperative course after radical surgery for esophageal cancer. Surg Today. 2012;42:659–665. doi: 10.1007/s00595-011-0105-5. [DOI] [PubMed] [Google Scholar]
- 50.Ono S, Aosasa S, Mochizuki H. Effects of a protease inhibitor on reduction of surgical stress in esophagectomy. Am J Surg. 1999;177:78–82. doi: 10.1016/s0002-9610(98)00300-6. [DOI] [PubMed] [Google Scholar]
- 51.Kerr SF, Klonizakis M, Glynne-Jones R. Suppression of the postoperative neutrophil leucocytosis following neoadjuvant chemoradiotherapy for rectal cancer and implications for surgical morbidity. Colorectal Dis. 2010;12:549–554. doi: 10.1111/j.1463-1318.2009.01858.x. [DOI] [PubMed] [Google Scholar]
- 52.Tanis E, Julié C, Emile JF, Mauer M, Nordlinger B, Aust D, et al. Prognostic impact of immune response in resectable colorectal liver metastases treated by surgery alone or surgery with perioperative FOLFOX in the randomised EORTC study 40983. Eur J Cancer. 2015;51:2708–2717. doi: 10.1016/j.ejca.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 53.Westerterp M, Boermeester MA, Omloo JM, Hulshof MC, Vervenne WL, Lutter R, et al. Differential responses of cellular immunity in patients undergoing neoadjuvant therapy followed by surgery for carcinoma of the oesophagus. Cancer Immunol Immunother. 2008;57:1837–1847. doi: 10.1007/s00262-008-0511-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang D, Yang XL, Chai XQ, Shu SH, Zhang XL, Xie YH, et al. A short-term increase of the postoperative naturally circulating dendritic cells subsets in flurbiprofen-treated patients with esophageal carcinoma undergoing thoracic surgery. Oncotarget. 2016;7:18705–18712. doi: 10.18632/oncotarget.7669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liakopoulos OJ, Dörge H, Schmitto JD, Nagorsnik U, Grabedünkel J, Schoendube FA. Effects of preoperative statin therapy on cytokines after cardiac surgery. Thorac Cardiovasc Surg. 2006;54:250–254. doi: 10.1055/s-2006-923836. [DOI] [PubMed] [Google Scholar]
- 56.Amar D, Zhang H, Park B, Heerdt PM, Fleisher M, Thaler HT. Inflammation and outcome after general thoracic surgery. Eur J Cardiothorac Surg. 2007;32:431–434. doi: 10.1016/j.ejcts.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 57.De Lorenzo A, Pittella F, Rocha A. Increased preoperative C-reactive protein levels are associated with inhospital death after coronary artery bypass surgery. Inflammation. 2012;35:1179–1183. doi: 10.1007/s10753-011-9426-1. [DOI] [PubMed] [Google Scholar]
- 58.Ishizuka M, Kubota K, Kita J, Shimoda M, Kato M, Sawada T. Usefulness of a modified inflammation-based prognostic system for predicting postoperative mortality of patients undergoing surgery for primary hepatocellular carcinoma. J Surg Oncol. 2011;103:801–806. doi: 10.1002/jso.21857. [DOI] [PubMed] [Google Scholar]
- 59.Josse JM, Cleghorn MC, Ramji KM, Jiang H, Elnahas A, Jackson TD, et al. The neutrophil-to-lymphocyte ratio predicts major perioperative complications in patients undergoing colorectal surgery. Colorectal Dis. 2016;18:O236–O242. doi: 10.1111/codi.13373. [DOI] [PubMed] [Google Scholar]
- 60.Mokart D, Capo C, Blache JL, Delpero JR, Houvenaeghel G, Martin C, et al. Early postoperative compensatory anti-inflammatory response syndrome is associated with septic complications after major surgical trauma in patients with cancer. Br J Surg. 2002;89:1450–1456. doi: 10.1046/j.1365-2168.2002.02218.x. [DOI] [PubMed] [Google Scholar]
- 61.Rettig TC, Verwijmeren L, Dijkstra IM, Boerma D, van de Garde EM, Noordzij PG. Postoperative interleukin-6 level and early detection of complications after elective major abdominal surgery. Ann Surg. 2016;263:1207–1212. doi: 10.1097/SLA.0000000000001342. [DOI] [PubMed] [Google Scholar]
- 62.Saeed K, Dale AP, Leung E, Cusack T, Mohamed F, Lockyer G, et al. Procalcitonin levels predict infectious complications and response to treatment in patients undergoing cytoreductive surgery for peritoneal malignancy. Eur J Surg Oncol. 2016;42:234–243. doi: 10.1016/j.ejso.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 63.Weighardt H, Heidecke CD, Westerholt A, Emmanuilidis K, Maier S, Veit M, et al. Impaired monocyte IL-12 production before surgery as a predictive factor for the lethal outcome of postoperative sepsis. Ann Surg. 2002;235:560–567. doi: 10.1097/00000658-200204000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Anitei MG, Zeitoun G, Mlecnik B, Marliot F, Haicheur N, Todosi AM, et al. Prognostic and predictive values of the immunoscore in patients with rectal cancer. Clin Cancer Res. 2014;20:1891–1899. doi: 10.1158/1078-0432.CCR-13-2830. [DOI] [PubMed] [Google Scholar]
- 65.Matsutani S, Shibutani M, Maeda K, Nagahara H, Fukuoka T, Nakao S, et al. Significance of tumor-infiltrating lymphocytes before and after neoadjuvant therapy for rectal cancer. Cancer Sci. 2018;109:966–979. doi: 10.1111/cas.13542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Kubota K. Systemic inflammatory response predicts perioperative central venous catheter-related bloodstream infection in patients Undergoing colorectal cancer surgery with administration of parenteral nutrition. Anticancer Res. 2012;32:4045–4050. [PubMed] [Google Scholar]
- 67.Strohmeyer JC, Blume C, Meisel C, Doecke WD, Hummel M, Hoeflich C, et al. Standardized immune monitoring for the prediction of infections after cardiopulmonary bypass surgery in risk patients. Cytometry B Clin Cytom. 2003;53:54–62. doi: 10.1002/cyto.b.10031. [DOI] [PubMed] [Google Scholar]
- 68.Song B, Zhen S, Meng F. T cell inflammation profile after surgical resection may predict tumor recurrence in HBV-related hepatocellular carcinoma. Int Immunopharmacol. 2016;41:35–41. doi: 10.1016/j.intimp.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 69.Chan AW, Chan SL, Wong GL, Wong VW, Chong CC, Lai PB, et al. Prognostic nutritional index (PNI) predicts tumor recurrence of very early/early stage hepatocellular carcinoma after surgical resection. Ann Surg Oncol. 2015;22:4138–4148. doi: 10.1245/s10434-015-4516-1. [DOI] [PubMed] [Google Scholar]
- 70.Lindenmann J, Fink-Neuboeck N, Avian A, Pichler M, Habitzruther M, Maier A, et al. Preoperative Glasgow prognostic score as additional independent prognostic parameter for patients with esophageal cancer after curative esophagectomy. Eur J Surg Oncol. 2017;43:445–453. doi: 10.1016/j.ejso.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 71.Toiyama Y, Inoue Y, Saigusa S, Kawamura M, Kawamoto A, Okugawa Y, et al. C-reactive protein as predictor of recurrence in patients with rectal cancer undergoing chemoradiotherapy followed by surgery. Anticancer Res. 2013;33:5065–5074. [PubMed] [Google Scholar]
- 72.Wei IH, Harmon CM, Arcerito M, Cheng DF, Minter RM, Simeone DM. Tumor-associated macrophages are a useful biomarker to predict recurrence after surgical resection of nonfunctional pancreatic neuroendocrine tumors. Ann Surg. 2014;260:1088–1094. doi: 10.1097/SLA.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Galizia G, Lieto E, Auricchio A, Cardella F, Mabilia A, Podzemny V, et al. Naples prognostic score, based on nutritional and inflammatory status, is an independent predictor of long-term outcome in patients undergoing surgery for colorectal cancer. Dis Colon Rectum. 2017;60:1273–1284. doi: 10.1097/DCR.0000000000000961. [DOI] [PubMed] [Google Scholar]
- 74.He YF, Luo HQ, Wang W, Chen J, Yao YW, Yan Y, et al. Preoperative NLR and PLR in the middle or lower ESCC patients with radical operation. Eur J Cancer Care (Engl) 2017;26:e12445. doi: 10.1111/ecc.12445. [DOI] [PubMed] [Google Scholar]
- 75.Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Shibuya N, Kubota K. Clinical significance of the C-reactive protein to albumin ratio for survival after surgery for colorectal cancer. Ann Surg Oncol. 2016;23:900–907. doi: 10.1245/s10434-015-4948-7. [DOI] [PubMed] [Google Scholar]
- 76.Ishizuka M, Oyama Y, Abe A, Kubota K. Combination of platelet count and neutrophil to lymphocyte ratio is a useful predictor of postoperative survival in patients undergoing surgery for gastric cancer. J Surg Oncol. 2014;110:935–941. doi: 10.1002/jso.23753. [DOI] [PubMed] [Google Scholar]
- 77.Malietzis G, Giacometti M, Askari A, Nachiappan S, Kennedy RH, Faiz OD, et al. A preoperative neutrophil to lymphocyte ratio of 3 predicts disease-free survival after curative elective colorectal cancer surgery. Ann Surg. 2014;260:287–292. doi: 10.1097/SLA.0000000000000216. [DOI] [PubMed] [Google Scholar]
- 78.Mimatsu K, Fukino N, Ogasawara Y, Saino Y, Oida T. Utility of inflammatory marker- and nutritional status-based prognostic factors for predicting the prognosis of stage IV gastric cancer patients undergoing non-curative surgery. Anticancer Res. 2017;37:4215–4222. doi: 10.21873/anticanres.11812. [DOI] [PubMed] [Google Scholar]
- 79.Watt DG, Martin JC, Park JH, Horgan PG, McMillan DC. Neutrophil count is the most important prognostic component of the differential white cell count in patients undergoing elective surgery for colorectal cancer. Am J Surg. 2015;210:24–30. doi: 10.1016/j.amjsurg.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 80.Yamamoto T, Yanagimoto H, Satoi S, Toyokawa H, Yamao J, Kim S, et al. Circulating myeloid dendritic cells as prognostic factors in patients with pancreatic cancer who have undergone surgical resection. J Surg Res. 2012;173:299–308. doi: 10.1016/j.jss.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 81.Zikos TA, Donnenberg AD, Landreneau RJ, Luketich JD, Donnenberg VS. Lung T-cell subset composition at the time of surgical resection is a prognostic indicator in non-small cell lung cancer. Cancer Immunol Immunother. 2011;60:819–827. doi: 10.1007/s00262-011-0996-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jin Z, Li R, Liu J, Lin J. Long-term prognosis after cancer surgery with inhalational anesthesia and total intravenous anesthesia: a systematic review and meta-analysis. Int J Physiol Pathophysiol Pharmacol. 2019;11:83–94. [PMC free article] [PubMed] [Google Scholar]
- 83.Weng M, Chen W, Hou W, Li L, Ding M, Miao C. The effect of neuraxial anesthesia on cancer recurrence and survival after cancer surgery: an updated meta-analysis. Oncotarget. 2016;7:15262–15273. doi: 10.18632/oncotarget.7683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Giger-Pabst U, Lange J, Maurer C, Bucher C, Schreiber V, Schlumpf R, et al. Short-term preoperative supplementation of an immunoenriched diet does not improve clinical outcome in well-nourished patients undergoing abdominal cancer surgery. Nutrition. 2013;29:724–729. doi: 10.1016/j.nut.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 85.Klek S, Sierzega M, Szybinski P, Szczepanek K, Scislo L, Walewska E, et al. The immunomodulating enteral nutrition in malnourished surgical patients - a prospective, randomized, double-blind clinical trial. Clin Nutr. 2011;30:282–288. doi: 10.1016/j.clnu.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 86.Chen L, Sun L, Lang Y, Wu J, Yao L, Ning J, et al. Fast-track surgery improves postoperative clinical recovery and cellular and humoral immunity after esophagectomy for esophageal cancer. BMC Cancer. 2016;16:449. doi: 10.1186/s12885-016-2506-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liu HT, Huang YC, Cheng SB, Huang YT, Lin PT. Effects of coenzyme Q10 supplementation on antioxidant capacity and inflammation in hepatocellular carcinoma patients after surgery: a randomized, placebo-controlled trial. Nutr J. 2016;15:85. doi: 10.1186/s12937-016-0205-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Parolari A, Camera M, Alamanni F, Naliato M, Polvani GL, Agrifoglio M, et al. Systemic inflammation after on-pump and off-pump coronary bypass surgery: a one-month follow-up. Ann Thorac Surg. 2007;84:823–828. doi: 10.1016/j.athoracsur.2007.04.048. [DOI] [PubMed] [Google Scholar]
- 89.Papadima A, Boutsikou M, Lagoudianakis EE, Kataki A, Konstadoulakis M, Georgiou L, et al. Lymphocyte apoptosis after major abdominal surgery is not influenced by anesthetic technique: a comparative study of general anesthesia versus combined general and epidural analgesia. J Clin Anesth. 2009;21:414–421. doi: 10.1016/j.jclinane.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 90.Reisinger KW, Derikx JP, van Vugt JL, Von Meyenfeldt MF, Hulsewé KW, Olde Damink SW, et al. Sarcopenia is associated with an increased inflammatory response to surgery in colorectal cancer. Clin Nutr. 2016;35:924–927. doi: 10.1016/j.clnu.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 91.Buttenschoen K, Schneider ME, Utz K, Kornmann M, Beger HG, Carli Buttenschoen D. Effect of major abdominal surgery on endotoxin release and expression of Toll-like receptors 2/4. Langenbecks Arch Surg. 2009;394:293–302. doi: 10.1007/s00423-008-0357-8. [DOI] [PubMed] [Google Scholar]
- 92.Brix-Christensen V, Tønnesen E, Sørensen IJ, Bilfinger TV, Sanchez RG, Stefano GB. Effects of anaesthesia based on high versus low doses of opioids on the cytokine and acute-phase protein responses in patients undergoing cardiac surgery. Acta Anaesthesiol Scand. 1998;42:63–70. doi: 10.1111/j.1399-6576.1998.tb05082.x. [DOI] [PubMed] [Google Scholar]
- 93.Greco F, Hoda MR, Wagner S, Reichelt O, Inferrera A, Fischer K, et al. Adipocytokine: a new family of inflammatory and immunologic markers of invasiveness in major urologic surgery. Eur Urol. 2010;58:781–787. doi: 10.1016/j.eururo.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 94.Iwasaki A, Shirakusa T, Maekawa T, Enatsu S, Maekawa S. Clinical evaluation of systemic inflammatory response syndrome (SIRS) in advanced lung cancer (T3 and T4) with surgical resection. Eur J Cardiothorac Surg. 2005;27:14–18. doi: 10.1016/j.ejcts.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 95.Bruce DM, Smith M, Walker CB, Heys SD, Binnie NR, Gough DB, et al. Minimal access surgery for cholelithiasis induces an attenuated acute phase response. Am J Surg. 1999;178:232–234. doi: 10.1016/s0002-9610(99)00160-9. [DOI] [PubMed] [Google Scholar]
- 96.Mokart D, Merlin M, Sannini A, Brun JP, Delpero JR, Houvenaeghel G, et al. Procalcitonin, interleukin 6 and systemic inflammatory response syndrome (SIRS): early markers of postoperative sepsis after major surgery. Br J Anaesth. 2005;94:767–773. doi: 10.1093/bja/aei143. [DOI] [PubMed] [Google Scholar]
- 97.Karth GD, Buberl A, Nikfardjam M, Meyer B, Wollenek G, Grimm M, et al. Role of amiodarone on the systemic inflammatory response induced by cardiac surgery: proinflammatory actions. Can J Anaesth. 2007;54:262–268. doi: 10.1007/BF03022770. [DOI] [PubMed] [Google Scholar]
- 98.Ni XC, Yi Y, Fu YP, He HW, Cai XY, Wang JX, et al. Prognostic value of the modified Glasgow prognostic score in patients undergoing radical surgery for hepatocellular carcinoma. Medicine (Baltimore) 2015;94:e1486. doi: 10.1097/MD.0000000000001486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ji F, Liang Y, Fu SJ, Guo ZY, Shu M, Shen SL, et al. A novel and accurate predictor of survival for patients with hepatocellular carcinoma after surgical resection: the neutrophil to lymphocyte ratio (NLR) combined with the aspartate aminotransferase/platelet count ratio index (APRI) BMC Cancer. 2016;16:137. doi: 10.1186/s12885-016-2189-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dias Rodrigues V, Barroso de Pinho N, Abdelhay E, Viola JP, Correia MI, Brum Martucci R. Nutrition and immune-modulatory intervention in surgical patients with gastric cancer. Nutr Clin Pract. 2017;32:122–129. doi: 10.1177/0884533616653807. [DOI] [PubMed] [Google Scholar]
- 101.Sun KY, Xu JB, Chen SL, Yuan YJ, Wu H, Peng JJ, et al. Novel immunological and nutritional-based prognostic index for gastric cancer. World J Gastroenterol. 2015;21:5961–5971. doi: 10.3748/wjg.v21.i19.5961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Xie X, Luo KJ, Hu Y, Wang JY, Chen J. Prognostic value of preoperative platelet-lymphocyte and neutrophil-lymphocyte ratio in patients undergoing surgery for esophageal squamous cell cancer. Dis Esophagus. 2016;29:79–85. doi: 10.1111/dote.12296. [DOI] [PubMed] [Google Scholar]
- 103.Liao R, Jiang N, Tang ZW, Li W, Huang P, Luo SQ, et al. Systemic and intratumoral balances between monocytes/macrophages and lymphocytes predict prognosis in hepatocellular carcinoma patients after surgery. Oncotarget. 2016;7:30951–30961. doi: 10.18632/oncotarget.9049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hyun MH, Lee CH, Kwon YJ, Cho SI, Jang YJ, Kim DH, et al. Robot versus laparoscopic gastrectomy for cancer by an experienced surgeon: comparisons of surgery, complications, and surgical stress. Ann Surg Oncol. 2013;20:1258–1265. doi: 10.1245/s10434-012-2679-6. [DOI] [PubMed] [Google Scholar]
- 105.Hsu JT, Wang CC, Le PH, Chen TH, Kuo CJ, Lin CJ, et al. Lymphocyte-to-monocyte ratios predict gastric cancer surgical outcomes. J Surg Res. 2016;202:284–290. doi: 10.1016/j.jss.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 106.Pang S, Zhou Z, Yu X, Wei S, Chen Q, Nie S, et al. The predictive value of integrated inflammation scores in the survival of patients with resected hepatocellular carcinoma: a retrospective cohort study. Int J Surg. 2017;42:170–177. doi: 10.1016/j.ijsu.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 107.Jain S, Gautam V, Naseem S. Acute-phase proteins: As diagnostic tool. J Pharm Bioallied Sci. 2011;3:118–127. doi: 10.4103/0975-7406.76489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Warschkow R, Tarantino I, Ukegjini K, Beutner U, Müller SA, Schmied BM, et al. Diagnostic study and meta-analysis of C-reactive protein as a predictor of postoperative inflammatory complications after gastroesophageal cancer surgery. Langenbecks Arch Surg. 2012;397:727–736. doi: 10.1007/s00423-012-0944-6. [DOI] [PubMed] [Google Scholar]
- 109.Warschkow R, Ukegjini K, Tarantino I, Steffen T, Müller SA, Schmied BM, et al. Diagnostic study and meta-analysis of C-reactive protein as a predictor of postoperative inflammatory complications after pancreatic surgery. J Hepatobiliary Pancreat Sci. 2012;19:492–500. doi: 10.1007/s00534-011-0462-x. [DOI] [PubMed] [Google Scholar]
- 110.Kim S, McClave SA, Martindale RG, Miller KR, Hurt RT. Hypoalbuminemia and Clinical Outcomes: What is the Mechanism behind the Relationship? Am Surg. 2017;83:1220–1227. doi: 10.1177/000313481708301123. [DOI] [PubMed] [Google Scholar]
- 111.Iwaku A, Kinoshita A, Onoda H, Fushiya N, Nishino H, Matsushima M, et al. The Glasgow prognostic score accurately predicts survival in patients with biliary tract cancer not indicated for surgical resection. Med Oncol. 2014;31:787. doi: 10.1007/s12032-013-0787-1. [DOI] [PubMed] [Google Scholar]
- 112.Dupré A, Malik HZ. Inflammation and cancer: what a surgical oncologist should know. Eur J Surg Oncol. 2018;44:566–570. doi: 10.1016/j.ejso.2018.02.209. [DOI] [PubMed] [Google Scholar]
- 113.Roxburgh CS, Salmond JM, Horgan PG, Oien KA, McMillan DC. The relationship between the local and systemic inflammatory responses and survival in patients undergoing curative surgery for colon and rectal cancers. J Gastrointest Surg. 2009;13:2011–2018. doi: 10.1007/s11605-009-1034-0. [DOI] [PubMed] [Google Scholar]
- 114.Guner A, Kim HI. ASO Author Reflections: Parameters for Predicting Surgical Outcomes for Gastric Cancer Patients: Simple Is Better Than Complex. Ann Surg Oncol. 2018;25:699–700. doi: 10.1245/s10434-018-6725-x. [DOI] [PubMed] [Google Scholar]
- 115.Lee JY, Kim HI, Kim YN, Hong JH, Alshomimi S, An JY, et al. Clinical significance of the prognostic nutritional index for predicting short- and long-term surgical outcomes after gastrectomy: a retrospective analysis of 7781 gastric cancer patients. Medicine (Baltimore) 2016;95:e3539. doi: 10.1097/MD.0000000000003539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kohira S, Oka N, Inoue N, Itatani K, Hanayama N, Kitamura T, et al. Effect of the neutrophil elastase inhibitor sivelestat on perioperative inflammatory response after pediatric heart surgery with cardiopulmonary bypass: a prospective randomized study. Artif Organs. 2013;37:1027–1033. doi: 10.1111/aor.12103. [DOI] [PubMed] [Google Scholar]
- 117.Ng CS, Lee TW, Wan S, Wan IY, Sihoe AD, Arifi AA, et al. Thoracotomy is associated with significantly more profound suppression in lymphocytes and natural killer cells than video-assisted thoracic surgery following major lung resections for cancer. J Invest Surg. 2005;18:81–88. doi: 10.1080/08941930590926320. [DOI] [PubMed] [Google Scholar]
- 118.Volk T, Schenk M, Voigt K, Tohtz S, Putzier M, Kox WJ. Postoperative epidural anesthesia preserves lymphocyte, but not monocyte, immune function after major spine surgery. Anesth Analg. 2004;98:1086–1092. doi: 10.1213/01.ANE.0000104586.12700.3A. [DOI] [PubMed] [Google Scholar]
- 119.Ammendola M, Sacco R, Zuccalà V, Luposella M, Patruno R, Gadaleta P, et al. Mast cells density positive to tryptase correlate with microvascular density in both primary gastric cancer tissue and loco-regional lymph node metastases from patients that have undergone radical surgery. Int J Mol Sci. 2016;17:1905. doi: 10.3390/ijms17111905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Decker D, Tolba R, Springer W, Lauschke H, Hirner A, von Ruecker A. Abdominal surgical interventions: local and systemic consequences for the immune system--a prospective study on elective gastrointestinal surgery. J Surg Res. 2005;126:12–18. doi: 10.1016/j.jss.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 121.Leal-Noval SR, Muñoz-Gómez M, Arellano V, Adsuar A, Jiménez-Sánchez M, Corcia Y, et al. Influence of red blood cell transfusion on CD4+ T-helper cells immune response in patients undergoing cardiac surgery. J Surg Res. 2010;164:43–49. doi: 10.1016/j.jss.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 122.Matsuda A, Furukawa K, Takasaki H, Suzuki H, Kan H, Tsuruta H, et al. Preoperative oral immune-enhancing nutritional supplementation corrects Th1/Th2 imbalance in patients undergoing elective surgery for colorectal cancer. Dis Colon Rectum. 2006;49:507–516. doi: 10.1007/s10350-005-0292-5. [DOI] [PubMed] [Google Scholar]
- 123.Kirman I, Belizon A, Balik E, Feingold D, Arnell T, Horst P, et al. Perioperative sargramostim (recombinant human GM-CSF) induces an increase in the level of soluble VEGFR1 in colon cancer patients undergoing minimally invasive surgery. Eur J Surg Oncol. 2007;33:1169–1176. doi: 10.1016/j.ejso.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 124.Crucitti A, Corbi M, Tomaiuolo PM, Fanali C, Mazzari A, Lucchetti D, et al. Laparoscopic surgery for colorectal cancer is not associated with an increase in the circulating levels of several inflammation-related factors. Cancer Biol Ther. 2015;16:671–677. doi: 10.1080/15384047.2015.1026476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Spittler A, Sautner T, Gornikiewicz A, Manhart N, Oehler R, Bergmann M, et al. Postoperative glycyl-glutamine infusion reduces immunosuppression: partial prevention of the surgery induced decrease in HLA-DR expression on monocytes. Clin Nutr. 2001;20:37–42. doi: 10.1054/clnu.2000.0153. [DOI] [PubMed] [Google Scholar]
- 126.Welters ID, Feurer MK, Preiss V, Müller M, Scholz S, Kwapisz M, et al. Continuous S-(+)-ketamine administration during elective coronary artery bypass graft surgery attenuates pro-inflammatory cytokine response during and after cardiopulmonary bypass. Br J Anaesth. 2011;106:172–179. doi: 10.1093/bja/aeq341. [DOI] [PubMed] [Google Scholar]
- 127.Ikuta S, Miki C, Hatada T, Inoue Y, Araki T, Tanaka K, et al. Allogenic blood transfusion is an independent risk factor for infective complications after less invasive gastrointestinal surgery. Am J Surg. 2003;185:188–193. doi: 10.1016/s0002-9610(02)01370-3. [DOI] [PubMed] [Google Scholar]
- 128.Leijte GP, Custers H, Gerretsen J, Heijne A, Roth J, Vogl T, et al. Increased plasma levels of danger-associated molecular patterns are associated with immune suppression and postoperative infections in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Front Immunol. 2018;9:663. doi: 10.3389/fimmu.2018.00663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Schilling T, Kozian A, Senturk M, Huth C, Reinhold A, Hedenstierna G, et al. Effects of volatile and intravenous anesthesia on the alveolar and systemic inflammatory response in thoracic surgical patients. Anesthesiology. 2011;115:65–74. doi: 10.1097/ALN.0b013e318214b9de. [DOI] [PubMed] [Google Scholar]
- 130.Zak-Nejmark T, Jankowska R, Passowicz-Muszynska E, Malolepszy J, Marciniak M, Jonkisz A, et al. Skin reactivity to histamine and expression of histamine receptors mRNA in lymphocytes of healthy subjects and non-small-cell lung cancer patients before and after surgery. Lung Cancer. 2004;45:31–38. doi: 10.1016/j.lungcan.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 131.Leaver HA, Craig SR, Yap PL, Walker WS. Lymphocyte responses following open and minimally invasive thoracic surgery. Eur J Clin Invest. 2000;30:230–238. doi: 10.1046/j.1365-2362.2000.00622.x. [DOI] [PubMed] [Google Scholar]
- 132.Qadan M, Battista C, Gardner SA, Anderson G, Akca O, Polk HC., Jr Oxygen and surgical site infection: a study of underlying immunologic mechanisms. Anesthesiology. 2010;113:369–377. doi: 10.1097/ALN.0b013e3181e19d1d. [DOI] [PubMed] [Google Scholar]
- 133.Kim HI, Kim H, Cho HW, Kim SY, Song KJ, Hyung WJ, et al. The ratio of intra-tumoral regulatory T cells (Foxp3+)/helper T cells (CD4+) is a prognostic factor and associated with recurrence pattern in gastric cardia cancer. J Surg Oncol. 2011;104:728–733. doi: 10.1002/jso.22038. [DOI] [PubMed] [Google Scholar]
- 134.Lee JY, Son T, Cheong JH, Hyung WJ, Noh SH, Kim CB, et al. Association between chemotherapy-response assays and subsets of tumor-infiltrating lymphocytes in gastric cancer: a pilot study. J Gastric Cancer. 2015;15:223–230. doi: 10.5230/jgc.2015.15.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lee S, Choi S, Kim SY, Yun MJ, Kim HI. Potential utility of FDG PET-CT as a non-invasive tool for monitoring local immune responses. J Gastric Cancer. 2017;17:384–393. doi: 10.5230/jgc.2017.17.e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zhuang Y, Peng LS, Zhao YL, Shi Y, Mao XH, Chen W, et al. CD8+ T cells that produce interleukin-17 regulate myeloid-derived suppressor cells and are associated with survival time of patients with gastric cancer. Gastroenterology. 2012;143:951–962.e8. doi: 10.1053/j.gastro.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 137.Gérard A, Beemiller P, Friedman RS, Jacobelli J, Krummel MF. Evolving immune circuits are generated by flexible, motile, and sequential immunological synapses. Immunol Rev. 2013;251:80–96. doi: 10.1111/imr.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Xie J, Tato CM, Davis MM. How the immune system talks to itself: the varied role of synapses. Immunol Rev. 2013;251:65–79. doi: 10.1111/imr.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Annunziato F, Romagnani C, Romagnani S. The 3 major types of innate and adaptive cell-mediated effector immunity. J Allergy Clin Immunol. 2015;135:626–635. doi: 10.1016/j.jaci.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 140.Romagnani S. T-cell subsets (Th1 versus Th2) Ann Allergy Asthma Immunol. 2000;85:9–18. doi: 10.1016/S1081-1206(10)62426-X. [DOI] [PubMed] [Google Scholar]
- 141.Moraga I, Spangler J, Mendoza JL, Garcia KC. Multifarious determinants of cytokine receptor signaling specificity. Adv Immunol. 2014;121:1–39. doi: 10.1016/B978-0-12-800100-4.00001-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Miller MC, Mayo KH. Chemokines from a structural perspective. Int J Mol Sci. 2017;18:18. doi: 10.3390/ijms18102088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lin E, Calvano SE, Lowry SF. Inflammatory cytokines and cell response in surgery. Surgery. 2000;127:117–126. doi: 10.1067/msy.2000.101584. [DOI] [PubMed] [Google Scholar]
- 144.Cavaillon JM, Singer M. Inflammation: From Molecular and Cellular Mechanisms to the Clinic. Weinheim: Wiley-VCH; 2017. [Google Scholar]
- 145.Datta J, Berk E, Xu S, Fitzpatrick E, Rosemblit C, Lowenfeld L, et al. Anti-HER2 CD4+ T-helper type 1 response is a novel immune correlate to pathologic response following neoadjuvant therapy in HER2-positive breast cancer. Breast Cancer Res. 2015;17:71. doi: 10.1186/s13058-015-0584-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kvarnström A, Swartling T, Kurlberg G, Bengtson JP, Bengtsson A. Pro-inflammatory cytokine release in rectal surgery: comparison between laparoscopic and open surgical techniques. Arch Immunol Ther Exp (Warsz) 2013;61:407–411. doi: 10.1007/s00005-013-0239-9. [DOI] [PubMed] [Google Scholar]
- 147.Wu FP, Sietses C, von Blomberg BM, van Leeuwen PA, Meijer S, Cuesta MA. Systemic and peritoneal inflammatory response after laparoscopic or conventional colon resection in cancer patients: a prospective, randomized trial. Dis Colon Rectum. 2003;46:147–155. doi: 10.1007/s10350-004-6516-2. [DOI] [PubMed] [Google Scholar]
- 148.Leung KL, Lai PB, Ho RL, Meng WC, Yiu RY, Lee JF, et al. Systemic cytokine response after laparoscopic-assisted resection of rectosigmoid carcinoma: a prospective randomized trial. Ann Surg. 2000;231:506–511. doi: 10.1097/00000658-200004000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ahlers O, Nachtigall I, Lenze J, Goldmann A, Schulte E, Höhne C, et al. Intraoperative thoracic epidural anaesthesia attenuates stress-induced immunosuppression in patients undergoing major abdominal surgery. Br J Anaesth. 2008;101:781–787. doi: 10.1093/bja/aen287. [DOI] [PubMed] [Google Scholar]
- 150.Sun HZ, Song YL, Wang XY. Effects of different anesthetic methods on cellular immune and neuroendocrine functions in patients with hepatocellular carcinoma before and after surgery. J Clin Lab Anal. 2016;30:1175–1182. doi: 10.1002/jcla.22000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Yeh CN, Lee HL, Liu YY, Chiang KC, Hwang TL, Jan YY, et al. The role of parenteral glutamine supplement for surgical patient perioperatively: result of a single center, prospective and controlled study. Langenbecks Arch Surg. 2008;393:849–855. doi: 10.1007/s00423-008-0405-4. [DOI] [PubMed] [Google Scholar]
- 152.Chen DW, Wei Fei Z, Zhang YC, Ou JM, Xu J. Role of enteral immunonutrition in patients with gastric carcinoma undergoing major surgery. Asian J Surg. 2005;28:121–124. doi: 10.1016/s1015-9584(09)60275-x. [DOI] [PubMed] [Google Scholar]
- 153.Watt SK, Hasselbalch HC, Skov V, Kjær L, Thomassen M, Kruse TA, et al. Whole blood gene expression profiling in patients undergoing colon cancer surgery identifies differential expression of genes involved in immune surveillance, inflammation and carcinogenesis. Surg Oncol. 2018;27:208–215. doi: 10.1016/j.suronc.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 154.Allen CJ, Griswold AJ, Schulman CI, Sleeman D, Levi JU, Livingstone AS, et al. Global gene expression change induced by major thoracoabdominal surgery. Ann Surg. 2017;266:981–987. doi: 10.1097/SLA.0000000000001992. [DOI] [PubMed] [Google Scholar]
- 155.Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Newman AM, Liu CL, Green MR, Gentles AJ, Feng W, Xu Y, et al. Robust enumeration of cell subsets from tissue expression profiles. Nat Methods. 2015;12:453–457. doi: 10.1038/nmeth.3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Altman DG, McShane LM, Sauerbrei W, Taube SE. Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK): explanation and elaboration. PLoS Med. 2012;9:e1001216. doi: 10.1371/journal.pmed.1001216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open. 2016;6:e012799. doi: 10.1136/bmjopen-2016-012799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Welsch T, Müller SA, Ulrich A, Kischlat A, Hinz U, Kienle P, et al. C-reactive protein as early predictor for infectious postoperative complications in rectal surgery. Int J Colorectal Dis. 2007;22:1499–1507. doi: 10.1007/s00384-007-0354-3. [DOI] [PubMed] [Google Scholar]
- 160.Lee K, Hwang H, Nam KT. Immune response and the tumor microenvironment: how they communicate to regulate gastric cancer. Gut Liver. 2014;8:131–139. doi: 10.5009/gnl.2014.8.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kim CH, Park SM, Kim JJ. The impact of preoperative low body mass index on postoperative complications and long-term survival outcomes in gastric cancer patients. J Gastric Cancer. 2018;18:274–286. doi: 10.5230/jgc.2018.18.e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Seo HS, Jung YJ, Kim JH, Park CH, Kim IH, Lee HH. Long-term nutritional outcomes of near-total gastrectomy in gastric cancer treatment: a comparison with total gastrectomy using propensity score matching analysis. J Gastric Cancer. 2018;18:189–199. doi: 10.5230/jgc.2018.18.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Lee HJ, Hyung WJ, Yang HK, Han SU, Park YK, An JY, et al. Short-term outcomes of a multicenter randomized controlled trial comparing laparoscopic distal gastrectomy with D2 lymphadenectomy to open distal gastrectomy for locally advanced gastric cancer (KLASS-02-RCT) Ann Surg. 2019 doi: 10.1097/SLA.0000000000003217. [DOI] [PubMed] [Google Scholar]
- 164.Kim HH, Han SU, Kim MC, Kim W, Lee HJ, Ryu SW, et al. Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage I gastric cancer: The KLASS-01 Randomized Clinical Trial. JAMA Oncol. 2019;5:506–513. doi: 10.1001/jamaoncol.2018.6727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Desiderio J, Stewart CL, Sun V, Melstrom L, Warner S, Lee B, et al. Enhanced recovery after surgery for gastric cancer patients improves clinical outcomes at a US Cancer Center. J Gastric Cancer. 2018;18:230–241. doi: 10.5230/jgc.2018.18.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mortensen K, Nilsson M, Slim K, Schäfer M, Mariette C, Braga M, et al. Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Br J Surg. 2014;101:1209–1229. doi: 10.1002/bjs.9582. [DOI] [PubMed] [Google Scholar]