Abstract
The cellular prion protein (PrPC) is an ubiquitous cell surface protein mostly expressed in neurons, where it localizes to both pre- and post-synaptic membranes. PrPC aberrant conformers are the major components of mammalian prions, the infectious agents responsible for incurable neurodegenerative disorders. PrPC was also proposed to bind aggregated misfolded proteins/peptides, and to mediate their neurotoxic signal. In spite of long-lasting research, a general consensus on the precise pathophysiologic mechanisms of PrPC has not yet been reached. Here we review our recent data, obtained by comparing primary neurons from PrP-expressing and PrP-knockout mice, indicating a central role of PrPC in synaptic transmission and Ca2+ homeostasis. Indeed, by controlling gene expression and signaling cascades, PrPC is able to optimize glutamate secretion and regulate Ca2+ entry via store-operated channels and ionotropic glutamate receptors, thereby protecting neurons from threatening Ca2+ overloads and excitotoxicity. We will also illustrate and discuss past and unpublished results demonstrating that Aβ oligomers perturb Ca2+ homeostasis and cause abnormal mitochondrial accumulation of reactive oxygen species by possibly affecting the PrP-dependent downregulation of Fyn kinase activity.
Keywords: prion protein, Ca2+ homeostasis, glutamate, neurotransmission, synapses, ROS, Aβ oligomers, Fyn, NADPH oxidase
1. Introduction
Nowadays, neurodegenerative disorders affecting elderly people is one major health problem worldwide, which is aggravated by lack of early diagnostic tools and pharmaceutical approaches. To name a few, they include amyotrophic lateral sclerosis and most common diseases such as Alzheimer’s (AD) and Parkinson′s. Despite its much less occurrence (1–2 cases per million), prion disorders have become renown after appearance of ′mad cow disease′ [1], and the development in man of a variant form of the Creutzfeldt–Jakob disease [2] caused by ingestion of bovine prion-tainted food. All these disorders may have a genetic origin, which, however, accounts for only a few percentages of cases. Typically, they share both a prevalent sporadic etiology and formation of toxic soluble oligomers of misfolded proteins or peptides, which may eventually deposit as amyloids [3]. Remarkably, the physiologic role of most disease-associated proteins is still largely obscure, thus precluding the design of appropriate (mechanism-based) interventions interfering with the neurodegenerative process.
Prion disorders are associated with formation and aggregation in the brain of a template-induced abnormal folding (termed PrPSc) of the constitutively expressed, α helix-rich prion protein (PrPC). Mostly present in the pre- and post-synaptic neuronal membranes [4,5,6,7], PrPC localizes to the cell surface through a glycosylphosphatidylinositol (GPI) anchor, and segregates in cholesterol-sphingolipid rich microdomains [8,9]. The β sheet-enriched PrPSc conformer is the major component of prions causing inevitably fatal diseases in humans and animals [10]. To date, prions are apparently the only neurodegenerative agent retaining the feature of transmissibility within or between mammalian species [3,11]. As to the modality leading to neuronal death, although PrPSc oligomers could be harmful per se, a growing body of evidence accumulated in in vitro and in vivo paradigms now conceives that the GPI-based tethering of PrPC to the plasma membrane (PM) is strictly required for PrPSc to unambiguously exert neurotoxicity [12,13,14,15,16]. It is hypothesized that PrPC forms receptor platforms with other surface and/or transmembrane partners engaged in a panoply of downhill beneficial functions, ranging from embryogenesis to cell survival and neuroprotective signaling [17,18,19,20,21]. It is therefore possible to assume that the demonstrated docking of pathogenic prion oligomers to PrPC [22,23] distorts PrPC native structure-function relationship, thus ultimately provoking subversion of advantageous signals into pathways noxious to the cell life.
The present review will first illustrate recent studies by our laboratory aimed to shed light on PrPC physiology, particularly on the action(s) of PrPC in synapses that precisely link the protein with post-synaptic Ca2+ fluxes, and downstream events. In addition, the second part of the presentation will provide unpublished in vitro data suggesting that the detrimental effect of AD-related Aβ1-42 peptides in neurons may include loss of PrPC protection over Ca2+ metabolism and production of reactive oxygen species (ROS).
2. PrPC Supports Correct Neuronal Activities by Regulating Gene Expression and Ca2+ Metabolism
2.1. Action of PrPC at Pre-Synapses
In a recent work [24], we exploited multiple experimental approaches to clarify the role of PrPC at pre-synaptic endings. Specifically, mass spectrometry was used to quantify glutamate release from depolarized primary cerebellar granule neurons (CGN) expressing, or not (PrP-KO), the protein; immunolabeling approaches to follow synaptic vesicle recycling; quantitative mass spectrometry, flanked by selected reaction monitoring and qRT-PCR for data validation, to determining the protein expression profile in the two neuronal types. These analyses clearly demonstrated that glutamate release and synaptic vesicle dynamics are profoundly compromised in PrP-KO CGN (by 40% and 60%, respectively), a result that could be attributed to the underrepresentation of proteins that, among others, are key actors in the two processes—i.e., Rab 3a, syntaxin 1b, and synaptogyrin 3—that are involved in neurotransmitter release, and other three Rab isoforms playing a role in vesicular trafficking. On the other hand, bioinformatic and biochemical approaches demonstrated that PrPC ensured proper gene expression of these proteins by acting on (at least) the transcription factor cAMP-response element binding protein 1 (CREB1) [25], which regulates most of the above genes.
By underscoring the contribution for optimal neurotransmitter secretion, this novel finding undoubtedly defines more accurately the significance of neuroprotective activities long attributed to PrPC [19,20]. At the same time, were such functions disrupted, it may also define that one key molecular pathway possibly contributing to disease phenotypes arises at pre-synapses. As aforementioned, one event likely changing the structure–function coupling of PrPC in prion diseases is the binding of accumulated prions to PrPC [22,26]. As a consequence, prions may displace PrPC from its native PM location, or may substitute its physiologic partners and/or modify their mode of interaction [26]. All these events could thus provoke loss of PrPC ability to properly regulate gene expression and neurotransmission therein.
Likewise, disastrous synaptic dysfunction and cognitive impairment may be generated by other neurotoxic species equally requiring PrPC as binding receptor; for example, extracellular soluble Aβ oligomers, the 50% of which bind PrPC [27,28,29] (but see [30,31]), and which are AD major initiators [32,33] together with intracellular aggregates of the hyper-phosphorylated tau protein [34]; or α-synuclein oligomers associated with synucleinopathies [35,36].
Intuitively, a critical extension for PrPC capacity to optimize secretion of glutamate, the prime excitatory neurotransmitter in the central nervous system, is that PrPC allows post-synaptic routes for Ca2+ entry to be adequately reached. A compromised PrPC function would instead preclude full activation of ionotropic (iGluR) and metabotropic (mGluR) glutamatergic receptors, ultimately resulting in an imbalanced intracellular Ca2+ homeostasis and, therefore, in defective Ca2+-based processes of learning and memory.
2.2. Action of PrPC on SOCE and iGluRs
To decipher other aspects of PrPC operational modes at synapses, we considered past reports on the impact of the protein on Ca2+-dependent pathways, and their deviation in prion and PrP-KO paradigms (reviewed in [37,38,39]), but also the ambivalent nature shared by PrPC (see above) and Ca2+. Ca2+ is a highly versatile transducer of extracellular signals mediating a myriad of cellular responses. Yet it triggers cell demise upon disruption of its homeostasis [40], as observed in neurodegenerative disorders such as AD [41,42]. Specifically, our studies focused on identifying the sites at which the PM-bound PrPC could regulate the entry of extracellular Ca2+, and the downstream distribution of the ion, which implied a strategy monitoring Ca2+ variations locally. To this end, we prevalently compared the signal of gene-encoded Ca2+-sensitive proteins (aequorins) engineered to target specific cell compartments [43] of primary cultures of CGN and cortical neurons expressing, or not, PrPC. We used aequorins addressing PM inner microdomains (thus ideally serving to sense the immediate Ca2+ transit through the PM [40]), or the bulk cytosol, or the mitochondrial matrix. Such an approach successfully demonstrated that, compared to PrP-KO neurons, the presence of PrPC profoundly attenuates external Ca2+ influx through different PM routes, i.e., the process known as store-operated Ca2+ entry (SOCE) [44,45], and iGluR-channels [46], as well as the subsequent Ca2+ transients in various cell compartments.
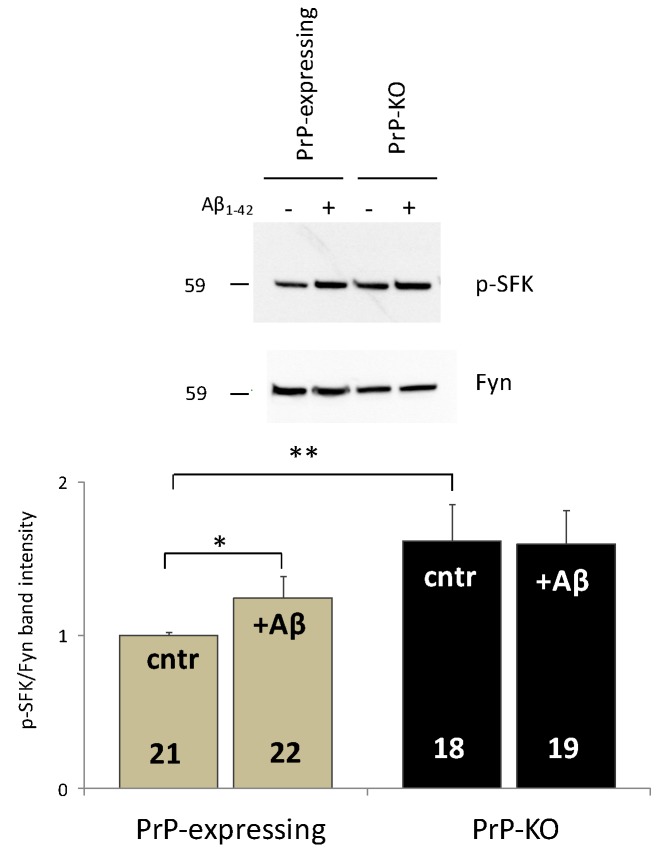
In the case of SOCE, this unusual but evolutionary conserved means for Ca2+ transport is triggered by depletion (physiological or, in vitro, by adding Ca2+ chelators) of endoplasmic reticulum (ER) Ca2+ stores, which is sensed by two ER membrane-spanning proteins (stromal interaction molecules, STIM1 and 2 [47,48] but also [45,49,50,51]). Following their conformational change, STIM1/2 migrate and concentrate in areas juxtaposed to the PM favoring interaction with, and opening of a specific Ca2+-permeable channel complex allowing SOCE [47]. STIM1 Tyr-phosphorylation by non-receptor Src family kinases (SFK) is crucial for SOCE full activation [48]. Our analyses proved that this event could well explain the lower Ca2+ transients (by around 35%) observed in PrP-expressing CGN compared to PrP-KO neurons [45]. Indeed, PrPC strongly downregulated (by around 50%) [45] the SFK member Fyn [52], possibly implicating group-I mGluRs [7,53,54] or other transmembrane proteins [55] to allow PrPC and Fyn communication from the opposite sides of the PM. In turn, PrPC-Fyn coupling decreased the amount of active STIM1 in PrP-expressing controls, and, accordingly, of SOCE [50]. Importantly, PrPC-driven limitation of Fyn activity was evident both under basal conditions (with Ca2+-filled ER stores) and with ER empty stores (as after addition of Ca2+ chelators, see above). Another consequence of SOCE attenuation in PrP-expressing neurons was a reduced Ca2+ accumulation in the cytosol, and likewise in the mitochondrial matrix [45]. This is important for the cell survival, because Ca2+ overflow in the matrix of mitochondria augments the permeability of the inner membrane, which threatens the organelle intactness and the cell life [56]. To note that enhanced SOCE [45], and a more active Fyn (Figure 1), equally pertained to PrP-KO cortical neurons.
Figure 1.
Soluble Aβ1–42 oligomers abrogate the PrP-dependent control over Fyn in PrP-expressing primary cortical neurons. Both the representative western blot (WB) obtained after probing PrP-expressing and PrP-KO cortical neurons (treated (+), or not (−), with Aβ1–42 oligomers) with antibody to active (auto-phosphorylated, p) SFK or total Fyn (upper panel), and the densitometric analysis of the pSFK immuno-reactive bands normalized to the corresponding signal of total Fyn (lower panel), show that Aβ addition significantly relieves the restriction on Fyn activation observed in untreated PrP-expressing controls relative to PrP-KO counterparts (cntr, grey and black bars, respectively). Conversely, no impact of Aβ was observed in PrP-KO neurons (see text for the explanation of the higher Fyn activation in untreated PrP-KO neurons). After seven days in culture, primary cortical neurons (isolated from PrP-expressing and PrP-KO mice lines Tg46 and F10, respectively [57] (Authorization n. 13/2012), and cultured as previously described [46]), were incubated (1 h, 37 °C), or not, with Aβ1–42 oligomers (5 µM, prepared and oligomerized as in [45]), and then lyzed using an ice-cold buffer containing glycerol (10% (w/v)), SDS (2% (w/v)), Tris/HCl (62.5 mM, pH 6.8), urea (1.8 M), Na3VO4 (5 mM), and cocktails of protease and phosphatase inhibitors (Roche). Total protein quantification, WB and densitometric analyses were accomplished as described elsewhere [45]. Here and after, values are expressed as mean ± SEM, and the number of replicates (i.e., different replicates from at least four primary cortical cultures prepared on different days) is indicated inside each bar diagram. * p < 0.05, ** p < 0.01 (Student’s t-test).
When iGluR-channels of CGN were individually activated by specific agonists [N-methyl-d-aspartate (NMDA), α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA), or kainate], or simultaneously stimulated by glutamate addition, a picture identical to SOCE-activated neurons was recorded at sub-PM Ca2+ ′hot spots′ and in the cytosol [46]. Indeed, the absence of PrPC augmented Ca2+ permeation (by a mean of 80%) via iGluRs compared to PrP-expressing counterparts. Similar effects were observed in cortical neurons [46]. As to how PrPC regulates iGluRs, while the ways by which PrPC depresses NMDA-sensitive receptors are known (i.e., interaction with the GluN2D regulatory subunit [58]; modulation of the affinity for the co-agonist glycine [59], we found that PrPC drastically reduces the presence of AMPA-sensitive channels at the cell surface. Such a control of receptor trafficking was likely due to the downregulation of extracellular signal-regulated kinase 1 and 2 (ERK1/2) by PrPC [46]. In fact, being that ERK1/2 is unable to restrict the activity of phosphodiesterases under this condition [60], the resulting low cAMP levels likely reduced the PKA-dependent phosphorylation (at Ser845) of the AMPA-sensitive receptor GluR1 subunit [46], which drives the correct receptor trafficking to the PM only in the active (phosphorylated) form [61].
Intriguingly, however, when testing mitochondrial Ca2+ uptake, we observed that only exposure of CGN to glutamate replicated exactly the effect of PrPC presence/absence on iGluRs, whereby a higher Ca2+ amount entered mitochondria of PrP-KO neurons [46]. Conversely, the opposite occurred when CGN iGluRs were stimulated individually (by NMDA or AMPA), in which case more Ca2+ entered mitochondria of PrP-expressing neurons. Another intriguing observation, collected by electron microscopy analysis of the two CGN populations, was that, on average, mitochondria of PrP-KO CGN were around 40% more detached from the PM (hence from iGluR-mediated Ca2+ influx) relative to PrP-expressing neurons. Thus, to understand which Ca2+ pool, among those exploited by mitochondria [40], could explain the dependence of mitochondrial Ca2+ uptake from the mode of iGluR stimulation, we focused on inositol triphosphate (IP3)- and ryanodine-sensitive channels that discharge Ca2+ from the ER. These channels deliver Ca2+ directly into mitochondria by establishing contacts with the mitochondrial membranes [62]. After excluding that the vanishing amounts of mGluRs detected in primary CGN could have contributed to Ca2+ release by activating IP3-sensitive channels [46], we concentrated on the signaling module, known as Ca2+-induced Ca2+-release (CICR) [63,64], which is particularly active in excitable cells and implicates ryanodine-sensitive channels. Such an assumption was proven correct because addition of inhibitory ryanodine concentrations abolished the difference in mitochondrial Ca2+ accumulation observed in the two untreated-CGN types. These results led us to conclude that the much higher Ca2+ quantity flowing into glutamate-stimulated PrP-KO CGN compared to PrP-expressing counterparts potently activates CICR, and the subsequent mitochondrial Ca2+ uptake, in spite of the larger mitochondria-PM distance. Conversely, the much smaller Ca2+ amounts entering via NMDA- or AMPA-stimulated iGluRs [46] could have been insufficient to influence CICR in both CGN genotypes, thus favoring an efficient sequestration of Ca2+ by mitochondria of PrP-expressing neurons, which are positioned much closer to the PM iGluRs.
Taken together, these observations highlight the central role played by PrPC in controlling major post-synaptic Ca2+ entry routes, which PrPC accomplishes by modulating kinase activities (Fyn for SOCE; ERK1/2 for AMPA-sensitive receptor channels). Furthermore, our data emphasize the capacity of PM-bound PrPC to finely tune Ca2+ transients in the cytosol and, most importantly, in the mitochondrial matrix by regulating CICR as in the case of CGN. In this way, location of PrPC to post-synaptic density [6,65] strongly contributes to avoid Ca2+ overload in the various neuronal compartments and the detrimental consequences therein, e.g., glutamate excitotoxic insults threatening neuronal integrity. Concurrently, PrPC is likely to play a role in finely regulating key functions attributed to SOCE, which include neuronal excitability and gene expression [66,67], such as recruitment of Ca2+-dependent transcriptional factors as demonstrated for c-fos and nuclear factor of activated T cells [68]. From all these reviewed data, it is therefore possible to conclude that, from whatever synaptic (pre- or post-) membrane its action originates, PrPC primarily controls post-synaptic Ca2+ metabolism and, consequently, Ca2+-linked synaptic plasticity. To accomplish the works described above, our experimental approach implied the use of a PrP-KO model to enlighten, by comparison, PrPC physiology, and to mimic (to a certain extent) the consequences of compromised PrPC functions. Yet, it is well known that the chronic ablation of PrPC does not result in evident neuronal phenotypes, which would be expected from a compromised pre-/post-synaptic cross-talk consequent to the reduced glutamate exocytosis. This contradiction could, however, be only apparent, because the higher activity of iGluRs (and SOCE) in these cells likely compensates for the deficient glutamate release, thereby ensuring that an adequate Ca2+ signal arrives to post-synaptic PrP-KO neurons.
3. Effects of Aβ Oligomers on PrPC-Linked Neuronal Controls
While analysing SOCE-mediated Ca2+ influx, we tested whether 1 h-treatment with soluble oligomers of Aβ1-42 peptides (mostly toxic for the pronounced propensity to aggregate [69]) had any impact on SOCE activity of CGN and cortical neurons. We found that Aβ disrupted the control of PrPC over SOCE but only in PrP-expressing neurons [45], and likewise that over the SOCE-regulator, Fyn kinase ([45], for CGN; Figure 1, for cortical neurons). These results indicate that, irrespective of the neuronal type, a PrP-dependent SOCE-mediated abnormal Ca2+ accumulation inside cells could well represent an early dangerous action of Aβ1-. Another important conclusion is that, because Fyn and SOCE of PrP-KO neurons are immune from Aβ addition, PrPC needs to be present for Aβ1–42 to alter Ca2+ fluxes.
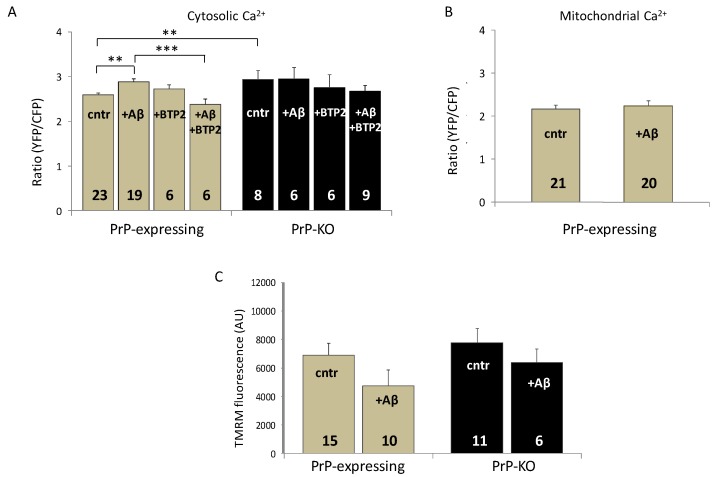
Next, in light of reports indicating that Aβ strongly impacted on Fyn-mGluR5 coupling, and on several downstream pathways, in PrP-expressing neurons under unstimulated settings [7,70], we replicated these conditions to assess Aβ1-42 influence on the resting cytosolic Ca2+ concentration (using a particularly sensitive chameleon probe that monitors low basal Ca2+ concentrations [71]) of Aβ-treated primary cortical neuronal cultures. As shown (Figure 2A), once again these aggregates were effective only in PrP-expressing neurons by augmenting the Ca2+ level up to a quantity similar to that displayed by PrP-KO counterparts. Regarding the molecular basis of this action, we favor the possibility that STIM1—and subsequently SOCE and Ca2+ influx—was stimulated by Aβ-induced over-activation of Fyn (Figure 1). Alternatively, or concurrently, one could consider that SOCE activation derived from Aβ ability to deplete ER Ca2+ stores, as suggested [72,73]. Whatever the true explanation, SOCE involvement is evident in light of the decreased cytosolic Ca2+ following inhibition of the pathway by BTP2 [74] (Figure 2A).
Figure 2.
Soluble Aβ1–42 oligomers abrogate the PrP-dependent regulation of resting cytosolic Ca2+ but does not affect mitochondrial Ca2+ levels and membrane potential in PrP-expressing primary cortical neurons. (A) Incubation with soluble Aβ1–42 oligomers (+ Aβ) increases resting cytosolic Ca2+ in PrP-expressing cortical neurons but not in PrP-KO neurons, nullifying the difference observed between the two untreated genotypes (cntr). While preincubation with the SOCE inhibitor N-{4-[3,5-bis(Trifluoromethyl)-1H-pyrazol-1-yl]phenyl}-4-methyl-1,2,3-thiadiazole-5-carboxamide (+ BTP2, 200 nM) leaves unaffected basal cytosolic Ca2+ in untreated cells, and it reverts the Aβ effect in PrP-expressing neurons (+ Aβ, + BTP2), upregulation of SOCE is the likely responsible for the Aβ-induced higher basal Ca2+ levels. (B) Conversely, Aβ does not affect Ca2+ levels in mitochondria of PrP-expressing neurons. Bar diagrams of panels A and B report the ratio between the FRET-acceptor (yellow fluorescent protein, YFP) and -donor (cyan fluorescent protein, CFP) fluorescence intensities of the used cameleon Ca2+ probe (D1cpv and 4mtD3cpv [71] in the cytosol and in the mitochondrial matrix, respectively). For these measurements, four days after isolation and plating, neurons were transduced with adeno-associated virus (AAV) coding for the chameleon bearing no targeting sequence (A), or a sequence directing the probe to the mitochondrial matrix (B), under the control of the pan-neuronal hSyn promoter [75]. Two days after infection, neurons were mounted into an open-topped chamber and maintained in 1 mM CaCl2-containing Krebs-Ringer buffer kept at 37 °C using a temperature-controlled apparatus (TC-324B, Warner Instruments). FRET measurements and analysis were performed as previously reported [75]. (C) No statistical variation is observed between the mitochondrial membrane potential of untreated, or Aβ-treated, PrP-expressing, and PrP-KO neurons. Here, the bar diagram reports the relative fluorescence quantification of the membrane potential-sensitive probe tetramethylrhodamine methyl ester (TMRM, Molecular Probes) [46] in experiments carried out with neurons loaded with TMRM (20 nM, 30 min, 37 °C) in the presence (+Aβ), or in the absence (cntr), of Aβ1-42 oligomers. ** p < 0.01, *** p < 0.001 (Student′s t-test). AU (arbitrary units). Other details are as in the legend to Figure 1.
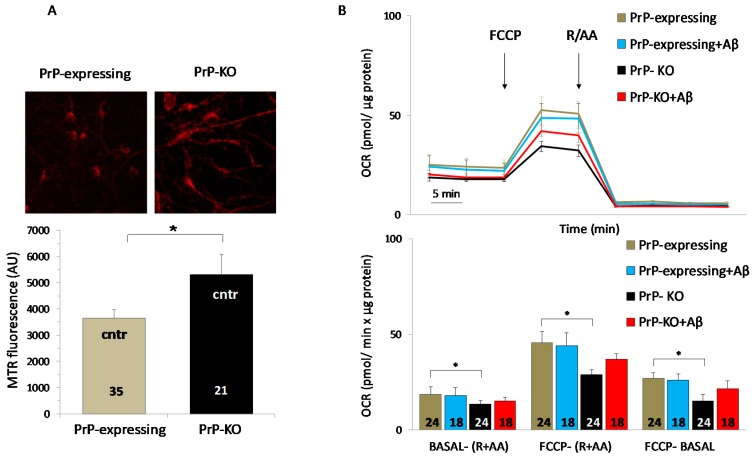
The fact that untreated PrP-KO cortical neurons maintained higher cytosolic Ca2+ levels also under basal conditions (Figure 2A) adds further emphasis to the assumption that PrPC controls Ca2+ metabolism. An explanation for such a finding may be traced in previous studies showing that PrP-KO CGN express lower amounts of sarcoplasmic/endoplasmic reticulum and PM Ca2+ pumps [44], which, therefore, restrict Ca2+ extrusion by these neurons relative to when PrPC is present. Plausibly, this is the same reason explaining the higher resting Ca2+ observed in PrP-KO cortical neurons. These results prompted us to inspect whether Aβ1-42 impacted also on mitochondrial Ca2+ fluxes. Figure 2B shows that in this case there was no effect, likely because Aβ-induced Ca2+ increase in the cytosol was insufficient to stimulate the mitochondrial uniport complex [62]. A possible additional factor unfavorable to Ca2+ uptake is that the membrane potential of mitochondria, and consequently the driving force for Ca2+ accumulation, did not significantly vary in both controls (see also [76] and in the presence of Aβ (Figure 2C), as also previously observed [77]. Interestingly, although Aβ oligomers generally depolarize mitochondria of neurons incubated with Aβ for a long period of time [78,79] there are also reports indicating that an acute treatment with Aβ (as was our case) may diminish the membrane potential and/or the oxygen consumption rate [80,81]. Both of these findings are in clear contrast with our observations (Figure 2C and Figure 3B), thereby supporting the possibility that experimental variables (e.g., type of the analyzed model system; type and preparation of the Aβ species, and the added amount, etc.) might be responsible for the contrasting results. We then tested ROS presence in mitochondria using a mitochondrial matrix-accumulating fluorescent probe, following the knowledge that mitochondrial oxidative stress and dysfunctions are common features in several neurological disorders [82,83,84], including AD [85,86,87,88]. One first observation was that, already under control conditions, ROS quantities in mitochondria of PrP-KO cortical neurons were around 45% higher than in PrP-expressing counterparts (Figure 3A). Because mitochondrial respiratory complexes are the major source of free radical production by leaking electrons to molecular oxygen [89], we then inspected mitochondrial oxygen consumption rate (OCR) by the two neuronal populations. The upper and lower panels of Fig. 3B report that PrP-KO cortical neurons exhibited an OCR value around 35% lower than PrP-expressing neurons, both under coupled and uncoupled (after addition of the protonophore FCCP) conditions. These results suggest that the enhanced production of oxygen radicals by mitochondria of control PrP-KO neurons (Figure 3A) may originate from the partially inhibited electron flow that, by rendering more reduced the redox centers of the respiratory complexes, favors their supply of electrons to oxygen and consequently the production of superoxide anion radicals. Albeit conducted under different experimental settings (e.g., polarographic detection of oxygen consumption by isolated brain mitochondria; use of quantitative electron paramagnetic resonance spectroscopy to assess superoxide production by brain submitochondrial particles), a previous study similarly found an increased generation of superoxide radicals in the absence of PrPC, which was imputed to a more reduced Complex I relative to the downstream respiratory chain components [90]. Yet, in contrast to our data, a similar respiratory rate under coupled conditions was observed in mitochondria derived from PrP-expressing, and PrP-KO, brains.
Figure 3.
PrPC controls mitochondrial oxygen consumption rate so as to reduce ROS production. (A) Higher quantities of reactive oxygen species (ROS) are present in mitochondria of control PrP-KO cortical neurons compared to the PrP-expressing counterparts. This is evident from both the upper panel, showing representative fluorescence micrographs of neurons loaded (30 min, 37 °C) with the ROS-sensitive mitochondrial matrix-accumulating cationic probe MitoTracker Red (MTR, 50 nM (λexc = 579 nm, λem = 599 nm), Molecular Probes), and the lower bar diagram reporting the corresponding MTR fluorescence quantification. Coverslip images were collected using an inverted microscope (Olympus IMT-2) equipped with a Xenon lamp, a 40× oil-immersion objective, appropriate excitation and emission filters and a cooled 16-bit digital CCD camera (Micromax, Princeton Instruments). Following the selection of mitochondria-rich fields in each coverslip, their mean MTR fluorescence was calculated after subtracting the background fluorescence collected in dark fields. (B) Compared to PrP-expressing neurons (grey), PrP-KO neurons (black) have a reduced oxygen consumption rate (OCR), as both OCR representative traces (upper panel), and their quantification (lower panel), indicate. Quantification of basal (BASAL-(R + AA)) and maximal (FCCP-(R + AA)) OCR values were calculated by subtracting non-mitochondrial OCR value, obtained after adding mitochondrial respiration blockers antimycin A (AA) and rotenone (R), from the OCR measured, respectively, before and after addition of the respiration uncoupler carbonyl cyanide 4-(trifluoromethoxy)phenylhydrazone (FCCP). Mitochondrial spare respiratory capacity (FCCP-BASAL) was calculated by subtracting the basal OCR value from the maximal OCR value. These results suggest that the slower electron flow by mitochondria of PrP-KO neurons renders more reduced the redox centers of the respiratory chain complexes of these cells, favoring the supply of electrons to oxygen and the production of superoxide anion radicals. However, Aβ-addition does not significantly alter the OCR in either PrP-expressing (light blue) and PrP-KO (red) neurons. For these measurements, neurons were isolated and plated onto XF24 microplate wells (Agilent) for seven days, at the end of which they were treated, or not, with Aβ1-42 oligomers. OCR values were real-time assessed with the XF24 Extracellular Flux Analyzer (Agilent), which allows to measure OCR changes after the sequential addition of FCCP (0.5 µM), and antimycin A (1 µM) plus rotenone (1 µM) together. Results were normalized to the protein content determined by a commercial kit (Total Protein Kit, micro Lowry, Peterson′s modification, Sigma). * p < 0.05 (Student′s t-test). Other details are as in the legend to Figure 1 and Figure 2.
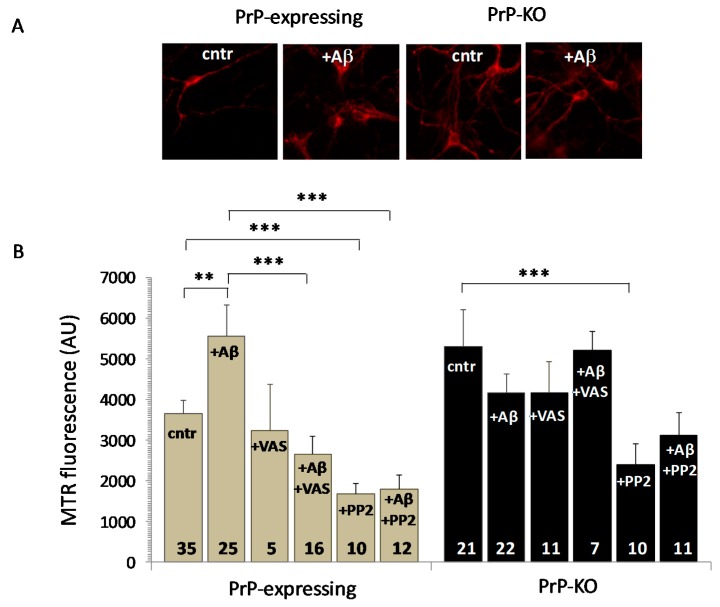
However, although Aβ1–42 oligomers did not significantly alter mitochondrial OCR in both neuronal genotypes (Figure 3B), nonetheless they once again consistently increased mitochondrial ROS only in PrP-expressing cells (Figure 4A,B).
Figure 4.
Aβ1–42 causes a PrP-dependent mitochondrial ROS overload in PrP-expressing neurons through activation of NADPH oxidase. (A,B) Starting from the higher ROS quantity present in mitochondria of untreated PrP-KO neurons than in the PrP-expressing counterparts (cntr), Aβ addition (+ Aβ) increases mitochondrial ROS only in PrP-expressing neurons as clearly demonstrated by the representative fluorescence micrographs of neurons loaded with the mitochondrial ROS-sensitive dye MTR and acquired with a 40× objective (A), and the bar diagram reporting MTR fluorescence quantification (B). The source of such an Aβ-dependent supplementary ROS content in mitochondria of PrP-expressing neurons is the cytosolic NADPH oxidase, in light of ROS diminution upon inhibiting the enzyme with 3-benzyl-7-(2-benzoxazolyl)thio-1,2,3-triazolo(4,5-d)pyrimidine (VAS 2870, 10 µM, 1 h, 37 °C) (+ Aβ + VAS). Also addition of the Fyn inhibitor 3-(4-chlorophenyl) 1-(1,1-dimethylethyl)-1H-pyrazolo(3,4-d)pyrimidin-4-amine (PP2, 10 µM, 1 h, 37 °C) reduces ROS presence in mitochondria of PrP-expressing neurons, either in the absence (+PP2) or the presence of Aβ oligomers (+ Aβ + PP2). This is consistent with the uphill stimulation of NADPH oxidase by Fyn and the relieve of the PrP-dependent block of Fyn activation by Aβ oligomers (Figure 1). However, the drastic ROS diminution observed in PrP-KO neurons treated with PP2 (+ PP2), but not with VAS (+ VAS), indicates that other Fyn-controlled (and PrP- and NADPH oxidase-independent) pro-oxidant pathways contribute to mitochondrial ROS accumulation. ** p < 0.01, *** p < 0.001 (Student′s t-test). Other details are as in the legend to Figure 1 and Figure 2.
Taken together, these results argue that Aβ-induced over-accumulating ROS in mitochondria likely originated mainly from sources outside the organelle. By NADPH oxidase, for example, the principal cytosolic ROS producer implicated in many neurodegenerative disorders [91], and already identified as a PrPC target [92]. Data of Figure 4B substantiate this possibility because Aβ-induced mitochondrial ROS overload in PrP-expressing neurons was abolished following inhibition of the enzyme by the specific drug VAS 2870 [93]. According to the literature, however, it is also possible that there is a contribution based on the crosstalk between NADPH oxidase-produced ROS and mitochondria (and vice versa) [94], which may stimulate a mitochondrial production of ROS via the ROS induced-ROS release mechanism [95,96]. Even so, taking into account that: (i) the SFK inhibitor PP2 [97] profoundly reduced Aβ-induced ROS presence in mitochondria, irrespective of Aβ addition and of the PrP genotype (Figure 4B); (ii) Aβ over-activates Fyn in PrP-expressing neurons by removing the PrP-dependent constitutive limitation on the kinase (Figure 1); (iii) Fyn is responsible for stimulating NADPH oxidase, possibly through the PKC pathway [92,98], it can be inferred that Aβ1-42 signaling requires PrPC for NADPH oxidase-dependent mitochondrial ROS surplus. Finally, considering that Fyn inhibition also decreased mitochondrial ROS of PrP-KO neurons, one can envisage Fyn as a multiple signal-integrating hub [55] amplifying other PrP-independent pro-oxidant pathways that may also include mitochondrial superoxide production [99].
In summary, the capacity of Aβ1–42 to bypass the PrP-dependent regulation of Fyn argues that, downhill to PrPC docking, Aβ exploits Fyn to increase cytosolic Ca2+ and mitochondrial oxidative stress, either of which may be prodromic to more aggressive insults endangering neuronal survival.
4. Conclusions
Having illustrated our studies dedicated to the physiology of PrPC, here we have highlighted that PrPC controls the release of neurotransmitters and post-synaptic Ca2+ entry, and protects neurons from ROS.
In particular, we have discussed the novel finding that PrPC plays an important role in pre-synaptic membranes by optimizing glutamate exocytosis. Glutamate is the main excitatory neurotransmitter responsible for learning and memory [100,101], whose Ca2+-mediated signal reaches post-synapses by activating i- and m-GluRs. Regarding iGluRs, our work has not only confirmed with different methodologies previous findings on PrPC capacity to attenuate the activity of NMDA-sensitive iGluRs, but has also demonstrated that the other (AMPA- and kainite-sensitive) iGluR sub-types fall under the same kind of control. Likewise, PrPC limits the activity of SOCE.
These results clearly imply that the operational framework of PrPC spans the entire synaptic junction. Although employing different means (regulation of gene expression at the pre-synaptic membrane; modulation of kinase activities at the post-synaptic membrane), the action of PrPC at the two synaptic sides is fully coherent under the notion of PrPC neuroprotective attributes. On one hand, the protein guarantees that the refined molecular machinery deputed to glutamate secretion (and possibly other neurotransmitters) operates optimally. On the other hand, PrPC also acts as a safeguard against excessive neuronal Ca2+ rise at the post-synaptic level (via, e.g., SOCE and iGluRs).
Although other PrP-dependent dysfunctions have been implicated in prion pathology [20,21,102], the here-reviewed data allow to predict that, once PrPC physiologic functions are acutely challenged, the favorable control of the protein over the above pre-/post-synaptic events gets irremediably broken provoking synapse deterioration and loss, which are well established markers of neurodegenerative processes [103]. Excitotoxicity mediated by oxidative stress and increased intracellular Ca2+ (for a review, see [104]) are also induced by Aβ oligomers. Having demonstrated that Aβ1-42 oligomers augment PM Ca2+ fluxes, the resting cytosolic level of the ion, as well as mitochondrial Ca2+ and ROS in PrP-expressing neurons, these data favor the contention that Aβ1-42 neurotoxic species perturb the normal protective activity of PrPC over Ca2+ metabolism and ROS production. Concurrently, they also highlight that PrPC assists Aβ in challenging neuronal integrity.
Acknowledgments
Authors acknowledge the Medical Research Council (MRC) Prion Unit, London UK, for kindly providing the mouse strains.
Abbreviations
| AA | antimycin |
| AD | Alzheimer′s disease |
| AMPA | α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid |
| BTP2 | N-{4-[3,5-bis(Trifluoromethyl)-1H-pyrazol-1-yl]phenyl}-4-methyl-1,2,3-thiadiazole-5-carboxamide, |
| CFP | cyan fluorescent protein |
| CGN | cerebellar granule neurons |
| CICR | Ca2+-induced Ca2+-release |
| CREB | cAMP-response element binding protein |
| ER | endoplasmic reticulum |
| ERK | extracellular signal-regulated kinase |
| FCCP | carbonyl cyanide 4-(trifluoromethoxy)phenylhydrazone |
| GPI | glycosylphosphatidylinositol |
| iGluR | ionotropic glutamatergic receptor |
| IP3 | inositol triphosphate |
| mGluR | metabotropic glutamatergic receptor |
| MTR | MitoTracker Red |
| NMDA | N-methyl-D-aspartate |
| OCR | oxygen consumption rate |
| PM | plasma membrane |
| PP2 | 3-(4-chlorophenyl) 1-(1,1-dimethylethyl)-1H-pyrazolo(3,4-d)pyrimidin-4-amine |
| PrPC | cellular prion protein |
| PrP-KO | PrP-knockout |
| PrPSc | abnormal PrPC conformer present in prions |
| R | Rotenone |
| ROS | reactive oxygen species |
| SEM | standard error of the mean |
| SFK | Src family kinases |
| SOCE | store-operated Ca2+ entry |
| STIM | stromal interaction molecules |
| TMRM | tetramethylrhodamine methyl ester |
| VAS 2870 | 3-benzyl-7-(2-benzoxazolyl)thio-1,2,3-triazolo(4,5-d)pyrimidine |
| YFP | yellow fluorescent protein |
| WB | western blot |
Funding
This research was funded by the University of Padova, grant number PRAT CPDA158035 to A.B.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Wells G.A., Scott A.C., Johnson C.T., Gunning R.F., Hancock R.D., Jeffrey M., Dawson M., Bradley R. A novel progressive spongiform encephalopathy in cattle. Vet. Rec. 1987;121:419–420. doi: 10.1136/vr.121.18.419. [DOI] [PubMed] [Google Scholar]
- 2.Bruce M.E., Will R.G., Ironside J.W., McConnell I., Drummond D., Suttie A., McCardle L., Chree A., Hope J., Birkett C., et al. Transmissions to mice indicate that ′new variant′ CJD is caused by the BSE agent. Nature. 1997;389:498–501. doi: 10.1038/39057. [DOI] [PubMed] [Google Scholar]
- 3.Aguzzi A., Lakkaraju A.K.K. Cell Biology of Prions and Prionoids: A Status Report. Trends Cell Biol. 2016;26:40–51. doi: 10.1016/j.tcb.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Sales N., Rodolfo K., Hassig R., Faucheux B., Di Giamberardino L., Moya K.L. Cellular prion protein localization in rodent and primate brain. Eur. J. Neurosci. 1998;10:2464–2471. doi: 10.1046/j.1460-9568.1998.00258.x. [DOI] [PubMed] [Google Scholar]
- 5.Herms J., Tings T., Gall S., Madlung A., Giese A., Siebert H., Schurmann P., Windl O., Brose N., Kretzschmar H. Evidence of presynaptic location and function of the prion protein. J. Neurosci. 1999;19:8866–8875. doi: 10.1523/JNEUROSCI.19-20-08866.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Um J.W., Nygaard H.B., Heiss J.K., Kostylev M.A., Stagi M., Vortmeyer A., Wisniewski T., Gunther E.C., Strittmatter S.M. Alzheimer amyloid-beta oligomer bound to postsynaptic prion protein activates Fyn to impair neurons. Nat. Neurosci. 2012;15:1227–1235. doi: 10.1038/nn.3178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Um J.W., Strittmatter S.M. Amyloid-β induced signaling by cellular prion protein and Fyn kinase in Alzheimer disease. Prion. 2013;7:37–41. doi: 10.4161/pri.22212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walmsley A.R., Zeng F., Hooper N.M. The N-terminal region of the prion protein ectodomain contains a lipid raft targeting determinant. J. Biol. Chem. 2003;278:37241–37248. doi: 10.1074/jbc.M302036200. [DOI] [PubMed] [Google Scholar]
- 9.Baron G.S., Caughey B. Effect of glycosylphosphatidylinositol anchor-dependent and -independent prion protein association with model raft membranes on conversion to the protease-resistant isoform. J. Biol. Chem. 2003;278:14883–14892. doi: 10.1074/jbc.M210840200. [DOI] [PubMed] [Google Scholar]
- 10.Prusiner S.B. Prions. Proc. Natl. Acad. Sci. USA. 1998;95:13363–13383. doi: 10.1073/pnas.95.23.13363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kara E., Marks J.D., Aguzzi A. Toxic Protein Spread in Neurodegeneration: Reality versus Fantasy. Trends Mol. Med. 2018;24:1007–1020. doi: 10.1016/j.molmed.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Bueler H., Aguzzi A., Sailer A., Greiner R.A., Autenried P., Aguet M., Weissmann C. Mice devoid of PrP are resistant to scrapie. Cell. 1993;73:1339–1347. doi: 10.1016/0092-8674(93)90360-3. [DOI] [PubMed] [Google Scholar]
- 13.Brandner S., Raeber A., Sailer A., Blattler T., Fischer M., Weissmann C., Aguzzi A. Normal host prion protein (PrPC) is required for scrapie spread within the central nervous system. Proc. Natl. Acad. Sci. USA. 1996;93:13148–13151. doi: 10.1073/pnas.93.23.13148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mallucci G., Dickinson A., Linehan J., Klöhn P., Brandner S., Collinge J. Depleting neuronal PrP in Prion Infection Prevents Disease and Reverses spongiosis. Science. 2003;302:871–874. doi: 10.1126/science.1090187. [DOI] [PubMed] [Google Scholar]
- 15.Chesebro B., Trifilo M., Race R., Meade-White K., Teng C., LaCasse R., Raymond L., Favara C., Baron G., Priola S., et al. Anchorless prion protein results in infectious amyloid disease without clinical scrapie. Science. 2005;308:1435–1439. doi: 10.1126/science.1110837. [DOI] [PubMed] [Google Scholar]
- 16.White M.D., Farmer M., Mirabile I., Brandner S., Collinge J., Mallucci G.R. Single treatment with RNAi against prion protein rescues early neuronal dysfunction and prolongs survival in mice with prion disease. Proc. Natl. Acad. Sci. USA. 2008;105:10238–10243. doi: 10.1073/pnas.0802759105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barton K.A., Caughey B. Is PrP the road to ruin? Embo J. 2011;30:1882–1884. doi: 10.1038/emboj.2011.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirsch T.Z., Hernandez-Rapp J., Martin-Lanneree S., Launay J.-M., Mouillet-Richard S. PrP(C) signalling in neurons: From basics to clinical challenges. Biochimie. 2014;104:2–11. doi: 10.1016/j.biochi.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Wulf M.-A., Senatore A., Aguzzi A. The biological function of the cellular prion protein: An update. BMC Biol. 2017;15:34. doi: 10.1186/s12915-017-0375-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Linden R. The Biological Function of the Prion Protein: A Cell Surface Scaffold of Signaling Modules. Front. Mol. Neurosci. 2017;10:77. doi: 10.3389/fnmol.2017.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watts J.C., Bourkas M.E.C., Arshad H. The function of the cellular prion protein in health and disease. Acta Neuropathol. 2018;135:159–178. doi: 10.1007/s00401-017-1790-y. [DOI] [PubMed] [Google Scholar]
- 22.Resenberger U.K., Harmeier A., Woerner A.C., Goodman J.L., Muller V., Krishnan R., Vabulas R.M., Kretzschmar H.A., Lindquist S., Hartl F.U., et al. The cellular prion protein mediates neurotoxic signalling of beta-sheet-rich conformers independent of prion replication. Embo. J. 2011;30:2057–2070. doi: 10.1038/emboj.2011.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scheckel C., Aguzzi A. Prions, prionoids and protein misfolding disorders. Nat. Rev. Genet. 2018;19:405–418. doi: 10.1038/s41576-018-0011-4. [DOI] [PubMed] [Google Scholar]
- 24.Peggion C., Stella R., Chemello F., Massimino M.L., Arrigoni G., Cagnin S., Biancotto G., Franchin C., Sorgato M.C., Bertoli A. The Prion Protein Regulates Synaptic Transmission by Controlling the Expression of Proteins Key to Synaptic Vesicle Recycling and Exocytosis. Mol. Neurobiol. 2019;56:3420–3436. doi: 10.1007/s12035-018-1293-4. [DOI] [PubMed] [Google Scholar]
- 25.Pradines E., Loubet D., Schneider B., Launay J.M., Kellermann O., Mouillet-Richard S. CREB-dependent gene regulation by prion protein: Impact on MMP-9 and β-dystroglycan. Cell. Signal. 2008;20:2050–2058. doi: 10.1016/j.cellsig.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 26.Pradines E., Hernandez-Rapp J., Villa-Diaz A., Dakowski C., Ardila-Osorio H., Haik S., Schneider B., Launay J.-M., Kellermann O., Torres J.-M., et al. Pathogenic prions deviate PrP(C) signaling in neuronal cells and impair A-beta clearance. Cell Death Dis. 2013;4:e456. doi: 10.1038/cddis.2012.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laurén J., Gimbel D.A., Nygaard H.B., Gilbert J.W., Strittmatter S.M. Cellular prion protein mediates impairment of synaptic plasticity by amyloid-beta oligomers. Nature. 2009;457:1128–1132. doi: 10.1038/nature07761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gimbel D.A., Nygaard H.B., Coffey E.E., Gunther E.C., Laurén J., Gimbel Z.A., Strittmatter S.M. Memory Impairment in Transgenic Alzheimer Mice Requires Cellular Prion Protein. J. Neurosci. 2010;30:6367–6374. doi: 10.1523/JNEUROSCI.0395-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu N.-W., Nicoll A.J., Zhang D., Mably A.J., O′Malley T., Purro S.A., Terry C., Collinge J., Walsh D.M., Rowan M.J. mGlu5 receptors and cellular prion protein mediate amyloid-beta-facilitated synaptic long-term depression in vivo. Nat. Commun. 2014;5:3374. doi: 10.1038/ncomms4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balducci C., Beeg M., Stravalaci M., Bastone A., Sclip A., Biasini E., Tapella L., Colombo L., Manzoni C., Borsello T., et al. Synthetic amyloid-beta oligomers impair long-term memory independently of cellular prion protein. Proc. Natl. Acad. Sci. USA. 2010;107:2295–2300. doi: 10.1073/pnas.0911829107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessels H.W., Nguyen L.N., Nabavi S., Malinow R. The prion protein as a receptor for amyloid-beta. Nature. 2010;466:E3–E4. discussion E4–E5. doi: 10.1038/nature09217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shankar G.M., Li S., Mehta T.H., Garcia-Munoz A., Shepardson N.E., Smith I., Brett F.M., Farrell M.A., Rowan M.J., Lemere C.A., et al. Amyloid-beta protein dimers isolated directly from Alzheimer′s brains impair synaptic plasticity and memory. Nat. Med. 2008;14:837–842. doi: 10.1038/nm1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Masters C.L., Selkoe D.J. Biochemistry of amyloid beta-protein and amyloid deposits in Alzheimer disease. Cold Spring Harb. Perspect. Med. 2012;2:a006262. doi: 10.1101/cshperspect.a006262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cowan C.M., Quraishe S., Mudher A. What is the pathological significance of tau oligomers? Biochem. Soc. Trans. 2012;40:693–697. doi: 10.1042/BST20120135. [DOI] [PubMed] [Google Scholar]
- 35.Aulic S., Masperone L., Narkiewicz J., Isopi E., Bistaffa E., Ambrosetti E., Pastore B., De Cecco E., Scaini D., Zago P., et al. alpha-Synuclein Amyloids Hijack Prion Protein to Gain Cell Entry, Facilitate Cell-to-Cell Spreading and Block Prion Replication. Sci. Rep. 2017;7:10050. doi: 10.1038/s41598-017-10236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferreira D.G., Temido-Ferreira M., Miranda H.V., Batalha V.L., Coelho J.E., Szego E.M., Marques-Morgado I., Vaz S.H., Rhee J.S., Schmitz M., et al. alpha-synuclein interacts with PrP(C) to induce cognitive impairment through mGluR5 and NMDAR2B. Nat. Neurosci. 2017;20:1569–1579. doi: 10.1038/nn.4648. [DOI] [PubMed] [Google Scholar]
- 37.Sorgato M.C., Bertoli A. From cell protection to death: May Ca2+ signals explain the chameleonic attributes of the mammalian prion protein? Biochem. Biophys. Res. Commun. 2009;379:171–174. doi: 10.1016/j.bbrc.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 38.Sorgato M.C., Peggion C., Bertoli A. Is, indeed, the prion protein a Harlequin servant of ′many′ masters? Prion. 2009;3:202–205. doi: 10.4161/pri.3.4.10012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peggion C., Bertoli A., Sorgato M.C. Possible role for Ca2+ in the pathophysiology of the prion protein? Biofactors. 2011;37:241–249. doi: 10.1002/biof.161. [DOI] [PubMed] [Google Scholar]
- 40.Filadi R., Pozzan T. Generation and functions of second messengers microdomains. Cell Calcium. 2015;58:405–414. doi: 10.1016/j.ceca.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 41.Green K.N., LaFerla F.M. Linking calcium to Abeta and Alzheimer′s disease. Neuron. 2008;59:190–194. doi: 10.1016/j.neuron.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 42.Demuro A., Parker I., Stutzmann G.E. Calcium signaling and amyloid toxicity in Alzheimer disease. J. Biol. Chem. 2010;285:12463–12468. doi: 10.1074/jbc.R109.080895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lim D., Bertoli A., Sorgato M.C., Moccia F. Generation and usage of aequorin lentiviral vectors for Ca(2+) measurement in sub-cellular compartments of hard-to-transfect cells. Cell Calcium. 2016;59:228–239. doi: 10.1016/j.ceca.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 44.Lazzari C., Peggion C., Stella R., Massimino M.L., Lim D., Bertoli A., Sorgato M.C. Cellular prion protein is implicated in the regulation of local Ca2+ movements in cerebellar granule neurons. J. Neurochem. 2011;116:881–890. doi: 10.1111/j.1471-4159.2010.07015.x. [DOI] [PubMed] [Google Scholar]
- 45.De Mario A., Castellani A., Peggion C., Massimino M.L., Lim D., Hill A.F., Sorgato M.C., Bertoli A. The prion protein constitutively controls neuronal store-operated Ca(2+) entry through Fyn kinase. Front. Cell. Neurosci. 2015;9:416. doi: 10.3389/fncel.2015.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De Mario A., Peggion C., Massimino M.L., Viviani F., Castellani A., Giacomello M., Lim D., Bertoli A., Sorgato M.C. The prion protein regulates glutamate-mediated Ca(2+) entry and mitochondrial Ca(2+) accumulation in neurons. J. Cell Sci. 2017;130:2736–2746. doi: 10.1242/jcs.196972. [DOI] [PubMed] [Google Scholar]
- 47.Soboloff J., Rothberg B.S., Madesh M., Gill D.L. STIM proteins: Dynamic calcium signal transducers. Nat. Rev. Mol. Cell Biol. 2012;13:549–565. doi: 10.1038/nrm3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lopez E., Jardin I., Berna-Erro A., Bermejo N., Salido G.M., Sage S.O., Rosado J.A., Redondo P.C. STIM1 tyrosine-phosphorylation is required for STIM1-Orai1 association in human platelets. Cell. Signal. 2012;24:1315–1322. doi: 10.1016/j.cellsig.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 49.Berna-Erro A., Braun A., Kraft R., Kleinschnitz C., Schuhmann M.K., Stegner D., Wultsch T., Eilers J., Meuth S.G., Stoll G., et al. STIM2 Regulates Capacitive Ca2+ Entry in Neurons and Plays a Key Role in Hypoxic Neuronal Cell Death. Sci. Signal. 2009;2:1–11. doi: 10.1126/scisignal.2000522. [DOI] [PubMed] [Google Scholar]
- 50.Zuo W.-L., Du J.-Y., Huang J.-H., Li S., Zhang G., Chen S.-L., Ruan Y.-C., Cheng C.H.K., Zhou W.-L. Tyrosine phosphorylation modulates store-operated calcium entry in cultured rat epididymal basal cells. J. Cell. Physiol. 2011;226:1069–1073. doi: 10.1002/jcp.22429. [DOI] [PubMed] [Google Scholar]
- 51.Lopez E., Frischauf I., Jardin I., Derler I., Muik M., Cantonero C., Salido G.M., Smani T., Rosado J.A., Redondo P.C. STIM1 phosphorylation at Y(316) modulates its interaction with SARAF and the activation of SOCE and I CRAC. J. Cell Sci. 2019;132 doi: 10.1242/jcs.226019. [DOI] [PubMed] [Google Scholar]
- 52.Erpel T., Courtneidge S. a Src family protein tyrosine kinases and cellular signal transduction pathways. Curr. Opin. Cell Biol. 1995;7:176–182. doi: 10.1016/0955-0674(95)80025-5. [DOI] [PubMed] [Google Scholar]
- 53.Larson M., Sherman M.A., Amar F., Nuvolone M., Schneider J.A., Bennett D.A., Aguzzi A., Lesné S.E. The complex PrP(c)-Fyn couples human oligomeric Aβ with pathological tau changes in Alzheimer′s disease. J. Neurosci. 2012;32:16857–16871. doi: 10.1523/JNEUROSCI.1858-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 54.Goniotaki D., Lakkaraju A.K.K., Shrivastava A.N., Bakirci P., Sorce S., Senatore A., Marpakwar R., Hornemann S., Gasparini F., Triller A., et al. Inhibition of group-I metabotropic glutamate receptors protects against prion toxicity. PLoS Pathog. 2017;13:e1006733. doi: 10.1371/journal.ppat.1006733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang H., Ren C.H., Gunawardana C.G., Schmitt-Ulms G. Overcoming barriers and thresholds-signaling of oligomeric Abeta through the prion protein to Fyn. Mol. Neurodegener. 2013;8:24. doi: 10.1186/1750-1326-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bernardi P., Rasola A., Forte M., Lippe G. The Mitochondrial Permeability Transition Pore: Channel Formation by F-ATP Synthase, Integration in Signal Transduction, and Role in Pathophysiology. Physiol. Rev. 2015;95:1111–1155. doi: 10.1152/physrev.00001.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mallucci G.R., Ratté S., Asante E.A., Linehan J., Gowland I., Jefferys J.G.R., Collinge J. Post-natal knockout of prion protein alters hippocampal CA1 properties, but does not result in neurodegeneration. Embo. J. 2002;21:202–210. doi: 10.1093/emboj/21.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khosravani H., Zhang Y., Tsutsui S., Hameed S., Altier C., Hamid J., Chen L., Villemaire M., Ali Z., Jirik F.R., et al. Prion protein attenuates excitotoxicity by inhibiting NMDA receptors. J. Cell Biol. 2008;181:551–555. doi: 10.1083/jcb.200711002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.You H., Tsutsui S., Hameed S., Kannanayakal T.J., Chen L., Xia P., Engbers J.D.T., Lipton S.A., Stys P.K., Zamponi G.W. Aβ neurotoxicity depends on interactions between copper ions, prion protein, and N-methyl-D-aspartate receptors. Proc. Natl. Acad. Sci. USA. 2012;109:1737–1742. doi: 10.1073/pnas.1110789109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Song R.S., Massenburg B., Wenderski W., Jayaraman V., Thompson L., Neves S.R. ERK regulation of phosphodiesterase 4 enhances dopamine-stimulated AMPA receptor membrane insertion. Proc. Natl. Acad. Sci. USA. 2013;110:15437–15442. doi: 10.1073/pnas.1311783110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Diering G.H., Heo S., Hussain N.K., Liu B., Huganir R.L. Extensive phosphorylation of AMPA receptors in neurons. Proc. Natl. Acad. Sci. USA. 2016;113:E4920–E4927. doi: 10.1073/pnas.1610631113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rizzuto R., Pinton P., Carrington W., Fay F.S., Fogarty K.E., Lifshitz L.M., Tuft R.A., Pozzan T. Close contacts with the endoplasmic reticulum as determinants of mitochondrial Ca2+ responses. Science. 1998;280:1763–1766. doi: 10.1126/science.280.5370.1763. [DOI] [PubMed] [Google Scholar]
- 63.Sneyd J. Calcium buffering and diffusion: On the resolution of an outstanding problem. Biophys. J. 1994;67:4–5. doi: 10.1016/S0006-3495(94)80448-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roderick H.L., Berridge M.J., Bootman M.D. Calcium-induced calcium release. Curr. Biol. 2003;13:R425. doi: 10.1016/S0960-9822(03)00358-0. [DOI] [PubMed] [Google Scholar]
- 65.Collins M.O., Husi H., Yu L., Brandon J.M., Anderson C.N.G., Blackstock W.P., Choudhary J.S., Grant S.G.N. Molecular characterization and comparison of the components and multiprotein complexes in the postsynaptic proteome. J. Neurochem. 2006;97(Suppl. 1):16–23. doi: 10.1111/j.1471-4159.2005.03507.x. [DOI] [PubMed] [Google Scholar]
- 66.Lalonde J., Saia G., Gill G. Store-operated calcium entry promotes the degradation of the transcription factor Sp4 in resting neurons. Sci. Signal. 2014;7:ra51. doi: 10.1126/scisignal.2005242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hartmann J., Karl R.M., Alexander R.P.D., Adelsberger H., Brill M.S., Ruhlmann C., Ansel A., Sakimura K., Baba Y., Kurosaki T., et al. STIM1 controls neuronal Ca(2+) signaling, mGluR1-dependent synaptic transmission, and cerebellar motor behavior. Neuron. 2014;82:635–644. doi: 10.1016/j.neuron.2014.03.027. [DOI] [PubMed] [Google Scholar]
- 68.Lin Y.-P., Bakowski D., Mirams G.R., Parekh A.B. Selective recruitment of different Ca2+-dependent transcription factors by STIM1-Orai1 channel clusters. Nat. Commun. 2019;10:2516. doi: 10.1038/s41467-019-10329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.LaFerla F.M., Green K.N., Oddo S. Intracellular amyloid-beta in Alzheimer’s disease. Nat. Rev. Neurosci. 2007;8:499–509. doi: 10.1038/nrn2168. [DOI] [PubMed] [Google Scholar]
- 70.Brody A.H., Strittmatter S.M. Synaptotoxic Signaling by Amyloid Beta Oligomers in Alzheimer′s Disease Through Prion Protein and Mgluradv. Adv. Pharmacol. 2018;82:293–323. doi: 10.1016/bs.apha.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Palmer A.E., Tsien R.Y. Measuring calcium signaling using genetically targetable fluorescent indicators. Nat. Protoc. 2006;1:1057–1065. doi: 10.1038/nprot.2006.172. [DOI] [PubMed] [Google Scholar]
- 72.Demuro A., Parker I. Cytotoxicity of intracellular abeta42 amyloid oligomers involves Ca2+ release from the endoplasmic reticulum by stimulated production of inositol trisphosphate. J. Neurosci. 2013;33:3824–3833. doi: 10.1523/JNEUROSCI.4367-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jensen L.E., Bultynck G., Luyten T., Amijee H., Bootman M.D., Roderick H.L. Alzheimer′s disease-associated peptide Abeta42 mobilizes ER Ca(2+) via InsP3R-dependent and independent mechanisms. Front. Mol. Neurosci. 2013;6:36. doi: 10.3389/fnmol.2013.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jairaman A., Prakriya M. Molecular pharmacology of store-operated CRAC channels. Channels. 2013;7:402–414. doi: 10.4161/chan.25292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Norante R.P., Massimino M.L., Lorenzon P., De Mario A., Peggion C., Vicario M., Albiero M., Sorgato M.C., Lopreiato R., Bertoli A. Generation and validation of novel adeno-associated viral vectors for the analysis of Ca2+ homeostasis in motor neurons. Sci. Rep. 2017;7 doi: 10.1038/s41598-017-06919-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lobao-Soares B., Bianchin M.M., Linhares M.N., Carqueja C.L., Tasca C.I., Souza M., Marques W.J., Brentani R., Martins V.R., Sakamoto A.C., et al. Normal brain mitochondrial respiration in adult mice lacking cellular prion protein. Neurosci. Lett. 2005;375:203–206. doi: 10.1016/j.neulet.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 77.Rui Y., Zheng J.Q. Amyloid beta oligomers elicit mitochondrial transport defects and fragmentation in a time-dependent and pathway-specific manner. Mol. Brain. 2016;9:79. doi: 10.1186/s13041-016-0261-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Han X.-J., Hu Y.-Y., Yang Z.-J., Jiang L.-P., Shi S.-L., Li Y.-R., Guo M.-Y., Wu H.-L., Wan Y.-Y. Amyloid beta-42 induces neuronal apoptosis by targeting mitochondria. Mol. Med. Rep. 2017;16:4521–4528. doi: 10.3892/mmr.2017.7203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Calvo-Rodriguez M., Hernando-Perez E., Nuñez L., Villalobos C. Amyloid β Oligomers Increase ER-Mitochondria Ca(2+) Cross Talk in Young Hippocampal Neurons and Exacerbate Aging-Induced Intracellular Ca(2+) Remodeling. Front. Cell. Neurosci. 2019;13:22. doi: 10.3389/fncel.2019.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Eckert A., Hauptmann S., Scherping I., Rhein V., Muller-Spahn F., Gotz J., Muller W.E. Soluble beta-amyloid leads to mitochondrial defects in amyloid precursor protein and tau transgenic mice. Neurodegener. Dis. 2008;5:157–159. doi: 10.1159/000113689. [DOI] [PubMed] [Google Scholar]
- 81.Lei Y., Yang L., Ye C.Y., Qin M.Y., Yang H.Y., Jiang H.L., Tang X.C., Zhang H.Y. Involvement of Intracellular and Mitochondrial Aβ in the Ameliorative Effects of Huperzine A against Oligomeric Aβ42-Induced Injury in Primary Rat Neurons. PLoS ONE. 2015;10:e0128366. doi: 10.1371/journal.pone.0128366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lin M.T., Beal M.F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443:787–795. doi: 10.1038/nature05292. [DOI] [PubMed] [Google Scholar]
- 83.Guo C., Sun L., Chen X., Zhang D. Oxidative stress, mitochondrial damage and neurodegenerative diseases. Neural Regen. Res. 2013;8:2003–2014. doi: 10.3969/j.issn.1673-5374.2013.21.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bhat A.H., Dar K.B., Anees S., Zargar M.A., Masood A., Sofi M.A., Ganie S.A. Oxidative stress, mitochondrial dysfunction and neurodegenerative diseases; a mechanistic insight. Biomed. Pharm. 2015;74:101–110. doi: 10.1016/j.biopha.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 85.Perry G., Cash A.D., Smith M.A. Alzheimer Disease and Oxidative Stress. J. Biomed. Biotechnol. 2002;2:120–123. doi: 10.1155/S1110724302203010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Guglielmotto M., Giliberto L., Tamagno E., Tabaton M. Oxidative stress mediates the pathogenic effect of different Alzheimer′s disease risk factors. Front. Aging Neurosci. 2010;2:3. doi: 10.3389/neuro.24.003.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang J., Chen G.-J. Mitochondria as a therapeutic target in Alzheimer′s disease. Genes Dis. 2016;3:220–227. doi: 10.1016/j.gendis.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Manoharan S., Guillemin G.J., Abiramasundari R.S., Essa M.M., Akbar M., Akbar M.D. The Role of Reactive Oxygen Species in the Pathogenesis of Alzheimer′s Disease, Parkinson′s Disease, and Huntington′s Disease: A Mini Review. Oxid. Med. Cell. Longev. 2016;2016:8590578. doi: 10.1155/2016/8590578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wong B.S., Pan T., Liu T., Li R., Gambetti P., Sy M.S. Differential contribution of superoxide dismutase activity by prion protein in vivo. Biochem. Biophys. Res. Commun. 2000;273:136–139. doi: 10.1006/bbrc.2000.2911. [DOI] [PubMed] [Google Scholar]
- 90.Paterson A.W.J., Curtis J.C., Macleod N.K. Complex I specific increase in superoxide formation and respiration rate by PrP-null mouse brain mitochondria. J. Neurochem. 2008;105:177–191. doi: 10.1111/j.1471-4159.2007.05123.x. [DOI] [PubMed] [Google Scholar]
- 91.Sorce S., Krause K.-H., Jaquet V. Targeting NOX enzymes in the central nervous system: Therapeutic opportunities. Cell. Mol. Life Sci. 2012;69:2387–2407. doi: 10.1007/s00018-012-1014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schneider B., Mutel V., Pietri M., Ermonval M., Mouillet-Richard S., Kellermann O. NADPH oxidase and extracellular regulated kinases 1/2 are targets of prion protein signaling in neuronal and nonneuronal cells. Proc. Natl. Acad. Sci. USA. 2003;100:13326–13331. doi: 10.1073/pnas.2235648100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.ten Freyhaus H., Huntgeburth M., Wingler K., Schnitker J., Baumer A.T., Vantler M., Bekhite M.M., Wartenberg M., Sauer H., Rosenkranz S. Novel Nox inhibitor VAS2870 attenuates PDGF-dependent smooth muscle cell chemotaxis, but not proliferation. Cardiovasc. Res. 2006;71:331–341. doi: 10.1016/j.cardiores.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 94.Dikalov S. Cross talk between mitochondria and NADPH oxidases. Free Radic. Biol. Med. 2011;51:1289–1301. doi: 10.1016/j.freeradbiomed.2011.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhou L., Aon M.A., Almas T., Cortassa S., Winslow R.L., O’Rourke B. A reaction-diffusion model of ROS-induced ROS release in a mitochondrial network. PLoS Comput. Biol. 2010;6:e1000657. doi: 10.1371/journal.pcbi.1000657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zorov D.B., Juhaszova M., Sollott S.J. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol. Rev. 2014;94:909–950. doi: 10.1152/physrev.00026.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bain J., McLauchlan H., Elliott M., Cohen P. The specificities of protein kinase inhibitors: An update. Biochem. J. 2003;371:199–204. doi: 10.1042/BJ20021535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chowdhury A.K., Watkins T., Parinandi N.L., Saatian B., Kleinberg M.E., Usatyuk P.V., Natarajan V. Src-mediated tyrosine phosphorylation of p47phox in hyperoxia-induced activation of NADPH oxidase and generation of reactive oxygen species in lung endothelial cells. J. Biol. Chem. 2005;280:20700–20711. doi: 10.1074/jbc.M411722200. [DOI] [PubMed] [Google Scholar]
- 99.Koo J.H., Lee W.H., Lee C.G., Kim S.G. Fyn inhibition by cycloalkane-fused 1,2-dithiole-3-thiones enhances antioxidant capacity and protects mitochondria from oxidative injury. Mol. Pharm. 2012;82:27–36. doi: 10.1124/mol.111.077149. [DOI] [PubMed] [Google Scholar]
- 100.Malenka R.C., Bear M.F. LTP and LTD: An embarrassment of riches. Neuron. 2004;44:5–21. doi: 10.1016/j.neuron.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 101.Henley J.M., Wilkinson K.A. AMPA receptor trafficking and the mechanisms underlying synaptic plasticity and cognitive aging. Dialogues Clin. Neurosci. 2013;15:11–27. doi: 10.31887/DCNS.2013.15.1/jhenley. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Castle A.R., Gill A.C. Physiological Functions of the Cellular Prion Protein. Front. Mol. Biosci. 2017;4:19. doi: 10.3389/fmolb.2017.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lewerenz J., Maher P. Chronic Glutamate Toxicity in Neurodegenerative Diseases-What is the Evidence? Front. Neurosci. 2015;9:469. doi: 10.3389/fnins.2015.00469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bezprozvanny I., Mattson M.P. Neuronal calcium mishandling and the pathogenesis of Alzheimer’s disease. Trends Neurosci. 2008;31:454–463. doi: 10.1016/j.tins.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]