Abstract
Immunoglobulin G4-related disease (IgG4) is an immune-mediated fibro-inflammatory entity which affects multiple organs, most frequently the pancreas. Although extrapancreatic inflammations are commonly seen in 18F-fluorodeoxyglucose positron emission tomography/computed tomography of majority of these patients at follow-up, simultaneous involvement of the gastric/biliary tract at presentation is rare. Here, we present imaging findings of a patient who presented with obstructive jaundice and initially thought to be due to cholangiocarcinoma, but was subsequently diagnosed as an IgG4-related inflammation.
Keywords: Cholangitis, fluorodeoxyglucose, gastritis, immunoglobulin G4, jaundice, pancreas, pancreatitis, positron emission tomography/computed tomography
62 year old male presented with complaints of weight loss, jaundice, and generalized itching for 1 month. Liver function tests on evaluation read as total bilirubin – 19.3 mg/dl (n – 0.1–1.2 mg/dl), direct bilirubin – 17.2 mg/dl (n< 0.3 mg/dl), serum glutamic-oxaloacetic transaminase – 78 IU/L (n – 8–33), serum glutamic-pyruvic transaminase – 56 IU/L (n – 4–36), gamma glutamyl transferase – 48 IU/L (n – 5–40), alkaline phosphatase 236 IU/L (n – 20–130), serum amylase 208 U/L (n – 0–95), and lipase 1240 U/L (n – 23–300). 18 F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) scan was done for a suspected diagnosis of cholangiocarcinoma on the basis of ultrasonography elsewhere. On intra-venous contrast enhancement CT, circumferential wall thickening with enhancement was noted in the common bile duct/peri-ampullary region, enlarged sausage-shaped tail of pancreas with homogenous enhancement and peripheral rim of low attenuation was noted and wall thickening in the antropyloric region of the stomach was noted [black arrows, Figure 1a, c and e]. The gall bladder was not distended, and there was no evidence of any significant dilatation of the intrahepatic biliary radicles or main pancreatic duct. On fused 18 F-FDG PET/CT images, there was increased FDG uptake noted in the common bile duct stricture (maximum standardized uptake value [SUVmax] – 7.20), tail of the pancreas (SUVmax– 4.72), and stomach wall thickening (SUVmax– 4.23) [white arrows Figure 1b, d and f, respectively]. Rest of the whole-body scan was unremarkable [Figure 2]. Based on these atypical findings, a diagnosis of immunoglobulin G4-related disease (IgG4-RD) was suggested, and subsequently done serum IgG4 levels were found to be elevated: 219 mg/dl (normal <135 mg/dl). Upper gastrointestinal endoscopy was done; ampullary biopsy was suggestive of dense lymphoplasmacytic infiltrate and was negative for any malignancy [Figure 3]. The patient subsequently improved symptomatically with a serial decline in bilirubin levels postendoscopic retrograde cholangiopancreatography stenting and medical management with steroids.
Figure 1.
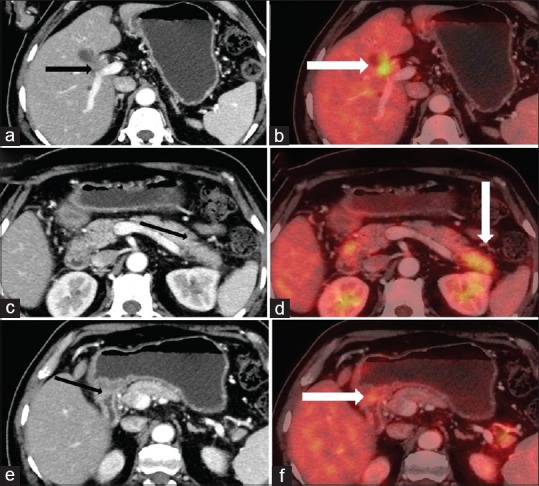
Computed tomography and positron emission tomography/computed tomography images showing cholangitis (a and b), pancreatitis (c and d), and gastritis (e and f)
Figure 2.
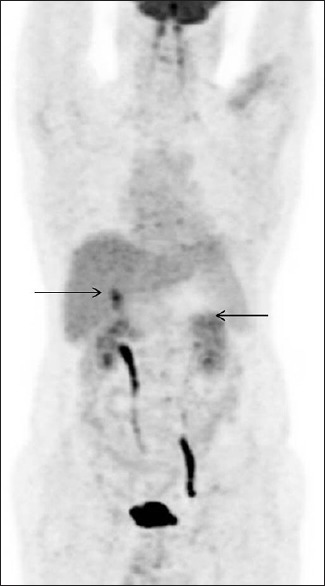
Maximum intensity projection image showing increased fluorodeoxyglucose uptake in the common bile duct and distal pancreas
Figure 3.
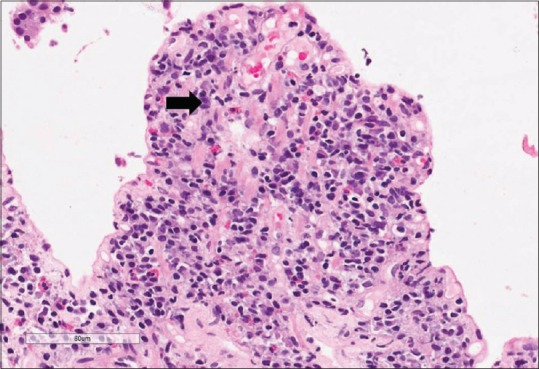
Hematoxylin and eosin stain (high power, ×400) of ampullary biopsy suggestive of dense plasmacytic infiltrate
The diagnosis of IgG4-RD (often masquerading as malignancy) is complex and based on a combination of clinical, immunological, and histological findings. Clinical findings suggestive of IgG4-RD include clinical history (such as abdominal pain, jaundice, and weight loss), physical examination (jaundice, exophthalmos, enlarged salivary glands/thyroid etc.), and characteristic imaging findings. Immunological findings include IgG4 levels in serum >135 mg/dl. Histological findings are considered as gold standard for diagnosis and include lymphoplasmacytic infiltration with storiform fibrosis and obliterative phlebitis.[1] The clinical manifestations are very variable resulting from the effect of inflammation-induced pseudotumors in the affected site. Of the affected sites encountered in this disease, the most common organ described is the pancreas which has characteristic CT imaging findings.[2] Extrapancreatic involvement of bile ducts is common and usually seen at follow-up or rarely may be seen at presentation.[3] Studies have also shown that IgG4-positive plasma cells have also been found to be significantly elevated in gastric mucosa in patients with auto-immune pancreatitis.[4,5]
The last decade has seen an increased utilization of 18 F-FDG PET/CT for diagnosis and follow-up of this disease. 18 F-FDG PET/CT appears to be especially useful with doubtful/atypical clinical/conventional imaging findings, especially when serum levels of IgG4 levels are not elevated.[6,7,8] PET/CT can aid in improving the pathological diagnosis by guiding biopsy from the most accessible and metabolically active component of the disease.[9] A prospective study done by Zhang et al. showed that whole-body18 F-FDG PET/CT imaging identifies additional organ involvement in 71% of the cases compared to conventional physical examination and CT scans.[10]
The simultaneous occurrence of pancreatic and extrapancreatic inflammation presented in this report establishes the systemic nature of IgG4-RD, re-emphasizing the need of whole-body PET imaging in this rare but increasingly recognized auto-immune disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lang D, Zwerina J, Pieringer H. IgG4-related disease: Current challenges and future prospects. Ther Clin Risk Manag. 2016;12:189–99. doi: 10.2147/TCRM.S99985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Obiorah IE, Henao Velasquez A, Özdemirli M. The clinicopathologic spectrum of igG4-related disease Balkan Med J. 2018;35:292–300. doi: 10.4274/balkanmedj.2018.0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirano K, Shiratori Y, Komatsu Y, Yamamoto N, Sasahira N, Toda N, et al. Involvement of the biliary system in autoimmune pancreatitis: A follow-up study. Clin Gastroenterol Hepatol. 2003;1:453–64. doi: 10.1016/s1542-3565(03)00221-0. [DOI] [PubMed] [Google Scholar]
- 4.Shinji A, Sano K, Hamano H, Unno H, Fukushima M, Nakamura N, et al. Autoimmune pancreatitis is closely associated with gastric ulcer presenting with abundant IgG4-bearing plasma cell infiltration. Gastrointest Endosc. 2004;59:506–11. doi: 10.1016/s0016-5107(03)02874-8. [DOI] [PubMed] [Google Scholar]
- 5.Uehara T, Hamano H, Kawa S, Sano K, Oki K, Kobayashi Y, et al. Chronic gastritis in the setting of autoimmune pancreatitis. Am J Surg Pathol. 2010;34:1241–9. doi: 10.1097/PAS.0b013e3181ec07ee. [DOI] [PubMed] [Google Scholar]
- 6.Mittal B, Parihar A, Kumar R, Singh H, Bhattacharya A. IgG4 related disease spectrum and 18F-FDG PET/CT: Where does it fit in the management algorithm? J Nucl Med. 2018;59(Suppl 1):60. [Google Scholar]
- 7.Nakatani K, Nakamoto Y, Togashi K. Utility of FDG PET/CT in IgG4-related systemic disease. Clin Radiol. 2012;67:297–305. doi: 10.1016/j.crad.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Parihar AS, Singh H, Kumar R, Gupta V, Singh H, Mittal BR. Pancreatic malignancy or not.: Role of 18F-FDG PET/CT in solving the diagnostic dilemma and evaluating treatment response? Clin Nucl Med. 2018;43:e115–e117. doi: 10.1097/RLU.0000000000001989. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen VX, De Petris G, Nguyen BD. Usefulness of PET/CT imaging in systemic IgG4-related sclerosing disease. A report of three cases. JOP. 2011;12:297–305. [PubMed] [Google Scholar]
- 10.Zhang J, Chen H, Ma Y, Xiao Y, Niu N, Lin W, et al. Characterizing IgG4-related disease with 18 F-FDG PET/CT: A prospective cohort study. Eur J Nucl Med Mol Imaging. 2014;41:1624–34. doi: 10.1007/s00259-014-2729-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


