Abstract
Background
The emergency department (ED) is the first point of care for many patients with concussion, and post-concussion syndrome can impact vocational outcomes like successful return to work. Evaluation of concussion in general adult populations is needed.
Aims
To document the occurrence and outcomes of work-related concussion presenting to the ED for treatment.
Methods
This study enrolled adults presenting with concussion to three urban Canadian EDs. Baseline ED interviews, physician questionnaires and patient phone interviews at 30 and 90 days documented work-related events, ED management, discharge advice, patient adherence and symptom severity. Work-related injury and return to work were modelled using logistic or linear regression, as appropriate.
Results
Overall, 172 enrolled workers completed at least one follow-up. Work-related concussions were uncommon (n = 28). Most employees (80%) missed at least 1 day of work (median = 7; interquartile range: 3–14). Most (91%) employees returned to work within 90 days, while 41% reported persistent symptoms. Manual labour and self-reported history of attention deficit hyperactivity disorder were associated with work-related concussion, while days of missed work increased with marital status (divorced), history of sleep disorder and physician’s advice to avoid work.
Conclusion
Work-related concussions are infrequent; however, most workers who sustain a concussion will miss work, and many return while still experiencing symptoms. Work-related concussion and days of missed work are mainly affected by non-modifiable factors. Workers, employers and the workers’ compensation system should take necessary precautions to ensure that workers return to work safely and successfully following a concussion.
Keywords: Accident and emergency departments, concussion, injury, occupational health
Key learning points.
What is already known about this subject:
• Concussions occur during everyday activities, including work, and most adults who sustain a concussion are employed.
• Misconceptions persist about the potential severity, signs and symptoms of concussions, and best-practice return-to-activity (i.e. work) recommendations.
• For many people with concussion, including injured workers, the first point of health contact occurs in the emergency department.
What this study adds:
• Although the majority (91%) of workers had returned to work within 90 days of their injury, a large proportion reported they were still experiencing symptoms.
• Although workers receiving return-to-work advice from the emergency physician stayed away from work longer, workers reported low adherence to the physician’s recommendations.
What impact this may have on practice or policy:
• Employers and the workers’ compensation system should be more mindful of the invisible nature of concussion symptoms and their potential impact on worker productivity following return to work.
• Validation of current sport-centric concussion guidelines for return-to-daily living and work activities may generate appropriate return-to-activity recommendations, including utilizing modified work activities to support safe return to work.
Introduction
Typically seen as sport injuries, concussions can produce short-term (e.g. headache, dizziness, confusion, etc.) and long-term (e.g., depression, sleep difficulties, cognitive impairment, etc.) symptoms that are a significant public health concern [1]. Although recent concussion research has focused on youth and elite athletes, the burden of concussions in the general population is concerning, as most concussions occur during daily living (e.g. driving, walking) or other non-sport activities [1]. Recently, efforts to understand the signs and symptoms, diagnosis, treatment and long-term sequelae of concussion [2] have increased, including post-concussion syndrome (PCS) which is characterized by the persistence of concussion symptoms past the usual time-to-recovery [3]. Despite this interest, misconceptions persist about the potential severity and signs and symptoms of concussions, as well as best-practice return-to-activity recommendations [4].
Research in non-athletes has paid little attention to work-related concussion and return to work (RTW) following concussion. For many people, including injured workers, the first point of health contact and the first opportunity to prevent PCS occurs in the emergency department (ED). Although most concussed workers return to work shortly after their injury, the high prevalence of concussions in North America may result in considerable lost productivity (i.e. presenteeism) for employers [5, 6]. This lost-productivity cost is in addition to those associated with poorer long-term mental, physical and socioeconomic outcomes for those workers unable to return to work due to PCS [7–9].
The objectives of this study were to document the occurrence of work-related concussion presenting to an ED for treatment. This study examines the work activities of those patients; the RTW advice they received; and the demographic, injury and treatment factors associated with work-related concussion and RTW outcomes.
Methods
The study protocol was approved by the Human Research Ethics Board at the University of Alberta (Pro00036497). A cohort study was carried out prospectively at three Canadian sites: one academic hospital with a dedicated trauma programme (Hospital 1; ~70 000 patients/year) and two community hospitals (Hospitals 2 and 3; combined ED census of ~115 000/year). All are 24-h EDs staffed by full-time emergency physicians and had one or more research assistants on site during the study period to enrol patients for multiple studies. The academic centre has a research programme with daily and weekend research coverage (~108 h/week), while the community hospitals had 40 h of weekly coverage. All physicians had access to a concussion-specific electronic clinical practice guideline (eCPG) through the local intranet. The eCPG had been developed previously with collaboration of emergency medicine, family medicine, neurosurgery, sports medicine, nursing, pharmacy, social work and psychology expertise utilizing the best evidence available at the time of development [10, 11]. This eCPG includes a handout for patients with information on usual symptoms and course of recovery, and a copy of the Sport Concussion Assessment Tool (SCAT)-2 to assist patients with self-evaluation of their symptoms at home [12].
English-speaking adults (≥17 years old) presenting with a Glasgow Coma Scale (GCS) score of 13–15 between April 2013 and April 2015, who met the World Health Organization Task Force on Mild Traumatic Brain Injury’s definition of concussion [5] and consented to participation were enrolled. GCS is a summary measure used to describe impaired consciousness; scores range from 15 (oriented and alert) to 3 (completely unresponsive); GSC <13 with history of head trauma is indicative of a brain injury more severe than a concussion.
Patients were excluded for the following reasons: loss of consciousness (LOC) >30 min; other significant injury (e.g. required intubation, hospitalized); structural brain injury seen on computed tomography (CT; e.g. intracranial haemorrhaging); non-traumatic cognitive impairment (e.g. substance use, dementia, etc.); history of neurological syndromes (e.g. epilepsy); history of recurrent falls in patients ≥65 years old; and repeat presentations for the same injury. Outwardly aggressive patients and those arriving via police escort were not approached for participation.
Enrolled patients were interviewed during their initial ED visit by trained staff using structured interview techniques to collect information on patient demographics (e.g. age, sex, marital status, etc.), circumstances of injury, symptoms immediately after the injury (e.g. LOC, headache, nausea, confusion, etc.) and current symptoms. Data on ED presentation, including mode of arrival, injury acuity (i.e. GCS and Canadian Triage Acuity Scale [CTAS] scores), signs and symptoms, and ED treatment, were extracted from patient charts and an electronic ED information system. CTAS prioritizes patients for care on a scale of 1 (requires resuscitation: should be seen by a doctor immediately) to 5 (non-urgent: should be seen by a doctor within 120 min). Additionally, the treating physician was asked to complete a structured questionnaire asking about diagnostic tests (e.g. CT, magnetic resonance imaging), treatments and RTW/sports advice provided to the patient. Although the concussion eCPG includes return-to-sport recommendations as part of the SCAT-2 [12], physicians were not required to follow these recommendations.
Patients were contacted at 30 and 90 days post-presentation to determine RTW status and persistence of symptoms, defined by a score ≥2 for any question of the Rivermead Post-concussion Questionnaire (RPQ). The RPQ is a validated questionnaire that asks patients to rate their concussion symptoms compared to before their injury on a scale of 0 (‘not experiencing at all’) to 5 (‘a severe problem’) [13]. Attempts at 90-day follow-ups were made for patients not reached at 30 days. All data were recorded onto standardized forms. Informed written and verbal consent was obtained from each patient before the baseline interview and for each follow-up, respectively. Written informed consent was obtained from physicians completing the physician questionnaire.
The sample size was a balance between what was practical and numbers that would provide reasonable 95% confidence intervals (CIs). Overall, a sample of 150 patients was expected to provide 95% CI ± ~8% for common outcomes (e.g. 50%; 95% CI 42–58), 95% CI ± ~5% for uncommon outcomes and 95% CI ± ~3% for rare outcomes.
All analyses were performed using STATA Statistical Software: Release 12 (StataCorp LP, College Station, TX, USA). The primary outcome was the proportion of patients with work-related concussions. Secondary outcomes included self-reported missed days of work and RTW with modified work restrictions. Factors potentially influencing these outcomes were also examined. Dichotomous variables were reported as percentages; continuous variables were reported as means and SDs or median and interquartile ranges (IQRs), as appropriate. Bi-variable comparisons of dichotomous data were completed using chi-square tests; continuous data were compared using t-tests or Mann–Whitney tests, as appropriate. Significance was set at P <0.05.
Two regression models were fit to examine: (i) factors associated with work-related concussion using multivariable logistic regression and (ii) the number of days of work missed using multivariable linear regression. Both regression models were built in a forward stepwise fashion: variables statistically significant at P <0.10 in a simple regression were added to the model 1 at a time in order of decreasing significance. Variables were removed from the model when P >0.05 in the combined model. Patients who were lost-to-follow-up were excluded from the regression analysis.
Results
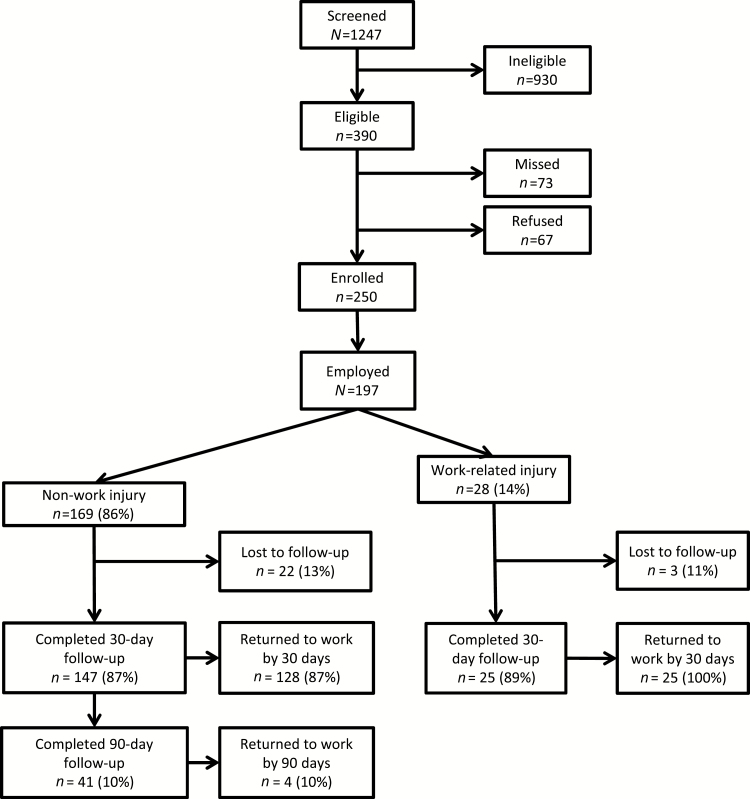
Enrolment and study flow are summarized in Figure 1. Only 73 potentially eligible patients presented to a study ED when no research staff were available, and 67 patients refused participation. Other reasons for exclusion were: presented >72 h after injury (n = 253); admitted to inpatient ward (n = 240); barriers to consent (i.e. neurological deficits, intoxication, language barrier, etc.; n = 140); and ‘other’ (n = 364), which included barriers to follow-up (e.g. no fixed address), history of neurological illness and intracranial haemorrhage, among others.
Figure 1.
Screening and enrolment for a study of employed patients with a concussion.
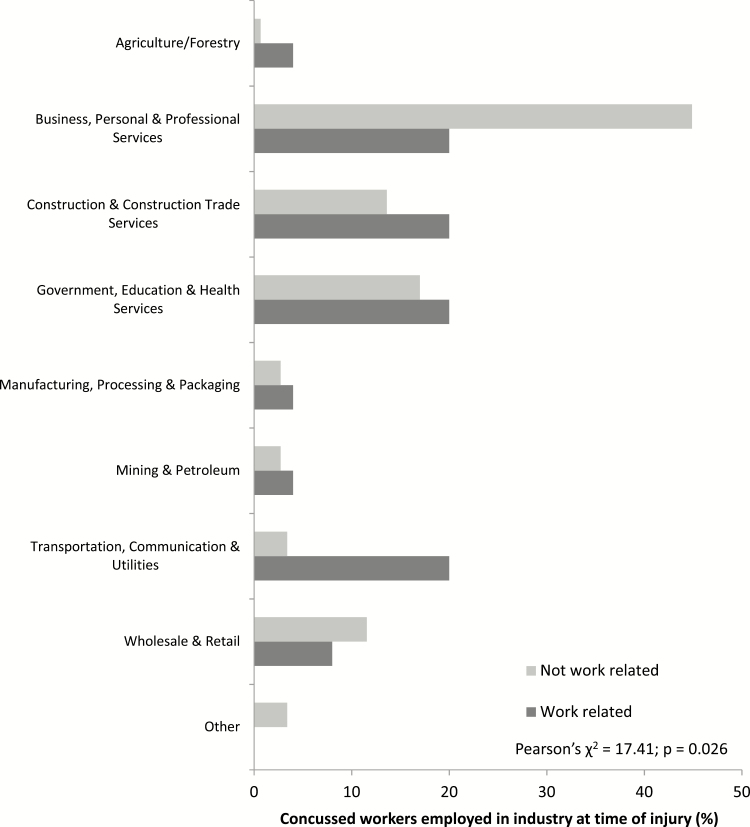
Overall, 197 employed patients (workers) were enrolled; 172 (87%) completed at least one follow-up (Figure 1). There were no differences between those who were contacted for follow-up and those who were unable to be contacted (Appendix 1). Demographics are presented by injury aetiology in Table 1. Employed patients who were concussed reported a variety of injury events, 14% of which occurred at work. Median age was 36 years, and 51% of concussed workers were male (n = 100). More work-related injuries involved males compared with workers concussed outside of work (Table 1; 68% versus 45%; Pearson’s χ 2 = 5.1876; P < 0.05). Patients injured at work were employed in different industries than those who were injured outside work (Figure 2; Pearson’s χ 2 = 17.41; P < 0.05). Most workers (120/197, 61%) reported physical labour was a regular part of their job, and 152/197 patients (77%) reported their job duties regularly required intensive mental concentration.
Table 1.
Characteristics of patients with concussion employed at their time of injury, by injury aetiology
| Variable | Total | Work-related injury | OR (95% CI) | |
|---|---|---|---|---|
| N = 197 | No, n = 169 | Yes, n = 28 | ||
| Median age in years (IQR) | 36 (24–48) | 36 (24–49) | 33.5 (24.5–46.5) | – |
| Male sex, n (%) | 100 (51) | 81(48) | 19 (68) | 2.29 (1.0–5.3) |
| Education, n (%)a | ||||
| Less than high school diploma | 16 (8) | 14 (8) | 2 (7) | Ref. |
| High school diploma | 55 (28) | 43 (25) | 12 (43) | 2.0 (0.4–9.8) |
| Some post-secondary | 28 (14) | 26 (15) | 2 (7) | 0.5 (0.1–4.2) |
| Post-secondary certificate, diploma or degree | 83 (42) | 72 (43) | 11 (39) | 1.1 (0.2–5.4) |
| One or more graduate degrees | 14 (7) | 13 (8) | 1 (4) | 0.5 (0.04–6.7) |
| Unknown/refused | 1 (1) | 1 (1) | 0 | – |
| Marital status, n (%)a | ||||
| Single | 84 (43) | 71 (42) | 13 (46) | Ref. |
| Married/common-law/living with partner | 84 (43) | 70 (41) | 14 (50) | 1.1 (0.5–2.5) |
| Divorced/separated /widowed | 28 (14) | 27 (16) | 1 (4) | 0.2 (0.03–1.6) |
| History of ADHD, n (%) | 18 (9) | 13 (8) | 5 (18) | 2.6 (0.8–7.9) |
| History of arthritis, n (%) | 30 (15) | 26 (15) | 4 (14) | 0.9 (0.3–2.8) |
| History of depression or anxiety, n (%) | 54 (27) | 47 (28) | 7 (25 | 0.9 (0.3–2.2) |
| History of depression or anxiety medication | 22 (11) | 20 (12) | 2 (7) | 0.7 (0.1–3.9) |
| History of sleep disorders, n (%) | 40 (20) | 32 (19) | 8 (32) | 1.7 (0.7–4.2) |
| History of chronic pain, n (%) | 37 (19) | 32 (19) | 5 (18) | 0.9 (0.3–2.6) |
| History of migraines, n (%) | 51 (26) | 43 (25) | 8 (32) | 1.2 (0.5–2.9) |
| Previous concussion(s), n (%) | 99 (50) | 85 (50) | 14 (50) | 1.0 (0.4–2.2) |
| Number of concussions, median (IQR) | 1 (1–3) | 1 (1–3) | 2 (1–4) | – |
aData missing for one patient.
Figure 2.
Industries of employed patients seeking care for a concussion in the ED.
Physicians commonly recommended avoidance of work (69%) and avoidance of sports (79%) after ED discharge. Patients injured at work were more likely to receive advice to miss work (odds ratio [OR] = 3.1; 95% CI 1.0–9.2) than those not injured at work. Patients’ self-reported adherence to avoidance advice was 36% and 40% for work and sports, respectively. Workers who sustained a work-related concussion received a median recovery timeline of 6 weeks (IQR: 4.5–15) compared with 3 weeks (IQR: 1.75–4.25) for workers injured outside work. Forty-one of the 250 (16%) patients were not diagnosed with concussion, despite meeting the study definition for diagnosis of concussion. Patients with a concussion diagnosis were significantly more likely to be advised to take time off of work (OR = 5.9; 95% CI 2.9–12.2).
The majority of workers (n = 137; 80%) missed at least 1 day of work as a result of their injury, with a median of 7 days (IQR: 3–14). While 91% of workers returned to work by 90 days, most did so within 30 days (81%); five concussed patients returned to work between 30 and 90 days (Table 2). Despite the high RTW rate, symptoms persisted at 90 days in 41% of workers (Table 2). Nineteen (11%) workers had modified work restrictions to accommodate their injury on RTW, which included reduced work hours (n = 5), limiting physical tasks (e.g., no lifting; n = 5), reduced work load (n = 3), limited computer use (n = 2) and limited operation of a motor vehicle (n = 1). Workers who returned with modified work restrictions missed significantly more days of work (median = 14; IQR: 7–30) than patients who returned without modified work restrictions (median = 7; IQR: 3–14; Mann–Whitney U = 650.0; z = −2.376; P < 0.05).
Table 2.
Outcomes of patients who sought care for a concussion in an ED, by injury aetiology
| Variable | Total | Work-related injury | OR (95% CI) | |
|---|---|---|---|---|
| N = 172 | No, n = 147 | Yes, n = 25 | ||
| RPQ score at baseline, median (IQR) | 17.5 (10–29) | 17 (10–29) | 18 (10–29) | – |
| RPQ score at 30 days, median (IQR) | 7.5 (0–23) | 8 (0–23) | 5.5 (0–22) | – |
| RPQ score at 90 days, median (IQR) | 6 (0–20) | 6 (2–20.5) | 4.5 (0–18) | – |
| Persistence of symptomsa at 30 days, n (%) | 107 (62) | 91 (62) | 16 (64) | 1.09 (0.45–2.64) |
| Persistence of symptomsa at 90 days, n (%) | 70 (41) | 61 (41) | 9 (36) | 0.79 (0.33–1.91) |
| Missed work, n (%) | 123 (72) | 107 (73) | 16 (64) | 0.66 (0.27–1.62) |
| Days, median (IQR) | 7 (3–14) | 7 (3–14) | 6 (3.5–15) | – |
| RTW by 30 days, n (%) | 151 (88) | 128 (87) | 23 (92) | 1.71 (0.37–7.83) |
| RTW by 90 days, n (%) | 156 (91) | 132 (90) | 24 (96) | 2.73 (0.31–21.62) |
| RTW with modified work restrictions | 19 (11) | 14 (10) | 5 (20) | 2.38 (0.77–7.33) |
| Returned to ED | 17 (10) | 15 (10) | 4 (16) | 1.96 (0.58–6.60) |
| Days to return, median (IQR) | 6 (4–9) | 5 (3–8) | 8 (6.5–25.5) | – |
aScore ≥2 on any question of the RPQ, per King et al. [13].
Variables fitted in the model for occurrence of work-related injury included: sex, age, employment requiring manual labour and history of attention deficit hyperactivity disorder (ADHD). All of these variables were retained in the final model (Table 3; McFadden’s pseudo-R2 = 0.1425; P < 0.001). While age and sex were non-significant, they were forced in the final model to correct for possible unidentified age and sex-related confounding. After adjusting for age, sex and history of ADHD, patients who performed manual labour were 10 times more likely to experience a work-related concussion compared with patients not performing manual labour (Table 3). After adjustment, patients with a history of ADHD were almost four times more likely to experience a work-related concussion compared with those without a history of ADHD (Table 3). ADHD and working in a job requiring manual labour did not exhibit collinearity in a sensitivity analysis regression of only those two variables (P > 0.05).
Table 3.
Multivariable logistic regression model of factors associated with occurrence of a work-related concussion among patients with concussion
| Variable | OR | df | 95% CI | z |
|---|---|---|---|---|
| Work-related concussion | ||||
| Age | 1.01 | 1 | 0.97–1.04 | 0.33 |
| Male sex | 1.23 | 1 | 0.46–3.30 | 0.41 |
| Manual labour | 10.28** | 1 | 2.17–48.61 | 2.94 |
| History of ADHD | 3.91* | 1 | 1.04–14.68 | 2.02 |
df, degrees of freedom.
*P < 0.05; **P < 0.01.
The regression model for factors associated with the number of days of missed work included: sex, age, marital status, medical history, symptoms (difficulty thinking or concentrating), measures of injury severity (ambulance arrival, CTAS score, receipt of head CT) and treatment (in-ED consult, physician advice, referrals to other therapeutic health services).
The model retained age, sex, marital status, CTAS score, history of a sleep disorder and emergency physician’s recommendation to avoid work (Table 4; adjusted R2 = 0.1447; P < 0.001). Once again, age and sex were non-significant but were retained in the final model to correct for possible unidentified age- and sex-related confounding. After adjustment, patients missed more days of work if they had a history of sleep disorders, were divorced/separated and if the treating physician advised they miss work (Table 4). While other types of treatment and recommendations, such as prescribed medications and recommendations for ‘physical rest’, ‘avoiding sports’ and ‘cognitive rest’, were examined, there were no associations with the number of days of work missed.
Table 4.
Multivariable linear regression model of factors associated with days of work missed by patients with concussion
| Variable | Coefficient | 95% CI | t |
|---|---|---|---|
| Age | −0.04 | −0.26 to 0.19 | −0.33 |
| Male sex | 3.76 | −1.95 to 9.46 | 1.30 |
| Marital status | |||
| Single | Ref. | – | – |
| Married/common law/living with partner | 9.49 | −3.39 to 10.37 | 1.0 |
| Divorced/separated/widowed | 12.33** | 3.13–21.53 | 2.65 |
| CTAS | |||
| 2 | 6.79* | 0.02–13.57 | 1.98 |
| 3 | Ref. | – | – |
| 4 | −4.57 | −11.33 to 2.19 | −1.34 |
| History of sleep disorder | 12.34** | 5.35–19.33 | 3.49 |
| Advice to miss work | 9.98** | 3.81–16.15 | 3.19 |
df, degrees of freedom.
*P < 0.05; **P < 0.01.
Discussion
A small proportion of concussions presenting to three EDs were work-related. Three-quarters of patients with concussion were employed, and nearly 80% of workers took time off work due to their injury. Adjusted analyses showed that work-related concussions in this sample were associated with a history of ADHD and working in a job involving manual labour. Days of missed work were higher in divorced patients, those reporting a history of a sleep disorder and those who received physician advice to miss work.
While this is the first prospective study of the ED treatment of concussions (both work-related and non-work-related) in workers, this study had several limitations. It is possible that missed patients (i.e. those presenting overnight) may have differed from the included patients, giving an incomplete picture of ED treatment of concussion in workers. While self-reported outcomes may have introduced recall bias, many of the symptoms of concussion are completely subjective and a patient’s experience of their symptoms cannot be measured in any other way. Similarly, it is possible that physicians who were aware of the study may have altered their usual treatment approach and that the treatment advice they reported is an over-estimate of actual behaviour. This study did not examine concurrent non-head injuries; however, strict inclusion criteria limited bias in outcomes due to multiple injuries. Finally, this study may be underpowered to detect factors contributing to work-related concussions. The low proportion of work-related injuries, combined with the complex nature of concussions and their recovery, may account for the relatively low measures of fit for both of the adjusted models.
Other prospective studies of concussion in adults also report that work-related events account for a modest proportion of concussions and that most concussed adults are employed at the time of their injury [14], are able to RTW within 1 month [6, 14–16] and frequently experience symptoms that persist beyond their RTW [14, 15]. Injury acuity and initial symptoms of a concussion do not appear associated with RTW status [17]. Although RTW advice may affect a patient’s time off of work, physician-related factors, rather than patients’ symptoms, may be more indicative of the RTW advice being provided [18]. Patients may also receive advice that they cannot adhere to or believe is irrelevant to their situation. This potential mismatch between a patient’s situation and the physician’s advice may partially explain the low adherence to RTW advice in this study; however, the current study was not designed to explore physician and adherence-related factors. Future investigations of factors affecting ED physician recommendations and patients’ responses to their delivery may elucidate more effective content and delivery of return-to-activity advice to support patients’ recovery. Moreover, similar to the use of graded return-to-sports activities recommended for athletes, the role of modified duties in successful RTW for workers with concussions warrants further exploration.
In the current study, patients who sustained a concussion at work took longer to RTW [19]; however, this study did not capture workers’ compensation claims, which could impact patients’ RTW. A successful claim may alleviate financial pressure to return to work before an injured worker is recovered or incentivize a worker not to return as soon as they were able. However, workers in Ontario, Canada reported that navigating the workers’ compensation remuneration system during concussion recovery was stressful for emotional, psychological and administrative reasons [20], and the stress associated with navigating the sometimes adversarial workers’ compensation system may delay recovery and increase symptom persistence in concussed workers [20, 21]. Although differences exist among workers’ compensation systems, future studies should work to elucidate the relationship between stress-induced concussion symptom persistence, which may affect both a patient’s ability to return to full health and the cost-effectiveness of disability compensation systems. Compensation case workers may benefit from education about the invisible disabilities resulting from concussion and the impacts of RTW when still symptomatic, as a large proportion of concussed workers do. Unfortunately, some employers do not make concessions to help patients reach full recovery after RTW or even address the hazard that initially led to injury [20]. Workers in jobs requiring manual labour should be mindful of the higher occurrence of workplace concussion and the well-documented increased risk of repeat injury.
Similar to previous findings [22], a considerable proportion of workers in this study experienced symptoms beyond 30 days. The substantive majority returned to work by 30 days, thereby undertaking physical and/or cognitive work, and the large proportion of patients returning to these activities with persistent symptoms is worrisome, as cognitive and physical activity in concussion patients has been linked to delayed recovery [23, 24]. RTW with persistent symptoms may affect not only their recovery, but also their productivity and overall work performance [25]. Employees performing manual labour are at higher risk of a concussion in the workplace [26, 27], and a higher risk of re-injury if they return while symptomatic [28], perhaps due to more hazardous workplaces, such as warehouses and construction sites, where machinery, physical obstacles and overhead objects are common. Employers should be aware of the dangers relevant in their industry and the type of work required and cooperate with employee requests to ensure a safe workplace and safe RTW after injury.
Unfortunately, best practice for RTW after a concussion is still unclear. Although interventional studies targeting persistent concussion symptoms are increasingly common, the current concussion guidelines were developed to assist athletes safely return to sports activities and have filtered into use for other populations without further evaluation of their effectiveness for return-to-general daily living and work activities. Validation of their use in a working population may shed light on appropriate RTW recommendations, including returning with modified work activities.
In conclusion, only one in ten working patients seen with concussion in the ED were injured at work. The usual period of time off from work may not be sufficient for resolution of concussion and/or PCS symptoms, which may affect workers’ abilities to fulfil their duties and may increase their risk of further injury. Collaboration between workers, employers and the workers’ compensation system should help workers safely and successfully return to work after a concussion.
Funding
This work was supported by the Workers’ Compensation Board of Alberta and the Canadian Institutes of Health Research (CIHR) (funder ID: 501100000024). L.E. was supported by a Frederick Banting and Charles Best Canada Graduate Scholarship from the CIHR (funder ID: 501100000024), the Health Quality Council of Alberta (HQCA) Studentship and the Walter H. Johns Graduate Fellowship from the University of Alberta (funder ID: 501100000190). At the time of the study, B.H.R. was supported by a Tier I Canada Research Chair (funder ID: 501100001804) in Evidence-based Emergency Medicine from the CIHR (funder ID: 501100000024) through the Government of Canada (Ottawa, Ontario) (funder ID: 501100000023). His research is currently supported by CIHR (funder ID: 501100000024) as the Scientific Director of the Institute of Circulatory and Respiratory Health (funder ID: 501100000028). The sponsors assume no responsibility for the conduct and opinions expressed in this manuscript.
Competing interests
None declared.
Supplementary Material
Acknowledgements
The authors would like to thank the research staff at the local hospitals who contributed to patient enrolment, follow-up and database management. The local site support from Dr Brian Deane (Sturgeon Community Hospital) and Dr Ed Berdusco (Northeast Community Health Center) was also greatly appreciated.
References
- 1. Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998–2000. Brain Inj 2005;19:85–91. [DOI] [PubMed] [Google Scholar]
- 2. Halstead ME, Walter KD; Council on Sports Medicine and Fitness American Academy of Pediatrics. Clinical report—sport-related concussion in children and adolescents. Pediatrics 2010;126:597–615. [DOI] [PubMed] [Google Scholar]
- 3. Leddy JJ, Sandhu H, Sodhi V, Baker JG, Willer B. Rehabilitation of concussion and post-concussion syndrome. Sports Health 2012;4:147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Eliyahu L, Kirkland S, Campbell S, Rowe BH. The effectiveness of early educational interventions in the emergency department to reduce incidence or severity of postconcussion syndrome following a concussion: a systematic review. Acad Emerg Med 2016;23:531–542. [DOI] [PubMed] [Google Scholar]
- 5. Cancelliere C, Kristman VL, Cassidy JD et al. Systematic review of return to work after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil 2014;95:S201–S209. [DOI] [PubMed] [Google Scholar]
- 6. Wäljas M, Iverson GL, Lange RT et al. Return to work following mild traumatic brain injury. J Head Trauma Rehabil 2014;29:443–450. [DOI] [PubMed] [Google Scholar]
- 7. Doctor JN, Castro J, Temkin NR, Fraser RT, Machamer JE, Dikmen SS. Workers’ risk of unemployment after traumatic brain injury: a normed comparison. J Int Neuropsychol Soc 2005;11:747–752. [DOI] [PubMed] [Google Scholar]
- 8. Beseoglu K, Roussaint N, Steiger HJ, Hänggi D. Quality of life and socio-professional reintegration after mild traumatic brain injury. Br J Neurosurg 2013;27:202–206. [DOI] [PubMed] [Google Scholar]
- 9. van der Horn HJ, Spikman JM, Jacobs B, van der Naalt J. Postconcussive complaints, anxiety, and depression related to vocational outcome in minor to severe traumatic brain injury. Arch Phys Med Rehabil 2013;94:867–874. [DOI] [PubMed] [Google Scholar]
- 10. Meurer D, Rowe B, Bullard M, Holroyd B. Using electronic clinical practice guidelines in emergency medicine. CJEM 2002;4:151–152. [Google Scholar]
- 11. Rowe B, Bullard M, Meurer D, Colman I, Holroyd B. The use of electronic clinical practice guideline resources in two Canadian emergency departments. Acad Emerg Med 2003;10:537. [Google Scholar]
- 12. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport—the Third International Conference on Concussion in Sport held in Zurich, November 2008. Phys Sportsmed 2009;37:141–159. [DOI] [PubMed] [Google Scholar]
- 13. King NS, Crawford S, Wenden FJ, Moss NE, Wade DT. The Rivermead Post Concussion Symptoms Questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol 1995;242:587–592. [DOI] [PubMed] [Google Scholar]
- 14. Losoi H, Silverberg ND, Wäljas M et al. Recovery from mild traumatic brain injury in previously healthy adults. J Neurotrauma 2016;33:766–776. [DOI] [PubMed] [Google Scholar]
- 15. van der Naalt J, van Zomeren AH, Sluiter WJ, Minderhoud JM. One year outcome in mild to moderate head injury: the predictive value of acute injury characteristics related to complaints and return to work. J Neurol Neurosurg Psychiatry 1999;66:207–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ruffolo CF, Friedland JF, Dawson DR, Colantonio A, Lindsay PH. Mild traumatic brain injury from motor vehicle accidents: factors associated with return to work. Arch Phys Med Rehabil 1999;80:392–398. [DOI] [PubMed] [Google Scholar]
- 17. Stulemeijer M, van der Werf S, Borm GF, Vos PE. Early prediction of favourable recovery 6 months after mild traumatic brain injury. J Neurol Neurosurg Psychiatry 2008;79:936–942. [DOI] [PubMed] [Google Scholar]
- 18. Silverberg ND, Iverson GL. Is rest after concussion ‘the best medicine?’: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil 2013;28:250–259. [DOI] [PubMed] [Google Scholar]
- 19. Pourat N, Kominski G, Roby D, Cameron M. Physician perceptions of access to quality care in California’s workers’ compensation system. J Occup Environ Med 2007;49:618–625. [DOI] [PubMed] [Google Scholar]
- 20. Mansfield E, Stergiou-Kita M, Cassidy JD et al. Return-to-work challenges following a work-related mild TBI: the injured worker perspective. Brain Inj 2015;29:1362–1369. [DOI] [PubMed] [Google Scholar]
- 21. King NS. Emotional, neuropsychological, and organic factors: their use in the prediction of persisting postconcussion symptoms after moderate and mild head injuries. J Neurol Neurosurg Psychiatry 1996;61:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cunningham J, Brison RJ, Pickett W. Concussive symptoms in emergency department patients diagnosed with minor head injury. J Emerg Med 2011;40:262–266. [DOI] [PubMed] [Google Scholar]
- 23. Brown NJ, Mannix RC, O’Brien MJ, Gostine D, Collins MW, Meehan WP 3rd. Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics 2014;133:e299–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Maerlender A, Rieman W, Lichtenstein J, Condiracci C. Programmed physical exertion in recovery from sports-related concussion: a randomized pilot study. Dev Neuropsychol 2015;40:273–278. [DOI] [PubMed] [Google Scholar]
- 25. Bottari C, Gosselin N, Chen JK, Ptito A. The impact of symptomatic mild traumatic brain injury on complex everyday activities and the link with alterations in cerebral functioning: exploratory case studies. Neuropsychol Rehabil 2017;27:871–890. [DOI] [PubMed] [Google Scholar]
- 26. Colantonio A, Comper P. Post-injury symptoms after work related traumatic brain injury in Canadian population. Work 2012;43:195–201. [DOI] [PubMed] [Google Scholar]
- 27. Chang VH, Lombard LA, Greher MR. Mild traumatic brain injury in the occupational setting. PM&R 2011;3:S387–S395. [DOI] [PubMed] [Google Scholar]
- 28. McCrea M, Guskiewicz K, Randolph C et al. Effects of a symptom-free waiting period on clinical outcome and risk of reinjury after sport-related concussion. Neurosurgery 2009;65:876–882; discussion 882. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.