Abstract
Sporadic Burkitt lymphoma (SBL) is a variant of Burkitt lymphoma that occurs worldwide, affecting mainly children and young adults. Association with Epstein-Barr virus (EBV) can be identified in approximately 20-30% of cases. Herein we described a case of a 63-year-old male presenting intraoral bilateral mandibular swelling, subjacent to fixed dental prosthesis, with one month of duration. Incisional biopsies were performed, and after two days, the patient was hospitalized due to malaise and breathing difficulty, and died after a week when an abdominal tumor was detected. The mandibular biopsies revealed a diffuse proliferation of medium-sized monomorphic atypical lymphoid cells exhibiting numerous mitoses and areas of “starry-sky” pattern. The tumor showed immunohistochemical positivity for CD20, CD10, Bcl-6, and Ki-67 (≈ 100%); it was negative for CD3, Bcl-2, Vs38c, and MUM-1. Positivity for EBV was found by in situ hybridization. The final diagnosis was intraoral SBL positive for EBV. Clinical, morphological and molecular criteria are necessary for the correct diagnosis of aggressive B-cell neoplasms positive for EBV in elderly patients.
Keywords: Burkitt lymphoma, Epstein-Barr virus, Non-Hodgkin Lymphoma, Mouth neoplasms
Introduction
Burkitt lymphoma (BL) is an aggressive B-cell lymphoma with three variants; endemic, sporadic, and immunodeficiency-associated, presenting specific epidemiologic and clinical features. Sporadic BL (SBL) occurs worldwide, being more common in children and young adults, rarely affecting elderly patients, who present significantly worse prognosis than the pediatric patients.1,2 Abdominal and ileocecal regions are the most frequent affected sites, while involvement of the oral cavity is rare.3
Approximately 20 to 30% of SBL cases are associated with Epstein-Barr virus (EBV), and Satou et al.4 indicated that the biological behavior and pathogenesis might be different between EBV positive and negative cases. BL usually present a translocation involving the MYC oncogene and it is composed by monomorphic medium-sized cells, which are positive for CD10, CD20, CD22, CD79a, Bcl-6 and the proliferation index assessed by Ki-67 is nearly 100%.5
Despite the apparently well-defined features of BL, some non-Hodgkin lymphomas (NHL) such as diffuse large B-cell lymphoma (DLBCL), may present morphological, immunohistochemical and molecular similarities, becoming a diagnostic challenge;6,7 leading the World Health Organization (WHO) to include modifications in the classification to better characterize these lymphomas. High-grade B-cell lymphoma (HGBL) is another entity considered as differential diagnosis, since some of its morphological and molecular features can be present in BL and DLBCL.1
We herein describe a rare case of intraoral SBL in a 63-year-old Mexican male with bilateral lesions affecting the mandibular posterior alveolar ridge. The differential diagnosis with variants of DLBCL and HGBL is discussed.
Case report
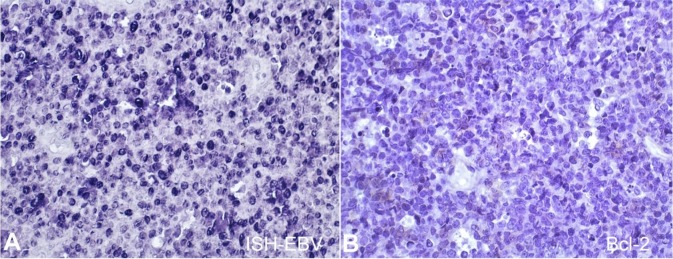
A 63-year-old male patient was referred to dental service, presenting bilateral, painful erythematous mandibular swellings affecting the posterior alveolar ridges, at the level of the premolars on the left side (Figure 1A) and molars on the right side. The lesion was subjacent to fixed dental prosthesis, which caused compression and bleeding of the augmented soft tissue (Figure 1B). After removal of the dental fixed prosthesis, the lesion showed a rapid increase in size in a week (Figure 1C, 1D).
Figure 1. Intraoral view of the lesion. A – bilateral, erythematous mandibular swelling affecting posterior alveolar ridges, at the level of premolars on the left side; B – Diffuse swelling involving the alveolar ridge at the molars level on the right side, subjacent to fixed dental prosthesis, which caused compression, and bleeding of the soft tissue swelling; C-D. The lesion showing a progressive increase after seven days of the dental fixed prosthesis removal.
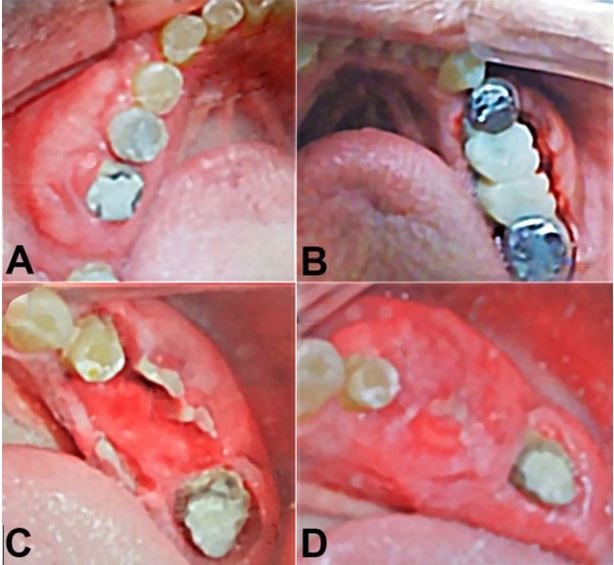
Incisional biopsies were performed in both sides under local anesthesia, and sent for histopathological study. However, after two days of the biopsy, the patient was hospitalized presenting malaise and breathing difficulties. By imaging studies, an abdominal tumor was detected, and patient died within 10 days. Microscopically, the oral lesions revealed a diffuse proliferation of monotonous, medium-sized lymphoid cells with scarce cytoplasm, round basophilic nuclei with fine chromatin, and multiple nucleoli. Nuclear pleomorphism, numerous mitotic and apoptotic figures were common (Figure 2A and B) including tingible body macrophages forming a “starry sky” pattern (Figure 2 C and D). The microscopical diagnosis of high-grade lymphoma was suggested. Immunohistochemistry and in situ hybridization (ISH) for EBV confirmed the diagnosis of SBL.
Figure 2. Histopathological features of sporadic Burkitt lymphoma. A, B – diffuse proliferation of lymphoid cells, with scarce cytoplasm, and round nuclei (H&E, A:10x, B:20x); C – The lymphoid cells are medium sized with multiple and single evident nucleoli, nuclear pleomorphism, numerous mitotic and apoptotic figures (H&E, 40x); D – The tumor cells and tingible body macrophages showing a “starry sky” pattern; the lymphoid cells show fine, granular and dense chromatin (H&E, 40x).
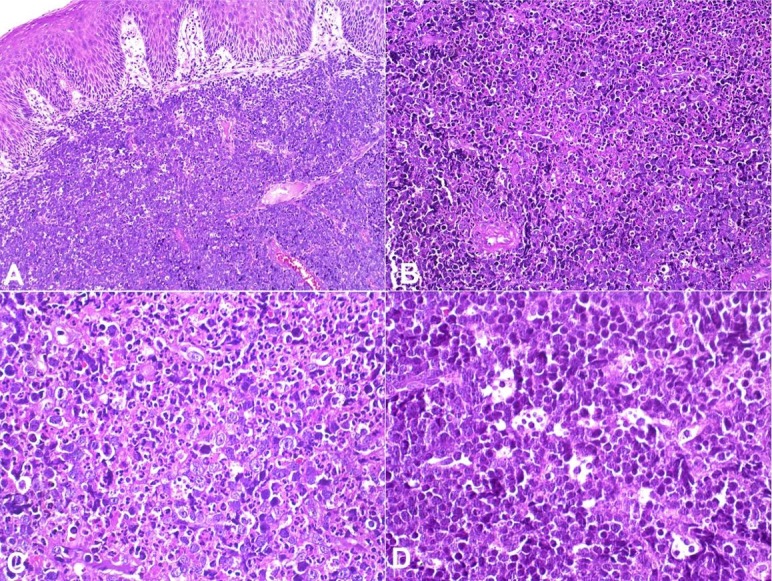
Immunohistochemically, the tumor was positive for CD20, CD10, Bcl-6, and for EBV-encoded RNA (EBER) by ISH (Figure 3A, 3B, 3C, 4A)¸ and negative for CD3, Bcl-2 (Figure 4B), Vs38c, and MUM-1. Ki67 index was near to 100% (Figure 3D). Based on histological and immunohistochemical findings, the final diagnosis (rendered postmortem) was of SBL.
Figure 3. Immunohistochemical features of sporadic Burkitt lymphoma. Most tumor cells showed positivity for CD20 (A), Bcl-6 (B), CD10 (C), and the proliferation index assessed by Ki-67 near to 100% (D) (A-D: IHC, 40x).
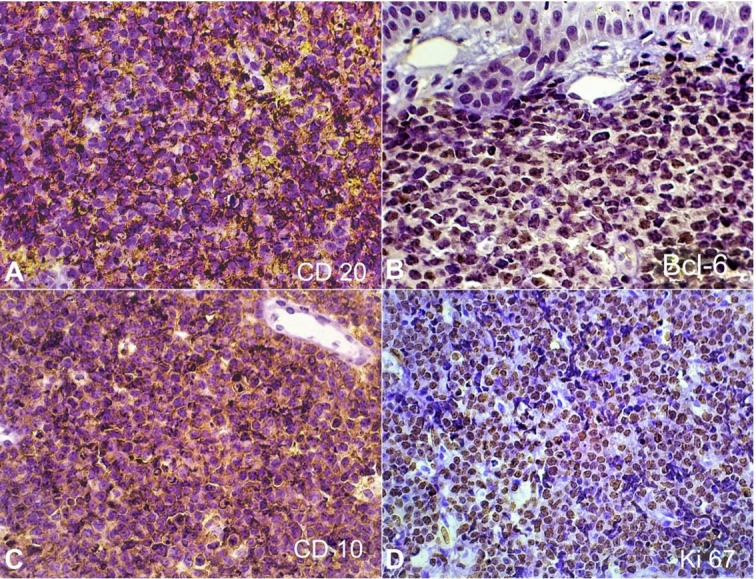
Figure 4. In situ hybridization and immunohistochemical features of sporadic Burkitt lymphoma. A – The tumor was EBV positive (ISH-EBV, 40x); B – Bcl-2 was negative (IHC, 40x).
Discussion
NHL represent the second most common malignant tumor of the head and neck; comprising approximately 3.5% of all oral cavity malignancies.8,9 Herein was described an unusual case of intraoral EBV-positive SBL in an elderly patient, discussing also the differential diagnosis between SBL and some aggressive B-cell lymphomas that were recently reclassified by the WHO.
DLBCL and BL are B-cell lymphomas that may present clinical, morphological, immunohistochemical and molecular similarities, being difficult the correct diagnosis.7 Epidemiologically, DLBCL is more common in adult patients, unlike BL, which accounts for 30-40% of NHL in children.10 The main diagnostic hypotheses considered initially for this case were EBV-positive diffuse large B-cell lymphoma, not otherwise specified (EBV+ DLBCL NOS); HGBL, and BL.
DLBCL NOS is the most common subtype of lymphoma involving the oral cavity in adults, some cases presenting a germinal center phenotype (CD20+, CD10+, Bcl-6+, Bcl-2-, MUM-1- and Ki-67 >90%), which is similar to immunophenotypical expression of BL. Since our case presented EBV positivity, and the patient was elderly with no known history of immunodeficiency or prior lymphoma, EBV+ DLBCL NOS was considered as a differential diagnosis.11 Microscopically our case did not show the polymorphous cell variant, that consists in a mixture of small lymphocytes, plasma cells, histiocytes, proliferation of large transformed cells, and Hodgkin/Reed-Sternberg- like cells. However, it was similar with the monomorphic variant, but areas of geographic necrosis commonly seen in EBV+ DLBCL NOS was absent in the present case.1,11-15
Immunohistochemically, only CD20 would coincide between our case and EBV+ DLBCL NOS, since the last have a non-germinal center phenotype, being positive for MUM-1 and commonly negative for CD10 and Bcl-6.1 Nevertheless, a study demonstrated one case of EBV+ DLBCL NOS expressing CD10, and two cases being Bcl-6-positive and MUM-1 negative.12
HGBL has two categories, the first has intermediate features between DLBCL and BL, presenting rearrangements of MYC/8q24 and Bcl-2/18q21, and/or Bcl-6/3q27, being so-called “double-hit” lymphomas (DHL) or “triple-hit” lymphomas (THL). Microscopically is characterized by a mixed population of intermediate to large transformed cells with apoptotic bodies, mitotic figures, and tingible body macrophages. Immunohistochemically, shows expression of CD19, CD20, CD79a, PAX5, CD10, and Bcl-6. DHL involving MYC and Bcl-2 cytogenetic abnormalities, exhibit strong expression of Bcl-2.1,11,16 The second category is the HGBL (NOS), and is composed of cells with blastoid appearance, resembling BL and DLBCL, but with absence of the genetic rearrangemets.1 Due the immunohistochemical and histopathological results of the present case, DHL was also considered in the differential diagnosis. However, the presence of EBV and negativity for Bcl-2 favors the diagnosis of BL.
Epidemiologically, endemic BL is more prevalent in children living in Africa; while SBL can occur worldwide also affecting mainly young patients being rare in the elderly. Gastrointestinal tract, abdomen, liver, oropharynx/nasopharynx, jaw/maxilla, ovaries, and central nervous system, are the predominant sites affected by SBL.17 According to the WHO criteria BL is characterized by a diffuse proliferation of monotonous, medium-sized lymphocytes with multiple nucleoli, and several mitotic figures, showing a “starry sky” pattern. BL is composed by mature B-cells positive for CD19, CD20, CD22 and CD79a, also exhibiting immunologic similarity to germinal center cells rather than activated B-cells, being also positive for Bcl-6, CD10 and negative for MUM-1, CD44, CD138 and Bcl-2.1 These findings are compatible with the present case, with the exception of EBV status, since only in geographic regions such as South Asia, Middle Eastern and South America, the EBV-positive BL rates are high (50-80%).17,18
Previously it was suggested that EBV-positive SBL constitute a distinct subgroup of BL, presenting some specific characteristics also found in our case: (1) less positivity for MUM1; (2) involvement of different anatomic topographies such as tonsils, adrenal gland, and cervical lymph nodes; (3) affect mainly patients older than 50 years and the frequency increases with age.4 The positivity of MUM-1 varies according to its origin, therefore, only a small group of BL originated from post-germinal center B cells shows positive expression. Despite MUM-1 is a potential adverse prognostic marker, its expression is not associated with EBV infection status.19
Although CD10-positivity can be seen in DLBCL NOS, the neoplastic cells are usually Bcl-2 positive and display a slightly lower Ki-67 proliferative index compared with BL that is close to 100%.7 Although the present case was not assessed for gene rearrangement and MYC immunohistochemical staining, there are cases in the literature without information about MYC gene rearrangement, and according to clinical, morphological and immunohistochemical characteristics were diagnosed as BL.20 It is well recognized that chromosomal translocations in the MYC oncogene are the biological hallmark of BL, but also may be present in other B-cell lymphomas; in this sense, when the morphological characteristics are compatible with BL, and the immunohistochemical findings show positivity for MYC and Bcl-2, it is recommended to perform molecular tests in the search for gene rearrangements to rule out DHL or THL.1,11,16 In this context, morphologic characteristics, Bcl-2 negativity, Ki-67>95% and EBV association, were the main features that supported the diagnosis of intraoral SBL.
Isolated oral SBL in adults is rare, with only few reports.21,22 Clinically, these lesions may resemble various oral pathologies¸ even of benign or reactive nature, including inflammatory periodontal processes.23 Although our case had bilateral presentation and it was associated to fixed dental prosthesis, its aggressive features such as considerable size and rapid growth, raised the suspicion of malignancy, and the lesions were biopsied. Additionally, the patient was hospitalized for sudden worsening of his systemic condition, and full body computed tomography revealed an abdominal mass, which diagnosis was not confirmed, however, it is very likely to represent a manifestation of disseminated SBL, due to its location and clinical presentation. The patient died 10 days after the biopsies, confirming the aggressiveness, systemic involvement of the tumor, and the poor prognosis of BL in elderly patients.
In summary, the role of the dentist is fundamental in early detection of primary and metastatic malignancies in the oral cavity, since the clinical spectrum can mimic benign or reactive conditions. Unfortunately, for most adult patients with BL, the prognosis remains poor despite therapy.
Footnotes
How to cite: Pedraza RM, Arboleda LPA, Sánchez-Romero C, et al. Intraoral EBV-positive sporadic Burkitt lymphoma in an elderly patient with bilateral presentation. 2019 Oct-Dec;9(4):e2019117. https://doi.org/10.4322/acr.2019.117
The manuscript is in accordance with the Institutional Ethics committee.
Financial support: This work was supported by the São Paulo State Research Foundation (FAPESP), Grant/Award Number: 2017/14880-3, and by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) - Finance Code 001.
References
- 1.Swerdlow SH, Campo E, Harris NL, et al. . WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. Lyon, France: IARC; 2017. [Google Scholar]
- 2.Bi C-F, Tang Y, Zhang W-Y, et al. . Sporadic Burkitt lymphomas of children and adolescents in Chinese: a clinicopathological study of 43 cases. Diagn Pathol. 2012;67(1):72. 10.1186/1746-1596-7-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swerdlow S, Campo E, Harris NL, et al. . WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 3rd ed. Lyon, France: IARC; 2008. [Google Scholar]
- 4.Satou A, Asano N, Nakazawa A, et al. . Epstein-Barr virus (EBV)-positive sporadic Burkitt lymphoma: an age-related lymphoproliferative disorder? Am J Surg Pathol. 2015;39(2):227-35. 10.1097/PAS.0000000000000332. [DOI] [PubMed] [Google Scholar]
- 5.Casulo C, Friedberg J. Treating burkitt lymphoma in adults. Curr Hematol Malig Rep. 2015;10(3):266-71. 10.1007/s11899-015-0263-4. [DOI] [PubMed] [Google Scholar]
- 6.Chuang SS, Ye H, Du MQ, et al. . Histopathology and immunohistochemistry in distinguishing Burkitt lymphoma from diffuse large B-cell lymphoma with very high proliferation index and with or without a starry-sky pattern: a comparative study with EBER and FISH. Am J Clin Pathol. 2007;128(4):558-64. 10.1309/EQJR3D3V0CCQGP04. [DOI] [PubMed] [Google Scholar]
- 7.Bellan C, Stefano L, Giulia F, Rogena EA, Lorenzo L. Burkitt lymphoma versus diffuse large B-cell lymphoma: a practical approach. Hematol Oncol. 2009;27(4):182-5. 10.1002/hon.914. [DOI] [PubMed] [Google Scholar]
- 8.Epstein JB, Epstein JD, Le ND, Gorsky M. Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(5):519-25. 10.1067/moe.2001.116062. [DOI] [PubMed] [Google Scholar]
- 9.Triantafillidou K, Dimitrakopoulos J, Iordanidis F, Gkagkalis A. Extranodal non-hodgkin lymphomas of the oral cavity and maxillofacial region: a clinical study of 58 cases and review of the literature. J Oral Maxillofac Surg. 2012;70(12):2776-85. 10.1016/j.joms.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 10.Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107(1):265-76. 10.1182/blood-2005-06-2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Owosho AA, Bilodeau EA, Surti U, Craig FE. Large B-cell lymphoma of the base of the tongue and oral cavity: a practical approach to identifying prognostically important subtypes. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(3):338-47. 10.1016/j.oooo.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Ozsan N, Cagirgan S, Saydam G, Gunes A, Hekimgil M. Epstein-Barr virus (EBV) positive diffuse large B cell lymphoma of the elderly-experience of a single center from Turkey. Pathol Res Pract. 2013;209(8):471-8. 10.1016/j.prp.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Adam P, Bonzheim I, Fend F, Quintanilla-Martínez L. Epstein-Barr virus-positive diffuse large B-cell lymphomas of the elderly. Adv Anat Pathol. 2011;18(5):349-55. 10.1097/PAP.0b013e318229bf08. [DOI] [PubMed] [Google Scholar]
- 14.Naeini YB, Wu A, O’Malley DP. Aggressive B-cell lymphomas: frequency, immunophenotype, and genetics in a reference laboratory population. Ann Diagn Pathol. 2016;25:7-14. 10.1016/j.anndiagpath.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Castillo JJ, Beltran BE, Miranda RN, Young KH, Chavez JC, Sotomayor EM. EBV-positive diffuse large B-cell lymphoma, not otherwise specified: 2018 update on diagnosis, risk-stratification and management. Am J Hematol. 2018;93(7):953-62. 10.1002/ajh.25112. [DOI] [PubMed] [Google Scholar]
- 16.Aukema SM, Kreuz M, Kohler CW, et al. . Biological characterization of adult MYC-translocation-positive mature B-cell lymphomas other than molecular Burkitt lymphoma. Haematologica. 2014;99(4):726-35. 10.3324/haematol.2013.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Queiroga EM, Gualco G, Weiss LM, et al. . Burkitt lymphoma in Brazil is characterized by geographically distinct clinicopathologic features. Am J Clin Pathol. 2008;130(6):946-56. 10.1309/AJCP64YOHAWLUMPK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen BJ, Chang ST, Weng SF, et al. . EBV-associated Burkitt lymphoma in Taiwan is not age-related. Leuk Lymphoma. 2016;57(3):644-53. 10.3109/10428194.2015.1076928. [DOI] [PubMed] [Google Scholar]
- 19.Cohen JI, Bollard CM, Khanna R, Pittaluga S. Current understanding of the role of Epstein-Barr virus in lymphomagenesis and therapeutic approaches to EBV-associated lymphomas. Leuk Lymphoma. 2008;49(Suppl 1):27-34. 10.1080/10428190802311417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang H, Liu ZL, Zeng H, et al. . Clinicopathological study of sporadic Burkitt lymphoma in children. Chin Med J (Engl). 2015;128(4):510-4. 10.4103/0366-6999.151106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia NG, Rodrigues MTV, Aleixo RQ, Oliveira DT. Burkitt Lymphoma in adult with atypical clinical presentation primarily involving the oral soft tissue. J Craniofac Surg. 2017;28(8):e795-7. 10.1097/SCS.0000000000003681. [DOI] [PubMed] [Google Scholar]
- 22.Kikuchi K, Inoue H, Miyazaki Y, et al. . Adult sporadic burkitt lymphoma of the oral cavity: a case report and literature review. J Oral Maxillofac Surg. 2012;70(12):2936-43. 10.1016/j.joms.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 23.Balasubramaniam R, Goradia A, Turner LN, et al. . Burkitt lymphoma of the oral cavity: an atypical presentation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):240-5. 10.1016/j.tripleo.2008.09.008. [DOI] [PubMed] [Google Scholar]