Abstract
Diet-based chemoprevention of cancer has emerged as an interesting approach to evade the disease or even target its early phases, reducing its incidence or slowing down tumor progression. In its basis in the essential role of angiogenesis for tumor growth and metastasis, angioprevention proposes the use of inhibitors of angiogenesis in cancer prevention. The anti-angiogenic potential exhibited by many natural compounds contained in many Mediterranean diet constituents makes this dietary pattern especially interesting as a source of chemopreventive agents, defined within the angioprevention strategy. In this review, we focus on natural bioactive compounds derived from the main foods included in the Mediterranean diet that display anti-angiogenic activity, as well as their possible use as angiopreventive agents.
Keywords: angiogenesis, cancer, chemoprevention, angioprevention, Mediterranean diet, bioactive compounds
1. Angiogenesis and Cancer
1.1. Angiogenesis as a Regulated Process
Angiogenesis, the neoformation of vessels from an existing vascular bed, is an important process during development; however, in adulthood most of the blood vessels remain largely quiescent, with some physiological exceptions, such as wound healing, ovulation and tissue repair. Angiogenic phenomena are crucial for normal physiological functions and must be carefully controlled to maintain healthy conditions. Therefore, it is not surprising that a deregulated angiogenesis plays an essential role in multiple pathological situations, including atherosclerosis, diabetic retinopathy, rheumatoid arthritis, macular degeneration, psoriasis, tumor growth, metastasis, and chronic inflammation [1].
The multistep process of angiogenesis starts with the vasodilation and increased permeability of existing vessels, endothelial cell activation and proliferation in response to angiogenic factors. Thereafter, the degradation of the capillary wall by extracellular proteinases occurs, followed by migration of endothelial cells, formation of new capillaries, and finally, the interconnection of the new vessels (anastomosis) and their stabilization by recruitment of pericytes [2]. All these steps are controlled by a tight balance, both spatially and temporally, between activators (growth factors, i.e., vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), platelet-derived growth factor (PDGF), a plethora of cytokines, bioactive lipids, matrix-degrading enzymes, and a number of small molecules) and inhibitors (angiostatin, interferons, endostatin, IL-12 and retinoids) that execute their function through different signaling pathways [3].
1.2. Angiogenesis as a Hallmark of Cancer
Cancer represents a leading cause of death in the developed world. Although massive efforts and investments have been made in cancer therapy to successfully treat localized tumors, medicine is nonetheless often helpless in the treatment of metastatic processes. Despite the huge diversity of oncologic diseases, all of them share some fundamental features, pointed out by Hanahan and Weinberg as “hallmarks of cancer” [4,5]. Interestingly, one of them is angiogenesis induction, since a persistently activated and deregulated angiogenesis is essential for tumor growth and metastasis. It is widely accepted that proliferating tumor cells need host support, including the connection of the so-called “angiogenic switch”. Activation of angiogenesis can occur at any step of the tumor progression and depends on the type of tumor and its microenvironment. For instance, many tumors start growing in an avascular phase until reaching a steady state within the proliferating cells. At this stage, the “angiogenic switch” activates endothelial cells to undergo a series of phenotypic changes to finally differentiate into a new vessel. Angiogenesis is therefore a rate-limiting step in progression to solid tumor malignancy. Blood vessels supply nutrients and oxygen, and serve as a route for the elimination of waste, contributing to exponentially enhance the tumor growth. Additionally, the new vasculature also provides a pathway for tumor cells to escape from the primary tumor, invade nearby tissues, move throughout the body, and colonize distant organs, giving rise to metastasis [6].
Tumor angiogenesis significantly differs from physiological angiogenesis. The newly-formed vasculature is aberrant, with altered interactions between endothelial cells and pericytes, abnormal blood flow, and increased permeability—all due to a chaotic and poorly-regulated expression of pro- and antiangiogenic factors. As a consequence, tumor vessels are often disorganized, incomplete, lacking structural integrity, and prone to collapse, resulting in areas of inadequate perfusion and transient hypoxia [7].
Angiogenesis has been defined as an “organizing principle” in biology, allowing connections between unrelated phenomena. Favoring therapies initially designed for the treatment of cancer could be used to treat other non-neoplastic angiogenesis-dependent diseases, including age-related macular degeneration, some retinopathies, psoriasis, or rheumatoid arthritis, among others [8].
1.3. Antiangiogenic Therapies in Cancer
The early hypothesis by Judah Folkman in 1971 that tumor dormancy could be maintained by preventing neovascularization of microscopic cancers could not be clinically validated until 2004, when the first antiangiogenic drug received the U.S. Food and Drug Administration (FDA) approval for the treatment of cancer patients [9,10]. Although many questions still remain unanswered, accumulating clinical evidence of antiangiogenic therapies in extending survival in cancer patients make antiangiogenesis one of the most promising anticancer targets [11]. Antiangiogenic inhibitors are unique cancer-fighting agents that can block the growth of blood vessels that support tumor growth rather than interfering with the growth of tumor cells themselves. Over the last decades, angiogenesis has become an appealing target in cancer therapy, being of great interest in the fields of pharmacology and drug discovery. Angiogenesis inhibitors can interfere with one or various steps of the blood vessel growth [10]. This has favored a continuous growth of antiangiogenic drugs in the cancer field, with a myriad of molecules being evaluated in preclinical studies and several hundred reaching clinical trials [12]. Importantly, several compounds have been already approved by the FDA, and they are registered for the clinical treatment of different tumors (Table 1). This list includes humanized antibodies such as bevacizumab or ramucirumab, fusion proteins such as aflibercept, and low molecular weight molecules, including sorafenib, sunitinib, or vandetanib, among others (recently reviewed in [13,14,15]).
Table 1.
Antiangiogenic drugs approved by Food and Drug Administration (FDA)/ European Medicines Agency (EMA) for the treatment of solid tumors. Referenced from [13,14,15].
| Drug | Type | Molecular Target | Malignancies |
|---|---|---|---|
| Axitinib (Inlyta) |
TKI | VEGFR-1-3, PDGFRβ |
Advanced RCC |
| Bevacizumab (Avastin) |
Humanized monoclonal antibody | VEGF | MCRC, NSCLC, OC, MBC, glioblastoma, metastatic RCC, endometrial cancer, Mesothelioma, and cervical cancers |
| Cabozantinib (Cometriq) |
TKI | VEGFR-2, Tie2 |
Refractory advanced RCC, metastatic medullary TC, and pancreatic neuroendocrine tumors |
| Cediranib | TKI | VEGFR-1-3 | OC |
| Everolimus (Afinitor) |
TKI | mTOR | RCC, gastrointestinal cancer, lung carcinoma, advanced breast cancer, pancreatic neuroendocrine tumors (PNETs), and subependymal giant cell astrocytoma |
| Lenalidomide (Revlimid) |
Amino acid | VEGF, bFGF | Myeloma (myelodysplastic syndrome (MDS)) and mantle cell lymphoma |
| Levantinib (Lenvima) |
TKI | VEGFR-1-3, PDGFRα, FGFR-1-4 |
TC, HCC, and RCC |
| Pazopanib (Votrient) |
TKI | VEGFR-1-3, PDGFRβ, FGFR-1-2 |
Metastatic STC and advanced RCC |
| Ramucirumab (Cyramza) |
Human monoclonal antibody | VEGFR-2 | MCRC, NSCLC, and gastric adenocarcinoma |
| Regorafenib (Stivarga) |
TKI | VEGFR-1-3, PDGFRβ, FGFR-1-2 |
Chemo-refractory MCRC, unresectable HCC, and GIST |
| Sorafenib (Nexavar) |
TKI | VEGFR-2, PDGFRβ |
Advanced RCC, metastatic differentiated TC, and unresectable HCC |
| Sunitinib (Sutent) |
TKI | VEGFR-1-2, PDGFRσ/β |
Metastatic RCC, gastrointestinal stromal tumors, and pancreatic neuroendocrine tumors |
| Thalidomide (Synovir, Thalomid) |
Amino acid | VEGF, bFGF | Multiple myeloma |
| Temsirolimus (Torisel) |
TKI | mTOR | RCC |
| Vandetanib (Caprelsa) |
TKI | VEGFR-2 | Unresectable or metastatic TC |
| Ziv-Aflibercept (VEGF-Trap) (Zaltrap) |
Fusion protein (VEGFR chimera) |
VEGF-A/B, PlGF |
MCRC |
VEGF (vascular endothelial growth factor), VEGFR (vascular endothelial growth factor receptor), bFGF (basic fibroblast growth factor), FGFR (fibroblast growth factor receptor), PDGFR (platelet-derived growth factor receptor), mTOR (mammalian target of rapamycin), PlGF (placental growth factor), TKI (tyrosine kinase inhibitor), MCRC (metastatic colorectal carcinoma), NSCLC (non-small cell lung cancer), OC (ovarian cancer), MBC (metastatic breast cancer), RCC (renal cell carcinoma), HCC (hepatocellular carcinoma), GIST (gastrointestinal stromal tumor), TC (thyroid carcinoma), STC (soft tissue carcinoma).
Clinical data have shown that angiogenesis inhibitors appear to be most effective when used in combination with other antiangiogenic or traditional anticancer therapies [16], probably due to a “normalization” of tumor vasculature that could help drugs to penetrate the mass and to function more effectively [17]. Nowadays, the use of antiangiogenic strategies is being actively explored to increase the effectiveness and diminish the risk of immune-related adverse effects of immunotherapy, a major therapeutic modality that is revolutionizing the treatment of cancer [18].
2. Angioprevention
In the last decades, many research efforts have focused on cancer chemoprevention, a concept firstly defined by Michael B. Sporn in 1976 as the use of natural, synthetic, or biologic agents to prevent, suppress, or reverse tumor progression [19]. Whereas early detection of cancer is a broadly accepted approach, cancer chemoprevention is still a matter of debate in the scientific community, mainly due to the controversial results obtained in some reported preventive interventions [20]. Cancer chemoprevention approaches are based in the interference of one or several of the hallmarks of cancer-using drugs that could slow down the initiation and progression of tumors. In this context, the concept of angioprevention, firstly coined by Adriana Albini and colleagues, arose as the prevention of cancer by inhibition of tumor angiogenesis [21]. Angioprevention applies angiogenesis inhibition to those predisposing conditions, including chronic inflammation, pre-neoplastic or hyperplastic lesions, and microscopic tumors, so that modulation of the tumor microenvironment could help the host defense systems to more efficiently avoid the development of clinically detectable tumors [22].
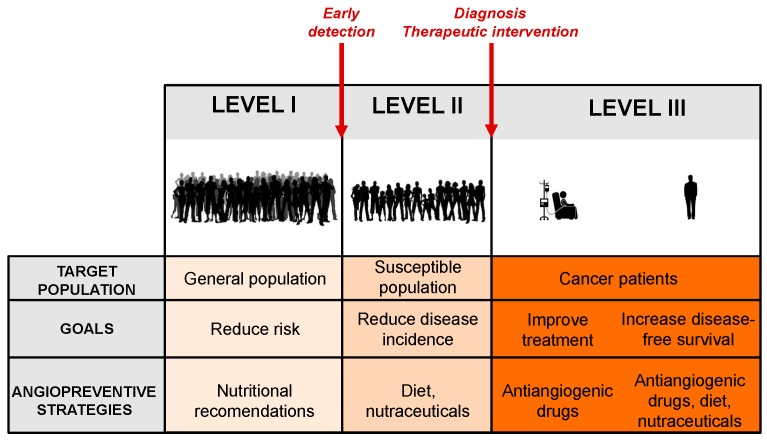
There are different levels at which the cancer preventive action could be implemented, depending on the targeted population (Figure 1) [23].
Figure 1.
The three levels of cancer chemoprevention. The figure represents the three levels at which cancer preventive action could be implemented, showing the targeted population, the main goals, and the angiopreventive strategies at each level.
The primary prevention stage is focused on decreasing the incidence of disease in a broad healthy population, mainly by reducing the exposure to carcinogenic factors or by increasing the individuals’ resistance to them. Possible interventions include nutritional recommendations, dietary supplements, and natural inhibitors of angiogenesis, which could help to stop early events in tumorigenesis. The primary preventive agents group also includes all supplements able to induce the intrinsic properties that suppress blood vessel formation by endogenous angiogenesis inhibitors present within the host microenvironment (endostatin, thrombospondin-1, angiostatin, and many others) [2].
Secondary prevention is directed at reducing the mortality from a particular cancer in higher-risk populations, with actions focused on early detection and treatment in the subclinical stages of the disease before symptoms appear. The high-risk population is composed of individuals with genetic abnormalities, usually associated with their lifestyle, specific syndromes, or family history. Improvement in the screening programs and the diagnostic tests will facilitate the early detection of tumors or pretumoral lesions. Inhibitors of angiogenesis may provide a valuable tool to prevent the growth of undetectable primary tumors in this population, a concept that was implicit in Judah Folkman’s visionary idea [9]. For secondary prevention of cancer, a number of natural or synthetic antiangiogenic compounds are available, including fumagillin, fumagillol, genistein, or difluoromethylornithine, among many others [10]. Because of the long-term nature of the earlier preventive strategies, these compounds should be fulfilled with some premises, namely minimal toxicity, low cost price, and capability to promote the physiological anti-tumoral responses of the tumor microenvironment [22].
Tertiary prevention is directed to cancer patients in more advanced stages of the disease and is aimed at improving the oncologic treatment results, their survival rate, and their quality of life. Preventive actions at this level include prevention of recurrence of a pre-existing cancer and the development of new secondary tumors. In this scenario, an aggressive and sustained chemopreventive approach may be required, as tumor cell dissemination is likely to exist. Tertiary prevention could include antiangiogenic cancer agents already approved by the regulatory agencies (Table 1), and others under clinical trials, used either along or after the treatment in order to prevent a relapse. In any case, more sustainable and less aggressive antiangiogenic strategies, such as those used for primary and secondary prevention, could also be of application for cancer patients in order to halt the growth of those undetectable microscopic metastasis that could remain after primary tumor resection.
Increasing evidence supports the angioprevention approach in preclinical models, as well as in epidemiological and clinical intervention studies in humans [24]. The availability of antiangiogenic molecules in dietary sources suggests that a rationally designed antiangiogenic diet could be a natural and cost-effective strategy for cancer prevention [25].
3. The Mediterranean Diet: A Cultural Heritage of Humanity
The influence of diet and diet components in health is currently an open study question. Among the known dietary models, the Mediterranean diet (MD) stands out. In as early as 1980, Ancel Keys reported in his Seven Countries Study that the MD was associated with lower risk of major chronic diseases and highest life expectancies [26]. Extended from centuries in the civilizations along the Mediterranean coast, the MD is mainly characterized by the general intake of fruits and vegetables, legumes, cereals, dried fruits, and nuts, together with a low consumption of red meat, low/moderate intake of dairy products, and moderate/high consumption of fish, seasoned by the daily intake of a low quantity of red wine with meals [27]. Although specific MD components exhibit some differences depending on the country, all the observed variants share a common component, that is, the use of virgin olive oil as main addition fat. However, diet components are not the only elements that define the MD, as this ancient dietary pattern—transmitted through generations—includes social and cultural aspects that make it a marker of identity of people who live in the Mediterranean basin, up to the point that the MD was included in 2013 in the Representative List of the Intangible Cultural Heritage of Humanity of UNESCO (United Nations Educational, Scientific and Cultural Organization) [28].
Despite the extended and ancient tradition of the MD in Mediterranean countries, in the last decades, the adherence to this diet has experienced a marked decline, turning to a dietary pattern closer to the western diet model (essentially the nemesis of MD, mainly characterized by the high intake of saturated fats, highly processed foods, regular consumption of red meat, high presence of added-sugar products, and low presence of vegetables, fruits, and fiber [29,30]). Suggested explanations of this so-called “westernization” process point to a rise in the availability of non-Mediterranean food products, together with socioeconomic factors such as the increasing prices of typical products of the MD [31,32]. Unlike this observed negative tendency, the evidence of the health benefits derived from the MD has sparked the interest of the scientific community. Indeed, MD adherence is related to a lower incidence of cardiovascular diseases, as was firstly reported in the Seven Countries Study and confirmed later by many other studies [33,34,35,36,37]. Besides its cardioprotective effects, MD has been associated with a lower risk of certain types of cancer and a decreased total cancer mortality [38,39,40,41], although a higher number of studies are needed to undoubtedly establish this relationship. Indeed, a recent exhaustive umbrella review of meta-analyses of observational studies and randomized trials evidenced that adherence to MD is related to a reduction in cancer incidence, with its role in overall cancer mortality still weakly suggested by current data [42].
The precise molecular mechanism responsible for the effects of MD in health is currently under research. At a molecular level, MD components include a high number of bioactive compounds, with it being difficult to define the precise contribution of any of them. In general, it has been suggested that the combination of components of the diet essentially exert a complex common role in reducing inflammation and oxidative stress, therefore counteracting the progress of several malignancies, including cardiovascular diseases and cancer [43]. It is noteworthy that MD adherence has revealed a protective role against these and many other of the most prevalent diseases [42], connecting this dietary pattern to chemoprevention. The cardioprotective role of MD is rather well defined, since its beneficial influence on traditional atherosclerotic and cardiovascular risk factors has been proven [44,45,46,47]. In contrast, the chemopreventive effect of this dietary pattern on cancer is still misunderstood, although encouraging studies point to the risk-reducing effect of the MD on certain types of cancer, as is the case of breast and colorectal cancer [39,48,49,50,51]. In this context, angioprevention is an important concept to take into account, since angiogenesis prevention through bioactive compounds present in the MD components could explain in part the chemopreventive effect of this diet model in cancer. By extension, angioprevention derived from the MD would be interesting in the prevention of other angiogenesis-dependent diseases, such as diabetic retinopathies or atherosclerosis. In this review, we propose an angiopreventive role of some of the most distinctive components of MD, based on their content of bioactive compounds exhibiting antiangiogenic properties.
4. Olive Oil as a Source of Antiangiogenic Molecules
Despite the differences in the components of MD depending on the country, the use of olive oil in cooking and seasonings could be considered the most remarkable common denominator of the diet. It is noteworthy that the health effects of olive oil in several pathologies have been long recognized [52]. Olive oil is defined as oil extracted from the fruit of olive trees (Olea europaea sativa). Depending on the degree of processing, olive oils can be classified into different categories. Virgin olive oils are obtained solely by mechanical means that do not lead to alterations in the oil, with extra virgin olive oil being the one of highest quality. Oils simply labelled as “olive oil” have normally been subjected to a refinement process [53].
Olive oil contains a complex mixture of different types of compounds, whose proportion will vary depending on the type of olive, maturation, growing conditions, storage, extraction method, and refinement degree [53,54,55]. In general, olive oil components fall into the saponifiable fraction (98–99% w/w) or the unsaponifiable fraction (1–2% w/w). The saponifiable fraction consists mainly of triglycerides, although diglycerides, monodiglycerides, and free fatty acids are also found in a much smaller proportion. The main triglyceride fatty acid in this fraction is oleic acid, representing 55–83% of the total fatty acid content. In the unsaponifiable fraction, a greater diversity of compounds are found, responsible for stabilizing and protecting the olive oil integrity, preserving its organoleptic characteristics [56]. In this fraction, mainly hydrocarbons, tocopherols, pigments, sterols, triterpene acids, volatile compounds, and phenolic compounds are included. Among them, phenolic compounds of olive oil (including simple phenols, flavonoids, secoiridoids, and lignans) have shown interesting biological activities [55,57]. Extra virgin olive oil shows the highest content of phenolic compound, which are almost absent in refined oils as they are lost during the refinement process [58].
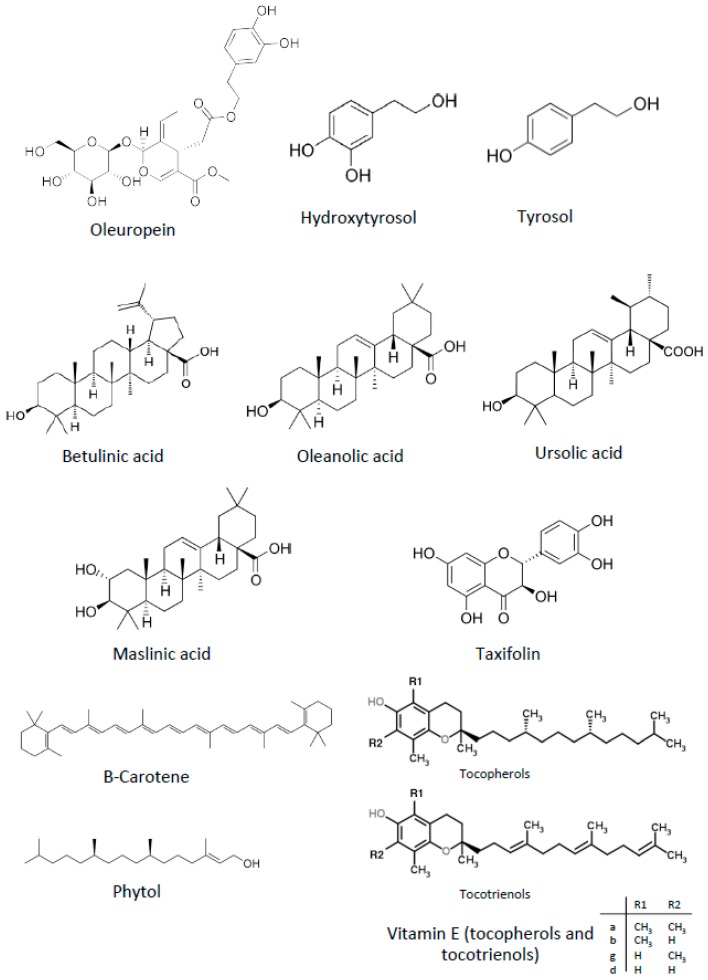
Although traditionally the health effects of olive oil were attributed to its high content in oleic acid, nowadays a high number of scientific studies has demonstrated that these effects must be also attributed to some minority compounds of olive oil, especially those included in the phenolic fraction [59]. Among other multiple biological activities, antiangiogenic properties have been reported for some compounds present in the olive oil, shown in Figure 2 and presented below.
Figure 2.
Chemical structures of antiangiogenic compounds present in extra virgin olive oil.
4.1. Oleuropein
Oleuropein, a secoiridoid present in olive oil, has been proposed to be a chemopreventive agent, based on its capability to modulate several oncogenic signaling pathways [60]. Regarding angiogenesis, it inhibits VEGFR-2 autophosphorylation at specific sites (Tyr951, Tyr1059, Tyr1175 and Tyr1214), suppressing the VEGF-induced proliferation and migration of macrovascular and microvascular human endothelial cells, as well as their morphogenic differentiation into tubular-like structures in Matrigel [61]. The antiangiogenic activity of this compound could be associated with the inhibition of PMA-induced COX-2 expression, and the decrease in MMP-9 protein release and gelatinolytic activity [62].
During olive ripening, the enzyme β-glucosidase transforms oleuropein into oleuropein aglycone, which by hydrolysis renders elenolic acid and hydroxytyrosol, an interesting bioactive compound that is discussed below.
4.2. Hydroxytyrosol
Hydroxytyrosol (2-(3,4-dihydroxyphenyl) ethanol) and tyrosol (2-(4-hydroxyphenyl) ethanol) are the most abundant simple phenols contained in olive oil, also being the major phenolic constituents of wine. Both compounds derive from the natural hydrolysis of the aglycone form of oleuropein and ligstroside, respectively, during olive maturation. In addition to other biological activities, including antitumoral, antiinflammatory, cardio-, and neuroprotective activities, hydroxytyrosol has been shown to inhibit angiogenesis in vitro and in vivo [63,64,65,66,67]. In vitro assays evidenced that hydroxytyrosol is able to inhibit the endothelial cell growth, migration, and tubular-like structures formation. The effect on the endothelial proteolytic balance was demonstrated by a decrease in the release of MMP-2 and MMP-9 by endothelial cells. Ex vivo (rat aortic ring) and in vivo (CAM) angiogenesis assays supported the antiangiogenic activity of hydroxytyrosol [66], which could be related to the inhibition of COX-2 and VEGFR-2 phosphorylation [61,67]. Recently, the antiangiogenic activity of synthetic molecules derived from hydroxytyrosol has been described, showing that chemical modifications in the original molecule may improve the bioactivity of the natural compound, therefore reinforcing their utility as angiopreventive compounds [68]. In contrast with the antiangiogenic activity described for hydroxytyrosol, the closely related compound tyrosol, also present in olive oil, did not show capability to inhibit angiogenesis in vitro [66].
4.3. Triterpene Acids
Pentacyclic triterpenes, such as betulinic, oleanolic, ursolic, and maslinic acids, are present in olives, olive tree leaves, and virgin olive oil. There is a large amount of literature that clearly illustrates the significant anti-neoplastic effects of triterpenes, exhibiting multiple biological and pharmacological properties.
Betulinic acid inhibited in vitro the bFGF-induced invasion and the tubular-like structure formation of bovine aortic endothelial cells (BAECs) [69]. This activity has been related to the activation of the proteasome-dependent degradation of the transcription factors, specifically protein Sp1, Sp3, and Sp4, which also regulate VEGF expression [70].
Oleanolic acid, also present in several traditionally-used plants used to treat cancer, is considered to be a chemopreventive compound, probably due to its capability to suppress multiple molecular targets involved in both the development and progression of cancer [71]. Oleanolic acid inhibits angiogenesis in vivo and in vitro via suppression of STAT3 and Hedgehog pathways, which could be one of the underlying mechanisms of its antitumoral effect [72]. Inhibition of VEGFR-2 signaling pathway has been recently linked to the antiangiogenic activity of this compound [73].
Ursolic acid antitumor activity has long been recognized, probably being responsible for the anticancer properties of some plants used in Chinese traditional medicine. The antiangiogenic activity of ursolic acid was evidenced by the early observation that it interfered several steps of the angiogenic process in vitro [74], later being characterized as an inhibitor of multiple signaling pathways controlling cancer growth and angiogenesis [75], including that of HIF-1α [76]. In addition, studies of the ursolic acid biodisponibility after oral administration in mice, and the toxicity, pharmacokinetic, and pharmacodynamics of liposomal ursolic acid in humans have shown promising results, supporting its use in cancer chemoprevention [77]. Extensive effort is being devoted to the synthesis of more effective ursolic acid derivatives with improved chemopreventive potential [78,79].
Maslinic acid, aside from its anti-oxidant, anti-inflammatory, and anti-viral activities, exhibits significant anticancer and antiangiogenic properties that could be mediated by the decrease in the expression levels of NF-κB-regulated genes. These include genes involved in tumor cell proliferation (Cyclin D1, COX-2, and c-Myc), apoptosis (Survivin, Bcl-2, Bcl-xl, XIAP, and IAP-1), invasion (MMP-9 and ICAM-1), and angiogenesis (VEGF) [80].
The pharmacological relevance of all the aforementioned activities of the natural triterpenes found in olive oil has fueled the interest either in the synthesis of new synthetic derivatives with higher potency and efficacy, or in the development of new delivery approaches that could increase the therapeutic potential of those compounds [81,82], which could be better used in the angioprevention of cancer.
4.4. Other Antiangiogenic Compounds Present in Olive Oil
The antineoplastic properties of some other compounds found in olive oil have been described, many of them also exhibiting antiangiogenic activities. They include flavonoids, carotenoids, vitamin E, diterpenoids, and sterols (Figure 2).
Taxifolin, a flavanonol (flavonoid) present in olive oil, inhibits the in vitro formation of tubular-like endothelial cell structures on Matrigel, as well as the in vivo formation of new blood vessels in the CAM and the murine dorsal skinfold chamber models [83]. Mechanistically, the antiangiogenic activity of taxifolin could be due to the inhibition of the autophosphorylation of several tyrosine residues in VEGFR-2 [61].
Carotenoids are C40 tetraterpenoids, a widely distributed group of lipid-soluble pigments found in vegetables and fruits. Olive oil contains several types of carotenoids, with lutein and β-carotene being the main compounds present. The antiangiogenic potential of β-carotene has been demonstrated by means of the rat aorta ex vivo and murine in vivo assays. This pigment has been described to inhibit—in vitro—endothelial proliferation, migration, and tube formation. β-Carotene downregulates the expression of MMP-2, MMP-9, prolyl-hydroxylase, and lysyl-oxidase, and upregulates the expression of the tissue inhibitors of metalloproteinases TIMP-1 and TIMP-2 [84]. Dietary lutein inhibits mammary tumor growth by induction of apoptosis in tumor cells, and inhibition of angiogenesis [85]. Since lutein/zeaxanthin is the eye macular pigment, an adequate intake of lutein-rich foods could also be recommended to the general population in order to reduce the progression of age-related macular eye disease and cataracts [86].
Vitamin E now refers to eight different isoforms that belong to two categories, tocopherols (four saturated analogues, α, β, γ, and δ), and tocotrienols (four unsaturated analogues), with all these compounds beiing found in virgin olive oil [87]. Tocotrienol, but not tocopherol, inhibits both the proliferation and tube formation of BAECs. The most active compound is δ-tocotrienol, which inhibits proliferation, migration, and tube formation of human endothelial cells at low micromolar doses, whereas similar doses of α-tocopherol did not show any effect [88,89]. Mechanistically, downregulation of VEGF expression, suppression of VEGFR-2 signaling, and activation of apoptosis in endothelial cells could be behind the antiangiogenic activity of this compound, confirmed in vivo by the CAM and the Matrigel plug assays [87,89,90].
Although less characterized, a putative antiangiogenic potential for the acyclic diterpenoid phytol, and campesterol and β-sitosterol—two components of sterol fraction of olive oil—has been suggested [91,92,93].
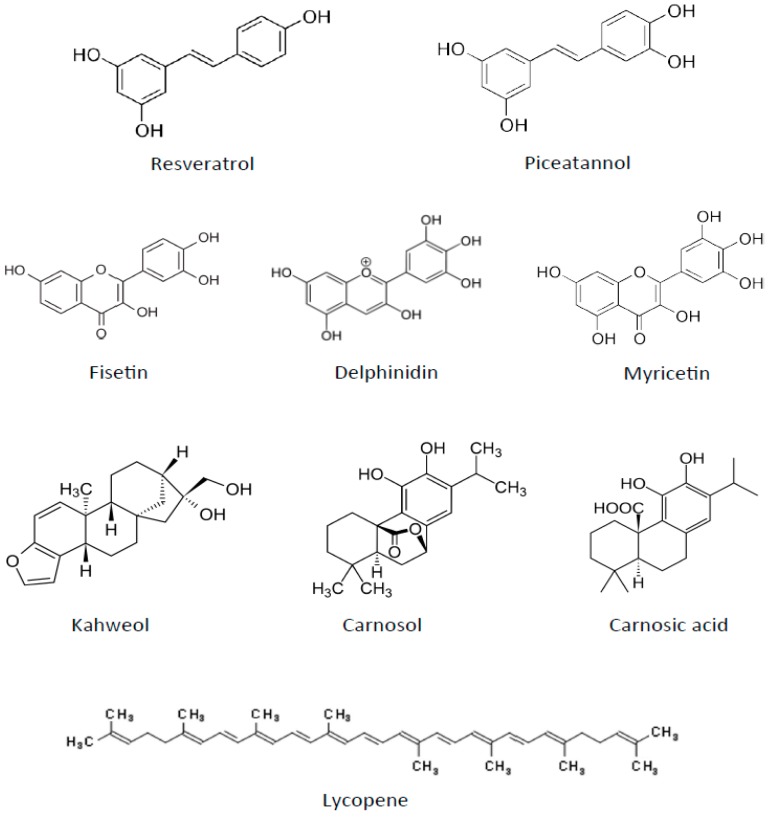
5. Antiangiogenic Polyphenols from Fruits and Red Wine
The MD is characterized by a high consumption of fruits and vegetables. It may also include having a glass of wine with lunch every day—mainly red wine, which has been shown to exert a positive influence upon health. Several non-alcoholic components of wine, mainly polyphenols, which are also present in grapes and other fruits, may be responsible for a considerable part of the reported cardioprotective effects of a moderate wine intake [94]. Red wine polyphenolic compounds also exhibit antitumoral activities, which could be, at least in part, mediated by their antiangiogenic activity [95]. Some of these compounds are presented here (Figure 3).
Figure 3.
Chemical structures of other antiangiogenic compounds present in the Mediterranean diet (MD) components.
5.1. Resveratrol
Resveratrol (3,4′,5-trans-trihydroxystilbene) is a non-flavonoid polyphenol contained in the skin of red grapes, but also found in peanuts and berries. It is probably the most studied red wine polyphenol, and it presents a clear antiangiogenic activity mediated by the inhibition of VEGF expression in tumor cells and by suppressing the endothelial cell response to this angiogenic factor [96,97]. Unlike this antiangiogenic role of resveratrol in cancer, this compound has been described as proangiogenic in some diseased contexts with defective vascularization [98,99,100]. This dual effect of resveratrol could be due to a dose-response activity, since high concentrations of resveratrol induce angiogenesis, whereas low doses are antiangiogenic [101]. The exact mechanisms of the antiangiogenic activity of this compound are not yet completely unraveled, although the modulation of the VEGF/VEGFR-2 pathway through several axes (HIF-1α and GSK3b/β-catenin/TCF) could be in the basis of this effect [102,103,104]. In vitro studies show that trans-resveratrol is the most active stereoisomer [105]. Because of the pharmacological interest of resveratrol, derivatives with improved antiangiogenic activity have been synthetized [106].
5.2. Piceatannol
Piceatannol (3,3′,4,5′-tetrahydroxystilbene), a natural occurring stilbene found in grapes and red wine, is a metabolite derived from resveratrol through the activity of the cytochrome P4501B1 enzyme [107]. This compound confers cardiovascular disease protection, preventing atherosclerosis [108], as well as exhibiting anti-aging, anti-inflammatory, anti-diabetic, and anti-tumoral activity [109]. Focusing on its antiangiogenic effects, piceatannol was found to inhibit the in vitro tubular-like structure formation by endothelial cells, most likely by the inhibition of the spleen tyrosine kinase [110]. Piceatannol was also found to decrease the levels of some pro-angiogenic and pro-lymphangiogenic factors, such as VEGF-A, VEGFR-2, VEGF-C, and LYVE-1, through modulation of NF-κB and STAT3 transcription factors in breast cancer in vivo, and diminished macrophage infiltration in tumor tissue via attenuating the MCP-1 and M-CSF chemoattractants [111].
5.3. Fisetin
Fisetin (3,3′,4′,7-tetrahydroxyflavone) is a bioactive flavonol found in wine, as well as in several fruits (strawberries, apples, mangoes, persimmons, kiwi, and grapes), vegetables (tomatoes, onions, and cucumbers) and nuts. This compound exhibits a multiple bioactive role in chronic diseases, showing anti-inflammatory, antidiabetic, antioxidant, antitumorigenic, antiinvasive, antiangiogenic, neuroprotective, and cardioprotective effects [112]. The inhibition of in vivo and in vitro angiogenesis by this compound suggests its angiopreventive potential [113]. Fisetin has been reported to decrease ADAM9, a disintegrin and metalloproteinase implied in tumorigenesis and angiogenesis, with this reduction being related to the inhibition of migration and invasion in glioma cells [114]. Indeed, fisetin diminishes VEGF expression in lung adenocarcinoma cells via a HIF-1α independent mechanism [115]. Inhibition of migration and invasion has also been seen in melanoma cells through reduction of MAPK and NFκB signaling pathways, and could be related to the observed disruption of angiogenesis in xenograft melanoma tumors [116,117]. However, the effects of fisetin are not exclusive to tumor cells, since this flavonoid causes microtubule stabilization in endothelial cells [118], that could be, at least partially, the cause of the observed inhibition of migration and tube formation of endothelial cells in vitro, and of the reduction on microvessel density in lung adenocarcinoma tumors [119].
5.4. Delphinidin
The antiangiogenic activity of delphinidin (3,3′,4′,5,5′,7-hexahydroxyflavylium), an anthocyanin present in red wine and in many pigmented fruits and vegetables, has been clearly demonstrated by a number of in vitro assays showing inhibitory effects on proliferation, migration, and tube formation by endothelial cells. This activity was confirmed in vivo by the CAM and the Matrigel plug models [120,121]. This activity has been linked to a blockade of VEGF and PDGF-signaling pathways [121,122], although recent results have indicated that it could be also mediated by inhibition of HIF-1α and VEGF expression in tumor cells [123].
5.5. Myricetin
Myricetin (3,3′,4′,5,5′,7-hexahydroxyflavone) is a flavonoid found in red wine and grapes, onions, and berries, with an interesting potential in chemoprevention of skin cancer [124]. With a similar chemical structure to that of delphinidin, its role as an angiogenesis inhibitor has been studied in different cancer types, being reported to inhibit the PI3-K/Akt pathway, both in tumor and endothelial cells [125]. Moreover, in a mouse model of skin tumorigenesis, myricetin inhibited UVB-induced angiogenesis, decreasing VEGF, HIF-1, MMP-2, MMP-9, and MMP-13 expression [126,127].
6. Other Components of the MD with Angiopreventive Potential
6.1. Fish
One of the characteristics of the MD is the high intake of oily cold-water fish, including sardines, tuna, mackerel, and anchovies. These all are known to contain high amounts of omega-3 fatty acids—long-chain polyunsaturated fatty acids with the first double bond three carbons from the methyl end of the chain. Humans cannot desaturate this double bond, and hence omega-3 fatty acids are essential and must be included in the diet, with their consumption being advisable instead of that of omega-6 fatty acids in order to prevent the onset of several types of cancer [128,129,130].
The beneficial effects of omega-3 fatty acids could be related to their inhibitory effects on angiogenesis, either by a direct antiangiogenic activity, or by a reduction of the levels of angiogenic factors and their receptors. In this regard, eicosapentanoic acid and derivatives have been shown to inhibit some angiogenic characteristics, such as tube formation, migration, metalloproteinase expression, and VEGFR-2 activation in vitro [131,132]. Docosahexanoic acid derivatives were also able to inhibit angiogenesis in vitro and in vivo [133]. Enzymes from the arachidonic acid metabolic pathway seem to be essential for the antiangiogenic activity of polyunsaturaled fatty acids [134,135]. In addition, dietary omega-3 diminished VEGF levels in several in vivo models of cancer [136], which is in agreement with the decreased levels of circulating VEGF observed in healthy volunteers after an omega-3 rich diet [137]. Furthermore, beneficial effects of omega-3 fatty acids in rats with 2-4-6-trinitrobenzen sulfonic acid (TNBS) induced colitis has been related to the downregulation of VEGFR-2 [138].
6.2. Tomatoes
As a consequence of Christopher Columbus’s voyages, novel foods from the New World were incorporated into the MD, including tomatoes (Solanum lycopersicum). Nowadays, tomatoes are essential in Mediterranean cuisine, being highly consumed either raw, in salads, or in cold soups such as the refreshing and tasty Andalusian gazpacho, or cooked as an essential ingredient of sauces and other meals. Increasing evidence supports a correlation between tomato consumption with a reduced risk of cardiovascular diseases and cancer [139,140]. Tomato is an important source of vitamin C, potassium, folic acid, and carotenoids, such as lycopene. The postulated cancer chemopreventive potential of lycopene [141,142,143,144] (Figure 3) could be reinforced by the use of this compound in angioprevention. Lycopene inhibits angionesis in vitro and in vivo at a concentration that should be achievable by dietary means [145]. This activity has been related to the MMP-2/uPA system inhibition through VEGFR-2-mediated PI3K-Akt and ERK/p38 signaling pathways [146]. Aside from lycopene, cystine-knot miniproteins present in tomato fruit (TCMPs) are now being postulated as useful inhibitors of angiogenesis. These proteins, present in mature tomato fruits, display resistance to gastrointestinal proteolytic attack and resistance to industrial processing [147]. Their antiangiogenic activities, demonstrated in vitro by the inhibition of endothelial tube formation and migration, as well as in vivo by using a zebrafish model, suggest that these proteins, along with lycopene and other antioxidants, may confer beneficial effects to tomato dietary intake [148,149].
6.3. Dairy Products
At a low level, the consumption of dairy products is included in the MD. These dairy products are, according to the ancient MD, mainly yoghurt (usually strained, a procedure that decreases lactose and increases protein content) and soft white fermented cheese (feta cheese in Greece or myzithra in Crete), with full-cream goat and sheep milk consumption being reserved for children [150]. Some components of milk have been studied in the context of angiogenesis modulation and chemoprevention of cancer, especially proteins and peptides [151,152], suggesting that milk components could play a role in angiogenesis inhibition and hence in angioprevention. In particular, the bovine milk proteins lactoferrin and lactoferricin (a pepsin-generated peptide derived from lactoferrin) have been described as angiogenesis inhibitors by using in vivo tumor models and in vitro approaches [153,154,155]. Mechanistically, both proteins seem to exert a similar activity by inhibiting the VEFG-A165-mediated angiogenesis in vivo [155,156]. Although these milk components support the potential role of dairy products in angioprevention, this property is not still well defined, as other proteins present in milk have shown proangiogenic activity. In particular, angiogenin-2, present in bovine milk and serum, has shown a proangiogenic effect in vivo using the CAM model [157]. Lactadherin (also known as MFG-E8 (milk fat globule epidermal growth factor-8)), another bioactive milk protein, has been described as a promoter of VEGF-dependent angiogenesis, exhibiting a protumoral role in different in vivo models [158,159,160].
6.4. Beverages
Attending to beverages included in the MD, apart from the daily consumption of water and the low intake of red wine within principal meals, the moderate consumption of coffee and herbal tea represents an important part of the MD [150]. Coffee contains a high variety of bioactive compounds, such as caffeine, chlorogenic acid, diterpenes, alkaloids, and polyphenols. Focusing in the potential role of coffee as an angiopreventive beverage, some of these compounds have shown its ability to inhibit angiogenesis [161,162]. This is the case of kahweol (Figure 3), an antioxidant diterpene present in coffee beans and unfiltered coffee beverages. Kahweol has been shown to inhibit key steps of angiogenesis in vitro, showing a potent antiangiogenic activity ex vivo (mouse aortic ring assay) and in vivo (CAM and zebrafish intersegmental vessel models) [161]. It also targeted inflammatory molecules such as COX-2 and MCP-1 in endothelial cells. Interestingly, kahweol palmitate, the diterpene ester derived from kahweol, maintained the antiangiogenic properties of kahweol in vitro, pointing to a mechanism of action that involves downregulation of the Akt pathway through negative modulation of VEGFR-2 [162]. Coffee is a highly consumed beverage worldwide, but the content of kahweol and other bioactive compounds is variable depending on the type of coffee and its processing (filtering of coffee is a critical step in affecting the content of kahweol). For this reason, it is important to remark that traditionally, the coffee included in the MD is the boiled (unfiltered) Greek coffee, which is rich in kahweol, as well in polyphenols and other antioxidants, and containing moderate amount of caffeine [163,164]. Indeed, in the interesting Ikaria study, the consumption of this type of coffee was associated with improved endothelial function [165].
6.5. Nuts
Other sources of bioactive compounds in the MD that are relevant to angioprevention are nuts. The MD includes mainly almonds, hazelnuts, walnuts, pistachios, and pine nuts, which are consumed moderately in the form of snacks, as part of cooked meals, or as nut-based desserts. The content in nutrients and phytochemicals in nuts is variable, but in general these foods are rich in unsaturated fats, vitamin B (folate), vitamin E (tocopherols), and polyphenols [166]. Among the key MD nuts, walnuts are especially relevant for angioprevention, as they represent a very important source of both linoleic and α-linolenic acid (omega-3 fatty acids) and contain significant amounts of the aforementioned inhibitor of angiogenesis—tocopherol. The effect of linoleic acid on angiogenesis modulation is contradictory, since both pro- and antiangiogenic roles have been described for this fatty acid in several models [167,168,169,170]. An interesting study showed that in vivo and in vitro treatments with linoleic acid produced an increase in the DNA methylation level of the VEGF-B promoter, which translated into lower levels of expression of the VEGF-B gene [171].
6.6. Seasonings
Traditional seasoning in the MD includes olive oil and herbs/spices. Although the quantity of herbs as a part of a diet is low, in the context of the MD, these traditional seasonings exhibit an interesting potential as a natural source of compounds able to inhibit angiogenesis. One of the most commonly used seasoning herbs in the MD is dry oregano (Origanum vulgare), which contains polyphenols in a high proportion [172]. Of note, the antiangiogenic effect of an ethanol extract of oregano (containing mainly phenolic acids and flavonol derivatives) was assessed in vivo and in vitro in the context of breast cancer, showing a decrease in the expression of VEGFR-2 in tumour cells [173]. Another example of a popular herb used in MD seasoning is rosemary (Rosmarinus officinalis), containing carnosol and carnosic acid, two diterpenes that have been described as inhibiting angiogenesis in vitro and in vivo by a mechanism that implies apoptosis induction in endothelial cells [174,175].
7. Conclusions
The scientific evidence pointing to the deep influence of diet on health involves an important change in biomedical research and clinical practice. Nutrients and bioactive compounds contained in foods have become essential players in numerous diseases at multiple levels, from initiation to progress, opening the possibility of studying the preventive and therapeutic role of certain elements of diet and even of specific dietary patterns. However, perhaps the main implication arising from this evidence is that the general population, to a certain extent, can control by themselves their own health easily by adapting their diet to a healthier model and consuming foods with bioactive compounds that could prevent the onset of certain diseases. A better understanding of how the genetic makeup of an individual modulates his/her differential response to nutrients, identifying and characterizing the gene–diet interactions, could help to optimize the individual dietary choices aimed at increasing quality of life, health, and longevity [176]. The use of integrative nutritional biomarkers could facilitate the achievement of “precision nutrition”, understood as personalized dietary recommendations that could produce optimal health effects in particular individuals [177].
In this context, the MD emerges as an interesting dietary pattern because of the reported beneficial effects of this diet on numerous pathologies, mainly cardiovascular diseases, but also diabetes, neurodegenerative diseases, and cancer [43]. The MD represents an important source of biologically active compounds and the preventive and therapeutic role of several of them in specific pathologic contexts constitutes a large subject to study. Aside from the interesting individual effects of the bioactive components of the MD, it is important to remark that these compounds usually are low-dose components of food, so it is feasible to argue that the preventive benefits of the MD on certain diseases could reside in the combination of foods containing different bioactive compounds that row in the same direction. This idea is reinforced by the fact that these diet-derived compounds exhibit relative non-toxic and safety profiles; hence, the long-term consumption of several of them in foods at the same time would rarely represent a risk.
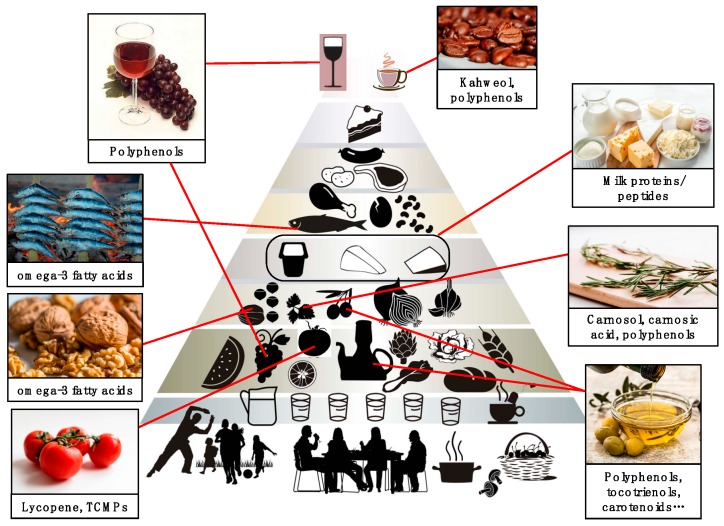
Angioprevention, and specifically diet-mediated angioprevention, is an emerging concept with important consequences for the prevention of cancer and other angiogenesis-dependent pathologies [22]. The link between angioprevention and MD has been minimally explored, even though there is clear implication of several MD components in angiogenesis inhibition, as reviewed here, which is summarized in Figure 4. The implementation of the MD concept at the three levels of cancer prevention would require in turn three levels of management (Figure 1). At the first level, adopting a high adherence to a MD would imply a certain level of angioprevention in the general population; at the second level, supplementation of the MD with specific purified components or even nutraceuticals would lead to a reinforced preventive effect on the risk population; and finally, in the third level, either isolated MD bioactive molecules or their derivatives could be administered as drugs to increase therapy efficacy, diminish side effects, or enlarge the disease-free time of cancer patients. Prevention is probably the most cost-effective long-term anticancer strategy. With increasing frequency, cancer becomes a chronic disorder for many patients, who must be treated for a long time. In this context, angiopreventive strategies based on the MD components could help to control the disease, with reasonable cost and minimizing long-term toxicities.
Figure 4.
The Mediterranean diet (MD) as a source of antiangiogenic compounds with potential use in cancer angioprevention. Schematic representation of the MD pyramid (modified from Fundación Dieta Mediterránea [27]), showing the main components that could have a role in angioprevention due to their content in antiangiogenic bioactive compounds.
In parallel to the growing evidences of the benefits of the MD in health, in recent years, a worrisome tendency towards a western diet in Mediterranean countries has been assessed, with clear possible implications in the general health status [29,30]. Hence, the importance in increasing the current adherence of the population to the MD is a crucial point in disease prevention. Present and future research about the molecular basis of the angiopreventive role of the MD could help to promote the return to a healthier way of life.
8. Future Perspectives
The Mediterranean diet arises as a rich and varied source of natural antitumoral and antiangiogenic compounds, pointing to a relevant chemopreventive potential that should be confirmed by clinical studies. For the general population, increasingly interested in the self-control of health, the knowledge of angiopreventive strategies based in consumption of selected foods should help to promote healthier dietary habits, preventing the initiation and/or progression of cancer. Personalized angiopreventive programs would be of useful application to the population with a high risk of developing cancer, for which improvement in the screening programs and the diagnostic tests are needed. Finally, cancer is becoming, with an increasing frequency, a chronic disorder for many patients, who must be treated for a long period of time. In this context, angiopreventive strategies based on MD components could help to control the disease with reasonable cost and minimizing long-term toxicities.
Author Contributions
Conceptualization, A.R.Q., B.M.-P., and M.A.M. writing—original draft preparation, A.R.Q., B.M.-P., J.A.T.-V., M.d.C.O., and M.G.-C.; writing—review and editing, A.R.Q., B.M.-P., and M.A.M.; drawing of figures, B.M.-P., J.A.T.-V., and A.R.Q.; supervision, A.R.Q. and B.M.-P.; funding acquisition, A.R.Q., B.M.-P., and M.A.M.
Funding
Supported by grants BIO2014-56092-R (MINECO and FEDER), P12-CTS-1507, and UMA18-FEDERJA-220 (Andalusian Government and FEDER), funds from “Plan Propio de Investigación y Transferencia” (University of Málaga) and from group BIO-267 (Andalusian Government). The “CIBER de enfermedades raras” is an initiative from the ISCIII (Spain). J.A.T.-V. and M.d.C.O. thank the Ministerio de Educación, Cultura y Deporte for their pre-doctoral fellowships (FPU programme).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Carmeliet P. Angiogenesis in life, disease and medicine. Nature. 2005;438:932–936. doi: 10.1038/nature04478. [DOI] [PubMed] [Google Scholar]
- 2.Potente M., Gerhardt H., Carmeliet P. Basis and therapeutic aspects of angiogenesis. Cell. 2011;146:873–887. doi: 10.1016/j.cell.2011.08.039. [DOI] [PubMed] [Google Scholar]
- 3.Quesada A.R., Muñoz-Chápuli R., Medina M. Ángel Angiogenesis and signal transduction in endothelial cells. Cell. Mol. Life Sci. 2004;61:2224–2243. doi: 10.1007/s00018-004-4070-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanahan D., Weinberg R.A. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 5.Hanahan D., Weinberg R.A. The hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 6.Bielenberg D.R., Zetter B.R. The Contribution of Angiogenesis to the Process of Metastasis. Cancer J. 2015;21:267–273. doi: 10.1097/PPO.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siemann D.W. The unique characteristics of tumor vasculature and preclinical evidence for its selective disruption by Tumor-Vascular Disrupting Agents. Cancer Treat. Rev. 2011;37:63–74. doi: 10.1016/j.ctrv.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Folkman J. Angiogenesis: An organizing principle for drug discovery? Nat. Rev. Drug Discov. 2007;6:273–286. doi: 10.1038/nrd2115. [DOI] [PubMed] [Google Scholar]
- 9.Sherwood L.M., Parris E.E., Folkman J. Tumor Angiogenesis: Therapeutic Implications. N. Engl. J. Med. 1971;285:1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 10.Quesada A.R., Medina M.A., Muñoz-Chápuli R. Anti-angiogenic drugs: From bench to clinical trials. Med. Res. Rev. 2006;26:483–530. doi: 10.1002/med.20059. [DOI] [PubMed] [Google Scholar]
- 11.Medina M.A., Muñoz-Chápuli R., Quesada A.R. Challenges of antiangiogenic cancer therapy: Trials and errors, and renewed hope. J. Cell. Mol. Med. 2007;11:374–382. doi: 10.1111/j.1582-4934.2007.00056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quesada A.R., Medina M.A., Muñoz-Chápuli R., Ponce Á.L. Do Not Say Ever Never More: The Ins and Outs of Antiangiogenic Therapies. Curr. Pharm. Des. 2010;16:3932–3957. doi: 10.2174/138161210794454950. [DOI] [PubMed] [Google Scholar]
- 13.Jayson G.C., Kerbel R., Ellis L.M., Harris A.L. Antiangiogenic therapy in oncology: Current status and future directions. Lancet. 2016;388:518–529. doi: 10.1016/S0140-6736(15)01088-0. [DOI] [PubMed] [Google Scholar]
- 14.Lin Z., Zhang Q., Luo W. Angiogenesis inhibitors as therapeutic agents in cancer: Challenges and future directions. Eur. J. Pharmacol. 2016;793:76–81. doi: 10.1016/j.ejphar.2016.10.039. [DOI] [PubMed] [Google Scholar]
- 15.Ramjiawan R.R., Griffioen A.W., Duda D.G. Anti-angiogenesis for cancer revisited: Is there a role for combinations with immunotherapy? Angiogenesis. 2017;20:185–204. doi: 10.1007/s10456-017-9552-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quesada A.R., Medina M.A., Alba E. Playing only one instrument may be not enough: Limitations and future of the antiangiogenic treatment of cancer. BioEssays. 2007;29:1159–1168. doi: 10.1002/bies.20655. [DOI] [PubMed] [Google Scholar]
- 17.Jain R.K. Normalization of Tumor Vasculature: An Emerging Concept in Antiangiogenic Therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 18.Fukumura D., Kloepper J., Amoozgar Z., Duda D.G., Jain R.K. Enhancing cancer immunotherapy using antiangiogenics: Opportunities and challenges. Nat. Rev. Clin. Oncol. 2018;15:325–340. doi: 10.1038/nrclinonc.2018.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sporn M.B. Approaches to prevention of epithelial cancer during the preneoplastic period. Cancer Res. 1976;36:2699–2702. [PubMed] [Google Scholar]
- 20.Meyskens F.L., Jr., Mukhtar H., Rock C.L., Cuzick J., Kensler T.W., Yang C.S., Ramsey S.D., Lippman S.M., Alberts D.S. Cancer Prevention: Obstacles, Challenges, and the Road Ahead. J. Natl. Cancer Inst. 2016;108 doi: 10.1093/jnci/djv309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tosetti F. ‘Angioprevention’: Angiogenesis is a common and key target for cancer chemopreventive agents. FASEB J. 2002;16:2–14. doi: 10.1096/fj.01-0300rev. [DOI] [PubMed] [Google Scholar]
- 22.Albini A., Tosetti F., Li V.W., Noonan D.M., Li W.W. Cancer prevention by targeting angiogenesis. Nat. Rev. Clin. Oncol. 2012;9:498–509. doi: 10.1038/nrclinonc.2012.120. [DOI] [PubMed] [Google Scholar]
- 23.Blackburn E.H. Highlighting the Science of Cancer Prevention. Cancer Prev. Res. 2010;3 doi: 10.1158/1940-6207.CAPR-10-0034. [DOI] [PubMed] [Google Scholar]
- 24.Wang Z., Dabrosin C., Yin X., Fuster M.M., Arreola A., Rathmell W.K., Generali D., Nagaraju G.P., El-Rayes B., Ribatti D., et al. Broad targeting of angiogenesis for cancer prevention and therapy. Semin. Cancer Boil. 2015;35:S224–S243. doi: 10.1016/j.semcancer.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li W.W., Li V.W., Hutnik M., Chiou A.S. Tumor angiogenesis as a target for dietary cancer prevention. J. Oncol. 2012;2012:879632. doi: 10.1155/2012/879623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keys A. Seven Countries. A Multivariate Analysis of Death and Coronary Heart Disease. Harvard University Press; Cambridge, MA, USA: 1980. [Google Scholar]
- 27.Fundación Dieta Mediterránea. [(accessed on 28 August 2019)]; Available online: https://dietamediterranea.com/
- 28.Mediterranean diet. [(accessed on 28 August 2019)]; Available online: https://ich.unesco.org/en/RL/mediterranean-diet-00884.
- 29.León-Muñoz L.M., Guallar-Castillón P., Graciani A., López-García E., Mesas A.E., Aguilera M.T., Banegas J.R., Rodríguez-Artalejo F. Adherence to the Mediterranean Diet Pattern Has Declined in Spanish Adults. J. Nutr. 2012;142:1843–1850. doi: 10.3945/jn.112.164616. [DOI] [PubMed] [Google Scholar]
- 30.Bonaccio M., Iacoviello L., De Gaetano G. The Mediterranean diet: the reasons for a success. Thromb. Res. 2012;129:401–404. doi: 10.1016/j.thromres.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Vareiro D., Bach-Faig A., Quintana B.R., Bertomeu I., Buckland G., De Almeida M.D.V., Serra-Majem L. Availability of Mediterranean and non-Mediterranean foods during the last four decades: Comparison of several geographical areas. Public Heath Nutr. 2009;12:1667–1675. doi: 10.1017/S136898000999053X. [DOI] [PubMed] [Google Scholar]
- 32.Bonaccio M., Bes-Rastrollo M., De Gaetano G., Iacoviello L. Challenges to the Mediterranean diet at a time of economic crisis. Nutr. Metab. Cardiovasc. Dis. 2016;26:1057–1063. doi: 10.1016/j.numecd.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 33.Gardener H., Wright C.B., Gu Y., Demmer R.T., Boden-Albala B., Elkind M.S., Sacco R.L., Scarmeas N. Mediterranean-style diet and risk of ischemic stroke, myocardial infarction, and vascular death: The Northern Manhattan Study. Am. J. Clin. Nutr. 2011;94:1458–1464. doi: 10.3945/ajcn.111.012799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoevenaar-Blom M.P., Nooyens A.C.J., Kromhout D., Spijkerman A.M.W., Beulens J.W.J., Van Der Schouw Y.T., Bueno-De-Mesquita B., Verschuren W.M.M. Mediterranean Style Diet and 12-Year Incidence of Cardiovascular Diseases: The EPIC-NL Cohort Study. PLoS ONE. 2012;7:e45458. doi: 10.1371/journal.pone.0045458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tektonidis T.G., Åkesson A., Gigante B., Wolk A., Larsson S.C. A Mediterranean diet and risk of myocardial infarction, heart failure and stroke: A population-based cohort study. Atherosclerosis. 2015;243:93–98. doi: 10.1016/j.atherosclerosis.2015.08.039. [DOI] [PubMed] [Google Scholar]
- 36.Tognon G., Lissner L., Sæbye D., Walker K.Z., Heitmann B.L. The Mediterranean diet in relation to mortality and CVD: A Danish cohort study. Br. J. Nutr. 2014;111:151–159. doi: 10.1017/S0007114513001931. [DOI] [PubMed] [Google Scholar]
- 37.Tong T.Y.N., Wareham N.J., Khaw K.T., Imamura F., Forouhi N.G. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: The EPIC-Norfolk study. BMC Med. 2016;14:135. doi: 10.1186/s12916-016-0677-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stojanovic J., Giraldi L., Arzani D., Pastorino R., Biondi A., Persiani R., Boccia S., Leoncini E. Adherence to Mediterranean diet and risk of gastric cancer: Results of a case–control study in Italy. Eur. J. Cancer Prev. 2017;26:491–496. doi: 10.1097/CEJ.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 39.Van den Brandt P.A., Schulpen M. Mediterranean diet adherence and risk of postmenopausal breast cancer: Results of a cohort study and meta-analysis. Int. J. Cancer. 2017;140:2220–2231. doi: 10.1002/ijc.30654. [DOI] [PubMed] [Google Scholar]
- 40.Farinetti A., Zurlo V., Manenti A., Coppi F., Mattioli A.V. Mediterranean diet and colorectal cancer: A systematic review. Nutrition. 2017;43:83–88. doi: 10.1016/j.nut.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 41.Mitrou P.N., Kipnis V., Thiébaut A.C.M., Reedy J., Subar A.F., Wirfält E., Flood A., Mouw T., Hollenbeck A.R., Leitzmann M.F., et al. Mediterranean Dietary Pattern and Prediction of All-Cause Mortality in a US Population. Arch. Intern. Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 42.Dinu M., Pagliai G., Casini A., Sofi F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2017;72:30–43. doi: 10.1038/ejcn.2017.58. [DOI] [PubMed] [Google Scholar]
- 43.Corella D., Coltell O., Macian F., Ordovás J.M. Advances in Understanding the Molecular Basis of the Mediterranean Diet Effect. Annu. Rev. Food Sci. Technol. 2018;9:227–249. doi: 10.1146/annurev-food-032217-020802. [DOI] [PubMed] [Google Scholar]
- 44.Martínez-González M.A., Salas-Salvadó J., Estruch R., Corella D., Fitó M., Ros E. Benefits of the Mediterranean Diet: Insights from the PREDIMED Study. Prog. Cardiovasc. Dis. 2015;58:50–60. doi: 10.1016/j.pcad.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 45.Gajendragadkar P.R., Hubsch A., Mäki-Petäjä K.M., Serg M., Wilkinson I.B., Cheriyan J. Effects of Oral Lycopene Supplementation on Vascular Function in Patients with Cardiovascular Disease and Healthy Volunteers: A Randomised Controlled Trial. PLoS ONE. 2014;9:e99070. doi: 10.1371/journal.pone.0099070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Casas R., Sacanella E., Urpi-Sarda M., Chiva-Blanch G., Ros E., Martínez-González M.A., Covas M.I., Salas-Salvadó J., Fiol M., Arós F., et al. The Effects of the Mediterranean Diet on Biomarkers of Vascular Wall Inflammation and Plaque Vulnerability in Subjects with High Risk for Cardiovascular Disease. A Randomized Trial. PLoS ONE. 2014;9:e100084. doi: 10.1371/journal.pone.0100084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Storniolo C.E., Rosello-Catafau J., Pintó X., Mitjavila M.T., Moreno J.J. Polyphenol fraction of extra virgin olive oil protects against endothelial dysfunction induced by high glucose and free fatty acids through modulation of nitric oxide and endothelin-1. Redox Boil. 2014;2:971–977. doi: 10.1016/j.redox.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Turati F., Carioli G., Bravi F., Ferraroni M., Serraino D., Montella M., Giacosa A., Toffolutti F., Negri E., Levi F., et al. Mediterranean Diet and Breast Cancer Risk. Nutrients. 2018;10:326. doi: 10.3390/nu10030326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cottet V., Touvier M., Fournier A., Touillaud M.S., Lafay L., Clavel-Chapelon F., Boutron-Ruault M.C. Postmenopausal Breast Cancer Risk and Dietary Patterns in the E3N-EPIC Prospective Cohort Study. Am. J. Epidemiol. 2009;170:1257–1267. doi: 10.1093/aje/kwp257. [DOI] [PubMed] [Google Scholar]
- 50.Donovan M.G., Selmin O.I., Doetschman T.C., Romagnolo D.F. Mediterranean Diet: Prevention of Colorectal Cancer. Front. Nutr. 2017;4:59. doi: 10.3389/fnut.2017.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rotelli M., Bocale D., De Fazio M., Ancona P., Scalera I., Memeo R., Travaglio E., Zbar A., Altomare D.F. IN-VITRO evidence for the protective properties of the main components of the Mediterranean diet against colorectal cancer: A systematic review. Surg. Oncol. 2015;24:145–152. doi: 10.1016/j.suronc.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 52.Quiles J.L., Ramirez-Tortosa M.C., Yaqoob P. Olive Oil and Health. CABI Publishing; Oxford, UK: 2006. [Google Scholar]
- 53.Frankel E., Bakhouche A., Lozano-Sánchez J., Segura-Carretero A., Fernández-Gutiérrez A. Literature Review on Production Process To Obtain Extra Virgin Olive Oil Enriched in Bioactive Compounds. Potential Use of Byproducts as Alternative Sources of Polyphenols. J. Agric. Food Chem. 2013;61:5179–5188. doi: 10.1021/jf400806z. [DOI] [PubMed] [Google Scholar]
- 54.Boskou D., Blekas G., Tsimidou M. Olive oil composition. In: Boskou D., editor. Olive Oil: Chemistry and Technology. 2nd ed. AOCS Press; Champaign, IL, USA: 2006. pp. 41–71. [Google Scholar]
- 55.Ghanbari R., Anwar F., Alkharfy K.M., Gilani A.H., Saari N. Valuable Nutrients and Functional Bioactives in Different Parts of Olive (Olea europaea L.)—A Review. Int. J. Mol. Sci. 2012;13:3291–3340. doi: 10.3390/ijms13033291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Servili M., Esposto S., Fabiani R., Urbani S., Taticchi A., Mariucci F., Selvaggini R., Montedoro G.F. Review Phenolic compounds in olive oil: Antioxidant, health and organoleptic activities according to their chemical structure. Inflammopharmacology. 2009;17:76–84. doi: 10.1007/s10787-008-8014-y. [DOI] [PubMed] [Google Scholar]
- 57.Gorzynik-Debicka M., Przychodzen P., Cappello F., Kuban-Jankowska A., Gammazza A.M., Knap N., Wozniak M., Gorska-Ponikowska M. Potential Health Benefits of Olive Oil and Plant Polyphenols. Int. J. Mol. Sci. 2018;19:686. doi: 10.3390/ijms19030686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.García A., Ruiz-Méndez M.V., Romero C., Brenes M. Effect of refining on the phenolic composition of crude olive oils. J. Am. Oil Chem. Soc. 2006;83:159–164. doi: 10.1007/s11746-006-1189-8. [DOI] [Google Scholar]
- 59.Covas M.I., Fitó M., Kušar A., Pravst I., Martín-Peláez S., Martín-Peláez S. Health effects of olive oil polyphenols: Recent advances and possibilities for the use of health claims. Mol. Nutr. Food Res. 2013;57:760–771. doi: 10.1002/mnfr.201200421. [DOI] [PubMed] [Google Scholar]
- 60.Farooqi A.A., Fayyaz S., Silva A.S., Sureda A., Nabavi S.F., Mocan A., Nabavi S.M., Bishayee A. Oleuropein and Cancer Chemoprevention: The Link is Hot. Molecules. 2017;22:705. doi: 10.3390/molecules22050705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lamy S., Ouanouki A., Beliveau R., Desrosiers R.R. Olive oil compounds inhibit vascular endothelial growth factor receptor-2 phosphorylation. Exp. Cell Res. 2014;322:89–98. doi: 10.1016/j.yexcr.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 62.Scoditti E., Calabriso N., Massaro M., Pellegrino M., Storelli C., Martines G., De Caterina R., Carluccio M.A. Mediterranean diet polyphenols reduce inflammatory angiogenesis through MMP-9 and COX-2 inhibition in human vascular endothelial cells: A potentially protective mechanism in atherosclerotic vascular disease and cancer. Arch. Biochem. Biophys. 2012;527:81–89. doi: 10.1016/j.abb.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 63.Vilaplana-Pérez C., Auñón D., García-Flores L.A., Gil-Izquierdo A. Hydroxytyrosol and Potential Uses in Cardiovascular Diseases, Cancer, and AIDS. Front. Nutr. 2014;1:18. doi: 10.3389/fnut.2014.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tejada S., Pinya S., Bibiloni M.D.M., Tur J.A., Pons A., Sureda A., Tejada S.P.S. Cardioprotective Effects of the Polyphenol Hydroxytyrosol from Olive Oil. Curr. Drug Targets. 2017;18:1477–1486. doi: 10.2174/1389450117666161005150650. [DOI] [PubMed] [Google Scholar]
- 65.Omar S.H., Scott C.J., Hamlin A.S., Obied H.K. The protective role of plant biophenols in mechanisms of Alzheimer’s disease. J. Nutr. Biochem. 2017;47:1–20. doi: 10.1016/j.jnutbio.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 66.Fortes C., García-Vilas J.A., Quesada A.R., Medina M.A. Evaluation of the anti-angiogenic potential of hydroxytyrosol and tyrosol, two bio-active phenolic compounds of extra virgin olive oil, in endothelial cell cultures. Food Chem. 2012;134:134–140. doi: 10.1016/j.foodchem.2012.02.079. [DOI] [Google Scholar]
- 67.García-Vilas J.A., Quesada A.R., Medina M. Ángel Hydroxytyrosol targets extracellular matrix remodeling by endothelial cells and inhibits both ex vivo and in vivo angiogenesis. Food Chem. 2017;221:1741–1746. doi: 10.1016/j.foodchem.2016.10.111. [DOI] [PubMed] [Google Scholar]
- 68.López-Jiménez A., Gallardo E., Espartero J.L., Madrona A., Quesada A.R., Medina M.A. Comparison of the anti-angiogenic potential of hydroxytyrosol and its five derivatives. Food Funct. 2018;9:4310–4316. doi: 10.1039/C8FO01140K. [DOI] [PubMed] [Google Scholar]
- 69.Kwon H.J., Shim J.S., Kim J.H., Cho H.Y., Na Yum Y., Kim S.H., Yu J. Betulinic Acid Inhibits Growth Factor-induced in vitro Angiogenesis via the Modulation of Mitochondrial Function in Endothelial Cells. Jpn. J. Cancer Res. 2002;93:417–425. doi: 10.1111/j.1349-7006.2002.tb01273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fulda S. Betulinic Acid for Cancer Treatment and Prevention. Int. J. Mol. Sci. 2008;9:1096–1107. doi: 10.3390/ijms9061096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shanmugam M.K., Dai X., Kumar A.P., Tan B.K., Sethi G., Bishayee A. Oleanolic acid and its synthetic derivatives for the prevention and therapy of cancer: Preclinical and clinical evidence. Cancer Lett. 2014;346:206–216. doi: 10.1016/j.canlet.2014.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li L., Lin J., Sun G., Wei L., Shen A., Zhang M., Peng J. Oleanolic acid inhibits colorectal cancer angiogenesis in vivo and in vitro via suppression of STAT3 and Hedgehog pathways. Mol. Med. Rep. 2016;13:5276–5282. doi: 10.3892/mmr.2016.5171. [DOI] [PubMed] [Google Scholar]
- 73.Niu G., Sun L., Pei Y., Wang D. Oleanolic Acid Inhibits Colorectal Cancer Angiogenesis by Blocking the VEGFR2 Signaling Pathway. Anti-Cancer Agents Med. Chem. 2018;18:583–590. doi: 10.2174/1871520617666171020124916. [DOI] [PubMed] [Google Scholar]
- 74.Cárdenas C., Quesada A.R., Medina M.A. Effects of ursolic acid on different steps of the angiogenic process. Biochem. Biophys. Res. Commun. 2004;320:402–408. doi: 10.1016/j.bbrc.2004.05.183. [DOI] [PubMed] [Google Scholar]
- 75.Lin J., Chen Y., Wei L., Hong Z., Sferra T.J., Peng J. Ursolic acid inhibits colorectal cancer angiogenesis through suppression of multiple signaling pathways. Int. J. Oncol. 2013;43:1666–1674. doi: 10.3892/ijo.2013.2101. [DOI] [PubMed] [Google Scholar]
- 76.Chi K.Q., Wei Z.Y., Wang K.S., Wu J., Chen W.Q., Jin X.J., Piao H.R. Design, synthesis, and evaluation of novel ursolic acid derivatives as HIF-1α inhibitors with anticancer potential. Bioorg. Chem. 2017;75:157–169. doi: 10.1016/j.bioorg.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 77.Shanmugam M.K., Dai X., Kumar A.P., Tan B.K., Sethi G., Bishayee A. Ursolic acid in cancer prevention and treatment: Molecular targets, pharmacokinetics and clinical studies. Biochem. Pharmacol. 2013;85:1579–1587. doi: 10.1016/j.bcp.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 78.Chen H., Gao Y., Wang A., Zhou X., Zheng Y., Zhou J. Evolution in Medicinal Chemistry of Ursolic Acid Derivatives as Anticancer Agents. Eur. J. Med. Chem. 2015;92:648–655. doi: 10.1016/j.ejmech.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kashyap D., Tuli H.S., Sharma A.K. Ursolic acid (UA): A metabolite with promising therapeutic potential. Life Sci. 2016;146:201–213. doi: 10.1016/j.lfs.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 80.Thakor P., Song W., Subramanian R.B., Thakkar V.R., Vesey D.A., Gobe G.C. Maslinic Acid Inhibits Proliferation of Renal Cell Carcinoma Cell Lines and Suppresses Angiogenesis of Endothelial Cells. J. Kidney Cancer VHL. 2017;4:16–24. doi: 10.15586/jkcvhl.2017.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Peron G., Marzaro G., Dall’Acqua S. Known Triterpenes and their Derivatives as Scaffolds for the Development of New Therapeutic Agents for Cancer. Curr. Med. Chem. 2018;25:1259–1269. doi: 10.2174/0929867324666170818111933. [DOI] [PubMed] [Google Scholar]
- 82.Valdés K., Morales J., Rodríguez L., Günther G. Potential use of nanocarriers with pentacyclic triterpenes in cancer treatments. Nanomedicine. 2016;12:3139–3156. doi: 10.2217/nnm-2016-0251. [DOI] [PubMed] [Google Scholar]
- 83.Haque W., Pattanayak S.P., Sinha B.N. Evaluation of taxifolin and phloretin as antiangiogenic flavonoids: An in vivo, in vitro experimental analysis. Int. J. Pharm. Sci. 2015;7:5–12. [Google Scholar]
- 84.Guruvayoorappan C., Kuttan G. β-Carotene Inhibits Tumor-Specific Angiogenesis by Altering the Cytokine Profile and Inhibits the Nuclear Translocation of Transcription Factors in B16F-10 Melanoma Cells. Integr. Cancer Ther. 2007;6:258–270. doi: 10.1177/1534735407305978. [DOI] [PubMed] [Google Scholar]
- 85.Chew B.P., Brown C.M., Park J.S., Mixter P.F. Dietary lutein inhibits mouse mammary tumor growth by regulating angiogenesis and apoptosis. Anticancer. Res. 2003;23:3333–3339. [PubMed] [Google Scholar]
- 86.Eggersdorfer M., Wyss A. Carotenoids in human nutrition and health. Arch. Biochem. Biophys. 2018;652:18–26. doi: 10.1016/j.abb.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 87.Aggarwal B.B., Sundaram C., Prasad S., Kannappan R. Tocotrienols, the Vitamin E of the 21st Century: It’s Potential Against Cancer and Other Chronic Diseases. Biochem. Pharmacol. 2010;80:1613–1631. doi: 10.1016/j.bcp.2010.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Inokuchi H., Hirokane H., Tsuzuki T., Nakagawa K., Igarashi M., Miyazawa T. Anti-angiogenic Activity of Tocotrienol. Biosci. Biotechnol. Biochem. 2003;67:1623–1627. doi: 10.1271/bbb.67.1623. [DOI] [PubMed] [Google Scholar]
- 89.Shibata A., Nakagawa K., Sookwong P., Tsuduki T., Oikawa S., Miyazawa T. δ-Tocotrienol Suppresses VEGF Induced Angiogenesis whereas α-Tocopherol Does Not. J. Agric. Food Chem. 2009;57:8696–8704. doi: 10.1021/jf9012899. [DOI] [PubMed] [Google Scholar]
- 90.Nakagawa K., Shibata A., Yamashita S., Tsuzuki T., Kariya J., Oikawa S., Miyazawa T. In vivo angiogenesis is suppressed by unsaturated vitamin E, tocotrienol. J. Nutr. 2007;137:1938–1943. doi: 10.1093/jn/137.8.1938. [DOI] [PubMed] [Google Scholar]
- 91.Sakthivel R., Malar D.S., Devi K.P. Phytol shows anti-angiogenic activity and induces apoptosis in A549 cells by depolarizing the mitochondrial membrane potential. Biomed. Pharmacother. 2018;105:742–752. doi: 10.1016/j.biopha.2018.06.035. [DOI] [PubMed] [Google Scholar]
- 92.Moon E.J., Lee Y.M., Lee O.H., Lee M.J., Lee S.K., Chung M.H., Park Y.I., Sung C.K., Choi J.S., Kim K.W. A novel angiogenic factor derived from Aloe vera gel: β-sitosterol, a plant sterol. Angiogenesis. 1999;3:117–123. doi: 10.1023/A:1009058232389. [DOI] [PubMed] [Google Scholar]
- 93.Choi J.M., Lee E.O., Lee H.J., Kim K.H., Ahn K.S., Shim B.S., Kim N.I., Song M.C., Baek N.I., Kim S.H. Identification of campesterol fromChrysanthemum coronarium L. and its antiangiogenic activities. Phytother. Res. 2007;21:954–959. doi: 10.1002/ptr.2189. [DOI] [PubMed] [Google Scholar]
- 94.Chiva-Blanch G., Arranz S., Lamuela-Raventos R.M., Estruch R. Effects of Wine, Alcohol and Polyphenols on Cardiovascular Disease Risk Factors: Evidences from Human Studies. Alcohol Alcohol. 2013;48:270–277. doi: 10.1093/alcalc/agt007. [DOI] [PubMed] [Google Scholar]
- 95.Oak M.H., El Bedoui J., Schini-Kerth V.B. Antiangiogenic properties of natural polyphenols from red wine and green tea. J. Nutr. Biochem. 2005;16:1–8. doi: 10.1016/j.jnutbio.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 96.Garvin S., Öllinger K., Dabrosin C. Resveratrol induces apoptosis and inhibits angiogenesis in human breast cancer xenografts in vivo. Cancer Lett. 2006;231:113–122. doi: 10.1016/j.canlet.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 97.Lin S.M., Chen J.C., Su Y.H., Tseng S.H., Huang H.Y. Resveratrol Suppresses the Angiogenesis and Tumor Growth of Gliomas in Rats. Clin. Cancer Res. 2004;10:2190–2202. doi: 10.1158/1078-0432.ccr-03-0105. [DOI] [PubMed] [Google Scholar]
- 98.Fukuda S., Kaga S., Zhan L., Bagchi D., Das D.K., Bertelli A., Maulik N. Resveratrol Ameliorates Myocardial Damage by Inducing Vascular Endothelial Growth Factor-Angiogenesis and Tyrosine Kinase Receptor Flk-1. Cell Biophys. 2006;44:43–49. doi: 10.1385/CBB:44:1:043. [DOI] [PubMed] [Google Scholar]
- 99.Gan L., Matsuura H., Ichiki T., Yin X., Miyazaki R., Hashimoto T., Cui J., Takeda K., Sunagawa K. Improvement of neovascularization capacity of bone marrow mononuclear cells from diabetic mice by ex vivo pretreatment with resveratrol. Hypertens. Res. 2009;32:542–547. doi: 10.1038/hr.2009.67. [DOI] [PubMed] [Google Scholar]
- 100.Hermann D.M., Zechariah A., Kaltwasser B., Bosche B., Çağlayan A.B., Kilic E., Doeppner T.R. Sustained neurological recovery induced by resveratrol is associated with angioneurogenesis rather than neuroprotection after focal cerebral ischemia. Neurobiol. Dis. 2015;83:16–25. doi: 10.1016/j.nbd.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 101.Kamaleddin M.A. The paradoxical pro- and antiangiogenic actions of resveratrol: Therapeutic applications in cancer and diabetes. Ann. N. Y. Acad. Sci. 2016;1386:3–15. doi: 10.1111/nyas.13283. [DOI] [PubMed] [Google Scholar]
- 102.Bråkenhielm E., Cao R., Cao Y. Suppression of angiogenesis, tumor growth, and wound healing by resveratrol, a natural compound in red wine and grapes. FASEB J. 2001;15:1798–1800. doi: 10.1096/fj.01-0028fje. [DOI] [PubMed] [Google Scholar]
- 103.Park S.Y., Jeong K.J., Lee J., Yoon D.S., Choi W.S., Kim Y.K., Han J.W., Kim Y.M., Kim B.K., Lee H.Y. Hypoxia enhances LPA-induced HIF-1α and VEGF expression: Their inhibition by resveratrol. Cancer Lett. 2007;258:63–69. doi: 10.1016/j.canlet.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 104.Wang H., Zhou H., Zou Y., Liu Q., Guo C., Gao G., Shao C., Gong Y. Resveratrol modulates angiogenesis through the GSK3β/β-catenin/TCF-dependent pathway in human endothelial cells. Biochem. Pharmacol. 2010;80:1386–1395. doi: 10.1016/j.bcp.2010.07.034. [DOI] [PubMed] [Google Scholar]
- 105.Belleri M., Ribatti D., Savio M., Stivala L.A., Forti L., Tanghetti E., Alessi P., Coltrini D., Bugatti A., Mitola S., et al. αvβ3 Integrin-dependent antiangiogenic activity of resveratrol stereoisomers. Mol. Cancer Ther. 2008;7:3761–3770. doi: 10.1158/1535-7163.MCT-07-2351. [DOI] [PubMed] [Google Scholar]
- 106.Kim D.H., Sung B., Kim J.A., Kang Y.J., Hwang S.Y., Hwang N.L., Suh H., Choi Y.H., Im E., Chung H.Y., et al. HS-1793, a resveratrol analogue, downregulates the expression of hypoxia-induced HIF-1 and VEGF and inhibits tumor growth of human breast cancer cells in a nude mouse xenograft model. Int. J. Oncol. 2017;51:715–723. doi: 10.3892/ijo.2017.4058. [DOI] [PubMed] [Google Scholar]
- 107.Potter G.A., Patterson L.H., Wanogho E., Perry P.J., Butler P.C., Ijaz T., Ruparelia K.C., Lamb J.H., Farmer P.B., Stanley L.A., et al. The cancer preventative agent resveratrol is converted to the anticancer agent piceatannol by the cytochrome P450 enzyme CYP1B1. Br. J. Cancer. 2002;86:774–778. doi: 10.1038/sj.bjc.6600197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Choi K.H., Kim J.E., Song N.R., Son J.E., Hwang M.K., Byun S., Kim J.H., Lee K.W., Lee H.J. Phosphoinositide 3-kinase is a novel target of piceatannol for inhibiting PDGF-BB-induced proliferation and migration in human aortic smooth muscle cells. Cardiovasc. Res. 2010;85:836–844. doi: 10.1093/cvr/cvp359. [DOI] [PubMed] [Google Scholar]
- 109.Surh Y.J., Na H.K. Therapeutic Potential and Molecular Targets of Piceatannol in Chronic Diseases. Adv. Exp. Med. Biol. 2016;928:185–211. doi: 10.1007/978-3-319-41334-1_9. [DOI] [PubMed] [Google Scholar]
- 110.Buharalioglu C.K., Song C.Y., Yaghini F.A., Ghafoor H.U.B., Motiwala M., Adris T., Estes A.M., Malik K.U. Angiotensin II-induced process of angiogenesis is mediated by spleen tyrosine kinase via VEGF receptor-1 phosphorylation. Am. J. Physiol. Circ. Physiol. 2011;301:H1043–H1055. doi: 10.1152/ajpheart.01018.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Song H., Jung J.I., Cho H.J., Her S., Kwon S.H., Yu R., Kang Y.H., Lee K.W., Park J.H.Y. Inhibition of tumor progression by oral piceatannol in mouse 4T1 mammary cancer is associated with decreased angiogenesis and macrophage infiltration. J. Nutr. Biochem. 2015;26:1368–1378. doi: 10.1016/j.jnutbio.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 112.Pal H.C., Pearlman R.L., Afaq F. Fisetin and Its Role in Chronic Diseases. Adv. Exp. Med. Biol. 2016;928:213–244. doi: 10.1007/978-3-319-41334-1_10. [DOI] [PubMed] [Google Scholar]
- 113.Bhat T.A., Nambiar D., Pal A., Agarwal R., Singh R.P. Fisetin inhibits various attributes of angiogenesis in vitro and in vivo--implications for angioprevention. Carcinogenesis. 2011;33:385–393. doi: 10.1093/carcin/bgr282. [DOI] [PubMed] [Google Scholar]
- 114.Chen C.M., Hsieh Y.H., Hwang J.M., Jan H.J., Hsieh S.C., Lin S.H., Lai C.Y. Fisetin suppresses ADAM9 expression and inhibits invasion of glioma cancer cells through increased phosphorylation of ERK1/2. Tumor Biol. 2015;36:3407–3415. doi: 10.1007/s13277-014-2975-9. [DOI] [PubMed] [Google Scholar]
- 115.Anso E., Zuazo A., Irigoyen M., Urdaci M.C., Rouzaut A., Martínez-Irujo J.J. Flavonoids inhibit hypoxia-induced vascular endothelial growth factor expression by a HIF-1 independent mechanism. Biochem. Pharmacol. 2010;79:1600–1609. doi: 10.1016/j.bcp.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 116.Pal H.C., Sharma S., Strickland L.R., Katiyar S.K., Ballestas M.E., Athar M., Elmets C.A., Afaq F. Fisetin Inhibits Human Melanoma Cell Invasion through Promotion of Mesenchymal to Epithelial Transition and by Targeting MAPK and NFκB Signaling Pathways. PLoS ONE. 2014;9:e86338. doi: 10.1371/journal.pone.0086338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pal H.C., Baxter R.D., Hunt K.M., Agarwal J., Elmets C.A., Athar M., Afaq F. Fisetin, a phytochemical, potentiates sorafenib-induced apoptosis and abrogates tumor growth in athymic nude mice implanted with BRAF-mutated melanoma cells. Oncotarget. 2015;6:28296–28311. doi: 10.18632/oncotarget.5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Touil Y.S., Fellous A., Scherman D., Chabot G.G. Flavonoid-induced morphological modifications of endothelial cells through microtubule stabilization. Nutr. Cancer. 2009;61:310–321. doi: 10.1080/01635580802521346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Touil Y.S., Seguin J., Scherman D., Chabot G.G. Improved antiangiogenic and antitumour activity of the combination of the natural flavonoid fisetin and cyclophosphamide in Lewis lung carcinoma-bearing mice. Cancer Chemother. Pharmacol. 2011;68:445–455. doi: 10.1007/s00280-010-1505-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Favot L., Martin S., Keravis T., Andriantsitohaina R., Lugnier C. Involvement of cyclin-dependent pathway in the inhibitory effect of delphinidin on angiogenesis. Cardiovasc. Res. 2003;59:479–487. doi: 10.1016/S0008-6363(03)00433-4. [DOI] [PubMed] [Google Scholar]
- 121.Lamy S., Blanchette M., Michaud-Levesque J., Lafleur R., Durocher Y., Moghrabi A., Barrette S., Gingras D., Béliveau R. Delphinidin, a dietary anthocyanidin, inhibits vascular endothelial growth factor receptor-2 phosphorylation. Carcinogenesis. 2006;27:989–996. doi: 10.1093/carcin/bgi279. [DOI] [PubMed] [Google Scholar]
- 122.Lamy S., Beaulieu É., Labbé D., Bédard V., Moghrabi A., Barrette S., Gingras D., Béliveau R. Delphinidin, a dietary anthocyanidin, inhibits platelet-derived growth factor ligand/receptor (PDGF/PDGFR) signaling. Carcinogenesis. 2008;29:1033–1041. doi: 10.1093/carcin/bgn070. [DOI] [PubMed] [Google Scholar]
- 123.Kim M.H., Jeong Y.J., Cho H.J., Hoe H.S., Park K.K., Park Y.Y., Choi Y.H., Kim C.H., Chang H.W., Park Y.J., et al. Delphinidin inhibits angiogenesis through the suppression of HIF-1α and VEGF expression in A549 lung cancer cells. Oncol. Rep. 2017;37:777–784. doi: 10.3892/or.2016.5296. [DOI] [PubMed] [Google Scholar]
- 124.Kang N.J., Jung S.K., Lee K.W., Lee H.J. Myricetin is a potent chemopreventive phytochemical in skin carcinogenesis. Ann. N. Y. Acad. Sci. 2011;1229:124–132. doi: 10.1111/j.1749-6632.2011.06122.x. [DOI] [PubMed] [Google Scholar]
- 125.Kim G.D. Myricetin inhibits angiogenesis by inducing apoptosis and suppressing PI3K/Akt/mTOR signaling in endothelial cells. J. Cancer Prev. 2017;22:219–227. doi: 10.15430/JCP.2017.22.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Huang H., Chen A.Y., Rojanasakul Y., Ye X., Rankin G.O., Chen Y.C. Dietary compounds galangin and myricetin suppress ovarian cancer cell angiogenesis. J. Funct. Foods. 2015;15:464–475. doi: 10.1016/j.jff.2015.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Jung S.K., Lee K.W., Byun S., Lee E.J., Kim J.E., Bode A.M., Dong Z., Lee H.J. Myricetin inhibits UVB-induced angiogenesis by regulating PI-3 kinase in vivo. Carcinogenesis. 2010;31:911–917. doi: 10.1093/carcin/bgp221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Eltweri A.M., Thomas A., Metcalfe M., Calder P., Dennison A., Bowrey D. Potential applications of fish oils rich in omega-3 polyunsaturated fatty acids in the management of gastrointestinal cancer. Clin. Nutr. 2017;36:65–78. doi: 10.1016/j.clnu.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 129.Fabian C.J., Kimler B.F., Hursting S.D. Omega-3 fatty acids for breast cancer prevention and survivorship. Breast Cancer Res. 2015;17:62. doi: 10.1186/s13058-015-0571-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kang J.X., Liu A. The role of the tissue omega-6/omega-3 fatty acid ratio in regulating tumor angiogenesis. Cancer Metastasis Rev. 2013;32:201–210. doi: 10.1007/s10555-012-9401-9. [DOI] [PubMed] [Google Scholar]
- 131.Tsuji M., Murota S.I., Morita I. Docosapentaenoic acid (22:5, n-3) suppressed tube-forming activity in endothelial cells induced by vascular endothelial growth factor. Prostaglandins Leukot. Essent. Fat. Acids. 2003;68:337–342. doi: 10.1016/S0952-3278(03)00025-5. [DOI] [PubMed] [Google Scholar]
- 132.Tsuzuki T., Shibata A., Kawakami Y., Nakagawa K., Miyazawa T. Conjugated eicosapentaenoic acid inhibits vascular endothelial growth factor-induced angiogenesis by suppressing the migration of human umbilical vein endothelial cells. J. Nutr. 2007;137:641–646. doi: 10.1093/jn/137.3.641. [DOI] [PubMed] [Google Scholar]
- 133.Zhang G., Panigrahy D., Mahakian L.M., Yang J., Liu J.Y., Lee K.S.S., Wettersten H.I., Ulu A., Hu X., Tam S., et al. Epoxy metabolites of docosahexaenoic acid (DHA) inhibit angiogenesis, tumor growth, and metastasis. Proc. Natl. Acad. Sci. USA. 2013;110:6530–6535. doi: 10.1073/pnas.1304321110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Szymczak M., Murray M., Petrovic N. Modulation of angiogenesis by ω-3 polyunsaturated fatty acids is mediated by cyclooxygenases. Blood. 2008;111:3514–3521. doi: 10.1182/blood-2007-08-109934. [DOI] [PubMed] [Google Scholar]
- 135.Sapieha P., Stahl A., Chen J., Seaward M.R., Willett K.L., Krah N.M., Dennison R.J., Connor K.M., Aderman C.M., Liclican E., et al. 5-Lipoxygenase Metabolite 4-HDHA Is a Mediator of the Antiangiogenic Effect of ω-3 Polyunsaturated Fatty Acids. Sci. Transl. Med. 2011;3 doi: 10.1126/scitranslmed.3001571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Calviello G., Di Nicuolo F., Gragnoli S., Piccioni E., Serini S., Maggiano N., Tringali G., Navarra P., Ranelletti F.O., Palozza P. n-3 PUFAs reduce VEGF expression in human colon cancer cells modulating the COX-2/PGE 2 induced ERK-1 and -2 and HIF-1α induction pathway. Carcinogenesis. 2004;25:2303–2310. doi: 10.1093/carcin/bgh265. [DOI] [PubMed] [Google Scholar]
- 137.Ambring A., Johansson M., Axelsen M., Gan L., Strandvik B., Friberg P. Mediterranean-inspired diet lowers the ratio of serum phospholipid n-6 to n-3 fatty acids, the number of leukocytes and platelets, and vascular endothelial growth factor in healthy subjects. Am. J. Clin. Nutr. 2006;83:575–581. doi: 10.1093/ajcn.83.3.575. [DOI] [PubMed] [Google Scholar]
- 138.Ibrahim A., Mbodji K., Hassan A., Aziz M., Boukhettala N., Coëffier M., Savoye G., Déchelotte P., Marion-Letellier R. Anti-inflammatory and anti-angiogenic effect of long chain n-3 polyunsaturated fatty acids in intestinal microvascular endothelium. Clin. Nutr. 2011;30:678–687. doi: 10.1016/j.clnu.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 139.Pannellini T., Iezzi M., Liberatore M., Sabatini F., Iacobelli S., Rossi C., Alberti S., Di Ilio C., Vitaglione P., Fogliano V., et al. A Dietary Tomato Supplement Prevents Prostate Cancer in TRAMP Mice. Cancer Prev. Res. 2010;3:1284–1291. doi: 10.1158/1940-6207.CAPR-09-0237. [DOI] [PubMed] [Google Scholar]
- 140.Perveen R., Suleria H.A.R., Anjum F.M., Butt M.S., Pasha I., Ahmad S. Tomato (Solanum lycopersicum) Carotenoids and Lycopenes Chemistry; Metabolism, Absorption, Nutrition, and Allied Health Claims—A Comprehensive Review. Crit. Rev. Food Sci. Nutr. 2015;55:919–929. doi: 10.1080/10408398.2012.657809. [DOI] [PubMed] [Google Scholar]
- 141.Hwang E.S., Bowen P.E. Can the consumption of tomatoes or lycopene reduce cancer risk? Integr. Cancer Ther. 2002;1:121–132. doi: 10.1177/153473540200100203. [DOI] [PubMed] [Google Scholar]
- 142.Palozza P., Simone R.E., Catalano A., Mele M.C. Tomato Lycopene and Lung Cancer Prevention: From Experimental to Human Studies. Cancers. 2011;3:2333–2357. doi: 10.3390/cancers3022333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zu K., Mucci L., Rosner B.A., Clinton S.K., Loda M., Stampfer M.J., Giovannucci E. Dietary Lycopene, Angiogenesis, and Prostate Cancer: A Prospective Study in the Prostate-Specific Antigen Era. J. Natl. Cancer Inst. 2014;106 doi: 10.1093/jnci/djt430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Bhatia N., Gupta P., Singh B., Koul A. Lycopene Enriched Tomato Extract Inhibits Hypoxia, Angiogenesis, and Metastatic Markers in early Stage N-Nitrosodiethylamine Induced Hepatocellular Carcinoma. Nutr. Cancer. 2015;67:1270–1277. doi: 10.1080/01635581.2015.1087040. [DOI] [PubMed] [Google Scholar]
- 145.Elgass S., Cooper A., Chopra M. Lycopene inhibits angiogenesis in human umbilical vein endothelial cells and rat aortic rings. Br. J. Nutr. 2012;108:431–439. doi: 10.1017/S0007114511005800. [DOI] [PubMed] [Google Scholar]
- 146.Chen M.L., Lin Y.H., Yang C.M., Hu M.L. Lycopene inhibits angiogenesis both in vitro and in vivo by inhibiting MMP-2/uPA system through VEGFR2-mediated PI3K-Akt and ERK/p38 signaling pathways. Mol. Nutr. Food Res. 2012;56:889–899. doi: 10.1002/mnfr.201100683. [DOI] [PubMed] [Google Scholar]
- 147.Treggiari D., Zoccatelli G., Chignola R., Molesini B., Minuz P., Pandolfini T. Tomato cystine-knot miniproteins possessing anti-angiogenic activity exhibit in vitro gastrointestinal stability, intestinal absorption and resistance to food industrial processing. Food Chem. 2017;221:1346–1353. doi: 10.1016/j.foodchem.2016.11.020. [DOI] [PubMed] [Google Scholar]
- 148.Cavallini C., Trettene M., Degan M., Delva P., Molesini B., Minuz P., Pandolfini T. Anti-angiogenic effects of two cystine-knot miniproteins from tomato fruit. Br. J. Pharmacol. 2011;162:1261–1273. doi: 10.1111/j.1476-5381.2010.01154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Treggiari D., Zoccatelli G., Molesini B., Degan M., Rotino G.L., Sala T., Cavallini C., Macrae C.A., Minuz P., Pandolfini T. A cystine-knot miniprotein from tomato fruit inhibits endothelial cell migration and angiogenesis by affecting vascular endothelial growth factor receptor (VEGFR) activation and nitric oxide production. Mol. Nutr. Food Res. 2015;59:2255–2266. doi: 10.1002/mnfr.201500267. [DOI] [PubMed] [Google Scholar]
- 150.Radd-Vagenas S., Kouris-Blazos A., Singh M.F., Flood V.M. Evolution of Mediterranean diets and cuisine: Concepts and definitions. Asia Pac. J. Clin. Nutr. 2017;26:749–763. doi: 10.6133/apjcn.082016.06. [DOI] [PubMed] [Google Scholar]
- 151.Hernández-Ledesma B., Hsieh C.C. Chemopreventive role of food-derived proteins and peptides: A review. Crit. Rev. Food Sci. Nutr. 2017;57:2358–2376. doi: 10.1080/10408398.2015.1057632. [DOI] [PubMed] [Google Scholar]
- 152.Medina M.A., Quesada A.R. Dietary proteins and angiogenesis. Nutrients. 2014;6:371–381. doi: 10.3390/nu6010371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Yoo Y.C., Watanabe S., Watanabe R., Hata K., Shimazaki K.I., Azuma I. Bovine Lactoferrin and Lactoferricin, a Peptide Derived from Bovine Lactoferrin, Inhibit Tumor Metastasis in Mice. Jpn. J. Cancer Res. 1997;88:184–190. doi: 10.1111/j.1349-7006.1997.tb00364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Shimamura M., Yamamoto Y., Ashino H., Oikawa T., Hazato T., Tsuda H., Iigo M. Bovine lactoferrin inhibits tumor-induced angiogenesis. Int. J. Cancer. 2004;111:111–116. doi: 10.1002/ijc.20187. [DOI] [PubMed] [Google Scholar]
- 155.Mader J.S., Smyth D., Marshall J., Hoskin D.W. Bovine Lactoferricin Inhibits Basic Fibroblast Growth Factor- and Vascular Endothelial Growth Factor165-Induced Angiogenesis by Competing for Heparin-Like Binding Sites on Endothelial Cells. Am. J. Pathol. 2006;169:1753–1766. doi: 10.2353/ajpath.2006.051229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Norrby K., Mattsby-Baltzer I., Innocenti M., Tuneberg S. Orally administered bovine lactoferrin systematically inhibits VEGF165-mediated angiogenesis in the rat. Int. J. Cancer. 2001;91:236–240. doi: 10.1002/1097-0215(200002)9999:9999<::AID-IJC1024>3.3.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 157.Strydom D.J., Bond M.D., Vallee B.L. An Angiogenic Protein from Bovine Serum and Milk—Purification and Primary Structure of Angiogenin-2. Eur. J. Biochem. 1997;247:535–544. doi: 10.1111/j.1432-1033.1997.00535.x. [DOI] [PubMed] [Google Scholar]
- 158.Silvestre J.S., Théry C., Hamard G., Boddaert J., Aguilar B., Delcayre A., Houbron C., Tamarat R., Blanc-Brude O., Heeneman S., et al. Lactadherin promotes VEGF-dependent neovascularization. Nat. Med. 2005;11:499–506. doi: 10.1038/nm1233. [DOI] [PubMed] [Google Scholar]
- 159.Sugano G., Bernard-Pierrot I., Laé M., Battail C., Allory Y., Stransky N., Krumeich S., Lepage M.L., Maille P., Donnadieu M.H., et al. Milk fat globule-epidermal growth factor-factor VIII (MFGE8)/lactadherin promotes bladder tumor development. Oncogene. 2011;30:642–653. doi: 10.1038/onc.2010.446. [DOI] [PubMed] [Google Scholar]
- 160.Neutzner M., López T., Feng X., Bergmann-Leitner E.S., Leitner W.W., Udey M.C. MFH-E8/lactadherin promotes tumor growth in an angiogenesis-dependent transgenic mouse model of multistage carcinogenesis. Cancer Res. 2007;67:6777–6785. doi: 10.1158/0008-5472.CAN-07-0165. [DOI] [PubMed] [Google Scholar]
- 161.Cã¡rdenas C., Quesada A.R., Medina M.A. Correction: Anti-Angiogenic and Anti-Inflammatory Properties of Kahweol, a Coffee Diterpene. PLoS ONE. 2011;6:e23407. doi: 10.1371/annotation/38262cc6-07cc-4074-8ce7-2181d4d0fbdc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Moeenfard M., Cortez A., Machado V., Costa R., Luís C., Coelho P., Soares R., Alves A., Borges N., Santos A. Anti-Angiogenic Properties of Cafestol and Kahweol Palmitate Diterpene Esters. J. Cell. Biochem. 2016;117:2748–2756. doi: 10.1002/jcb.25573. [DOI] [PubMed] [Google Scholar]
- 163.Niseteo T., Komes D., Belščak-Cvitanović A., Horžić D., Budeč M. Bioactive composition and antioxidant potential of different commonly consumed coffee brews affected by their preparation technique and milk addition. Food Chem. 2012;134:1870–1877. doi: 10.1016/j.foodchem.2012.03.095. [DOI] [PubMed] [Google Scholar]
- 164.Samanidou V.F., Tsagiannidis A., Sarakatsianos I. Simultaneous determination of polyphenols and major purine alkaloids in Greek Sideritis species, herbal extracts, green tea, black tea, and coffee by high-performance liquid chromatography-diode array detection. J. Sep. Sci. 2012;35:608–615. doi: 10.1002/jssc.201100894. [DOI] [PubMed] [Google Scholar]
- 165.Siasos G., Oikonomou E., Chrysohoou C., Tousoulis D., Panagiotakos D., Zaromitidou M., Zisimos K., Kokkou E., Marinos G., Papavassiliou A.G., et al. Consumption of a boiled Greek type of coffee is associated with improved endothelial function: The Ikaria Study. Vasc. Med. 2013;18:55–62. doi: 10.1177/1358863X13480258. [DOI] [PubMed] [Google Scholar]
- 166.Ros E. Contribution of nuts to the Mediterranean diet. In: Preedy V., Watson R., editors. The Mediterranean Diet: An Evidence-Based Approach. Academic Press; London, UK: 2015. pp. 175–184. [Google Scholar]
- 167.Smith A.N., Muffley L.A., Bell A.N., Numhom S., Hocking A.M. Unsaturated fatty acids induce mesenchymal stem cells to increase secretion of angiogenic mediators. J. Cell. Physiol. 2012;227:3225–3233. doi: 10.1002/jcp.24013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Nishioka N., Matsuoka T., Yashiro M., Hirakawa K., Olden K., Roberts J.D. Linoleic acid enhances angiogenesis through suppression of angiostatin induced by plasminogen activator inhibitor. Br. J. Cancer. 2011;105:1750–1758. doi: 10.1038/bjc.2011.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Moon E.J., Lee Y.M., Kim K.W. Anti-angiogenic activity of conjugated linoleic acid on basic fibroblast growth factor-induced angiogenesis. Oncol. Rep. 2003;10:617–621. [PubMed] [Google Scholar]
- 170.Masso-Welch P.A., Zangani D., Ip C., Vaughan M.M., Shoemaker S., Ramirez R.V., Ip M.M. Inhibition of angiogenesis by the cancer chemopreventive agent conjugated linoleic acid. Cancer Res. 2002;62:4383–4389. [PubMed] [Google Scholar]
- 171.Monastero R., García-Serrano S., Lago-Sampedro A., Rodríguez-Pacheco F., Colomo N., Morcillo S., Martín-Nuñez G.M., Gomez-Zumaquero J.M., García-Fuentes E., Soriguer F., et al. Methylation patterns of Vegfb promoter are associated with gene and protein expression levels: The effects of dietary fatty acids. Eur. J. Nutr. 2017;56:715–726. doi: 10.1007/s00394-015-1115-7. [DOI] [PubMed] [Google Scholar]
- 172.Bower A., Marquez S., Gonzalez de Mejia E. The health benefits of selected culinay herbs and spices found in the traditional mediterranean diet. Crit. Rev. Food Sci. Nutr. 2016;56:2728–2746. doi: 10.1080/10408398.2013.805713. [DOI] [PubMed] [Google Scholar]
- 173.Kubatka P., Kello M., Kajo K., Kruzliak P., Výbohová D., Mojžiš J., Adamkov M., Fialová S., Veizerová L., Zulli A., et al. Oregano demonstrates distinct tumour-suppressive effects in the breast carcinoma model. Eur. J. Nutr. 2017;56:1303–1316. doi: 10.1007/s00394-016-1181-5. [DOI] [PubMed] [Google Scholar]
- 174.López-Jiménez A., García-Caballero M., Medina M.A., Quesada A.R. Anti-angiogenic properties of carnosol and carnosic acid, two major dietary compounds from rosemary. Eur. J. Nutr. 2013;52:85–95. doi: 10.1007/s00394-011-0289-x. [DOI] [PubMed] [Google Scholar]
- 175.Kashyap D., Kumar G., Sharma A., Sak K., Tuli H.S., Mukherjee T.K. Mechanistic insight into carnosol-mediated pharmacological effects: Recent trends and advancements. Life Sci. 2017;169:27–36. doi: 10.1016/j.lfs.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 176.Theodoratou E., Timofeeva M., Li X., Meng X., Ioannidis J.P. Nature, nurture and cancer risks: Genetic and nutritional contributions to cancer. Annu. Rev. Nutr. 2017;37:293–320. doi: 10.1146/annurev-nutr-071715-051004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Picó C., Serra F., Rodríguez A.M., Keijer J., Palou A. Biomarkers of Nutrition and Health: New Tools for New Approaches. Nutrients. 2019;11:1092. doi: 10.3390/nu11051092. [DOI] [PMC free article] [PubMed] [Google Scholar]