Abstract
In the last few decades, many pathogenic or likely pathogenic genetic mutations in over hundred different genes have been described for non-ischemic, genetic cardiomyopathies. However, the functional knowledge about most of these mutations is still limited because the generation of adequate animal models is time-consuming and challenging. Therefore, human induced pluripotent stem cells (iPSCs) carrying specific cardiomyopathy-associated mutations are a promising alternative. Since the original discovery that pluripotency can be artificially induced by the expression of different transcription factors, various patient-specific-induced pluripotent stem cell lines have been generated to model non-ischemic, genetic cardiomyopathies in vitro. In this review, we describe the genetic landscape of non-ischemic, genetic cardiomyopathies and give an overview about different human iPSC lines, which have been developed for the disease modeling of inherited cardiomyopathies. We summarize different methods and protocols for the general differentiation of human iPSCs into cardiomyocytes. In addition, we describe methods and technologies to investigate functionally human iPSC-derived cardiomyocytes. Furthermore, we summarize novel genome editing approaches for the genetic manipulation of human iPSCs. This review provides an overview about the genetic landscape of inherited cardiomyopathies with a focus on iPSC technology, which might be of interest for clinicians and basic scientists interested in genetic cardiomyopathies.
Keywords: induced pluripotent stem cells, cardiomyopathies, cardiovascular genetics, cardiomyocytes, ARVC, DCM, HCM, RCM, NCCM, LVNC
1. Introduction
At the beginning of this century, the human genome project was finished [1]. The development of next generation sequencing (NGS) technologies significantly reduced the price and time, allowing for efficient genome and exome analyses, even in clinical routine procedures. However, even 20 years later, the clinical interpretation of genetic sequence variants (GSVs) is still challenging because the functional and structural impact of many variants is unknown. Therefore, multi-disciplinary approaches are often necessary for the interpretation and functional analysis of novel GSVs [2]. At present, in clinical routine procedures, the pathological impact of GSVs is classified due to standards and guidelines of the American College of Medical Genetics and Genomics (ACMG) [3].
Cardiomyopathies are diseases that affect the heart muscle, leading to functional and structural abnormalities [4], and are the main indication for heart transplantation (HTx) [5]. Beside environmental factors, like myocarditis or cardiotoxicity of cancer drugs, non-ischemic cardiomyopathies often have a genetic etiology with dominant inheritance. However, because pathogenic mutations in more than 100 different genes are associated with non-ischemic cardiomyopathies, the interpretation of novel GSVs is still challenging [6]. Moreover, little is currently known on digenic, or even polygenic, etiologies of cardiomyopathies [7]. Incomplete penetrance, different expressivity, and pleiotropy make the clinical interpretation even more challenging.
Functional analyses using adequate cell and animal models can lead to a more sophisticated interpretation of GSVs, which might be not only relevant for genetic counseling but also for the development of personalized therapies. According to the ACMG guidelines, in vitro or/and in vivo functional analyses provide strong criteria (PS3) for the classification of GSVs [3,8]. However, the generation of animal models is still time consuming and expensive. Moreover, in some cases, human cardiomyopathies cannot be modeled using animal models because of species differences. For example, TMEM43-p.S358L is a mutation with full penetrance in several families with arrhythmogenic cardiomyopathy (ACM) [9,10,11]. In contrast, the Tmem43 knock-out, as well as the knock-in mice carrying this specific mutation, do not develop an ACM phenotype [12]. Because of these limitations, human iPSC-derived cardiomyocytes are unprecedented research tools to model and investigate genetic cardiomyopathies.
Here, we provide an overview about the genetic landscape of inherited cardiomyopathies and summarize the development of important human iPSC lines for modelling human cardiomyopathies in vitro. In addition, we review the differentiation into cardiomyocytes and discuss relevant methods used for the cellular and molecular characterization of human iPSC-derived cardiomyocytes.
2. Clinical Background
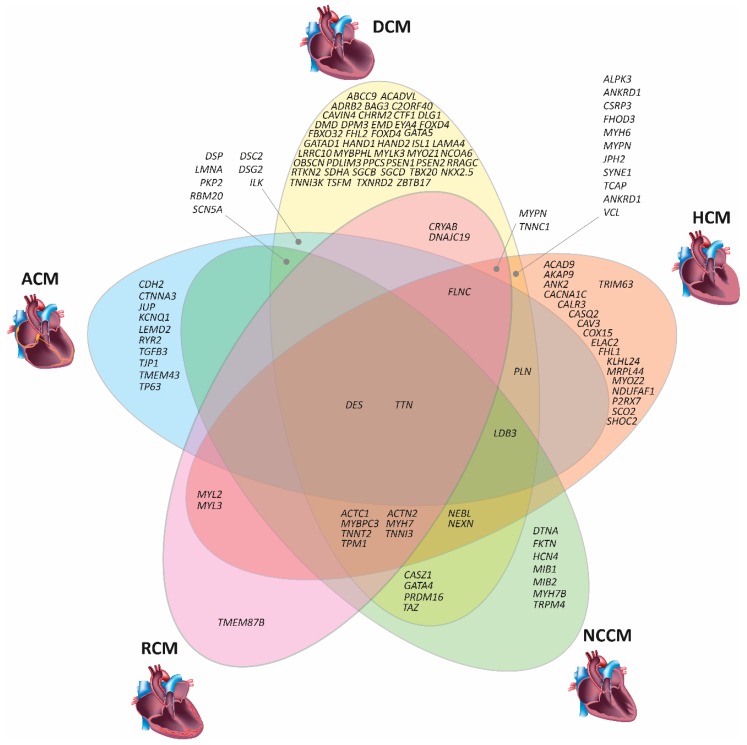
In clinical cardiology, cardiomyopathies are classified into five major structural subtypes (Figure 1). Dilated cardiomyopathy (DCM, MIM #604145) is mainly characterized by left-ventricular dilation in combination with a decrease of the wall diameter [13]. These structural changes decrease the cardiac ejection fraction. Hypertrophic cardiomyopathy (HCM, MIM #160760) is characterized by the hypertrophy of the ventricular walls and/or the septum [14], leading to a reduced cardiac output. Restrictive cardiomyopathy (RCM, MIM #115210) is caused by an increase in ventricular stiffness, leading to dilated atria and diastolic dysfunction [15]. Hyper-trabeculation of the left ventricular wall is a hallmark for (left-ventricular) non-compaction cardiomyopathy (NCCM, MIM #604169) [16]. It mainly affects the left ventricle, but isolated right ventricular or biventricular forms of NCCM have been reported [17]. Ventricular arrhythmias and predominant right or biventricular dilation are the main clinical symptoms of ACM (MIM #609040) [18]. The fibro fatty replacement of the myocardial tissue is a pathognomonic feature characteristic of ACM [19]. However, at the early stage of the disease, structural changes may be absent or subtle [20]. Because ACM is a progressive disease, left ventricular involvement develops frequently at a later stage [21].
Figure 1.
Schematic overview on cardiomyopathy associated genes and related clinical phenotypes. DCM—Dilated cardiomyopathy. HCM—Hypertrophic cardiomyopathy, ACM—Arrhythmogenic cardiomyopathy, NCCM—Non-compaction cardiomyopathy, RCM—Restrictive cardiomyopathy (Images of the DCM or HCM heart were licensed from shutterstock.com).
3. Genetic Basis of Inherited Cardiomyopathies
Thirty years ago, Seidmans’ group discovered the first pathogenic mutation in MYH7, encoding for β-myosin heavy chain, in a four-generation family, in which several members developed HCM [22]. At present, genetic variants have been described in more than 100 different genes associated with non-ischemic cardiomyopathies or syndromes with cardiac involvement such as Marfan or Leopard syndrome (for an overview, see Table 1). Of note, the spectrum of affected genes and mutations partially overlaps between the different non-ischemic cardiomyopathies (Figure 1). For example, mutations in DES, encoding the muscle specific intermediate filament protein desmin, might cause DCM [23,24], HCM [25], ACM [26,27], RCM [28], or NCCM [29,30,31]. Similarly, mutations in TTN, encoding the giant sarcomere protein titin, can also cause different types of structural, non-ischemic cardiomyopathies [32,33,34]. However, the molecular reasons why mutations in the same gene can cause different cardiac phenotypes are largely unknown.
Table 1.
Overview of cardiomyopathy associated genes carrying mutations.
| Gene | Protein | Function | HCM | DCM | NCCM | ACM | RCM |
|---|---|---|---|---|---|---|---|
| ABCC9 | ATP Binding Cassette Subfamily C Member 9 | ABC transporter | [77] | ||||
| ACAD9 | Acyl-CoA Dehydrogenase Member 9 | Dehydrogenase | [78] | ||||
| ACADVL | Acyl-CoA Dehydrogenase Very Long Chain | Dehydrogenase | [79] | ||||
| ACTC1 | Cardiac Actin | Sarcomere protein | [43,80] | [81] | [82] | [83] | |
| ACTN2 | α-Actinin 2 | Z-band protein | [84] | [85] | [86] | [69] | |
| ADRB2 | Adrenoreceptor β2 | G-protein coupled receptor | [87] | ||||
| AKAP9 | A Kinase Anchoring Protein 9 | Scaffolding protein | [88] | ||||
| ALMS1 | Alstrom Syndrome Protein 1 | Microtubule organization | [89] 1 | ||||
| ALPK3 | α-Kinase 3 | Kinase | [90] | [90] | |||
| ANK2 | Ankyrin 2 | Cytoskeleton linker protein | [91] | [92] | |||
| ANKRD1 | Ankyrin Repeat Domain Containing Protein 1 | Transcription factor | [93] | [94,95] | |||
| BAG3 | Bcl-2 Associated Athanogene 3 | Co-chaperone | [96] | [69,97] | |||
| BRAF | B-Raf Proto-Oncogene, Serine/Threonine Kinase | Kinase | [98] 2 | ||||
| C2ORF40 | Chromosome 2 Open Reading Frame 40 | Hormone | [99] | ||||
| CACNA1C | Calcium Voltage-Gated Channel Subunit α1C | Calcium channel | [100] | ||||
| CALM3 | Calmodulin 3 | Calcium binding | [101] 3 | ||||
| CALR3 | Calreticulin 3 | Calcium binding chaperone | [46] | ||||
| CASQ2 | Calsequestrin 2 | Calcium binding | [46] | ||||
| CASZ1 | Castor Zinc Finger 1 | Transcription factor | [102] | [103] | |||
| CAV3 | Caveolin 3 | Scaffolding protein | [104] | ||||
| CAVIN4 | Muscle Restricted Coiled Coil Protein | Myofibrillar organization | [105] | ||||
| CDH2 | N-Cadherin | Cell–cell adhesion | [106,107] | ||||
| CHRM2 | Cholinergic Receptor Muscarinic 2 | G-protein coupled receptor | [108] | ||||
| COL3A1 | Collagen Type III Alpha 1 Chain | Extra cellular matrix protein | [109] 4 | ||||
| COX15 | Cytochrome C Oxidase Assembly Homolog COX15 | Mitochondrial respiratory chain | [110] | ||||
| CRYAB | αB-Crystallin | Chaperone-like activity | [111] | [112] | |||
| CSRP3 | Muscle LIM Protein | Scaffolding protein | [113,114,115] | [116] | |||
| CTF1 | Cardiotrophin 1 | Cytokine | [117] | ||||
| CTNNA3 | αT-Catenin | Cell–cell adhesion | [118] | ||||
| DES | Desmin | Intermediate filament protein | [25] | [24,119] | [30] | [26] | [28] |
| DLG1 | Discs Large MAGUK Scaffold Protein 1 | Scaffolding protein | [88] | ||||
| DMD | Dystrophin | Dystrophin–glycoprotein complex | [120] | ||||
| DNAJC19 | DNAJ Heat Shock Protein Family C19 | Co-chaperone | [121] | [121] | |||
| DOLK | Dolichol Kinase | Phosphorylation of dolichol | [122] 5 | ||||
| DPM3 | Dolichyl-Phosphate Mannosyltransferase Subunit 3 | Mannosyltransferase | [123] | ||||
| DSC2 | Desmocollin 2 | Cell–cell adhesion | [35] | [124] | |||
| DSG2 | Desmoglein 2 | Cell–cell adhesion | [125] | [126,127] | |||
| DSP | Desmoplakin | Cell–cell adhesion | [128] | [129] | [130] | ||
| DTNA | α-Dystrobrevin | Dystrophin-glycoprotein complex | [131] | ||||
| ELAC2 | ElaC Ribonuclease Z2 | 3′-tRNA endoribonuclease | [132] | ||||
| EMD | Emerin | Nuclear lamina associated protein | [133] | ||||
| EYA4 | Eyes Absent Homolog 4 | Transcription factor | [51] | ||||
| FBN1 | Fibrillin 1 | Extra cellular matrix protein | [134] 6 | [135] 7 | [136] 7 | ||
| FBXO32 | F-Box Only Protein 32 | Ubiquitin–protein ligase complex | [137,138] | ||||
| FHL1 | Four and a Half LIM Domain Protein 1 | Scaffolding protein | [41] | ||||
| FHL2 | Four and a Half LIM Domain Protein 2 | Scaffolding protein | [139] | ||||
| FHOD3 | Formin Homology 2 Domain Containing Protein 3 | Organization of actin-polymerization | [140] | [141] | |||
| FKRP | Fukutin Related Protein | Posttranslational modification of dystroglycan | [142] 8 | ||||
| FKTN | Fukutin | Glycosyltransferase of dystroglycan | [143] | ||||
| FLNC | Filamin C | Cell junction organization | [45] | [144,145] | [145] | [72] | |
| FOXD4 | Forkhead Box Protein D4 | Transcription factor | [146] | ||||
| FXN | Frataxin | Regulation of mitochondrial iron transport | [147] 9 | ||||
| GAA | α-Glucosidase | Glycogen metabolism | [148] 9 | ||||
| GATA4 | GATA Binding Protein 4 | Transcription factor | [149] | [150] 10 | |||
| GATA5 | GATA Binding Protein 5 | Transcription factor | [151] | ||||
| GATAD1 | GATA Zink Finger Domain Containing Protein 1 | Gene expression regulation | [152] | ||||
| GLA | Galactosidase α | Galactose metabolism | [153] 11 | ||||
| GTPBP3 | GTP Binding Protein 3, Mitochondrial | Mitochondrial tRNA modification | [154] 12 | ||||
| HAND1 | Heart and Neural Crest Derivatives Expressed 1 | Transcription factor | [155] | ||||
| HAND2 | Heart and Neural Crest Derivatives Expressed 2 | Transcription factor | [156] | ||||
| HCN4 | Hyperpolarization Activated Cyclic Nucleotide Gated Potassium Channel 4 | Potassium channel | [157] | ||||
| HRAS | HRas Proto-Oncogene GTPase | Signaling protein | [158]13 | ||||
| ILK | Integrin Linked Kinase | Scaffolding protein | [159,160] | [68] | |||
| ISL1 | ISL LIM Homeobox 1 | Transcription factor | [161] | ||||
| ITGA7 | Integrin Subunit A7 | Cell–cell and cell–matrix junction protein | [162] 14 | ||||
| ITPA | Inosine Triphosphate Pyrophosphatase | Nucleotide metabolism | [163] 15 | ||||
| JPH2 | Junctophilin 2 | Junctional complex | [164] | [165] | |||
| JUP | Plakoglobin | Cell–cell adhesion | [58] | ||||
| KCNQ1 | Potassium Channel Voltage Gated KQT-Like Subfamily Member 1 | Potassium channel | [166] | ||||
| KLHL24 | Kelch Like 24 | Ubiquitin ligase substrate receptor | [167] | ||||
| LAMA4 | Laminin α4 | Extra cellular matrix protein | [159] | ||||
| LAMP2 | Lysosomal Associated Membrane Protein 2 | Chaperone-mediated autophagy | [168] 16 | ||||
| LDB3 | LIM Domain Binding Protein 3 | Z-band protein | [169] | [170,171] | [170,172] | [173] | |
| LEMD2 | LEM Domain Containing Protein 2 | Nuclear lamina associated protein | [64,174] 17 | ||||
| LMNA | Lamin A/C | Nuclear lamina associated protein | [49] | [175] | [63] | ||
| LRRC10 | Leucine Rich Repeat Containing Protein 10 | Actin and α-actinin binding protein | [176] | ||||
| MIB1 | Mindbomb Drosophila Homolog 1 | Ubiquitin ligase | [177] | ||||
| MIB2 | Mindbomb Drosophila Homolog 2 | Ubiquitin ligase | [178] 18 | ||||
| MRPL3 | Mitochondrial Ribosomal Protein L3 | Mitochondrial ribosomal protein | [179] 19 | ||||
| MRPL44 | Mitochondrial Ribosomal Protein L44 | Mitochondrial ribosomal protein | [180,181] | ||||
| MYBPC3 | Myosin Binding Protein C3 | Sarcomere protein | [182,183] | [184] | [185] | [186] | |
| MYBPHL | Myosin Binding Protein H-Like | Sarcomere protein | [187] | ||||
| MYH6 | Myosin Heavy Chain 6 | Sarcomere protein | [188] | [188] | |||
| MYH7 | Myosin Heavy Chain 7 | Sarcomere protein | [22] | [48] | [7] | [189] | |
| MYH7B | Myosin Heavy Chain 7B | Sarcomere protein | [162] 20 | ||||
| MYL2 | Myosin Light Chain 2 | Sarcomere protein | [190] | [191] | |||
| MYL3 | Myosin Light Chain 3 | Sarcomere protein | [192] | [192] | |||
| MYLK3 | Myosin Light Chain Kinase 3 | Kinase | [193] | ||||
| MYOZ1 | Myozenin 1 | Calcineurin interacting protein | [194] | ||||
| MYOZ2 | Myozenin 2 | Calcineurin interacting protein | [195] | ||||
| MYPN | Myopalladin | Z-band protein | [196] | [94,197] | [196,198] | ||
| NCOA6 | Nuclear Receptor Coactivator 6 | Gene expression regulation | [199] | ||||
| NDUFAF1 | NADH: Ubiquinone Oxidoreductase Complex Assembly Factor 1 | Mitochondrial respiratory chain | [200] | ||||
| NDUFV2 | NADH: Ubiquinone Oxidoreductase Core Subunit V2 | Mitochondrial respiratory chain | [201,202] 21 | ||||
| NEBL | Nebulette | Z-band protein | [203] | [204] | [203] | ||
| NEXN | Nexilin | Sarcomere protein | [205] | [206] | [207] | ||
| NKX2.5 | NK2 Homeobox 5 | Transcription factor | [208] | ||||
| OBSCN | Obscurin | Scaffolding protein | [209] | ||||
| P2RX7 | Purinergic receptor P2X7 | ATP gated ion channel | [210] | ||||
| PDLIM3 | PDZ And LIM Domain 3 | Z-band protein | [194] | ||||
| PKP2 | Plakophilin 2 | Cell-cell adhesion | [35] | [211] | [212] | ||
| PLN | Phospholamban | Regulator of SERCA | [46] | [213,214] | [67] | ||
| PPCS | Phosphopantothenoylcystein Synthetase | Co-enzyme A synthesis | [215] | ||||
| PRDM16 | PR Domain Containing Protein 16 | Transcription factor | [216] | [217] | |||
| PRKAG2 | Protein Kinase AMP Activated Non-catalytic G2 | Energy sensor kinase | [218,219] 22 | ||||
| PSEN1 | Presenilin 1 | γ-Secretase | [220,221] | ||||
| PSEN2 | Presenilin 2 | γ-Secretase | [220] | ||||
| PTEN | Phosphatase and Tensin Homolog | Phosphatase | [150] 23 | ||||
| PTPN11 | Protein Tyrosine Phosphatase Non-Receptor Type 1 | Phosphatase | [222] 24 | ||||
| RAF1 | Raf-1 Proto-Oncogene, Serine/Threonine Kinase | Kinase | [223,224] 25 | [225] | |||
| RBM20 | RNA Binding Protein 20 | Splicing factor | [52,226] | [227] | [228,229] | ||
| RRAGC | Ras Related GTP Binding C | GTR/RAG GTP-binding protein | [230] | ||||
| RTKN2 | Rhotekin 2 | Scaffolding protein | [99] | ||||
| RYR2 | Ryanodine Receptor 2 | Calcium channel | [66] | ||||
| SCN5A | Sodium Channel Voltage Gated Type V Subunit A | Sodium channel | [50,231] | [232] | |||
| SCO2 | SCO2 Cytochrome C Oxidase Assembly Protein | Metallo-chaperone | [233] | ||||
| SDHA | Succinate Dehydrogenase Complex Subunit A | Mitochondrial respiratory chain | [234] | ||||
| SGCB | Sarcoglycan β | Dystrophin-glycoprotein complex | [235] | ||||
| SGCD | Sarcoglycan δ | Dystrophin-glycoprotein complex | [236] | ||||
| SHOC2 | Suppressor Of Clear, C. Elegans, Homolog | Scaffolding protein | [237] | ||||
| SYNE1 | Nesprin 1 | Component of the LINC complex | [238] | [239] | |||
| TAZ | Tafazzin | Cardiolipin metabolism | [240] 26 | [241,242] | |||
| TBX20 | T-Box Factor 20 | Transcription factor | [243,244] | ||||
| TCAP | Thelethonin | Titin binding | [245] | [244,245] | |||
| TGFB3 | Transforming Growth Factor β3 | Growth factor | [246] | ||||
| TJP1 | Zonula Occludens 1 | Tight junction adapter protein | [247] | ||||
| TMEM43 | Transmembrane Protein 43 | Nuclear lamina associated protein | [9,10] | ||||
| TMEM87B | Transmembrane Protein 87B | Endosome-to-trans-Golgi retrograde transport | [248] | ||||
| TNNC1 | Cardiac Troponin C | Sarcomere protein | [39] | [249] | [250] | ||
| TNNI3 | Cardiac Troponin I | Sarcomere protein | [40] | [251] | [252] | [71] | |
| TNNI3K | TNNI3 Interacting Kinase | Kinase | [253] | ||||
| TNNT2 | Cardiac Troponin T | Sarcomere protein | [38] | [254] | [255] | [83] | |
| TP63 | Tumor Protein 63 | Transcription factor | [256] | ||||
| TPM1 | Tropomyosin 1 | Sarcomere protein | [38,257] | [258] | [259] | [191] | |
| TRIM63 | Tripartite Motif Containing Protein 63 | Ubiquitin ligase | [260] | ||||
| TRPM4 | Transient Receptor Potential Cation Channel Subfamily M | Cation channel | [261] | ||||
| TSFM | Mitochondrial Translation Elongation Factor Ts | Translation elongation factor | [262] | ||||
| TTN | Titin | Sarcomere protein | [263] | [32,264] | [87,265] | [33] | [34] |
| TTR | Transthyretin | Carrier protein | [266,267] 27 | ||||
| TXNRD2 | Thioredoxin Reductase 2 | Reduces thioredoxins | [268] | ||||
| VCL | Vinculin | Cell–cell and cell–matrix junction protein | [269,270] | [271] | |||
| ZBTB17 | Zinc Finger and BTB Domain Containing Protein 17 | Transcription factor | [272,273] |
1 Alström syndrome (MIM #203800); 2 Cardiofaciocutaneous syndrome (MIM #115150); 3 Modifier gene; 4 Ehlers–Danlos syndrome (MIM #130090); 5 Multi-organ involvement; 6 Digenetic with PTPN11 mutations, combined with Marfan and Leopard syndrome; 7 Marfan Syndrome (MIM #154700); 8 Limb-girdle muscular dystrophy; 9 Friedreich ataxia (MIM #229300); 10 Digenetic with PTEN; 11 Fabry disease; 12 In combination with lactic acidosis and encephalopathy; 13 Costello syndrome (MIM #218040); 14 Digenetic with MYH7B;15 Martsolf-like syndrome (MIM #212720) in combination with DCM; 16 Danon disease (MIM #300257); 17 In combination with cataract; 18 In combination with giant hypertrophic gastritis (MIM #137280, Ménétrier disease); 18 In combination with psychomotor retardation; 19 Digenetic with ITGA7; 20 In combination with encephalopathy; 21 Wolff–Parkinson–White syndrome (MIM #194200); 22 Digenetic with GATA4 mutation; 23 Noonan syndrome; 24 Noonan syndrome or Leopard syndrome; 25 Barth syndrome (MIM #302060); 26 Amyloid cardiomyopathy (MIM #105210); 27 Fabry disease.
From a genetic point of view, non-ischemic cardiomyopathies are quite heterogeneous [35,36,37]. However, the different non-ischemic cardiomyopathies are characterized by an accumulation of mutations in a distinct set of genes encoding for proteins that are essential for cardiomyocyte function. For example, HCM is mainly caused by mutations in genes encoding sarcomeric proteins such as MYH7 or MYBPC3 (Figure 1). Further mutations in other genes, encoding sarcomere proteins, like TPM1 [38], TNNC1 [39], TNNI3 [40], TNNT2 [38], FHL1 [41,42], or ACTC1 [43], have also been identified in patients with HCM (Table 1). In addition, in rare cases, mutations in genes encoding for Z-disc proteins, like ACTN2 [44] or FLNC [45], or genes encoding for proteins involved in the Ca2+-homeostasis like PLN [46], are also known to cause HCM (see Figure 1).
TTN is the most prevalent DCM-related gene with truncating TTN mutations identified in about 20–25% of DCM patients [32,47]. However, several other genes with a lower prevalence can also cause DCM. Besides, mutations have been identified in genes coding proteins of the sarcomere (e.g., MYH7 [48]), the cytoskeleton (e.g., DES [23,24]), the nuclear lamina (e.g., LMNA [49]), ion channels (e.g., SCN5A [50]), and transcription (e.g., EYA4 [51]) or splicing factors (e.g., RBM20 [52]) (Table 1). RBM20 mutations cause an aggressive early onset phenotype including arrhythmias, sudden cardiac death, and DCM, especially in males [53]. In total, mutations associated with DCM have been described in about 80 different genes (see Figure 1 and Table 1).
NCCM is the third most frequent non-ischemic cardiomyopathy [54,55] and can occur as a primary cardiomyopathy or can be part of a syndromic disease like the Barth syndrome (MIM, #302060) [56]. Mutations in over 20 different genes having a significant overlap with HCM- or DCM-associated genes have been described in NCCM patients so far (see Figure 1 and Table 1). Comparable to HCM, the most prevalent NCCM-associated genes are MYH7 and MYBPC3 [57], which encode sarcomeric proteins (Table 1).
ACM is mainly caused by mutations in genes, encoding structural components of the cardiac desmosomes, and adherens junctions [26,58,59]. The cardiac desmosomes are cell–cell junctions mediating the adhesion of the cardiomyocytes [60]. In about 50% of the ACM patients, one or more mutations in desmosomal genes can be identified [26,59,61] (Table 1). Cardiac desmosomes are linked through the intermediate filaments formed mainly by desmin (DES) with several other cell organelles like the Z-bands or the nuclei. Of note, mutations in the DES gene can also cause ACM by abnormal cytoplasmic desmin aggregation [26,62]. In addition, mutations in genes of the nuclear envelope like LMNA [63], TMEM43 [9,10], or LEMD2 [64] are associated with ACM (Table 1). Furthermore, some rare mutations in non-desmosomal and non-nuclear genes like RYR2 [65,66], PLN [67], or ILK [68] have been identified in ACM patients.
Currently, the genetic etiology of RCM is poorly characterized. Recently, Kostareva et al. and Gallego-Delgado et al. genotyped two small cohorts of unrelated RCM index patients and identified likely pathogenic or pathogenic mutations in 50–75% of them [69,70]. The majority of affected RCM genes, which partially overlap with the group of HCM-associated genes, encode for sarcomere or cytoskeleton proteins (see Figure 1 and Table 1). The first RCM-associated mutation was identified in TNNI3, encoding cardiac troponin I [71]. More recently, there is growing evidence that FLNC mutations, encoding the cytolinker protein filamin-C, are frequently associated with RCM [72,73,74,75,76].
In summary, a relevant amount of all non-ischemic cardiomyopathies have a genetic etiology. Although in most cases, cardiomyopathies are inherited monogenetically, the underlying genetic landscape is complex, diverse, and currently only partially known.
4. Generation of Patient-Specific-Induced Pluripotent Stem Cells Via Reprogramming
In the 1960s, Gurdon et al. cloned Xenopus laevis for the first time [274,275]. Consequently, Gurdon was awarded the Nobel Prize in medicine in 2012, together with Yamanaka [276]. The cloning of mammals by nuclear transfer from somatic cells into enucleated unfertilized mammalian eggs over twenty years ago demonstrated that the cellular differentiation can be artificially turned back into a pluripotent state [277]. The next breakthrough was the identification of essential reprogramming factors by the Yamanaka group [278,279]. Initially, reprogramming was performed with 24 candidate transcription factor genes. Out of these, four critical genes were identified to be crucial for iPSC generation: Sox2, Oct4, Klf4, and c-Myc [278]. Depending on the donor cell type, the set of reprogramming factors can vary since specific cell types might endogenously express some of the necessary factors. For example, c-Myc is not required for the reprogramming of fibroblasts [280].
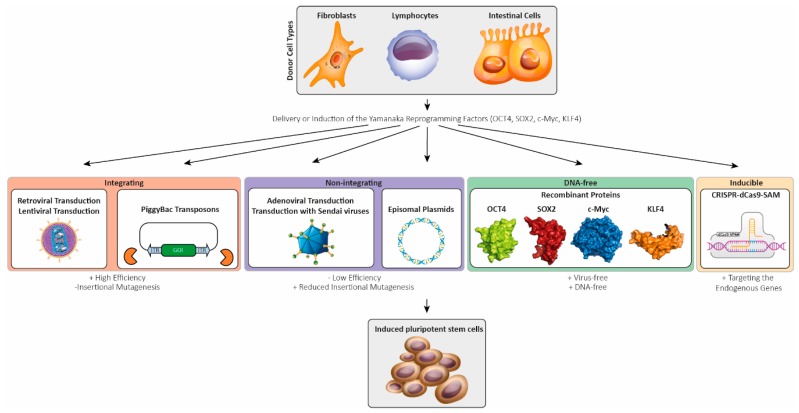
Different delivery methods were developed for reprogramming of somatic cell types like fibroblasts, lymphocytes, keratinocytes, urine-derived, or intestinal cells into iPSCs (see Figure 2). Initially, iPSCs were generated using retroviral transduction [278,279,281]. The Moloney-based retroviral vector system used by the Yamanaka lab has the advantage of undergoing silencing in the iPSCs state but is restricted to dividing cell types. Therefore, lentiviruses were used to improve the transduction efficiency of dividing and non-dividing cell types. However, after lentiviral transduction, the expression of the reprogramming factors are poorly silenced [282,283], leading to difficult differentiation of these iPSCs [284]. Therefore, inducible systems were used, allowing for the silencing of the Yamanaka factors in iPSCs [284,285].
Figure 2.
Schematic overview about different delivery methods of the Yamanaka factors into somatic primary cells for reprogramming (sub-figures for the cell types and viruses were licensed from shutterstock.com).
However, usage of integrating viral systems enhances the risk for insertional mutagenesis, limiting their application [286]. Furthermore, the transgene reactivation of c-Myc showed increased tumorigenicity in chimeric mice [280], limiting the usage of iPSCs for clinical approaches. To overcome these limitations, non-integrating delivery methods have been developed. Transient transfection of the PiggyBac transposon with a Cre-mediated excisable system was one of the first non-integrating methods (Figure 2). Minimized genome modification, in combination with silencing of the reprogramming factor expression in the iPSC state, are the main advantages of this system [287]. Another approach is the adenoviral transduction leading to an overexpression of the reprogramming factors in the host cells without genomic integration [288]. Transient transfection or electroporation with episomal plasmids encoding the reprogramming factors is an alternative method to produce virus-free iPSCs [289] (Figure 2). However, the efficiency of this delivery method is quite low [290]. More promising non-inserting delivery methods include the use of Sendai viruses [291], which are RNA viruses that do not enter the nucleus, thereby decreasing the risk of genomic insertion.
Reprogramming using miRNAs that are specifically expressed in embryonic pluripotent stem cells (ESCs) can enhance the reprogramming efficiency [292]. For example, the miR302/367 cluster is highly expressed in pluripotent cells, but not in differentiated cells, and its promoter is transcriptionally regulated by the reprogramming factors Oct4 and Sox2 [293]. This cluster is functionally involved in regulation of the cell cycle and maintenance of pluripotency. Overexpression of the miRNA cluster miR302/367 can promote the reprogramming of somatic cells [294]. In combination with the reprogramming factors, a higher efficiency can be achieved [292]. Although RNA-based reprogramming methods show higher efficiency compared to Sendai virus and episomal methods, the reliability is significantly lower [295]. Non-integrating delivery methods provide iPSCs that are more applicable for clinical disease modeling. Besides the integrating and non-integrating delivery systems, DNA-free approaches with transgene free reprogramming have been established. Small compounds or recombinant reprogramming factors were used (Figure 2) [296,297]. For example, the histone deacetylase inhibitor valproic acid improves the reprogramming efficiency [298,299]. The efficient synthesis of large amounts of purified native recombinant proteins and the permeabilization of the plasma membranes are crucial for this reprogramming method [300]. More recently, the CRISPR-dCas9-based synergistic activation mediator (SAM) system has been developed and applied for reprogramming [301,302]. This system is based on a fusion protein of the enzymatic inactive form of Cas9 (dCas9) and a transcription activator domain forming an artificial transcription factor which, in combination with specific guide RNAs, is able to activate the transcription of endogenous genes with minimal off-target activity. Weltner et al. successfully used this system for the expression of different reprogramming factors to generate iPSCs [302].
In summary, different integrating and non-integrating approaches have been developed for reprogramming different cell types into iPSCs to improve the efficiency and to reduce the risk of further genomic alterations (see Figure 2).
5. Genetic Modification of Induced Pluripotent Stem Cell Lines
Besides the generation of human iPSCs from the primary cells of mutation carriers by direct reprogramming [278,281], specific genetic mutations can also be inserted using genome editing techniques like clustered regularly interspaced short palindromic repeats associated protein 9 (CRISPR-Cas9) [303], CPF1 [304], or transcription activator-like effector nucleases (TALENs) [305,306]. In addition to genome editing approaches, iPSCs or the differentiated cardiomyocytes can be genetically modified by overexpressing specific mutant proteins [307,308] or by decreasing the expression of specific mutant proteins, e.g., by RNA interference [309].
Using patient-derived iPSCs, it is sometimes challenging to correlate directly functional effects in vitro with the specific genetic variants because the genetic and epigenetic background of the cells is largely unknown [310]. In contrast to patient-derived iPSCs, which carry the sum of all genetic sequence variants of the affected patients, genome edited iPSC lines carry specifically inserted mutations. Therefore, the effects of particular mutations can be directly compared with their corresponding isogenic wild-type controls in genome-edited iPSCs.
Genome editing techniques like CRISPR-Cas9 are based on endonuclease activity, which insert double-strand breaks (DSBs) into the DNA double helix at specific sites. Different endogenous cellular repair mechanisms like non-homologous end joining (NHEJ) or homology directed repair (HDR) are used for the repair of these DSBs. However, NHEJ is an imprecise process, which might lead to the insertion, deletion, or substitution of nucleotides [311]. Indel variants frequently cause frameshifts, and consequently, premature termination codons (PTCs). PTCs are recognized by nonsense mediated RNA decay (NMD) degrading the mutant mRNA. Therefore, DSBs can be efficiently used to generate knock-out models. In contrast, HDR uses DNA template molecules for the specific repair of the DSBs. In combination with suitable donor molecules, e.g., single-stranded oligonucleotides or double-stranded DNA templates like PCR products or plasmids, HDR can be used to insert specific point mutations [312], small peptide-encoding tags [313], or even larger fluorescence proteins at specific positions [314,315,316]. Unfortunately, the ratio of HDR to NHEJ is low, limiting the efficiency of knock-in strategies [317]. Therefore, different approaches for inhibiting NHEJ or promoting HDR have been developed (for reviews, see References [317,318,319]). The delivery of donor template molecules in close proximity to the DSBs by coupling Cas9 with the donor molecule might be a promising strategy [320,321,322]. An alternative are dCas9-related base pair editors [323,324,325], which can be used to exchange relevant nucleotides at specific positions.
6. Differentiation of Human Induced Pluripotent Stem Cells into Cardiomyocytes
The human adult heart is a post-mitotic organ with a very limited capacity for regeneration [326]. Beside the murine, atrial cardiomyocytes-related HL-1 cell line [327], no further contracting human cardiomyocytes cell lines are therefore currently available. Because of ethical and technical issues, the isolation of primary human cardiomyocytes from human surgical material and their long-time culture is in most cases impossible. Primary cardiomyocytes isolated from rodent hearts have characteristic differences like a different electrophysiology in comparison to the human ones. Therefore, cardiomyocytes derived from human ESCs or iPSCs are the predominant human cell resource [328,329].
Originally, Zhang et al. described the differentiation of cardiomyocytes from human iPSCs [330]. Comparable to ESCs, human iPSCs form embryonic bodies in suspension that can be further differentiated into cardiomyocytes [330,331,332,333,334]. However, the efficiency of this process was limited. In addition, monolayers of iPSC-derived cardiomyocytes can be generated [335,336]. In vivo, cardiogenesis is a complex cellular and molecular process where different transcription factors, growth factors, and miRNAs are time dependently expressed and regulated [337,338,339,340,341]. Driven by discoveries from development biology, it has been recognized that different recombinant growth factors, e.g., BMP4, can also be used to increase the efficiency of in vitro differentiation into cardiomyocytes [342,343,344]. In addition, modulation of the Wnt pathway by small molecules, e.g., CHIR99021 and IWP2, efficiently increases the differentiation into cardiomyocytes about 90% [344,345]. Furthermore, metabolic selection by glucose depletion, in combination with lactate supplementation, can be applied for further accumulation of cardiomyocytes [346,347]. Recently, Zhao et al. developed a method for the differentiation and generation of heteropolar cardiac tissue with atrial and ventricular ends [348]. Talkhabi et al. has previously reviewed the differentiation of iPSCs into cardiomyocytes in detail [349].
7. Methods for the Functional Analysis of Cardiomyocytes Derived from Induced Pluripotent Stem Cells
Besides general histochemical or molecular methods, e.g., RNA-Seq or proteomics, specific techniques for the functional in vitro analysis of the electrophysiological and contractile properties of iPSC-derived cardiomyocytes are frequently used. Patch clamping and multiple electron arrays (MEAs) are frequently used for the electrophysiological analysis of iPSC-derived cardiomyocyte monolayers [350,351]. The application of Ca2+ specific fluorescence dyes, e.g., Indo1 or Fura-2, allows for the microscopic analysis of Ca2+ transients [352,353,354]. Additionally, voltage-sensitive fluorescence dyes like di-4-ANEPPS can be used for the analysis of the electrophysiological properties [355]. For the analysis of the contractile properties of iPSC-derived cardiomyocytes, microscopic techniques like traction force measurements have also been used [356]. Atomic force microscopy can also be applied for measuring the contraction forces of iPSC-derived cardiomyocytes [357,358]. Feaster and coworkers developed a method to culture iPSC-derived cardiomyocytes on Matrigel mattresses, allowing for the contractility measurement by cell shortening [359].
8. Overview about Existing iPSC Lines Carrying Cardiomyopathy Associated Mutations
In 2010, Carvajal-Vergara and co-workers published a landmark paper about the generation of an iPSC line carrying the heterozygous mutation PTPN11-p.T468M [360]. Mutations in PTPN11 cause the Leopard syndrome [361,362], which is frequently associated with severe HCM [363]. Interestingly, these iPSC-derived cardiomyocytes were larger and presented an abnormal, nuclear localization of NFATc4 [360]. Members of the NFAT family are involved in the calcineurin-NFAT signaling regulating hypertrophy [364]. Since this original report, about 70 different iPSC lines carrying cardiomyopathy-associated mutations in several different genes have been generated (Table 2). The majority of these mutant iPSC lines have been used for phenotypic modeling of genetic cardiomyopathies using electrophysiological and/or contraction measurements (Table 2). Besides modeling genetic cardiomyopathies, iPSC-derived cardiomyocytes were also used for the modeling of non-genetic causes of cardiomyopathies, e.g., doxorubicin cardiotoxicity [263,365], hypoxia [366], peripartum [367], or diabetic cardiomyopathy [368,369,370,371], or even infection with Trypanosoma cruzi [372] or with coxsackievirus B3 [373].
Table 2.
Overview about important iPSC lines carrying mutations in genes associated with genetic cardiomyopathies or related diseases.
| Gene | Protein | Mutation(s) | Method of Generation | Main Phenotypic Findings | Associated Disease | References |
|---|---|---|---|---|---|---|
| ACTC1 | Cardiac Actin | p.E99K |
|
Arrhythmias | HCM/LVNC | [380] |
| ALPK3 | α-Kinase 3 | p.W1264Xhom | Electroporation with episomal plasmids |
|
HCM | [381] |
| BAG3 | Bcl-2 Associated Athanogene 3 |
|
|
|
DCM | [374] |
| BRAF | B-Raf Proto-Oncogene, Serine/Threonine Kinase |
|
|
|
CFCS/HCM | [382] |
| CAV | Caveolin |
|
Electroporation with episomal plasmids | NA | MP | [383] |
| CRYAB | αB-Crystallin |
|
Retroviral transduction and genome editing (zinc finger nucleases) |
|
MFM | [384] |
| DES | Desmin | p.N116S | Lentiviral transduction | NA | ACM | [385] |
| DES | Desmin | c.735+1G > A | Sendai virus transduction | NA | DRC | [386] |
| DES | Desmin | p.A285V | Retroviral transduction |
|
DCM | [387] |
| DMD | Dystrophin |
|
Sendai virus transduction |
|
DMD | [388] |
| DMD | Dystrophin |
|
Sendai virus transduction in combination with CRISPR-Cas9 |
|
DMD | [379] |
| DMD | Dystrophin |
|
Lentiviral transduction CRISPR-Cas9 |
|
DMD | [389,390] |
| DSG2 | Desmoglein-2 | p.G638R | Sendai virus transduction |
|
ACM | [391] |
| DSP | Desmoplakin | p.R451G | Sendai virus transduction & genome editing for correction (CRISPR-Cas9) | Reduced desmoplakin expression | ACM | [392] |
| FBN1 | Fibrillin 1 | c.4028G > A | Sendai virus transduction | NA | Marfan Syndrome (HCM) | [393] |
| FKRP | Fukutin Related Protein | c.826C > Ahom | Lentiviral transduction |
|
Limb-Girdle Muscular Dystrophy (DCM) | [394] |
| FXN | Frataxin | Expanded GAA repeats | Retroviral transduction |
|
Friedreich Ataxia (HCM) | [395] |
| FXN | Frataxin | Expanded GAA repeats
|
Lentiviral transduction |
|
Friedreich Ataxia (HCM) | [396] |
| GLA | Galactosidase α | IVS4+919G > A | Retroviral transduction |
|
Fabry Disease (HCM) | [397,398] |
| LAMP2 | Lysosomal Associated Membrane Protein 2 | IVS6+1_4delGTGA | Sendai virus transduction | Autophagy dysfunction | Danon Disease (CM) | [399] |
| LAMP2 | Lysosomal Associated Membrane Protein 2 |
|
Unknown |
|
Danon Disease (CM) | [400] |
| LAMP2 | Lysosomal Associated Membrane Protein 2 |
|
|
|
Danon Disease (CM) | [401] |
| LMNA | Lamin A/C | p.S143P | Sendai virus transduction |
|
DCM | [402] |
| LMNA | Lamin A/C | p.S18fsX | Combined lentiviral and retroviral transduction | Normal nuclear membrane morphology | DCM | [403] |
| LMNA | Lamin A/C | p.R225X | Lentiviral transduction |
|
DCM | [404] |
| LMNA | Lamin A/C |
|
Lentiviral transduction |
|
DCM & conduction disorders | [405] |
| LMNA | Lamin A/C | p.K219T | Lentiviral transduction |
|
DCM & conduction disorders | [406] |
| MT-RNR2 | Mitochondrially Encoded 16S rRNA | m.2336T > C | Retroviral transduction |
|
HCM | [407] |
| MYBPC3 | Myosin Binding Protein C3 |
|
Sendai virus transduction | Abnormal Ca2+ handling | HCM | [408] |
| MYBPC3 | Myosin Binding Protein C3 | p.R326Q | Electroporation with episomal plasmids | Ca2+ handling deficits | HCM | [409] |
| MYBPC3 | Myosin Binding Protein C3 | c.2373 | Lentiviral transduction |
|
HCM | [410,411] |
| MYBPC3 | Myosin Binding Protein C3 | p.R502W | Electroporation with episomal plasmids | NA | HCM | [412] |
| MYBPC3 | Myosin Binding Protein C3 |
|
CRISPR-Cas9 |
|
HCM | [413] |
| MYBPC3 | Myosin Binding Protein C3 |
|
Sendai virus transduction & genome editing for correction (CRISPR-Cas9) |
|
HCM | [414,415] |
| MYBPC3 | Myosin Binding Protein C3 | p.G999-Q1004del | Sendai virus transduction |
|
HCM | [416] |
| MYBPC3 | Myosin Binding Protein C3 | p.Q1061X |
|
Arrhythmias | HCM | [417,418] |
| MYBPC3 | Myosin Binding Protein C3 | p.V454CfsX21 | Retroviral transduction |
|
HCM | [419] |
| MYBPC3 | Myosin Binding Protein C3 | ∆25 bp in intron 32 including the splicing branch point & p.D389V (same allele) | Sendai virus transduction |
|
HCM | [420] |
| MYBPHL | Myosin Binding Protein H-Like | p.R255X | Electroporation with episomal plasmids | Haploinsufficiency by nonsense mediated mRNA decay | DCM & conduction disorders | [187] |
| MYH7 | Myosin Heavy Chain 7 | p.R663H | Sendai virus transduction | Abnormal Ca2+ handling | HCM | [408] |
| MYH7 | Myosin Heavy Chain 7 |
|
CRISPR-Cas9 |
|
HCM | [421] |
| MYH7 | Myosin Heavy Chain 7 |
|
CRISPR-Cas9 |
|
HCM | [413] |
| MYH7 | Myosin Heavy Chain 7 | p.V698A | Electroporation with episomal plasmids | NA | HCM | [422] |
| MYH7 | Myosin Heavy Chain 7 | p.E848G | Electroporation with episomal plasmids | Reduced contractile function | HCM | [423,424] |
| MYH7 | Myosin Heavy Chain 7 | p.R403Q | Electroporation with episomal plasmids | NA | HCM | [425] |
| MYH7 | Myosin Heavy Chain 7 | p.R633H | Lentiviral transduction |
|
HCM | [414,426] |
| MYH7 | Myosin Heavy Chain 7 | p.R442G | Retroviral transduction |
|
HCM | [427] |
| MYL2 | Myosin Light Chain 2 | p.R58Q | Non-integrating mRNA/miRNA technology |
|
HCM | [428] |
| MYL3 | Myosin Light Chain 3 |
|
CRISPR-Cas9 |
|
HCM | [375] |
| PKP2 | Plakophilin-2 | p.L614P | Retroviral transduction |
|
ACM | [429] |
| PKP2 | Plakophilin-2 |
|
Retroviral transduction |
|
ACM | [430,431,432] |
| PKP2 | Plakophilin-2 | c.972insT | Retroviral transduction |
|
ACM | [433] |
| PKP2 | Plakophilin-2 |
|
Sendai virus transduction | NA | ACM | [434] |
| PKP2 | Plakophilin-2 | c.2569_3018del50 | Electroporation with episomal plasmids | NA | ACM | [435] |
| PLN | Phospholamban | p.R9C | CRISPR-Cas9 |
|
DCM | [414,436] |
| PLN | Phospholamban | p.R14del | Transfection with mRNAs& genome editing (TALENs) for mutation correction |
|
DCM | [437,438] |
| PRGAG2 | Protein Kinase AMP-Activated Non-Catalytic Subunit Gamma 2 | p.R302Q | Sendai virus transduction & genome editing for correction (CRISPR-Cas9) |
|
Wolff–Parkinson–White Syndrome (HCM) | [439] |
| PRKAG2 | Protein Kinase AMP-Activated Non-Catalytic Subunit Gamma 2 | p.N488I | Lentiviral transduction & genome editing for correction (TALEN) |
|
HCM | [440] |
| PTPN11 | Protein Tyrosine Phosphatase Non-Receptor Type 11 | p.T468M | Retroviral transduction |
|
LEOPARD Syndrome (HCM) | [360] |
| PTPN11 | Protein Tyrosine Phosphatase Non-Receptor Type 11 | p.Q510P | Sendai virus transduction | NA | LEOPARD Syndrome (HCM) | [441] |
| RAF1 | Raf-1 Proto-Oncogene, Serine/Threonine Kinase | p.S257L | Electroporation of episomal plasmids & genome editing for correction (CRISPR-Cas9) |
|
Noonan Syndrome (HCM) | [442] |
| RBM20 | RNA Binding Motif Protein 20 | p.S635A | Lentiviral transduction |
|
DCM | [443] |
| RBM20 | RNA Binding Motif Protein 20 | p.R636S | Sendai virus transduction |
|
DCM | [444,445] |
| RYR2 | Ryanodine Receptor 2 | p.F2483I | Retroviral transduction |
|
CPVT | [350] |
| RYR2 | Ryanodine Receptor 2 |
|
Sendai virus transduction |
|
CPVT | [376] |
| SCN5A | Sodium Voltage-Gated Channel Alpha Subunit 5 |
|
Sendai virus transduction & CRISPR-Cas9 for correction |
|
ACM | [446] |
| SCN5A | Sodium Voltage-Gated Channel Alpha Subunit 5 | p.R219H | Sendai virus transduction |
|
ACM/DCM | [447] |
| SCO2 | SCO2 Cytochrome C Oxidase Assembly Protein |
|
Sendai virus transduction |
|
HCM | [448] |
| TAZ | Tafazzin |
|
Transfection with synthetic mRNAs & CRISPR-Cas9 for correction |
|
Barth Syndrome | [449] |
| TBX20 | T-Box Factor 20 |
|
Sendai virus transduction |
|
LVNC | [450] |
| TNNT2 | Cardiac Troponin T | p.R92W | Sendai virus transduction & CRISPR-Cas9 for correction | Abnormal Ca2+ handling | HCM | [408] |
| TNNT2 | Cardiac Troponin T | p.R173W | Lentiviral transduction |
|
DCM | [414,451,452,453,454] |
| TNNT2 | Cardiac Troponin T |
|
TALEN |
|
DCM/HCM | [453] |
| TNNT2 | Cardiac Troponin T | p.I79N | CRISPR-Cas9 |
|
HCM | [455,456] |
| TPM1 | Tropomyosin-1 | p.D175N |
|
Arrhythmias | HCM | [417,418] |
| TTN | Titin |
|
|
|
DCM | [457] |
| TTN | Titin | p.S14450fsX4 | Sendai virus transduction | Antisense-mediated exon skipping restores titin expression | DCM | [377] |
| TTN | Titin |
|
Lentiviral transduction |
|
DCM | [458] |
| TTR | Transthyretin | p.L55P | Lentiviral transduction | Increased oxidative stress | Hereditary Transthyretin Amyloidosis | [459] |
ACM—Arrhythmogenic cardiomyopathy; CFCS—Cardio facio cutaneous syndrome; CM—Cardiomyopathy; CPVT—Catecholaminergic polymorphic ventricular tachycardia; DCM—Dilated cardiomyopathy; DMD—Duchenne muscular dystrophy; DRC—Desmin-related cardiomyopathy; HCM—Hypertrophic cardiomyopathy; LVNC—Left-ventricular non-compaction cardiomyopathy; MFM—Myofibrillar myopathy; MP—Myopathy; NA—Not assessed; RCM—Restrictive cardiomyopathy.
In the beginning, iPSC lines generated from healthy probands were frequently used as controls for experiments. However, because different iPSC lines have a variable genetic background, this approach has limitations. Since the development of efficient genome editing technologies like CRISPR-Cas9 or TALENs [303], it is common to generate isogenic control lines [374]. Interestingly, the reverse approach by inserting specific mutations in iPSCs from healthy control persons is also sometimes used [375]. In some cases, the rationale of these studies is the functional characterization of specific cardiomyopathy-associated mutations, which might contribute to a pathogenicity classification. In addition, iPSC-derived cardiomyocytes were used for the development of therapeutic strategies, e.g., genome editing. An interesting application of iPSC-derived cardiomyocytes is the testing of specific gene therapeutic concepts [376]. For example, Gramlich et al. applied antisense-mediated exon skipping in iPSC-derived cardiomyocytes with a truncating TTN (TTNtv) mutation for restoring the expression of titin [377]. However, at present, it appears that some of the TTNtv do not lead to premature translation termination in failing human hearts [378]. Thus, iPSCs might therefore be useful in future to check and modulate possible read-throughs of TTNtv mutations as well. Similarly, Kyrychenko et al. used CRISPR-Cas9 to delete whole exons within the DMD gene to correct the reading frame [379]. Of note, this strategy restores contractility in the iPSC-derived cardiomyocytes [379]. Hopefully, the combination of iPSC-derived cardiomyocytes with adequate modern genetic engineering tools will contribute in future to the development of therapeutic options in the context of personalized medicine.
9. Limitations of Human Induced Pluripotent Stem-Cell-Derived Cardiomyocytes
Besides cardiomyocytes, the human adult heart consists of several different cell types like fibroblasts, endothelial cells, leukocytes, pericytes, and smooth muscle cells. It has been estimated that the proportion of cardiomyocytes in myocardial tissue is around 25–35%, indicating that the majority of the cardiac cells are non-cardiomyocytes [460]. However, the molecular and cellular interactions and interferences between the different cardiac cell types are poorly understood. In particular, under pathological conditions like inflammation or fibrosis, the cellular composition of the heart of cardiomyopathy patients can vary and might change over time. Therefore, it is in general challenging to model the complex cellular and molecular networks using iPSC-derived cardiomyocytes in vitro, although the artificial generation of cardiac tissue has been impressively improved during the last few years [461,462,463,464,465]. Besides these general limitations, iPSCs and iPSC-derived cardiomyocytes have some specific limitations, which are outlined in the following paragraphs.
9.1. Genomic Instability
Genomic instability of iPSCs can be a fundamental problem limiting the clinical application of iPSC-derived cells because of safety concerns [466]. Mayshar et al. showed that a significant portion of iPSC and ESC lines carry full or partial chromosomal aberrations [467]. However, even for in vitro analysis, genomic instability could be an important issue, especially in the context of modeling genetic diseases like cardiomyopathies. Therefore, novel iPSC lines should be genetically characterized in general. Karyotype analysis using Giemsa staining or comparative genomic hybridization arrays can be used to detect larger chromosomal abnormalities, while next generation sequencing assays can be applied for genetic analysis at the single nucleotide level.
Three different mechanisms contribute to the mutagenesis in iPSCs: besides the existence of genetic variants in the parental somatic donor cells, mutations can be introduced during reprogramming procedure or during the long-time culture of iPSCs [468]. Of note, mutations might accumulate in iPSCs over the culturing time [469]. Therefore, it is advisable to use early passages and to repeat analyses for genetic stability from time to time.
9.2. Heterogeneity of iPSC-Derived Cardiomyocytes
Although cardiac differentiation protocols for iPSCs have been improved significantly over recent years [345,470], it should be kept in mind that iPSC-derived cardiomyocytes are still a heterogeneous cell population. Especially for bulk down-stream applications like proteomics, genomics, or metabolomics, this might have a significant impact.
9.3. Cellular, Molecular, and Functional Differences of Adult Ventricular Cardiomyocytes and iPSC-Derived Cardiomyocytes
Even though human iPSC-derived cardiomyocytes are contractile cell types, there are important cellular, molecular, and functional differences compared to adult cardiomyocytes. The most obvious differences are the size and shape of iPSC-derived cardiomyocytes. Adult ventricular cardiomyocytes have a typical rod-like shape and are relatively large cells with lengths of about 100 µm and diameters of 10–25 µm [471]. In contrast, iPSC-derived cardiomyocytes are much smaller [472] and are morphologically heterogeneous. The geometry of iPSC-derived cardiomyocytes ranges from round to rectangular or polygonal shapes [473,474]. In adult ventricular cardiomyocytes, the sarcomeric structure is highly organized and the Z-bands are in parallel with the intercalated disc. On the contrary, iPSC-derived cardiomyocytes have a more irregular and amorphous sarcomeric organization with diverse orientations [462,475]. In human myocardial tissue, the closed-ends of the plasma membranes connect the cardiomyocytes longitudinally and these ends of the cardiomyocytes “cylinders” are called intercalated discs. Multi-protein complexes mediate the cell–cell interactions at the intercalated discs and are subdivided into desmosomes, adherens, and gap junctions [476]. Although desmosomes and adherens junctions are also formed in iPSC-derived cardiomyocytes [472,477], the cellular distribution of these cell–cell junctions are not conserved [478,479]. Another important difference is the number of nuclei. Whereas a significant number of the human cardiomyocytes in vivo are binuclear cells [480], iPSC-derived cardiomyocytes are mononuclear cells [481]. In addition, there are significant differences in contraction and electrical properties of iPSC-derived cardiomyocytes in comparison to adult ones [474]. In summary, the structural and functional properties of iPSC-derived cardiomyocytes are more similar to fetal cardiomyocytes than to adult cardiomyocytes [482]. To overcome these limitations, different natural engineering approaches were established to drive cardiomyocytes maturation. One method is to stimulate the cardiomyocytes with electrical or mechanical impulses [483]. The composition of the extracellular matrix can also affect the interaction of the CMs, therefore influencing the cellular behavior [484,485]. Another promising approach is the co-culture of iPSC-derived cardiomyocytes with non-cardiomyocytes, enabling a more likely cardiac environment with different cellular interactions [486]. Physical, chemical, electrical, and genetic factors are being tested as stimuli for further maturation [487]. However, maturation of iPSC-derived cardiomyocytes is incompletely understood at the molecular level and more studies are needed in future.
10. Testing of Gene Therapies Using iPSC-Derived Cardiomyocytes as in Vitro Models
An interesting research topic is the development of personalized therapeutic strategies for genetic cardiomyopathies in vitro. Beyond the opportunities that reprogramming technologies offer for therapeutic myocardial regeneration, iPSC-derived cardiomyocytes are a promising platform to develop and test different gene therapies for genetic, non-ischemic cardiomyopathies. In general, the pathomechanisms of inherited cardiomyopathies can be classified into loss of function (LOF) or gain of function (GOF) mechanisms. LOF can be caused by (haplo)insufficiency or by the expression of non-functional proteins. For example, several HCM-associated MYBPC3 mutations cause haploinsufficiency [415,488]. GOF is caused by mutant and toxic proteins such as those shown for several DES missense mutations [489,490].
Genome editing using CRISPR-Cas9 or TALENs has been applied to repair different mutations in iPSC-derived cardiomyocytes. After the insertion of DSBs, iPSCs repair these DSBs using NHEJ or HDR. Template molecules like oligonucleotides, plasmids, PCR products, or even the second chromosome might be used for HDR. Recently, Ma et al. even applied CRISPR-Cas9 for the repair of a pathogenic MYBPC3 mutation in human pre-implanted embryos [491]. However, because the efficiency of HDR is low, the direct repair of mutations in iPSCs via genome editing is challenging. Therefore, single iPSC clones were frequently generated in vitro and the direct translational transfer of this method is consequently limited. A second therapeutic strategy is exon skipping [492]. Exon skipping corrects the open reading frame (ORF) of an affected gene via skipping of the mutant or multiple exons and restores the expression of the truncated, but still functional, protein. For this approach, specific antisense oligonucleotides binding to the mutant exons can be used [493]. Besides its application in iPSC-derived cardiomyocytes carrying mutations in DMD [494] or TTN [377], antisense-mediated exon skipping was also directly applied in human patients with Duchenne’s muscular dystrophy [495]. Recently, Eric Olson’s group applied CRISPR-CPF1 or -Cas9-mediated genome editing for exon skipping in iPSC-derived cardiomyocytes [379,496,497]. Prondzynski et al. applied trans-splicing and total gene replacement for the artificial increased expression of MYBPC3 in iPSC-derived cardiomyocytes carrying a heterozygous frameshift mutation in MYBPC3 [419]. The authors used adeno-associated viruses (serotype 2/9, AAV2/9) for the transduction of iPSC-derived cardiomyocytes with 5′- and 3′-pre-trans-splicing molecules and the total cDNA of MYBPC3. However, the efficiency of the trans-splicing approach was low. In contrast, the total gene replacement strategy increased the MYBPC3 expression to over 80% in comparison with wild-type controls and was able to prevent cellular hypertrophy [419].
The combination of the iPSC-derived cardiomyocytes platform with gene therapy tools is a promising therapeutic approach enabling pre-clinical demonstration of proof-of-principle for inherited cardiomyopathies.
11. Summary
Human iPSC-derived cardiomyocytes represent the only available human cellular model for the direct functional analysis of specific genetic cardiomyopathies and might therefore overcome the limitation of species differences. Impressive progress in the reprogramming and differentiation procedure during the last decade allows, in combination with novel genome editing techniques like CRISPR-Cas9, for the development of defined/patient specific cardiomyocyte models including generation of their isogenic control lines. In summary, iPSC-derived cardiomyocytes have been used for: (a) the characterization of genetic variants of unknown significance, which might be helpful for genetic counseling [375]; (b) analyses of the molecular pathomechanisms [415]; and (c) the development of specific therapies [377,497].
However, the cellular and molecular crosstalk between inflammatory cells, fibroblasts, myoblasts, and cardiomyocytes is difficult to model using iPSC-derived cardiomyocytes. Therefore, in our opinion, iPSC-derived cardiomyocytes should also be combined with animal models or with ex vivo investigations of explanted human myocardial tissue whenever possible to overcome the specific limitations of iPSC-derived cardiomyocytes.
Interestingly, for some genes like DMD, PKP2, MYBPC3, or MYH7, several different iPSC lines have been generated. In contrast, for rare cardiomyopathy genes, e.g., TMEM43, no iPSC lines have been developed yet. The genetic analysis in the past few decades has revealed a high heterogeneity of inherited, non-ischemic cardiomyopathies. In our view, it is therefore important to generate further novel iPSC lines also carrying mutations in rare cardiomyopathy genes to compare the molecular differences and commonalities leading to non-ischemic cardiomyopathies. Hopefully, iPSC-derived cardiomyocytes will contribute to unravelling the pathomechanisms of genetic cardiomyopathies and will help in efficient drug development in future.
Gene names follow the official guidelines of the HUGO Gene Nomenclature Committee (HGNC, https://www.genenames.org/) [498].
Abbreviations
| ACMG | American College of Medical Genetics and Genomics Institute |
| ACM | Arrhythmogenic Cardiomyopathy |
| CM | Cardiomyopathy |
| DCM | Dilated Cardiomyopathy |
| ESC | Embryonic Stem Cell |
| HCM | Hypertrophic Cardiomyopathy |
| iPSC | Induced Pluripotent Stem Cell |
| HTx | Heart Transplantation |
| NCCM | Non-Compaction Cardiomyopathy |
| MP | Myopathy |
| NMD | Nonsense Mediated RNA Decay |
| RCM | Restrictive Cardiomyopathy |
Author Contributions
Writing and original draft preparation—A.B., H.E., and S.R; figure preparation—A.B.; review and editing—M.A.D., A.G., J.G., and H.M.
Funding
A.B., J.G., and H.M. are thankful for financial support of the German Foundation for Heart Research (DSHF, F07/17) and by the University of Bielefeld (Forschungsfonds Medizin in der Region OWL). H.E. received a Kaltenbach scholarship from the German Heart Foundation. H.M. received a grant from the German Research Foundation (DFG, MI-1146/2-1).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Green E.D., Watson J.D., Collins F.S. Human genome project: Twenty-five years of big biology. Nat. News. 2015;526:29–31. doi: 10.1038/526029a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brodehl A., Ebbinghaus H., Gaertner-Rommel A., Stanasiuk C., Klauke B., Milting H. Functional analysis of DES-p.L398P and RBM20-p.R636C. Genet. Med. 2019;21:1246–1247. doi: 10.1038/s41436-018-0291-2. [DOI] [PubMed] [Google Scholar]
- 3.Richards S., Aziz N., Bale S., Bick D., Das S., Gastier-Foster J., Grody W.W., Hegde M., Lyon E., Spector E., et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genet. and Genomics and the Association for Molecular Pathology. Genet. Med. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maron B.J., Towbin J.A., Thiene G., Antzelevitch C., Corrado D., Arnett D., Moss A.J., Seidman C.E., Young J.B., American Heart A., et al. Contemporary definitions and classification of the cardiomyopathies: An american heart association scientific statement from the council on clinical cardiology, heart failure and transplantation committee; Quality of care and outcomes research and functional genomics and translational biology interdisciplinary working groups; and council on epidemiology and prevention. Circulation. 2006;113:1807–1816. doi: 10.1161/CIRCULATIONAHA.106.174287. [DOI] [PubMed] [Google Scholar]
- 5.Alraies M.C., Eckman P. Adult heart transplant: Indications and outcomes. J. Thorac. Dis. 2014;6:1120–1128. doi: 10.3978/j.issn.2072-1439.2014.06.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minoche A.E., Horvat C., Johnson R., Gayevskiy V., Morton S.U., Drew A.P., Woo K., Statham A.L., Lundie B., Bagnall R.D., et al. Genome sequencing as a first-line genetic test in familial dilated cardiomyopathy. Genet. Med. 2019;21:650–662. doi: 10.1038/s41436-018-0084-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kolokotronis K., Kuhnisch J., Klopocki E., Dartsch J., Rost S., Huculak C., Mearini G., Stork S., Carrier L., Klaassen S., et al. Biallelic mutation in MYH7 and MYBPC3 leads to severe cardiomyopathy with left ventricular noncompaction phenotype. Hum. Mutat. 2019;40:1101–1114. doi: 10.1002/humu.23757. [DOI] [PubMed] [Google Scholar]
- 8.Hershberger R.E., Givertz M.M., Ho C.Y., Judge D.P., Kantor P.F., McBride K.L., Morales A., Taylor M.R.G., Vatta M., Ware S.M., et al. Genetic evaluation of cardiomyopathy: A clinical practice resource of the American College of Medical Genet. and Genomics (ACMG) Genet. Med. 2018;20:899–909. doi: 10.1038/s41436-018-0039-z. [DOI] [PubMed] [Google Scholar]
- 9.Merner N.D., Hodgkinson K.A., Haywood A.F., Connors S., French V.M., Drenckhahn J.D., Kupprion C., Ramadanova K., Thierfelder L., McKenna W., et al. Arrhythmogenic right ventricular cardiomyopathy type 5 is a fully penetrant, lethal arrhythmic disorder caused by a missense mutation in the TMEM43 gene. Am. J. Hum. Genet. 2008;82:809–821. doi: 10.1016/j.ajhg.2008.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Milting H., Klauke B., Christensen A.H., Musebeck J., Walhorn V., Grannemann S., Munnich T., Saric T., Rasmussen T.B., Jensen H.K., et al. The TMEM43 Newfoundland mutation p.S358L causing ARVC-5 was imported from Europe and increases the stiffness of the cell nucleus. Eur. Heart J. 2015;36:872–881. doi: 10.1093/eurheartj/ehu077. [DOI] [PubMed] [Google Scholar]
- 11.Christensen A.H., Andersen C.B., Tybjaerg-Hansen A., Haunso S., Svendsen J.H. Mutation analysis and evaluation of the cardiac localization of TMEM43 in arrhythmogenic right ventricular cardiomyopathy. Clin. Genet. 2011;80:256–264. doi: 10.1111/j.1399-0004.2011.01623.x. [DOI] [PubMed] [Google Scholar]
- 12.Stroud M.J., Fang X., Zhang J., Guimaraes-Camboa N., Veevers J., Dalton N.D., Gu Y., Bradford W.H., Peterson K.L., Evans S.M., et al. Luma is not essential for murine cardiac development and function. Cardiovasc. Res. 2018;114:378–388. doi: 10.1093/cvr/cvx205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Figulla H.R., Wiegand V., Kreuzer H. Dilated cardiomyopathy. Dtsch. Med. Wochenschr. 1989;114:66–70. doi: 10.1055/s-2008-1066555. [DOI] [PubMed] [Google Scholar]
- 14.Seidman C.E., Seidman J.G. Identifying sarcomere gene mutations in hypertrophic cardiomyopathy: A personal history. Circ. Res. 2011;108:743–750. doi: 10.1161/CIRCRESAHA.110.223834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muchtar E., Blauwet L.A., Gertz M.A. Restrictive cardiomyopathy: Genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ. Res. 2017;121:819–837. doi: 10.1161/CIRCRESAHA.117.310982. [DOI] [PubMed] [Google Scholar]
- 16.Shariati J., Schlosser T., Erbel R. Noncompaction cardiomyopathy. Herz. 2015;40:583–590. doi: 10.1007/s00059-015-4233-3. [DOI] [PubMed] [Google Scholar]
- 17.Fazio G., Corrado G., Novo G., Zachara E., Rapezzi C., Sulafa A.K., Sutera L., D’Angelo L., Visconti C., Stollberger C., et al. Ventricular dysfunction and number of non compacted segments in non compaction: Non-independent predictors. Int. J. Cardiol. 2010;141:250–253. doi: 10.1016/j.ijcard.2008.11.199. [DOI] [PubMed] [Google Scholar]
- 18.Gandjbakhch E., Redheuil A., Pousset F., Charron P., Frank R. Clinical diagnosis, imaging, and genetics of arrhythmogenic right ventricular cardiomyopathy/dysplasia: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2018;72:784–804. doi: 10.1016/j.jacc.2018.05.065. [DOI] [PubMed] [Google Scholar]
- 19.Basso C., Corrado D., Marcus F.I., Nava A., Thiene G. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373:1289–1300. doi: 10.1016/S0140-6736(09)60256-7. [DOI] [PubMed] [Google Scholar]
- 20.Marcus F.I., Fontaine G.H., Guiraudon G., Frank R., Laurenceau J.L., Malergue C., Grosgogeat Y. Right ventricular dysplasia: A report of 24 adult cases. Circulation. 1982;65:384–398. doi: 10.1161/01.CIR.65.2.384. [DOI] [PubMed] [Google Scholar]
- 21.Corrado D., Basso C., Thiene G., McKenna W.J., Davies M.J., Fontaliran F., Nava A., Silvestri F., Blomstrom-Lundqvist C., Wlodarska E.K., et al. Spectrum of clinicopathologic manifestations of arrhythmogenic right ventricular cardiomyopathy/dysplasia: A multicenter study. J. Am. Coll. Cardiol. 1997;30:1512–1520. doi: 10.1016/S0735-1097(97)00332-X. [DOI] [PubMed] [Google Scholar]
- 22.Geisterfer-Lowrance A.A., Kass S., Tanigawa G., Vosberg H.P., McKenna W., Seidman C.E., Seidman J.G. A molecular basis for familial hypertrophic cardiomyopathy: A beta cardiac myosin heavy chain gene missense mutation. Cell. 1990;62:999–1006. doi: 10.1016/0092-8674(90)90274-I. [DOI] [PubMed] [Google Scholar]
- 23.Li D., Tapscoft T., Gonzalez O., Burch P.E., Quinones M.A., Zoghbi W.A., Hill R., Bachinski L.L., Mann D.L., Roberts R. Desmin mutation responsible for idiopathic dilated cardiomyopathy. Circulation. 1999;100:461–464. doi: 10.1161/01.CIR.100.5.461. [DOI] [PubMed] [Google Scholar]
- 24.Brodehl A., Dieding M., Biere N., Unger A., Klauke B., Walhorn V., Gummert J., Schulz U., Linke W.A., Gerull B., et al. Functional characterization of the novel DES mutation p.L136P associated with dilated cardiomyopathy reveals a dominant filament assembly defect. J. Mol. Cell. Cardiol. 2016;91:207–214. doi: 10.1016/j.yjmcc.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 25.Harada H., Hayashi T., Nishi H., Kusaba K., Koga Y., Koga Y., Nonaka I., Kimura A. Phenotypic expression of a novel desmin gene mutation: Hypertrophic cardiomyopathy followed by systemic myopathy. J. Hum. Genet. 2018;63:249–254. doi: 10.1038/s10038-017-0383-x. [DOI] [PubMed] [Google Scholar]
- 26.Klauke B., Kossmann S., Gaertner A., Brand K., Stork I., Brodehl A., Dieding M., Walhorn V., Anselmetti D., Gerdes D., et al. De novo desmin-mutation N116S is associated with arrhythmogenic right ventricular cardiomyopathy. Hum. Mol. Genet. 2010;19:4595–4607. doi: 10.1093/hmg/ddq387. [DOI] [PubMed] [Google Scholar]
- 27.Bermudez-Jimenez F.J., Carriel V., Brodehl A., Alaminos M., Campos A., Schirmer I., Milting H., Abril B.A., Alvarez M., Lopez-Fernandez S., et al. Novel desmin mutation p.Glu401Asp impairs filament formation, disrupts cell membrane integrity, and causes severe arrhythmogenic left ventricular cardiomyopathy/dysplasia. Circulation. 2018;137:1595–1610. doi: 10.1161/CIRCULATIONAHA.117.028719. [DOI] [PubMed] [Google Scholar]
- 28.Pruszczyk P., Kostera-Pruszczyk A., Shatunov A., Goudeau B., Draminska A., Takeda K., Sambuughin N., Vicart P., Strelkov S.V., Goldfarb L.G., et al. Restrictive cardiomyopathy with atrioventricular conduction block resulting from a desmin mutation. Int. J. Cardiol. 2007;117:244–253. doi: 10.1016/j.ijcard.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 29.Fan P., Lu C.X., Dong X.Q., Zhu D., Yang K.Q., Liu K.Q., Zhang D., Zhang Y., Meng X., Tan H.Q., et al. A novel phenotype with splicing mutation identified in a Chinese family with desminopathy. Chin. Med. J. 2019;132:127–134. doi: 10.1097/CM9.0000000000000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marakhonov A.V., Brodehl A., Myasnikov R.P., Sparber P.A., Kiseleva A.V., Kulikova O.V., Meshkov A.N., Zharikova A.A., Koretsky S.N., Kharlap M.S., et al. Non-compaction cardiomyopathy is caused by a novel in-frame desmin (DES) deletion mutation within the 1A coiled-coil rod segment leading to a severe filament assembly defect. Hum. Mutat. 2019 doi: 10.1002/humu.23747. [DOI] [PubMed] [Google Scholar]
- 31.Brodehl A., Gaertner-Rommel A., Milting H. Molecular insights into cardiomyopathies associated with desmin (DES) mutations. Biophys. Rev. 2018;10:983–1006. doi: 10.1007/s12551-018-0429-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gerull B., Gramlich M., Atherton J., McNabb M., Trombitas K., Sasse-Klaassen S., Seidman J.G., Seidman C., Granzier H., Labeit S., et al. Mutations of TTN, encoding the giant muscle filament titin, cause familial dilated cardiomyopathy. Nat. Genet. 2002;30:201–204. doi: 10.1038/ng815. [DOI] [PubMed] [Google Scholar]
- 33.Taylor M., Graw S., Sinagra G., Barnes C., Slavov D., Brun F., Pinamonti B., Salcedo E.E., Sauer W., Pyxaras S., et al. Genetic variation in titin in arrhythmogenic right ventricular cardiomyopathy-overlap syndromes. Circulation. 2011;124:876–885. doi: 10.1161/CIRCULATIONAHA.110.005405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peled Y., Gramlich M., Yoskovitz G., Feinberg M.S., Afek A., Polak-Charcon S., Pras E., Sela B.A., Konen E., Weissbrod O., et al. Titin mutation in familial restrictive cardiomyopathy. Int. J. Cardiol. 2014;171:24–30. doi: 10.1016/j.ijcard.2013.11.037. [DOI] [PubMed] [Google Scholar]
- 35.Haas J., Frese K.S., Peil B., Kloos W., Keller A., Nietsch R., Feng Z., Muller S., Kayvanpour E., Vogel B., et al. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur. Heart J. 2015;36:1123–1135. doi: 10.1093/eurheartj/ehu301. [DOI] [PubMed] [Google Scholar]
- 36.Pugh T.J., Kelly M.A., Gowrisankar S., Hynes E., Seidman M.A., Baxter S.M., Bowser M., Harrison B., Aaron D., Mahanta L.M., et al. The landscape of genetic variation in dilated cardiomyopathy as surveyed by clinical DNA sequencing. Genet. Med. 2014;16:601–608. doi: 10.1038/gim.2013.204. [DOI] [PubMed] [Google Scholar]
- 37.Klauke B., Gaertner-Rommel A., Schulz U., Kassner A., Zu Knyphausen E., Laser T., Kececioglu D., Paluszkiewicz L., Blanz U., Sandica E., et al. High proportion of genetic cases in patients with advanced cardiomyopathy including a novel homozygous Plakophilin 2-gene mutation. PLoS ONE. 2017;12:e0189489. doi: 10.1371/journal.pone.0189489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thierfelder L., Watkins H., MacRae C., Lamas R., McKenna W., Vosberg H.P., Seidman J.G., Seidman C.E. Alpha-tropomyosin and cardiac troponin T mutations cause familial hypertrophic cardiomyopathy: A disease of the sarcomere. Cell. 1994;77:701–712. doi: 10.1016/0092-8674(94)90054-X. [DOI] [PubMed] [Google Scholar]
- 39.Landstrom A.P., Parvatiyar M.S., Pinto J.R., Marquardt M.L., Bos J.M., Tester D.J., Ommen S.R., Potter J.D., Ackerman M.J. Molecular and functional characterization of novel hypertrophic cardiomyopathy susceptibility mutations in TNNC1-encoded troponin C. J. Mol. Cell. Cardiol. 2008;45:281–288. doi: 10.1016/j.yjmcc.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kimura A., Harada H., Park J.E., Nishi H., Satoh M., Takahashi M., Hiroi S., Sasaoka T., Ohbuchi N., Nakamura T., et al. Mutations in the cardiac troponin I gene associated with hypertrophic cardiomyopathy. Nat. Genet. 1997;16:379–382. doi: 10.1038/ng0897-379. [DOI] [PubMed] [Google Scholar]
- 41.Knoblauch H., Geier C., Adams S., Budde B., Rudolph A., Zacharias U., Schulz-Menger J., Spuler A., Yaou R.B., Nurnberg P., et al. Contractures and hypertrophic cardiomyopathy in a novel FHL1 mutation. Ann. Neurol. 2010;67:136–140. doi: 10.1002/ana.21839. [DOI] [PubMed] [Google Scholar]
- 42.Gaertner-Rommel A., Tiesmeier J., Jakob T., Strickmann B., Veit G., Bachmann-Mennenga B., Paluszkiewicz L., Klingel K., Schulz U., Laser K.T., et al. Molecular autopsy and family screening in a young case of sudden cardiac death reveals an unusually severe case of FHL1 related hypertrophic cardiomyopathy. Mol. Genet. Genom. Med. 2019;7:e841. doi: 10.1002/mgg3.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mogensen J., Klausen I.C., Pedersen A.K., Egeblad H., Bross P., Kruse T.A., Gregersen N., Hansen P.S., Baandrup U., Borglum A.D. Alpha-cardiac actin is a novel disease gene in familial hypertrophic cardiomyopathy. J. Clin. Investig. 1999;103:R39–R43. doi: 10.1172/JCI6460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haywood N.J., Wolny M., Rogers B., Trinh C.H., Shuping Y., Edwards T.A., Peckham M. Hypertrophic cardiomyopathy mutations in the calponin-homology domain of ACTN2 affect actin binding and cardiomyocyte Z-disc incorporation. Biochem. J. 2016;473:2485–2493. doi: 10.1042/BCJ20160421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Valdes-Mas R., Gutierrez-Fernandez A., Gomez J., Coto E., Astudillo A., Puente D.A., Reguero J.R., Alvarez V., Moris C., Leon D., et al. Mutations in filamin C cause a new form of familial hypertrophic cardiomyopathy. Nat. Commun. 2014;5:5326. doi: 10.1038/ncomms6326. [DOI] [PubMed] [Google Scholar]
- 46.Chiu C., Tebo M., Ingles J., Yeates L., Arthur J.W., Lind J.M., Semsarian C. Genetic screening of calcium regulation genes in familial hypertrophic cardiomyopathy. J. Mol. Cell. Cardiol. 2007;43:337–343. doi: 10.1016/j.yjmcc.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 47.Herman D.S., Lam L., Taylor M.R., Wang L., Teekakirikul P., Christodoulou D., Conner L., DePalma S.R., McDonough B., Sparks E., et al. Truncations of titin causing dilated cardiomyopathy. N. Engl. J. Med. 2012;366:619–628. doi: 10.1056/NEJMoa1110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Daehmlow S., Erdmann J., Knueppel T., Gille C., Froemmel C., Hummel M., Hetzer R., Regitz-Zagrosek V. Novel mutations in sarcomeric protein genes in dilated cardiomyopathy. Biochem. Biophys. Res. Commun. 2002;298:116–120. doi: 10.1016/S0006-291X(02)02374-4. [DOI] [PubMed] [Google Scholar]
- 49.Fatkin D., MacRae C., Sasaki T., Wolff M.R., Porcu M., Frenneaux M., Atherton J., Vidaillet H.J., Jr., Spudich S., De Girolami U., et al. Missense mutations in the rod domain of the lamin A/C gene as causes of dilated cardiomyopathy and conduction-system disease. N. Engl. J. Med. 1999;341:1715–1724. doi: 10.1056/NEJM199912023412302. [DOI] [PubMed] [Google Scholar]
- 50.McNair W.P., Ku L., Taylor M.R., Fain P.R., Dao D., Wolfel E., Mestroni L., Familial cardiomyopathy registry research G. SCN5A mutation associated with dilated cardiomyopathy, conduction disorder, and arrhythmia. Circulation. 2004;110:2163–2167. doi: 10.1161/01.CIR.0000144458.58660.BB. [DOI] [PubMed] [Google Scholar]
- 51.Schonberger J., Wang L., Shin J.T., Kim S.D., Depreux F.F., Zhu H., Zon L., Pizard A., Kim J.B., Macrae C.A., et al. Mutation in the transcriptional coactivator EYA4 causes dilated cardiomyopathy and sensorineural hearing loss. Nat. Genet. 2005;37:418–422. doi: 10.1038/ng1527. [DOI] [PubMed] [Google Scholar]
- 52.Brauch K.M., Karst M.L., Herron K.J., de Andrade M., Pellikka P.A., Rodeheffer R.J., Michels V.V., Olson T.M. Mutations in ribonucleic acid binding protein gene cause familial dilated cardiomyopathy. J. Am. Coll. Cardiol. 2009;54:930–941. doi: 10.1016/j.jacc.2009.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hey T.M., Rasmussen T.B., Madsen T., Aagaard M.M., Harbo M., Molgaard H., Moller J.E., Eiskjaer H., Mogensen J. Pathogenic RBM20-variants are associated with a severe disease expression in male patients with dilated cardiomyopathy. Circ. Heart Fail. 2019;12:e005700. doi: 10.1161/CIRCHEARTFAILURE.118.005700. [DOI] [PubMed] [Google Scholar]
- 54.Nugent A.W., Daubeney P.E., Chondros P., Carlin J.B., Cheung M., Wilkinson L.C., Davis A.M., Kahler S.G., Chow C.W., Wilkinson J.L., et al. The epidemiology of childhood cardiomyopathy in Australia. N. Engl. J. Med. 2003;348:1639–1646. doi: 10.1056/NEJMoa021737. [DOI] [PubMed] [Google Scholar]
- 55.Jefferies J.L., Wilkinson J.D., Sleeper L.A., Colan S.D., Lu M., Pahl E., Kantor P.F., Everitt M.D., Webber S.A., Kaufman B.D., et al. Pediatric cardiomyopathy registry, I. Cardiomyopathy phenotypes and outcomes for children with left ventricular myocardial noncompaction: Results from the pediatric cardiomyopathy registry. J. Card. Fail. 2015;21:877–884. doi: 10.1016/j.cardfail.2015.06.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marziliano N., Mannarino S., Nespoli L., Diegoli M., Pasotti M., Malattia C., Grasso M., Pilotto A., Porcu E., Raisaro A., et al. Barth syndrome associated with compound hemizygosity and heterozygosity of the TAZ and LDB3 genes. Am. J. Med. Genet. Part A. 2007;143A:907–915. doi: 10.1002/ajmg.a.31653. [DOI] [PubMed] [Google Scholar]
- 57.Probst S., Oechslin E., Schuler P., Greutmann M., Boye P., Knirsch W., Berger F., Thierfelder L., Jenni R., Klaassen S. Sarcomere gene mutations in isolated left ventricular noncompaction cardiomyopathy do not predict clinical phenotype. Circ. Cardiovasc. Genet. 2011;4:367–374. doi: 10.1161/CIRCGENETICS.110.959270. [DOI] [PubMed] [Google Scholar]
- 58.McKoy G., Protonotarios N., Crosby A., Tsatsopoulou A., Anastasakis A., Coonar A., Norman M., Baboonian C., Jeffery S., McKenna W.J. Identification of a deletion in plakoglobin in arrhythmogenic right ventricular cardiomyopathy with palmoplantar keratoderma and woolly hair (Naxos disease) Lancet. 2000;355:2119–2124. doi: 10.1016/S0140-6736(00)02379-5. [DOI] [PubMed] [Google Scholar]
- 59.Gerull B., Heuser A., Wichter T., Paul M., Basson C.T., McDermott D.A., Lerman B.B., Markowitz S.M., Ellinor P.T., MacRae C.A., et al. Mutations in the desmosomal protein plakophilin-2 are common in arrhythmogenic right ventricular cardiomyopathy. Nat. Genet. 2004;36:1162–1164. doi: 10.1038/ng1461. [DOI] [PubMed] [Google Scholar]
- 60.Patel D.M., Green K.J. Desmosomes in the heart: A review of clinical and mechanistic analyses. Cell Commun. Adhes. 2014;21:109–128. doi: 10.3109/15419061.2014.906533. [DOI] [PubMed] [Google Scholar]
- 61.Xu T., Yang Z., Vatta M., Rampazzo A., Beffagna G., Pilichou K., Scherer S.E., Saffitz J., Kravitz J., Zareba W., et al. Multidisciplinary study of right ventricular dysplasia, I. Compound and digenic heterozygosity contributes to arrhythmogenic right ventricular cardiomyopathy. J. Am. Coll. Cardiol. 2010;55:587–597. doi: 10.1016/j.jacc.2009.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Brodehl A., Hedde P.N., Dieding M., Fatima A., Walhorn V., Gayda S., Saric T., Klauke B., Gummert J., Anselmetti D., et al. Dual color photoactivation localization microscopy of cardiomyopathy-associated desmin mutants. J. Biol. Chem. 2012;287:16047–16057. doi: 10.1074/jbc.M111.313841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Quarta G., Syrris P., Ashworth M., Jenkins S., Zuborne Alapi K., Morgan J., Muir A., Pantazis A., McKenna W.J., Elliott P.M. Mutations in the Lamin A/C gene mimic arrhythmogenic right ventricular cardiomyopathy. Eur. Heart J. 2012;33:1128–1136. doi: 10.1093/eurheartj/ehr451. [DOI] [PubMed] [Google Scholar]
- 64.Abdelfatah N., Chen R., Duff H.J., Seifer C.M., Buffo I., Huculak C., Clarke S., Clegg R., Jassal D.S., Gordon P.M.K., et al. Characterization of a unique form of arrhythmic cardiomyopathy caused by recessive mutation in LEMD2. JACC Basic Transl. Sci. 2019;4:204–221. doi: 10.1016/j.jacbts.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tiso N., Stephan D.A., Nava A., Bagattin A., Devaney J.M., Stanchi F., Larderet G., Brahmbhatt B., Brown K., Bauce B., et al. Identification of mutations in the cardiac ryanodine receptor gene in families affected with arrhythmogenic right ventricular cardiomyopathy type 2 (ARVD2) Hum. Mol. Genet. 2001;10:189–194. doi: 10.1093/hmg/10.3.189. [DOI] [PubMed] [Google Scholar]
- 66.Milting H., Lukas N., Klauke B., Korfer R., Perrot A., Osterziel K.J., Vogt J., Peters S., Thieleczek R., Varsanyi M. Composite polymorphisms in the ryanodine receptor 2 gene associated with arrhythmogenic right ventricular cardiomyopathy. Cardiovasc. Res. 2006;71:496–505. doi: 10.1016/j.cardiores.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 67.Van der Zwaag P.A., van Rijsingen I.A., Asimaki A., Jongbloed J.D., van Veldhuisen D.J., Wiesfeld A.C., Cox M.G., van Lochem L.T., de Boer R.A., Hofstra R.M., et al. Phospholamban R14del mutation in patients diagnosed with dilated cardiomyopathy or arrhythmogenic right ventricular cardiomyopathy: Evidence supporting the concept of arrhythmogenic cardiomyopathy. Eur. J. Heart Fail. 2012;14:1199–1207. doi: 10.1093/eurjhf/hfs119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brodehl A., Rezazadeh S., Williams T., Munsie N.M., Liedtke D., Oh T., Ferrier R., Shen Y., Jones S.J.M., Stiegler A.L., et al. Mutations in ILK, encoding integrin-linked kinase, are associated with arrhythmogenic cardiomyopathy. Transl. Res. 2019;208:15–29. doi: 10.1016/j.trsl.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kostareva A., Kiselev A., Gudkova A., Frishman G., Ruepp A., Frishman D., Smolina N., Tarnovskaya S., Nilsson D., Zlotina A., et al. Genetic spectrum of idiopathic restrictive cardiomyopathy uncovered by next-generation sequencing. PLoS ONE. 2016;11:e0163362. doi: 10.1371/journal.pone.0163362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gallego-Delgado M., Delgado J.F., Brossa-Loidi V., Palomo J., Marzoa-Rivas R., Perez-Villa F., Salazar-Mendiguchia J., Ruiz-Cano M.J., Gonzalez-Lopez E., Padron-Barthe L., et al. Idiopathic restrictive cardiomyopathy Is primarily a genetic disease. J. Am. Coll. Cardiol. 2016;67:3021–3023. doi: 10.1016/j.jacc.2016.04.024. [DOI] [PubMed] [Google Scholar]
- 71.Mogensen J., Kubo T., Duque M., Uribe W., Shaw A., Murphy R., Gimeno J.R., Elliott P., McKenna W.J. Idiopathic restrictive cardiomyopathy is part of the clinical expression of cardiac troponin I mutations. J. Clin. Investig. 2003;111:209–216. doi: 10.1172/JCI200316336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brodehl A., Ferrier R.A., Hamilton S.J., Greenway S.C., Brundler M.A., Yu W., Gibson W.T., McKinnon M.L., McGillivray B., Alvarez N., et al. Mutations in FLNC are associated with familial restrictive cardiomyopathy. Hum. Mutat. 2016;37:269–279. doi: 10.1002/humu.22942. [DOI] [PubMed] [Google Scholar]
- 73.Tucker N.R., McLellan M.A., Hu D., Ye J., Parsons V.A., Mills R.W., Clauss S., Dolmatova E., Shea M.A., Milan D.J., et al. Novel mutation in FLNC (Filamin C) causes familial restrictive cardiomyopathy. Circ. Cardiovasc. Genet. 2017;10:e001780. doi: 10.1161/CIRCGENETICS.117.001780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kiselev A., Vaz R., Knyazeva A., Khudiakov A., Tarnovskaya S., Liu J., Sergushichev A., Kazakov S., Frishman D., Smolina N., et al. De novo mutations in FLNC leading to early-onset restrictive cardiomyopathy and congenital myopathy. Hum. Mutat. 2018;39:1161–1172. doi: 10.1002/humu.23559. [DOI] [PubMed] [Google Scholar]
- 75.Schubert J., Tariq M., Geddes G., Kindel S., Miller E.M., Ware S.M. Novel pathogenic variants in filamin C identified in pediatric restrictive cardiomyopathy. Hum. Mutat. 2018;39:2083–2096. doi: 10.1002/humu.23661. [DOI] [PubMed] [Google Scholar]
- 76.Roldan-Sevilla A., Palomino-Doza J., de Juan J., Sanchez V., Dominguez-Gonzalez C., Salguero-Bodes R., Arribas-Ynsaurriaga F. Missense mutations in the FLNC gene causing familial restrictive cardiomyopathy. Circ. Genom. Precis. Med. 2019;12:e002388. doi: 10.1161/CIRCGEN.118.002388. [DOI] [PubMed] [Google Scholar]
- 77.Bienengraeber M., Olson T.M., Selivanov V.A., Kathmann E.C., O’Cochlain F., Gao F., Karger A.B., Ballew J.D., Hodgson D.M., Zingman L.V., et al. ABCC9 mutations identified in human dilated cardiomyopathy disrupt catalytic KATP channel gating. Nat. Genet. 2004;36:382–387. doi: 10.1038/ng1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Collet M., Assouline Z., Bonnet D., Rio M., Iserin F., Sidi D., Goldenberg A., Lardennois C., Metodiev M.D., Haberberger B., et al. High incidence and variable clinical outcome of cardiac hypertrophy due to ACAD9 mutations in childhood. Eur. J. Hum. Genet. 2016;24:1112–1116. doi: 10.1038/ejhg.2015.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carlus S.J., Almuzaini I.S., Karthikeyan M., Loganathan L., Al-Harbi G.S., Abdallah A.M., Al-Harbi K.M. Next-generation sequencing identifies a homozygous mutation in ACADVL associated with pediatric familial dilated cardiomyopathy. Eur. Rev. Med. Pharmacol. Sci. 2019;23:1710–1721. doi: 10.26355/eurrev_201902_17133. [DOI] [PubMed] [Google Scholar]
- 80.Monserrat L., Hermida-Prieto M., Fernandez X., Rodriguez I., Dumont C., Cazon L., Cuesta M.G., Gonzalez-Juanatey C., Peteiro J., Alvarez N., et al. Mutation in the alpha-cardiac actin gene associated with apical hypertrophic cardiomyopathy, left ventricular non-compaction, and septal defects. Eur. Heart J. 2007;28:1953–1961. doi: 10.1093/eurheartj/ehm239. [DOI] [PubMed] [Google Scholar]
- 81.Olson T.M., Michels V.V., Thibodeau S.N., Tai Y.S., Keating M.T. Actin mutations in dilated cardiomyopathy, a heritable form of heart failure. Science. 1998;280:750–752. doi: 10.1126/science.280.5364.750. [DOI] [PubMed] [Google Scholar]
- 82.Klaassen S., Probst S., Oechslin E., Gerull B., Krings G., Schuler P., Greutmann M., Hurlimann D., Yegitbasi M., Pons L., et al. Mutations in sarcomere protein genes in left ventricular noncompaction. Circulation. 2008;117:2893–2901. doi: 10.1161/CIRCULATIONAHA.107.746164. [DOI] [PubMed] [Google Scholar]
- 83.Kaski J.P., Syrris P., Burch M., Tome-Esteban M.T., Fenton M., Christiansen M., Andersen P.S., Sebire N., Ashworth M., Deanfield J.E., et al. Idiopathic restrictive cardiomyopathy in children is caused by mutations in cardiac sarcomere protein genes. Heart. 2008;94:1478–1484. doi: 10.1136/hrt.2007.134684. [DOI] [PubMed] [Google Scholar]
- 84.Chiu C., Bagnall R.D., Ingles J., Yeates L., Kennerson M., Donald J.A., Jormakka M., Lind J.M., Semsarian C. Mutations in alpha-actinin-2 cause hypertrophic cardiomyopathy: A genome-wide analysis. J. Am. Coll. Cardiol. 2010;55:1127–1135. doi: 10.1016/j.jacc.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 85.Mohapatra B., Jimenez S., Lin J.H., Bowles K.R., Coveler K.J., Marx J.G., Chrisco M.A., Murphy R.T., Lurie P.R., Schwartz R.J., et al. Mutations in the muscle LIM protein and alpha-actinin-2 genes in dilated cardiomyopathy and endocardial fibroelastosis. Mol. Genet. Metab. 2003;80:207–215. doi: 10.1016/S1096-7192(03)00142-2. [DOI] [PubMed] [Google Scholar]
- 86.Bagnall R.D., Molloy L.K., Kalman J.M., Semsarian C. Exome sequencing identifies a mutation in the ACTN2 gene in a family with idiopathic ventricular fibrillation, left ventricular noncompaction, and sudden death. BMC Med. Genet. 2014;15:99. doi: 10.1186/s12881-014-0099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Waldmuller S., Schroeder C., Sturm M., Scheffold T., Imbrich K., Junker S., Frische C., Hofbeck M., Bauer P., Bonin M., et al. Targeted 46-gene and clinical exome sequencing for mutations causing cardiomyopathies. Mol. Cell. Probes. 2015;29:308–314. doi: 10.1016/j.mcp.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 88.Forleo C., D’Erchia A.M., Sorrentino S., Manzari C., Chiara M., Iacoviello M., Guaricci A.I., De Santis D., Musci R.L., La Spada A., et al. Targeted next-generation sequencing detects novel gene-phenotype associations and expands the mutational spectrum in cardiomyopathies. PLoS ONE. 2017;12:e0181842. doi: 10.1371/journal.pone.0181842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nerakh G., Ranganath P. Alstrom syndrome presenting as isolated dilated cardiomyopathy. Indian J. Pediatr. 2019;86:296–298. doi: 10.1007/s12098-018-2807-9. [DOI] [PubMed] [Google Scholar]
- 90.Almomani R., Verhagen J.M., Herkert J.C., Brosens E., van Spaendonck-Zwarts K.Y., Asimaki A., van der Zwaag P.A., Frohn-Mulder I.M., Bertoli-Avella A.M., Boven L.G., et al. Biallelic truncating mutations in ALPK3 cause severe pediatric cardiomyopathy. J. Am. Coll. Cardiol. 2016;67:515–525. doi: 10.1016/j.jacc.2015.10.093. [DOI] [PubMed] [Google Scholar]
- 91.Lopes L.R., Syrris P., Guttmann O.P., O’Mahony C., Tang H.C., Dalageorgou C., Jenkins S., Hubank M., Monserrat L., McKenna W.J., et al. Novel genotype-phenotype associations demonstrated by high-throughput sequencing in patients with hypertrophic cardiomyopathy. Heart. 2015;101:294–301. doi: 10.1136/heartjnl-2014-306387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Roberts J.D., Murphy N.P., Hamilton R.M., Lubbers E.R., James C.A., Kline C.F., Gollob M.H., Krahn A.D., Sturm A.C., Musa H., et al. Ankyrin-B dysfunction predisposes to arrhythmogenic cardiomyopathy and is amenable to therapy. J. Clin. Investig. 2019;129:3171–3184. doi: 10.1172/JCI125538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Arimura T., Bos J.M., Sato A., Kubo T., Okamoto H., Nishi H., Harada H., Koga Y., Moulik M., Doi Y.L., et al. Cardiac ankyrin repeat protein gene (ANKRD1) mutations in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2009;54:334–342. doi: 10.1016/j.jacc.2008.12.082. [DOI] [PubMed] [Google Scholar]
- 94.Duboscq-Bidot L., Charron P., Ruppert V., Fauchier L., Richter A., Tavazzi L., Arbustini E., Wichter T., Maisch B., Komajda M., et al. Mutations in the ANKRD1 gene encoding CARP are responsible for human dilated cardiomyopathy. Eur. Heart J. 2009;30:2128–2136. doi: 10.1093/eurheartj/ehp225. [DOI] [PubMed] [Google Scholar]
- 95.Moulik M., Vatta M., Witt S.H., Arola A.M., Murphy R.T., McKenna W.J., Boriek A.M., Oka K., Labeit S., Bowles N.E., et al. ANKRD1, the gene encoding cardiac ankyrin repeat protein, is a novel dilated cardiomyopathy gene. J. Am. Coll. Cardiol. 2009;54:325–333. doi: 10.1016/j.jacc.2009.02.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Norton N., Li D., Rieder M.J., Siegfried J.D., Rampersaud E., Zuchner S., Mangos S., Gonzalez-Quintana J., Wang L., McGee S., et al. Genome-wide studies of copy number variation and exome sequencing identify rare variants in BAG3 as a cause of dilated cardiomyopathy. Am. J. Hum. Genet. 2011;88:273–282. doi: 10.1016/j.ajhg.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Schanzer A., Rupp S., Graf S., Zengeler D., Jux C., Akinturk H., Gulatz L., Mazhari N., Acker T., Van Coster R., et al. Dysregulated autophagy in restrictive cardiomyopathy due to Pro209Leu mutation in BAG3. Mol. Genet. Metab. 2018;123:388–399. doi: 10.1016/j.ymgme.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 98.Gripp K.W., Lin A.E., Nicholson L., Allen W., Cramer A., Jones K.L., Kutz W., Peck D., Rebolledo M.A., Wheeler P.G., et al. Further delineation of the phenotype resulting from BRAF or MEK1 germline mutations helps differentiate cardio-facio-cutaneous syndrome from Costello syndrome. Am. J. Med. Genet. Part A. 2007;143A:1472–1480. doi: 10.1002/ajmg.a.31815. [DOI] [PubMed] [Google Scholar]
- 99.Shakeel M., Irfan M., Khan I.A. Rare genetic mutations in Pakistani patients with dilated cardiomyopathy. Gene. 2018;673:134–139. doi: 10.1016/j.gene.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 100.Boczek N.J., Ye D., Jin F., Tester D.J., Huseby A., Bos J.M., Johnson A.J., Kanter R., Ackerman M.J. Identification and functional characterization of a novel CACNA1C-mediated cardiac disorder characterized by prolonged QT intervals with hypertrophic cardiomyopathy, congenital heart defects, and sudden cardiac death. Circ. Arrhythm. Electrophysiol. 2015;8:1122–1132. doi: 10.1161/CIRCEP.115.002745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Friedrich F.W., Bausero P., Sun Y., Treszl A., Kramer E., Juhr D., Richard P., Wegscheider K., Schwartz K., Brito D., et al. A new polymorphism in human calmodulin III gene promoter is a potential modifier gene for familial hypertrophic cardiomyopathy. Eur. Heart J. 2009;30:1648–1655. doi: 10.1093/eurheartj/ehp153. [DOI] [PubMed] [Google Scholar]
- 102.Qiu X.B., Qu X.K., Li R.G., Liu H., Xu Y.J., Zhang M., Shi H.Y., Hou X.M., Liu X., Yuan F., et al. CASZ1 loss-of-function mutation contributes to familial dilated cardiomyopathy. Clin. Chem. Lab. Med. 2017;55:1417–1425. doi: 10.1515/cclm-2016-0612. [DOI] [PubMed] [Google Scholar]
- 103.Guo J., Li Z., Hao C., Guo R., Hu X., Qian S., Zeng J., Gao H., Li W. A novel de novo CASZ1 heterozygous frameshift variant causes dilated cardiomyopathy and left ventricular noncompaction cardiomyopathy. Mol. Genet. Genom. Med. 2019;7:e828. doi: 10.1002/mgg3.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hayashi T., Arimura T., Ueda K., Shibata H., Hohda S., Takahashi M., Hori H., Koga Y., Oka N., Imaizumi T., et al. Identification and functional analysis of a caveolin-3 mutation associated with familial hypertrophic cardiomyopathy. Biochem. Biophys. Res. Commun. 2004;313:178–184. doi: 10.1016/j.bbrc.2003.11.101. [DOI] [PubMed] [Google Scholar]
- 105.Rodriguez G., Ueyama T., Ogata T., Czernuszewicz G., Tan Y., Dorn G.W., II, Bogaev R., Amano K., Oh H., Matsubara H., et al. Molecular genetic and functional characterization implicate muscle-restricted coiled-coil gene (MURC) as a causal gene for familial dilated cardiomyopathy. Circ. Cardiovasc. Genet. 2011;4:349–358. doi: 10.1161/CIRCGENETICS.111.959866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mayosi B.M., Fish M., Shaboodien G., Mastantuono E., Kraus S., Wieland T., Kotta M.C., Chin A., Laing N., Ntusi N.B., et al. Identification of Cadherin 2 (CDH2) mutations in arrhythmogenic right ventricular cardiomyopathy. Circ. Cardiovasc. Genet. 2017;10:e001605. doi: 10.1161/CIRCGENETICS.116.001605. [DOI] [PubMed] [Google Scholar]
- 107.Turkowski K.L., Tester D.J., Bos J.M., Haugaa K.H., Ackerman M.J. Whole exome sequencing with genomic triangulation implicates CDH2-encoded N-cadherin as a novel pathogenic substrate for arrhythmogenic cardiomyopathy. Congenit. Heart Dis. 2017;12:226–235. doi: 10.1111/chd.12462. [DOI] [PubMed] [Google Scholar]
- 108.Zhang L., Hu A., Yuan H., Cui L., Miao G., Yang X., Wang L., Liu J., Liu X., Wang S., et al. A missense mutation in the CHRM2 gene is associated with familial dilated cardiomyopathy. Circ. Res. 2008;102:1426–1432. doi: 10.1161/CIRCRESAHA.107.167783. [DOI] [PubMed] [Google Scholar]
- 109.Lan N.S.R., Fietz M., Pachter N., Paul V., Playford D. A case of vascular Ehlers-Danlos Syndrome with a cardiomyopathy and multi-system involvement. Cardiovasc. Pathol. 2018;35:48–51. doi: 10.1016/j.carpath.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 110.Antonicka H., Mattman A., Carlson C.G., Glerum D.M., Hoffbuhr K.C., Leary S.C., Kennaway N.G., Shoubridge E.A. Mutations in COX15 produce a defect in the mitochondrial heme biosynthetic pathway, causing early-onset fatal hypertrophic cardiomyopathy. Am. J. Hum. Genet. 2003;72:101–114. doi: 10.1086/345489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Inagaki N., Hayashi T., Arimura T., Koga Y., Takahashi M., Shibata H., Teraoka K., Chikamori T., Yamashina A., Kimura A. αB-crystallin mutation in dilated cardiomyopathy. Biochem. Biophys. Res. Commun. 2006;342:379–386. doi: 10.1016/j.bbrc.2006.01.154. [DOI] [PubMed] [Google Scholar]
- 112.Brodehl A., Gaertner-Rommel A., Klauke B., Grewe S.A., Schirmer I., Peterschroder A., Faber L., Vorgerd M., Gummert J., Anselmetti D., et al. The novel αB-crystallin (CRYAB) mutation p.D109G causes restrictive cardiomyopathy. Hum. Mutat. 2017;38:947–952. doi: 10.1002/humu.23248. [DOI] [PubMed] [Google Scholar]
- 113.Newman B., Cescon D., Woo A., Rakowski H., Erikkson M.J., Sole M., Wigle E.D., Siminovitch K.A. W4R variant in CSRP3 encoding muscle LIM protein in a patient with hypertrophic cardiomyopathy. Mol. Genet. Metab. 2005;84:374–375. doi: 10.1016/j.ymgme.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 114.Geier C., Gehmlich K., Ehler E., Hassfeld S., Perrot A., Hayess K., Cardim N., Wenzel K., Erdmann B., Krackhardt F., et al. Beyond the sarcomere: CSRP3 mutations cause hypertrophic cardiomyopathy. Hum. Mol. Genet. 2008;17:2753–2765. doi: 10.1093/hmg/ddn160. [DOI] [PubMed] [Google Scholar]
- 115.Janin A., Bessiere F., Chauveau S., Chevalier P., Millat G. First identification of homozygous truncating CSRP3 variants in two unrelated cases with hypertrophic cardiomyopathy. Gene. 2018;676:110–116. doi: 10.1016/j.gene.2018.07.036. [DOI] [PubMed] [Google Scholar]
- 116.Hershberger R.E., Parks S.B., Kushner J.D., Li D., Ludwigsen S., Jakobs P., Nauman D., Burgess D., Partain J., Litt M. Coding sequence mutations identified in MYH7, TNNT2, SCN5A, CSRP3, LBD3, and TCAP from 313 patients with familial or idiopathic dilated cardiomyopathy. Clin. Transl. Sci. 2008;1:21–26. doi: 10.1111/j.1752-8062.2008.00017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Erdmann J., Hassfeld S., Kallisch H., Fleck E., Regitz-Zagrose V. Genetic variants in the promoter (g983G>T) and coding region (A92T) of the human cardiotrophin-1 gene (CTF1) in patients with dilated cardiomyopathy. Hum. Mutat. 2000;16:448. doi: 10.1002/1098-1004(200011)16:5<448::AID-HUMU19>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 118.Van Hengel J., Calore M., Bauce B., Dazzo E., Mazzotti E., De Bortoli M., Lorenzon A., Li Mura I.E., Beffagna G., Rigato I., et al. Mutations in the area composita protein alphaT-catenin are associated with arrhythmogenic right ventricular cardiomyopathy. Eur. Heart J. 2013;34:201–210. doi: 10.1093/eurheartj/ehs373. [DOI] [PubMed] [Google Scholar]
- 119.Taylor M.R., Slavov D., Ku L., Di Lenarda A., Sinagra G., Carniel E., Haubold K., Boucek M.M., Ferguson D., Graw S.L., et al. Prevalence of desmin mutations in dilated cardiomyopathy. Circulation. 2007;115:1244–1251. doi: 10.1161/CIRCULATIONAHA.106.646778. [DOI] [PubMed] [Google Scholar]
- 120.Towbin J.A., Hejtmancik J.F., Brink P., Gelb B., Zhu X.M., Chamberlain J.S., McCabe E.R., Swift M. X-linked dilated cardiomyopathy. Molecular genetic evidence of linkage to the Duchenne muscular dystrophy (dystrophin) gene at the Xp21 locus. Circulation. 1993;87:1854–1865. doi: 10.1161/01.CIR.87.6.1854. [DOI] [PubMed] [Google Scholar]
- 121.Ojala T., Polinati P., Manninen T., Hiippala A., Rajantie J., Karikoski R., Suomalainen A., Tyni T. New mutation of mitochondrial DNAJC19 causing dilated and noncompaction cardiomyopathy, anemia, ataxia, and male genital anomalies. Pediatr. Res. 2012;72:432–437. doi: 10.1038/pr.2012.92. [DOI] [PubMed] [Google Scholar]
- 122.Rush E.T., Baker C.V., Rizzo W.B. Dolichol kinase deficiency (DOLK-CDG): Two new cases and expansion of phenotype. Am. J. Med. Genet. Part A. 2017;173:2428–2434. doi: 10.1002/ajmg.a.38287. [DOI] [PubMed] [Google Scholar]
- 123.Svahn J., Laforet P., Vial C., Streichenberger N., Romero N., Bouchet-Seraphin C., Bruneel A., Dupre T., Seta N., Menassa R., et al. Dilated cardiomyopathy and limb-girdle muscular dystrophy-dystroglycanopathy due to novel pathogenic variants in the DPM3 gene. Neuromuscul. Disord. 2019;29:497–502. doi: 10.1016/j.nmd.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 124.Heuser A., Plovie E.R., Ellinor P.T., Grossmann K.S., Shin J.T., Wichter T., Basson C.T., Lerman B.B., Sasse-Klaassen S., Thierfelder L., et al. Mutant desmocollin-2 causes arrhythmogenic right ventricular cardiomyopathy. Am. J. Hum. Genet. 2006;79:1081–1088. doi: 10.1086/509044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Posch M.G., Posch M.J., Geier C., Erdmann B., Mueller W., Richter A., Ruppert V., Pankuweit S., Maisch B., Perrot A., et al. A missense variant in desmoglein-2 predisposes to dilated cardiomyopathy. Mol. Genet. Metab. 2008;95:74–80. doi: 10.1016/j.ymgme.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 126.Awad M.M., Dalal D., Cho E., Amat-Alarcon N., James C., Tichnell C., Tucker A., Russell S.D., Bluemke D.A., Dietz H.C., et al. DSG2 mutations contribute to arrhythmogenic right ventricular dysplasia/cardiomyopathy. Am. J. Hum. Genet. 2006;79:136–142. doi: 10.1086/504393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pilichou K., Nava A., Basso C., Beffagna G., Bauce B., Lorenzon A., Frigo G., Vettori A., Valente M., Towbin J., et al. Mutations in desmoglein-2 gene are associated with arrhythmogenic right ventricular cardiomyopathy. Circulation. 2006;113:1171–1179. doi: 10.1161/CIRCULATIONAHA.105.583674. [DOI] [PubMed] [Google Scholar]
- 128.Norgett E.E., Hatsell S.J., Carvajal-Huerta L., Cabezas J.C., Common J., Purkis P.E., Whittock N., Leigh I.M., Stevens H.P., Kelsell D.P. Recessive mutation in desmoplakin disrupts desmoplakin-intermediate filament interactions and causes dilated cardiomyopathy, woolly hair and keratoderma. Hum. Mol. Genet. 2000;9:2761–2766. doi: 10.1093/hmg/9.18.2761. [DOI] [PubMed] [Google Scholar]
- 129.Williams T., Machann W., Kuhler L., Hamm H., Muller-Hocker J., Zimmer M., Ertl G., Ritter O., Beer M., Schonberger J. Novel desmoplakin mutation: Juvenile biventricular cardiomyopathy with left ventricular non-compaction and acantholytic palmoplantar keratoderma. Clin. Res. Cardiol. 2011;100:1087–1093. doi: 10.1007/s00392-011-0345-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rampazzo A., Nava A., Malacrida S., Beffagna G., Bauce B., Rossi V., Zimbello R., Simionati B., Basso C., Thiene G., et al. Mutation in human desmoplakin domain binding to plakoglobin causes a dominant form of arrhythmogenic right ventricular cardiomyopathy. Am. J. Hum. Genet. 2002;71:1200–1206. doi: 10.1086/344208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cao Q., Shen Y., Liu X., Yu X., Yuan P., Wan R., Liu X., Peng X., He W., Pu J., et al. Phenotype and functional analyses in a transgenic mouse model of left ventricular noncompaction caused by a DTNA mutation. Int. Heart J. 2017;58:939–947. doi: 10.1536/ihj.16-019. [DOI] [PubMed] [Google Scholar]
- 132.Haack T.B., Kopajtich R., Freisinger P., Wieland T., Rorbach J., Nicholls T.J., Baruffini E., Walther A., Danhauser K., Zimmermann F.A., et al. ELAC2 mutations cause a mitochondrial RNA processing defect associated with hypertrophic cardiomyopathy. Am. J. Hum. Genet. 2013;93:211–223. doi: 10.1016/j.ajhg.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang M., Chen J., Si D., Zheng Y., Jiao H., Feng Z., Hu Z., Duan R. Whole exome sequencing identifies a novel EMD mutation in a Chinese family with dilated cardiomyopathy. BMC Med. Genet. 2014;15:77. doi: 10.1186/1471-2350-15-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tang S., Hoshida H., Kamisago M., Yagi H., Momma K., Matsuoka R. Phenotype-genotype correlation in a patient with co-occurrence of Marfan and LEOPARD syndromes. Am. J. Med. Genet. Part A. 2009;149A:2216–2219. doi: 10.1002/ajmg.a.32735. [DOI] [PubMed] [Google Scholar]
- 135.Jacobs A.M., Toudjarska I., Racine A., Tsipouras P., Kilpatrick M.W., Shanske A. A recurring FBN1 gene mutation in neonatal Marfan syndrome. Arch. Pediatr. Adolesc. Med. 2002;156:1081–1085. doi: 10.1001/archpedi.156.11.1081. [DOI] [PubMed] [Google Scholar]
- 136.Parent J.J., Towbin J.A., Jefferies J.L. Fibrillin-1 gene mutations in left ventricular non-compaction cardiomyopathy. Pediatr. Cardiol. 2016;37:1123–1126. doi: 10.1007/s00246-016-1404-9. [DOI] [PubMed] [Google Scholar]
- 137.Al-Yacoub N., Shaheen R., Awad S.M., Kunhi M., Dzimiri N., Nguyen H.C., Xiong Y., Al-Buraiki J., Al-Habeeb W., Alkuraya F.S., et al. FBXO32, encoding a member of the SCF complex, is mutated in dilated cardiomyopathy. Genome Biol. 2016;17:2. doi: 10.1186/s13059-015-0861-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Al-Hassnan Z.N., Shinwari Z.M., Wakil S.M., Tulbah S., Mohammed S., Rahbeeni Z., Alghamdi M., Rababh M., Colak D., Kaya N., et al. A substitution mutation in cardiac ubiquitin ligase, FBXO32, is associated with an autosomal recessive form of dilated cardiomyopathy. BMC Med. Genet. 2016;17:3. doi: 10.1186/s12881-016-0267-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Arimura T., Hayashi T., Matsumoto Y., Shibata H., Hiroi S., Nakamura T., Inagaki N., Hinohara K., Takahashi M., Manatsu S.I., et al. Structural analysis of four and half LIM protein-2 in dilated cardiomyopathy. Biochem. Biophys. Res. Commun. 2007;357:162–167. doi: 10.1016/j.bbrc.2007.03.128. [DOI] [PubMed] [Google Scholar]
- 140.Ochoa J.P., Sabater-Molina M., Garcia-Pinilla J.M., Mogensen J., Restrepo-Cordoba A., Palomino-Doza J., Villacorta E., Martinez-Moreno M., Ramos-Maqueda J., Zorio E., et al. Formin Homology 2 Domain Containing 3 (FHOD3) Is a genetic basis for hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2018;72:2457–2467. doi: 10.1016/j.jacc.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 141.Arimura T., Takeya R., Ishikawa T., Yamano T., Matsuo A., Tatsumi T., Nomura T., Sumimoto H., Kimura A. Dilated cardiomyopathy-associated FHOD3 variant impairs the ability to induce activation of transcription factor serum response factor. Circ. J. 2013;77:2990–2996. doi: 10.1253/circj.CJ-13-0255. [DOI] [PubMed] [Google Scholar]
- 142.Muller T., Krasnianski M., Witthaut R., Deschauer M., Zierz S. Dilated cardiomyopathy may be an early sign of the C826A Fukutin-related protein mutation. Neuromuscul. Disord. 2005;15:372–376. doi: 10.1016/j.nmd.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 143.Amiya E., Morita H., Hatano M., Nitta D., Hosoya Y., Maki H., Motozawa Y., Sato N., Ishiura H., Numakura S., et al. Fukutin gene mutations that cause left ventricular noncompaction. Int. J. Cardiol. 2016;222:727–729. doi: 10.1016/j.ijcard.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 144.Begay R.L., Tharp C.A., Martin A., Graw S.L., Sinagra G., Miani D., Sweet M.E., Slavov D.B., Stafford N., Zeller M.J., et al. FLNC gene splice mutations cause dilated cardiomyopathy. JACC Basic Transl. Sci. 2016;1:344–359. doi: 10.1016/j.jacbts.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ortiz-Genga M.F., Cuenca S., Dal Ferro M., Zorio E., Salgado-Aranda R., Climent V., Padron-Barthe L., Duro-Aguado I., Jimenez-Jaimez J., Hidalgo-Olivares V.M., et al. Truncating FLNC mutations are associated with high-risk dilated and arrhythmogenic cardiomyopathies. J. Am. Coll. Cardiol. 2016;68:2440–2451. doi: 10.1016/j.jacc.2016.09.927. [DOI] [PubMed] [Google Scholar]
- 146.Minoretti P., Arra M., Emanuele E., Olivieri V., Aldeghi A., Politi P., Martinelli V., Pesenti S., Falcone C. A W148R mutation in the human FOXD4 gene segregating with dilated cardiomyopathy, obsessive-compulsive disorder, and suicidality. Int. J. Mol. Med. 2007;19:369–372. doi: 10.3892/ijmm.19.3.369. [DOI] [PubMed] [Google Scholar]
- 147.Payne R.M., Wagner G.R. Cardiomyopathy in Friedreich ataxia: Clinical findings and research. J. Child Neurol. 2012;27:1179–1186. doi: 10.1177/0883073812448535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Campuzano V., Montermini L., Molto M.D., Pianese L., Cossee M., Cavalcanti F., Monros E., Rodius F., Duclos F., Monticelli A., et al. Friedreich’s ataxia: Autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271:1423–1427. doi: 10.1126/science.271.5254.1423. [DOI] [PubMed] [Google Scholar]
- 149.Li R.G., Li L., Qiu X.B., Yuan F., Xu L., Li X., Xu Y.J., Jiang W.F., Jiang J.Q., Liu X., et al. GATA4 loss-of-function mutation underlies familial dilated cardiomyopathy. Biochem. Biophys. Res. Commun. 2013;439:591–596. doi: 10.1016/j.bbrc.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 150.Tang V.T., Arscott P., Helms A.S., Day S.M. Whole-exome sequencing reveals GATA4 and PTEN mutations as a potential digenic cause of left ventricular noncompaction. Circ. Genom. Precis. Med. 2018;11:e001966. doi: 10.1161/CIRCGEN.117.001966. [DOI] [PubMed] [Google Scholar]
- 151.Zhang X.L., Dai N., Tang K., Chen Y.Q., Chen W., Wang J., Zhao C.M., Yuan F., Qiu X.B., Qu X.K., et al. GATA5 loss-of-function mutation in familial dilated cardiomyopathy. Int. J. Mol. Med. 2015;35:763–770. doi: 10.3892/ijmm.2014.2050. [DOI] [PubMed] [Google Scholar]
- 152.Theis J.L., Sharpe K.M., Matsumoto M.E., Chai H.S., Nair A.A., Theis J.D., de Andrade M., Wieben E.D., Michels V.V., Olson T.M. Homozygosity mapping and exome sequencing reveal GATAD1 mutation in autosomal recessive dilated cardiomyopathy. Circ. Cardiovasc. Genet. 2011;4:585–594. doi: 10.1161/CIRCGENETICS.111.961052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Arad M., Penas-Lado M., Monserrat L., Maron B.J., Sherrid M., Ho C.Y., Barr S., Karim A., Olson T.M., Kamisago M., et al. Gene mutations in apical hypertrophic cardiomyopathy. Circulation. 2005;112:2805–2811. doi: 10.1161/CIRCULATIONAHA.105.547448. [DOI] [PubMed] [Google Scholar]
- 154.Kopajtich R., Nicholls T.J., Rorbach J., Metodiev M.D., Freisinger P., Mandel H., Vanlander A., Ghezzi D., Carrozzo R., Taylor R.W., et al. Mutations in GTPBP3 cause a mitochondrial translation defect associated with hypertrophic cardiomyopathy, lactic acidosis, and encephalopathy. Am. J. Hum. Genet. 2014;95:708–720. doi: 10.1016/j.ajhg.2014.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zhou Y.M., Dai X.Y., Qiu X.B., Yuan F., Li R.G., Xu Y.J., Qu X.K., Huang R.T., Xue S., Yang Y.Q. HAND1 loss-of-function mutation associated with familial dilated cardiomyopathy. Clin. Chem. Lab. Med. 2016;54:1161–1167. doi: 10.1515/cclm-2015-0766. [DOI] [PubMed] [Google Scholar]
- 156.Liu H., Xu Y.J., Li R.G., Wang Z.S., Zhang M., Qu X.K., Qiao Q., Li X.M., Di R.M., Qiu X.B., et al. HAND2 loss-of-function mutation causes familial dilated cardiomyopathy. Eur. J. Med. Genet. 2018 doi: 10.1016/j.ejmg.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 157.Milano A., Vermeer A.M., Lodder E.M., Barc J., Verkerk A.O., Postma A.V., van der Bilt I.A., Baars M.J., van Haelst P.L., Caliskan K., et al. HCN4 mutations in multiple families with bradycardia and left ventricular noncompaction cardiomyopathy. J. Am. Coll. Cardiol. 2014;64:745–756. doi: 10.1016/j.jacc.2014.05.045. [DOI] [PubMed] [Google Scholar]
- 158.Hiippala A., Vasilescu C., Tallila J., Alastalo T.P., Paetau A., Tyni T., Suomalainen A., Euro L., Ojala T. The rare Costello variant HRAS c.173C>T (p.T58I) with severe neonatal hypertrophic cardiomyopathy. Am. J. Med. Genet. Part A. 2016;170:1433–1438. doi: 10.1002/ajmg.a.37596. [DOI] [PubMed] [Google Scholar]
- 159.Knoll R., Postel R., Wang J., Kratzner R., Hennecke G., Vacaru A.M., Vakeel P., Schubert C., Murthy K., Rana B.K., et al. Laminin-alpha4 and integrin-linked kinase mutations cause human cardiomyopathy via simultaneous defects in cardiomyocytes and endothelial cells. Circulation. 2007;116:515–525. doi: 10.1161/CIRCULATIONAHA.107.689984. [DOI] [PubMed] [Google Scholar]
- 160.Meder B., Haas J., Keller A., Heid C., Just S., Borries A., Boisguerin V., Scharfenberger-Schmeer M., Stahler P., Beier M., et al. Targeted next-generation sequencing for the molecular genetic diagnostics of cardiomyopathies. Circ. Cardiovasc. Genet. 2011;4:110–122. doi: 10.1161/CIRCGENETICS.110.958322. [DOI] [PubMed] [Google Scholar]
- 161.Xu Y.J., Wang Z.S., Yang C.X., Di R.M., Qiao Q., Li X.M., Gu J.N., Guo X.J., Yang Y.Q. Identification and functional characterization of an ISL1 mutation predisposing to dilated cardiomyopathy. J. Cardiovasc. Transl. Res. 2019;12:257–267. doi: 10.1007/s12265-018-9851-8. [DOI] [PubMed] [Google Scholar]
- 162.Esposito T., Sampaolo S., Limongelli G., Varone A., Formicola D., Diodato D., Farina O., Napolitano F., Pacileo G., Gianfrancesco F., et al. Digenic mutational inheritance of the integrin alpha 7 and the myosin heavy chain 7B genes causes congenital myopathy with left ventricular non-compact cardiomyopathy. Orphanet J. Rare Dis. 2013;8:91. doi: 10.1186/1750-1172-8-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Handley M.T., Reddy K., Wills J., Rosser E., Kamath A., Halachev M., Falkous G., Williams D., Cox P., Meynert A., et al. ITPase deficiency causes a Martsolf-like syndrome with a lethal infantile dilated cardiomyopathy. PLoS Genet. 2019;15:e1007605. doi: 10.1371/journal.pgen.1007605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Matsushita Y., Furukawa T., Kasanuki H., Nishibatake M., Kurihara Y., Ikeda A., Kamatani N., Takeshima H., Matsuoka R. Mutation of junctophilin type 2 associated with hypertrophic cardiomyopathy. J. Hum. Genet. 2007;52:543–548. doi: 10.1007/s10038-007-0149-y. [DOI] [PubMed] [Google Scholar]
- 165.Sabater-Molina M., Navarro M., Garcia-Molina Saez E., Garrido I., Pascual-Figal D., Gonzalez Carrillo J., Gimeno Blanes J.R. Mutation in JPH2 cause dilated cardiomyopathy. Clin. Genet. 2016;90:468–469. doi: 10.1111/cge.12825. [DOI] [PubMed] [Google Scholar]
- 166.Xiong Q., Cao Q., Zhou Q., Xie J., Shen Y., Wan R., Yu J., Yan S., Marian A.J., Hong K. Arrhythmogenic cardiomyopathy in a patient with a rare loss-of-function KCNQ1 mutation. J. Am. Heart Assoc. 2015;4:e001526. doi: 10.1161/JAHA.114.001526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hedberg-Oldfors C., Abramsson A., Osborn D.P.S., Danielsson O., Fazlinezhad A., Nilipour Y., Hubbert L., Nennesmo I., Visuttijai K., Bharj J., et al. Cardiomyopathy with lethal arrhythmias associated with inactivation of KLHL24. Hum. Mol. Genet. 2019;28:1919–1929. doi: 10.1093/hmg/ddz032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Arad M., Maron B.J., Gorham J.M., Johnson W.H., Jr., Saul J.P., Perez-Atayde A.R., Spirito P., Wright G.B., Kanter R.J., Seidman C.E., et al. Glycogen storage diseases presenting as hypertrophic cardiomyopathy. N. Engl. J. Med. 2005;352:362–372. doi: 10.1056/NEJMoa033349. [DOI] [PubMed] [Google Scholar]
- 169.Fratev F., Mihaylova E., Pajeva I. Combination of genetic screening and molecular dynamics as a useful tool for identification of disease-related mutations: ZASP PDZ domain G54S mutation case. J. Chem. Inf. Model. 2014;54:1524–1536. doi: 10.1021/ci5001136. [DOI] [PubMed] [Google Scholar]
- 170.Vatta M., Mohapatra B., Jimenez S., Sanchez X., Faulkner G., Perles Z., Sinagra G., Lin J.H., Vu T.M., Zhou Q., et al. Mutations in Cypher/ZASP in patients with dilated cardiomyopathy and left ventricular non-compaction. J. Am. Coll. Cardiol. 2003;42:2014–2027. doi: 10.1016/j.jacc.2003.10.021. [DOI] [PubMed] [Google Scholar]
- 171.Arimura T., Hayashi T., Terada H., Lee S.Y., Zhou Q., Takahashi M., Ueda K., Nouchi T., Hohda S., Shibutani M., et al. A Cypher/ZASP mutation associated with dilated cardiomyopathy alters the binding affinity to protein kinase C. J. Biol. Chem. 2004;279:6746–6752. doi: 10.1074/jbc.M311849200. [DOI] [PubMed] [Google Scholar]
- 172.Shan S., He X., He L., Wang M., Liu C. Coexistence of congenital left ventricular aneurysm and prominent left ventricular trabeculation in a patient with LDB3 mutation: A case report. J. Med. Case Rep. 2017;11:229. doi: 10.1186/s13256-017-1405-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lopez-Ayala J.M., Ortiz-Genga M., Gomez-Milanes I., Lopez-Cuenca D., Ruiz-Espejo F., Sanchez-Munoz J.J., Oliva-Sandoval M.J., Monserrat L., Gimeno J.R. A mutation in the Z-line Cypher/ZASP protein is associated with arrhythmogenic right ventricular cardiomyopathy. Clin. Genet. 2015;88:172–176. doi: 10.1111/cge.12458. [DOI] [PubMed] [Google Scholar]
- 174.Boone P.M., Yuan B., Gu S., Ma Z., Gambin T., Gonzaga-Jauregui C., Jain M., Murdock T.J., White J.J., Jhangiani S.N., et al. Hutterite-type cataract maps to chromosome 6p21.32-p21.31, cosegregates with a homozygous mutation in LEMD2, and is associated with sudden cardiac death. Mol. Genet. Genom. Med. 2016;4:77–94. doi: 10.1002/mgg3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Liu Z., Shan H., Huang J., Li N., Hou C., Pu J. A novel lamin A/C gene missense mutation (445 V > E) in immunoglobulin-like fold associated with left ventricular non-compaction. Europace. 2016;18:617–622. doi: 10.1093/europace/euv044. [DOI] [PubMed] [Google Scholar]
- 176.Qu X.K., Yuan F., Li R.G., Xu L., Jing W.F., Liu H., Xu Y.J., Zhang M., Liu X., Fang W.Y., et al. Prevalence and spectrum of LRRC10 mutations associated with idiopathic dilated cardiomyopathy. Mol. Med. Rep. 2015;12:3718–3724. doi: 10.3892/mmr.2015.3843. [DOI] [PubMed] [Google Scholar]
- 177.Luxan G., Casanova J.C., Martinez-Poveda B., Prados B., D’Amato G., MacGrogan D., Gonzalez-Rajal A., Dobarro D., Torroja C., Martinez F., et al. Mutations in the NOTCH pathway regulator MIB1 cause left ventricular noncompaction cardiomyopathy. Nat. Med. 2013;19:193–201. doi: 10.1038/nm.3046. [DOI] [PubMed] [Google Scholar]
- 178.Piccolo P., Attanasio S., Secco I., Sangermano R., Strisciuglio C., Limongelli G., Miele E., Mutarelli M., Banfi S., Nigro V., et al. MIB2 variants altering NOTCH signalling result in left ventricle hypertrabeculation/non-compaction and are associated with Menetrier-like gastropathy. Hum. Mol. Genet. 2017;26:33–43. doi: 10.1093/hmg/ddw365. [DOI] [PubMed] [Google Scholar]
- 179.Galmiche L., Serre V., Beinat M., Assouline Z., Lebre A.S., Chretien D., Nietschke P., Benes V., Boddaert N., Sidi D., et al. Exome sequencing identifies MRPL3 mutation in mitochondrial cardiomyopathy. Hum. Mutat. 2011;32:1225–1231. doi: 10.1002/humu.21562. [DOI] [PubMed] [Google Scholar]
- 180.Carroll C.J., Isohanni P., Poyhonen R., Euro L., Richter U., Brilhante V., Gotz A., Lahtinen T., Paetau A., Pihko H., et al. Whole-exome sequencing identifies a mutation in the mitochondrial ribosome protein MRPL44 to underlie mitochondrial infantile cardiomyopathy. J. Med. Genet. 2013;50:151–159. doi: 10.1136/jmedgenet-2012-101375. [DOI] [PubMed] [Google Scholar]
- 181.Distelmaier F., Haack T.B., Catarino C.B., Gallenmuller C., Rodenburg R.J., Strom T.M., Baertling F., Meitinger T., Mayatepek E., Prokisch H., et al. MRPL44 mutations cause a slowly progressive multisystem disease with childhood-onset hypertrophic cardiomyopathy. NeuroGenet. 2015;16:319–323. doi: 10.1007/s10048-015-0444-2. [DOI] [PubMed] [Google Scholar]
- 182.Watkins H., Conner D., Thierfelder L., Jarcho J.A., MacRae C., McKenna W.J., Maron B.J., Seidman J.G., Seidman C.E. Mutations in the cardiac myosin binding protein-C gene on chromosome 11 cause familial hypertrophic cardiomyopathy. Nat. Genet. 1995;11:434–437. doi: 10.1038/ng1295-434. [DOI] [PubMed] [Google Scholar]
- 183.Carrier L., Bonne G., Bahrend E., Yu B., Richard P., Niel F., Hainque B., Cruaud C., Gary F., Labeit S., et al. Organization and sequence of human cardiac myosin binding protein C gene (MYBPC3) and identification of mutations predicted to produce truncated proteins in familial hypertrophic cardiomyopathy. Circ. Res. 1997;80:427–434. doi: 10.1161/01.res.0000435859.24609.b3. [DOI] [PubMed] [Google Scholar]
- 184.Ehlermann P., Weichenhan D., Zehelein J., Steen H., Pribe R., Zeller R., Lehrke S., Zugck C., Ivandic B.T., Katus H.A. Adverse events in families with hypertrophic or dilated cardiomyopathy and mutations in the MYBPC3 gene. BMC Med. Genet. 2008;9:95. doi: 10.1186/1471-2350-9-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Dellefave L.M., Pytel P., Mewborn S., Mora B., Guris D.L., Fedson S., Waggoner D., Moskowitz I., McNally E.M. Sarcomere mutations in cardiomyopathy with left ventricular hypertrabeculation. Circ. Cardiovasc. Genet. 2009;2:442–449. doi: 10.1161/CIRCGENETICS.109.861955. [DOI] [PubMed] [Google Scholar]
- 186.Wu W., Lu C.X., Wang Y.N., Liu F., Chen W., Liu Y.T., Han Y.C., Cao J., Zhang S.Y., Zhang X. Novel phenotype-genotype correlations of restrictive cardiomyopathy with Myosin-Binding Protein C (MYBPC3) gene mutations tested by next-generation sequencing. J. Am. Heart Assoc. 2015;4:e001879. doi: 10.1161/JAHA.115.001879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Barefield D.Y., Puckelwartz M.J., Kim E.Y., Wilsbacher L.D., Vo A.H., Waters E.A., Earley J.U., Hadhazy M., Dellefave-Castillo L., Pesce L.L., et al. Experimental modeling supports a role for MyBP-HL as a novel myofilament component in arrhythmia and dilated cardiomyopathy. Circulation. 2017;136:1477–1491. doi: 10.1161/CIRCULATIONAHA.117.028585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Carniel E., Taylor M.R., Sinagra G., Di Lenarda A., Ku L., Fain P.R., Boucek M.M., Cavanaugh J., Miocic S., Slavov D., et al. α-myosin heavy chain: A sarcomeric gene associated with dilated and hypertrophic phenotypes of cardiomyopathy. Circulation. 2005;112:54–59. doi: 10.1161/CIRCULATIONAHA.104.507699. [DOI] [PubMed] [Google Scholar]
- 189.Greenway S.C., Wilson G.J., Wilson J., George K., Kantor P.F. Sudden death in an infant with angina, restrictive cardiomyopathy, and coronary artery bridging: An unusual phenotype for a beta-myosin heavy chain (MYH7) sarcomeric protein mutation. Circ. Heart Fail. 2012;5:e92–e93. doi: 10.1161/CIRCHEARTFAILURE.112.969303. [DOI] [PubMed] [Google Scholar]
- 190.Flavigny J., Richard P., Isnard R., Carrier L., Charron P., Bonne G., Forissier J.F., Desnos M., Dubourg O., Komajda M., et al. Identification of two novel mutations in the ventricular regulatory myosin light chain gene (MYL2) associated with familial and classical forms of hypertrophic cardiomyopathy. J. Mol. Med. 1998;76:208–214. doi: 10.1007/s001090050210. [DOI] [PubMed] [Google Scholar]
- 191.Caleshu C., Sakhuja R., Nussbaum R.L., Schiller N.B., Ursell P.C., Eng C., De Marco T., McGlothlin D., Burchard E.G., Rame J.E. Furthering the link between the sarcomere and primary cardiomyopathies: Restrictive cardiomyopathy associated with multiple mutations in genes previously associated with hypertrophic or dilated cardiomyopathy. Am. J. Med. Genet. Part A. 2011;155A:2229–2235. doi: 10.1002/ajmg.a.34097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Choi J.O., Yu C.W., Chun Nah J., Rang Park J., Lee B.S., Jeong Choi Y., Cho B.R., Lee S.C., Woo Park S., Kimura A., et al. Long-term outcome of 4 Korean families with hypertrophic cardiomyopathy caused by 4 different mutations. Clin. Cardiol. 2010;33:430–438. doi: 10.1002/clc.20795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Tobita T., Nomura S., Morita H., Ko T., Fujita T., Toko H., Uto K., Hagiwara N., Aburatani H., Komuro I. Identification of MYLK3 mutations in familial dilated cardiomyopathy. Sci. Rep. 2017;7:17495. doi: 10.1038/s41598-017-17769-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Arola A.M., Sanchez X., Murphy R.T., Hasle E., Li H., Elliott P.M., McKenna W.J., Towbin J.A., Bowles N.E. Mutations in PDLIM3 and MYOZ1 encoding myocyte Z line proteins are infrequently found in idiopathic dilated cardiomyopathy. Mol. Genet. Metab. 2007;90:435–440. doi: 10.1016/j.ymgme.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 195.Osio A., Tan L., Chen S.N., Lombardi R., Nagueh S.F., Shete S., Roberts R., Willerson J.T., Marian A.J. Myozenin 2 is a novel gene for human hypertrophic cardiomyopathy. Circ. Res. 2007;100:766–768. doi: 10.1161/01.RES.0000263008.66799.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Purevjav E., Arimura T., Augustin S., Huby A.C., Takagi K., Nunoda S., Kearney D.L., Taylor M.D., Terasaki F., Bos J.M., et al. Molecular basis for clinical heterogeneity in inherited cardiomyopathies due to myopalladin mutations. Hum. Mol. Genet. 2012;21:2039–2053. doi: 10.1093/hmg/dds022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Meyer T., Ruppert V., Ackermann S., Richter A., Perrot A., Sperling S.R., Posch M.G., Maisch B., Pankuweit S. Novel mutations in the sarcomeric protein myopalladin in patients with dilated cardiomyopathy. Eur. J. Hum. Genet. 2013;21:294–300. doi: 10.1038/ejhg.2012.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Huby A.C., Mendsaikhan U., Takagi K., Martherus R., Wansapura J., Gong N., Osinska H., James J.F., Kramer K., Saito K., et al. Disturbance in Z-disk mechanosensitive proteins induced by a persistent mutant myopalladin causes familial restrictive cardiomyopathy. J. Am. Coll. Cardiol. 2014;64:2765–2776. doi: 10.1016/j.jacc.2014.09.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Roh J.I., Cheong C., Sung Y.H., Lee J., Oh J., Lee B.S., Lee J.E., Gho Y.S., Kim D.K., Park C.B., et al. Perturbation of NCOA6 leads to dilated cardiomyopathy. Cell Rep. 2014;8:991–998. doi: 10.1016/j.celrep.2014.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Fassone E., Taanman J.W., Hargreaves I.P., Sebire N.J., Cleary M.A., Burch M., Rahman S. Mutations in the mitochondrial complex I assembly factor NDUFAF1 cause fatal infantile hypertrophic cardiomyopathy. J. Med. Genet. 2011;48:691–697. doi: 10.1136/jmedgenet-2011-100340. [DOI] [PubMed] [Google Scholar]
- 201.Benit P., Beugnot R., Chretien D., Giurgea I., De Lonlay-Debeney P., Issartel J.P., Corral-Debrinski M., Kerscher S., Rustin P., Rotig A., et al. Mutant NDUFV2 subunit of mitochondrial complex I causes early onset hypertrophic cardiomyopathy and encephalopathy. Hum. Mutat. 2003;21:582–586. doi: 10.1002/humu.10225. [DOI] [PubMed] [Google Scholar]
- 202.Benit P., Slama A., Cartault F., Giurgea I., Chretien D., Lebon S., Marsac C., Munnich A., Rotig A., Rustin P. Mutant NDUFS3 subunit of mitochondrial complex I causes Leigh syndrome. J. Med. Genet. 2004;41:14–17. doi: 10.1136/jmg.2003.014316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Perrot A., Tomasov P., Villard E., Faludi R., Melacini P., Lossie J., Lohmann N., Richard P., De Bortoli M., Angelini A., et al. Mutations in NEBL encoding the cardiac Z-disk protein nebulette are associated with various cardiomyopathies. Arch. Med. Sci. 2016;12:263–278. doi: 10.5114/aoms.2016.59250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Arimura T., Nakamura T., Hiroi S., Satoh M., Takahashi M., Ohbuchi N., Ueda K., Nouchi T., Yamaguchi N., Akai J., et al. Characterization of the human nebulette gene: A polymorphism in an actin-binding motif is associated with nonfamilial idiopathic dilated cardiomyopathy. Hum. Genet. 2000;107:440–451. doi: 10.1007/s004390000389. [DOI] [PubMed] [Google Scholar]
- 205.Wang H., Li Z., Wang J., Sun K., Cui Q., Song L., Zou Y., Wang X., Liu X., Hui R., et al. Mutations in NEXN, a Z-disc gene, are associated with hypertrophic cardiomyopathy. Am. J. Hum. Genet. 2010;87:687–693. doi: 10.1016/j.ajhg.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Hassel D., Dahme T., Erdmann J., Meder B., Huge A., Stoll M., Just S., Hess A., Ehlermann P., Weichenhan D., et al. Nexilin mutations destabilize cardiac Z-disks and lead to dilated cardiomyopathy. Nat. Med. 2009;15:1281–1288. doi: 10.1038/nm.2037. [DOI] [PubMed] [Google Scholar]
- 207.Yuen T., Borle K., Wenzel K., Eileen P., French V., Brodehl A., Lauzon J., Sharma P., Klaassen S., Gerull B. Novel Variants in Nexilin are Associated with Left Ventricular Noncompaction Cardiomyopathy. Circulation. 2014;130:A17287. [Google Scholar]
- 208.Xu J.H., Gu J.Y., Guo Y.H., Zhang H., Qiu X.B., Li R.G., Shi H.Y., Liu H., Yang X.X., Xu Y.J., et al. Prevalence and spectrum of NKX2-5 mutations associated with sporadic adult-onset dilated cardiomyopathy. Int. Heart J. 2017;58:521–529. doi: 10.1536/ihj.16-440. [DOI] [PubMed] [Google Scholar]
- 209.Marston S., Montgiraud C., Munster A.B., Copeland O., Choi O., Dos Remedios C., Messer A.E., Ehler E., Knoll R. OBSCN mutations associated with dilated cardiomyopathy and haploinsufficiency. PLoS ONE. 2015;10:e0138568. doi: 10.1371/journal.pone.0138568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Biswas A., Raza A., Das S., Kapoor M., Jayarajan R., Verma A., Shamsudheen K.V., Murry B., Seth S., Bhargava B., et al. Loss of function mutation in the P2X7, a ligand-gated ion channel gene associated with hypertrophic cardiomyopathy. Purinergic Signall. 2019;15:205–210. doi: 10.1007/s11302-019-09660-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ramond F., Janin A., Di Filippo S., Chanavat V., Chalabreysse L., Roux-Buisson N., Sanlaville D., Touraine R., Millat G. Homozygous PKP2 deletion associated with neonatal left ventricle noncompaction. Clin. Genet. 2017;91:126–130. doi: 10.1111/cge.12780. [DOI] [PubMed] [Google Scholar]
- 212.Gerull B., Kirchner F., Chong J.X., Tagoe J., Chandrasekharan K., Strohm O., Waggoner D., Ober C., Duff H.J. Homozygous founder mutation in desmocollin-2 (DSC2) causes arrhythmogenic cardiomyopathy in the Hutterite population. Circ. Cardiovasc. Genet. 2013;6:327–336. doi: 10.1161/CIRCGENETICS.113.000097. [DOI] [PubMed] [Google Scholar]
- 213.Haghighi K., Kolokathis F., Pater L., Lynch R.A., Asahi M., Gramolini A.O., Fan G.C., Tsiapras D., Hahn H.S., Adamopoulos S., et al. Human phospholamban null results in lethal dilated cardiomyopathy revealing a critical difference between mouse and human. J. Clin. Investig. 2003;111:869–876. doi: 10.1172/JCI17892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Schmitt J.P., Kamisago M., Asahi M., Li G.H., Ahmad F., Mende U., Kranias E.G., MacLennan D.H., Seidman J.G., Seidman C.E. Dilated cardiomyopathy and heart failure caused by a mutation in phospholamban. Science. 2003;299:1410–1413. doi: 10.1126/science.1081578. [DOI] [PubMed] [Google Scholar]
- 215.Iuso A., Wiersma M., Schuller H.J., Pode-Shakked B., Marek-Yagel D., Grigat M., Schwarzmayr T., Berutti R., Alhaddad B., Kanon B., et al. Mutations in PPCS, encoding phosphopantothenoylcysteine synthetase, cause autosomal-recessive dilated cardiomyopathy. Am. J. Hum. Genet. 2018;102:1018–1030. doi: 10.1016/j.ajhg.2018.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Long P.A., Evans J.M., Olson T.M. Diagnostic yield of whole exome sequencing in pediatric dilated cardiomyopathy. J. Cardiovasc. Dev. Dis. 2017;4:11. doi: 10.3390/jcdd4030011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Arndt A.K., Schafer S., Drenckhahn J.D., Sabeh M.K., Plovie E.R., Caliebe A., Klopocki E., Musso G., Werdich A.A., Kalwa H., et al. Fine mapping of the 1p36 deletion syndrome identifies mutation of PRDM16 as a cause of cardiomyopathy. Am. J. Hum. Genet. 2013;93:67–77. doi: 10.1016/j.ajhg.2013.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Blair E., Redwood C., Ashrafian H., Oliveira M., Broxholme J., Kerr B., Salmon A., Ostman-Smith I., Watkins H. Mutations in the γ(2) subunit of AMP-activated protein kinase cause familial hypertrophic cardiomyopathy: Evidence for the central role of energy compromise in disease pathogenesis. Hum. Mol. Genet. 2001;10:1215–1220. doi: 10.1093/hmg/10.11.1215. [DOI] [PubMed] [Google Scholar]
- 219.Vaughan C.J., Hom Y., Okin D.A., McDermott D.A., Lerman B.B., Basson C.T. Molecular genetic analysis of PRKAG2 in sporadic Wolff-Parkinson-White syndrome. J. Cardiovasc. Electrophysiol. 2003;14:263–268. doi: 10.1046/j.1540-8167.2003.02394.x. [DOI] [PubMed] [Google Scholar]
- 220.Li D., Parks S.B., Kushner J.D., Nauman D., Burgess D., Ludwigsen S., Partain J., Nixon R.R., Allen C.N., Irwin R.P., et al. Mutations of presenilin genes in dilated cardiomyopathy and heart failure. Am. J. Hum. Genet. 2006;79:1030–1039. doi: 10.1086/509900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Gianni D., Li A., Tesco G., McKay K.M., Moore J., Raygor K., Rota M., Gwathmey J.K., Dec G.W., Aretz T., et al. Protein aggregates and novel presenilin gene variants in idiopathic dilated cardiomyopathy. Circulation. 2010;121:1216–1226. doi: 10.1161/CIRCULATIONAHA.109.879510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Tartaglia M., Mehler E.L., Goldberg R., Zampino G., Brunner H.G., Kremer H., van der Burgt I., Crosby A.H., Ion A., Jeffery S., et al. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat. Genet. 2001;29:465–468. doi: 10.1038/ng772. [DOI] [PubMed] [Google Scholar]
- 223.Razzaque M.A., Nishizawa T., Komoike Y., Yagi H., Furutani M., Amo R., Kamisago M., Momma K., Katayama H., Nakagawa M., et al. Germline gain-of-function mutations in RAF1 cause Noonan syndrome. Nat. Genet. 2007;39:1013–1017. doi: 10.1038/ng2078. [DOI] [PubMed] [Google Scholar]
- 224.Pandit B., Sarkozy A., Pennacchio L.A., Carta C., Oishi K., Martinelli S., Pogna E.A., Schackwitz W., Ustaszewska A., Landstrom A., et al. Gain-of-function RAF1 mutations cause Noonan and LEOPARD syndromes with hypertrophic cardiomyopathy. Nat. Genet. 2007;39:1007–1012. doi: 10.1038/ng2073. [DOI] [PubMed] [Google Scholar]
- 225.Dhandapany P.S., Razzaque M.A., Muthusami U., Kunnoth S., Edwards J.J., Mulero-Navarro S., Riess I., Pardo S., Sheng J., Rani D.S., et al. RAF1 mutations in childhood-onset dilated cardiomyopathy. Nat. Genet. 2014;46:635–639. doi: 10.1038/ng.2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Guo W., Schafer S., Greaser M.L., Radke M.H., Liss M., Govindarajan T., Maatz H., Schulz H., Li S., Parrish A.M., et al. RBM20, a gene for hereditary cardiomyopathy, regulates titin splicing. Nat. Med. 2012;18:766–773. doi: 10.1038/nm.2693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Sedaghat-Hamedani F., Haas J., Zhu F., Geier C., Kayvanpour E., Liss M., Lai A., Frese K., Pribe-Wolferts R., Amr A., et al. Clinical genetics and outcome of left ventricular non-compaction cardiomyopathy. Eur. Heart J. 2017;38:3449–3460. doi: 10.1093/eurheartj/ehx545. [DOI] [PubMed] [Google Scholar]
- 228.Van den Hoogenhof M.M.G., Beqqali A., Amin A.S., van der Made I., Aufiero S., Khan M.A.F., Schumacher C.A., Jansweijer J.A., van Spaendonck-Zwarts K.Y., Remme C.A., et al. RBM20 mutations induce an arrhythmogenic dilated cardiomyopathy related to disturbed calcium handling. Circulation. 2018;138:1330–1342. doi: 10.1161/CIRCULATIONAHA.117.031947. [DOI] [PubMed] [Google Scholar]
- 229.Parikh V.N., Caleshu C., Reuter C., Lazzeroni L.C., Ingles J., Garcia J., McCaleb K., Adesiyun T., Sedaghat-Hamedani F., Kumar S., et al. Regional variation in RBM20 causes a highly penetrant arrhythmogenic cardiomyopathy. Circ. Heart Fail. 2019;12:e005371. doi: 10.1161/CIRCHEARTFAILURE.118.005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Long P.A., Zimmermann M.T., Kim M., Evans J.M., Xu X., Olson T.M. De novo RRAGC mutation activates mTORC1 signaling in syndromic fetal dilated cardiomyopathy. Hum. Genet. 2016;135:909–917. doi: 10.1007/s00439-016-1685-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Mann S.A., Castro M.L., Ohanian M., Guo G., Zodgekar P., Sheu A., Stockhammer K., Thompson T., Playford D., Subbiah R., et al. R222Q SCN5A mutation is associated with reversible ventricular ectopy and dilated cardiomyopathy. J. Am. Coll. Cardiol. 2012;60:1566–1573. doi: 10.1016/j.jacc.2012.05.050. [DOI] [PubMed] [Google Scholar]
- 232.Erkapic D., Neumann T., Schmitt J., Sperzel J., Berkowitsch A., Kuniss M., Hamm C.W., Pitschner H.F. Electrical storm in a patient with arrhythmogenic right ventricular cardiomyopathy and SCN5A mutation. Europace. 2008;10:884–887. doi: 10.1093/europace/eun065. [DOI] [PubMed] [Google Scholar]
- 233.Jaksch M., Ogilvie I., Yao J., Kortenhaus G., Bresser H.G., Gerbitz K.D., Shoubridge E.A. Mutations in SCO2 are associated with a distinct form of hypertrophic cardiomyopathy and cytochrome c oxidase deficiency. Hum. Mol. Genet. 2000;9:795–801. doi: 10.1093/hmg/9.5.795. [DOI] [PubMed] [Google Scholar]
- 234.Levitas A., Muhammad E., Harel G., Saada A., Caspi V.C., Manor E., Beck J.C., Sheffield V., Parvari R. Familial neonatal isolated cardiomyopathy caused by a mutation in the flavoprotein subunit of succinate dehydrogenase. Eur. J. Hum. Genet. 2010;18:1160–1165. doi: 10.1038/ejhg.2010.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Van Spaendonck-Zwarts K.Y., van Rijsingen I.A., van den Berg M.P., Lekanne Deprez R.H., Post J.G., van Mil A.M., Asselbergs F.W., Christiaans I., van Langen I.M., Wilde A.A., et al. Genetic analysis in 418 index patients with idiopathic dilated cardiomyopathy: Overview of 10 years’ experience. Eur. J. Heart Fail. 2013;15:628–636. doi: 10.1093/eurjhf/hft013. [DOI] [PubMed] [Google Scholar]
- 236.Tsubata S., Bowles K.R., Vatta M., Zintz C., Titus J., Muhonen L., Bowles N.E., Towbin J.A. Mutations in the human δ-sarcoglycan gene in familial and sporadic dilated cardiomyopathy. J. Clin. Investig. 2000;106:655–662. doi: 10.1172/JCI9224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Hoban R., Roberts A.E., Demmer L., Jethva R., Shephard B. Noonan syndrome due to a SHOC2 mutation presenting with fetal distress and fatal hypertrophic cardiomyopathy in a premature infant. Am. J. Med. Genet. Part A. 2012;158A:1411–1413. doi: 10.1002/ajmg.a.35318. [DOI] [PubMed] [Google Scholar]
- 238.Sandra M., Maria Pia L., Stefano C., Pietro P., Crociani P., Aldo R., Giuseppe D.S., Massimo C. Emery-dreifuss muscular dystrophy type 4: A new SYNE1 mutation associated with hypertrophic cardiomyopathy masked by a perinatal distress-related spastic diplegia. Clin. Case Rep. 2019;7:1078–1082. doi: 10.1002/ccr3.2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Puckelwartz M.J., Kessler E.J., Kim G., Dewitt M.M., Zhang Y., Earley J.U., Depreux F.F., Holaska J., Mewborn S.K., Pytel P., et al. Nesprin-1 mutations in human and murine cardiomyopathy. J. Mol. Cell. Cardiol. 2010;48:600–608. doi: 10.1016/j.yjmcc.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Bione S., D’Adamo P., Maestrini E., Gedeon A.K., Bolhuis P.A., Toniolo D. A novel X-linked gene, G4.5. is responsible for Barth syndrome. Nat. Genet. 1996;12:385–389. doi: 10.1038/ng0496-385. [DOI] [PubMed] [Google Scholar]
- 241.Xing Y., Ichida F., Matsuoka T., Isobe T., Ikemoto Y., Higaki T., Tsuji T., Haneda N., Kuwabara A., Chen R., et al. Genetic analysis in patients with left ventricular noncompaction and evidence for genetic heterogeneity. Mol. Genet. Metab. 2006;88:71–77. doi: 10.1016/j.ymgme.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 242.Wang C., Hata Y., Hirono K., Takasaki A., Ozawa S.W., Nakaoka H., Saito K., Miyao N., Okabe M., Ibuki K., et al. A wide and specific spectrum of genetic variants and genotype-phenotype correlations revealed by next-generation sequencing in patients with left ventricular noncompaction. J. Am. Heart Assoc. 2017;6:e006210. doi: 10.1161/JAHA.117.006210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Kirk E.P., Sunde M., Costa M.W., Rankin S.A., Wolstein O., Castro M.L., Butler T.L., Hyun C., Guo G., Otway R., et al. Mutations in cardiac T-box factor gene TBX20 are associated with diverse cardiac pathologies, including defects of septation and valvulogenesis and cardiomyopathy. Am. J. Hum. Genet. 2007;81:280–291. doi: 10.1086/519530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Zhao C.M., Bing S., Song H.M., Wang J., Xu W.J., Jiang J.F., Qiu X.B., Yuan F., Xu J.H., Yang Y.Q. TBX20 loss-of-function mutation associated with familial dilated cardiomyopathy. Clin. Chem. Lab. Med. 2016;54:325–332. doi: 10.1515/cclm-2015-0328. [DOI] [PubMed] [Google Scholar]
- 245.Hayashi T., Arimura T., Itoh-Satoh M., Ueda K., Hohda S., Inagaki N., Takahashi M., Hori H., Yasunami M., Nishi H., et al. Tcap gene mutations in hypertrophic cardiomyopathy and dilated cardiomyopathy. J. Am. Coll. Cardiol. 2004;44:2192–2201. doi: 10.1016/j.jacc.2004.08.058. [DOI] [PubMed] [Google Scholar]
- 246.Beffagna G., Occhi G., Nava A., Vitiello L., Ditadi A., Basso C., Bauce B., Carraro G., Thiene G., Towbin J.A., et al. Regulatory mutations in transforming growth factor-beta3 gene cause arrhythmogenic right ventricular cardiomyopathy type 1. Cardiovasc. Res. 2005;65:366–373. doi: 10.1016/j.cardiores.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 247.De Bortoli M., Postma A.V., Poloni G., Calore M., Minervini G., Mazzotti E., Rigato I., Ebert M., Lorenzon A., Vazza G., et al. Whole-exome sequencing identifies pathogenic variants in TJP1 gene associated with arrhythmogenic cardiomyopathy. Circ. Genom. Precis. Med. 2018;11:e002123. doi: 10.1161/CIRCGEN.118.002123. [DOI] [PubMed] [Google Scholar]
- 248.Yu H.C., Coughlin C.R., Geiger E.A., Salvador B.J., Elias E.R., Cavanaugh J.L., Chatfield K.C., Miyamoto S.D., Shaikh T.H. Discovery of a potentially deleterious variant in TMEM87B in a patient with a hemizygous 2q13 microdeletion suggests a recessive condition characterized by congenital heart disease and restrictive cardiomyopathy. Cold Spring Harb. Mol. Case Stud. 2016;2:a000844. doi: 10.1101/mcs.a000844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Mogensen J., Murphy R.T., Shaw T., Bahl A., Redwood C., Watkins H., Burke M., Elliott P.M., McKenna W.J. Severe disease expression of cardiac troponin C and T mutations in patients with idiopathic dilated cardiomyopathy. J. Am. Coll. Cardiol. 2004;44:2033–2040. doi: 10.1016/j.jacc.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 250.Ploski R., Rydzanicz M., Ksiazczyk T.M., Franaszczyk M., Pollak A., Kosinska J., Michalak E., Stawinski P., Ziolkowska L., Bilinska Z.T., et al. Evidence for troponin C (TNNC1) as a gene for autosomal recessive restrictive cardiomyopathy with fatal outcome in infancy. Am. J. Med. Genet. Part A. 2016;170:3241–3248. doi: 10.1002/ajmg.a.37860. [DOI] [PubMed] [Google Scholar]
- 251.Murphy R.T., Mogensen J., Shaw A., Kubo T., Hughes S., McKenna W.J. Novel mutation in cardiac troponin I in recessive idiopathic dilated cardiomyopathy. Lancet. 2004;363:371–372. doi: 10.1016/S0140-6736(04)15468-8. [DOI] [PubMed] [Google Scholar]
- 252.Fujino M., Tsuda E., Hirono K., Nakata M., Ichida F., Hata Y., Nishida N., Kurosaki K. The TNNI3 Arg192His mutation in a 13-year-old girl with left ventricular noncompaction. J. Cardiol. Cases. 2018;18:33–36. doi: 10.1016/j.jccase.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Fan L.L., Huang H., Jin J.Y., Li J.J., Chen Y.Q., Zhao S.P., Xiang R. Whole exome sequencing identifies a novel mutation (c.333 + 2T > C) of TNNI3K in a Chinese family with dilated cardiomyopathy and cardiac conduction disease. Gene. 2018;648:63–67. doi: 10.1016/j.gene.2018.01.055. [DOI] [PubMed] [Google Scholar]
- 254.Hanson E.L., Jakobs P.M., Keegan H., Coates K., Bousman S., Dienel N.H., Litt M., Hershberger R.E. Cardiac troponin T lysine 210 deletion in a family with dilated cardiomyopathy. J. Card. Fail. 2002;8:28–32. doi: 10.1054/jcaf.2002.31157. [DOI] [PubMed] [Google Scholar]
- 255.Luedde M., Ehlermann P., Weichenhan D., Will R., Zeller R., Rupp S., Muller A., Steen H., Ivandic B.T., Ulmer H.E., et al. Severe familial left ventricular non-compaction cardiomyopathy due to a novel troponin T (TNNT2) mutation. Cardiovasc. Res. 2010;86:452–460. doi: 10.1093/cvr/cvq009. [DOI] [PubMed] [Google Scholar]
- 256.Poloni G., Calore M., Rigato I., Marras E., Minervini G., Mazzotti E., Lorenzon A., Li Mura I.E.A., Telatin A., Zara I., et al. A targeted next-generation gene panel reveals a novel heterozygous nonsense variant in the TP63 gene in patients with arrhythmogenic cardiomyopathy. Heart Rhythm. 2019;16:773–780. doi: 10.1016/j.hrthm.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 257.Karibe A., Tobacman L.S., Strand J., Butters C., Back N., Bachinski L.L., Arai A.E., Ortiz A., Roberts R., Homsher E., et al. Hypertrophic cardiomyopathy caused by a novel α-tropomyosin mutation (V95A) is associated with mild cardiac phenotype, abnormal calcium binding to troponin, abnormal myosin cycling, and poor prognosis. Circulation. 2001;103:65–71. doi: 10.1161/01.CIR.103.1.65. [DOI] [PubMed] [Google Scholar]
- 258.Lakdawala N.K., Dellefave L., Redwood C.S., Sparks E., Cirino A.L., Depalma S., Colan S.D., Funke B., Zimmerman R.S., Robinson P., et al. Familial dilated cardiomyopathy caused by an α-tropomyosin mutation: The distinctive natural history of sarcomeric dilated cardiomyopathy. J. Am. Coll. Cardiol. 2010;55:320–329. doi: 10.1016/j.jacc.2009.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Chang B., Nishizawa T., Furutani M., Fujiki A., Tani M., Kawaguchi M., Ibuki K., Hirono K., Taneichi H., Uese K., et al. Identification of a novel TPM1 mutation in a family with left ventricular noncompaction and sudden death. Mol. Genet. Metab. 2011;102:200–206. doi: 10.1016/j.ymgme.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 260.Chen S.N., Czernuszewicz G., Tan Y., Lombardi R., Jin J., Willerson J.T., Marian A.J. Human molecular genetic and functional studies identify TRIM63, encoding muscle RING finger protein 1, as a novel gene for human hypertrophic cardiomyopathy. Circ. Res. 2012;111:907–919. doi: 10.1161/CIRCRESAHA.112.270207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Saito Y., Nakamura K., Nishi N., Igawa O., Yoshida M., Miyoshi T., Watanabe A., Morita H., Ito H. TRPM4 mutation in patients with ventricular noncompaction and cardiac conduction disease. Circ. Genom. Precis. Med. 2018;11:e002103. doi: 10.1161/CIRCGEN.118.002103. [DOI] [PubMed] [Google Scholar]
- 262.Perli E., Pisano A., Glasgow R.I.C., Carbo M., Hardy S.A., Falkous G., He L., Cerbelli B., Pignataro M.G., Zacara E., et al. Novel compound mutations in the mitochondrial translation elongation factor (TSFM) gene cause severe cardiomyopathy with myocardial fibro-adipose replacement. Sci. Rep. 2019;9:5108. doi: 10.1038/s41598-019-41483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Satoh M., Takahashi M., Sakamoto T., Hiroe M., Marumo F., Kimura A. Structural analysis of the titin gene in hypertrophic cardiomyopathy: Identification of a novel disease gene. Biochem. Biophys. Res. Commun. 1999;262:411–417. doi: 10.1006/bbrc.1999.1221. [DOI] [PubMed] [Google Scholar]
- 264.Itoh-Satoh M., Hayashi T., Nishi H., Koga Y., Arimura T., Koyanagi T., Takahashi M., Hohda S., Ueda K., Nouchi T., et al. Titin mutations as the molecular basis for dilated cardiomyopathy. Biochem. Biophys. Res. Commun. 2002;291:385–393. doi: 10.1006/bbrc.2002.6448. [DOI] [PubMed] [Google Scholar]
- 265.Li S., Zhang C., Liu N., Bai H., Hou C., Song L., Pu J. Titin-truncating variants are associated with heart failure events in patients with left ventricular noncompaction cardiomyopathy. Clin. Cardiol. 2019;42:530–535. doi: 10.1002/clc.23172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Saraiva M.J., Almeida Mdo R., Sherman W., Gawinowicz M., Costa P., Costa P.P., Goodman D.S. A new transthyretin mutation associated with amyloid cardiomyopathy. Am. J. Hum. Genet. 1992;50:1027–1030. [PMC free article] [PubMed] [Google Scholar]
- 267.Holmgren G., Hellman U., Anan I., Lundgren H.E., Jonasson J., Stafberg C., Fahoum S., Suhr O.B. Cardiomyopathy in Swedish patients with the Gly53Glu and His88Arg transthyretin variants. Amyloid. 2005;12:184–188. doi: 10.1080/13506120500223126. [DOI] [PubMed] [Google Scholar]
- 268.Sibbing D., Pfeufer A., Perisic T., Mannes A.M., Fritz-Wolf K., Unwin S., Sinner M.F., Gieger C., Gloeckner C.J., Wichmann H.E., et al. Mutations in the mitochondrial thioredoxin reductase gene TXNRD2 cause dilated cardiomyopathy. Eur. Heart J. 2011;32:1121–1133. doi: 10.1093/eurheartj/ehq507. [DOI] [PubMed] [Google Scholar]
- 269.Vasile V.C., Will M.L., Ommen S.R., Edwards W.D., Olson T.M., Ackerman M.J. Identification of a metavinculin missense mutation, R975W, associated with both hypertrophic and dilated cardiomyopathy. Mol. Genet. Metab. 2006;87:169–174. doi: 10.1016/j.ymgme.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 270.Vasile V.C., Ommen S.R., Edwards W.D., Ackerman M.J. A missense mutation in a ubiquitously expressed protein, vinculin, confers susceptibility to hypertrophic cardiomyopathy. Biochem. Biophys. Res. Commun. 2006;345:998–1003. doi: 10.1016/j.bbrc.2006.04.151. [DOI] [PubMed] [Google Scholar]
- 271.Olson T.M., Illenberger S., Kishimoto N.Y., Huttelmaier S., Keating M.T., Jockusch B.M. Metavinculin mutations alter actin interaction in dilated cardiomyopathy. Circulation. 2002;105:431–437. doi: 10.1161/hc0402.102930. [DOI] [PubMed] [Google Scholar]
- 272.Buyandelger B., Mansfield C., Kostin S., Choi O., Roberts A.M., Ware J.S., Mazzarotto F., Pesce F., Buchan R., Isaacson R.L., et al. ZBTB17 (MIZ1) is important for the cardiac stress response and a novel candidate gene for cardiomyopathy and heart failure. Circ. Cardiovasc. Genet. 2015;8:643–652. doi: 10.1161/CIRCGENETICS.113.000690. [DOI] [PubMed] [Google Scholar]
- 273.Sun Y.M., Wang J., Xu Y.J., Wang X.H., Yuan F., Liu H., Li R.G., Zhang M., Li Y.J., Shi H.Y., et al. ZBTB17 loss-of-function mutation contributes to familial dilated cardiomyopathy. Heart Vessels. 2018;33:722–732. doi: 10.1007/s00380-017-1110-4. [DOI] [PubMed] [Google Scholar]
- 274.Gurdon J.B., Elsdale T.R., Fischberg M. Sexually mature individuals of Xenopus laevis from the transplantation of single somatic nuclei. Nature. 1958;182:64–65. doi: 10.1038/182064a0. [DOI] [PubMed] [Google Scholar]
- 275.Elsdale T.R., Gurdon J.B., Fischberg M. A description of the technique for nuclear transplantation in Xenopus laevis. J. Embryol. Exp. Morphol. 1960;8:437–444. [PubMed] [Google Scholar]
- 276.Holmes D. Stem cell scientists share 2012 Nobel Prize for medicine. Lancet. 2012;380:1295. doi: 10.1016/S0140-6736(12)61743-7. [DOI] [PubMed] [Google Scholar]
- 277.Wilmut I., Schnieke A.E., McWhir J., Kind A.J., Campbell K.H. Viable offspring derived from fetal and adult mammalian cells. Nature. 1997;385:810–813. doi: 10.1038/385810a0. [DOI] [PubMed] [Google Scholar]
- 278.Takahashi K., Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 279.Okita K., Ichisaka T., Yamanaka S. Generation of germline-competent induced pluripotent stem cells. Nature. 2007;448:313–317. doi: 10.1038/nature05934. [DOI] [PubMed] [Google Scholar]
- 280.Nakagawa M., Koyanagi M., Tanabe K., Takahashi K., Ichisaka T., Aoi T., Okita K., Mochiduki Y., Takizawa N., Yamanaka S. Generation of induced pluripotent stem cells without Myc from mouse and human fibroblasts. Nat. Biotechnol. 2008;26:101–106. doi: 10.1038/nbt1374. [DOI] [PubMed] [Google Scholar]
- 281.Takahashi K., Tanabe K., Ohnuki M., Narita M., Ichisaka T., Tomoda K., Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 282.Blelloch R., Venere M., Yen J., Ramalho-Santos M. Generation of induced pluripotent stem cells in the absence of drug selection. Cell Stem Cell. 2007;1:245–247. doi: 10.1016/j.stem.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Yu J., Vodyanik M.A., Smuga-Otto K., Antosiewicz-Bourget J., Frane J.L., Tian S., Nie J., Jonsdottir G.A., Ruotti V., Stewart R., et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 284.Brambrink T., Foreman R., Welstead G.G., Lengner C.J., Wernig M., Suh H., Jaenisch R. Sequential expression of pluripotency markers during direct reprogramming of mouse somatic cells. Cell Stem Cell. 2008;2:151–159. doi: 10.1016/j.stem.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Soldner F., Hockemeyer D., Beard C., Gao Q., Bell G.W., Cook E.G., Hargus G., Blak A., Cooper O., Mitalipova M., et al. Parkinson’s disease patient-derived induced pluripotent stem cells free of viral reprogramming factors. Cell. 2009;136:964–977. doi: 10.1016/j.cell.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Hacein-Bey-Abina S., von Kalle C., Schmidt M., Le Deist F., Wulffraat N., McIntyre E., Radford I., Villeval J.L., Fraser C.C., Cavazzana-Calvo M., et al. A serious adverse event after successful gene therapy for X-linked severe combined immunodeficiency. N. Engl. J. Med. 2003;348:255–256. doi: 10.1056/NEJM200301163480314. [DOI] [PubMed] [Google Scholar]
- 287.Kaji K., Norrby K., Paca A., Mileikovsky M., Mohseni P., Woltjen K. Virus-free induction of pluripotency and subsequent excision of reprogramming factors. Nature. 2009;458:771–775. doi: 10.1038/nature07864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Zhou W., Freed C.R. Adenoviral gene delivery can reprogram human fibroblasts to induced pluripotent stem cells. Stem Cells. 2009;27:2667–2674. doi: 10.1002/stem.201. [DOI] [PubMed] [Google Scholar]
- 289.Meraviglia V., Zanon A., Lavdas A.A., Schwienbacher C., Silipigni R., Di Segni M., Chen H.S., Pramstaller P.P., Hicks A.A., Rossini A. Generation of induced pluripotent stem cells from frozen buffy coats using non-integrating episomal plasmids. J. Vis. Exp. 2015;100:e52885. doi: 10.3791/52885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Okita K., Nakagawa M., Hyenjong H., Ichisaka T., Yamanaka S. Generation of mouse induced pluripotent stem cells without viral vectors. Science. 2008;322:949–953. doi: 10.1126/science.1164270. [DOI] [PubMed] [Google Scholar]
- 291.Fusaki N., Ban H., Nishiyama A., Saeki K., Hasegawa M. Efficient induction of transgene-free human pluripotent stem cells using a vector based on Sendai virus, an RNA virus that does not integrate into the host genome. Proc. Acad. Ser. B. 2009;85:348–362. doi: 10.2183/pjab.85.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Judson R.L., Babiarz J.E., Venere M., Blelloch R. Embryonic stem cell-specific microRNAs promote induced pluripotency. Nat. Biotechnol. 2009;27:459–461. doi: 10.1038/nbt.1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Card D.A., Hebbar P.B., Li L., Trotter K.W., Komatsu Y., Mishina Y., Archer T.K. Oct4/Sox2-regulated miR-302 targets cyclin D1 in human embryonic stem cells. Mol. Cell. Biol. 2008;28:6426–6438. doi: 10.1128/MCB.00359-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Anokye-Danso F., Trivedi C.M., Juhr D., Gupta M., Cui Z., Tian Y., Zhang Y., Yang W., Gruber P.J., Epstein J.A., et al. Highly efficient miRNA-mediated reprogramming of mouse and human somatic cells to pluripotency. Cell Stem Cell. 2011;8:376–388. doi: 10.1016/j.stem.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Schlaeger T.M., Daheron L., Brickler T.R., Entwisle S., Chan K., Cianci A., DeVine A., Ettenger A., Fitzgerald K., Godfrey M., et al. A comparison of non-integrating reprogramming methods. Nat. Biotechnol. 2015;33:58–63. doi: 10.1038/nbt.3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Freberg C.T., Dahl J.A., Timoskainen S., Collas P. Epigenetic reprogramming of OCT4 and NANOG regulatory regions by embryonal carcinoma cell extract. Mol. Biol. Cell. 2007;18:1543–1553. doi: 10.1091/mbc.e07-01-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Kim D., Kim C.H., Moon J.I., Chung Y.G., Chang M.Y., Han B.S., Ko S., Yang E., Cha K.Y., Lanza R., et al. Generation of human induced pluripotent stem cells by direct delivery of reprogramming proteins. Cell Stem Cell. 2009;4:472–476. doi: 10.1016/j.stem.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Huangfu D., Maehr R., Guo W., Eijkelenboom A., Snitow M., Chen A.E., Melton D.A. Induction of pluripotent stem cells by defined factors is greatly improved by small-molecule compounds. Nat. Biotechnol. 2008;26:795–797. doi: 10.1038/nbt1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Li W., Ding S. Small molecules that modulate embryonic stem cell fate and somatic cell reprogramming. Trends Pharmacol. Sci. 2010;31:36–45. doi: 10.1016/j.tips.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 300.Bru T., Clarke C., McGrew M.J., Sang H.M., Wilmut I., Blow J.J. Rapid induction of pluripotency genes after exposure of human somatic cells to mouse ES cell extracts. Exp. Cell Res. 2008;314:2634–2642. doi: 10.1016/j.yexcr.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Konermann S., Brigham M.D., Trevino A.E., Joung J., Abudayyeh O.O., Barcena C., Hsu P.D., Habib N., Gootenberg J.S., Nishimasu H., et al. Genome-scale transcriptional activation by an engineered CRISPR-Cas9 complex. Nature. 2015;517:583–588. doi: 10.1038/nature14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Weltner J., Balboa D., Katayama S., Bespalov M., Krjutskov K., Jouhilahti E.M., Trokovic R., Kere J., Otonkoski T. Human pluripotent reprogramming with CRISPR activators. Nat. Commun. 2018;9:2643. doi: 10.1038/s41467-018-05067-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Jinek M., Chylinski K., Fonfara I., Hauer M., Doudna J.A., Charpentier E. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science. 2012;337:816–821. doi: 10.1126/science.1225829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Zetsche B., Gootenberg J.S., Abudayyeh O.O., Slaymaker I.M., Makarova K.S., Essletzbichler P., Volz S.E., Joung J., van der Oost J., Regev A., et al. Cpf1 is a single RNA-guided endonuclease of a class 2 CRISPR-Cas system. Cell. 2015;163:759–771. doi: 10.1016/j.cell.2015.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Joung J.K., Sander J.D. TALENs: A widely applicable technology for targeted genome editing. Nat. Rev. Mol. Cell Biol. 2013;14:49–55. doi: 10.1038/nrm3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Nemudryi A.A., Valetdinova K.R., Medvedev S.P., Zakian S.M. TALEN and CRISPR/Cas genome editing systems: Tools of discovery. Acta Nat. 2014;6:19–40. doi: 10.32607/20758251-2014-6-3-19-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Debus J.D., Milting H., Brodehl A., Kassner A., Anselmetti D., Gummert J., Gaertner-Rommel A. In vitro analysis of arrhythmogenic cardiomyopathy associated desmoglein-2 (DSG2) mutations reveals diverse glycosylation patterns. J. Mol. Cell. Cardiol. 2019;129:303–313. doi: 10.1016/j.yjmcc.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 308.Sharma A., Toepfer C.N., Schmid M., Garfinkel A.C., Seidman C.E. Differentiation and contractile analysis of GFP-sarcomere reporter hiPSC-cardiomyocytes. Curr. Protoc. Hum. Genet. 2018;96:21.12.1–21.12.12. doi: 10.1002/cphg.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Matsa E., Dixon J.E., Medway C., Georgiou O., Patel M.J., Morgan K., Kemp P.J., Staniforth A., Mellor I., Denning C. Allele-specific RNA interference rescues the long–QT syndrome phenotype in human-induced pluripotency stem cell cardiomyocytes. Eur. Heart J. 2014;35:1078–1087. doi: 10.1093/eurheartj/eht067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Dzilic E., Lahm H., Dressen M., Deutsch M.A., Lange R., Wu S.M., Krane M., Doppler S.A. Genome editing redefines precision medicine in the cardiovascular field. Stem Cells Int. 2018;2018:4136473. doi: 10.1155/2018/4136473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Gallagher D.N., Haber J.E. Repair of a site-specific DNA cleavage: Old-school lessons for Cas9-mediated gene editing. ACS Chem. Biol. 2018;13:397–405. doi: 10.1021/acschembio.7b00760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Wei H., Zhang X.H., Clift C., Yamaguchi N., Morad M. CRISPR/Cas9 Gene editing of RyR2 in human stem cell-derived cardiomyocytes provides a novel approach in investigating dysfunctional Ca(2+) signaling. Cell Calcium. 2018;73:104–111. doi: 10.1016/j.ceca.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Anderson D.M., Anderson K.M., Chang C.L., Makarewich C.A., Nelson B.R., McAnally J.R., Kasaragod P., Shelton J.M., Liou J., Bassel-Duby R., et al. A micropeptide encoded by a putative long noncoding RNA regulates muscle performance. Cell. 2015;160:595–606. doi: 10.1016/j.cell.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Roberts B., Hendershott M.C., Arakaki J., Gerbin K.A., Malik H., Nelson A., Gehring J., Hookway C., Ludmann S.A., Yang R., et al. Fluorescent gene tagging of transcriptionally silent genes in hiPSCs. Stem Cell Rep. 2019;12:1145–1158. doi: 10.1016/j.stemcr.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Xiang X., Li C., Chen X., Dou H., Li Y., Zhang X., Luo Y. CRISPR/Cas9-mediated gene tagging: A step-by-step protocol. Methods Mol. Biol. 2019;1961:255–269. doi: 10.1007/978-1-4939-9170-9_16. [DOI] [PubMed] [Google Scholar]
- 316.Haupt A., Grancharova T., Arakaki J., Fuqua M.A., Roberts B., Gunawardane R.N. Endogenous protein tagging in human induced pluripotent stem cells using CRISPR/Cas9. J. Vis. Exp. 2018;138:e58130. doi: 10.3791/58130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Liu M., Rehman S., Tang X., Gu K., Fan Q., Chen D., Ma W. Methodologies for Improving HDR efficiency. Front. Genet. 2018;9:691. doi: 10.3389/fgene.2018.00691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Smirnikhina S.A., Anuchina A.A., Lavrov A.V. Ways of improving precise knock-in by genome-editing technologies. Hum. Genet. 2019;138:1–19. doi: 10.1007/s00439-018-1953-5. [DOI] [PubMed] [Google Scholar]
- 319.Pawelczak K.S., Gavande N.S., VanderVere-Carozza P.S., Turchi J.J. Modulating DNA repair pathways to improve precision genome engineering. ACS Chem. Biol. 2018;13:389–396. doi: 10.1021/acschembio.7b00777. [DOI] [PubMed] [Google Scholar]
- 320.Gu B., Posfai E., Rossant J. Efficient generation of targeted large insertions by microinjection into two-cell-stage mouse embryos. Nat. Biotechnol. 2018;36:632–637. doi: 10.1038/nbt.4166. [DOI] [PubMed] [Google Scholar]
- 321.Savic N., Ringnalda F.C., Lindsay H., Berk C., Bargsten K., Li Y., Neri D., Robinson M.D., Ciaudo C., Hall J., et al. Covalent linkage of the DNA repair template to the CRISPR-Cas9 nuclease enhances homology-directed repair. eLife. 2018;7:e33761. doi: 10.7554/eLife.33761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Savic N., Ringnalda F.C., Berk C., Bargsten K., Hall J., Jinek M., Schwank G. In vitro generation of CRISPR-Cas9 complexes with covalently bound repair templates for genome editing in mammalian cells. Bio Protoc. 2019;9:e3136. doi: 10.21769/BioProtoc.3136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Komor A.C., Kim Y.B., Packer M.S., Zuris J.A., Liu D.R. Programmable editing of a target base in genomic DNA without double-stranded DNA cleavage. Nature. 2016;533:420–424. doi: 10.1038/nature17946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Zafra M.P., Schatoff E.M., Katti A., Foronda M., Breinig M., Schweitzer A.Y., Simon A., Han T., Goswami S., Montgomery E., et al. Optimized base editors enable efficient editing in cells, organoids and mice. Nat. Biotechnol. 2018;36:888–893. doi: 10.1038/nbt.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Villiger L., Grisch-Chan H.M., Lindsay H., Ringnalda F., Pogliano C.B., Allegri G., Fingerhut R., Haberle J., Matos J., Robinson M.D., et al. Treatment of a metabolic liver disease by in vivo genome base editing in adult mice. Nat. Med. 2018;24:1519–1525. doi: 10.1038/s41591-018-0209-1. [DOI] [PubMed] [Google Scholar]
- 326.Carvalho A.B., de Carvalho A.C. Heart regeneration: Past, present and future. World J. Cardiol. 2010;2:107–111. doi: 10.4330/wjc.v2.i5.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Claycomb W.C., Lanson N.A., Jr., Stallworth B.S., Egeland D.B., Delcarpio J.B., Bahinski A., Izzo N.J., Jr. HL-1 cells: A cardiac muscle cell line that contracts and retains phenotypic characteristics of the adult cardiomyocyte. Proc. Natl. Acad. Sci. USA. 1998;95:2979–2984. doi: 10.1073/pnas.95.6.2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Mazzotta S., Lynch A.T., Hoppler S. Cardiomyocyte differentiation from human embryonic stem cells. Methods Mol. Biol. 2018;1816:67–78. doi: 10.1007/978-1-4939-8597-5_5. [DOI] [PubMed] [Google Scholar]
- 329.Hatani T., Miki K., Yoshida Y. Induction of human induced pluripotent stem cells to cardiomyocytes using embryoid bodies. Methods Mol. Biol. 2018;1816:79–92. doi: 10.1007/978-1-4939-8597-5_6. [DOI] [PubMed] [Google Scholar]
- 330.Zhang J., Wilson G.F., Soerens A.G., Koonce C.H., Yu J., Palecek S.P., Thomson J.A., Kamp T.J. Functional cardiomyocytes derived from human induced pluripotent stem cells. Circ. Res. 2009;104:e30–e41. doi: 10.1161/CIRCRESAHA.108.192237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Pesl M., Acimovic I., Pribyl J., Hezova R., Vilotic A., Fauconnier J., Vrbsky J., Kruzliak P., Skladal P., Kara T., et al. Forced aggregation and defined factors allow highly uniform–sized embryoid bodies and functional cardiomyocytes from human embryonic and induced pluripotent stem cells. Heart Vessels. 2014;29:834–846. doi: 10.1007/s00380-013-0436-9. [DOI] [PubMed] [Google Scholar]
- 332.Yokoo N., Baba S., Kaichi S., Niwa A., Mima T., Doi H., Yamanaka S., Nakahata T., Heike T. The effects of cardioactive drugs on cardiomyocytes derived from human induced pluripotent stem cells. Biochem. Biophys. Res. Commun. 2009;387:482–488. doi: 10.1016/j.bbrc.2009.07.052. [DOI] [PubMed] [Google Scholar]
- 333.Zwi L., Caspi O., Arbel G., Huber I., Gepstein A., Park I.H., Gepstein L. Cardiomyocyte differentiation of human induced pluripotent stem cells. Circulation. 2009;120:1513–1523. doi: 10.1161/CIRCULATIONAHA.109.868885. [DOI] [PubMed] [Google Scholar]
- 334.Burridge P.W., Thompson S., Millrod M.A., Weinberg S., Yuan X., Peters A., Mahairaki V., Koliatsos V.E., Tung L., Zambidis E.T. A universal system for highly efficient cardiac differentiation of human induced pluripotent stem cells that eliminates interline variability. PLoS ONE. 2011;6:e18293. doi: 10.1371/journal.pone.0018293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Mummery C.L., Zhang J., Ng E.S., Elliott D.A., Elefanty A.G., Kamp T.J. Differentiation of human embryonic stem cells and induced pluripotent stem cells to cardiomyocytes: A methods overview. Circ. Res. 2012;111:344–358. doi: 10.1161/CIRCRESAHA.110.227512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Besser R.R., Ishahak M., Mayo V., Carbonero D., Claure I., Agarwal A. Engineered microenvironments for maturation of stem cell derived cardiac myocytes. Theranostics. 2018;8:124–140. doi: 10.7150/thno.19441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Tzahor E. Wnt/beta-catenin signaling and cardiogenesis: Timing does matter. Dev. Cell. 2007;13:10–13. doi: 10.1016/j.devcel.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 338.Nakajima Y., Yamagishi T., Hokari S., Nakamura H. Mechanisms involved in valvuloseptal endocardial cushion formation in early cardiogenesis: Roles of transforming growth factor (TGF)-β and bone morphogenetic protein (BMP) Anat. Rec. 2000;258:119–127. doi: 10.1002/(SICI)1097-0185(20000201)258:2<119::AID-AR1>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 339.Mably J.D., Liew C.C. Factors involved in cardiogenesis and the regulation of cardiac-specific gene expression. Circ. Res. 1996;79:4–13. doi: 10.1161/01.RES.79.1.4. [DOI] [PubMed] [Google Scholar]
- 340.Govindsamy A., Naidoo S., Cerf M.E. Cardiac development and transcription factors: Insulin signalling, insulin resistance, and intrauterine nutritional programming of cardiovascular disease. J. Nutr. Metab. 2018;2018:8547976. doi: 10.1155/2018/8547976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Yan S., Jiao K. Functions of miRNAs during mammalian heart development. Int. J. Mol. Sci. 2016;17:789. doi: 10.3390/ijms17050789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Rajala K., Pekkanen-Mattila M., Aalto-Setala K. Cardiac differentiation of pluripotent stem cells. Stem Cells Int. 2011;2011:383709. doi: 10.4061/2011/383709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Yassa M.E., Mansour I.A., Sewelam N.I., Hamza H., Gaafar T. The impact of growth factors on human induced pluripotent stem cells differentiation into cardiomyocytes. Life Sci. 2018;196:38–47. doi: 10.1016/j.lfs.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 344.Kim M.S., Horst A., Blinka S., Stamm K., Mahnke D., Schuman J., Gundry R., Tomita-Mitchell A., Lough J. Activin-A and Bmp4 levels modulate cell type specification during CHIR-induced cardiomyogenesis. PLoS ONE. 2015;10:e0118670. doi: 10.1371/journal.pone.0118670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Fonoudi H., Ansari H., Abbasalizadeh S., Larijani M.R., Kiani S., Hashemizadeh S., Zarchi A.S., Bosman A., Blue G.M., Pahlavan S., et al. A universal and robust integrated platform for the scalable production of human cardiomyocytes from pluripotent stem cells. Stem Cells Transl. Med. 2015;4:1482–1494. doi: 10.5966/sctm.2014-0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Hemmi N., Tohyama S., Nakajima K., Kanazawa H., Suzuki T., Hattori F., Seki T., Kishino Y., Hirano A., Okada M., et al. A massive suspension culture system with metabolic purification for human pluripotent stem cell-derived cardiomyocytes. Life Sci. 2014;3:1473–1483. doi: 10.5966/sctm.2014-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Burridge P.W., Holmstrom A., Wu J.C. Chemically defined culture and cardiomyocyte differentiation of human pluripotent stem cells. Curr. Protoc. Hum. Genet. 2015;87:21.3.1–21.3.15. doi: 10.1002/0471142905.hg2103s87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Zhao Y., Rafatian N., Feric N.T., Cox B.J., Aschar-Sobbi R., Wang E.Y., Aggarwal P., Zhang B., Conant G., Ronaldson-Bouchard K., et al. A platform for generation of chamber-specific cardiac tissues and disease modeling. Cell. 2019;176:913–927.e18. doi: 10.1016/j.cell.2018.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Talkhabi M., Aghdami N., Baharvand H. Human cardiomyocyte generation from pluripotent stem cells: A state-of-art. Life Sci. 2016;145:98–113. doi: 10.1016/j.lfs.2015.12.023. [DOI] [PubMed] [Google Scholar]
- 350.Fatima A., Xu G., Shao K., Papadopoulos S., Lehmann M., Arnaiz-Cot J.J., Rosa A.O., Nguemo F., Matzkies M., Dittmann S., et al. In vitro modeling of ryanodine receptor 2 dysfunction using human induced pluripotent stem cells. Cell. Physiol. Biochem. 2011;28:579–592. doi: 10.1159/000335753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Pradhapan P., Kuusela J., Viik J., Aalto-Setala K., Hyttinen J. Cardiomyocyte MEA data analysis (CardioMDA)—A novel field potential data analysis software for pluripotent stem cell derived cardiomyocytes. PLoS ONE. 2013;8:e73637. doi: 10.1371/journal.pone.0073637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Penttinen K., Siirtola H., Avalos-Salguero J., Vainio T., Juhola M., Aalto-Setala K. Novel analysis software for detecting and classifying Ca2+ transient abnormalities in stem cell-derived cardiomyocytes. PLoS ONE. 2015;10:e0135806. doi: 10.1371/journal.pone.0135806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Tsurumi F., Baba S., Yoshinaga D., Umeda K., Hirata T., Takita J., Heike T. The intracellular Ca2+ concentration is elevated in cardiomyocytes differentiated from hiPSCs derived from a Duchenne muscular dystrophy patient. PLoS ONE. 2019;14:e0213768. doi: 10.1371/journal.pone.0213768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Ahola A., Polonen R.P., Aalto-Setala K., Hyttinen J. Simultaneous measurement of contraction and calcium transients in stem cell derived cardiomyocytes. Ann. Biomed. Eng. 2018;46:148–158. doi: 10.1007/s10439-017-1933-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Hortigon-Vinagre M.P., Zamora V., Burton F.L., Green J., Gintant G.A., Smith G.L. The use of ratiometric fluorescence measurements of the voltage sensitive dye Di-4-ANEPPS to examine action potential characteristics and drug effects on human induced pluripotent stem cell-derived cardiomyocytes. Toxicol. Sci. 2016;154:320–331. doi: 10.1093/toxsci/kfw171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Wheelwright M., Win Z., Mikkila J.L., Amen K.Y., Alford P.W., Metzger J.M. Investigation of human Ipsc-derived cardiac myocyte functional maturation by single cell traction force microscopy. PLoS ONE. 2018;13:e0194909. doi: 10.1371/journal.pone.0194909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Pesl M., Pribyl J., Acimovic I., Vilotic A., Jelinkova S., Salykin A., Lacampagne A., Dvorak P., Meli A.C., Skladal P., et al. Atomic force microscopy combined with human pluripotent stem cell derived cardiomyocytes for biomechanical sensing. Biosens. Bioelectron. 2016;85:751–757. doi: 10.1016/j.bios.2016.05.073. [DOI] [PubMed] [Google Scholar]
- 358.Liu J., Sun N., Bruce M.A., Wu J.C., Butte M.J. Atomic force mechanobiology of pluripotent stem cell-derived cardiomyocytes. PLoS ONE. 2012;7:e37559. doi: 10.1371/journal.pone.0037559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Feaster T.K., Cadar A.G., Wang L., Williams C.H., Chun Y.W., Hempel J.E., Bloodworth N., Merryman W.D., Lim C.C., Wu J.C., et al. Matrigel mattress: A method for the generation of single contracting human-induced pluripotent stem cell-derived cardiomyocytes. Circ. Res. 2015;117:995–1000. doi: 10.1161/CIRCRESAHA.115.307580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Carvajal-Vergara X., Sevilla A., D’Souza S.L., Ang Y.S., Schaniel C., Lee D.F., Yang L., Kaplan A.D., Adler E.D., Rozov R., et al. Patient-specific induced pluripotent stem-cell-derived models of LEOPARD syndrome. Nature. 2010;465:808–812. doi: 10.1038/nature09005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Digilio M.C., Conti E., Sarkozy A., Mingarelli R., Dottorini T., Marino B., Pizzuti A., Dallapiccola B. Grouping of multiple-lentigines/LEOPARD and Noonan syndromes on the PTPN11 gene. Am. J. Hum. Genet. 2002;71:389–394. doi: 10.1086/341528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Ganigara M., Prabhu A., Kumar R.S. LEOPARD syndrome in an infant with severe hypertrophic cardiomyopathy and PTPN11 mutation. Ann. Pediatr. Cardiol. 2011;4:74–76. doi: 10.4103/0974-2069.79631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Limongelli G., Pacileo G., Russo M.G., Sarkozy A., Felicetti M., Di Salvo G., Morelli C., Calabro P., Paladini D., Marino B., et al. Severe, early onset hypertrophic cardiomyopathy in a family with LEOPARD syndrome. J. Prenat. Med. 2008;2:24–26. [PMC free article] [PubMed] [Google Scholar]
- 364.Molkentin J.D. Calcineurin-NFAT signaling regulates the cardiac hypertrophic response in coordination with the MAPKs. Cardiovasc. Res. 2004;63:467–475. doi: 10.1016/j.cardiores.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 365.Adamcova M., Skarkova V., Seifertova J., Rudolf E. Cardiac troponins are among targets of doxorubicin-induced cardiotoxicity in hiPCS-CMs. Int. J. Mol. Sci. 2019;20:2638. doi: 10.3390/ijms20112638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Lu Y., Bu M., Yun H. Sevoflurane prevents hypoxia/reoxygenation-induced cardiomyocyte apoptosis by inhibiting PI3KC3-mediated autophagy. Hum. Cell. 2019;32:150–159. doi: 10.1007/s13577-018-00230-4. [DOI] [PubMed] [Google Scholar]
- 367.Naftali-Shani N., Molotski N., Nevo-Caspi Y., Arad M., Kuperstein R., Amit U., Huber I., Zeltzer L.A., Levich A., Abbas H., et al. Modeling peripartum cardiomyopathy with human induced pluripotent stem cells reveals distinctive abnormal function of cardiomyocytes. Circulation. 2018;138:2721–2723. doi: 10.1161/CIRCULATIONAHA.118.035950. [DOI] [PubMed] [Google Scholar]
- 368.Graneli C., Hicks R., Brolen G., Synnergren J., Sartipy P. Diabetic cardiomyopathy modelling using induced pluripotent stem cell derived cardiomyocytes: Recent advances and emerging models. Stem Cell Rev. 2019;15:13–22. doi: 10.1007/s12015-018-9858-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Drawnel F.M., Boccardo S., Prummer M., Delobel F., Graff A., Weber M., Gerard R., Badi L., Kam-Thong T., Bu L., et al. Disease modeling and phenotypic drug screening for diabetic cardiomyopathy using human induced pluripotent stem cells. Cell Rep. 2014;9:810–821. doi: 10.1016/j.celrep.2014.09.055. [DOI] [PubMed] [Google Scholar]
- 370.Ng K.M., Lau Y.M., Dhandhania V., Cai Z.J., Lee Y.K., Lai W.H., Tse H.F., Siu C.W. Empagliflozin ammeliorates high glucose induced-cardiac dysfuntion in human iPSC-derived cardiomyocytes. Sci. Rep. 2018;8:14872. doi: 10.1038/s41598-018-33293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Pant T., Mishra M.K., Bai X., Ge Z.D., Bosnjak Z.J., Dhanasekaran A. Microarray analysis of long non-coding RNA and mRNA expression profiles in diabetic cardiomyopathy using human induced pluripotent stem cell-derived cardiomyocytes. Diabetes Vasc. Dis. Res. 2019;16:57–68. doi: 10.1177/1479164118813888. [DOI] [PubMed] [Google Scholar]
- 372.Bozzi A., Sayed N., Matsa E., Sass G., Neofytou E., Clemons K.V., Correa-Oliveira R., Stevens D.A., Wu J.C. Using human induced pluripotent stem cell-derived cardiomyocytes as a model to study Trypanosoma cruzi infection. Stem Cell Rep. 2019;12:1232–1241. doi: 10.1016/j.stemcr.2019.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Sharma A., Marceau C., Hamaguchi R., Burridge P.W., Rajarajan K., Churko J.M., Wu H., Sallam K.I., Matsa E., Sturzu A.C., et al. Human induced pluripotent stem cell-derived cardiomyocytes as an in vitro model for coxsackievirus B3-induced myocarditis and antiviral drug screening platform. Circ. Res. 2014;115:556–566. doi: 10.1161/CIRCRESAHA.115.303810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Judge L.M., Perez-Bermejo J.A., Truong A., Ribeiro A.J., Yoo J.C., Jensen C.L., Mandegar M.A., Huebsch N., Kaake R.M., So P.L., et al. A BAG3 chaperone complex maintains cardiomyocyte function during proteotoxic stress. JCI Insight. 2017;2:e94623. doi: 10.1172/jci.insight.94623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Ma N., Zhang J., Itzhaki I., Zhang S.L., Chen H., Haddad F., Kitani T., Wilson K.D., Tian L., Shrestha R., et al. Determining the pathogenicity of a genomic variant of uncertain significance using CRISPR/Cas9 and human-induced pluripotent stem cells. Circulation. 2018;138:2666–2681. doi: 10.1161/CIRCULATIONAHA.117.032273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Bezzerides V.J., Caballero A., Wang S., Ai Y., Hylind R.J., Lu F., Heims-Waldron D.A., Chambers K.D., Zhang D., Abrams D.J., et al. Gene therapy for catecholaminergic polymorphic ventricular tachycardia by inhibition of Ca(2+)/calmodulin-dependent kinase II. Circulation. 2019;140:405–419. doi: 10.1161/CIRCULATIONAHA.118.038514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Gramlich M., Pane L.S., Zhou Q., Chen Z., Murgia M., Schotterl S., Goedel A., Metzger K., Brade T., Parrotta E., et al. Antisense-mediated exon skipping: A therapeutic strategy for titin-based dilated cardiomyopathy. EMBO Mol. Med. 2015;7:562–576. doi: 10.15252/emmm.201505047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Van Heesch S., Witte F., Schneider-Lunitz V., Schulz J.F., Adami E., Faber A.B., Kirchner M., Maatz H., Blachut S., Sandmann C.L., et al. The translational landscape of the human heart. Cell. 2019;178:242–260.e29. doi: 10.1016/j.cell.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 379.Kyrychenko V., Kyrychenko S., Tiburcy M., Shelton J.M., Long C., Schneider J.W., Zimmermann W.H., Bassel-Duby R., Olson E.N. Functional correction of dystrophin actin binding domain mutations by genome editing. JCI Insight. 2017;2:e95918. doi: 10.1172/jci.insight.95918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Smith J.G.W., Owen T., Bhagwan J.R., Mosqueira D., Scott E., Mannhardt I., Patel A., Barriales-Villa R., Monserrat L., Hansen A., et al. Isogenic pairs of hiPSC-CMs with hypertrophic cardiomyopathy/LVNC-associated ACTC1 E99K mutation unveil differential functional deficits. Stem Cell Rep. 2018;11:1226–1243. doi: 10.1016/j.stemcr.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Phelan D.G., Anderson D.J., Howden S.E., Wong R.C., Hickey P.F., Pope K., Wilson G.R., Pebay A., Davis A.M., Petrou S., et al. ALPK3-deficient cardiomyocytes generated from patient-derived induced pluripotent stem cells and mutant human embryonic stem cells display abnormal calcium handling and establish that ALPK3 deficiency underlies familial cardiomyopathy. Eur. Heart J. 2016;37:2586–2590. doi: 10.1093/eurheartj/ehw160. [DOI] [PubMed] [Google Scholar]
- 382.Josowitz R., Mulero-Navarro S., Rodriguez N.A., Falce C., Cohen N., Ullian E.M., Weiss L.A., Rauen K.A., Sobie E.A., Gelb B.D. Autonomous and Non-autonomous defects underlie hypertrophic cardiomyopathy in BRAF-mutant hiPSC-derived cardiomyocytes. Stem Cell Rep. 2016;7:355–369. doi: 10.1016/j.stemcr.2016.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Meraviglia V., Benzoni P., Landi S., Murano C., Langione M., Motta B.M., Baratto S., Silipigni R., Di Segni M., Pramstaller P.P., et al. Generation of human induced pluripotent stem cells (EURACi001-A, EURACi002-A, EURACi003-A) from peripheral blood mononuclear cells of three patients carrying mutations in the CAV3 gene. Stem Cell Res. 2018;27:25–29. doi: 10.1016/j.scr.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 384.Mitzelfelt K.A., Limphong P., Choi M.J., Kondrat F.D., Lai S., Kolander K.D., Kwok W.M., Dai Q., Grzybowski M.N., Zhang H., et al. The human 343delT HSPB5 chaperone associated with early-onset skeletal myopathy causes defects in protein solubility. J. Biol. Chem. 2016;291:14939–14953. doi: 10.1074/jbc.M116.730481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Fatima A., Dittmann S., Kaifeng S., Linke M., Zechner U., Hennies H.C., Stork I., Rosenkranz S., Farr M., Milting H., et al. Derivation of induced pluripotent stem (iPS) cells from a patient with an arrhythmogenic right ventricular cardiomyopathy (ARVC) J. Stem Cells Regen. Med. 2010;6:97. [PubMed] [Google Scholar]
- 386.Khudiakov A., Kostina D., Zlotina A., Nikulina T., Sergushichev A., Gudkova A., Tomilin A., Malashicheva A., Kostareva A. Generation of iPSC line from desmin-related cardiomyopathy patient carrying splice site mutation of DES gene. Stem Cell Res. 2017;24:77–80. doi: 10.1016/j.scr.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 387.Tse H.F., Ho J.C., Choi S.W., Lee Y.K., Butler A.W., Ng K.M., Siu C.W., Simpson M.A., Lai W.H., Chan Y.C., et al. Patient-specific induced-pluripotent stem cells-derived cardiomyocytes recapitulate the pathogenic phenotypes of dilated cardiomyopathy due to a novel DES mutation identified by whole exome sequencing. Hum. Mol. Genet. 2013;22:1395–1403. doi: 10.1093/hmg/dds556. [DOI] [PubMed] [Google Scholar]
- 388.Eisen B., Ben Jehuda R., Cuttitta A.J., Mekies L.N., Shemer Y., Baskin P., Reiter I., Willi L., Freimark D., Gherghiceanu M., et al. Electrophysiological abnormalities in induced pluripotent stem cell-derived cardiomyocytes generated from Duchenne muscular dystrophy patients. J. Cell. Mol. Med. 2019;23:2125–2135. doi: 10.1111/jcmm.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Pioner J.M., Guan X., Klaiman J.M., Racca A.W., Pabon L., Muskheli V., Macadangdang J., Ferrantini C., Hoopmann M.R., Moritz R.L., et al. Absence of full-length dystrophin impairs normal maturation and contraction of cardiomyocytes derived from human induced pluripotent stem cells. Cardiovasc. Res. 2019 doi: 10.1093/cvr/cvz109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Guan X., Mack D.L., Moreno C.M., Strande J.L., Mathieu J., Shi Y., Markert C.D., Wang Z., Liu G., Lawlor M.W., et al. Dystrophin-deficient cardiomyocytes derived from human urine: New biologic reagents for drug discovery. Stem Cell Res. 2014;12:467–480. doi: 10.1016/j.scr.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.El-Battrawy I., Zhao Z., Lan H., Cyganek L., Tombers C., Li X., Buljubasic F., Lang S., Tiburcy M., Zimmermann W.H., et al. Electrical dysfunctions in human-induced pluripotent stem cell-derived cardiomyocytes from a patient with an arrhythmogenic right ventricular cardiomyopathy. Europace. 2018;20:f46–f56. doi: 10.1093/europace/euy042. [DOI] [PubMed] [Google Scholar]
- 392.Ng R., Manring H.R., Papoutsidakis N., Albertelli T., Tsai N., See C., Li X., Park J., Stevens T.L., Bobbili P.J., et al. Patient mutations linked to arrhythmogenic cardiomyopathy enhance calpain-mediated desmoplakin degradation. JCI Insight. 2019;4:e128643. doi: 10.1172/jci.insight.128643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Klein S., Dvornik J.L., Yarrabothula A.R., Schaniel C. A Marfan syndrome human induced pluripotent stem cell line with a heterozygous FBN1 c.4082G > A mutation, ISMMSi002-B, for disease modeling. Stem Cell Res. 2017;23:73–76. doi: 10.1016/j.scr.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 394.El-Battrawy I., Zhao Z., Lan H., Li X., Yucel G., Lang S., Sattler K., Schunemann J.D., Zimmermann W.H., Cyganek L., et al. Ion channel dysfunctions in dilated cardiomyopathy in limb-girdle muscular dystrophy. Circ. Genom. Precis. Med. 2018;11:e001893. doi: 10.1161/CIRCGEN.117.001893. [DOI] [PubMed] [Google Scholar]
- 395.Lee Y.K., Ho P.W., Schick R., Lau Y.M., Lai W.H., Zhou T., Li Y., Ng K.M., Ho S.L., Esteban M.A., et al. Modeling of Friedreich ataxia-related iron overloading cardiomyopathy using patient-specific-induced pluripotent stem cells. Pflugers Arch. Eur. J. Physiol. 2014;466:1831–1844. doi: 10.1007/s00424-013-1414-x. [DOI] [PubMed] [Google Scholar]
- 396.Hick A., Wattenhofer-Donze M., Chintawar S., Tropel P., Simard J.P., Vaucamps N., Gall D., Lambot L., Andre C., Reutenauer L., et al. Neurons and cardiomyocytes derived from induced pluripotent stem cells as a model for mitochondrial defects in Friedreich’s ataxia. Dis. Models Mech. 2013;6:608–621. doi: 10.1242/dmm.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Chien Y., Chou S.J., Chang Y.L., Leu H.B., Yang Y.P., Tsai P.H., Lai Y.H., Chen K.H., Chang W.C., Sung S.H., et al. Inhibition of arachidonate 12/15-lipoxygenase improves α-galactosidase efficacy in iPSC-derived cardiomyocytes from fabry patients. Int. J. Mol. Sci. 2018;19:1480. doi: 10.3390/ijms19051480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Chou S.J., Yu W.C., Chang Y.L., Chen W.Y., Chang W.C., Chien Y., Yen J.C., Liu Y.Y., Chen S.J., Wang C.Y., et al. Energy utilization of induced pluripotent stem cell–derived cardiomyocyte in Fabry disease. Int. J. Cardiol. 2017;232:255–263. doi: 10.1016/j.ijcard.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 399.Yoshida S., Nakanishi C., Okada H., Mori M., Yokawa J., Yoshimuta T., Ohta K., Konno T., Fujino N., Kawashiri M.A., et al. Characteristics of induced pluripotent stem cells from clinically divergent female monozygotic twins with Danon disease. J. Mol. Cell. Cardiol. 2018;114:234–242. doi: 10.1016/j.yjmcc.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 400.Hashem S.I., Murphy A.N., Divakaruni A.S., Klos M.L., Nelson B.C., Gault E.C., Rowland T.J., Perry C.N., Gu Y., Dalton N.D., et al. Impaired mitophagy facilitates mitochondrial damage in Danon disease. J. Mol. Cell. Cardiol. 2017;108:86–94. doi: 10.1016/j.yjmcc.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 401.Chi C., Leonard A., Knight W.E., Beussman K.M., Zhao Y., Cao Y., Londono P., Aune E., Trembley M.A., Small E.M., et al. LAMP-2B regulates human cardiomyocyte function by mediating autophagosome-lysosome fusion. Proc. Natl. Acad. Sci. USA. 2019;116:556–565. doi: 10.1073/pnas.1808618116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Shah D., Virtanen L., Prajapati C., Kiamehr M., Gullmets J., West G., Kreutzer J., Pekkanen-Mattila M., Helio T., Kallio P., et al. Modeling of LMNA-related dilated cardiomyopathy using human induced pluripotent stem cells. Cells. 2019;8:594. doi: 10.3390/cells8060594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Ho J.C., Zhou T., Lai W.H., Huang Y., Chan Y.C., Li X., Wong N.L., Li Y., Au K.W., Guo D., et al. Generation of induced pluripotent stem cell lines from 3 distinct laminopathies bearing heterogeneous mutations in lamin A/C. Aging. 2011;3:380–390. doi: 10.18632/aging.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Siu C.W., Lee Y.K., Ho J.C., Lai W.H., Chan Y.C., Ng K.M., Wong L.Y., Au K.W., Lau Y.M., Zhang J., et al. Modeling of lamin A/C mutation premature cardiac aging using patient-specific induced pluripotent stem cells. Aging. 2012;4:803–822. doi: 10.18632/aging.100503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Lee Y.K., Lau Y.M., Cai Z.J., Lai W.H., Wong L.Y., Tse H.F., Ng K.M., Siu C.W. Modeling treatment response for lamin A/C related dilated cardiomyopathy in human induced pluripotent stem cells. J. Am. Heart Assoc. 2017;6:e005677. doi: 10.1161/JAHA.117.005677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Salvarani N., Crasto S., Miragoli M., Bertero A., Paulis M., Kunderfranco P., Serio S., Forni A., Lucarelli C., Dal Ferro M., et al. The K219T-Lamin mutation induces conduction defects through epigenetic inhibition of SCN5A in human cardiac laminopathy. Nat. Commun. 2019;10:2267. doi: 10.1038/s41467-019-09929-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Li S., Pan H., Tan C., Sun Y., Song Y., Zhang X., Yang W., Wang X., Li D., Dai Y., et al. Mitochondrial dysfunctions contribute to hypertrophic cardiomyopathy in patient iPSC-derived cardiomyocytes with MT-RNR2 mutation. Stem Cell Rep. 2018;10:808–821. doi: 10.1016/j.stemcr.2018.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Wu H., Yang H., Rhee J.W., Zhang J.Z., Lam C.K., Sallam K., Chang A.C.Y., Ma N., Lee J., Zhang H., et al. Modelling diastolic dysfunction in induced pluripotent stem cell-derived cardiomyocytes from hypertrophic cardiomyopathy patients. Eur. Heart J. 2019 doi: 10.1093/eurheartj/ehz326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Dementyeva E.V., Medvedev S.P., Kovalenko V.R., Vyatkin Y.V., Kretov E.I., Slotvitsky M.M., Shtokalo D.N., Pokushalov E.A., Zakian S.M. Applying patient-specific induced pluripotent stem cells to create a model of hypertrophic cardiomyopathy. Biochemistry (Mosc) 2019;84:291–298. doi: 10.1134/S0006297919030118. [DOI] [PubMed] [Google Scholar]
- 410.Dambrot C., Braam S.R., Tertoolen L.G., Birket M., Atsma D.E., Mummery C.L. Serum supplemented culture medium masks hypertrophic phenotypes in human pluripotent stem cell derived cardiomyocytes. J. Cell. Mol. Med. 2014;18:1509–1518. doi: 10.1111/jcmm.12356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Birket M.J., Ribeiro M.C., Kosmidis G., Ward D., Leitoguinho A.R., van de Pol V., Dambrot C., Devalla H.D., Davis R.P., Mastroberardino P.G., et al. Contractile defect caused by mutation in MYBPC3 revealed under conditions optimized for human PSC-cardiomyocyte function. Cell Rep. 2015;13:733–745. doi: 10.1016/j.celrep.2015.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Holliday M., Ross S.B., Lim S., Semsarian C. Generation of an induced pluripotent stem cell line from a hypertrophic cardiomyopathy patient with a pathogenic myosin binding protein C (MYBPC3) p.Arg502Trp mutation. Stem Cell Res. 2018;33:56–59. doi: 10.1016/j.scr.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 413.Cohn R., Thakar K., Lowe A., Ladha F.A., Pettinato A.M., Romano R., Meredith E., Chen Y.S., Atamanuk K., Huey B.D., et al. A contraction stress model of hypertrophic cardiomyopathy due to sarcomere mutations. Stem Cell Rep. 2019;12:71–83. doi: 10.1016/j.stemcr.2018.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Davis J., Davis L.C., Correll R.N., Makarewich C.A., Schwanekamp J.A., Moussavi-Harami F., Wang D., York A.J., Wu H., Houser S.R., et al. A tension-based model distinguishes hypertrophic versus dilated cardiomyopathy. Cell. 2016;165:1147–1159. doi: 10.1016/j.cell.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Seeger T., Shrestha R., Lam C.K., Chen C., McKeithan W.L., Lau E., Wnorowski A., McMullen G., Greenhaw M., Lee J., et al. A premature termination codon mutation in MYBPC3 causes hypertrophic cardiomyopathy via chronic activation of nonsense-mediated decay. Circulation. 2019;139:799–811. doi: 10.1161/CIRCULATIONAHA.118.034624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Tanaka A., Yuasa S., Mearini G., Egashira T., Seki T., Kodaira M., Kusumoto D., Kuroda Y., Okata S., Suzuki T., et al. Endothelin-1 induces myofibrillar disarray and contractile vector variability in hypertrophic cardiomyopathy-induced pluripotent stem cell-derived cardiomyocytes. J. Am. Heart Assoc. 2014;3:e001263. doi: 10.1161/JAHA.114.001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Ojala M., Prajapati C., Polonen R.P., Rajala K., Pekkanen-Mattila M., Rasku J., Larsson K., Aalto-Setala K. Mutation-specific phenotypes in hiPSC-derived cardiomyocytes carrying either myosin-binding protein C or α-tropomyosin mutation for hypertrophic cardiomyopathy. Stem Cells Int. 2016;2016:1684792. doi: 10.1155/2016/1684792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Prajapati C., Ojala M., Aalto-Setala K. Divergent effects of adrenaline in human induced pluripotent stem cell-derived cardiomyocytes obtained from hypertrophic cardiomyopathy. Dis. Models Mech. 2018;11:dmm032896. doi: 10.1242/dmm.032896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Prondzynski M., Kramer E., Laufer S.D., Shibamiya A., Pless O., Flenner F., Muller O.J., Munch J., Redwood C., Hansen A., et al. Evaluation of MYBPC3 trans-splicing and gene replacement as therapeutic options in human iPSC-derived cardiomyocytes. Mol. Ther. Nucleic Acids. 2017;7:475–486. doi: 10.1016/j.omtn.2017.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Viswanathan S.K., Puckelwartz M.J., Mehta A., Ramachandra C.J.A., Jagadeesan A., Fritsche-Danielson R., Bhat R.V., Wong P., Kandoi S., Schwanekamp J.A., et al. Association of cardiomyopathy with MYBPC3 D389V and MYBPC3Delta25bpIntronic deletion in South Asian descendants. JAMA Cardiol. 2018;3:481–488. doi: 10.1001/jamacardio.2018.0618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Mosqueira D., Mannhardt I., Bhagwan J.R., Lis-Slimak K., Katili P., Scott E., Hassan M., Prondzynski M., Harmer S.C., Tinker A., et al. CRISPR/Cas9 editing in human pluripotent stem cell-cardiomyocytes highlights arrhythmias, hypocontractility, and energy depletion as potential therapeutic targets for hypertrophic cardiomyopathy. Eur. Heart J. 2018;39:3879–3892. doi: 10.1093/eurheartj/ehy249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Ross S.B., Fraser S.T., Nowak N., Semsarian C. Generation of induced pluripotent stem cells (iPSCs) from a hypertrophic cardiomyopathy patient with the pathogenic variant p.Val698Ala in β-myosin heavy chain (MYH7) gene. Stem Cell Res. 2017;20:88–90. doi: 10.1016/j.scr.2017.02.015. [DOI] [PubMed] [Google Scholar]
- 423.Yang K.C., Breitbart A., De Lange W.J., Hofsteen P., Futakuchi-Tsuchida A., Xu J., Schopf C., Razumova M.V., Jiao A., Boucek R., et al. Novel adult-onset systolic cardiomyopathy due to MYH7 E848G mutation in patient-derived induced pluripotent stem cells. JACC Basic Transl. Sci. 2018;3:728–740. doi: 10.1016/j.jacbts.2018.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Pioner J.M., Racca A.W., Klaiman J.M., Yang K.C., Guan X., Pabon L., Muskheli V., Zaunbrecher R., Macadangdang J., Jeong M.Y., et al. Isolation and mechanical measurements of myofibrils from human induced pluripotent stem cell-derived cardiomyocytes. Stem Cell Rep. 2016;6:885–896. doi: 10.1016/j.stemcr.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Holliday M., Ross S.B., Lim S., Mangala M., Hill A., Szappanos H.C., Hool L., Semsarian C. Development of induced pluripotent stem cells from a patient with hypertrophic cardiomyopathy who carries the pathogenic myosin heavy chain 7 mutation p.Arg403Gln. Stem Cell Res. 2018;33:269–273. doi: 10.1016/j.scr.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 426.Lan F., Lee A.S., Liang P., Sanchez-Freire V., Nguyen P.K., Wang L., Han L., Yen M., Wang Y., Sun N., et al. Abnormal calcium handling properties underlie familial hypertrophic cardiomyopathy pathology in patient-specific induced pluripotent stem cells. Cell Stem Cell. 2013;12:101–113. doi: 10.1016/j.stem.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Han L., Li Y., Tchao J., Kaplan A.D., Lin B., Li Y., Mich-Basso J., Lis A., Hassan N., London B., et al. Study familial hypertrophic cardiomyopathy using patient-specific induced pluripotent stem cells. Cardiovasc. Res. 2014;104:258–269. doi: 10.1093/cvr/cvu205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Zhou W., Bos J.M., Ye D., Tester D.J., Hrstka S., Maleszewski J.J., Ommen S.R., Nishimura R.A., Schaff H.V., Kim C.S., et al. Induced pluripotent stem cell-derived cardiomyocytes from a patient with MYL2-R58Q-mediated apical hypertrophic cardiomyopathy show hypertrophy, myofibrillar disarray, and calcium perturbations. J. Cardiovasc. Transl. Res. 2019:1–10. doi: 10.1007/s12265-019-09873-6. [DOI] [PubMed] [Google Scholar]
- 429.Ma D., Wei H., Lu J., Ho S., Zhang G., Sun X., Oh Y., Tan S.H., Ng M.L., Shim W., et al. Generation of patient-specific induced pluripotent stem cell-derived cardiomyocytes as a cellular model of arrhythmogenic right ventricular cardiomyopathy. 15Eur. Heart J. 2013;34:1122–1133. doi: 10.1093/eurheartj/ehs226. [DOI] [PubMed] [Google Scholar]
- 430.Kim C., Wong J., Wen J., Wang S., Wang C., Spiering S., Kan N.G., Forcales S., Puri P.L., Leone T.C., et al. Studying arrhythmogenic right ventricular dysplasia with patient-specific iPSCs. Nature. 2013;494:105–110. doi: 10.1038/nature11799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Martewicz S., Luni C., Serena E., Pavan P., Chen H.V., Rampazzo A., Elvassore N. Transcriptomic characterization of a human in vitro model of arrhythmogenic cardiomyopathy under topological and mechanical stimuli. Ann. Biomed. Eng. 2019;47:852–865. doi: 10.1007/s10439-018-02134-8. [DOI] [PubMed] [Google Scholar]
- 432.Akdis D., Saguner A.M., Shah K., Wei C., Medeiros-Domingo A., von Eckardstein A., Luscher T.F., Brunckhorst C., Chen H.S.V., Duru F. Sex hormones affect outcome in arrhythmogenic right ventricular cardiomyopathy/dysplasia: From a stem cell derived cardiomyocyte-based model to clinical biomarkers of disease outcome. Eur. Heart J. 2017;38:1498–1508. doi: 10.1093/eurheartj/ehx011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Caspi O., Huber I., Gepstein A., Arbel G., Maizels L., Boulos M., Gepstein L. Modeling of arrhythmogenic right ventricular cardiomyopathy with human induced pluripotent stem cells. Circ. Cardiovasc. Genet. 2013;6:557–568. doi: 10.1161/CIRCGENETICS.113.000188. [DOI] [PubMed] [Google Scholar]
- 434.Khudiakov A., Kostina D., Zlotina A., Yany N., Sergushichev A., Pervunina T., Tomilin A., Kostareva A., Malashicheva A. Generation of iPSC line from patient with arrhythmogenic right ventricular cardiomyopathy carrying mutations in PKP2 gene. Stem Cell Res. 2017;24:85–88. doi: 10.1016/j.scr.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 435.Ermon B., Volpato C.B., Cattelan G., Silipigni R., Di Segni M., Cantaloni C., Casella M., Pramstaller P.P., Pompilio G., Sommariva E., et al. Derivation of human induced pluripotent stem cell line EURACi004-A from skin fibroblasts of a patient with arrhythmogenic cardiomyopathy carrying the heterozygous PKP2 mutation c.2569_3018del50. Stem Cell Res. 2018;32:78–82. doi: 10.1016/j.scr.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Ceholski D.K., Turnbull I.C., Kong C.W., Koplev S., Mayourian J., Gorski P.A., Stillitano F., Skodras A.A., Nonnenmacher M., Cohen N., et al. Functional and transcriptomic insights into pathogenesis of R9C phospholamban mutation using human induced pluripotent stem cell-derived cardiomyocytes. J. Mol. Cell. Cardiol. 2018;119:147–154. doi: 10.1016/j.yjmcc.2018.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Karakikes I., Stillitano F., Nonnenmacher M., Tzimas C., Sanoudou D., Termglinchan V., Kong C.W., Rushing S., Hansen J., Ceholski D., et al. Correction of human phospholamban R14del mutation associated with cardiomyopathy using targeted nucleases and combination therapy. Nat. Commun. 2015;6:6955. doi: 10.1038/ncomms7955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Stillitano F., Turnbull I.C., Karakikes I., Nonnenmacher M., Backeris P., Hulot J.S., Kranias E.G., Hajjar R.J., Costa K.D. Genomic correction of familial cardiomyopathy in human engineered cardiac tissues. Eur. Heart J. 2016;37:3282–3284. doi: 10.1093/eurheartj/ehw307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Ben Jehuda R., Eisen B., Shemer Y., Mekies L.N., Szantai A., Reiter I., Cui H., Guan K., Haron-Khun S., Freimark D., et al. CRISPR correction of the PRKAG2 gene mutation in the patient’s induced pluripotent stem cell-derived cardiomyocytes eliminates electrophysiological and structural abnormalities. Heart Rhythm. 2018;15:267–276. doi: 10.1016/j.hrthm.2017.09.024. [DOI] [PubMed] [Google Scholar]
- 440.Hinson J.T., Chopra A., Lowe A., Sheng C.C., Gupta R.M., Kuppusamy R., O’Sullivan J., Rowe G., Wakimoto H., Gorham J., et al. Integrative analysis of PRKAG2 cardiomyopathy iPS and microtissue models identifies AMPK as a regulator of metabolism, survival, and fibrosis. Cell Rep. 2017;19:2410. doi: 10.1016/j.celrep.2017.05.038. [DOI] [PubMed] [Google Scholar]
- 441.Li R., Baskfield A., Lin Y., Beers J., Zou J., Liu C., Jaffre F., Roberts A.E., Ottinger E.A., Kontaridis M.I., et al. Generation of an induced pluripotent stem cell line (TRNDi003-A) from a Noonan syndrome with multiple lentigines (NSML) patient carrying a p.Q510P mutation in the PTPN11 gene. Stem Cell Res. 2019;34:101374. doi: 10.1016/j.scr.2018.101374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Jaffre F., Miller C.L., Schanzer A., Evans T., Roberts A.E., Hahn A., Kontaridis M.I. iPSC-derived cardiomyocytes reveal aberrant ERK5 and MEK1/2 signaling concomitantly promote hypertrophic cardiomyopathy in RAF1-associated noonan syndrome. Circulation. 2019;140:207–224. doi: 10.1161/CIRCULATIONAHA.118.037227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Streckfuss-Bomeke K., Tiburcy M., Fomin A., Luo X., Li W., Fischer C., Ozcelik C., Perrot A., Sossalla S., Haas J., et al. Severe DCM phenotype of patient harboring RBM20 mutation S635A can be modeled by patient-specific induced pluripotent stem cell-derived cardiomyocytes. J. Mol. Cell. Cardiol. 2017;113:9–21. doi: 10.1016/j.yjmcc.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 444.Wyles S.P., Li X., Hrstka S.C., Reyes S., Oommen S., Beraldi R., Edwards J., Terzic A., Olson T.M., Nelson T.J. Modeling structural and functional deficiencies of RBM20 familial dilated cardiomyopathy using human induced pluripotent stem cells. Hum. Mol. Genet. 2016;25:254–265. doi: 10.1093/hmg/ddv468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Wyles S.P., Hrstka S.C., Reyes S., Terzic A., Olson T.M., Nelson T.J. Pharmacological modulation of calcium homeostasis in familial dilated cardiomyopathy: An in vitro analysis from an RBM20 patient-derived iPSC model. Clin. Transl. Sci. 2016;9:158–167. doi: 10.1111/cts.12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Te Riele A.S., Agullo-Pascual E., James C.A., Leo–Macias A., Cerrone M., Zhang M., Lin X., Lin B., Sobreira N.L., Amat-Alarcon N., et al. Multilevel analyses of SCN5A mutations in arrhythmogenic right ventricular dysplasia/cardiomyopathy suggest non-canonical mechanisms for disease pathogenesis. Cardiovasc. Res. 2017;113:102–111. doi: 10.1093/cvr/cvw234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Moreau A., Gosselin-Badaroudine P., Mercier A., Burger B., Keller D.I., Chahine M. A leaky voltage sensor domain of cardiac sodium channels causes arrhythmias associated with dilated cardiomyopathy. Sci. Rep. 2018;8:13804. doi: 10.1038/s41598-018-31772-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Hallas T., Eisen B., Shemer Y., Ben Jehuda R., Mekies L.N., Naor S., Schick R., Eliyahu S., Reiter I., Vlodavsky E., et al. Investigating the cardiac pathology of SCO2-mediated hypertrophic cardiomyopathy using patients induced pluripotent stem cell-derived cardiomyocytes. J. Cell. Mol. Med. 2018;22:913–925. doi: 10.1111/jcmm.13392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Wang G., McCain M.L., Yang L., He A., Pasqualini F.S., Agarwal A., Yuan H., Jiang D., Zhang D., Zangi L., et al. Modeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologies. Nat. Med. 2014;20:616–623. doi: 10.1038/nm.3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Kodo K., Ong S.G., Jahanbani F., Termglinchan V., Hirono K., InanlooRahatloo K., Ebert A.D., Shukla P., Abilez O.J., Churko J.M., et al. iPSC-derived cardiomyocytes reveal abnormal TGF-β signalling in left ventricular non-compaction cardiomyopathy. Nat. Cell Biol. 2016;18:1031–1042. doi: 10.1038/ncb3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Sun N., Yazawa M., Liu J., Han L., Sanchez-Freire V., Abilez O.J., Navarrete E.G., Hu S., Wang L., Lee A., et al. Patient-specific induced pluripotent stem cells as a model for familial dilated cardiomyopathy. Sci. Transl. Med. 2012;4:130ra47. doi: 10.1126/scitranslmed.3003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Wu H., Lee J., Vincent L.G., Wang Q., Gu M., Lan F., Churko J.M., Sallam K.I., Matsa E., Sharma A., et al. Epigenetic regulation of phosphodiesterases 2A and 3A underlies compromised β-adrenergic signaling in an iPSC model of dilated cardiomyopathy. Cell Stem Cell. 2015;17:89–100. doi: 10.1016/j.stem.2015.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Karakikes I., Termglinchan V., Cepeda D.A., Lee J., Diecke S., Hendel A., Itzhaki I., Ameen M., Shrestha R., Wu H., et al. A comprehensive TALEN-based knockout library for generating human-induced pluripotent stem cell-based models for cardiovascular diseases. Circ. Res. 2017;120:1561–1571. doi: 10.1161/CIRCRESAHA.116.309948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Broughton K.M., Li J., Sarmah E., Warren C.M., Lin Y.H., Henze M.P., Sanchez-Freire V., Solaro R.J., Russell B. A myosin activator improves actin assembly and sarcomere function of human-induced pluripotent stem cell-derived cardiomyocytes with a troponin T point mutation. Am. J. Physiol. Heart Circ. Physiol. 2016;311:H107–H117. doi: 10.1152/ajpheart.00162.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Wang L., Kryshtal D.O., Kim K., Parikh S., Cadar A.G., Bersell K.R., He H., Pinto J.R., Knollmann B.C. Myofilament calcium-buffering dependent action potential triangulation in human-induced pluripotent stem cell model of hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2017;70:2600–2602. doi: 10.1016/j.jacc.2017.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Wang L., Kim K., Parikh S., Cadar A.G., Bersell K.R., He H., Pinto J.R., Kryshtal D.O., Knollmann B.C. Hypertrophic cardiomyopathy-linked mutation in troponin T causes myofibrillar disarray and pro-arrhythmic action potential changes in human iPSC cardiomyocytes. J. Mol. Cell. Cardiol. 2018;114:320–327. doi: 10.1016/j.yjmcc.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Hinson J.T., Chopra A., Nafissi N., Polacheck W.J., Benson C.C., Swist S., Gorham J., Yang L., Schafer S., Sheng C.C., et al. Titin mutations in iPS cells define sarcomere insufficiency as a cause of dilated cardiomyopathy. Science. 2015;349:982–986. doi: 10.1126/science.aaa5458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Schick R., Mekies L.N., Shemer Y., Eisen B., Hallas T., Ben Jehuda R., Ben-Ari M., Szantai A., Willi L., Shulman R., et al. Functional abnormalities in induced pluripotent stem cell-derived cardiomyocytes generated from titin-mutated patients with dilated cardiomyopathy. PLoS ONE. 2018;13:e0205719. doi: 10.1371/journal.pone.0205719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Leung A., Nah S.K., Reid W., Ebata A., Koch C.M., Monti S., Genereux J.C., Wiseman R.L., Wolozin B., Connors L.H., et al. Induced pluripotent stem cell modeling of multisystemic, hereditary transthyretin amyloidosis. Stem Cell Rep. 2013;1:451–463. doi: 10.1016/j.stemcr.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Pinto A.R., Ilinykh A., Ivey M.J., Kuwabara J.T., D’Antoni M.L., Debuque R., Chandran A., Wang L., Arora K., Rosenthal N.A., et al. Revisiting cardiac cellular composition. Circ. Res. 2016;118:400–409. doi: 10.1161/CIRCRESAHA.115.307778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Castro L., Geertz B., Reinsch M., Aksehirlioglu B., Hansen A., Eschenhagen T., Reichenspurner H., Weinberger F., Pecha S. Implantation of hiPSC-derived cardiac-muscle patches after myocardial injury in a Guinea pig model. J. Vis. Exp. 2019;145:e58810. doi: 10.3791/58810. [DOI] [PubMed] [Google Scholar]
- 462.Lemoine M.D., Mannhardt I., Breckwoldt K., Prondzynski M., Flenner F., Ulmer B., Hirt M.N., Neuber C., Horvath A., Kloth B., et al. Human iPSC-derived cardiomyocytes cultured in 3D engineered heart tissue show physiological upstroke velocity and sodium current density. Sci. Rep. 2017;7:5464. doi: 10.1038/s41598-017-05600-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.Breckwoldt K., Letuffe-Breniere D., Mannhardt I., Schulze T., Ulmer B., Werner T., Benzin A., Klampe B., Reinsch M.C., Laufer S., et al. Differentiation of cardiomyocytes and generation of human engineered heart tissue. Nat. Protoc. 2017;12:1177–1197. doi: 10.1038/nprot.2017.033. [DOI] [PubMed] [Google Scholar]
- 464.Weinberger F., Mannhardt I., Eschenhagen T. Engineering cardiac muscle tissue: A maturating field of research. Circ. Res. 2017;120:1487–1500. doi: 10.1161/CIRCRESAHA.117.310738. [DOI] [PubMed] [Google Scholar]
- 465.Meyer T., Tiburcy M., Zimmermann W.H. Cardiac macrotissues-on-a-plate models for phenotypic drug screens. Adv. Drug Deliv. Rev. 2019;140:93–100. doi: 10.1016/j.addr.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 466.Garber K. RIKEN suspends first clinical trial involving induced pluripotent stem cells. Nat. Biotechnol. 2015;33:890–891. doi: 10.1038/nbt0915-890. [DOI] [PubMed] [Google Scholar]
- 467.Mayshar Y., Ben-David U., Lavon N., Biancotti J.C., Yakir B., Clark A.T., Plath K., Lowry W.E., Benvenisty N. Identification and classification of chromosomal aberrations in human induced pluripotent stem cells. Cell Stem Cell. 2010;7:521–531. doi: 10.1016/j.stem.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 468.Yoshihara M., Hayashizaki Y., Murakawa Y. Genomic instability of iPSCs: Challenges towards their clinical applications. Stem Cell Rev. 2017;13:7–16. doi: 10.1007/s12015-016-9680-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Liu P., Kaplan A., Yuan B., Hanna J.H., Lupski J.R., Reiner O. Passage number is a major contributor to genomic structural variations in mouse iPSCs. Stem Cells. 2014;32:2657–2667. doi: 10.1002/stem.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Kempf H., Zweigerdt R. Engineering and Application of Pluripotent Stem Cells. Volume 163. Springer; Cham, Switzerland: 2017. Scalable cardiac differentiation of pluripotent stem cells using specific growth factors and small molecules; pp. 39–69. [DOI] [PubMed] [Google Scholar]
- 471.Goktepe S., Abilez O.J., Parker K.K., Kuhl E. A multiscale model for eccentric and concentric cardiac growth through sarcomerogenesis. J. Theor. Biol. 2010;265:433–442. doi: 10.1016/j.jtbi.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 472.Gherghiceanu M., Barad L., Novak A., Reiter I., Itskovitz-Eldor J., Binah O., Popescu L.M. Cardiomyocytes derived from human embryonic and induced pluripotent stem cells: Comparative ultrastructure. J. Cell. Mol. Med. 2011;15:2539–2551. doi: 10.1111/j.1582-4934.2011.01417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Jiang Y., Park P., Hong S.M., Ban K. Maturation of cardiomyocytes derived from human pluripotent stem cells: Current strategies and limitations. Mol. Cells. 2018;41:613–621. doi: 10.14348/molcells.2018.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Koivumaki J.T., Naumenko N., Tuomainen T., Takalo J., Oksanen M., Puttonen K.A., Lehtonen S., Kuusisto J., Laakso M., Koistinaho J., et al. Structural immaturity of human iPSC-derived cardiomyocytes: In silico investigation of effects on function and disease modeling. Front. Physiol. 2018;9:80. doi: 10.3389/fphys.2018.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Bedada F.B., Wheelwright M., Metzger J.M. Maturation status of sarcomere structure and function in human iPSC-derived cardiac myocytes. Biochim. Biophys. Acta. 2016;1863:1829–1838. doi: 10.1016/j.bbamcr.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Vermij S.H., Abriel H., van Veen T.A. Refining the molecular organization of the cardiac intercalated disc. Cardiovasc. Res. 2017;113:259–275. doi: 10.1093/cvr/cvw259. [DOI] [PubMed] [Google Scholar]
- 477.Fujiwara M., Yan P., Otsuji T.G., Narazaki G., Uosaki H., Fukushima H., Kuwahara K., Harada M., Matsuda H., Matsuoka S., et al. Induction and enhancement of cardiac cell differentiation from mouse and human induced pluripotent stem cells with cyclosporin-A. PLoS ONE. 2011;6:e16734. doi: 10.1371/journal.pone.0016734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Zuppinger C., Gibbons G., Dutta-Passecker P., Segiser A., Most H., Suter T.M. Characterization of cytoskeleton features and maturation status of cultured human iPSC-derived cardiomyocytes. Eur. J. Histochem. 2017;61:2763. doi: 10.4081/ejh.2017.2763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.Scuderi G.J., Butcher J. Naturally engineered maturation of cardiomyocytes. Front. Cell Dev. Biol. 2017;5:50. doi: 10.3389/fcell.2017.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Brodsky V., Chernyaev A.L., Vasilyeva I.A. Variability of the cardiomyocyte ploidy in normal human hearts. Virchows Archiv. B. 1991;61:289–294. doi: 10.1007/BF02890430. [DOI] [PubMed] [Google Scholar]
- 481.Feric N.T., Radisic M. Maturing human pluripotent stem cell-derived cardiomyocytes in human engineered cardiac tissues. Adv. Drug Deliv. Rev. 2016;96:110–134. doi: 10.1016/j.addr.2015.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 482.Veerman C.C., Kosmidis G., Mummery C.L., Casini S., Verkerk A.O., Bellin M. Immaturity of human stem-cell-derived cardiomyocytes in culture: Fatal flaw or soluble problem? Stem Cells Dev. 2015;24:1035–1052. doi: 10.1089/scd.2014.0533. [DOI] [PubMed] [Google Scholar]
- 483.Nguyen M.D., Tinney J.P., Ye F., Elnakib A.A., Yuan F., El-Baz A., Sethu P., Keller B.B., Giridharan G.A. Effects of physiologic mechanical stimulation on embryonic chick cardiomyocytes using a microfluidic cardiac cell culture model. Anal. Chem. 2015;87:2107–2113. doi: 10.1021/ac503716z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 484.Sarig U., Sarig H., de-Berardinis E., Chaw S.Y., Nguyen E.B., Ramanujam V.S., Thang V.D., Al-Haddawi M., Liao S., Seliktar D., et al. Natural myocardial ECM patch drives cardiac progenitor based restoration even after scarring. Acta Biomater. 2016;44:209–220. doi: 10.1016/j.actbio.2016.08.031. [DOI] [PubMed] [Google Scholar]
- 485.Chen W.C., Wang Z., Missinato M.A., Park D.W., Long D.W., Liu H.J., Zeng X., Yates N.A., Kim K., Wang Y. Decellularized zebrafish cardiac extracellular matrix induces mammalian heart regeneration. Sci. Adv. 2016;2:e1600844. doi: 10.1126/sciadv.1600844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 486.Kim C., Majdi M., Xia P., Wei K.A., Talantova M., Spiering S., Nelson B., Mercola M., Chen H.S. Non-cardiomyocytes influence the electrophysiological maturation of human embryonic stem cell–derived cardiomyocytes during differentiation. Stem Cells Dev. 2010;19:783–795. doi: 10.1089/scd.2009.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 487.Kolanowski T.J., Antos C.L., Guan K. Making human cardiomyocytes up to date: Derivation, maturation state and perspectives. Int. J. Cardiol. 2017;241:379–386. doi: 10.1016/j.ijcard.2017.03.099. [DOI] [PubMed] [Google Scholar]
- 488.Glazier A.A., Thompson A., Day S.M. Allelic imbalance and haploinsufficiency in MYBPC3-linked hypertrophic cardiomyopathy. Pflugers Archiv Eur. J. Physiol. 2019;471:781–793. doi: 10.1007/s00424-018-2226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Clemen C.S., Stockigt F., Strucksberg K.H., Chevessier F., Winter L., Schutz J., Bauer R., Thorweihe J.M., Wenzel D., Schlotzer-Schrehardt U., et al. The toxic effect of R350P mutant desmin in striated muscle of man and mouse. Acta Neuropathol. 2015;129:297–315. doi: 10.1007/s00401-014-1363-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 490.Sugawara M., Kato K., Komatsu M., Wada C., Kawamura K., Shindo P.S., Yoshioka P.N., Tanaka K., Watanabe S., Toyoshima I. A novel de novo mutation in the desmin gene causes desmin myopathy with toxic aggregates. Neurology. 2000;55:986–990. doi: 10.1212/WNL.55.7.986. [DOI] [PubMed] [Google Scholar]
- 491.Ma H., Marti-Gutierrez N., Park S.W., Wu J., Lee Y., Suzuki K., Koski A., Ji D., Hayama T., Ahmed R., et al. Correction of a pathogenic gene mutation in human embryos. Nature. 2017;548:413–419. doi: 10.1038/nature23305. [DOI] [PubMed] [Google Scholar]
- 492.Echigoya Y., Lim K.R.Q., Nakamura A., Yokota T. Multiple Exon skipping in the duchenne muscular dystrophy hot spots: Prospects and challenges. J. Personal. Med. 2018;8:41. doi: 10.3390/jpm8040041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Aartsma-Rus A., van Ommen G.J. Antisense-mediated exon skipping: A versatile tool with therapeutic and research applications. Rna. 2007;13:1609–1624. doi: 10.1261/rna.653607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 494.Dick E., Kalra S., Anderson D., George V., Ritso M., Laval S.H., Barresi R., Aartsma-Rus A., Lochmuller H., Denning C. Exon skipping and gene transfer restore dystrophin expression in human induced pluripotent stem cells-cardiomyocytes harboring DMD mutations. Stem Cells Dev. 2013;22:2714–2724. doi: 10.1089/scd.2013.0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 495.Van Deutekom J.C., Janson A.A., Ginjaar I.B., Frankhuizen W.S., Aartsma-Rus A., Bremmer-Bout M., den Dunnen J.T., Koop K., van der Kooi A.J., Goemans N.M., et al. Local dystrophin restoration with antisense oligonucleotide PRO051. N. Engl. J. Med. 2007;357:2677–2686. doi: 10.1056/NEJMoa073108. [DOI] [PubMed] [Google Scholar]
- 496.Zhang Y., Long C., Li H., McAnally J.R., Baskin K.K., Shelton J.M., Bassel-Duby R., Olson E.N. CRISPR-Cpf1 correction of muscular dystrophy mutations in human cardiomyocytes and mice. Sci. Adv. 2017;3:e1602814. doi: 10.1126/sciadv.1602814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497.Min Y.L., Li H., Rodriguez-Caycedo C., Mireault A.A., Huang J., Shelton J.M., McAnally J.R., Amoasii L., Mammen P.P.A., Bassel-Duby R., et al. CRISPR-Cas9 corrects Duchenne muscular dystrophy exon 44 deletion mutations in mice and human cells. Sci. Adv. 2019;5:eaav4324. doi: 10.1126/sciadv.aav4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 498.White J.A., McAlpine P.J., Antonarakis S., Cann H., Eppig J.T., Frazer K., Frezal J., Lancet D., Nahmias J., Pearson P., et al. Guidelines for human gene nomenclature (1997). HUGO nomenclature committee. Genomics. 1997;45:468–471. doi: 10.1006/geno.1997.4979. [DOI] [PubMed] [Google Scholar]