Abstract
Background:
There is a longstanding interest in the field of management science to study high performance organizations. Applied to medicine, research on hospital performance indicates that some hospitals are high performing, while others are not. The objective of this study was to identify a cluster of high performing emergency general surgery (EGS) hospitals and assess whether high performance at one EGS operation was associated with high performance on all EGS operations.
Methods:
Adult patients who underwent 1 of 8 EGS operations were identified in the California State Inpatient Database (2010–2011), which we linked to the American Hospital Association database. Beta regression was used to estimate a hospital’s risk-adjusted mortality, accounting for patient- and hospital-level factors. Centroid cluster analysis grouped hospitals by patterns of mortality rates across the 8 EGS operations using z-scores. Multinomial logistic regression compared hospital characteristics by cluster.
Results:
A total of 220 acute care hospitals were included. Three distinct clusters of hospitals were defined based on assessment of mortality for each operation type: high performing hospitals (n=66), average performing (n=99), and low performing (n=55). The mortality by individual operation type at the high performing cluster was consistently at least 1.5 standard deviations better than the low performing cluster (p<0.001). Within-cluster variation was minimal at high performing hospitals compared to wide variation at low performing hospitals. A hospital’s high performance in one EGS operation type predicted high performance on all EGS operation types.
Conclusions:
High performing EGS hospitals attain excellence across all types of EGS operations, with minimal variability in mortality. Poor performing hospitals are persistently below average, even for low-risk operations. These findings suggest that top-performing EGS hospitals are highly reliable, with systems of care in place to achieve consistently superior results. Further investigation and collaboration are needed to identify the factors associated with high performance.
Level of Evidence:
Level III, Study Type Prognostic
Keywords: Emergency General Surgery, Hospital Performance, Cluster Analysis
BACKGROUND
There is a longstanding interest in the field of management science to study high performance businesses and corporations to determine what organizational advantages fuel their success (1–5). The study of these operational systems and management policies has proven crucial for the identification of effective and efficient practices, and subsequently allows for their application and dissemination to other institutions, fields and industries(6). At the core of management science is an interdisciplinary approach to solving the inherent problems of human organizations, thereby establishing how a business can best manage itself to maximize productivity, ensure effective processes, and maintain strong decision-making systems. While rooted in the understanding and practice of businesses, the foundational concepts of management science are not limited to the corporate setting – rather, they have widespread applicability to medicine and hospital performance (7–9).
Research on hospital performance across a range of procedures indicates that some hospitals are high performing, while others are not (note that in this manuscript, we refer to “hospital performance” in the context of morbidity and mortality, not in the context of profitability or patient satisfaction) (10–12). Although the exact characteristics of these high performers are varied, they include aspects of organizational culture, expertise, and interdisciplinary teamwork(13,14). In hospitals that perform urgent and emergent operations, given the challenges of time-dependent conditions and the high-acuity patient population, the importance of high-functioning organizational habits is crucial to patient outcomes (15).
With this management science framework in mind, the current study had three objectives: First, to identify a cluster of high performing emergency general surgery (EGS) hospitals based on their mortality outcomes. Second, to assess whether high performance at one EGS operation was associated with high performance on all EGS operations. And third, to determine what hospital level factors were independently associated with high performance.
METHODS
Data Source
The California State Inpatient Database (SID) was used to identify patients undergoing common EGS operations over a 2-year period (2010–2011). The SID is published as part of the Healthcare Cost and Utilization Project, itself sponsored by the Agency for Healthcare Research and Quality. The database consists of data on patients’ demographics, diagnoses, procedures, comorbidities, length of stay, and in-hospital mortality. The California hospitals identified in the SID were matched to the American Healthcare Association (AHA) Annual Survey of Hospitals database over the same two-year period. The AHA database provided in-depth hospital-level characteristics such as bed size, trauma center status and teaching center affiliation.
California was chosen due to its large, diverse population (37.7 million in 2011) as well as its heterogeneity in hospital systems, urban and rural settings, and private and academic hospital-based centers (16).
Patient Selection
Patients included for analysis were 18 years or older and underwent one of eight commonly performed EGS operations as identified by the International Classification of Disease, 9th edition (ICD-9) procedural and diagnosis codes at examined hospitals (these codes are listed in Appendix A). The examined diagnoses were specific to those associated with EGS operations; diagnoses related to trauma were excluded from this analysis. Hospitals included for analysis performed 3 or more of all eight procedures over the two-year study period. The examined operations included: laparoscopic and open appendectomy; laparoscopic and open cholecystectomy; partial and total colectomy, inguinal or ventral hernia repair, adhesiolysis, small bowel resection and repair of a perforated viscus.
We included only acute care hospitals in the analysis, and thus excluded federal hospitals such as the Veteran’s Administration (VA) Hospitals, specialty rehabilitation hospitals, and pediatric hospitals. Patients who were transferred either into or out of an examined hospital were excluded as responsibility of a transferred patient’s outcome is difficult to solely ascribe to the transferring or receiving hospital. Patients who underwent more than one procedure only had their first procedure included for analysis and were not included more than once.
Analyzed Variables
Patient variables included for analysis included gender, race, age, payer status, Van Walraven Comorbidity Score, and in-hospital mortality. The Van Walraven score is a comorbidity scale established as a modification of the Elixhauser classification system and has been validated for use with administrative datasets (17–19). Hospital variables analyzed included state designated as well as American College of Surgeons verified level I or II Trauma Center Status, total operative volume among the eight examined procedure classes, teaching center status (defined as having an affiliation to a medical school), and high technology capability (defined as performing cardiac surgery, liver transplantation, or cardiac transplant).
Statistical Methods
The statistical analysis had three parts. In Part I we performed model-based risk adjustment of the proportion of patients who died at each hospital. Modeling was done separately for each operation, thus each hospital had a risk-adjusted death rate for each of the 8 operation types. In Part II, these 8 values were then used in a cluster analysis to elucidate subgroups of hospitals with similar death rate patterns across operation types. In Part III, the set of clusters was treated as a nominal categorical outcome variable in a generalized multinomial logistic regression to explore other characteristics that differentiate the hospital clusters.
Part I: Risk-Adjusted Modeling of Mortality Rates
Using the hospital as the unit of analysis, beta-logistic generalized linear regression modeling was employed to risk-adjust hospital level mortality, separately for each of the EGS operations. The dependent variable was the hospital’s ratio of the number of deaths versus the total number of operations of a given type, which yielded proportions of patients who died at the hospital from the procedure. Beta regression is used to model a continuous dependent variable with a limited range between 0 and 1, often representing probabilities or proportions. The Beta distribution accounts for the continuous dependent proportion random variable. The logit link function enables model coefficients to be interpreted on the natural-log odds scale, which can be exponentiated to produce odds ratios. The Beta probability distribution, coupled with the logit link, adequately captures the expected sigmoidal relationship between proportion of mortality and a linear function of the predictors, and ensures proper risk-adjusted proportions will properly be within the (0, 1) range. Our model adjusted the death rates over the two-year period for hospital’s patient case mix and for hospital level institutional factors.
Part II: Cluster Analysis
We used k-means cluster analysis (i.e. centroid clustering) using the 8 adjusted hospital mortality proportions as the variables defining the clusters to identify subgroups of hospitals with similar patterns of mortality proportions across the 8 operation types. Our aim was to find a set of clusters that met statistical criteria for separation, were meaningfully differentiable, and had straightforward and useful interpretations.
The 8 outcomes were separately standardized to have mean=0 and variance=1. Having all means=0 facilitates interpretation: positive/negative values are above/below ‘average’, respectively. Having all variances=1 gives all operation types equal weight in the algorithm for the cluster solution; without standardization of variances the procedures with the highest variability among hospital rates of mortality would have undue influence on the cluster solution. We did not believe it was appropriate to prioritize any procedures to determine the clusters in this analysis. An R-squared statistic was calculated to assess the relative fit of each cluster model solution to test the performance of increasing or decreasing the number of clusters in the model. Within-cluster variation refers to the variability for each operation across the hospitals within that cluster. The wider the operation-specific mortality rate ranges across all hospitals in a cluster, the greater the within-cluster variation. Larger within-cluster variation is an indication of greater heterogeneity in standardized hospital mortality rates in that cluster compared with other clusters.
Part III: Covariates of Cluster Membership
We considered two types of covariates: those that were institutional characteristics of the hospitals (trauma center status, high technology statues, medical school affiliation, and number of beds > 100) and those that were characteristic of the patient case-mix of the hospitals (mean age at admission, mean comorbidity severity score, % gender, % race, % payer status.) Multinomial logistic regression was performed to characterize institutional hospital variables that were significantly associated with cluster assignment.
All data was analyzed using SAS 9.4 (SAS Institute, Cary, NC). A p-value of <0.05 was considered to be statistically significant. Effect sizes of continuous variables were measured with the eta-squared statistic (20) while the effect size of categorical variables was measured with Cramér’s V statistic φc (21). This study was approved by the Yale University Human Research Protection Program (HRPP) Institutional Review Board (IRB) for biomedical research, known as the Human Investigation Committee (HIC).
RESULTS
A total of 220 hospitals were included in the analysis, at which a total of 145,901 common EGS operations were performed. The breakdown of operations performed is as follows: appendectomy 47,970 (33%); cholecystectomy, 62,416 (43%); colectomy, 11,496 (8%); inguinal hernia repair, 3436 (2%); lysis of adhesions, 8467 (6%); repair of perforated viscus, 2103 (1%); small bowel resection, 6801 (5%); ventral hernia repair, 3212 (2%).
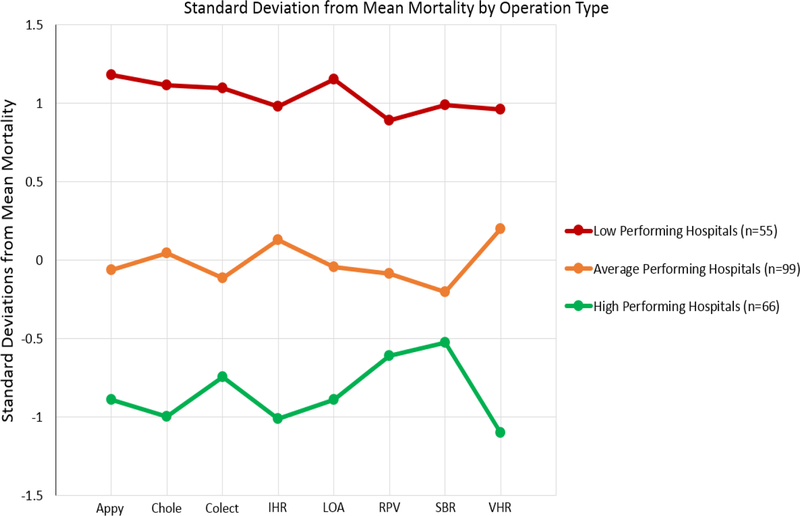
The centroid clustering model delineated three unique clusters of hospitals based on mortality performance: 30% of the hospitals were high performing (n=66), 45% were average (n=99), and 25% performed below average (n=55). Mortality by operation varied significantly between the cluster types (see Figure I). The high performing hospitals had lower mean standardized mortality rates for every operation type compared to the average and low performing hospitals. The average performing hospitals also had lower mean standardized mortality rates for every operation type compared to the low performing hospitals.
Figure I:
Standard Deviation from Mean Mortality Stratified by Operation Type
The number of standard deviations from the mean adjusted mortality (i.e. within operation type mortality ‘z-score’), when stratified by procedure, was universally worse than the mean for the poor performing cluster of hospitals, at the mean for the average performing hospitals, and better than the mean for the high performing hospitals. The high performing hospitals consistently had mortality rates 2 standard deviations better than the low performing hospitals, across every operation type.
The centroid of the clusters of hospitals that emerged indicated that performance level for one operation type was consistent with performance level across all other operation types (see Figure I). Specifically, a hospital’s high performance level in one EGS operation type was consistently observed with high performance on all other EGS operation types. Likewise, the centroids of the low performing cluster remained low performing at all eight types of operations, regardless of the complexity of the procedure performed. There was not one operation type where a centroid of the low performing cluster of hospitals was better than a corresponding centroid of the other clusters of hospitals.
The high performing hospitals demonstrated their greatest deviation below mean mortality (meaning better than the mean) among ventral hernia repair (−1.098) and least deviation from average when performing small bowel resection (−0.523). Conversely, the low performing cohort demonstrated its greatest deviation above mean mortality (meaning worse than the mean) when performing appendectomy (1.179) and its least deviation when performing repair of perforated viscus (0.889). High performing hospitals exceeded low performing hospitals by nearly 2 standard deviations across all operations with the greatest observed difference among appendectomy (−2.1), adhesiolysis (−2.1), and ventral hernia repair (−2.1). The smallest observed difference between the high and low performers occurred among repair of perforated viscus (−1.5).
Because there are 8 standardized variables in the cluster analysis, the total variance for the data is 8.00. The within-cluster variance was smallest at high performing hospitals (2.80) compared to average performing hospitals (3.75) and low performing hospitals (5.77). Further cluster specific standardized mortality by procedure types are displayed in Table I. The 3-cluster solution is easily interpretable and meaningful and explained 40.6% of the total variance (2-clusters:40.0%, 4-clusters 55.5%). Mean risk-adjusted mortality stratified by procedure type is shown in Table II.
Table I:
Procedure Specific Standard Deviation from Mean Mortality Stratified by Cluster
| Operation | Average Performing Hospitals | Low Performing Hospitals | High Performing Hospitals |
|---|---|---|---|
| Appendectomy | −0.062 | 1.179 | −0.889 |
| Cholecystectomy | 0.045 | 1.114 | −0.996 |
| Colectomy | −0.113 | 1.098 | −0.746 |
| Inguinal Hernia Repair | 0.128 | 0.981 | −1.009 |
| Adhesiolysis | −0.046 | 1.153 | −0.891 |
| Repair of Perforated Viscus | −0.087 | 0.889 | −0.610 |
| Small Bowel Resection | −0.202 | 0.990 | −0.523 |
| Ventral Hernia Repair | 0.197 | 0.962 | −1.098 |
| Within Class Variance | 5.801 | 3.694 | 2.811 |
Table II:
Procedure Specific Mean Risk-Adjusted Mortality Stratified by Procedure Type
| Operation | Low Performing Hospitals | Average Performing Hospitals | High Performing Hospitals | p-value |
|---|---|---|---|---|
| Mean risk-adjusted mortality (with SD) * NOT pt. level | ||||
| Appendectomy | 0.0083 (0.0042) | 0.0038 (0.0016) | 0.0023 (0.0008) | <0.001 |
| Cholecystectomy | 0.0146 (0.0082) | 0.0082 (0.0021) | 0.0049 (0.0010) | <0.001 |
| Colectomy | 0.1489 (0.0292) | 0.1131 (0.0181) | 0.0975 (0.0137) | <0.001 |
| Inguinal Hernia Repair | 0.0949 (0.0347) | 0.0611 (0.0223) | 0.0337 (0.0100) | <0.001 |
| Adhesion lysis | 0.0925 (0.0293) | 0.0554 (0.0144) | 0.0386 (0.0099) | <0.001 |
| Repair of Perforated Viscus | 0.2258 (0.0638) | 0.1682 (0.0471) | 0.1410 (0.0308) | <0.001 |
| Small Bowel Resection | 0.1511 (0.0388) | 0.1079 (0.0262) | 0.0977 (0.0211) | <0.001 |
| Ventral Hernia Repair | 0.1038 (0.0454) | 0.0648 (0.0232) | 0.0302 (0.0100) | <0.001 |
Hospitals level characteristics differed by cluster as demonstrated in Table III. The high performing cluster had a higher proportion of bed size > 100 compared to both average and poor performing hospitals. They also had a higher proportion of designated or certified trauma center status (38%) as compared to average performing (21%) or low performing (4%) hospitals (p<0.001). High performing hospitals also demonstrated the highest proportion of high technology capability as well as an increased proportion of affiliation with a medical school.
Table III:
Hospital Characteristics Stratified by Cluster
| N = 220 | Low Performing Hospitals (N = 55) |
Average Performing Hospitals (N = 99) |
High Performing Hospitals (N = 66) |
P Value |
|---|---|---|---|---|
| Procedure count | ||||
| N (N Missing) | 55 (0) | 99 (0) | 66 (0) | |
| Mean (SD) | 291.51 (116.10) | 577.16 (156.25) | 1101.95 (330.37) | <0.001 |
| Median (Range) | 292.0 (93.0 – 611.0) | 565.0 (269.0 – 1005.0) | 1027.0 (633.0 – 2132.0) | <0.001 |
| Trauma Center Status | ||||
| Missing | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | <0.001 |
| No | 53 (96.36%) | 78 (78.79%) | 41 (62.12%) | |
| Yes | 2 (3.64%) | 21 (21.21%) | 25 (37.88%) | |
| High Technology Hospital | ||||
| Missing | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | <0.001 |
| No | 36 (65.45%) | 24 (24.24%) | 8 (12.12%) | |
| Yes | 19 (34.55%) | 75 (75.76%) | 58 (87.88%) | |
| Medical School Affiliation | ||||
| Missing | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | <0.001 |
| Yes | 5 (9.09%) | 32 (32.32%) | 28 (42.42%) | |
| No | 50 (90.91%) | 67 (67.68%) | 38 (57.58%) | |
| More than 100 Beds | ||||
| Missing | 18 (32.73%) | 24 (24.24%) | 13 (19.70%) | <0.001 |
| No | 27 (72.97%) | 27 (36.00%) | 5 (9.43%) | |
| Yes | 10 (27.03%) | 48 (64.00%) | 48 (90.57%) | |
Individual patient characteristics also differed when stratified across performance categories (Table IV). Mean Van Walraven comorbidity scores were highest among poor performing hospitals and lowest among high performing hospitals (p<0.001). Poor performing hospitals had almost twice the proportion of black patients as high performing hospitals and were 10% less likely to treat patients with private insurance (p<0.001). High performing hospitals treated slightly younger patients while low performing hospitals treated the highest proportion of male patients. (p<0.001). Patient-level characteristics stratified across cluster type for each analyzed operation are shown in Appendix B.
Table IV:
Patient Characteristics Stratified by Cluster
| N = 145901 | Low Performing Hospitals (N = 16033) |
Average Performing Hospitals (N = 57139) |
High Performing Hospitals (N = 72729) |
P Value | Effect Size Index |
|---|---|---|---|---|---|
| Age in years at admission | |||||
| N (N Missing) | 16033 (0) | 57139 (0) | 72729 (0) | ||
| Mean (SD) | 50.33 (20.32) | 50.45 (19.87) | 49.26 (19.57) | <0.001 | 0.00 |
| Median (Range) | 49.0 (18.0 – 99.0) | 49.0 (18.0 – 99.0) | 47.0 (18.0 – 101.0) | <0.001 | |
| Van Walraven Comorbidity Score | |||||
| N (N Missing) | 16033 (0) | 57139 (0) | 72729 (0) | ||
| Mean (SD) | 2.85 (6.39) | 2.29 (5.90) | 2.00 (5.64) | <0.001 | 0.00 |
| Median (Range) | 0.0 (−14.0 – 47.0) | 0.0 (−17.0 – 46.0) | 0.0 (−16.0 – 45.0) | <0.001 | |
| Indicator of sex | |||||
| Missing | 807 | 2526 | 2232 | 0.002 | 0.01 |
| Male | 6261 (41.12%) | 23231 (42.54%) | 29471 (41.80%) | ||
| Female | 8965 (58.88%) | 31382 (57.46%) | 41026 (58.20%) | ||
| Race | |||||
| Missing | 2441 | 7230 | 6960 | <0.001 | 0.06 |
| White | 6368 (46.85%) | 26720 (53.54%) | 32411 (49.28%) | ||
| Black | 1119 (8.23%) | 2573 (5.16%) | 3039 (4.62%) | ||
| Asian | 943 (6.94%) | 3648 (7.31%) | 3896 (5.92%) | ||
| Other | 5162 (37.98%) | 16968 (34.00%) | 26423 (40.18%) | ||
| Ethnicity | |||||
| Missing | 2505 | 7453 | 7156 | <0.001 | 0.05 |
| Hispanic | 4897 (36.20%) | 16123 (32.45%) | 24886 (37.95%) | ||
| Non-Hispanic | 8631 (63.80%) | 33563 (67.55%) | 40687 (62.05%) | ||
| Payer Status | |||||
| Missing | 1 | 10 | 8 | <0.001 | 0.08 |
| Medicare | 4613 (28.77%) | 15450 (27.04%) | 17459 (24.01%) | ||
| Medicaid | 4120 (25.70%) | 9137 (15.99%) | 13901 (19.12%) | ||
| Private insurance | 4643 (28.96%) | 24665 (43.17%) | 28192 (38.77%) | ||
| Other | 2656 (16.57%) | 7877 (13.79%) | 13169 (18.11%) | ||
Multinomial logistic regression found that high technology and trauma center status had a significant impact on hospital performance. Adjusting for covariates, hospitals with trauma centers were 7.7 times more likely to be in the highest performing cluster as compared to the lowest performing cluster (Odds Ratio [OR]: 0.13, p=0.01). High technology hospitals were 4.5 times more likely to be average performing as compared to low performing (OR: 0.22, p<0.0001) and 9.0 times more likely to be high performing as compared to low performing (OR: 0.111, p<0.0001). The results for all covariates of the multinomial regression are displayed in Table V.
Table V:
Multinomial Logistic Regression Modeling Cluster Assignment
| Variable | Cluster Type | Odds Ratio | 95% CI | P-value | |
|---|---|---|---|---|---|
| Trauma Center Status | 0.02 | ||||
| Low vs. Average | 0.252 | 0.053 | 1.192 | 0.08 | |
| High vs. Average | 1.994 | 0.962 | 4.135 | 0.06 | |
| Low vs. High | 0.126 | 0.026 | 0.610 | 0.01 | |
| High Technology | <.0001 | ||||
| Low vs. Average | 0.220 | 0.105 | 0.465 | <.0001 | |
| High vs. Average | 1.990 | 0.813 | 4.868 | 0.13 | |
| Low vs. High | 0.111 | 0.042 | 0.291 | <.0001 | |
| Teaching Hospital | 0.17 | ||||
| Low vs. Average | 0.394 | 0.134 | 1.161 | 0.09 | |
| High vs. Average | 1.151 | 0.575 | 2.301 | 0.69 | |
| Low vs. High | 0.342 | 0.109 | 1.071 | 0.07 | |
DISCUSSION
Hospital mortality performance of common emergency general surgery (EGS) operations separates into three distinct clusters: high performance, average performance, and poor performance hospitals. The high performing EGS hospitals attain excellence across all types of EGS operations, with minimal variability in mortality relative to the mean. Likewise, the poorly performing cluster consistently has worse survival rates across the spectrum of EGS operations, even for relatively low-risk operations.
The clustering phenomenon suggests that top-performing EGS hospitals are highly reliable and consistent, with systems of care in place to achieve superior results. High reliability and low variability are hallmarks of high performing organizations, and are manifested as organizational systems and processes in which common culture promotes constant learning, evaluation, and communication(22). High performing hospitals also distinguish themselves on their increased levels of efficiency and ability to maximize production output which in some studies has also led to cost savings (23,24). Other characterisitics and processes of care present at high performance hospitals include access to high specialty providers or services, compliance with evidence based practices, and effective distribution of hospital based resources(25–29)
Although hospital level performance in general is continually being studied, it is unknown what aspects contribute most to high performance among emergency general surgery operations. High performance EGS requires many different aspects of a high-performance institution, mainly the ability to deal with time-dependent conditions, treat a diverse range of patients and do so in a efficient manner. The importance of determining what makes an institution high performing as well as elucidating what characteristics are associated with low performance will likely have widespread implications for the emerging public health crisis of emergency surgical care. Although our study demonstrated that low performing hospitals were more likely to have patients with higher comorbodity scores as well as a higher proportion of black or Medicaid patients, it is important to recognize that the low effect size indices indicates that these differences are so small as to likely have only a trivial effect on cluster seperation.
The present study defines the landscape of EGS hospitals by clusters of mortality-performance, and defines some hospital characteristics associated with performance status. However, the question of why this clustering phenomenon is so robust will require additional investigation. The exact hospital traits, management structures, processes of care, and decision-making systems that contribute to EGS performance are unknown. It is also unknown if the hospital attributes that contribute to its high EGS performance likewise contribute to its elective surgical performance or even to its overall hospital performance in non-surgical disciplines. Determining the true drivers of cluster seperation will likely require development of well structured qualitative research efforts able to gather and analyze more complex data than currently available for study within administrative datasets. It is unclear exactly why certain lower acuity operations, such as ventral or inguinal hernia repair, seem to discriminate performance clusters to a greater extent than higher acuity operations such as colectomy or enterectomy. One potential explanation for this observation may be that the high performance characteristics in place at top performing hospitals demonstarate an enhanced protective factor among lower acuity operations or conversely that the poor performance habits at the lowest performing cluster differentially affect lower acuity operations.
The present study suggests that areas for initial exploration into how to improve hospital wide EGS performance can be guided by the two independent factors found to influence hospital mortality: high technology status and trauma center status. High technology contributes to improved patient outcomes through several potential mechanisms. As our definition of high technology includes variables that reflect higher capability operative settings (cardiac surgery) as well as increased postoperative resuscitation capability (liver transplantation), it may be that patients at these hospitals benefit from better intraoperative care as well as better postoperative systems of care. Better ancillary provider support such as higher-level nursing or pharmacy care may also be contributing mechanisms behind this observation. Similarly, trauma center status may also reflect more experienced operative and postoperative capabilities as well as an increased capability and comfort with treating time dependent pathology. Additionally, the increased performance seen among institutions associated with trauma centers may reflect the positive benefit of matured prehospital systems of care coupled with greater Emergency Department capabilities and on-site Acute Care Surgeons.
Although most (45%) of the hospitals were average performing, there were sizeable number of both high performers (35%) and low performers (25%). The relative size of these clusters has two important implications: First, the size of the high performing cluster indicates that excellent outcomes after EGS operations are not for the elite few, as they were achieved by a third of analyzed hospitals. Second, rather than the lowest performing tier being occupied by a few “bad apples” it encompasses fully one fourth of examined hospitals. These results provide a contrast to previous studies which suggest that the highest and lowest performing hospitals across EGS operations represent less than 10% of the overall cohort (30).
The present analysis is based on valid, straightforward statistical methodology, which is a strength of our analysis. First, the analysis is appropriately an analysis of hospitals, not patients-within-hospitals. Beta-logistic regression to model proportions of deaths at the hospital level, rather than using binomial-logistic regression or Poisson regression at the patient-within-hospitals level, assigns equal weight to each hospital in the analysis. Secondly, centroid clustering is more appropriate than other clustering strategies such as hierarchical clustering, as a hierarchical structure is not theoretically justified. Thirdly, multinomial logistic regression, rather than pairwise logits, allows a simultaneous comparison of clusters using all data.
Our study has limitations. Its retrospective nature is subject to all the inherent biases in a study of this type. There may be unmeasured variables that could influence our analysis that were unaccunted for. Our study did not risk-adjust for different diagnosis codes within a procedure class (e.g. perforated vs. non-perforated appendicitis), a source of potential bias if certain hospitals were more likely to perform operations related to specific diagnosis codes than others. This study utilizes administrative data; there may be errors in variable reporting or database coding that are unaccounted for and thus may bias the results in unknown ways. Importantly, the capture of comorbidities at the time of emergency admission may be incomplete or inaccurate, possibly leading to residual confounding or bias. Differences in prehospital care specifically, although reflective of hospital systems, may contribute in unmeasured ways to this analysis. Our findings are limited to hospitals that performed at least three of a wide variety of EGS operations over a two-year period and may not be applicable to hospitals performing outside these parameters. Likewise, as our study uses California-based data, its geographic separation may lower its validity when applied nationally.
In conclusion, this study demonstrates that hospitals that perform common EGS operations can be grouped into three unique clusters based on their mortality performance: the high performing cluster of hospitals, the average performing, and the poor performing. These clusters are clinically distinct and persist across all examined operations. Hospital technology status and trauma center affiliation were independently associated with high performance. Further investigation is necessary to identify hospital-level factors associated with high, low, and average performance, and to elucidate interventions and processes of care aimed at improving overall system-wide performance.
Supplementary Material
ACKNOWLEGEMENTS
Dr. Becher acknowledges that this publication was made possible by the support of: the Yale Center for Clinical Investigation CTSA Grant Number KL2 TR001862 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH); and the American Association for the Surgery of Trauma (AAST) Emergency General Surgery Research Scholarship Award. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the AAST or the NIH. Dr. Gill acknowledges the support of the Academic Leadership Award (K07AG043587) and Claude D. Pepper Older Americans Independence Center (P30AG021342) from the National Institute on Aging.
Footnotes
Conflicts of Interest:
No competing financial interests exist.
Presented at:
The 77th Annual Meeting of the American Association for the Surgery of Trauma September 26th-29th, 2018, San Diego, CA
REFERENCES
- 1.Gittell JH, Seidner R, Wimbush J. A Relational Model of How High-Performance Work Systems Work. Organ. Sci 2009. July 21;21(2):490–506. [Google Scholar]
- 2.Damanpour F, Walker RM, Avellaneda CN. Combinative Effects of Innovation Types and Organizational Performance: A Longitudinal Study of Service Organizations. J. Manag. Stud 2009. June 1;46(4):650–75. [Google Scholar]
- 3.Lawler EE. Creating high performance organizations. Asia Pac. J. Hum. Resour 2005. April 1;43(1):10–7. [Google Scholar]
- 4.Muldrow TW, Buckley T, Schay BW. Creating high-performance organizations in the public sector. Hum Resour Manage 2002. September 1;41(3):341–54. [Google Scholar]
- 5.Dyer JH, Nobeoka K. Creating and Managing a High-Performance Knowledge-Sharing Network: The Toyota Case. Strategic Manage J. 2000;21(3):345–67. [Google Scholar]
- 6.Public Policy Committee of the American College of Physicians, Ginsburg JA, Doherty RB, Ralston JF, Senkeeto N, Cooke M, Cutler C, Fleming DA, Freeman BP, Gluckman RA, Liebow M et al. Achieving a high-performance health care system with universal access: what the United States can learn from other countries. Ann Intern Med. 2008. January 1;148(1):55–75. [DOI] [PubMed] [Google Scholar]
- 7.Braithwaite J, Marks D, Taylor N. Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. Int J Qual Health Care. 2014. June 1;26(3):321–9. [DOI] [PubMed] [Google Scholar]
- 8.Dias C, Escoval A. Improvement of hospital performance through innovation: toward the value of hospital care. Health Care Manag (Frederick). 2013. September;32(3):268–79. [PubMed] [Google Scholar]
- 9.McConnell KJ, Lindrooth RC, Wholey DR, Maddox TM, Bloom N. Modern Management Practices and Hospital Admissions. Health Econ. 2016. April;25(4):470–85. [DOI] [PubMed] [Google Scholar]
- 10.Birkmeyer JD, Dimick JB. Understanding and Reducing Variation in Surgical Mortality. Annu Rev Med. 2009;60(1):405–15. [DOI] [PubMed] [Google Scholar]
- 11.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Suter LG, Bernheim SM, et al. Hospital readmission performance and patterns of readmission: retrospective cohort study of Medicare admissions. BMJ. 2013. November;347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009. December;250(6):1029–34. [DOI] [PubMed] [Google Scholar]
- 13.Taylor N, Clay-Williams R, Hogden E, Braithwaite J, Groene O. High performing hospitals: a systematic review of associated factors and practical strategies for improvement. BMC Health Serv Res. 2015. June;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brewster AL, Cherlin EJ, Ndumele CD, Collins D, Burgess JF, Charns MP, Bradley EH, Curry LA. What Works in Readmissions Reduction: How Hospitals Improve Performance. Med Care. 2016;54(6):600–7. [DOI] [PubMed] [Google Scholar]
- 15.Pearse RM, Dana EC, Lanigan CJ, Pook JA. Organisational failures in urgent and emergency surgery. A potential peri-operative risk factor. Anaesthesia. 2001. July;56(7):684–9. [DOI] [PubMed] [Google Scholar]
- 16.Bureau USC. American FactFinder - Results [Internet]. [cited 2018 May 8]. Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF
- 17.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009. June;47(6):626–33. [DOI] [PubMed] [Google Scholar]
- 18.Ladha KS, Zhao K, Quraishi SA, Kurth T, Eikermann M, Kaafarani HM, Klein EN, Seethala R, Lee, J. The Deyo-Charlson and Elixhauser-van Walraven Comorbidity Indices as predictors of mortality in critically ill patients. BMJ Open. 2015. September 8;5(9):e008990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thompson NR, Fan Y, Dalton JE, Jehi L, Rosenbaum BP, Vadera S, Griffith SD. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care. 2015. April;53(4):374–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salkind NJ. Encyclopedia of Research Design - 1st Ed Thousand Oaks, CA: SAGE Publications; 2010 [Google Scholar]
- 21.Allen M The SAGE Encyclopedia of Communication Research Methods. Thousand Oaks, CA: SAGE Publications; 2017 [Google Scholar]
- 22.Weick KE. Organizational Culture as a Source of High Reliability. California Management Review. 1987. January 1;29(2):112–27. [Google Scholar]
- 23.Valdmanis VG, Rosko MD, Mutter RL. Hospital Quality, Efficiency, and Input Slack Differentials. Health Serv Res. 2008. October;43(5 Pt 2):1830–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJO, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012. January;255(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mesman R, Westert GP, Berden BJMM, Faber MJ. Why do high-volume hospitals achieve better outcomes? A systematic review about intermediate factors in volume–outcome relationships. Health Policy. 2015. August 1;119(8):1055–67. [DOI] [PubMed] [Google Scholar]
- 26.Billingsley KG, Morris AM, Dominitz JA, Matthews B, Dobie S, Barlow W, Wright GE, Baldwin LM. Surgeon and Hospital Characteristics as Predictors of Major Adverse Outcomes Following Colon Cancer Surgery: Understanding the Volume-Outcome Relationship. Arch Surg. 2007. January 1;142(1):23–31. [DOI] [PubMed] [Google Scholar]
- 27.Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010. November 17;92(16):2643–52. [DOI] [PubMed] [Google Scholar]
- 28.Litvak E, Fineberg HV. Smoothing the way to high quality, safety, and economy. N Engl J Med. 2013. October 24;369(17):1581–3. [DOI] [PubMed] [Google Scholar]
- 29.Haberfelde M, Bedecarré D, Buffum M. Nurse-sensitive patient outcomes: an annotated bibliography. J Nurs Adm. 2005. June;35(6):293–9. [DOI] [PubMed] [Google Scholar]
- 30.Ingraham AM, Cohen ME, Bilimoria KY, Raval MV, Ko CY, Nathens AB, Hall BL. Comparison of 30-day outcomes after emergency general surgery procedures: potential for targeted improvement. Surgery. 2010. August;148(2):217–38. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.