Abstract
Past literature suggests that Certificate of Need (CON) regulations for cardiac care were ineffective in improving quality, but less is known about the effect of CON on patient costs. We analyzed Medicare data for 1991-2002 to test whether states that dropped CON experienced changes in costs or reimbursements for coronary artery bypass graft (CABG) surgery or percutaneous coronary interventions (PCI). We found that states that dropped CON experienced lower costs per patient for CABG, but not for PCI. Average Medicare reimbursement was lower for both procedures in states that dropped CON. The cost savings from removing CON regulations slightly exceed the total fixed costs of new CABG facilities that entered after deregulation. Assuming continued cost savings past 2002, the savings from deregulating CABG surgery outweigh the fixed costs of new entry. Thus, CON regulations for CABG may not be justified in terms of either improving quality or controlling cost growth.
Keywords: Certificate of Need, CABG, PCI, panel data methods
INTRODUCTION
Policy makers and researchers have debated the merits and disadvantages of state Certificate of Need (CON) programs for many years. In 1974, federal law authorized funding for CON programs, which were adopted to curb needless duplication of services and consequent excess capacity.(Conover & Sloan, 1998) Providers in states that did not implement a CON program were ineligible to receive funds under the Public Health Service Act for the development, expansion, or support of health resources. The federal law supporting CON expired in 1986, leading many states to discontinue their CON programs. Yet 34 states retained CON for at least one service in 2010 (American Health Planning Association, 2010).
The debate over CON regulations for open heart surgery and cardiac catheterization has been particularly contentious, because acute cardiac care is viewed as highly profitable (Pallarito, 1998; Swartz, 2004). Currently 25 states maintain CON regulations for open heart surgery, and 26 states regulate PCI. Past research found that states that dropped cardiac CON regulations in the late 1990s experienced a 15.2 percent increase in the number of hospitals performing coronary artery bypass graft surgery (CABG) and a 12.1 percent rise in the number of hospitals performing percutaneous coronary interventions (PCI) (Ho, Ku-Goto, & Jollis, 2009). More than half of this increased entry occurred in the year that CON regulations were removed and one year after. The higher hospital entry rates prevailed as many as five years after the removal of these regulations. However, the total number of procedures statewide was unaffected by the removal of CON, so that average procedure volume per hospital fell.
These findings regarding the redistribution of cardiac care among hospitals after the removal of CON regulations, along with other past research, can be used to construct a conceptual framework for understanding how CON regulations might influence the costs and quality of cardiac care. Given that past studies have found that hospitals performing higher numbers of complex procedures have better outcomes (Halm, Lee, & Chassin, 2002), many were concerned that lower average procedure volume resulting from cardiac CON removal would lead to worse outcomes for patients. However, two recent studies find no evidence that CON regulations are associated with better patient outcomes for CABG, and one of these studies reaches the same conclusion for PCI.(Ho et al., 2009; Cutler, Huckman, & Kolstad, 2010).
These findings suggest that CON regulations may only be justified if they effectively control cost growth, or improve quality in a manner not captured by mortality statistics. Increased competition associated with the removal of CON regulations may influence both the costs and quality of cardiac care. More competition in the market for acute myocardial infarction (AMI) patients has been associated with higher quality and lower costs per patient (Kessler, 2007). Greater competition from removal of CON laws may have raised quality by lowering post-surgical complications, which are costly to remedy (Dimick et al., 2004). New competition after cardiac CON removal may also have led providers to deliver care at lower costs, in an effort to charge lower prices that would attract more patients. Although the previous statement suggests that CON removal would encourage adoption of lower cost technologies, it is also possible that added competition may have caused hospitals to adopt more advanced and costly technologies in a medical arms race (Devers, Brewster, & Casalino, 2003). Broader studies of CON regulations suggest that the laws have slowed the diffusion of some costly medical technologies, but not all (Conover & Sloan, 1998).
While the effects of increased competition on the marginal costs of patient treatment are ambiguous, fixed costs are unambiguously higher with the entry of additional hospitals to the cardiac care market after CON removal. The fixed costs of opening a new cardiac surgery program have been estimated to be $12 to $14 million, and the costs for a new cardiac catheterization laboratory that is required to perform PCI is approximately $2.7 million (Robinson, Nash, Moxey, & O’Connor, 2001; Huckman, 2006). In addition, if there are economies of scale in the provision of CABG or PCI, then the decline in average hospital volume after deregulation could raise costs per patient.
We currently lack knowledge on the relationship between CON regulations and unit patient costs. Most prior studies have examined the association between CON regulations and hospital spending for all patients, not just those receiving cardiac care. Two of these studies concluded that the regulations have been ineffective in controlling growth in hospital spending (Lanning, Morrisey, & Oshfedlt, 1991; Conover & Sloan, 1998), although a more recent study suggests that CON regulations may have reduced expenditures by 2 percent (Hellinger, 2009). However, these studies examined hospital expenditures or healthcare expenditures per capita; i.e. total expenditures in a state divided by the state’s population. Thus, these studies did not distinguish between changes in average cost per procedure performed, versus changes in the number of patients in the state receiving treatment. For example, costs per patient treated may have been lower in states with CON laws; but this cost savings could be masked if states with CON laws also treated more patients. A more detailed study of the removal of CON regulations for nursing homes found no association between CON repeal and either Medicaid nursing home expenditures or utilization (Grabowski, Ohsfeldt, & Morrisey, 2003).
Another prior study specifically examined the association between cardiac CON regulations and per patient costs for CABG and PCI (Ho, 2007). This study concluded that CON lowered patient costs, because hospitals in CON states treated more cardiac patients, and higher patient volume was associated with lower mean costs. However, this study mixed cost changes for states that dropped CON in the mid-1980s with those of states that dropped cardiac CON regulations more than 10 years afterwards. If technology for cardiac surgery has improved over time, then the blending of cost changes that resulted after CON removal, but along different points of the technology continuum, may yield misleading results.
This study tests whether states that dropped CON between 1995 and 1998 experienced a change in average costs or reimbursements for providing CABG or PCI to Medicare patients. We focus specifically on cardiac care to reduce heterogeneity in patient casemix when examining the relationship between regulation and resource utilization. Cardiac care is worthy of attention, given that 1.3 million PCI procedures and 253,000 CABG operations were performed in 2006, and coronary heart disease hospital costs reached $56.6 billion in 2010.(Lloyd-Jones et al., 2010)
We examine cost changes in terms of both hospitals’ reported costs, as well as Medicare reimbursements, which reflect the cost to the taxpayer treatments provided to the elderly. This paper compares states’ experiences before versus after removal of cardiac CON regulations. We compare trends in costs and reimbursements per cardiac patient for states that dropped CON, with states that maintained CON throughout the sample period. In doing so, we are better able to control for changes in resource utilization, which are contemporaneous with the removal of CON, but unrelated to the regulations. The cost per patient treated could be influenced by a volume-cost effect, changes in costs resulting from greater competition, or changes in quality associated with CON that influence costs. We attempt to examine each of these hypotheses.
The results have important implications for regulators, who seek to determine the advantages and disadvantages of CON regulation. By examining both the changes in unit costs of cardiac care and the fixed costs of these procedures, we can determine whether the CON regulations increase or decrease the total costs of patient treatment.
NEW CONTRIBUTION
This study compares the experience of states that lifted cardiac CON regulations in the mid 1990s to those that maintained CON, providing the most rigorous examination to date of the cost implications of CON. Unlike previous studies, we are also able to evaluate the aggregate cost implications of cardiac CON, taking into account both direct patient costs and the fixed costs of building new facilities. The results can be combined with previous literature on the association between cardiac CON regulations and patient outcomes, in order to make policy recommendations regarding whether cardiac CON programs should be maintained or discontinued.
METHODS
We obtained data for Medicare beneficiaries ages 65 and over who received CABG surgery or PCI (including stents) between 1991 and 2002 from the CMS MedPAR files. The specific ICD-9-CM codes for these procedures were defined previously.(Ho et al., 2009) If multiple admissions for CABG or PCI occurred, all admits are included in the sample. Patients were counted once for both PCI and CABG if they received both during a hospital stay, but multiple occurrences of the same type of revascularization during the same hospital stay were not counted.
We use this data to estimate regressions of the following general form:
where Costijt is the average cost per stay for patient i in hospital j in year t. Regressions with average reimbursement per patient stay as the dependent variable are also estimated. Patient costs were estimated by multiplying total charges in the MedPAR claims by hospital- and year-specific cost-to-charge ratios derived from Medicare cost reports. The hospital cost-to-charge ratio was calculated excluding outpatient service cost centers. Reimbursement was estimated by summing the Medicare DRG price (including patient copyaments and deductibles), any outlier payments, and the “pass through” amount. The pass through amount compensates hospitals for capital related costs, direct medical education costs, bad debt, and kidney acquisition costs if applicable. Costs and reimbursements were adjusted to reflect 2002 dollars using the all-urban consumer price index. Patients were excluded from the analysis sample if 1) their estimated costs were less than $1,000 or greater than $500,000, or 2) if the reported DRG prices exceeded $200,000 and the outlier amount equaled 0, or 3) reported reimbursement was lower than $1,000, or 4) the reported charge was less than the reported outlier amount. All of these criteria were assumed to reflect coding errors, except for costs exceeding $500,000. We do not have sufficient data to model these extremely high cost patients.
The explanatory variable of interest CON droppedit is whether the patient is treated in a period after the removal of state CON regulations for cardiac care. CON droppedit is set equal to 1 in the year when CON regulations are lifted in a state and in all subsequent years. The variable takes a value of 0 in years prior to the removal of CON and for all years in states that maintained CON regulations through 2002. Information on CON status for open-heart surgery and PCI were obtained from a survey of state health departments by the American Health Planning Agency (AHPA) that was described previously (Ho, Ross, Nallamothu, & Krumholz, 2007). Seven states DE, ND, NE, NV, OH, OR, and PA) dropped CON for open-heart surgery during the sample period, and they did so in a narrow time period (1995-1998). Six of these states simultaneously dropped CON for cardiac catheterization.
States were generally considering the removal of CON regulations in this period, because of evidence that CON was unsuccessful in controlling aggregate cost growth, combined with the view that managed care growth was more effective in controlling overutilization (Conover & Sloan, 1998; Maruca, 2012). This sentiment was conveyed in a report commissioned by the Delaware General Assembly prior to its removal of CON regulation in 1996 (Cost Containment Committee for the Delaware Health Care Commission, 1996). Pennsylvania dropped its CON more by accident, when its legislative session ended before the state Senate finished making adjustments the program’s reauthorization bill (Moore Jr & ., 1997). We were unable to locate any reports documenting reasons that other states removed cardiac CON rules in this time period.
To control for possible economies of scale in the performance of complex procedures, the number of CABG or PCI procedures performed by the admitting hospital during the year the patient was treated (Volumejt) was included as an explanatory variable in the patient-level regressions. We excluded patients treated in hospitals with <3 procedures a year because of miscoding concerns.
Several variables Xijt were included in the patient-level regressions for risk adjustment including sex, age, race, estimated median household income based on income by zip code in the U.S. Census, comorbidities, indicators for acute myocardial infarction (AMI) at admission, transfer or urgent/emergent cases, and CABG- and PCI- specific treatments (e.g. cardiac catheterization or PCI on the same data as CABG). Detailed definitions of these variables have been provided previously (Ho et al., 2009).
A number of hospital and market level variables Zijt are also included in the regressions. The percent of the population with managed care insurance in the patient’s county of residence is included as an explanatory variable, because higher managed care penetration has been associated with lower costs (Chernew, Hirth, Sonnad, Ermann, & Fendrick, 1998). This data was drawn from the annual HMO Census conducted by Health Leaders - Interstudy. A Herfindahl index of market concentration based on the sum of the market shares squared for each hospital performing either CABG or PCI in the patient’s hospital referral region (HRR) is included to account for the possible association between market competition and costs (Kessler & McClellan, 2000). Previous studies have also defined markets based on HRRs (Carey, Burgess, & Young, 2009). The regressions include a relative measure of hospital wages, because labor costs comprise a large portion of overall costs. The natural log of the Center for Medicare and Medicaid Services (CMS) inpatient prospective payment wage index for each hospital and year is used. This wage index varies by core based statistical areas (CBSAs) defined by the Office of Management and Budget. To allow for the possibility that hospitals that enter the market after CON regulations are lifted may have costs that differ from those of incumbents, an indicator variable for entrants is included in the regressions. The regressions include year fixed effects (τt), state fixed effects (θs), and a patient-specific error term εijt.
We also test whether any observed variation in health events during hospitalization are consistent with our findings regarding the relationship between CON regulations and costs. We examine length of stay for CABG and PCI hospitalizations, as well as recognized complications for these operations in the literature. The complications for CABG surgery are atrial fibrillation, cardiac arrest, renal failure, and stroke (Speir, Kasirajan, Barnett, & Fonner E Jr, 2009; Tarakji, Sabik, III, Bhudia, Batizy, & Blackstone, 2011). The necessity of performing CABG after hospitalization for PCI is viewed as a complication for the latter procedure (Jollis et al., 1994).
Statistical Analysis
Mean hospital procedure volumes and costs for CABG and PCI by year and whether states maintained cardiac CON or dropped the regulations during the sample period are graphed to illustrate unadjusted differences in the data by CON status. Multivariable regressions are used to estimate the association between CON status and costs, reimbursements, and returns, adjusting for covariates. Separate regressions were estimated for CABG and PCI.
We only include data from the seven states that dropped CON during the sample period, the 27 states that maintained CON for open-heart surgery, and the 25 states that maintained CON for PCI through 2002. In doing so, we obtain a direct comparison of trends in states that dropped cardiac CON regulations versus those that maintained CON. We compare the before-versus-after resource utilization of states that dropped CON during the sample period, to the contemporaneous experience of states that maintained CON. Changes in resource utilization in states that maintained CON serve as a control group for factors unrelated to CON that influenced outcomes in all states. The regressions also include state-level fixed effects. Therefore, the coefficient on the CON variable provides a within-state measurement of the association between dropping CON and the dependent variables of interest.
To test whether the effects of dropping CON change over time, we estimate additional regressions interacting CON with indicator variables for whether a patient was treated in a state 1 year before CON was dropped, the year CON was dropped, 1 year after, 2 years after, or 3 or more years after CON was dropped. Testing for an effect the year before CON regulations are dropped serves as a consistency check. We should find no significant association between dropping CON and resource utilization the year preceding the lifting of CON regulations. The regressions are estimated in Stata 10.0. The standard errors are adjusted to account for the clustering of patients within hospitals.(Wooldridge, 2003)
RESULTS
After excluding 2,772 CABG and 41,014 PCI observations based on the criteria defining outliers described above, the sample contained data on 1,428,105 CABG and 1,723,783 PCI procedures. Table 1 reports mean values of the dependent and independent variables at the start of the sample (1991) and the end (2002). Figure 1 graphs both the mean procedure volume and costs for CABG and PCI for states that maintained cardiac CON regulations through 2002, and those states that dropped the regulations during the study period.
Table 1:
Mean Costs, Hospital Volume, Patient and Market Characteristics in 1991 and 2002 by CON status
| CABG |
||||||
|---|---|---|---|---|---|---|
| Dropped CON in 1995-1998 |
Kept CON |
|||||
| 1991 | 2002 | % change 1991-2002 | 1991 | 2002 | % change 1991-2002 | |
| Cost per patient | 48310 | 27148 | −43.8 | 46265 | 28822 | −37.7 |
| Annual hospital volume | 343 | 265 | −22.7 | 308 | 319 | 3.5 |
| Age | 72.016 | 74.583 | 3.6 | 72.199 | 74.215 | 2.8 |
| Female | 0.355 | 0.365 | 2.8 | 0.351 | 0.353 | 0.6 |
| Income, (patient’s zipcode) | 23314 | 24997 | 7.2 | 24465 | 26013 | 6.3 |
| Black | 0.024 | 0.028 | 16.7 | 0.034 | 0.055 | 61.8 |
| Other nonwhite race | 0.053 | 0.020 | −62.3 | 0.046 | 0.029 | −37.0 |
| Transferred from other hospital | 0.260 | 0.195 | −25.0 | 0.212 | 0.193 | −9.0 |
| Admitted from ER | 0.153 | 0.196 | 28.1 | 0.193 | 0.191 | −1.0 |
| Emergency admission | 0.304 | 0.282 | −7.2 | 0.303 | 0.263 | −13.2 |
| Urgent admission | 0.285 | 0.235 | −17.5 | 0.268 | 0.275 | 2.6 |
| Same day PCI | 0.015 | 0.008 | −46.7 | 0.014 | 0.007 | −50.0 |
| Same day cardiac cath | 0.059 | 0.066 | 11.9 | 0.065 | 0.070 | 7.7 |
| Prior balloon angioplasty | 0.019 | 0.021 | 10.5 | 0.011 | 0.020 | 81.8 |
| Principal diagnosis of AMI | 0.113 | 0.205 | 81.4 | 0.139 | 0.203 | 46.0 |
| HIV and AIDS | 0.000 | 0.000 | 0.0 | 0.000 | 0.000 | 0.0 |
| Alcohol abuse | 0.003 | 0.004 | 33.3 | 0.002 | 0.006 | 200.0 |
| Rheumatoid arthritis | 0.006 | 0.009 | 50.0 | 0.005 | 0.009 | 80.0 |
| Anemia deficiency | 0.024 | 0.051 | 112.5 | 0.025 | 0.051 | 104.0 |
| Blood loss | 0.006 | 0.009 | 50.0 | 0.007 | 0.010 | 42.9 |
| Congestive heart failure | 0.021 | 0.038 | 81.0 | 0.020 | 0.035 | 75.0 |
| Chronic pulmonary disease | 0.078 | 0.091 | 16.7 | 0.071 | 0.092 | 29.6 |
| Coagulation deficiency | 0.004 | 0.008 | 100.0 | 0.004 | 0.009 | 125.0 |
| Depression | 0.004 | 0.021 | 425.0 | 0.005 | 0.019 | 280.0 |
| Diabetes w/o chronic comp | 0.127 | 0.143 | 12.6 | 0.110 | 0.140 | 27.3 |
| Diabetes w/ chronic comp | 0.035 | 0.026 | −25.7 | 0.039 | 0.027 | −30.8 |
| Drug abuse | 0.000 | 0.000 | 0.0 | 0.000 | 0.001 | N.A. |
| Hypertension | 0.210 | 0.302 | 43.8 | 0.197 | 0.304 | 54.3 |
| Hypothyroidism | 0.018 | 0.045 | 150.0 | 0.015 | 0.043 | 186.7 |
| Liver disease | 0.001 | 0.002 | 100.0 | 0.001 | 0.003 | 200.0 |
| Lymphoma | 0.001 | 0.002 | 100.0 | 0.001 | 0.002 | 100.0 |
| Fluid and electrolyte disorders | 0.052 | 0.057 | 9.6 | 0.057 | 0.059 | 3.5 |
| Metastatic cancer | 0.001 | 0.002 | 100.0 | 0.002 | 0.002 | 0.0 |
| Other neurological disorders | 0.008 | 0.011 | 37.5 | 0.007 | 0.012 | 71.4 |
| Obesity | 0.013 | 0.025 | 92.3 | 0.011 | 0.023 | 109.1 |
| Paralysis | 0.003 | 0.005 | 66.7 | 0.003 | 0.006 | 100.0 |
| Peripheral vascular disease | 0.052 | 0.061 | 17.3 | 0.046 | 0.064 | 39.1 |
| Psychoses | 0.002 | 0.005 | 150.0 | 0.002 | 0.004 | 100.0 |
| Pulmonary circ disorders | 0.000 | 0.003 | N.A. | 0.000 | 0.002 | N.A. |
| Renal failure | 0.012 | 0.023 | 91.7 | 0.012 | 0.023 | 91.7 |
| Solid tumor w/o metastasis | 0.006 | 0.010 | 66.7 | 0.005 | 0.009 | 80.0 |
| Chronic peptic ulcer disease | 0.001 | 0.001 | 0.0 | 0.001 | 0.000 | −100.0 |
| Valvular disease | 0.014 | 0.032 | 128.6 | 0.012 | 0.026 | 116.7 |
| Weight loss | 0.001 | 0.003 | 200.0 | 0.001 | 0.003 | 200.0 |
| New Post-CON Facility | 0.000 | 0.139 | N.A. | 0.000 | 0.000 | 0.0 |
| Ln(Labor Costs) | 0.004 | −0.025 | −725.0 | −0.019 | −0.008 | −57.9 |
| HMO penetration | 0.165 | 0.240 | 45.5 | 0.146 | 0.232 | 58.9 |
| Hospital Market Concentration | 0.444 | 0.364 | −18.0 | 0.488 | 0.450 | −7.8 |
| N | 21,863 | 77,982 | 21,881 | 92,104 | ||
| PCI |
||||||
| Dropped CON in 1995-1998 |
Kept CON |
|||||
| 1991 | 2002 | % change 1991-2002 | 1991 | 2002 | % change 1991-2002 | |
| Cost per patient | 18294 | 12342 | −32.5 | 18235 | 12711 | −30.3 |
| Annual hospital volume | 268 | 468 | 74.5 | 279 | 605 | 117.2 |
| Age | 71.918 | 75.007 | 4.3 | 72.158 | 74.781 | 3.6 |
| Female | 0.437 | 0.433 | −0.9 | 0.433 | 0.430 | −0.7 |
| Income, (patient’s zipcode) | 23202 | 25037 | 7.9 | 24504 | 26038 | 6.3 |
| Black | 0.030 | 0.037 | 23.3 | 0.039 | 0.063 | 61.5 |
| Other nonwhite race | 0.046 | 0.022 | −52.2 | 0.045 | 0.030 | −33.3 |
| Transferred from other hospital | 0.248 | 0.189 | −23.8 | 0.205 | 0.191 | −6.8 |
| Admitted from ER | 0.207 | 0.276 | 33.3 | 0.246 | 0.272 | 10.6 |
| Emergency admission | 0.356 | 0.351 | −1.4 | 0.356 | 0.343 | −3.7 |
| Urgent admission | 0.297 | 0.271 | −8.8 | 0.267 | 0.299 | 12.0 |
| Coronary stent insertion | 0.000 | 0.864 | N.A. | 0.000 | 0.857 | N.A. |
| Principal diagnosis of AMI | 0.200 | 0.281 | 40.5 | 0.220 | 0.275 | 25.0 |
| HIV and AIDS | 0.000 | 0.000 | 0.0 | 0.000 | 0.000 | 0.0 |
| Alcohol abuse | 0.002 | 0.004 | 100.0 | 0.003 | 0.005 | 66.7 |
| Rheumatoid arthritis | 0.008 | 0.012 | 50.0 | 0.008 | 0.013 | 62.5 |
| Anemia deficiency | 0.026 | 0.062 | 138.5 | 0.026 | 0.062 | 138.5 |
| Blood loss | 0.007 | 0.010 | 42.9 | 0.006 | 0.010 | 66.7 |
| Congestive heart failure | 0.015 | 0.046 | 206.7 | 0.014 | 0.047 | 235.7 |
| Chronic pulmonary disease | 0.071 | 0.111 | 56.3 | 0.076 | 0.114 | 50.0 |
| Coagulation deficiency | 0.003 | 0.011 | 266.7 | 0.005 | 0.012 | 140.0 |
| Depression | 0.006 | 0.031 | 416.7 | 0.006 | 0.027 | 350.0 |
| Diabetes w/o chronic comp | 0.114 | 0.156 | 36.8 | 0.108 | 0.159 | 47.2 |
| Diabetes w/ chronic comp | 0.033 | 0.031 | −6.1 | 0.036 | 0.030 | −16.7 |
| Drug abuse | 0.000 | 0.001 | N.A. | 0.001 | 0.001 | 0.0 |
| Hypertension | 0.220 | 0.347 | 57.7 | 0.208 | 0.353 | 69.7 |
| Hypothyroidism | 0.023 | 0.057 | 147.8 | 0.019 | 0.054 | 184.2 |
| Liver disease | 0.001 | 0.003 | 200.0 | 0.001 | 0.003 | 200.0 |
| Lymphoma | 0.001 | 0.002 | 100.0 | 0.001 | 0.002 | 100.0 |
| Fluid and electrolyte disorders | 0.054 | 0.067 | 24.1 | 0.059 | 0.071 | 20.3 |
| Metastatic cancer | 0.003 | 0.003 | 0.0 | 0.002 | 0.003 | 50.0 |
| Other neurological disorders | 0.009 | 0.017 | 88.9 | 0.009 | 0.017 | 88.9 |
| Obesity | 0.019 | 0.029 | 52.6 | 0.013 | 0.028 | 115.4 |
| Paralysis | 0.004 | 0.006 | 50.0 | 0.003 | 0.008 | 166.7 |
| Peripheral vascular disease | 0.042 | 0.069 | 64.3 | 0.038 | 0.069 | 81.6 |
| Psychoses | 0.004 | 0.005 | 25.0 | 0.003 | 0.006 | 100.0 |
| Pulmonary circ disorders | 0.000 | 0.002 | N.A. | 0.000 | 0.003 | N.A. |
| Renal failure | 0.013 | 0.028 | 115.4 | 0.011 | 0.028 | 154.5 |
| Solid tumor w/o metastasis | 0.006 | 0.012 | 100.0 | 0.005 | 0.012 | 140.0 |
| Chronic peptic ulcer disease | 0.002 | 0.000 | −100.0 | 0.001 | 0.001 | 0.0 |
| Valvular disease | 0.006 | 0.019 | 216.7 | 0.007 | 0.020 | 185.7 |
| Weight loss | 0.001 | 0.005 | 400.0 | 0.001 | 0.004 | 300.0 |
| New Post-CON Facility | 0.000 | 0.166 | N.A. | 0.056 | 0.057 | 1.8 |
| Ln(Labor Costs) | 0.003 | −0.029 | −1066.7 | −0.026 | −0.007 | −73.1 |
| HMO penetration | 0.165 | 0.238 | 44.2 | 0.140 | 0.232 | 65.7 |
| Hospital Market Concentration | 0.390 | 0.347 | −11.0 | 0.499 | 0.449 | −10.0 |
| N | 16,693 | 62,798 | 37,062 | 177,355 | ||
Figure 1:
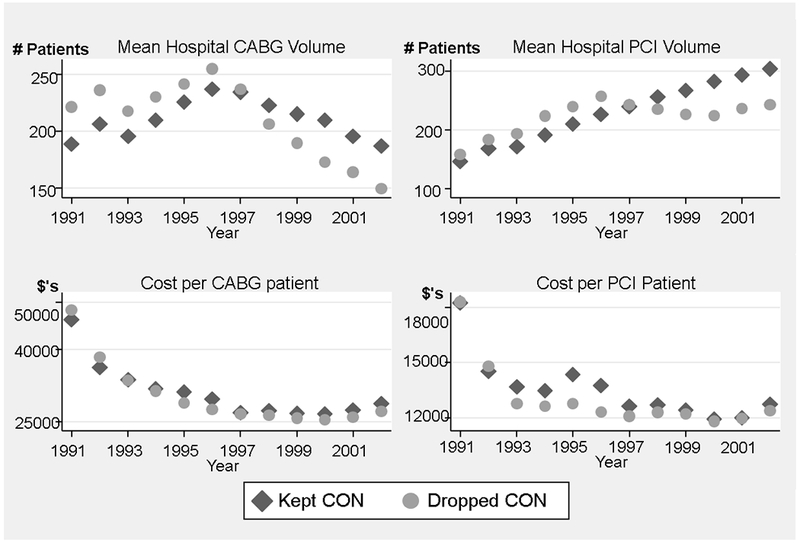
Mean Procedure Volume and Patient Cost by CON Status
For both CABG and PCI, mean hospital volume peaks in 1996 for states that dropped cardiac CON regulations between 1995 and 1998. For both CABG and PCI, mean hospital volume in 1998 for these states falls below that for states that maintained CON; and remains lower through 2002. For both CABG and PCI, mean costs fell substantially in the early 1990’s. Mean costs seem to be higher in states that dropped CON for most years from 1995 onwards for CABG and 1993 onwards for PCI. But there are no striking patterns coinciding with the lifting of CON regulations, as was observed for trends in hospital volume. Table 2 presents estimates of the association between CON status and both costs and Medicare reimbursements. The dependent variables in the cost and reimbursement regressions are expressed in natural logs, so that the coefficients represent percent changes associated with a unit increase in the explanatory variables. Columns 1 and 2 report cost regression results excluding hospital fixed effects. Both of these columns suggest that lifting CON is associated with an approximately 2% decrease in costs per patient, but the effect is not precisely estimated. However, Column 3, which includes fixed effects, indicates that removing CON is associated with a 4.2% (p=0.013) decline in cost per CABG. These results suggest that the fixed effects capture systematic differences in costs across hospitals that are not measured by the other covariates, and their omission biased the estimated effect of lifting CON towards zero.
Table 2:
Regression Estimates of the Association between CON and CABG Patient Costs and Medicare Reimbursement
| ln(Cost) | ln(Reimbursement) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | |
| After CON dropped | −0.023 (−1.00) | −0.017 (−1.13) | −0.042* (−2.50) | −0.038* (−2.32) | −0.049* (−2.05) | −0.056 (−1.42) | −0.084** (−7.22) | ||
| 1 year before CON dropped | −0.018 (−1.13) | −0.019 (−1.46) | |||||||
| year CON dropped | −0.023 (−1.18) | −0.058** (−3.32) | |||||||
| 1 year after CON dropped | −0.021 (−1.21) | −0.117** (−5.24) | |||||||
| 2 years after CON dropped | −0.049* (−2.32) | −0.144** (−6.32) | |||||||
| 3+ years after CON dropped | −0.063** (−2.72) | −0.072** (−4.47) | |||||||
| New Post-CON Facility | −0.111 (−1.54) | −0.102 (−1.86) | −0.055 (−1.11) | −0.095 (−1.73) | −0.034 (−1.45) | −0.083 (−1.75) | −0.094* (−2.00) | ||
| ln(Hospital Volume) | −0.046** (−3.17) | −0.055** (−3.62) | −0.046** (−2.88) | −0.046** (−2.88) | 0.003 (0.30) | −0.017 (−1.59) | −0.027** (−2.67) | −0.027** (−2.69) | |
| ln(Labor Costs) | 0.706** (11.44) | 0.835** (8.20) | 0.811** (7.83) | 0.833** (8.16) | 0.993** 17.19 | 0.923** (12.37) | 0.924** (12.36) | ||
| HMO Penetration | −0.213** (−3.36) | −0.134** (−2.81) | −0.158** (−3.19) | −0.137** (−2.85) | −0.100 (−1.49) | −0.108** (−1.95) | −0.103 (−1.86) | ||
| Hospital Market Concentration | −0.036 (−1.21) | −0.017 (−0.49) | −0.032 (−0.95) | −0.017 (−0.50) | −0.045** (−1.65) | −0.039 (−1.75) | −0.039 (−1.74) | ||
| Other Controlsa | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Fixed Effects | No | No | Yes | Yes | Yes | No | No | Yes | Yes |
Other controls include indicator variables for each sample year, sex, age, race, transfer patient, urgent and emergent admissions, principal diagnosis of AMI, Elixhauser comorbidities, as well as income, a constant, and state-level fixed effects. CABG regressions also include indicators for same-day PCI, same-day cardiac catheterization, and use of an intra-aortic balloon pump on the day prior to CABG. Sample size = 1,428,105
p-value≤.05
p-value≤.01
This estimate changes only slightly and remains precisely estimated when hospital procedure volume for CABG is excluded from the regression in Column 4. Thus, economies of scale do not appear to play an important role in explaining cost changes associated with deregulation. The estimates in Column 5 suggest that the lower patient costs associated with CON removal only become tangible 2 or more years after the regulations are removed. The fixed effects estimates in Column 8 suggest that lifting CON is also associated with an 8.4% (p<0.001) decline in Medicare reimbursements per CABG patient. Column 9’s estimates suggest that the negative association between CON removal and reimbursements begins in the year CON is lifted and persists 3+ years afterwards.
Table 3 contains regression estimates of the association between CON removal and costs for PCI procedures. We find no significant association between removing CON and patient costs in any of the specifications in Columns 1 through 5. The estimates in Columns 6 and 7 find no significant association between CON removal and Medicare reimbursements per patient. However, the fixed effect estimates in Column 8 suggest that CON removal is associated with 4.3% (p<0.001) lower mean Medicare reimbursements for PCI, and the negative association is precisely estimated for each individual year listed in Column 9. However, the estimates in column 9 indicate that mean reimbursements were 2.5% lower (p=0.007) one year prior to CON removal, suggesting that these effects may not be attributable solely to removal of the regulations. PCI facilities that entered the market after CON had reimbursements that were an additional 7.4% (p=0.03) lower than for existing hospitals.
Table 3:
Regression Estimates of the Association between CON and PCI Patient Costs and Reimbursement
| ln(Cost) | ln(Reimbursement) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | |
| after CON dropped | 0.008 (0.34) | −0.015 (−0.64) | 0.015 (0.73) | 0.019 (0.96) | 0.007 (0.23) | −0.020 (−1.41) | −0.043** (−4.67) | ||
| 1 year before CON dropped | −0.021 (−1.00) | −0.025** (−2.69) | |||||||
| year CON dropped | −0.003 (−0.12) | −0.045** (−4.36) | |||||||
| 1 year after CON dropped | 0.020 (0.79) | −0.063** (−4.34) | |||||||
| 2 years after CON dropped | 0.022 (0.82) | −0.075** (−5.87) | |||||||
| 3+ years after CON dropped | 0.003 (0.13) | −0.049** (−3.87) | |||||||
| New Post-CON facility | −0.005 (−0.13) | −0.029 (−0.50) | 0.008 (0.14) | −0.026 (−0.44) | −0.035 (−0.66) | −0.071* (−2.06) | −0.074* (−2.18) | ||
| PCI Volume | −0.0008** (−4.96) | −0.0006** (−3.93) | −0.0005** (−3.78) | −0.0005** (−3.74) | 9.03e-05 (−0.78) | 1.17e-05 (−0.14) | −0.00005 (−0.63) | −0.00005 (−0.69) | |
| PCI Volume2 | 8.38e-07** (3.22) | 6.61e-07** (2.78) | 6.26e-07** (2.66) | 6.23e-07** (2.63) | −1.91e-07 (−1.19) | −1.23e-07 (−1.07) | −4.58e-08 (−0.43) | −4.01e-08 (−0.38) | |
| PCI Volume3 | −2.51e-10* (−2.59) | −2.17e-10* (−2.47) | −1.97e-10** (−2.23) | −1.96e-10* (−2.19) | 8.07e-11 (1.40) | 5.64e-11 (−1.41) | 3.16e-11 (0.90) | 2.97e-11 (0.84) | |
| ln(Labor Costs) | 0.295** (2.83) | 0.435** (3.98) | 0.423** (3.78) | 0.434** (3.97) | 1.026 (21.96) | 0.945** (15.17) | 0.945** (15.15) | ||
| HMO Penetration | −0.241** (−3.36) | −0.104 (−1.62) | −0.101 (−1.51) | −0.106 (−1.63) | −0.035 (−0.92) | −0.041 (−1.23) | −0.039 (−1.17) | ||
| Hospital Market Concentration | −0.041 (−1.21) | −0.035 (−1.01) | −0.049 (−1.40) | −0.035 (−1.01) | −0.046 (−2.19) | −0.046* (−2.27) | −0.046* (−2.26) | ||
| Other Controlsa | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Fixed Effects | No | No | Yes | Yes | Yes | No | No | Yes | Yes |
Other controls include indicator variables for each sample year, sex, age, race, transfer patient, urgent and emergent admissions, principal diagnosis of AMI, Elixhauser comorbidities, as well as income, a constant, and state-level fixed effects. PCI regressions also include indicators for multivessel PCI and coronary stent placement. NOTE: Sample size = 1,723,783
p-value≤.05
p-value≤.01
Specification tests indicated that log(Volume) provided a better fit for the CABG regressions, while a polynomial of Volume to the third power was more appropriate for the PCI regressions (Wooldridge, 2000). In both cases, higher hospital volume was associated with lower costs per patient. The remaining coefficients in the regressions in Tables 1 and 2 generally behave as hypothesized. Costs for hospitals that enter states after open heart CON regulations are lifted are not significantly different from those for existing hospitals. However, post-regulation entrants appear to collect lower mean Medicare reimbursements. Higher labor costs are associated with both higher costs and reimbursements per patient. Greater HMO penetration is associated with both lower costs and reimbursements per patient for CABG. Yet HMO penetration does not influence these variables for PCI. We found no association between hospital market concentration and patient costs for either CABG or PCI. When hospital market concentration was removed from the regressions, the coefficients on the CON variables remained virtually unchanged.
We estimated two alternate types of specifications of the regressions reported in Tables 1 and 2 which we do not present due to space constraints. First, we re-estimated the cost and reimbursement regressions for CABG and PCI with state random effects instead of fixed effects. In each case, a Hausman specification test rejected the null hypothesis that the random effects yielded consistent coefficient estimates.
Second, we considered whether the effects of lifting CON were similar across states. Among the seven states that removed CON for open heart surgery and the six states that lifted CON for cardiac catheterization, 99,276 Ohio patients received CABG, and more patients received PCI. Pennsylvania had even more of both patient types. We re-estimated the fixed effect cost and reimbursement regressions and interacted CON droppedit with one of these states. Unlike the estimates for all states combined, we could not reject the hypothesis that Ohio CABG patients experienced zero change in costs after CON regulations were lifted. However, Pennsylvania CABG patient costs were still lower after CON regulations were lifted. Pennsylvania’s costs per PCI patient dropped more than other states’ after removing CON, while Ohio’s change in costs were not significantly different from zero. As was reported for all states combined, reimbursements dropped in Ohio (2.8 percent, p=.012), and in Pennsylvania (8.8 percent, p<0.001). These estimates suggest that the effects of lifting CON regulations were stronger in Pennsylvania than in Ohio. We did not estimate similar regressions for the other states, because the patient numbers were much smaller. Ohio and Pennsylvania patients outnumbered those in other individual states by a factor of at least four.
Table 4 examines the association between CON regulations and both length of stay and common complications for CABG and PCI patients. Lifting CON is associated with shorter lengths of stay and fewer strokes during admission for CABG patients. In additional regressions that are not reported in Table 4, we examined the association between CON removal and three other well recognized CABG complications (cardiac arrest, renal failure, and atrial fibrillation). Lifting CON had no significant association with these three other complications. We also found no significant association between lifting CON for cardiac catheterization and either length of stay or the need for CABG after PCI for PCI patients.
Table 4:
Regression Estimates of the Association between CON and Length of Stay and Complications for CABG and PCI
| CABG | PCI | |||
|---|---|---|---|---|
| Length of Stay (1) |
Stroke (2) |
Length of Stay (3) |
CABG after PCI (4) |
|
| After CON dropped | −0.294 (−1.62) | −0.103* (−2.15) | 0.083 −0.86 | 0.108 −1.54 |
| New Post-CON Facility | −0.971**(−3.08) | 0.043 0.41 | 0.015 (0.1) | −0.153 (−1.12) |
| PCI Volume | −0.0008 (−1.73) | 0.0002 −0.82 | ||
| PCI Volume2 | 2.37E-07 −0.38 | −7.60E-07 (−1.67) | ||
| PCI Volume3 | 8.14E-11 −0.36 | 2.54E-10 −1.32 | ||
| Ln(Hospital Volume) | −0.078 (−0.81) | 0.01 −0.55 | ||
| HMO Penetration | −1.267* (−2.54) | 0.241* 2.31 | −0.457* (−2.29) | 0.148 −1.05 |
| Hospital Market Concentration | −0.886** (−4.11) | −0.005 (−0.11) | −0.289** (−2.86) | −0.029 (−0.40) |
Regressions include indicator variables for each sample year, sex, age, race, transfer patient, urgent and emergent admissions, principal diagnosis of AMI, Elixhauser comorbidities, as well as income, a constant, and state-level fixed effects. CABG regressions also include indicators for same-day PCI, same-day cardiac catheterization, and use of an intra-aortic balloon pump on the day prior to CABG. PCI regressions also include indicators for multivessel PCI and coronary stent placement.
Sample Size = 1,428,105
p-value≤.05
p-value≤.01
We can combine the results of our regression analysis with other data to estimate the aggregate cost impact of removing CON regulations. We first compute the mean costs per CABG patient by year for states with CON regulations. We then calculate the estimated 4.2 % cost savings per patient implied by Table 2. These cost savings are then multiplied by the number of patients treated in each state and year after open heart surgery CON regulations were removed. Our sample includes only patients age 65+, so we adjust these numbers proportionately to account for CABG patients under age 65 using data by age and year reported in the Agency for Healthcare Research and Quality’s online HCUPnet system (http://hcupnet.ahrq.gov/) The total cost savings are estimated to be $248.6 million in 2002 dollars. We do not have data on the number of CABG patients treated beyond 2002. But assuming that costs per CABG patient continue to be lower in states that repealed CON for open heart surgery beyond 2002, then the overall cost savings of removing these regulations will be even larger.
Past research estimates that lifting open heart surgery CON regulations is associated with a 15.2% increase in the number of hospitals performing CABG (Ho et al., 2009). During the sample period, 115 hospitals performed CABG in the years that states dropped CON for open heart surgery. A 15.2% increase in the number of hospitals performing CABG therefore implies 18 additional new facilities. The previous literature’s estimates of the fixed costs for a new CABG facility range from $12 million to $14 million in year 2000 dollars. Taking a mean of $13 million, adjusting this value to 2002 dollars, and multiplying by 18 new facilities suggests that the aggregate fixed costs for building new CABG facilities is $244.5 million in 2002 dollars. The total cost savings in patient care from lifting CON regulations through 2002 are slightly larger than the fixed costs of the new facilities that enter the market after deregulation. Assuming these cost savings continued past 2002, the savings from removing CON regulation for CABG outweigh the fixed costs associated with new entry.
DISCUSSION
We find that removal of cardiac CON regulations is associated with a reduction in mean patient costs for CABG surgery. Why might this relationship occur? A recent study of hospital discharge data in Pennsylvania concluded that CABG operations were redistributed to higher quality surgeons after CON for open heart surgery was removed in that state in 1996 (Cutler et al., 2010). The authors suggest that the relative desirability of high quality surgeons improves after CON removal, as more hospitals enter the market for open heart surgery and compete for patients. As an entrant’s share of CABG patients in an HRR rose from zero to 10 percent, the average high-quality surgeon (top 10 percent of surgeons based on risk-adjusted mortality) gained 2.6 percentage points of local market share. This reallocation represents a sizeable 53 percent increase (relative to the mean) for high versus standard quality surgeons.
Our Medicare data does not contain identifiers for the surgeon operating on each patient, so we cannot directly test the hypothesis that operations were reallocated to higher quality surgeons. Another valid quality measure is the number of complications experienced during hospitalization. Past research has determined that hospitals with fewer surgical complications have lower costs (Dimick et al., 2004). Thus, the removal of CON may have led to a larger portion of CABG operations being conducted by high-quality surgeons, which in turn lowered costs due to fewer surgical complications. Our finding that removal of CON is associated with both lower patient costs and fewer complications from a stroke during hospitalization are consistent with Cutler et al.’s findings. One might be concerned that lower costs for CABG patients after the removal of CON regulations is the result of a shift in patient casemix towards lower risk patients. However, past research suggests that removal of CON for open heart surgery was associated with a slight increase in casemix severity for CABG patients (Ho et al., 2009).
For PCI, we found no association between CON removal and reduced costs or complications. PCI is a more straightforward procedure than CABG, that doesn’t require a large surgical incision on the patient, and requires shorter operative time and substantially lower mortality rates. Thus, the reallocation of procedures among existing and new facilities may not tangibly influence the quality of care or resources provided to each patient.
It may also be that state regulators used CON to favor certain providers over others, leading to inefficiency in the market for open heart surgery. Campbell and Fournier found that regulators in Florida were more likely to approve CON applications for the provision of services from facilities that directed a higher proportion of their revenues to indigent care (Campbell & Fournier, 1993). These facilities may have been more inefficient than those providers who were barred from providing open heart surgery prior to the lifting of CON. However, we did not find direct evidence that hospitals that entered the open heart surgery market after CON was removed had lower costs than other providers.
Removal of CON regulations is also associated with lower Medicare reimbursements per patient for both CABG and PCI. The lower reimbursements for CABG patients occur the year that CON for open heart surgery is dropped and continue in all years afterwards. But we note with caution that lower Medicare reimbursements for PCI patients are tangible the year before CON for cardiac catheterization is dropped. Thus, there may be other (unobservable) factors that contributed to lower reimbursements for this PCI. We attempted to test for changes in the four to five most common DRGs used by hospitals for payment for CABG or PCI after CON regulations were dropped. We do not report these regressions, but we did not find any significant changes in DRG coding after CON regulations were lifted. The analysis was complicated by the fact that Medicare reclassified the DRGs involving both CABG and PCI during the sample period. The underlying reasons for lower Medicare reimbursements after the lifting of CON regulations is worthy of future study, because the cost savings to Medicare are substantial.
We find that the cost savings for direct patient care associated with removing CON regulations ($248.6 million) slightly exceed the fixed costs of new CABG facilities that entered the market after deregulation ($244.5 million). When we broke down the cost estimates by the number years after CON removal, the cost savings for CABG patients continued 3+ years after deregulation. Thus, additional cost savings for direct patient care would likely accumulate over time. These findings, combined with previous studies suggesting that CON for open heart surgery does not improve the quality of patient care, call into doubt the value of these regulations for CABG surgery. One might argue that regulating cardiac catheterization under CON may still be justified, given that we found no savings in costs per patient associated with removing these regulations. However, one must first determine why Medicare reimbursements per patient appear to be lower for PCI patients after these regulations are removed.
Some caveats remain to our analysis. One may be concerned that removal of cardiac CON regulations is endogenous. States with policy makers who had greater confidence in the ability of managed care to control costs may have been more likely to remove CON regulations. However, Figure 1 reveals that trends in costs per patient for CABG and PCI were similar in states that maintained or removed CON regulations, although there was a slight uptick in costs for PCI patients in states that retained CON in 1995 and 1996. Moreover, HMO penetration was included as an explanatory variable in the regressions to address this concern. As mentioned previously, we cannot rule out the possibility that factors other than CON removal led to lower PCI reimbursement rates, given that these rates were significantly lower in the year prior to CON removal in our sample. However, we did not find this effect in any of our regression estimates for CABG, or for estimates of factors affecting PCI costs. We only had access to Medicare Part A claims and are therefore missing information on physician costs from the Part B files. CON regulations are aimed at hospitals and not physicians. However, it would be useful to examine in future research whether CON regulations influence physician costs.
Although data for multiple admissions for some patients are in the sample, we did not adjust the standard errors for this fact. As a robustness test, we dropped patients with multiple admissions from the sample and re-estimated the regressions in Tables 2 and 3 that include the full set of explanatory variables and state fixed effects. For CABG, 2% of observations represented multiple admissions. The statistical precision of the effect of dropping CON regulations remained the same, with estimates changing only in the third decimal point. For PCI 40% of observations represented multiple admissions. Nevertheless, the effects of dropping CON were the same as for the full sample; no effect of removing CON on costs, but a significant reduction in reimbursements (changing only in the third decimal place). We also estimated a linear probability model with the same explanatory variables and state fixed effects to test whether the probability of multiple admissions for PCI changed after CON regulations were dropped, but we found no effect.
Given that CON regulations are almost 50 years old, it may be surprising that the literature has discovered several new findings regarding the impact of these regulations on patient outcomes and costs in just the last few years. Some of the recent progress is attributable to advances in computing power, which have enabled the Center for Medicare and Medicaid Services to make the entirety of their claims data more accessible to researchers. Increased computing power has also improved the sophistication of the analyses that can be applied to these data. Nevertheless, the recent findings that CON may not improve the quality of cardiac care, and that the regulations influence the cost of patient care in ways that were not predicted, should be a lesson to policy makers as they consider other major changes to the delivery of healthcare in the future.
Acknowledgments
Support was provided from a grant awarded to Dr. Ho by the National Heart, Lung, and Blood Institute (R01 HL073825-01A1).
Contributor Information
Vivian Ho, James A. Baker III Institute for Public Policy, Rice University, Department of Economics, Rice University, Dept of Medicine, Baylor College of Medicine.
Meei-Hsiang Ku-Goto, James A. Baker III Institute for Public Policy, Rice University.
Reference List
- American Health Planning Association (2010). National Directory, State Certificate of Need Programs, Health Planning Agencies, 2010. (21st ed) Falls Church, VA. [Google Scholar]
- Campbell ES & Fournier GM (1993). Certificate-of-need deregulation and indigent hospital care. Journal of Health Politics, Policy and Law, 18, 905–925. [DOI] [PubMed] [Google Scholar]
- Carey K, Burgess JF, & Young GJ (2009). Single specialty hospitals and service competition. Inquiry, 46, 162–171. [DOI] [PubMed] [Google Scholar]
- Chernew ME, Hirth RA, Sonnad SS, Ermann R, & Fendrick AM (1998). Managed care, medical technology, and health care cost growth: a review of the evidence. Medical Care Research and Review, 55, 259–288. [DOI] [PubMed] [Google Scholar]
- Conover CJ & Sloan FA (1998). Does removing Certificate-of-Need regulations lead to a surge in health care spending? Journal of Health Politics, Policy and Law, 23, 455–481. [DOI] [PubMed] [Google Scholar]
- Cost Containment Committee for the Delaware Health Care Commission (1996). Evaluation of Certificate of Need and other health planning mechanisms. Delaware: The Commission. [Google Scholar]
- Cutler DM, Huckman RS, & Kolstad JT (2010). Is entry efficient when inputs are constrained? Lessons from cardiac surgery. American Economic Journal: Economic Policy, 2, 51–76. [Google Scholar]
- Devers KJ, Brewster LR, & Casalino LP (2003). Changes in hospital competitive strategy: a new medical arms race? Health Services Research, 38, 447–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, & Campbell DA Jr. (2004). Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. Journal of the American College of Surgeons, 199, 531–537. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Ohsfeldt RL, & Morrisey MA (2003). The effects of CON repeal on Medicaid nursing home and long-term expenditures. Inquiry, 40, 146–157. [DOI] [PubMed] [Google Scholar]
- Halm EA, Lee C, & Chassin MR (2002). Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Annals of Internal Medicine, 137, 511–520. [DOI] [PubMed] [Google Scholar]
- Hellinger FJ (2009). The effect of certificate-of-need laws on hospital beds and healthcare expenditures: an empirical analysis. American Journal of Managed Care, 15, 737–744. [PubMed] [Google Scholar]
- Ho V (2007). Does Certificate of Need affect cardiac outcomes and costs? International Journal of Health Care Finance and Economics, 6, 300–324. [DOI] [PubMed] [Google Scholar]
- Ho V, Ku-Goto MH, & Jollis JG (2009). Certificate of Need (CON) for cardiac care: controversy over the contributions of CON. Health Services Research, 44, 483–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho V, Ross JS, Nallamothu BK, & Krumholz HM (2007). Cardiac Certificate of Need regulations and the availability and use of revascularization services. American Heart Journal, 154, 767–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huckman RS (2006). Hospital integration and vertical consolidation: An analysis of acquisitions in New York State. Journal of Health Economics, 25[1], 58–80. [DOI] [PubMed] [Google Scholar]
- Jollis JG et al. (1994). The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. The New England Journal of Medicine, 334, 1625–1629. [DOI] [PubMed] [Google Scholar]
- Kessler D (2007). Cost shifting in California hospitals: what is the effect on private payers? Stanford, CA: California Foundation for Commerce and Education. [Google Scholar]
- Kessler DP & McClellan MB (2000). Is hospital competition socially wasteful? The Quarterly Journal of Economics, 115, 577–615. [Google Scholar]
- Lanning JA, Morrisey MA, & Oshfedlt RL (1991). Endogenous hospital regulation and its effects on hospital and non-hospital expenditures. Journal of Regulatory Economics, 3, 137–154. [Google Scholar]
- Lloyd-Jones D et al. (2010). Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation, 121, e46–e215. [DOI] [PubMed] [Google Scholar]
- Maruca WH (1997, February). PA’s certificate of need sunset. Physician’s News Digest. Retreived from http://www.physiciansnews.com
- Moore JD Jr and . (1997, August 11). Focus report: CON survival struggle: Certificate of Need: Gone in many states but not dead yet. Modern Healthcare, 32. [PubMed] [Google Scholar]
- Pallarito K (1998, July 20). Change of heart: N.J. expansion of cardiac CONs proving controversial. Modern Healthcare, 44. [PubMed] [Google Scholar]
- Robinson JL, Nash DB, Moxey E, & O’Connor JP (2001). Certificate of need and the quality of cardiac surgery. American Journal of Medical Quality, 16, 155–160. [DOI] [PubMed] [Google Scholar]
- Speir AM, Kasirajan V, Barnett SD, & Fonner E Jr (2009). Additive costs of postoperative complications for isolated coronary artery bypass grafting patients in Virginia. Annals of Thoracic Surgery, 88, 40–45. [DOI] [PubMed] [Google Scholar]
- Swartz K (2004, April 2). Florida senate approves open-heart surgery programs. The Palm Beach Post. p.2 [Google Scholar]
- Tarakji KG, Sabik JF III, Bhudia SK, Batizy LH, & Blackstone EH (2011). Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. The Journal of the American Medical Association, 305, 381–390. [DOI] [PubMed] [Google Scholar]
- Wooldridge JM (2000). Introductory Econometrics: A Modern Approach. Mason, OH: South-Western College Publishing. [Google Scholar]
- Wooldridge JM (2003). Cluster-sample methods in applied econometrics. American Economic Review, 93, 133–138. [Google Scholar]


