Summary
Physicians need better training to manage patients with obesity. Our study capitalized on the intimate nature of an extracurricular obesity workshop, creating an interactive educational programme. We assessed the short‐ and long‐term impact of the workshop on trainees' knowledge, competence and confidence in caring for patients with obesity in an outpatient setting. This is a cross‐sectional study, involving regionally diverse mix of resident and fellow physicians. A live 2.5‐day continuing medical education summit was held 11 to 13 March 2016. Obesity‐related topics were reviewed using state‐of‐the art pedagogical techniques. Pre‐/post‐levels of knowledge, competence and clinical practice strategies were analysed. Sixty‐three candidates interested in additional obesity medicine training were nominated by US residency and fellowship programme directors and selected to attend the summit. On average, learners experienced a 110% relative increase in knowledge and competence. The overall effect size was 0.95, with participants being ~54% more knowledgeable about the management of patients with obesity. All participants self‐reported that this activity increased their knowledge about the subject matter, improving their performance in caring for patients when asked about their practice in a follow‐up survey 6 months following the workshop. This immersive summit promoted robust gains in knowledge and confidence, ultimately translating to reported practice improvements at the individual and health system levels. Future research is warranted on the sustainability of gained skills.
Keywords: medical education and training, obesity, primary care
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Primary care physicians infrequently discuss obesity during outpatient visits due to numerous barriers, notably a lack of confidence and knowledge in weight loss counselling.
One approach to better prepare healthcare providers to manage patients with obesity is improving education of primary care residents and fellows.
Two major barriers to the incorporation of more comprehensive obesity education within graduate medical education are the lack of available time in a crowded curriculum and insufficient faculty who are knowledgeable and experienced in obesity care.
WHAT THIS STUDY ADDS
Our study describes a model for an innovative, extramural, immersive approach to educate trainees on the various aspects of obesity management.
We assessed the participants' knowledge, competence and confidence before and after the educational intervention while also assessing the long‐term data 6 months after the workshop.
By participating in the workshop described, participants achieved more than a 100% relative increase in knowledge/competence and were approximately 54% more likely to be knowledgeable about the management of patients with obesity than they were prior to learning.
1. INTRODUCTION
Obesity is a chronic, relapsing disease that is inadequately addressed in the primary care setting. The literature consistently demonstrates that primary care physicians infrequently discuss obesity during outpatient visits due to numerous barriers, notably a lack of confidence and knowledge in weight loss counselling.1 The authors of a 2016 study2 delivered a web‐based survey to approximately 1500 US physicians and nurse practitioners in family medicine, internal medicine and obstetrics and gynaecology, and reported that 59% of respondents stated they wait until patients with obesity broach the subject of weight before addressing it. Physicians and advanced practice providers have reported that they believe dieticians and nutritionists are more inclined to counsel patients on obesity than themselves.2 Other studies have shown that primary care providers commonly address obesity only as a risk factor for other chronic medical diseases, such as diabetes, than focus on and treat obesity as a separate medical problem.3
Because prevalence rates of obesity continue to increase, improvements in the ability of primary care physicians to counsel patients on obesity management is urgently warranted.4 One such improvement could be targeting the medical education of trainees. To address these concerns, many have called for improvements in the education of primary care residents and fellows.5, 6 Multiple studies demonstrated that residents lack competency in weight loss counselling and reported low self‐efficacy in their counselling skills.7, 8, 9 Few published studies examined the current state of medical residency education on weight loss counselling, but the evidence suggests that minimal curriculum time is spent on obesity, nutrition and physical activity counselling.10 Programme directors and residents have called for a greater emphasis on teaching specific counselling techniques and providing additional opportunities to practice counselling skills and use assessment tools that facilitate feedback as well as identify areas for improvement.9, 10
However, two major barriers to the incorporation of more comprehensive obesity education within graduate medical education are the lack of available time in a crowded curriculum and insufficient faculty who are knowledgeable and experienced in obesity care. To directly address these obstacles, an innovative, extramural, immersive approach to educate trainees on the various aspects of obesity management may be beneficial.
The first objective of our study was to design and implement an interactive and immersive extracurricular obesity workshop for a select group of medical residents and fellows. The second objective was to assess the short‐ and long‐term impact of the workshop on trainees' knowledge, competence and confidence in caring for patients with obesity in an outpatient setting.
2. MATERIALS AND METHODS
2.1. Participants
Approximately 3 months prior to hosting the summit, letters were mailed to 184 residency and fellowship programme directors across the United States. Programme directors were asked to select one candidate who was interested in additional training in obesity medicine and could serve as an educational champion to disseminate the learned information to the home institution. We asked that candidate recommendations be submitted by 5 February 2016. Sixty‐nine applications were received, from which 63 candidates were chosen to participate to maintain an intimate learning environment with approximate 8:1 attendee‐to‐faculty ratio. Selection was based on order of submission and to maximize geographic diversity. Chosen participants were informed of their selection via email within 1 week of application submission. Participant confirmation of attendance was expected within 1 to 2 weeks after receipt of email. One week prior to the workshop, participants received agenda details as well as pre‐workshop materials, which they were expected to review prior to arrival.
The first day of the summit involved a thorough review of objectives and expectations, and the details of the study. Attendees were asked to sign written informed consent and were given the option to withdraw from participating in the study, if desired.
2.2. Programme description
The current study includes a cross‐sectional design to assess a live 2.5‐day continuing medical education meeting held in Orlando, Florida, 11 to 13 March 2016. The immersive summit included eight overarching educational objectives (Table 1). Vindico Medical Education and eight faculty experts specializing in the care of obesity, diabetes mellitus or related conditions capitalized on the intimate nature of the summit to provide a uniquely designed series of highly engaging and interactive educational formats to pair with standard didactic lectures. These formats are described in Table 2. All costs related to the summit, including travel and faculty honoraria, were provided by Vindico Medical Education.
Table 1.
Educational objectives of the obesity summit
| Learning objectives |
| 1. Review etiologic factors implicated in the development of obesity. |
| 2. Describe the biology and pathophysiology of obesity, including the roles of genetic factors as well as hypothalamic and adipose tissue function. |
| 3. Identify barriers to communicating with patients about obesity. |
| 4. Define the components of effective counselling for obesity. |
| 5. Examine approaches to the assessment and management of dietary and physical activity factors in patients with overweight and obesity. |
| 6. Address issues involved in assessing and managing behavioural and psychological components of obesity. |
| 7. Review the safety and efficacy of pharmacologic therapies for obesity, including recently approved medications. |
| 8. Identify considerations involved in selecting candidates for bariatric surgery. |
Table 2.
Unique educational formats used in the obesity summit
| Learning modality | Description |
|---|---|
| Four corners: Obesity exploration! | By physically moving to a designated corner of the room, learners voice whether they strongly agree, agree, disagree or strongly disagree with controversial topics regarding obesity (eg, Is obesity a disease?) |
| Individual readiness assurance test (iRAT) | Learners were held accountable for completion of the pre‐study material by answering multiple choice questions based on the content; responses were displayed via an audience response system |
| Group readiness assurance test (gRAT) | Learners worked as a team to answer additional multiple choice questions based on case studies. |
| Hot topics in obesity | Faculty‐led discussion on cutting‐edge topics in obesity (eg, Why do patients regain weight?) |
| Obesity in the media | Faculty provide a media clip and lead discussion on both sides of the issue (eg, Atkins diet, detoxification) |
| Addressing the stigma | Presentation by faculty and a patient with obesity |
| Think‐pair‐share | Learners think independently about challenging obesity cases then discuss as a pair and finally share their response with the group. |
| Wheel of obesity knowledge | Group is divided into teams to answer questions based on topics covered throughout the summit. A leader board promoted friendly competition. |
2.3. Study design
The obesity summit workshop featured many unique formats, with outcomes measured in a variety of ways. First, a pre‐activity survey was distributed to attendees to assess demographic data, exposure to obesity medicine during their training and knowledge and attitude towards obesity counselling (Appendix A). Also, using an audience response system (ARS) for the individual readiness assurance test, participants were asked to answer multiple choice questions based on information in the pre‐study material distributed 1 week prior to the summit (Appendix B).
Changes in knowledge and competence after each educational session were assessed with pre‐/post‐testing. Unique, state‐of‐the‐art pedagogical approaches to teaching were used in the summit as outlined in Table 1. Specifically, during these educational sessions, the ARS helped to facilitate the collection of responses to case‐based questions, as well as other interactive and gamified components of the summit. With presentation of results immediately following data collection, the faculty was able to lead discussion based on audience response. For instance, participants did not reach consensus on several case‐based polling questions, prompting the faculty to interject their perspectives on best practices. Examples of such questions are outlined in Appendix C.
The summit was evaluated using Moore's outcomes framework for assessing learners and evaluating instructional activities.11 Specifically, level 2 (satisfaction) was used for the assessment (Appendix D). Finally, qualitative follow‐up data were collected 180 days after the activity to assess a longer‐term impact of the educational initiative on physician confidence, practice patterns and patient outcomes (Appendix E).
2.4. Analyses
Participant demographics and characteristics were assessed with univariate analyses. Paired t tests were used to assess pre‐/post‐levels of competence and clinical practice strategies. P value (<.05) determined the significance in change in knowledge and confidence in pre‐ to post‐learning. In addition, Cohen's d effect size analyses were performed to calculate an effect size of the difference between participants' pre‐/post‐overall knowledge related to objectives and material content. A low, medium or large effect size is represented by a non‐overlap of 15%, 33% and 47%, respectively.12 All analyses were conducted using Microsoft Excel (Version 1807).
3. RESULTS
A total of 63 US residents or fellows attended the workshop, representing the following specialties: family medicine (38%), internal medicine (37%), endocrinology (13%) and obstetrics and gynaecology (13%) (Table 3 ). Attendees represented a total of 57 institutions that were geographically diverse: West (14%), Midwest (23%), South (37%) and Northeast (26%). Do note, the sum of these percentages may not equal 100 due to rounding.
Table 3.
Obesity summit participant demographics (n = 63)
| Demographic | Response | % |
|---|---|---|
| Training level | PGY1 | 6 |
| PGY2 | 48 | |
| PGY3 | 24 | |
| PGY4 | 13 | |
| PGY5 | 5 | |
| PGY6 | 4 | |
| Degree | MD | 87 |
| DO | 6 | |
| MD, PhD | 2 | |
| MBBS | 5 | |
| Specialty | Family Medicine | 38 |
| Internal Medicine | 37 | |
| Endocrinology | 13 | |
| Ob/Gyn | 13 |
3.1. Participant pre‐activity polling
Of the participant learners, 66% and 56% reported very little to no obesity education and training in medical school and residency, respectively. More than one‐half of attendees (58%) reported that they do not have an expert in obesity medicine at their institution. In addition, only 24% of attendees reported that they had an opportunity to rotate through an obesity treatment clinic during their training.
3.2. Confidence in ability polling
A relative increase in participants' self‐reported confidence was found across various aspects of obesity care, as reflected in Table 4, including retention of confidence in the follow‐up data.
Table 4.
Percentage of participants reporting high levels of confidence using a 4‐point Likert scale (those answering very or extremely were rated as high)
| Changes to practice | Pre‐activity (%) | Post‐activity (%) | Relative increase from pre‐ to post‐activity (%) | 6‐mo follow‐up (%) | Relative increase from pre‐activity to 6 mo post (%) |
|---|---|---|---|---|---|
| Providing dietary counselling | 26 | 83 | 219 | 83 | 219 |
| Providing physical activity counselling | 28 | 90 | 221 | 67 | 139 |
| Recommending bariatric surgery | 14 | 75 | 436 | 33 | 136 |
| Providing behavioural counselling | 7 | 70 | 900 | 50 | 614 |
| Providing pharmacotherapy for obesity | 8 | 70 | 775 | 50 | 525 |
| Providing post‐surgery follow‐up care | 8 | 54 | 575 | 83 | 938 |
3.3. Pre‐/Post‐test assessment of knowledge and competence
A significant increase in knowledge and competence was noted for resident and fellow trainees who participated in the obesity summit workshop, which can positively impact their patient population. On average, learners experienced a 110% relative increase in knowledge and competence regarding the overall management of patients with obesity by participating in this continuing medical education activity. The overall effect size was 0.95, with participants being approximately 54% more likely to be knowledgeable about the management of patients with obesity than they were prior to learning. Do note, these percentages are based on n = 62, rather than the total number of attendees (n = 63) because one participant's response was missing.
3.4. Participant satisfaction
All participants (100%) reported that this activity increased their knowledge about the subject matter and will improve their performance in caring for patients. Nearly all participants (95%) reported that they are more likely to use a comprehensive therapeutic approach to induce and maintain weight loss in patients with overweight and obesity; 5% already do so. Finally, 99% of participants reported that the activity better prepared them to care for patients.
3.5. Follow‐up feedback
The follow‐up data included qualitative feedback collected via self‐reported electronic survey sent 180 days after completion of the workshop. The findings indicated numerous positive practice changes implemented by participants; consequently, 70% of respondents noted improvement in their patient's health, achieving weight loss, improvement in haemoglobin A1C, increased adherence to a weight loss plan and/or improved psychological or behavioural health. Of importance, increases in participants' confidence were maintained (Table 2), and numerous positive practice changes had been implemented. For example, some participants reported their routine assessment of patients for obesity and implementation of effective counselling strategies.
4. DISCUSSION
Current primary care practice behaviours must change to sufficiently address the obesity epidemic. Barriers to changing the current culture include, but are not limited to, inadequate obesity education that results in provider lack of knowledge and confidence in counselling skills.8 Two of the major educational obstacles are lack of sufficient time in the curricula and few faculty members available who are trained in obesity medicine. To address this dilemma, we developed a 2.5‐day immersive, extramural, obesity summit workshop for those planning to enter the field of primary care or endocrinology that was attended by select residents and fellow trainees from across the United States.
Overall, the workshop promoted gains in knowledge, competence and confidence for the resident and fellow participants, ultimately translating to practice changes at both the individual and health system levels. Participants achieved more than a 100% relative increase in knowledge/competence and were approximately 54% more likely to be knowledgeable about the management of patients with obesity than they were prior to learning. Importantly, this gain in knowledge may have positively impacted patient care from the subjective data gathered 6 months after the education in the follow‐up survey. Noting that in the in‐patient or out‐patient setting, 58 residents/fellows see 30 patients per week on average with either overweight or obesity, at least 1713 patients seen per week by participants of this activity are 54% more likely to receive evidence‐based care than those seen by nonparticipants of this activity. However, we did not ask participants the nature of the patient encounter. Thus, it is possible that some patients were being seen for a reason other than an annual physical examination, yet the physicians were inquiring about obesity. In the follow‐up survey, physicians reported numerous improvements in patients' health, including weight and cardiovascular benefits, in addition to improvements in mental health and overall patient morale.
Our summit workshop followed the 2016 study by Burton et al,13 with some key differences. First, our study was an immersive 2.5‐day programme compared with a 3‐hour educational session in their study. We invited select residents and fellows from across the United States with an established interest in entering a primary care‐related field after training. We assessed the participants' knowledge, competence and confidence before and after the educational intervention while also assessing the long‐term data 6 months after the workshop. The obesity summit included a wide range of topics—from obesity biology and pathophysiology to the pharmacologic and surgical management of patients with obesity. Alternatively, Burton et al13 focused on motivational interviewing related to obesity management. Finally, our study was uniquely distinguished in providing state‐of‐the‐art, highly engaging educational formats paired with standard didactic lectures that were tailored specifically to meet the preferred educational learning style of a younger, technology‐savvy audience. These differences highlight the strengths of our study in comprehensibility, inclusion of a regionally diverse sample of trainees across multiple disciplines, long‐term data collection and innovativeness.
There are some limitations to our study. Sample size is small, although we have a regionally diverse mix of participants that allows the results to be more generalizable. To expand the educational format to a greater number of trainees, additional resources would be needed, including faculty and funding. Expenses were covered for participants' attendance to the summit and this may have contributed to selection bias, though if costs had not been covered, we speculate it would have led to fewer trainees participating in the summit. Due to the scarcity of providers, it is challenging for institutions without such experts to host an obesity summit or to incorporate such a workshop into a residency or fellowship programme. Finally, we did not assess direct patient outcomes in this study although subjective data was collected 6 months following completion of the workshop that suggested improvements in patients' health. Although this provided us insight into observed changes in clinical practice, these results may be influenced by belief and/or confirmation bias.
Future research is warranted to determine the sustainability of a trainee's gained skills from this type of obesity summit workshop. In addition, data collection of direct patient outcomes is needed. Feedback from participants also elucidated topic areas of interest that could be added to the curriculum, such as long‐term obesity management. Overall, our study demonstrated a feasible, creative and time‐efficient extramural workshop to strengthen obesity education among medical trainees that should effectively improve their knowledge, competence and confidence in the management of patients with obesity.
AUTHOR CONTRIBUTIONS
R.F.K. conceived the study and its design. K.J.H.R., J.L.F. and R.F.K. made substantial contributions to design, analysis and interpretation of the data. R.F.K. served as course chair and faculty of the obesity summit. A.V. and R.F.K. were involved in writing of the manuscript. All authors critically reviewed and revised the manuscript. All authors read and approved the final manuscript.
CONFLICT OF INTEREST
A.V. was a participant in the obesity summit and received travel and lodging support. A.V. has no conflict of interest disclosures. R.F.K. serves on the medical advisory board for Novo Nordisk, Weight Watchers and Retrofit. K.J.H.R. and J.L.F. are employees of Vindico Medical Education. R.F.K. received consulting honorarium from Novo Nordisk as a member of their advisory board. R.F.K. received payment from Vindico for writing/reviewing the manuscript, including print and video continuing medical education materials.
ACKNOWLEDGEMENTS
The authors thank the faculty, including Daniel H. Bessesen, W. Timothy Garvey, Holly Herrington, Scott Kahan, Donna H. Ryan, Patrick M. O'Neil and Christopher D. Still. Additionally, the authors thank the participants, support staff and all those involved in helping to accomplish this pilot programme. This study received unrestricted educational grant from Novo Nordisk, Inc. and Takeda Pharmaceuticals U.S.A., Inc.
Obesity summit pre‐activity survey
| Area of interest | Question |
|---|---|
| Demographic data | 1. What is your degree? |
| a. MD | |
| b. DO | |
| c. MD, PhD | |
| d. MBBS | |
| 2. What is your specialty? | |
| a. Family Medicine | |
| b. Internal Medicine | |
| c. Endocrinology | |
| d. Ob/Gyn | |
| 3. Approximately how many patients with overweight or obesity do you see per week in the in‐patient and outpatient setting combined? | |
| a. Less than 10 | |
| b. 10 to 30 | |
| c. 31 to 50 | |
| d. More than 50 | |
| e. NA | |
| 4. What training programme are you currently in? | |
| a. Internal Medicine | |
| b. Family Medicine | |
| c. Endocrinology | |
| d. Ob/Gyn | |
| 5. What year are you? | |
| a. PGY1 | |
| b. PGY2 | |
| c. PGY3 | |
| d. PGY4 | |
| e. PGY5 | |
| f. PGY6 | |
| Medical training and direction | 1. How much obesity education and training did you get in medical school? |
| a. Adequate | |
| b. Some | |
| c. Very little | |
| d. None | |
| 2. How much obesity education and training did you get in residency? | |
| a. Adequate | |
| b. Some | |
| c. Very little | |
| d. None | |
| 3. How much obesity education and training did you get in fellowship? | |
| a. Adequate | |
| b. Some | |
| c. Very little | |
| d. None | |
| e. NA | |
| 4. Do you have an obesity medicine expert at your institution? | |
| a. Yes | |
| b. No | |
| 5. Do you have the opportunity to rotate through an obesity treatment clinic during your training? | |
| a. Yes | |
| b. No | |
| 6. Following the conclusion of training, to what degree do you see obesity medicine as a focus of your practice? | |
| a. It will be the main focus of my clinical practice | |
| b. I want to be a local expert | |
| c. Somewhat of a focus | |
| d. Not sure | |
| Knowledge in obesity counselling | 1. How would you rate your level of knowledge regarding biology and pathophysiology of obesity? |
| a. Very knowledgeable | |
| b. Knowledgeable | |
| c. Somewhat knowledgeable | |
| d. Not knowledgeable | |
| Attitude towards obesity counselling | 1. What is your opinion to the following statement? Obesity is a disease. |
| a. Agree | |
| b. Somewhat agree | |
| c. Somewhat disagree | |
| d. Disagree | |
| 2. How important is it for physicians to directly provide obesity care? | |
| a. Very important | |
| b. Important | |
| c. Somewhat important | |
| d. Not important |
Individual readiness assurance test (iRAT) questions and wheel of knowledge questions
B.1. IRAT QUESTIONS
- A 48‐year‐old patient with Class II obesity presents for weight loss management. She states that she is always hungry and never feels full. In addition to providing guidance on diet, physical activity, and behavioural change, you decide to prescribe phentermine, an adrenergic anti‐obesity medication. After 1 week of therapy, her appetite is significantly diminished, allowing her to follow a calorie‐reduced diet with more control. Which neuropeptide caused her to initially always feel hungry?
- Neuropeptide Y (NPY) (correct answer)
- Pro‐opiomelanocortin (POMC)
- Cocaine‐ and amphetamine‐regulated transcript (CART)
- α‐Melanocyte stimulating hormone (α‐MSH)
You are conducting a feeding study on a subject in the Clinical Research Center. The following graph displays the circulating concentration of a peptide over 24 hours prior to and after consuming breakfast (BR), lunch (LU), and dinner (DI). Which gut peptide has this circulating characteristic?
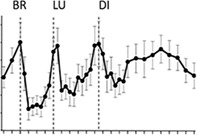
Peptide YY3‐36
Glucagon‐like peptide 1
Ghrelin (correct answer)
Cholecystokinin
A 56‐year‐old woman with a 5‐year history of hypertension comes to the office for a consultation regarding weight loss. She has gained 15 pounds during the past year and reports gaining more weight around her abdomen. Her body mass index (BMI) is 27 kg/m2. Which of the following is the most appropriate method of measuring this patient's waist circumference to assess her cardiometabolic risk?
After fasting for 8 hours
After the patient exhales deeply
At the level of the iliac crest (correct answer)
With the patient's hands above her head
B.2. WHEEL OF KNOWLEDGE QUESTIONS
- A gastric sleeve procedure is associated with which of the following nutritional considerations?
- Iron deficiency (correct answer)
- Malabsorption of protein
- Copper deficiency
- Zinc deficiency
- When talking about weight with a patient, it is often recommended to use the words “overweight” or “excess weight” rather than “obese.” The reason for this recommendation is because the word obese:
- May be offensive to the patient (correct answer)
- Signifies weight bias
- Specifically denotes excess fat
- Is culturally defined
- If I refer patients to a community‐based counselling programme based on the Diabetes Prevention Programme manual, how much weight can I expect them to lose in 6 months?
- At least 7%
- On average, 7% (correct answer)
- At least 10%
- On average, 10%
- Among patients with congestive heart failure, which BMI group has the lowest mortality?
- <20 kg/m2
- 20 to 25 kg/m2
- 25 to 30 kg/m2
- 30 to 35 kg/m2 (correct answer)
- Lorcaserin works by which of the following mechanisms of action?
- Acts as a selective 5‐hydroxytryptamine 2C receptor (5‐HT2C)
- Acts as a selective 5‐HT2C receptor agonist (correct answer)
- Deactivates melanocortin‐4 receptors (MC4‐R)
- Deactivates proopiomelanocortin (POMC) neurons
- The part of the brain that is responsible for generating the rewarding qualities of highly palatable food is which of the following structures?
- The arcuate nucleus of the hypothalamus
- The ventral striatum (correct answer)
- The lateral hypothalamus
- The prefrontal cortex
- Which of the following antidepressant medications is associated with weight LOSS?
- Paroxetine
- Amitriptyline
- Bupropion (correct answer)
- Mirtazapine
- Which of the following is an important principle when discussing weight with patients?
- Avoiding open‐ended questions
- Establishing control and exclusive direction of the physician‐patient relationship
- Asking the patient's permission to discuss the challenges of achieving weight loss (correct answer)
- Informing the patient of changes that need to be implemented to achieve weight loss
- A randomized, controlled trial of lifestyle modifications for weight loss has been shown to reduce mortality in which of the following populations?
- Unselected obese adults
- Obese adults with pre‐diabetes (correct answer)
- Obese adults with diabetes
- Obese adults with cancer
- Which weight loss agent would be the best choice for a 54‐year‐old man with a BMI of 33.5 kg/m2 and a history of depression, drug abuse and chronic pancreatitis? He is currently taking sertraline 200 mg daily.
- Lorcaserin
- Phentermine/topiramate extended release (ER) 7.5/46 mg once daily (QD)
- Liraglutide 3.0 mg subcutaneous once daily (QD)
- Naltrexone/buproprion extended release 32/360 mg QD (correct answer)
Audience response system‐facilitated questions
C.1. CASE 1: A 48‐YEAR‐OLD MAN WITH DIABETES AND HYPERTENSION
Summary: A 48‐year‐old male accountant returns for medical visit, with a known history of depression since college, hypertension, type 2 diabetes mellitus for 4 years and recent gastro‐oesophageal reflux disease. The patient has suffered from progressive weight gain over the past 15 years that has accelerated over the past year. His medications include those listed below. Family history includes diabetes and cardiovascular disease. He is married and lives with his wife and two children, ages 16 and 13. The patient was a healthy weight until he married at age 30, with continuous 30‐pound weight gain thereafter, especially over the past year (8 pounds). The patient attributes his weight gain to a busy lifestyle, travelling, not choosing healthy foods, eating large portions and not enough exercise. He previously saw a registered dietician for one visit for carbohydrate counting when he was diagnosed with type 2 diabetes.
-
Medications:
Metformin 1000 mg BID
Losartan 100 mg QD
Hydrochlorothiazide 25 mg QD
Glyburide 10 mg BID
Escitalopram 20 mg QD
Aspirin 81 mg QD
-
Lifestyle history:
Diet: Patient skips breakfast with his first meal between 1:00 and 2:00 pm when he usually eats with clients or at his desk. He snacks around 4:00 pm on food around the workplace and then eats dinner at 7:30 pm with his family.
Physical activity: Limited to activities of daily living. He has a treadmill in the basement but does not use it.
Physical examination:
Weight: 236 pounds; height: 70 inches; BMI: 34.0 kg/m2; waist circumference: 41 inches
BP: 140/88 mm Hg
HR: 92 bpm
Palpable crepitus of both knees
Remainder of the examination is unremarkable
Labs
Fasting blood sugar (FBS): 122 mg/dL
A1C: 7.0%
Blood urea nitrogen: 19 mg/dL
Estimated glomerular filtration rate: 73 mL/min/1.73 m2
Lipids:
Total cholesterol (TC): 182 mg/dL
Low‐density lipoprotein (LDL‐C): 90 mg/dL
Triglycerides (TG): 181 mg/dL
High‐density lipoprotein (HDL‐C): 38 mg/dL
C.2. CASE 1 QUESTIONS
- What is the focus of your attention at this time?
- No changes are indicated. He is in good reasonable control.
- Focus primarily on improved hypertension control because this is his major concern.
- Focus primarily on improved diabetes control because he is not at goal.
- Focus primarily on weight loss because his blood pressure and glucose should favourably respond. (correct answer)
- What dietary recommendations would you make at this time?
- Give him practical tips on healthy eating. (correct answer)
- Refer to registered dietitian (RD) for medical nutrition therapy.
- Prescribe 2 meal replacement shakes +1 meal per day.
- Refer to Weight Watchers.
- Recommend that he join an internet‐based programme, such as eDiets.
- The patient follows your nutritional advice and has a better understanding of calories, carbohydrates, and energy balance. He returns within 1 month for follow‐up and weighs 232 pounds. His blood pressure is 138/86 mm Hg and fasting glucose is 118 mg/dL. The patient asks what the next steps are regarding his medication management. What medication would you consider as the best option for this patient?
- Lorcaserin
- Phentermine/topiramate ER
- Phentermine
- Naltrexone SR/bupropion SR
- Orlistat
- Liraglutide 1.8 mg or 3.0 mg (titration) (correct answer)
- Dapagliflozin 5 mg QD
- Through shared decision‐making, you decide on adding the additional medication. Over the next 6 months, the patient loses 30 pounds (13% of initial body weight), making his new BMI 29.5 kg/m2. His blood pressure improves to 130/82 mm Hg, and his labs include: Glucose 88 mg/dL, A1C 6.2%, TC 174 mg/dL, LDL‐C 104 mg/dL, HDL‐C 42 mg/dL and TG 95 mg/dL. What do you recommend at this time?
- No changes ‐ stay the course.
- Discontinue hydrochlorothiazide and losartan.
- Discontinue glyburide. (correct answer)
- Discontinue the added medication.
- Add an additional medication for further weight loss.
Evaluation of the obesity summit using Moore's outcomes framework (level 2)
On a scale of 1 to 5, with 5 being the highest rating, please choose the number that best describes your reaction to the following statements:
Overall, the activity supports achievement of the identified learning objectives.
The activity better prepared me to care for my patients.
The content covered was useful and relevant to my practice.
The activity addressed and provided strategies for overcoming barriers to optimal patient care.
The activity reinforced my current practice patterns.
Please rate your reaction to the following statements (Yes/No/Not Applicable):
Further activities concerning this subject matter are necessary.
The activity was presented objectively and was free of commercial bias.
I would recommend this activity to my peers.
This activity increased by knowledge about the subject matter.
The activity increased my competence in managing these patients.
This activity will improve my performance in caring for patients.
This activity will improve patient outcomes in my practice.
This activity provided me with resources to use in my practice and/or with my patients.
It allowed me to interact with my peers and faculty.
It provided information in ways that I can review again later.
It gave me the opportunity to apply information to the realistic scenarios I confront in practice.
It facilitated the sharing of experiences and best practices.
As a result of this activity, please choose Yes, No, Already Do So or NA if I plan to make the following changes:
I am more likely to assess and evaluate patients routinely for overweight and obesity.
I am more likely to consider pharmacology for the management of patients with obesity.
I am more likely to use a comprehensive therapeutic approach to induce and maintain weight loss in patients with overweight and obesity.
Qualitative questions collected 180 days post‐activity
- Please indicate your degree:
- MD
- DO
- MD, PhD
- MBBS
- Other: Please indicate
-
Please indicate your primary specialty:
Family Medicine/General Practice
Internal Medicine
Endocrinology
Ob/Gyn
Other: Please indicate
-
Approximately how many patients with obesity do you see or manage per month?
1 to 9
10 to 20
31 to 50
More than 50
NA
- After participation in the Obesity Summit for Residents and Fellows, which of the following changes have you implemented in practice? (Yes; No; No, but planning to)
- Routinely assess patients for obesity.
- Address the topic of weight in patients with obesity who are not managing their disease.
- Encourage patients with obesity to implement lifestyle modifications for disease management.
- Implement effective counselling strategies in the management of patients with obesity.
- Appropriately assess and manage behavioural and psychological health in patients with obesity.
- Select patients with obesity for pharmacotherapy as appropriate.
- Refer patients for bariatric surgery as appropriate.
- Follow‐up with patients routinely.
- Stay current on evolving therapeutic strategies for the management of patients with obesity.
- Share knowledge with colleagues to provide enhanced management of patients with obesity throughout my practice.
- If you have implemented changes in your practice, which of the following patient improvements have you observed? (Yes; No; NA)
- Weight loss
- Improved self‐esteem
- Patients are more engaged in their care
- Improvements in A1C
- Patients are more adherent to weight loss plans
- Improved cholesterol or lipid panels
- More energy
- Improved behavioural or psychological health
-
In addition to the improvements above, how else have your patients with obesity benefited from your recent practice changes? Please be as specific as possible.
- Regarding your patients with overweight or obesity, please rate your confidence in your ability to: (Extremely Confident, Very Confident, Somewhat Confident, Not at all Confident)
- Provide dietary counselling
- Provide physical activity counselling
- Provide behavioural counselling
- Provide or prescribe pharmacotherapy
- Recommend bariatric surgery
- Provide follow‐up care
- These are the most significant barriers that I face in my current practice setting that may impact outcomes for patients with obesity: (Select 2)
- Lack of evidence‐based guidelines
- Limited number of effective treatments
- Limited knowledge of available agents and recommendations for use
- Lack of patient adherence
- Frequency of treatment‐related adverse events
- Cost
- Limited time to stay up to date on the latest clinical evidence
- Other (please specify)
Please provide any additional comments (free text): _______.
Velazquez A, Robinson KJH, Frederick JL, Kushner RF. Development and outcomes of an immersive obesity summit workshop for medical resident and fellow education. Clin Obes. 2019;9:e12315 10.1111/cob.12315
Funding information Vindico Medical Education
REFERENCES
- 1. Kraschnewski JL, Sciamanna CN, Stuckey HL, et al. A silent response to the obesity epidemic: decline in US physician weight counseling. Med Care. 2013;51(2):186‐192. [DOI] [PubMed] [Google Scholar]
- 2. Petrin C, Kahan S, Turner M, Gallagher C, Dietz WH. Current attitudes and practices of obesity counselling by health care providers. Obes Res Clin Pract. 2017;11(3):352‐359. [DOI] [PubMed] [Google Scholar]
- 3. Kahan S, Kushner RF. Obesity medicine: a core competency for primary care providers. Med Clin North Am. 2018;102(1):xvii‐xix. [DOI] [PubMed] [Google Scholar]
- 4.The State of Obesity. Obesity rates and trends overview. https://stateofobesity.org/obesity-rates-trends-overview/. Accessed January 30, 2018.
- 5. Lenders CM, Deen DD, Bistrian B, et al. Residency and specialties training in nutrition: a call for action. Am J Clin Nutr. 2014;99(5 suppl):S1174‐S1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Colbert JA, Jangi S. Training physicians to manage obesity—back to the drawing board. N Engl J Med. 2013;369(15):1389‐1391. [DOI] [PubMed] [Google Scholar]
- 7. Ruser CB, Sanders L, Brescia GR, et al. Identification and management of overweight and obesity by internal medicine residents. J Gen Intern Med. 2005;20(12):1139‐1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition? An evaluation of attitudes, self‐perceived proficiency and knowledge. J Am Coll Nutr. 2008;27(2):287‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smith S, Seeholzer EL, Gullett H, et al. Primary care residents' knowledge, attitudes, self‐efficacy, and perceived professional norms regarding obesity, nutrition, and physical activity counseling. J Grad Med Educ. 2015;7(3):388‐394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Antognoli EL, Seeholzer EL, Gullett H, Jackson B, Smith S, Flocke SA. Primary care resident training for obesity, nutrition, and physical activity counseling: a mixed‐methods study. Health Promot Pract. 2017;18(5):672‐680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moore DE Jr, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 2009;29(1):1‐15. [DOI] [PubMed] [Google Scholar]
- 12. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Earlbaum; 1988. [Google Scholar]
- 13. Burton AM, Brezausek CM, Agne AA, Hankins SL, Willett LL, Cherrington AL. Evaluation of a workshop to improve residents' patient‐centred obesity counselling skills. Postgrad Med J. 2016;92(1090):455‐459. 10.1136/postgradmedj-2015-133590. [DOI] [PMC free article] [PubMed] [Google Scholar]


