Abstract
Seasonal influenza vaccines represent a positive intervention to limit the spread of the virus and protect public health. Yet continual influenza evolution and its ability to evade immunity pose a constant threat. For these reasons, vaccines with improved potency and breadth of protection remain an important need. We previously developed a next-generation influenza vaccine that displays the trimeric influenza hemagglutinin (HA) on a ferritin nanoparticle (NP) to optimize its presentation. Similar to other vaccines, HA-nanoparticle vaccine efficacy is increased by the inclusion of adjuvants during immunization. To identify the optimal adjuvants to enhance influenza immunity, we systematically analyzed TLR agonists for their ability to elicit immune responses. HA-NPs were compatible with nearly all adjuvants tested, including TLR2, TLR4, TLR7/8, and TLR9 agonists, squalene oil-in-water mixtures, and STING agonists. In addition, we chemically conjugated TLR7/8 and TLR9 ligands directly to the HA-ferritin nanoparticle. These TLR agonist-conjugated nanoparticles induced stronger antibody responses than nanoparticles alone, which allowed the use of a 5000-fold-lower dose of adjuvant than traditional admixtures. One candidate, the oil-in-water adjuvant AF03, was also tested in non-human primates and showed strong induction of neutralizing responses against both matched and heterologous H1N1 viruses. These data suggest that AF03, along with certain TLR agonists, enhance strong neutralizing antibody responses following influenza vaccination and may improve the breadth, potency, and ultimately vaccine protection in humans.
Keywords: Influenza vaccine, nanoparticles, adjuvants, TLR agonists, STING agonists, AF03
INTRODUCTION
The limited effectiveness of currently licensed influenza vaccines to elicit potent, broad and long-lasting immunity underscores the need for a more effective vaccine. These vaccines are presently derived from inactivated (IIV) or live-attenuated viruses (LAIV) and display efficacies of 10-60% (https://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm/), depending on the match of the vaccine strain to circulating viruses. Due to the extended manufacturing process, the selection of vaccine strains needs to occur six to eight months in advance [1], and loss of vaccine efficacy is often due to the viral drift [2] or shift [3] that occurs between the strain selection and administration of the vaccine. Mutations introduced during the process of egg-adaption may also contribute to lower vaccine efficacy [4, 5].
Influenza virus contains three surface proteins: hemagglutinin (HA), neuraminidase (NA), and an ion channel (M2). Among them, HA is the most important vaccine target: antibodies directed to HA can provide sterilizing immunity by blocking viral entry into cells (reviewed in [6]). We have previously developed a nanoparticle displaying the HA-trimer [7] as a novel immunogen. Briefly, the HA gene was genetically fused to a bacterial ferritin. The resulting fusion protein readily expressed and self-assembled into nanoparticles in mammalian cell culture. The HA is expressed on the 3-fold axis of symmetry, allowing the native trimers to form. Immunization experiments in mice and ferrets showed that the HA nanoparticles (HA-NP) elicit more potent responses than IIV [7]. The nanoparticle technology has been used to display HAs from diverse subtypes and can elicit broadly neutralizing antibodies, further demonstrating its utility as a non-virus-based vaccine [8].
Like most other protein subunit or peptide-based vaccines, HA-NP immunogenicity is greatly improved with the addition of an adjuvant [7]. Conventional adjuvants have been made using oil-in-water emulsions often containing squalene or alum salts. More recently, toll-like receptor (TLR) agonists have been developed as potential adjuvants [9]. TLRs, expressed on numerous immune cells, are an important part of the innate immune system that recognize pathogen associated molecular patterns (PAMPs), such as components of bacterial cell walls or viral nucleic acids. Upon engagement of a TLR, a signal cascade is initiated ultimately resulting in the suppression or upregulation of immune and inflammatory genes, including cytokine production. In this way, both innate and adaptive responses can be upregulated through engagement of TLRs [10]. TLR agonists, both natural and synthetic, have been successfully incorporated into HBV and HPV vaccines (TLR4 and TLR9 agonists) and anti-cancer immunotherapies (TLR 7/8 agonists). Stimulator of interferon genes (STING), a cytosolic DNA sensor and another branch of the PAMP-recognition innate immune system, can also be activated to boost immunogenicity of vaccines, although research so far has been limited to pre-clinical studies.
Here, we assembled a panel of adjuvants including TLR agonists and STING agonists, which can induce type I interferon production, and three conventional adjuvants to test with our HA-NP. We sought to determine the effect of adjuvants on HA-NP immunogenicity. Induction of neutralizing antibodies was measured with a functional neutralization assay, and select immune sera were evaluated by hemagglutination inhibition (HAI) and microneutralization (MN) analyses. We also hypothesized that co-delivery of the adjuvant and antigen would improve the immunogenicity of the vaccine while allowing lower effective antigen and adjuvant doses, potentially reducing systemic toxicity. To this end, we designed a vaccine with the adjuvant chemically conjugated to the HA-NP utilizing thiol-maleimide and azide-alkyne based click chemistries. With this technology, immune-stimulatory TLR agonists were attached directly to nanoparticles. Finally, the immunogenicity of one of the most potent candidate adjuvants, AF03, was further assessed in non-human primates.
METHODS
Plasmids
The A/New Caledonia/20/1999 HA ectodomain was genetically fused to the N-terminus of a modified H.pylori ferritin [7, 11]. This sequence contained the Y98F mutation [12] in HA, and three modifications in ferritin: N19Q, which removed an N-linked glycosylation site, a C31S mutation to remove a native Cys, and one engineered Cys at ferritin position 111. The N19Q site was partially glycosylated and the removal of this site allowed us to produce more homogenous protein and simplified mass spectrometry-based analytics. The S111C mutation was introduced to serve as a site for conjugation, and C31S, a site that was cysteinylated in the native protein, was removed to ensure that there were no off-target conjugation sites. Conjugation experiments used a HA-NP plasmid with an engineered TEV cleavage site separating the HA domain from the ferritin domain. All genes were codon-optimized for expression in human cell lines. The original gene was synthesized (Genscript) and subsequent mutations were introduced by site-direct mutagenesis (Agilent) or USER cloning (NEB).
HA nanoparticle production
The SIB-0002 mammalian expression plasmid [13] containing the A/New Caledonia/20/1999 (NC99) HA-NP gene was transfected into Expi293F cells per manufacturer’s protocol (Thermo), and supernatant was harvested five to six days later. HA-NPs were purified by anion exchange chromatography with an HP-Q column (GE Healthcare) followed by size exclusion chromatography (SEC, Superose 6 16/70 column, GE Healthcare). Correct assembly and size were confirmed by SEC retention volume, SDS-PAGE, and dynamic light scattering (DLS, Wyatt DynaPro Plate Reader II). Endotoxin levels were measured by Endosafe PTS with LAL cartridges (Charles River Laboratories).
Adjuvant preparation
Doses for each adjuvant are indicated in parentheses following the adjuvant name. Some adjuvants were formulated as preparations mixed 1:1 with the antigen, labelled “1:1 mixture”; 25 μL of each was used per dose. Pam2CSK4 (5 μg), Pam3CSK4 (20 μg), FSL-1 (20 μg), MPLA (0.5 μg), CpG ODN1826 (50 μg), and 2’3’-cGAMP (50 μg) were purchased from Invivogen and reconstituted per manufacturer’s recommendation. Sigma Adjuvant System (SAS, 1:1 mixture) was purchased from Sigma. DMXAA (7.1 μg) was purchased from Ark Pharm, Inc. Alum (1:1 mixture) purchased from Brenntag Biosector (“Alhydrogel 85”) and was used at a dose of 50 μg. 3M012 (5 μg) was acquired from WuXI. The remaining adjuvants were produced in house. Neoseptin-3 (5 μg) was synthesized in house following the steps outlined in [14]. AF03 (1:1 mixture), AF04 (1:1 mixture), and GLA-SE and GLA-Alum (both 1:1 mixtures) were prepared using the methods of Klucker, et. al. [15], Haensler, et. al. [16], and Misquith, et. al. [17] respectively. ADU-S100 (50 μg) was synthesized following published methods [18]. Due to poor aqueous solubility, MPLA, Neoseptin-3, 3M012, and DMXAA were dissolved in DMSO. To keep DMSO content in the final injection below five percent, the amount of these compounds that we were able to use was limited.
Immunization
Mouse experiments were carried out in accordance with all federal regulations in an AAALAC-accredited facility per the standards of the Guide for the Care and Use of Laboratory Animals, 8th ed., NRC. Protocols were reviewed and approved for scientific rigor and animal welfare by the Sanofi Institutional Animal Care and Use Committee (IACUC). BALB/C mice (female, 4-5/group) were immunized intramuscularly at week 0 and week 3. All immunization volumes were 50 μL total. Blood draws were performed at weeks 2, 5, 6, 7, and a terminal bleed was performed at week 8. For adjuvant screening studies and initial conjugation experiments, HA-NPs were dosed 0.22 μg. For each conjugation experiment, an equimolar admixture control was included wherein unconjugated HA-NPs were mixed with the amount of TLR agonist contained in the conjugated particle. The amount of TLR agonist to include in the equimolar controls was calculated based on 100% conjugation efficacy. A “high dose” control was also included wherein the unconjugated HA-NPs were mixed with 10 μg TLR7/8 agonist or 20 μg of CpG. Additionally, a dose-response study was carried out with HA-NP doses of 0.1 μg, 0.5 μg, 2.5 μg, and 12.5 μg. In this study, the amount of TLR agonist used for the “equimolar” admix control and the “high dose” admix control were calculated to maintain the ratio of antigen to adjuvant used in the initial conjugation study (0.22 μg HA-NP with either 1.7 ng 3M012 for “equimolar” or 10 μg for “high dose”).
ELISA binding assays
ELISA binding was performed on samples collected two weeks after the boost. Maxisorp 96-well plates (Nunc) were coated overnight with 0.1 μg/well of NC99 HA trimer in PBS. Plates were washed with PBS-T, and blocked with 5% skim milk, 1% BSA in PBS-T. Serum was added in serial dilutions and incubated for one hour at room temperature. Serum binding was detected with an anti-mouse HRP secondary antibody (GE Healthcare). For IgG1 and IgG2a ELISAs, HRP-labeled isotype specific secondaries were used (Southern Biotech). TMB substrate (SeraCare) was added and the reaction was quenched with 0.5 M H2SO4. Plates were read at 450 nm. Endpoint titers were calculated in Graphpad PRISM version 7 with a threshold value of approximately three times background (typically 0.1 or 0.2 AU).
Lentivirus reporter neutralization assays
The lentivirus reporter neutralization assay was performed as previously described [19-23]. Reporter lentivirus was generated by transfecting HEK293T cells with plasmids for HA, NA, TMPRSS2, CMVΔR8.2 and pHR’CMV-Luc (Promega Profection Mammalian Transfection System—Calcium Phosphate). Media was changed one day later, and lentiviral vector was harvested two and three days post-transfection and stored at −80°C until use. Neutralization assays were performed by incubating serial dilutions of serum with the lentivirus, then infecting HEK293A cells. Media was changed one day later and infection was quantified three days post-infection by reading luciferase activity (Promega Luciferase Assay System) on a MicroBeta2 LumiJET (PerkinElmer). Neutralization curves were plotted in Graphpad PRISM version 7 and IC50 values were calculated using a non-linear four-parameter function.
Hemagglutinin inhibition assay
Hemagglutinin (HA)-specific antibody was measured by the Hemagglutination Inhibition (HAI) assay on serum samples collected 5 weeks after the boost. The HAI assays were done in V-bottom 96-well plates using four hemagglutinating units of virus and 0.5% turkey red blood cells. The serum samples were pre-treated overnight with Receptor-Destroying Enzyme (RDE) and heat-inactivated prior to testing. Each sample was tested in duplicate and each assay contained positive and negative control reference sera.
Chemical conjugation
Chemical conjugations were designed to allow TLR agonists to be attached to the ferritin portion of the nanoparticle. HA is hyper-glycosylated and attempts to generate accurate, repeatable mass spectrometry readings were challenging or impossible. A Tobacco Etch Virus (TEV) cleavage site was added between HA and ferritin. Cleavage would remove HA from the ferritin nanoparticle and allow for mass spectrometry confirmation of conjugation of adjuvants to the particle core. Plasmids contained the previously mentioned ferritin modifications, including an N-linked glycosylation site removal with an N to Q mutation and the removal of a native cysteine with a C to S mutation. Lastly, a cysteine amino acid was added onto a surface-accessible residue on the ferritin nanoparticle (S111C). Modified nanoparticles were expressed, purified, and characterized as described above.
TLR agonist conjugation involved two steps. First a DBCO-PEG4-maleimide linker (Sigma) was added to reduce nanoparticles and incubated at room temperature for 1-2 hours. Excess linker was removed via ultrafiltration. Subsequently, an azido-modified TLR7/8 agonist (3M012-PEG4-azide, synthesized in house) or TLR9 agonist (CpG-azide, ISS1018 [24], synthesized by IDT or Avencia) was added to the malemide-conjugated nanoparticle. Samples were incubated at room temperature for 1-4 hours and then at 4°C for 2-4 days. Excess reagent was removed by ultrafiltration or SEC. Conjugations were confirmed by mass-spectrometry (HA-NP-3M012) and gel shift assay (HA-NP-3M012 and HA-NP-CpG). Bradford assays were used to determine protein concentrations.
Intact mass spectrometry analysis
To confirm the chemical conjugation on the HA-ferritin protein, the intact mass measurement of enzymatically released ferritin proteins from nanoparticles was applied. Agilent 1290 HPLC coupled to Agilent 6210 TOF-MS system was used for the protein separation and MS detection. For each LC-MS run, ~5μg of native or chemically-conjugated nanoparticles were loaded onto a column (Agilent ZORBAX PLRP-S 1000Å, 2.1 × 50 mm). The mobile phase for the reversed-phase HPLC were 0.1% formic acid in water as mobile phase A (MPA) and 0.1 % formic acid in acetonitrile as mobile phase B (MPB). The protein samples were loaded on column at a flow rate of 0.4 mL/min with 5% MPB for 2 min, then ramped to 30% MPB over 15 min, and finally to 90% MPB over 5 min. Under the above RPLC separation condition, the ferritin nanoparticles collapsed into monomers and their masses were monitored by the TOF-MS. The MS was running at positive ion mode with Agilent Jet Stream ESI ion source. Drying gas temperature was set at 325°C and 12 L/min. Sheath gas flow was applied at 11 L/min and heated at 400°C. Capillary voltage was set at 5 kV. Fragmentor voltage was set at 175 V. The data obtained from LC-MS were analyzed using Agilent MassHunter Qualitative Analysis software B.06 and Agilent MassHunter BioConfirm software B.06 package. Multiple charged MS spectra were deconvoluted by Maximum Entropy algorithm to measure the averaged intact mass of proteins ([M+H]+). The extracted peak area of each protein forms were extracted for the quantitative analysis. The intact MS peaks were compared to the theoretical values (average mass calculated by protein sequences and modifications).
Electron microscopy
Samples were absorbed for one minute to a hydrophobic carbon-coated grid, following a 30 second exposure to a glow discharge. Filter paper was used to remove excess liquid, samples were stained for 30 seconds with 0.75% uranyl formate, and excess liquid was removed with filter paper. Grids were examined with a TecnaiG2 Spirit BioTWIN and images were recorded with an AMT 2k CCD camera.
Non-human primate experiments
The study was reviewed and approved by the National Institute of Allergy and Infectious Diseases (NIAID) Institutional Animal Care and Use Committee (IACUC) and was conducted at the National Institutes of Health. All federal regulations and NIH guidelines were followed. Twelve adult rhesus macaques (Macaca mulatta) were divided into 3 groups (n = 4). All macaques were screened and confirmed negative for influenza antibody prior to the study. Macaques were intramuscularly immunized on weeks 0 and 8 with 15 μg of HA-NPs either unadjuvanted or adjuvanted with AF03, or with HA-matched inactivated influenza vaccine. Serum samples were collected periodically to assess antibody responses throughout the study.
Microneutralization assays
Microneutralization (MN) assays against NC99 virus was performed following the 2013 WHO Laboratory Procedures guidelines. Briefly, serum samples were treated with Receptor Destroying Enzyme II for 18-20 hours and heat-inactivated at 56°C for 40 mins. Serial dilutions of serum were incubated with influenza virus for 1 hour at 37°C degrees before transferring to 96-well plates with MDCK target cells. Two days later, non-neutralized influenza virus was measured by ELISA and the endpoint antibody titer was calculated. Reference serum was included as a control.
Statistics
Adjuvant treatments were compared by group (TLR2, TLR4, etc.) to the unadjuvanted control by analysis of variance (ANOVA) with Dunnett correction for multiple comparisons. Because the ANOVA test showed statistical significance (p-value < 0.05) among treatment groups for all assay results, a multiple comparison analysis was performed using Tukey-Kramer HSD method to further understand the statistical significance between any paired treatment groups. In general, a p-value less than 0.05 by Tukey-Kramer HSD analysis indicates the two treatment groups are statistically significant. Select adjuvants were down-selected for additional analyses including HAI and tests against heterologous strains. ANOVA was used to compare these adjuvants to unadjuvanted controls. Data from NHP experiments was also analyzed by comparing the AF03 treatment group to the unadjuvanted HA-NP group and the IIV treatment group using ANOVA. Calculations were performed using Graphpad PRISM version 7. For conjugation experiments (ELISA binding, neutralization, and HAI), ANOVA and post-tests were performed as described above using the log10-transformed titer. Values below the limit of detection were assumed to be half the value of the limit of detection.
RESULTS
Diverse adjuvants can boost neutralizing antibody responses.
A panel of sixteen adjuvants, including alum, oil-in-water emulsions, TLR agonists, and STING activators, were tested for their ability to boost neutralizing antibody titers in mice with the HA-NP (Table 1). Alum and one oil-in-water emulsion adjuvant, squalene-based AF03, boosted antibody titers (Figure 1A) compared to non-adjuvanted HA-NP (p<0.05, and p<0.001, respectively).
Table 1.
List of adjuvants evaluated.
| Adjuvant | Known Target |
Description and Dosage | Refs. |
|---|---|---|---|
| Pam3CSK4 | TLR2/1 | A tripalmitoylated synthetic lipopeptide containing the CSKKKK amino acid sequence that can agonize TLR2. TLR2 is expressed on the cell surface of numerous immune cells including monocytes, macrophages, B and T cells. Engagement of TLR2 initiates a cell signaling pathway that ultimately leads to the production of cytokines and biases the immune system towards a Th1 response. Dose: 25 μg Pam3CSK4. |
[34, 36, 93] |
| Pam2CSK4 | TLR2 | A diacylated synthetic lipopeptide containing the CSKKKK amino acid sequence that can agonize TLR2. Dose: 5 μg Pam2CSK4. |
[34] |
| FSL-1 | TLR2/6 | A synthetic lipopeptide, similar to Pam2CSK4, but with a CGDPKHPKSF peptide that can agonize TLR2. Dose: 20 μg FSL-1. |
[35, 94] |
| MPLA | TLR4 | A derivative of lipid A from Salmonella minnesota R595 lipopolysaccharide (LPS) that agonizes TLR4. It is widely considered less toxic than LPS. Engagement of TLR4 causes conformational changes in the receptor which initiates a signaling cascade resulting in NF-ƘB engagement and production of cytokines including TNF-α and IL-1. Dose: 0.5 μg MPLA. |
[95-97] |
| Neoseptin 3 | TLR4/MD-2 | A small molecule petidomimic with no structural similarity to LPS or MPLA. It activates TLR4 via MD-2. Dose: 5 μg Neoseptin 3. |
[48] |
| GLA-SE | TLR4 | A formulation of Glucioyranosyl Lipid Adjuvant (GLA) in a stable nano-emulsion (SE) of squalene oil in water. GLA is a synthetic hexaacylated lipid A derivative that engages TLR4 and induces a Th1 response. Dose: 25 μL mixed with 25 μL of antigen, resulting in a final concentration of 2% squalene and 2.5 μg GLA. |
[17, 51, 98, 99] |
| GLA-Alum | TLR4 | A Glucioyranosyl Lipid Adjuvant formulated with aluminum salts (Alum). GLA is a synthetic hexaacylated lipid A derivative that engages TLR4. Dose: 25 μL mixed with 25 μL of antigen, resulting in a final concentration of 33 μg Alum and 5 μg GLA. |
[17, 99] |
| SAS | TLR4 | Sigma Adjuvant System is a stable oil-in-water emulsion containing MPLA and synthetic trehalose dicorynomycolate. Dose: 25μL of reconstituted SAS added to 25 μL of antigen, resulting in a final concentration of 2% squalene, 12.5 ng of MPLA, and 12.5 ng of trehalose ducorynomycolate. |
[100-102] |
| AF04 | TLR4 | A formulation of a synthetic phospholipid dimer of a triacyl phospholipid (E6020) that mimics natural lipid A mixed with AF03, a squalene oil-in-water emulsion-based adjuvant. E6020 engages TLR4. Dose: 25 μL mixed with 25 μL of antigen, resulting in a final concentration of 2.5% squalene and 1.0 μg E6020. |
[16, 49] |
| 3M012 | TLR7/8 | An imidazoquinoline compound that mimics single-stranded RNA and can activate TLR7 and TLR8. TLR7 and TLR8 are endosomal receptors found on numerous immune cells. Receptor engagement induces a signaling cascade, NF-ƘB engagement, and production of pro-inflammatory cytokines. TLR7 engagement can activate pDCs and B-cells, and results in production of TNF-α. TLR8 engagement can activate mDCs and monocytes which induces the expression of TNF-α, IL-12, and MIP-1α. Dose: 5 μg 3M012. |
[57, 66] |
| CpG | TLR9 | A DNA oligonucleotide (ODN) that contains unmethylated CpG dinucleotides motifs. CpGs can engage TLR9, which are expressed in the endosome of numerous immune cells including NK cells, DCs, macrophages, and some APCs. Engagement of TLR9 leads to cellular activation and the release of pro-inflammatory cytokines such as INFα, TNFα, IL-6 IL-12. Dose: 50 μg of CpG. |
[24, 67, 68, 103] |
| DMXAA | STING | A flavone-acetic acid-based small molecule als known as vadimezan or ASA404, which can activate STING, resulting in the production of Type I interferon. STING is expressed in numerous immune cells including NK cells, T cells, myeloid cells, and monocytes. Dose: 7.1 μg of DMXAA. |
[28, 29, 104] |
| 2'3'-cGAMP | STING | A cyclic di-nucleotide (CDN) also known as non-canonical cGAMP that can activate STING and induce a Type I interferon response. Dose: 50 μg 2’3’-cGAMP. |
[105] |
| ADU-S100 | STING | A synthetic cyclic di-nucleotide (CDN) with phosphodiesterase-resistant [RP,RP] dithio cyclic di-AMP diastereomer. It is also known as ML-RR-S2-CDA and MIW815. ADU-S100 activates STING and induces a Type I interferon response. Dose: 50 μg ADU-S100. |
[31, 32, 85] |
| AF03 | A stable squalene oil-in-water emulsion that has been used to adjuvant human pandemic influenza vaccines in clinical trials. It is similar to MF59 and AS03, both of which were utilized in marketed pandemic influenza vaccines. This class of adjuvants can stimulate both B and T cell responses, although the specific mechanism of action is unknown. Dose: 25 μL AF03 mixed with 25 μL of antigen, resulting in a final concentration of 2.5% squalene. |
[15, 88, 106, 107] | |
| Alum | Aluminum hydroxide, is one of the most commonly used and oldest adjuvants. Alum is a strong inducer of Th2 responses, but poorly induces Th1 responses. Dose: 25 μL of Alum mixed with 25 μL of antigen, resulting in a final concentration of 50 μg aluminum hydroxide. |
[108, 109] |
Figure 1. Comparison of adjuvants to elicit influenza neutralizing antibodies.
The neutralizing antibody response induced by HA-NP immunization was measured by lentivirus reporter neutralization assays against homologous NC99 virus (A). Mice were vaccinated at week 0 and week 3, with serum collections at week 2, 5, 6, 7, and a terminal bleed at week 8. Lentivirus reporter neutralization assays were performed with sera from week 6 and HAI was performed with sera from week 8. The nanoparticles were tested alone and with traditional adjuvants, including Alum and AF03; TLR agonists; and STING agonists. Adjuvants that induced high neutralizing titers as measured by the neutralization assay were selected for additional HAI analyses against homologous NC99 virus (B). All measured treatments significantly boosted HAI titers (p<0.0001) over unadjuvanted HA-NP. Mean ± SEM is graphed. **** p<0.0001; *** p<0.001; **p<0.01; *p<0.05.
TLRs represent innate immune sensors that recognize molecular signatures on invading bacteria or viruses, and various TLR agonists have been employed to boost vaccine efficacy [25] or antitumor immunity [26, 27]. We tested specific agonists for TLR2, TLR4, TLR7/8, and TLR9 as adjuvants. Among the various adjuvants evaluated with HA-NP, FSL-1 (TLR2), AF04 (TLR4), and CpG (TLR9) elicited significantly higher titers of neutralizing antibodies than unadjuvanted controls, demonstrating the compatibility of HA-NP with many different types of TLR agonists (Figure 1A). One mouse treated Pam2CSK4 and one mouse treated with GLA-SE both showed no detectable neutralizing antibody response despite a robust neutralizing titer in the remaining three mice per group, suggesting more variability with these adjuvants. Wide variation was also seen in the response of mice immunized with HA-NP and 3M012, although this may be partially explained by challenges in formulating 3M012.
In addition to the panel of TLR agonists, we also investigated the adjuvant potential of three STING agonists. A mouse specific STING agonist DMXAA [28, 29] did not show any measurable neutralizing antibody titer (Figure 1A). However, two cyclic-dinucleotides 2’3’-cGAMP [30] and the ADU-S100 compound [31, 32] improved the immunogenicity of HA-NP, and the ADU-S100 compound induced neutralizing antibody titers 128-fold higher than unadjuvanted HA-NP (p=0.0017, Figure 1A).
The top adjuvant from each class (i.e., the best TLR2 agonist adjuvant, the best TLR4 agonist adjuvant, the best TLR9 agonist adjuvant, and the best STING agonist adjuvant), were selected for further analyses. AF03, which has been previously used with IIV against the 2009 pandemic influenza in human studies, was also included in the panel, and served as a helpful benchmark. HAI titers were also evaluated on these immune sera and showed that all adjuvants improved the antibody response against the homologous NC99 virus (Figure 1B, p<0.0001). HAI is a less sensitive assay than the lentivirus neutralization assay and also does not detect stem-directed antibodies. However, HAI is a well-established correlate of protection.
To probe the mechanisms of immunogenicity further, select sera were screened for IgG1 and IgG2a ELISA binding titers (Supplemental Figure 1). HA-NP without any adjuvant had a preponderance of IgG1 binding antibodies, indicating a Th2-directed immune response. While AF03 induced a stronger overall antibody response, the IgG isotype ratio remained heavily skewed towards IgG1 (Th2). FSL-1, AF04, and ADU-S100 resulted in a slightly more balanced IgG isotype ratio, and CpG skewed the ratio towards IgG2a (Th1) response.
Diverse adjuvants can induce broad, cross-neutralizing antibodies.
To evaluate the breadth of neutralization, sera were analyzed for their ability to neutralize the heterologous H1N1 viruses A/Beijing/262/95 (Beij-95) and A/Brisbane/59/2007 (Bris-07) (Figure 2). Mice immunized with HA-NP in the absence of adjuvant failed to induce detectable neutralizing or HAI antibody responses. All adjuvants elicited neutralizing antibodies in immunized mice against the heterologous viruses (Figure 2A). Furthermore, AF03 and AF04 induced cross reactive HAI responses (Figure 2B), suggesting that the breadth elicited following immunization with the HA-NP can be further improved with the inclusion of specific adjuvants.
Figure 2. Breadth of immune responses induced by adjuvants used in immunization.
Adjuvants that induced high neutralizing titers against homologous virus were selected for analyses against two additional H1 viruses, Beij95 and Bris07. Lentivirus reporter neutralization (A) and HAI (B) were used to measure the breadth of neutralization in mouse serum following two immunizations. Mean ± SEM is graphed. **** p<0.0001; *p<0.05.
TLR7/8 and TLR9 agonist-conjugated HA-NPs are immunogenic.
These data showed that HA-targeting antibody responses were improved with the addition of TLR agonists. Based on this promising result, we developed an adjuvant-conjugated vaccine with a TLR agonist directly coupled to the HA-nanoparticle. We hypothesized that targeted co-delivery of antigen and adjuvant would mitigate non-specific inflammation and potentially allow for dose sparing. To investigate, we selected two TLR agonists, 3M012 and CpG, which were chemically modified to add a functional group for conjugation (Figure 3A). Conjugated HA-NPs were analyzed by gel shift assays, SEC, DLS, mass spectrometry, and EM (Figure 3B and Supplemental Figure 2). To determine the immune response in vivo, mice were immunized with conjugated HA-NP. Compared to unadjuvanted HA-NP controls or HA-NP mixed with an equal molar amount of 3M012 (1.7 ng), the HA-NP-3M012 conjugate induced significantly higher ELISA binding titers. In fact, the titer from the conjugate was comparable to HA-NP mixed with a ~5000-fold higher dose of 3M012 (Figure 4A, 10 μg, left). A similar trend was observed with neutralizing antibody titers (Figure 4A, middle): HA-NP-3M012 induced higher neutralizing titers in the lentivirus reporter assay compared to the equimolar admixture containing HA-NP and 1.7 ng 3M012 group (p<0.0001). The 3M012-conjugated HA-NP also elicited more robust HAI responses compared to the equimolar admixture (p<0.05, Figure 4A, right). Similar improvements over HA-NP mixed with equimolar amounts of CpG (21 ng) were seen with CpG-conjugated nanoparticles (HA-NP-CpG), including a boost in ELISA binding titers (p<0.001) and neutralizing antibody titers in the lentivirus reporter assay (p<0.0001, Figure 4B, left and middle). HAI titers were also improved in the HA-NP-CpG conjugated group compared to the mixture HA-NP and a matched amount of CpG (p<0.0001, Figure 4B, right). Both HA-NP-3M012 and HA-NP-CpG had stronger IgG2a responses than unconjugated HA-NP, with HA-NP-3M012 having higher titers of IgG2a than IgG1 (Supplemental Figure 3).
Figure 3. Characterization of TLR conjugated HA-NPs.

(A) Molecular structures of the linker-TLR7/8-agonist complex and linker-TLR9-agonist complex are shown. (B) Electron micrographs of particles before and after conjugation confirm intact nanoparticle formation.
Figure 4. ELISA binding, neutralization, and HAI titers of a TLR7/8-agonist- and a TLR9- agonist conjugated to HA-NP.
The immunogenicity of HA-NP-3M012 conjugated nanoparticles (A) and HA-NP-CpG conjugated nanoparticles (B) were tested in mice and analyzed by ELISA binding, lentivirus reporter neutralization, and HAI assays. Admixture controls included a mix of HA-NP and 10 μg 3M012 or 20 μg CpG, and a mix of HA-NP and 1.7 ng 3M012 or 21 ng CpG (equimolar matches to the conjugates). A matched dose of unconjugated HA-NP was also included in the analyses. Mean ± SEM is graphed. **** p<0.0001; *** p<0.001; **p<0.01; *p<0.05.
Next, we determined if the immunogenicity of the 3M012 conjugate could be improved when given at a higher dose. For this purpose, we tested the conjugate, an equimolar admixture, a higher dose admixture, and unconjugated nanoparticles at 0.1 μg, 0.5 μg, 2.5 μg, and 12.5 μg doses of HA-NP (Figure 5). At the 0.1 μg and 0.5 μg HA-NP dose, minimal response was seen in neutralization and HAI assays except for the high admixture dose. At the 2.5 μg dose, the unconjugated HA-NP and the equimolar admixture of HA-NP and 3M012 both induced minimum antibody responses. Compared to the high dose admixture group, the 3M012-conjugated HA-NP induced similar antibody responses despite containing over 5000-fold less 3M012, documenting the efficacy of direct conjugation and targeted delivery of a TLR agonist.
Figure 5. Dose-dependent antibody responses of a TLR7/8-agonist-conjugated nanoparticle.
HA-NP-3M012 immunogenicity was tested in mice at four doses: 0.1 μg, 0.5 μg, 2.5 μg, and 12.5 μg. Admixture controls and unconjugated nanoparticle were included for comparison. Serum neutralization was measured in the NC99 lentivirus reporter assay (left) and NC99 HAI assay (right). Arrows highlight the 2.5 μg dose, wherein the HA-NP-3M012 conjugate induced similar antibody titers to HA-NP + 3M012, despite containing over 5000-fold less 3M012 adjuvant. Mean ± SEM is graphed.
HA-NP adjuvanted with AF03 boosts immunogenicity in non-human primates (NHP).
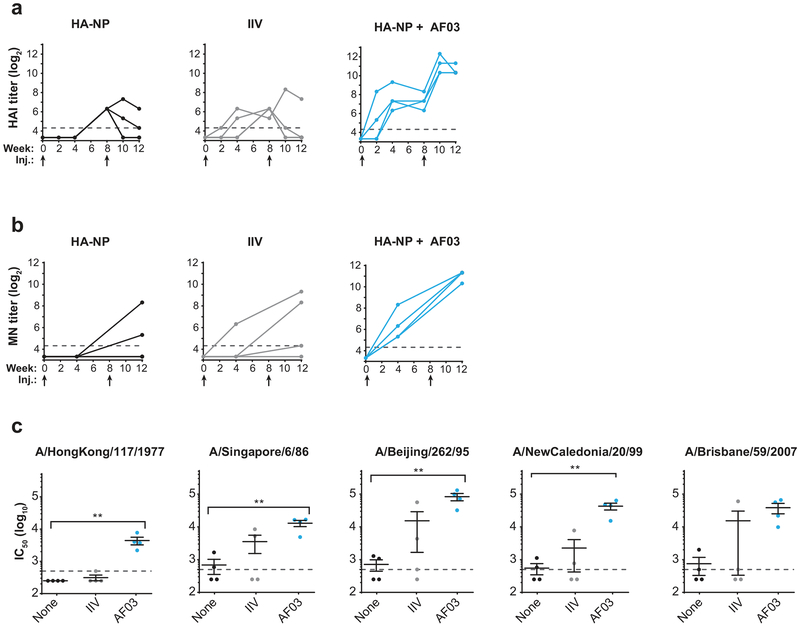
With evidence of superior immunogenicity (both homologous and heterologous) of AF03-adjuvanted HA-NPs in mice, the AF03 formulation was evaluated in NHP. AF03 was previously included in some formulations of the 2009 H1N1 pandemic inactivated influenza vaccine but has not been previously tested with our nanoparticle vaccine. Four weeks after prime and boost injections, serum from monkeys immunized with adjuvanted HA-NP showed significantly higher HAI titers than non-adjuvanted controls (Figure 6A, AF03 vs. no adjuvant, p<0.001; AF03 vs. IIV, p<0.001) and significantly higher microneutralization (MN) titers (Figure 6B, AF03 vs. no adjuvant, p<0.001; AF03 vs. IIV, p<0.001). Because we observed strong immune responses against the homologous, matched virus, we examined the breadth against a heterologous panel including H1N1 viruses A/Hong Kong/117/1977, A/Singapore/6/86, A/Beijing/262/95, and A/Brisbane/59/2007. Overall, the addition of AF03 to HA-NPs significantly boosted responses against HK77, Sing86, and Beij95 (p<0.001) compared to unadjuvanted nanoparticles.
Figure 6. Immune responses induced by adjuvanted immunizations in NHP.
Monkeys were immunized at week 0 and week 8 with 15 μg of HA-NPs adjuvanted with AF03, unadjuvanted HA-NP, or a matched dose of NC99 IIV, and antibody responses were monitored at 0, 2, and 4 weeks after each immunization. HAI titers (A) and microneutralization titers (B) were significantly boosted in the AF03 treatment group over controls at week 12. Homologous and heterologous neutralization titers were measured by lentivirus reporter neutralization assays at week 12 ((C); **p<0.01).
DISCUSSION
Adjuvants represent an important modality for improving immunogenicity of next generation seasonal or pandemic influenza vaccines. Their ability to improve the immune response has both immunological and practical consequences. On the practical side, adjuvants may exert dose sparing effects, allowing lower doses of antigens in each vaccine. Alternatively, they may increase the maximal response, with or without dose sparing. Immunologically, adjuvants boost innate responses and activate B and T cell responses. Adjuvants may be of particular importance in the very young or elderly populations where immune responses are often blunted. Their selection can have implications for polarizing immunity towards a Th1 or Th2-type response, and therefore selection should take into account the pathology and immunology of the disease target. Adjuvant activity and effectiveness is dependent on the antigen itself, formulation, and modality of delivery. Therefore, we compared adjuvant approaches using a highly studied HA antigen from the NC99 H1N1 strain of influenza delivered on a self-assembling nanoparticle. HA-NP has been demonstrated previously to improve potency and breadth of anti-influenza antibody responses [7], and its flexibility as a influenza vaccine platform [8] makes it an ideal candidate for further development and clinical testing.
Here, we screened a panel of 16 adjuvants, encompassing many different classes of molecules and mechanisms of immune stimulation, including agonists against TLR and STING. TLRs represent innate sensors that recognize molecular signatures on invading bacteria or viruses, and various TLR agonists have been employed to boost vaccine efficacy [25] or antitumor immunity [26, 27]. We tested specific agonists for TLR2, TLR4, TLR7/8, and TLR9 as adjuvants. Pam3CSK4 [33, 34], Pam2CSK4 [34], and FSL-1 [35] were chosen as TLR2 agonists. TLR2 recognizes a diverse set of molecules from bacterial cell walls, and the TLR2 agonists in our panel represent synthetic lipopeptides that mimic portions of bacterial wall lipopeptides. When activated, TLR2 forms a heterodimer with either TLR1 or TLR6. The heterodimers activate a signaling cascade, resulting in NF-κB induction, cytokine production, and activation of the adaptive immune system [36]. TLR4 recognizes components of bacterial outer membranes such as lipopolysaccharide (LPS). MPL®, a compound similar to MPLA, is included in four vaccines against hepatitis B virus (HBV), human papilloma virus (HPV), varicella zoster virus (VZV), and the malaria parasite Plasmodium falciparum [37-40]. In the HBV and HPV vaccines MPL® is combined with Alum and in the VZV and in the malaria vaccines, MPL® is combined with a saponin molecule QS-21 and formulated in liposomes (reviewed in [41]). Additionally, MPLA is a component in the widely used SAS and has been tested as an adjuvant for Mycobacterium tuberculosis [42], leishmaniosis [43], Toxoplasma gondii [44], and HIV [45] and has conferred protective immunity with IIV in mice [46, 47]. The TLR4 agonist panel also included Neoseptin-3, a small molecule agonist with no structural similarity to LPS [48], and formulations of glucopyranosyl lipid adjuvant (GLA) and E6020, synthetic phospholipids that mimic lipid A [49]. Both GLA and E6020 were tested in a squalene oil-in-water emulsion formulation (GLA-SE [50-52] and AF04 [16]), and with aluminum salts (GLA-Alum, [17, 49, 53, 54]). Notably, RC529, a synthetic MPLA-analogue [55], was included in a licensed HBV vaccine in Argentina [56]. TLR7 and TLR8 are agonized by small molecules that mimic viral single-stranded RNA. TLR7 is expressed on plasmacytoid dendritic cells (pDCs) and B cells, and TLR8 is expressed on monocytes and other DC subsets, allowing for TLR7/8 agonists to stimulate a large variety of immune cells [57]. TLR7/8 agonists have shown potent immune-stimulatory effects in various vaccines against Staphylococcus aureus [58], Leishmania donovani [59], HIV [60, 61], RSV [62], and IIV [63]. Topical imiquimod, a TLR7/8 agonist, has been approved for use to treat actinic keratosis, basal cell carcinoma [64], and genital warts [65]. One such TLR7/8 agonist, an imidazoquinoline compound 3M012 [66] was tested. TLR9 can be agonized by CpG, which are short DNA oligonucleotides containing certain C-G nucleotide motifs. CpG stimulation of TLR9 induces type I interferons and can boost both cytotoxic T lymphocyte (CTL) responses and antibody responses [67, 68]. CpGs have shown potent adjuvanting properties when tested with anthrax [69], malaria [70, 71], HBV [72, 73], RSV [74], West Nile [75], and IIV in mice [47, 76] and ferrets [77]. A recently licensed HBV vaccine, requiring fewer doses than previous vaccines, is adjuvanted by the CpG ISS-1018 [78, 79]. In lieu of challenge studies, we performed HAI assays, a well-established correlate of protection. Titers over 1:40 are generally considered to confer 50% protection against influenza infection. Our studies demonstrated that the inclusion of TLR2-, TLR4-, and TLR9-agonists in the HA-NP vaccine formulation significantly improved neutralizing antibody responses in mice. The one TLR7/8 agonist tested in the initial studies did not significantly boost the anti-HA antibody response. This may be due to solubility issues which resulted in a lower dose of adjuvant. However, formulated TLR7/8 agonists have been successfully used in the past with IIV, suggesting that alternative formulations of TLR7/8 agonists may be promising adjuvants [63, 80].
The STING receptor is activated by cyclic dinucleotides or compounds that mimic their chemical structure [81]. STING activators have shown promise in cancer immunotherapies [82] and in vaccination studies in animals models of hepatitis C [83], HIV [84], and Mycobacterium tuberculosis [85]. Three STING agonists, not previously evaluated as adjuvants for influenza vaccines, were included in our study. Recent publications report an increase in IgA and IgG titers following the use of a STING agonist with IIV in an intranasal immunization [86]. Protection from influenza infection following immunization with microparticles encapsulating STING agonists has also been reported [87]. Together with our observations, these findings suggest that STING agonists may be useful influenza vaccine adjuvants and further exploration is warranted.
This study also identified a promising adjuvant for HA-NP vaccine, AF03, with potent activity in mice and NHP. AF03 has been evaluated previously in human studies of a 2009 H1N1 pandemic influenza vaccine [15, 88] and has an acceptable safety profile, but it had not been evaluated together with a HA-NP vaccine. Against both the matched and the heterologous strains, AF03 induced strong antibody responses in non-human primates. This finding represents the first published study of HA-NPs in non-human primates and confirms that this vaccine is immunogenic in this animal model. Additionally, AF03 could potentially be used with other vaccine targets vaccine.
Since numerous TLR agonists served as potent adjuvants in admixtures, we sought to reduce the amount of adjuvant needed without compromising the immune response. To this end, we hypothesized that direct conjugation of TLR agonists to the nanoparticle would accomplish this goal. Adjuvant/antigen co-delivery should reduce systemic toxicity and mitigate off-target effects, thus improving the overall safety profile of the vaccine. The ferritin nanoparticle proved to be an optimal platform for chemical conjugation. By conjugating onto ferritin directly, we avoid potentially disrupting or re-engineering the HA antigen. Additionally, conjugation to ferritin allows us to “plug and play” and apply the same platform and conjugation technology to other antigens and adjuvants. The two-step conjugation chemistry we developed was robust and is amendable to a variety of linkers and immune-modulators, so long as the appropriate functional groups can be incorporated into the adjuvant molecules.
Our results showed that both HA-NP-3M012 and HA-NP-CpG conjugates were biologically active. Both conjugates induced stronger antibody responses than matched-dose mixtures or unconjugated HA-NP alone. We selected HA-NP-3M012 to see how the conjugate compared to unconjugated and admixture controls at different doses. To our surprise, antibody responses of the HA-NP-3M012 conjugate and the HA-NP plus high dose 3M012 overlapped, despite the fact that the conjugate contained more than 5000-fold less 3M012 than the admixture. These results support our hypothesis that direct conjugation allows for significantly lower amounts of adjuvant. Such increases in adjuvant potency may be due to the co-delivery of antigen and adjuvant. The size of the HA-NP ensures that it is efficiently trafficked into the lymphatic system and directed towards draining lymph nodes [89, 90]. Systemic dispersion of the adjuvant is presumably minimal, reducing the likelihood of adjuvant-induced toxicity. This is the first report of conjugation of TLR agonists to HA-NP, and to the best of our knowledge, the first report of directed, site-specific conjugation of TLR agonists to HA antigens. Our findings suggest that further evaluation of HA with adjuvant may improve the breadth and potency of influenza vaccines.
In summary, these studies have shown that HA-NPs are compatible with numerous adjuvants, covering a large range of molecules and formulations, including TLR agonists and STING agonists. Adjuvanted HA-NP vaccinations resulted in high titer neutralizing antibody responses and strong HAI responses. HA-NPs mixed with AF03 were also evaluated in NHPs, confirming the initial promising results from mice. AF03 has previously been used in human trials and may be suitable for further development of clinical HA-NP vaccine candidates. Further pre-clinical development, including extensive safety testing, may be needed for additional adjuvant candidates such as the TLR agonists. These studies should probe mechanistic differences between immune responses induced by differing adjuvants. A HA-NP vaccine targeting H2 influenza in currently being evaluated in phase 1 clinical trials (), and this study will help identify adjuvants that can be used to further boost immunogenicity in humans. Lastly, we developed a directly conjugated HA-NP vaccine by physically coupling a TLR agonist onto the vaccine nanoparticle core. Immunogenicity studies in mice demonstrated that direct conjugation allows for an over 5000-fold reduction in the amount of TLR agonist needed compared to traditional admixture formulations. Direct chemical conjugation may be useful for other ferritin-nanoparticle based vaccines, including Pan-H1 flu vaccines [8], universal stem-based flu vaccines [91], and vaccines targeting other diseases such as EBV [11] and HIV [92].
Supplementary Material
ACKNOWLEDGEMENTS
We thank Alison Schroeer for the preparation of figures and all members of the Sanofi Breakthrough Lab for helpful advice and discussions. We thank Maria Ericsson (Harvard Medical School) for performing negative stain EM; Amy Sullivan, Megan Pike, Kelly Balko, Terry Wilper, Karen Norton and Sara Savage from Sanofi Comparative Medicine department for technical assistance with mouse studies; Hanne Andersen Elyard and Laurent Pessaint of Bioqual for preforming the HAI and microneutralization assays; Tim Alefantis, Steve Anderson, and Irina Ustyugova of Sanofi Pasteur for valuable discussions during the course of this study; and John-Paul Todd, Hana Bao, Diana Scorpio, Elizabeth McCarthy, Amy Noe, Kathy Foulds, Shing-Fen Kao, Valerie Ficca, Nadesh Nji, Dillon Flebbe, and Michelle C. Crank of the Vaccine Research Center, NIH, for help with the non-human primate study; and Jerry Weir of the Center for Biologics Evaluation and Research, FDA, for providing influenza viruses.
ABBREVIATIONS
- HA-NP
hemagglutinin on a ferritin nanoparticle
- TLR
toll-like receptor
- STING
stimulator of interferon genes
- IIV
inactivated influenza virus
- LAIV
live-attenuated influenza virus
- HA
hemagglutinin
- NA
neuraminidase
- PAMP
pathogen-associated molecular patterns
- HAI
hemagglutination inhibition
- MN
microneutralization
- TEV
tobacco etch virus
- SEC
size exclusion chromatography
- DLS
dynamic light scattering
- ELISA
enzyme-linked immunosorbent assay
- SDS-PAGE
sodium dodecyl sulfate polyacrylamide gel electrophoresis
- MPLA
monophosphoryl Lipid A
- SAS
Sigma Adjuvant System
- GLA
glucipyranosyl lipid adjuvant
- PBS
phosphate-buffered saline
- HRP
horseradish peroxidase
- TMB
3,3',5,5'-tetramethylbenzidine
- TMPRSS2
transmembrane serine protease 2
- RDE
Receptor-Destroying Enzyme
- DBCO
dibenzocyclooctyne
- PEG
polyethylene glycol
- TOF-MS
time of flight mass spectrometry
- LC-MS
liquid chromatography mass spectrometry
- MPA
mobile phase A
- MPB
mobile phase B
- ANOVA
analysis of variance
- cGAMP
cyclic guanosine monophosphate-adenosine monophosphate
- NC99
New Caledonia 1999
- NHP
non-human primates
- LPS
lipopolysaccharide
- HBV
hepatitis B virus
- HPV
human papilloma virus
- VZV
varicella zoster virus
- DC
pDC plasmacytoid dendritic cells
- CTL
cytotoxic T lymphocyte
- RSV
respiratory syncytial virus
- HIV
human immunodeficiency virus
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Weir JP, Gruber MF. An overview of the regulation of influenza vaccines in the United States. Influenza Other Respir Viruses. 2016;10:354–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Krammer F. Novel universal influenza virus vaccine approaches. Curr Opin Virol. 2016;17:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Zost SJ, Parkhouse K, Gumina ME, Kim K, Diaz Perez S, Wilson PC, et al. Contemporary H3N2 influenza viruses have a glycosylation site that alters binding of antibodies elicited by egg-adapted vaccine strains. Proc Natl Acad Sci U S A. 2017;114:12578–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wu NC, Zost SJ, Thompson AJ, Oyen D, Nycholat CM, McBride R, et al. A structural explanation for the low effectiveness of the seasonal influenza H3N2 vaccine. PLoS Pathog. 2017;13:e1006682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Neu KE, Henry Dunand CJ, Wilson PC. Heads, stalks and everything else: how can antibodies eradicate influenza as a human disease? Curr Opin Immunol. 2016;42:48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kanekiyo M, Wei CJ, Yassine HM, McTamney PM, Boyington JC, Whittle JR, et al. Self-assembling influenza nanoparticle vaccines elicit broadly neutralizing H1N1 antibodies. Nature. 2013;499:102–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Darricarrere N, Pougatcheva S, Duan X, Rudicell RS, Chou TH, DiNapoli J, et al. Development of a Pan-H1 Influenza Vaccine. J Virol. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Maisonneuve C, Bertholet S, Philpott DJ, De Gregorio E. Unleashing the potential of NOD-and Toll-like agonists as vaccine adjuvants. Proc Natl Acad Sci U S A. 2014;111:12294–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Medzhitov R Recognition of microorganisms and activation of the immune response. Nature. 2007;449:819–26. [DOI] [PubMed] [Google Scholar]
- [11].Kanekiyo M, Bu W, Joyce MG, Meng G, Whittle JR, Baxa U, et al. Rational Design of an Epstein-Barr Virus Vaccine Targeting the Receptor-Binding Site. Cell. 2015;162:1090–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Whittle JR, Wheatley AK, Wu L, Lingwood D, Kanekiyo M, Ma SS, et al. Flow cytometry reveals that H5N1 vaccination elicits cross-reactive stem-directed antibodies from multiple Ig heavy-chain lineages. J Virol. 2014;88:4047–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Xu L, Pegu A, Rao E, Doria-Rose N, Beninga J, McKee K, et al. Trispecific broadly neutralizing HIV antibodies mediate potent SHIV protection in macaques. Science. 2017;358:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Boger DL, Beutler B. TLR-Independent Small Molecule Adjuvants. C07D 307/78 (2006.01) A61K31/343 (2006.01) C07D 209/04 (2006.01) A61K31/404 (2006.01) C07D 209/12 (2006.01) ed2016.
- [15].Klucker MF, Dalencon F, Probeck P, Haensler J. AF03, an alternative squalene emulsion-based vaccine adjuvant prepared by a phase inversion temperature method. J Pharm Sci. 2012;101:4490–500. [DOI] [PubMed] [Google Scholar]
- [16].Haensler J, Probeck P, Su J, Piras F, Dalencon F, Cotte JF, et al. Design and preclinical characterization of a novel vaccine adjuvant formulation consisting of a synthetic TLR4 agonist in a thermoreversible squalene emulsion. Int J Pharm. 2015;486:99–111. [DOI] [PubMed] [Google Scholar]
- [17].Misquith A, Fung HW, Dowling QM, Guderian JA, Vedvick TS, Fox CB. In vitro evaluation of TLR4 agonist activity: formulation effects. Colloids Surf B Biointerfaces. 2014;113:312–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Dubensky TW Jr., Kanne DB, Leong MLL, Glickman LH, Vance RE, Lemmens EE. COMPOSITIONS AND METHODS FOR ACTIVATING "STIMULATOR OF INTERFERON GENE"-DEPENDENT SIGNALLING. USA2014.
- [19].Wei CJ, Boyington JC, McTamney PM, Kong WP, Pearce MB, Xu L, et al. Induction of broadly neutralizing H1N1 influenza antibodies by vaccination. Science. 2010;329:1060–4. [DOI] [PubMed] [Google Scholar]
- [20].Kong WP, Hood C, Yang ZY, Wei CJ, Xu L, Garcia-Sastre A, et al. Protective immunity to lethal challenge of the 1918 pandemic influenza virus by vaccination. Proc Natl Acad Sci U S A. 2006;103:15987–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Wei CJ, Xu L, Kong WP, Shi W, Canis K, Stevens J, et al. Comparative efficacy of neutralizing antibodies elicited by recombinant hemagglutinin proteins from avian H5N1 influenza virus. J Virol. 2008;82:6200–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wei CJ, Boyington JC, Dai K, Houser KV, Pearce MB, Kong WP, et al. Cross-neutralization of 1918 and 2009 influenza viruses: role of glycans in viral evolution and vaccine design. Sci Transl Med. 2010;2:24ra1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Yang ZY, Wei CJ, Kong WP, Wu L, Xu L, Smith DF, et al. Immunization by avian H5 influenza hemagglutinin mutants with altered receptor binding specificity. Science. 2007;317:825–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Freed DC, Towne VM, Casimiro DR, Zhao Q, Fu TM. Evaluating functional antibodies in rhesus monkeys immunized with hepatitis B virus surface antigen vaccine with novel adjuvant formulations. Vaccine. 2011;29:9385–90. [DOI] [PubMed] [Google Scholar]
- [25].Vasou A, Sultanoglu N, Goodbourn S, Randall RE, Kostrikis LG. Targeting Pattern Recognition Receptors (PRR) for Vaccine Adjuvantation: From Synthetic PRR Agonists to the Potential of Defective Interfering Particles of Viruses. Viruses. 2017;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Adams S Toll-like receptor agonists in cancer therapy. Immunotherapy. 2009;1:949–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Huang L, Xu H, Peng G. TLR-mediated metabolic reprogramming in the tumor microenvironment: potential novel strategies for cancer immunotherapy. Cell Mol Immunol. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Tang CK, Aoshi T, Jounai N, Ito J, Ohata K, Kobiyama K, et al. The chemotherapeutic agent DMXAA as a unique IRF3-dependent type-2 vaccine adjuvant. PLoS One. 2013;8:e60038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Gao P, Zillinger T, Wang W, Ascano M, Dai P, Hartmann G, et al. Binding-pocket and lid-region substitutions render human STING sensitive to the species-specific drug DMXAA. Cell Rep. 2014;8:1668–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Zhang X, Shi H, Wu J, Zhang X, Sun L, Chen C, et al. Cyclic GMP-AMP containing mixed phosphodiester linkages is an endogenous high-affinity ligand for STING. Mol Cell. 2013;51:226–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Corrales L, Glickman LH, McWhirter SM, Kanne DB, Sivick KE, Katibah GE, et al. Direct Activation of STING in the Tumor Microenvironment Leads to Potent and Systemic Tumor Regression and Immunity. Cell Rep. 2015;11:1018–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Fu J, Kanne DB, Leong M, Glickman LH, McWhirter SM, Lemmens E, et al. STING agonist formulated cancer vaccines can cure established tumors resistant to PD-1 blockade. Sci Transl Med. 2015;7:283ra52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Caproni E, Tritto E, Cortese M, Muzzi A, Mosca F, Monaci E, et al. MF59 and Pam3CSK4 boost adaptive responses to influenza subunit vaccine through an IFN type I-independent mechanism of action. J Immunol. 2012;188:3088–98. [DOI] [PubMed] [Google Scholar]
- [34].Buwitt-Beckmann U, Heine H, Wiesmuller KH, Jung G, Brock R, Akira S, et al. Toll-like receptor 6-independent signaling by diacylated lipopeptides. Eur J Immunol. 2005;35:282–9. [DOI] [PubMed] [Google Scholar]
- [35].Okusawa T, Fujita M, Nakamura J, Into T, Yasuda M, Yoshimura A, et al. Relationship between structures and biological activities of mycoplasmal diacylated lipopeptides and their recognition by toll-like receptors 2 and 6. Infect Immun. 2004;72:1657–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Ozinsky A, Underhill DM, Fontenot JD, Hajjar AM, Smith KD, Wilson CB, et al. The repertoire for pattern recognition of pathogens by the innate immune system is defined by cooperation between toll-like receptors. Proc Natl Acad Sci U S A. 2000;97:13766–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Dooling KL, Guo A, Patel M, Lee GM, Moore K, Belongia EA, et al. Recommendations of the Advisory Committee on Immunization Practices for Use of Herpes Zoster Vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Chlibek R, Bayas JM, Collins H, de la Pinta ML, Ledent E, Mols JF, et al. Safety and immunogenicity of an AS01-adjuvanted varicella-zoster virus subunit candidate vaccine against herpes zoster in adults >=50 years of age. J Infect Dis. 2013;208:1953–61. [DOI] [PubMed] [Google Scholar]
- [39].Polhemus ME, Remich SA, Ogutu BR, Waitumbi JN, Otieno L, Apollo S, et al. Evaluation of RTS,S/AS02A and RTS,S/AS01B in adults in a high malaria transmission area. PLoS One. 2009;4:e6465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Szarewski A Cervarix(R): a bivalent vaccine against HPV types 16 and 18, with cross-protection against other high-risk HPV types. Expert Rev Vaccines. 2012;11:645–57. [DOI] [PubMed] [Google Scholar]
- [41].Didierlaurent AM, Laupeze B, Di Pasquale A, Hergli N, Collignon C, Garcon N. Adjuvant system AS01: helping to overcome the challenges of modern vaccines. Expert Rev Vaccines. 2017;16:55–63. [DOI] [PubMed] [Google Scholar]
- [42].Tian M, Zhou Z, Tan S, Fan X, Li L, Ullah N. Formulation in DDA-MPLA-TDB Liposome Enhances the Immunogenicity and Protective Efficacy of a DNA Vaccine against Mycobacterium tuberculosis Infection. Front Immunol. 2018;9:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Margaroni M, Agallou M, Athanasiou E, Kammona O, Kiparissides C, Gaitanaki C, et al. Vaccination with poly(D,L-lactide-co-glycolide) nanoparticles loaded with soluble Leishmania antigens and modified with a TNFalpha-mimicking peptide or monophosphoryl lipid A confers protection against experimental visceral leishmaniasis. Int J Nanomedicine. 2017;12:6169–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Song P, He S, Zhou A, Lv G, Guo J, Zhou J, et al. Vaccination with toxofilin DNA in combination with an alum-monophosphoryl lipid A mixed adjuvant induces significant protective immunity against Toxoplasma gondii. BMC Infect Dis. 2017;17:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Poteet E, Lewis P, Li F, Zhang S, Gu J, Chen C, et al. A Novel Prime and Boost Regimen of HIV Virus-Like Particles with TLR4 Adjuvant MPLA Induces Th1 Oriented Immune Responses against HIV. PLoS One. 2015;10:e0136862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Dong W, Bhide Y, Marsman S, Holtrop M, Meijerhof T, de Vries-Idema J, et al. Monophosphoryl Lipid A-Adjuvanted Virosomes with Ni-Chelating Lipids for Attachment of Conserved Viral Proteins as Cross-Protective Influenza Vaccine. Biotechnol J. 2018;13:e1700645. [DOI] [PubMed] [Google Scholar]
- [47].Ko EJ, Lee YT, Lee Y, Kim KH, Kang SM. Distinct Effects of Monophosphoryl Lipid A, Oligodeoxynucleotide CpG, and Combination Adjuvants on Modulating Innate and Adaptive Immune Responses to Influenza Vaccination. Immune Netw. 2017;17:326–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Wang Y, Su L, Morin MD, Jones BT, Whitby LR, Surakattula MM, et al. TLR4/MD-2 activation by a synthetic agonist with no similarity to LPS. Proc Natl Acad Sci U S A. 2016;113:E884–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Ishizaka ST, Hawkins LD. E6020: a synthetic Toll-like receptor 4 agonist as a vaccine adjuvant. Expert Rev Vaccines. 2007;6:773–84. [DOI] [PubMed] [Google Scholar]
- [50].Heeke DS, Lin R, Rao E, Woo JC, McCarthy MP, Marshall JD. Identification of GLA/SE as an effective adjuvant for the induction of robust humoral and cell-mediated immune responses to EBV-gp350 in mice and rabbits. Vaccine. 2016;34:2562–9. [DOI] [PubMed] [Google Scholar]
- [51].Coler RN, Baldwin SL, Shaverdian N, Bertholet S, Reed SJ, Raman VS, et al. A synthetic adjuvant to enhance and expand immune responses to influenza vaccines. PLoS One. 2010;5:e13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Bertholet S, Ireton GC, Ordway DJ, Windish HP, Pine SO, Kahn M, et al. A defined tuberculosis vaccine candidate boosts BCG and protects against multidrug-resistant Mycobacterium tuberculosis. Sci Transl Med. 2010;2:53ra74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Nkolola JP, Cheung A, Perry JR, Carter D, Reed S, Schuitemaker H, et al. Comparison of multiple adjuvants on the stability and immunogenicity of a clade C HIV-1 gp140 trimer. Vaccine. 2014;32:2109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Visan L, Sanchez V, Kania M, de Montfort A, de la Maza LM, Ausar SF. Phosphate substitution in an AlOOH - TLR4 adjuvant system (SPA08) modulates the immunogenicity of Serovar E MOMP from Chlamydia trachomatis. Hum Vaccin Immunother. 2016;12:2341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Evans JT, Cluff CW, Johnson DA, Lacy MJ, Persing DH, Baldridge JR. Enhancement of antigen-specific immunity via the TLR4 ligands MPL adjuvant and Ribi.529. Expert Rev Vaccines. 2003;2:219–29. [DOI] [PubMed] [Google Scholar]
- [56].Dupont J, Altclas J, Lepetic A, Lombardo M, Vazquez V, Salgueira C, et al. A controlled clinical trial comparing the safety and immunogenicity of a new adjuvanted hepatitis B vaccine with a standard hepatitis B vaccine. Vaccine. 2006;24:7167–74. [DOI] [PubMed] [Google Scholar]
- [57].Vasilakos JP, Tomai MA. The use of Toll-like receptor 7/8 agonists as vaccine adjuvants. Expert Rev Vaccines. 2013;12:809–19. [DOI] [PubMed] [Google Scholar]
- [58].Bagnoli F, Fontana MR, Soldaini E, Mishra RP, Fiaschi L, Cartocci E, et al. Vaccine composition formulated with a novel TLR7-dependent adjuvant induces high and broad protection against Staphylococcus aureus. Proc Natl Acad Sci U S A. 2015;112:3680–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Wang Q, Barry MA, Seid CA, Hudspeth EM, McAtee CP, Heffernan MJ. 3M-052 as an adjuvant for a PLGA microparticle-based Leishmania donovani recombinant protein vaccine. J Biomed Mater Res B Appl Biomater. 2018;106:1587–94. [DOI] [PubMed] [Google Scholar]
- [60].Wille-Reece U, Flynn BJ, Lore K, Koup RA, Kedl RM, Mattapallil JJ, et al. HIV Gag protein conjugated to a Toll-like receptor 7/8 agonist improves the magnitude and quality of Th1 and CD8+ T cell responses in nonhuman primates. Proc Natl Acad Sci U S A. 2005;102:15190–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Feng Y, Forsell MN, Flynn B, Adams W, Lore K, Seder R, et al. Chemical cross-linking of HIV-1 Env for direct TLR7/8 ligand conjugation compromises recognition of conserved antigenic determinants. Virology. 2013;446:56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Francica JR, Lynn GM, Laga R, Joyce MG, Ruckwardt TJ, Morabito KM, et al. Thermoresponsive Polymer Nanoparticles Co-deliver RSV F Trimers with a TLR-7/8 Adjuvant. Bioconjug Chem. 2016;27:2372–85. [DOI] [PubMed] [Google Scholar]
- [63].Van Hoeven N, Fox CB, Granger B, Evers T, Joshi SW, Nana GI, et al. A Formulated TLR7/8 Agonist is a Flexible, Highly Potent and Effective Adjuvant for Pandemic Influenza Vaccines. Sci Rep. 2017;7:46426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Keller CD. Imiquimod to treat basal cell and squamous cell carcinomas. Am Fam Physician. 2005;72:41. [PubMed] [Google Scholar]
- [65].Berman B, Wolf J. The role of imiquimod 3.75% cream in the treatment of external genital warts. Skin Therapy Lett. 2012;17:5–7. [PubMed] [Google Scholar]
- [66].Park H, Adamson L, Ha T, Mullen K, Hagen SI, Nogueron A, et al. Polyinosinic-polycytidylic acid is the most effective TLR adjuvant for SIV Gag protein-induced T cell responses in nonhuman primates. J Immunol. 2013;190:4103–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Klinman DM, Klaschik S, Sato T, Tross D. CpG oligonucleotides as adjuvants for vaccines targeting infectious diseases. Adv Drug Deliv Rev. 2009;61:248–55. [DOI] [PubMed] [Google Scholar]
- [68].Krieg AM. CpG motifs in bacterial DNA and their immune effects. Annu Rev Immunol. 2002;20:709–60. [DOI] [PubMed] [Google Scholar]
- [69].Klinman DM, Xie H, Little SF, Currie D, Ivins BE. CpG oligonucleotides improve the protective immune response induced by the anthrax vaccination of rhesus macaques. Vaccine. 2004;22:2881–6. [DOI] [PubMed] [Google Scholar]
- [70].Jones TR, Obaldia N 3rd, Gramzinski RA, Charoenvit Y, Kolodny N, Kitov S, et al. Synthetic oligodeoxynucleotides containing CpG motifs enhance immunogenicity of a peptide malaria vaccine in Aotus monkeys. Vaccine. 1999;17:3065–71. [DOI] [PubMed] [Google Scholar]
- [71].Near KA, Stowers AW, Jankovic D, Kaslow DC. Improved immunogenicity and efficacy of the recombinant 19-kilodalton merozoite surface protein 1 by the addition of oligodeoxynucleotide and aluminum hydroxide gel in a murine malaria vaccine model. Infect Immun. 2002;70:692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Halperin SA, Van Nest G, Smith B, Abtahi S, Whiley H, Eiden JJ. A phase I study of the safety and immunogenicity of recombinant hepatitis B surface antigen co-administered with an immunostimulatory phosphorothioate oligonucleotide adjuvant. Vaccine. 2003;21:2461–7. [DOI] [PubMed] [Google Scholar]
- [73].Cooper CL, Davis HL, Morris ML, Efler SM, Adhami MA, Krieg AM, et al. CPG 7909, an immunostimulatory TLR9 agonist oligodeoxynucleotide, as adjuvant to Engerix-B HBV vaccine in healthy adults: a double-blind phase I/II study. J Clin Immunol. 2004;24:693–701. [DOI] [PubMed] [Google Scholar]
- [74].Shafique M, Wilschut J, de Haan A. Induction of mucosal and systemic immunity against respiratory syncytial virus by inactivated virus supplemented with TLR9 and NOD2 ligands. Vaccine. 2012;30:597–606. [DOI] [PubMed] [Google Scholar]
- [75].Demento SL, Bonafe N, Cui W, Kaech SM, Caplan MJ, Fikrig E, et al. TLR9-targeted biodegradable nanoparticles as immunization vectors protect against West Nile encephalitis. J Immunol. 2010;185:2989–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Cheng WK, Plumb AW, Lai JC, Abraham N, Dutz JP. Topical CpG Oligodeoxynucleotide Adjuvant Enhances the Adaptive Immune Response against Influenza A Infections. Front Immunol. 2016;7:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Fang Y, Rowe T, Leon AJ, Banner D, Danesh A, Xu L, et al. Molecular characterization of in vivo adjuvant activity in ferrets vaccinated against influenza virus. J Virol. 2010;84:8369–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Schillie S, Harris A, Link-Gelles R, Romero J, Ward J, Nelson N. Recommendations of the Advisory Committee on Immunization Practices for Use of a Hepatitis B Vaccine with a Novel Adjuvant. MMWR Morb Mortal Wkly Rep. 2018;67:455–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Hyer R, McGuire DK, Xing B, Jackson S, Janssen R. Safety of a two-dose investigational hepatitis B vaccine, HBsAg-1018, using a toll-like receptor 9 agonist adjuvant in adults. Vaccine. 2018;36:2604–11. [DOI] [PubMed] [Google Scholar]
- [80].Holbrook BC, D'Agostino RB Jr., Tyler Aycock S, Jorgensen MJ, Hadimani MB, Bruce King S, et al. Adjuvanting an inactivated influenza vaccine with conjugated R848 improves the level of antibody present at 6months in a nonhuman primate neonate model. Vaccine. 2017;35:6137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Burdette DL, Monroe KM, Sotelo-Troha K, Iwig JS, Eckert B, Hyodo M, et al. STING is a direct innate immune sensor of cyclic di-GMP. Nature. 2011;478:515–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Iurescia S, Fioretti D, Rinaldi M. Targeting Cytosolic Nucleic Acid-Sensing Pathways for Cancer Immunotherapies. Front Immunol. 2018;9:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Landi A, Law J, Hockman D, Logan M, Crawford K, Chen C, et al. Superior immunogenicity of HCV envelope glycoproteins when adjuvanted with cyclic-di-AMP, a STING activator or archaeosomes. Vaccine. 2017;35:6949–56. [DOI] [PubMed] [Google Scholar]
- [84].Hanson MC, Crespo MP, Abraham W, Moynihan KD, Szeto GL, Chen SH, et al. Nanoparticulate STING agonists are potent lymph node-targeted vaccine adjuvants. J Clin Invest. 2015;125:2532–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Van Dis E, Sogi KM, Rae CS, Sivick KE, Surh NH, Leong ML, et al. STING-Activating Adjuvants Elicit a Th17 Immune Response and Protect against Mycobacterium tuberculosis Infection. Cell Rep. 2018;23:1435–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Takaki H, Takashima K, Oshiumi H, Ainai A, Suzuki T, Hasegawa H, et al. cGAMP Promotes Germinal Center Formation and Production of IgA in Nasal-Associated Lymphoid Tissue. Med Sci (Basel). 2017;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Junkins RD, Gallovic MD, Johnson BM, Collier MA, Watkins-Schulz R, Cheng N, et al. A robust microparticle platform for a STING-targeted adjuvant that enhances both humoral and cellular immunity during vaccination. J Control Release. 2018;270:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Tregoning JS, Russell RF, Kinnear E. Adjuvanted influenza vaccines. Hum Vaccin Immunother. 2018;14:550–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Peek LJ, Middaugh CR, Berkland C. Nanotechnology in vaccine delivery. Adv Drug Deliv Rev. 2008;60:915–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Zhao L, Seth A, Wibowo N, Zhao CX, Mitter N, Yu C, et al. Nanoparticle vaccines. Vaccine. 2014;32:327–37. [DOI] [PubMed] [Google Scholar]
- [91].Yassine HM, Boyington JC, McTamney PM, Wei CJ, Kanekiyo M, Kong WP, et al. Hemagglutinin-stem nanoparticles generate heterosubtypic influenza protection. Nat Med. 2015;21:1065–70. [DOI] [PubMed] [Google Scholar]
- [92].Sliepen K, Han BW, Bontjer I, Mooij P, Garces F, Behrens AJ, et al. Structure and immunogenicity of a stabilized HIV-1 envelope trimer based on a group-M consensus sequence. Nat Commun. 2019;10:2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Aliprantis AO, Yang RB, Mark MR, Suggett S, Devaux B, Radolf JD, et al. Cell activation and apoptosis by bacterial lipoproteins through toll-like receptor-2. Science. 1999;285:736–9. [DOI] [PubMed] [Google Scholar]
- [94].Takeuchi O, Kawai T, Muhlradt PF, Morr M, Radolf JD, Zychlinsky A, et al. Discrimination of bacterial lipoproteins by Toll-like receptor 6. Int Immunol. 2001;13:933–40. [DOI] [PubMed] [Google Scholar]
- [95].Sastry M, Zhang B, Chen M, Joyce MG, Kong WP, Chuang GY, et al. Adjuvants and the vaccine response to the DS-Cav1-stabilized fusion glycoprotein of respiratory syncytial virus. PLoS One. 2017;12:e0186854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Cui W, Joshi NS, Liu Y, Meng H, Kleinstein SH, Kaech SM. TLR4 ligands lipopolysaccharide and monophosphoryl lipid a differentially regulate effector and memory CD8+ T Cell differentiation. J Immunol. 2014;192:4221–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Rhee EG, Kelley RP, Agarwal I, Lynch DM, La Porte A, Simmons NL, et al. TLR4 ligands augment antigen-specific CD8+ T lymphocyte responses elicited by a viral vaccine vector. J Virol. 2010;84:10413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Dubois Cauwelaert N, Desbien AL, Hudson TE, Pine SO, Reed SG, Coler RN, et al. The TLR4 Agonist Vaccine Adjuvant, GLA-SE, Requires Canonical and Atypical Mechanisms of Action for TH1 Induction. PLoS One. 2016;11:e0146372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Coler RN, Bertholet S, Moutaftsi M, Guderian JA, Windish HP, Baldwin SL, et al. Development and characterization of synthetic glucopyranosyl lipid adjuvant system as a vaccine adjuvant. PLoS One. 2011;6:e16333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Gavin AL, Hoebe K, Duong B, Ota T, Martin C, Beutler B, et al. Adjuvant-enhanced antibody responses in the absence of toll-like receptor signaling. Science. 2006;314:1936–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Wang L, Shi W, Joyce MG, Modjarrad K, Zhang Y, Leung K, et al. Evaluation of candidate vaccine approaches for MERS-CoV. Nat Commun. 2015;6:7712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Ni Eidhin DB, O'Brien JB, McCabe MS, Athie-Morales V, Kelleher DP. Active immunization of hamsters against Clostridium difficile infection using surface-layer protein. FEMS Immunol Med Microbiol. 2008;52:207–18. [DOI] [PubMed] [Google Scholar]
- [103].Krieg AM, Yi AK, Matson S, Waldschmidt TJ, Bishop GA, Teasdale R, et al. CpG motifs in bacterial DNA trigger direct B-cell activation. Nature. 1995;374:546–9. [DOI] [PubMed] [Google Scholar]
- [104].Prantner D, Perkins DJ, Lai W, Williams MS, Sharma S, Fitzgerald KA, et al. 5,6-Dimethylxanthenone-4-acetic acid (DMXAA) activates stimulator of interferon gene (STING)-dependent innate immune pathways and is regulated by mitochondrial membrane potential. J Biol Chem. 2012;287:39776–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Wu J, Sun L, Chen X, Du F, Shi H, Chen C, et al. Cyclic GMP-AMP is an endogenous second messenger in innate immune signaling by cytosolic DNA. Science. 2013;339:826–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Levie K, Leroux-Roels I, Hoppenbrouwers K, Kervyn AD, Vandermeulen C, Forgus S, et al. An adjuvanted, low-dose, pandemic influenza A (H5N1) vaccine candidate is safe, immunogenic, and induces cross-reactive immune responses in healthy adults. J Infect Dis. 2008;198:642–9. [DOI] [PubMed] [Google Scholar]
- [107].Caillet C, Piras F, Bernard MC, de Montfort A, Boudet F, Vogel FR, et al. AF03-adjuvanted and non-adjuvanted pandemic influenza A (H1N1) 2009 vaccines induce strong antibody responses in seasonal influenza vaccine-primed and unprimed mice. Vaccine. 2010;28:3076–9. [DOI] [PubMed] [Google Scholar]
- [108].McKee AS, Marrack P. Old and new adjuvants. Curr Opin Immunol. 2017;47:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Marrack P, McKee AS, Munks MW. Towards an understanding of the adjuvant action of aluminium. Nat Rev Immunol. 2009;9:287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.