Summary
We assess the relative importance of demand and supply factors as determinants of regional variation in healthcare expenditures in the Netherlands. Our empirical approach follows individuals who migrate between regions. We use individual data on annual healthcare expenditures for the entire Dutch population between the years 2006 and 2013. Regional variation in healthcare expenditures is mostly driven by demand factors, with an estimated share of around 70%. The relative importance of different causes varies with the groups of regions being compared.
Keywords: healthcare expenditures, regional variation, the Netherlands, movers
1. INTRODUCTION
Regional variation in healthcare utilization and expenditures is well‐documented for many countries, and it is known to persist over time (Skinner, 2012; OECD, 2014). In this study, we look at regional variation in healthcare expenditures in the Netherlands. The Netherlands is a country with a rather standardized health system. Nevertheless, in 2013, the average individual living in the province of Limburg spent €2,181 on healthcare services included in the basic health insurance package. This figure is 24% higher than that for the province of Utrecht, where the average individual spent €1,758 in 2013.
There are many possible causes of regional variation in healthcare expenditures. These causes can be grouped into demand‐ and supply‐side factors (Skinner, 2012; Chandra & Skinner, 2012). Demand‐side factors refer to anything that is related to patients, such as health status, preferences regarding healthcare use, and level of education. Supply‐side factors, in turn, refer to regional characteristics such as the number of physicians in a region, their practice style, the availability of technology, but also factors such as regional climate and level of air pollution. This definition of demand‐ and supply‐side factors is standard in the literature on regional variation, and we follow it throughout our analysis.
Traditionally, the literature on regional variation emphasizes the role of differences in supply‐side factors such as clinical practice as main drivers of the observed variations (Phelps, 2000; Grytten & Sørensen, 2003; Chan, 2016; Cutler, Skinner, Stern, & Wennberg, 2019). Existing studies for the Netherlands focus on differences in physician remuneration schemes (Douven, Mocking, & Mosca, 2015) and variations in medical practice (Westert & Groenewegen, 1999; de Jong, Groenewegen, Spreeuwenberg, Schellevis, & Westert, 2010; de Jong, Groenewegen, Spreeuwenberg, Westert, & de Bakker, 2009). Policy measures implemented in the Netherlands aiming at reducing existing variation mainly tackle the supply side, and they reflect the idea that variations are caused by inefficient and excessive use of care in some regions. These measures include, among others, issuing detailed treatment guidelines for supply‐sensitive procedures and releasing information depicting existing variations in healthcare expenditures across regions (Wammes, Atsma, de Mann, Groenewound, & Westert, 2018). However, such policies may be failing to target some of the main causes of regional variation in healthcare expenditures, as recent studies show that demand‐side factors are an important source of regional variation for Medicare patients in the United States (Finkelstein, Gentzkow, & Williams, 2016) and for outpatient care in Germany (Salm & Wübker, 2017).
In this study, we examine the relative importance of demand and supply factors as causes of regional variation in healthcare expenditures in the Netherlands. Disentangling different causes is challenging. For example, supply factors such as physician density can also be a response to demand. One way to separate the effects of individual and environmental factors is to look at persons who migrate between different environments. This approach has become popular within health economics (see Song et al., 2010; Grytten & Sørensen, 2003; Molitor, 2018; Agha, Frandsen, & Rebitzer, 2019; Godøy & Huitfeldt, 2018) and in other fields of economics (e.g., Chetty & Hendren, 2018; Bronnenberg, Dubé, & Gentzkow, 2012). Finkelstein et al. (2016) have exploited patient migration in the context of regional variation in healthcare utilization for the Medicare population in the United States. We follow their approach, and we expand upon it, for example, by choosing comparison regions based on alternative criteria and by assessing heterogeneous effects across additional age groups.
We use two alternative empirical specifications. The first specification consists of an event‐study analysis. We follow patients over time as they move between different regions in the Netherlands, and we examine how their healthcare expenditures change at the time of move. If regional variation could be entirely attributed to patient characteristics, then healthcare expenditures should not change as patients move from a region with low average healthcare expenditures such as Utrecht to a region with high average healthcare expenditures such as Limburg. If, on the other hand, regional variation can be entirely attributed to regional characteristics then we expect individual expenditures to immediately adjust to the level of expenditures in the destination region. If both patients and regional characteristics contribute to regional variation, then the observed change in expenditures upon the move is informative about the relative importance of demand and supply factors.
Our second empirical specification is a decomposition analysis, which allows assessing whether the results from the event‐study analysis for the sample of movers hold for an alternative empirical approach based on the general population. This approach relies on a model in which healthcare expenditures are a function of regional indicators, patient demographics, individual fixed effects, and other characteristics. The estimation sample consists of both movers and nonmovers. The presence of movers in the sample allows the identification of both region and individual fixed effects.
The analysis is carried out using individual level data on annual healthcare expenditures for the entire Dutch population over an 8‐year period. One advantage of our data is that it is not restricted to a certain population group as is the case for Medicare data. The Dutch healthcare setting is interesting because it combines universal coverage, private insurance, and regulated market competition. As the United States debate over options to achieve universal coverage, some of the emerging solutions, such as the Massachusetts reforms in 2006 and the Affordable Care Act, share some of the main features of the current healthcare system in the Netherlands.
Our study makes two main contributions. First, we show that patient characteristics are the main driver of regional variation in healthcare expenditures in the Netherlands, accounting for about 70% of regional variation.
Second, our analysis shows that the relative importance of different causes of regional variation greatly depends on the regions being compared. Finkelstein et al. (2016) compare regions at different points of the distribution of healthcare utilization, and they find that the demand and supply shares are similar across comparison groups. However, demand and supply shares can vary if we compare regions based on criteria other than healthcare expenditures. If we compare regions based on the share of elderly, we find a higher demand share than if we compare regions based on supply characteristics.
The remainder of this paper proceeds as follows. The next section provides an overview of the main institutional features of the Dutch healthcare system. Section 3 introduces our dataset and provides descriptive evidence of existence and persistence of regional variation in healthcare expenditures in the Netherlands. The methods are covered in Section 4, and the results are presented in Section 5. Section 6 concludes.
2. INSTITUTIONAL SETTING
The current organization of the Dutch healthcare sector was shaped by the Health Insurance Act (Zorgverzekeringswet), which came into place in 2006. All individuals age 18 or older who live in the Netherlands are required to purchase a basic health insurance package, and those under 18 are insured through their parents. Incentives for cherry‐picking of least costly individuals by insurers are reduced via a risk‐equalization system, and insurers cannot reject anyone who wishes to purchase insurance from them. The basic health insurance package is highly standardized: All insurers are required to offer it, and plan characteristics such as the range of services covered and the level of the mandatory deductible are defined by the Dutch government.
The range of services covered by the basic health insurance package includes GP care, maternity care, hospital care, and pharmaceuticals, among others. For services not included in the basic health insurance package (i.e., most dental care for individuals over 18, eye care, etc.), individuals can purchase supplementary insurance. Insurers are free to define all plan characteristics of the supplementary health insurance packages they wish to offer. There are nine health insurance groups operating in the Netherlands. All insurers operate at the national level. Individuals do not have to change their health insurance plan when they move.
Because the Dutch healthcare system is rather standardized, one may expect little scope for variations in healthcare expenditure across regions. Supply‐side differences in healthcare expenditures can arise from different practice styles across regions, differences in the availability of technical equipment, and the concentration of healthcare providers. Another potential factor is different prices for similar services. In the Netherlands, some prices are freely negotiable between insurers and providers, whereas others are subject to price ceilings set at the national level. For example, prices for many hospital services are subject to negotiations, whereas prices for GP care are regulated at the national level. Douven, Burger, and Schut ([Link]) show substantial price variation for similar hospital products between hospitals (and within a hospital for the same product across insurers). In our empirical approach, such regional differences in prices are attributed to the supply side.
3. DATA
We use proprietary administrative data on annual individual healthcare expenditures by category of care included in the basic health insurance package for the period between the years 2006 and 2013. The data are available at the Netherlands Bureau for Economic Policy Analysis (CPB) and were assembled by Vektis, a private firm that receives and processes information from all health insurers operating in the Netherlands.
Due to the mandatory nature of basic health insurance in the Netherlands, we have information on the entire population living in the Netherlands for each of the years in our study period. A detailed description of the data cleaning process can be found in Appendix S2. Our final dataset comprises over 107 million observations, corresponding to about 14.5 million individuals, who are observed for at most 8 years.
For our baseline analysis, we measure total healthcare expenditures as the natural logarithm of total healthcare expenditures of individual i in year t plus 1, . The logarithm takes into account that the distribution of healthcare expenditures is highly skewed, and adding 1 inside the logarithm operator takes into account that individuals may incur zero healthcare expenditures during a given year. Our measure of total healthcare expenditures in the basic package excludes expenditures on mental healthcare, as this was added to the basic health insurance package starting from 2008. In robustness checks, we also consider alternative outcome variables, such as , , , the inverse hyperbolic sine of expenditures, expenditures in levels, and binary variables for being above certain expenditure percentiles.
Additionally, we separately study individual expenditures on the largest categories of care (GP care, hospital care, and pharmaceuticals) and heterogeneous effects by age and gender.
We define the relevant regions as provinces. There are 12 provinces in the Netherlands, whose population size varies between 380,000 and 3.6 million inhabitants in Zeeland and Zuid‐Holland, respectively. Figure 1 provides descriptive evidence of regional variation in individual healthcare expenditures across provinces. For this, we compute the annual average individual healthcare expenditures in each of the Dutch provinces (in € pooled for all years in our sample), and then we plot the percentage difference of these numbers relative to the national average. The difference between the lowest and highest spending provinces is about 20%. The ranking of regions is stable over time, with a Spearman correlation coefficient of 0.81 between the earlier and later periods of the data (2006–2009 and 2010–2013, respectively).
Figure 1.
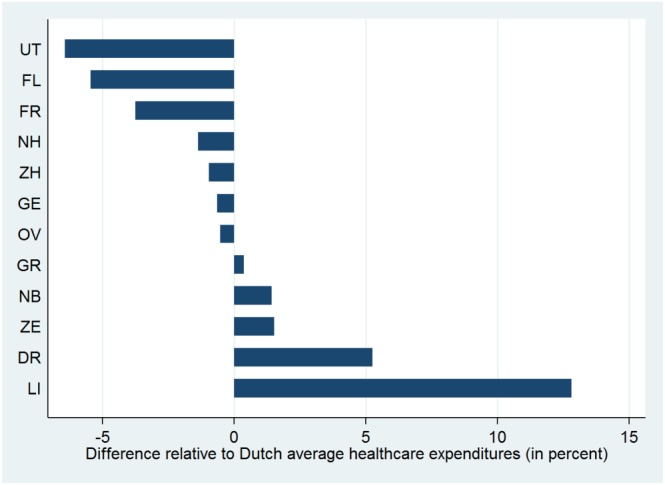
Average individual healthcare expenditure per province, relative to Dutch average. The figure displays the average individual annual health expenditure in € per Dutch province, relative to the Dutch average, for the period 2006–2013. The abbreviation of province names is as follows: DR, Drenthe; FL, Flevoland; FR, Friesland; GE, Gelderland; GR, Groningen; LI, Limburg; OV, Overijssel; NB, Noord‐Brabant; NH, Noord‐Holland; UT, Utrecht; ZE, Zeeland; ZH, Zuid‐Holland. The sample consists of 107,364,200 observations, corresponding to 15,008,220 individuals [Colour figure can be viewed at wileyonlinelibrary.com]
We define regions based on provinces for two reasons. First, provinces have distinct cultures, and Dutch individuals tend to identify strongly with their provinces. Second, we want to choose relatively large regional units in order to minimize the probability that movers will still seek care in their region of origin after a move. As an alternative definition of regions we use smaller administrative areas that are relevant for providing healthcare (GHOR regions, see Appendix S3B). In other robustness checks, we restrict our sample to individuals moving distances longer than 75 and 100 km (see Appendix S3C).
We identify movers using individual information on the four‐digit postal code of residence at the end of the year, which we match with the corresponding province. Movers are defined as individuals who move to a new province in the Netherlands only once over the time horizon under analysis. According to this definition, our estimation sample contains around 0.5 million individuals who are movers, corresponding to around 4 million observations.
A key variable for our empirical approach is the percentage difference in average individual healthcare expenditures between the origin and destination region of individual i. This variable is denoted by , where and are the average logarithm of individual healthcare expenditures plus 1 in the destination and origin province of individual i, respectively. A positive δ i therefore means that an individual moves to a province with higher average healthcare expenditures. The larger the absolute value of δ i, the larger the difference between the two provinces in terms of average healthcare expenditures. δ i can take 12×11=132 distinct values, corresponding to the number of possible paths a mover can take. All movers with the same path will have the same δ i, regardless of when they move.
Figure 2 shows the histogram of δ i, which conveys that moves take place both from high‐ to low‐expenditure regions and vice versa. The two highest bars in Figure 2 correspond to moves between Zuid‐ and Noord‐Holland. These are the provinces where the three largest Dutch cities (Amsterdam, Rotterdam, and The Hague) are located. In specifications studying GP care, hospital care, and pharmaceuticals, δ i is defined as the difference between the average of log healthcare expenditures plus 1 in each specific category of care in the origin and destination region of patient i. The corresponding histograms for the δ i exhibit a similar pattern (see online Appendix S7).
Figure 2.
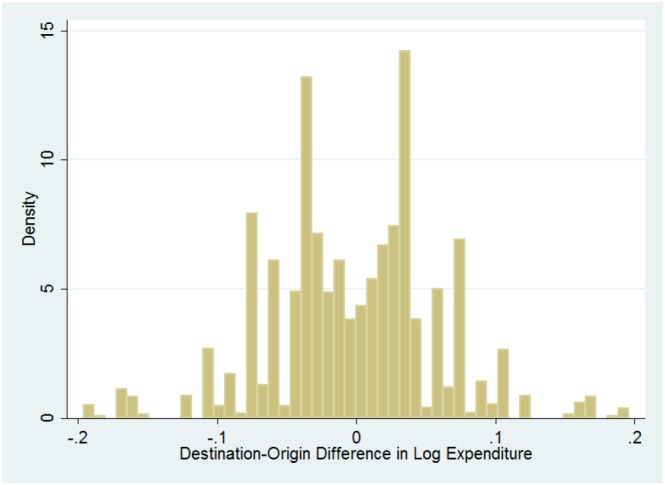
Distribution of destination‐origin difference in log health expenditure (δ i). This figure shows the histogram of δ i, the destination‐origin difference in the average log individual healthcare expenditure. Regions are defined as provinces. The histogram was built using 50 bins and the sample of all 549,500 individuals who are movers, corresponding to 4,146,945 observations [Colour figure can be viewed at wileyonlinelibrary.com]
Summary statistics for the movers and nonmovers in our sample are shown in Table 1. Movers are approximately 8 years younger than nonmovers, slightly more likely to be women, and exhibit lower healthcare expenditures than nonmovers. They are also less likely than nonmovers to have consumed any care. All these differences are statistically significant at the 5% level. Finally, movers and nonmovers are observed for about the same number of time periods.
Table 1.
Summary statistics for movers and nonmovers
| Variable | Nonmovers | Movers | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (years) | 41.08 | (22.95) | 32.78 | (18.51) |
| Gender (% of women) | 50.93 | (0.50) | 52.61 | (0.50) |
| Total healthcare expenditures, annual (€) | 1,767.70 | (5,562.78) | 1,305.85 | (4,491,30) |
| of which: | ||||
| GP expenditures, annual (€) | 129.76 | (101.52) | 116.45 | (91.97) |
| Hospital expenditures, annual (€) | 1,078.02 | (4,713.46) | 781.11 | (3,754.96) |
| Pharmacy expenditures, annual (€) | 308.81 | (1,400.29) | 203.91 | (1,239.60) |
| Any healthcare expenditures (%) | 99.4 | (0.08) | 98.9 | (0.11) |
| Any GP expenditures (%) | 99.0 | (0.10) | 98.2 | (0.13) |
| Any hospital expenditures (%) | 57.4 | (0.49) | 50.8 | (0.50) |
| Any pharma expenditures (%) | 72.3 | (0.45) | 66.8 | (0.47) |
| # individuals | 14,458,720 | 549,500 | ||
| Average # of years observed | 7.60 | 7.72 | ||
| # individual‐years | 103,217,255 | 4,146,945 | ||
Note. Numbers for “any expenditures” correspond to the percentage of individuals in our dataset who incurred positive healthcare expenditures.
4. METHODS
4.1. Event‐study analysis
The idea behind the event study is to follow movers over time and use the change in healthcare expenditures upon the year of move in order to estimate the relative importance of demand and supply factors as sources of regional variation in healthcare expenditures. We specify our baseline model as follows:
| (1) |
where y it, the outcome variable, is a measure of the healthcare expenditures incurred by individual i in year t. The main explanatory variable is δ i interacted with an indicator variable taking value 1 in years after the move and value 0 otherwise. This indicator is denoted , where τ i is the year of move for individual i. θ is the main parameter of interest, measuring the changes in healthcare expenditures y it for years after the move. θ can be interpreted as the share of regional variation in healthcare expenditures attributed to supply‐side factors.
Other independent variables included in Equation (1) are year fixed effects ζ t; indicators for years since the year of the move, included in the vector ; a vector of individual characteristics, X it, including gender and age (in bins of 5 years in order to account for nonlinear effects, separately for men and women); and unobservable individual fixed effects α i. β and κ are vectors of parameters to be estimated. Finally, ε it includes time‐varying individual characteristics that are unobservable. We estimate the model using fixed effects, with robust standard errors clustered at the individual level.
Equation (1) is estimated for the sample of movers only. Identification comes from observing individuals that move at distinct points in time and have different origin and destination regions.
For the model to be valid, we need the error term to be orthogonal to the regressors: . There are several threats to this exogeneity assumption. For example, this assumption would be violated if there are underlying time trends in individual healthcare expenditures that are systematically related to δ i. Such trends can arise if individuals with deteriorating health status tend to move to regions with higher healthcare expenditures. In this case, higher healthcare expenditures after the move could be explained by trends in unobserved health and not by the higher average healthcare expenditure in the new region. In other words, we would overestimate θ. In order to assess whether there is evidence of premove individual trends, we estimate the following generalization of Equation (1):
| (2) |
where we allow for θ to vary over time. That is, the subscript r on θ stands for year relative to move, formally r(i,t)≡t−τ i. We normalize the coefficient for the year before the move to 0 (θ −1=0). By testing whether the estimated coefficients in periods before the move are 0, one can assess whether premove trends are present. By looking at the estimated coefficients in periods after the move, we can examine the adaptation process of individuals to the new region in the sense that they might gradually adjust their healthcare expenditures towards the average healthcare expenditure in the destination region (Bronnenberg et al., 2012). In Appendix S4, we discuss other threats to the validity of the exogeneity assumption, and we show that our results cannot be explained by nonlinear effects of δ i on healthcare expenditures or by changes in the relative importance of demand and supply factors over time.
Finally, we assess heterogeneous effects by gender and age, and the robustness of our results with respect to the functional form of the outcome variable, the definition of the relevant regions, and the definition of the sample.
4.2. Decomposition analysis
In addition to the event‐study analysis, we use an alternative estimation approach based on a decomposition analysis. One advantage of using two alternative estimation approaches is that it allows us to assess the robustness of our results to a different specification. The decomposition approach also allows comparing specific regions, and it uses data for the full population, including movers and nonmovers. This approach is based on the following equation:
| (3) |
where y ijt is a measure of the healthcare expenditures of patient i living in province j at time t. This is a function of province indicators, γ j, and other variables that were previously defined. ε ijt is an error term.
Equation (3) is estimated based on data for the full population. Note that we can separately identify individual and region fixed effects (α i and γ j, respectively) due to the fact that the dataset includes movers. In case there were no movers in the dataset, then place and individual effects would be perfectly correlated. Identification of the region‐specific effects γ j comes solely from movers. As a result, we are implicitly assuming that regions affect nonmovers in the same way as they affect movers. For example, if for movers average expenditures in region a are 10% lower than in region b, then we assume that if nonmovers would counterfactually move from region a to region b, then their expenditures would also increase by 10%. Note that different levels of average expenditures between movers and nonmovers as depicted in Table 1 need not violate this assumption.
We assess the relative importance of the different causes of regional variation using the estimates for the region‐specific parameters γ j in Equation (3) in order to compare two regions or two groups of regions. Regions can be grouped in many ways. For now, let us compare two groups that we label a and b. Then, the share of regional variation in healthcare expenditures coming from the supply side is defined as follows:
| (4) |
where and are the mean of the estimation coefficients for the regions included in groups a and b, respectively. and correspond to the average predicted outcomes based on Equation (3), among individuals located in the regions included in groups a and b, respectively. Δ refers to the difference between the two groups (i.e., ). The share of regional variation attributable to patient characteristics is given by S patient=1−S region.
The relative importance of different causes of regional variation may depend on the choice of regions being compared. Finkelstein et al. (2016) group regions based on average healthcare utilization, for example, comparing the top 25% of regions in terms of healthcare utilization with the bottom 25%, and they find that causes of variation are constant for different comparison groups. Yet the causes of variation could be different if we choose comparison regions based on criteria other than healthcare utilization. This can be the case if the influence of demand and supply factors is not proportional. For example, we expect a high demand share if we compare regions that differ widely in their demographic structure but are similar in supply characteristics. In our study, we alternatively group regions based on healthcare expenditures, demographics and supply characteristics. Specifically, we compare the following groups of regions: (a) provinces above the median healthcare expenditure in the Netherlands with those below the median; (b) provinces above the 75th percentile of the expenditure distribution with those below the 25th percentile; (c) provinces above the 75th percentile in terms of share of elderly population (65+) with those below the 25th percentile and; (d) provinces above the 75th percentile in terms of estimated region fixed effects ( ) with those below the 25th percentile.
5. RESULTS
5.1. Event‐study analysis
We report our event‐study results in Table 2, for the baseline specification, for specific categories of care, and for the analysis of heterogeneous effects across distinct population groups. We only present the estimates of θ, the coefficient of interest. For total healthcare expenditures, the estimated coefficient of interest is 0.274, meaning that the share of regional variation attributed to supply factors is 27.4%. The remaining 72.6% correspond to the share of regional variation attributed to the demand side. This demand share is higher than the 50% share attributable to patients for healthcare utilization of Medicare beneficiaries in the United States (Finkelstein et al., 2016), but it is lower than the 80–90% share attributable to patients for outpatient care utilization in Germany (Salm & Wübker, 2017). The relative importance of demand‐ and supply‐side factors as sources of regional variation differs little across different categories of care. We find evidence that the relative importance of supply‐side factors is about twice as large for women than for men (38.9% vs. 17.8%) but find no statistically significant differences between distinct age groups.
Table 2.
Results from the event‐study analysis: estimates of θ
| Model | Estimate | SE |
|---|---|---|
| Baseline | ||
| θ, total expenditures | 0.274*** | 0.026 |
| By type of care | ||
| θ, GP expenditures | 0.214*** | 0.027 |
| θ, hospital expenditures | 0.266*** | 0.025 |
| θ, pharmaceutical expenditures | 0.282*** | 0.014 |
| By gender | ||
| θ, men | 0.178*** | 0.033 |
| θ, women | 0.389*** | 0.037 |
| By age group | ||
| θ, age <18 | 0.430*** | 0.062 |
| θ, 18≤ age < 40 | 0.445*** | 0.027 |
| θ, age ≥65 | 0.263** | 0.125 |
Note. Estimates of θ based on Equation (1). For total expenditures, the dependent variable is log(total expenditures+1), unless otherwise stated. For the regressions by category of care, the dependent variables are log(GP expenditures+1), log(hospital expenditures+1), and log(pharma expenditures+1) for expenditures with GP care, hospital care, and pharmaceuticals, respectively. Regressions assessing heterogeneous effects use δ i for the corresponding population group and regressions for distinct types of care use δ i for the corresponding category of care. The number of observations is 4,146,945, corresponding to all 549,500 individuals who are movers. Standard errors are robust standard errors, clustered at individual level.
* Significant at 10%.
** Significant at 5%.
*** Significant at 1%.
The results from the estimation of Equation (2) are summarized in Figure 3, where we plot the estimated year‐specific coefficients θ r and their corresponding 95% confidence interval. There is evidence of a small pretrend, with the coefficients for 2 and 3 years before the year of move being individually statistically different from 0 at 5%. In some robustness checks, premove coefficients are also significantly negative, suggesting that our estimates may be overstating the supply share (see Figure Appendix S3A). We find no evidence of a gradual adjustment of healthcare expenditures after the move as the coefficients for periods after the move are not significantly different from each other at any conventional significance level. Since we find some evidence of pretrends, we also perform an additional robustness check that restricts the sample alternatively to 1, 2, and 3 years around the move, and we obtain results that are similar to the baseline (see Table Appendix S4A).
Figure 3.
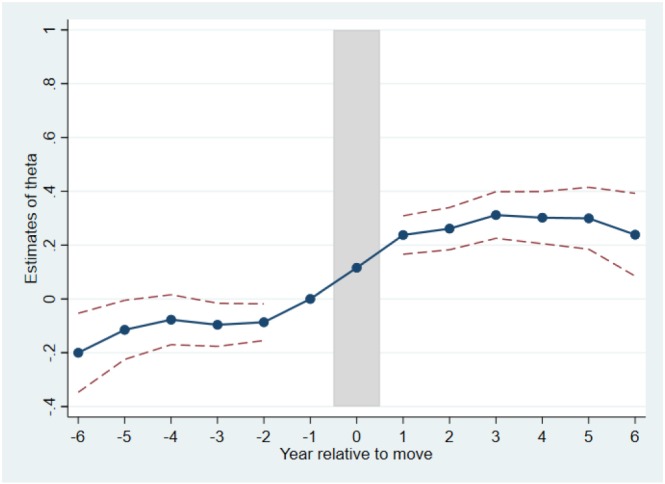
Assessment of premove and postmove trends. The figure plots the estimated coefficients θ r based on Equation (2). The coefficient for the year just before the move, r=−1, was normalized to 0. The solid line connects all estimated coefficients, and the dashed lines connect the upper and lower bounds of their 95% confidence intervals. The sample consists of all 549,500 individuals who are movers [Colour figure can be viewed at wileyonlinelibrary.com]
Overall, our event‐study results are robust to alternative functional forms of the outcome variable (Appendix S3A), alternative definitions of regions (Appendix S3B), and alternative definitions of the sample (Appendix S3C).
5.2. Decomposition analysis
The results for the decomposition analysis of total healthcare expenditures are reported in Table 3. In general, the results show that most regional variation in total healthcare expenditures is driven by demand rather than supply‐side characteristics. Demand explains about 70% of the difference in healthcare expenditures between provinces in the top and bottom 25% of the expenditure distribution. This is consistent with our findings from the event‐study analysis. When comparing provinces above and below the median of the expenditure distribution, patients explain only 56% of the variation. The estimated shares of demand and supply vary widely with the choice of comparison regions. If we compare regions based on the share of elderly population in the region, we find that 87% of regional variation can be attributed to the demand side. In contrast, when comparing regions with large differences in supply characteristics, only 18% of total variation is explained by demand‐side factors. These results quantify how the relative importance of different causes of regional variation depends on the choice of comparison regions, suggesting that the influence of demand and supply factors is not proportional across regions (see the discussion in Section 4.2 and in footnote 7).
Table 3.
Additive decomposition of log total healthcare expenditures
| Above/below median | Top/bottom 25% | High/low | High/low | ||
|---|---|---|---|---|---|
| expenditure | expenditure | share elderly |
|
||
| Difference in overall log total expenditure | |||||
| Overall ( ) | 0.068 | 0.139 | 0.129 | 0.107 | |
| Due to place ( ) | 0.030 | 0.044 | 0.017 | 0.087 | |
| Due to patients | 0.038 | 0.095 | 0.112 | 0.020 | |
| Share of difference due to | |||||
| Place | 0.444 | 0.313 | 0.129 | 0.816 | |
| Patients | 0.556 | 0.687 | 0.871 | 0.184 | |
| (0.042) | (0.036) | (0.149) | (0.044) | ||
| 95% CI for patient share | [0.474, 0.638] | [0.616, 0.757] | [0.579, 1.163] | [0.098, 0.270] | |
Note. Results based on Equation (3) with y ijt=log(total expenditure+1). The columns indicate the groups of provinces being compared. The first row shows the difference in average log expenditure between the two groups of provinces; the second and third rows report the difference in average log expenditure due to place and patients, respectively; Rows 4 and 5 report the estimated shares attributable to supply (place) and demand (patients), respectively; finally, Rows 6 and 7 show the standard errors for the patient share and the corresponding 95% confidence interval. The standard errors for the patient share are obtained by bootstrapping with 50 repetitions drawn at the individual level. The sample consists of movers and nonmovers and excludes the year of move, amounting to 106,814,700 observations.
Results for the decomposition analysis by type of care are similar to those of the event‐study analysis. In almost all specifications, the demand share dominates the supply share, and the groups of regions being compared have a substantial impact on the results. Detailed results from the decomposition analysis by type of care and by GHOR regions are presented in Appendices S5 and S6.
An alternative way to assess the magnitude of supply‐side variation is to estimate how much expenditures could be reduced if all region effects would be equalized at the 25th percentile of the distribution of region fixed effects. We find that equalizing region effects in this way results in a 2.8% reduction in healthcare expenditures. Given a mean annual expenditure per person of €1,767.70 (see Table 1), this implies a reduction of €49.50 per person and year.
The results from the event‐study analysis and the decomposition analysis are generally similar but not exactly the same. This is due to the fundamentally distinct nature of these two approaches. The event‐study analysis is restricted to movers, relates the change in expenditures upon the move to the difference in average expenditures between regions, and averages the patient share across all movers. In contrast, the decomposition analysis makes use of the full sample of individuals, estimates region fixed effects, and compares the patient share between two specific groups of regions.
6. CONCLUSION
In this study, we exploit patient migration in order to examine the relative importance of supply and demand factors as causes of regional variation in healthcare expenditures in the Netherlands. We use two alternative empirical approaches, an event‐study analysis and a decomposition analysis. Our results from the event‐study analysis suggest that regional variation is mostly demand driven, with an estimated demand share of around 0.7. Overall, the decomposition analysis conveys a similar picture, with demand‐side factors accounting for a larger share of regional variation in most of our specifications. Even completely equalizing supply‐side factors at the level of the 25th percentile of all provinces would result in only modest savings of around 2.8% of healthcare expenditures in the basic package. Our findings contribute to the Dutch policy debate. We aim at raising awareness that demand‐side differences account for the largest share of the observed variations.
We further show that the relative importance of different factors depends on the regions being compared. Demand factors are more important if we compare regions with large differences in the share of older people, whereas supply factors are more important if we compare regions with large differences in supply characteristics. Our results add to the evolving understanding that causes of regional variation in healthcare expenditures can vary by context and institutional setting.
Supporting information
Appendix S1. Regions compared in the decomposition analysis
Appendix S2. Details on the dataset and data cleaning process
Appendix S3. Additional analysis using the event‐study framework
Table Appendix S3A: Event‐study Analysis: estimates of θ for alternative outcome variables
Figure Appendix S3A: Assessment of pre‐ and post‐move trends for alternative outcome variables
Table Appendix S3B: Event‐study Analysis: estimates of θ using GHOR regions
Table Appendix S3C: Event‐study Analysis: estimates of θ , additional robustness checks
Appendix S4. Assessment of threats to the exogeneity assumption
Figure Appendix S4A: Testing the linearity assumption on δi
Table Appendix S4A: Event‐study Analysis: estimates of θ, assessing model assumptions
Appendix S5. Decomposition Analysis per type of care
Table Appendix S5: Additive decomposition by type of care, GP and Hospital
Appendix S6. Decomposition Analysis using GHOR regions
Table Appendix S6: Additive decomposition of log total healthcare expenditures using GHOR regions
Appendix S7. Histograms of δi by type of care
Figure Appendix S7: Distribution of destination‐origin difference in expenditures by type of care (δi)
OnlineAppendix.tex
ACKNOWLEDGEMENTS
We thank Pilar García‐Gómez, Leida M. Lamers, Maarten Lindeboom, Silvana Robone, and seminar participants at Tilburg University, the CPB, the 4th EuHEA PhD Student‐Supervisor Conference in Lausanne, the 15th Portuguese Health Economics Conference in Coimbra, the LolaHESG in Hoenderloo, and the 12th European Conference on Health Economics in Maastricht for their valuable comments.
Moura A, Salm M, Douven R, Remmerswaal M. Causes of regional variation in Dutch healthcare expenditures: Evidence from movers. Health Economics. 2019;28:1088–1098. 10.1002/hec.3917
Footnotes
These figures are based on own calculations from our data and exclude expenditures on mental healthcare. The magnitude of regional variation is similar to Germany, where average healthcare expenditures for publicly insured individuals vary by about 20% between states (Göpffarth, Kopetsch, & Schmitz, 2016). According to Reich, Weins, Schusterschitz, and Thöni (2012), variations in health expenditures per capita between Swiss cantons are of much larger magnitude, reaching 146% between Geneva (6,308CHF) and Appenzell Inner‐Rhodes (2,562CHF). In the United States, variation in personal healthcare spending per capita reaches 247% between the state of Massachusetts (6,683USD) and Utah (1,926USD), as discussed in Martin et al. (2007).
An overview of the Dutch healthcare system is provided in van Kleef, Schut, and van de Ven (2014), Schut and Varkevisser (2016) (in Dutch), and Kroneman et al. (2016) (in English).
The number of individuals without basic health insurance is very low, mostly because insurance is mandatory. Also, uninsured individuals are actively tracked down and fined. As of 2013, there were only about 28,000 uninsured individuals in the Netherlands (Kroneman et al., 2016), corresponding to 0.2% of the population above age 18.
The inclusion of indicators for years since the move accounts for direct effects of moving that might affect health and are unrelated to δ i, for example, caused by the hassle of moving.
Specifically, for each group, we compute a group‐specific δ. For example, when studying heterogeneous effects by gender, the estimated equation is , where I w and I m are group indicators and θ w and θ m are group‐specific supply‐share parameters to be estimated. Thus, we compare men (women) with other men (women) who move at different points in time and to different destinations.
For the decomposition approach, we always have to choose two regions or groups of regions which we compare. This is because the γ j coefficient for one of the regions is normalized to 0 when estimating Equation (3), meaning that only the differences between γ js are informative.
To illustrate this with an example, consider a country with four regions: Region A has a large share of elderly in the population (high demand) and few physicians (low supply). Region B has a large share of elderly (high demand) and many physicians (high supply). Region C has a low share of elderly (low demand) and few physicians (low supply). Region D has a low share of elderly (low demand) and many physicians (high supply). Depending on how we group these regions, we will find different demand shares. For example, if we compare Regions A and C, we will find a high demand share. In contrast, if we compare Regions A and B, we will find a low demand share.
For log(total expenditures+1), provinces above the median are Flevoland, Zuid‐Holland, Noord‐Brabant, Zeeland, Limburg, and Drenthe; provinces above the 75th percentile are Zeeland, Limburg, and Drenthe; provinces below the 25th percentile are Utrecht, Gelderland, and Friesland. Provinces above the 75th percentile in terms of share of elderly population are Zeeland, Limburg, and Overijssel. Provinces below the 25th percentile in terms of share of elderly population are Noord‐Holland, Flevoland, and Utrecht. Finally, provinces above the 75th percentile in terms of estimated region fixed effects are Flevoland, Zeeland, and Limburg. Provinces below the 25th percentile in terms of estimated region fixed effects are Groningen, Drenthe, and Gelderland. See Appendix S1 for the relevant maps.
Estimated coefficients start to increase in the year prior to the move. Such a pattern could be explained by delays in updating addresses by the insurer. However, this is unlikely in the Netherlands. Movers must register with the new municipality within the first 5 days after the move or face a fine of €325. Municipalities automatically forward the new address to the health insurer. However, it is possible that people already use care in the destination region before they officially move, for example, if they move only some time after starting a job or when they have a new relationship in the destination region.
REFERENCES
- Agha, L. , Frandsen, B. , & Rebitzer, J. B. (2019). Fragmented division of labor and healthcare costs: Evidence from moves across regions. Journal of Public Economics, 169, 144–159. [Google Scholar]
- Bronnenberg, B. J. , Dubé, J.‐P. H , & Gentzkow, M. (2012). The evolution of brand preferences: Evidence from consumer migration. American Economic Review, 102(6), 2472–2508. [Google Scholar]
- Chan, D. C. (2016). Informational frictions and practice variation: Evidence from physicians in training. (Working Paper 21855). Cambridge, MA: National Bureau of Economic Research. [Google Scholar]
- Chandra, A. , & Skinner, J. (2012). Technology growth and expenditure growth in health care. Journal of Economic Literature, 50(3), 645–680. [Google Scholar]
- Chetty, R. , & Hendren, N. (2018). The impacts of neighborhoods on intergenerational mobility I: Childhood exposure effects. The Quarterly Journal of Economics, 133(3), 1107–1162. [Google Scholar]
- Cutler, D. , Skinner, J. , Stern, A. D. , & Wennberg, D. (2019). Physician beliefs and patient preferences: A new look at regional variation in health care spending. American Economic Journal: Economic Policy, 11(1), 192–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong, J. , Groenewegen, P. , Spreeuwenberg, P. , Schellevis, F. , & Westert, G. (2010). Do guidelines create uniformity in medical practice? Social Science & Medicine, 70, 209–216. [DOI] [PubMed] [Google Scholar]
- de Jong, J. , Groenewegen, P. , Spreeuwenberg, P. , Westert, G. , & de Bakker, D. (2009). Do decision support systems influence variation in prescription? BMC Health Services Research, 9, 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douven, R. , Burger, M. , & Schut, E. (forthcoming). Does managed competition constrain hospitals' contract prices? Evidence from the Netherlands. Health Economics, Policy and Law. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douven, R. , Mocking, R. , & Mosca, I. (2015). The effect of physician remuneration on regional variation in hospital treatments. International Journal of Health Economics and Management, 15(2), 215–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein, A. , Gentzkow, M. , & Williams, H. (2016). Sources of geographic variation in health care: Evidence from patient migration. Quarterly Journal of Economics, 131(4), 1681–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godøy, A. , & Huitfeldt, I. (2018). Regional variation in healthcare utilization and mortality. (Discussion Paper 890). Oslo: Statistics Norway, Research Department. [Google Scholar]
- Göpffarth, D. , Kopetsch, T. , & Schmitz, H. (2016). Determinants of regional variation in healthcare expenditures in Germany. Health Economics, 25(7), 801–815. [DOI] [PubMed] [Google Scholar]
- Grytten, J. , & Sørensen, R. (2003). Practice variation and physician‐specific effects. Journal of Health Economics, 22(3), 403–418. [DOI] [PubMed] [Google Scholar]
- Kroneman, M. , Boerma, W. , van den Berg, M. , Groenewegen, P. , de Jong, J. , & van Ginneken, E. (2016). Netherlands: Health system review. Health Systems in Transition, 18(2), 1–239. [PubMed] [Google Scholar]
- Martin, A. B. , Whittle, L. , Heffler, S. , Barron, M. C. , Sisko, A. , & Washington, B. (2007). Health spending by state of residence, 1991‐2004. Health Affairs, 26(6), w651–w663. [DOI] [PubMed] [Google Scholar]
- Molitor, D. (2018). The evolution of physician practice styles: Evidence from cardiologist migration. American Economic Journal: Economic Policy, 10(1), 326–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD (2014). Geographic variations in health care: What do we know and what can be done to improve health system performance? Paris:OECD Publishing. [Google Scholar]
- Phelps, C. E. (2000). Information diffusion and best practice adoption In Culyer A. J., & Newhouse J. P. (Eds.), Handbook of health economics, Vol. 1 North Holland:Elsevier, pp. 223–264. [Google Scholar]
- Reich, O. , Weins, C. , Schusterschitz, C. , & Thöni, M. (2012). Exploring the disparities of regional health care expenditures in Switzerland: some empirical evidence. European Journal of Health Economics, 13, 193–202. [DOI] [PubMed] [Google Scholar]
- Salm, M. , & Wübker, A. (2017). Causes of regional variation in healthcare utilization in Germany. (RUHR Economic Papers 675). Bochum, Dortmund, and Essen: Ruhr‐University Bochum, TU Dortmund University, University of Duisburg‐Essen. [Google Scholar]
- Schut, E. , & Varkevisser, M. (2016). Economie van de gezondheidszorg. Houten:Bohn Stafleu van Loghum; [Google Scholar]
- Skinner, J. (2012). Causes and consequences of regional variations in health care In McGuire M. P. T. G., & Barros P. P. (Eds.), Handbook of health economics, Vol. 2 North Holland:Elsevier, pp. 45–93. [Google Scholar]
- Song, Y. , Skinner, J. , Bynum, J. , Sutherland, J. , Wennberg, J. E. , & Fisher, E. S. (2010). Regional variations in diagnostic practices. New England Journal of Medicine, 363(1), 45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Kleef, R. , Schut, E. , & van de Ven, W. (2014). Evaluatie zorgstelsel en risicoverevening acht jaar na invoering zorgverzekeringswet: Succes verzekerd?.Rotterdam: iBMG Erasmus Universiteit Rotterdam. [Google Scholar]
- Wammes, J. , Atsma, F. , de Mann, Y. , Groenewound, S. , & Westert, G. (2018). De zorg is niet overal hetzelfde; het reduceren van ongewenste verschillen in kwalliteit en kosten in Nederland In Jeurissen P., Maarse H., & Tanke M. (Eds.), Betaalbare zorg. Den Haag:Sdu Uitgevers, pp. 311–332. [Google Scholar]
- Westert, G. , & Groenewegen, P. (1999). Medical practice variations: Changing the theoretical approach. Scandinavian Journal of Public Health, 27, 173–180. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Regions compared in the decomposition analysis
Appendix S2. Details on the dataset and data cleaning process
Appendix S3. Additional analysis using the event‐study framework
Table Appendix S3A: Event‐study Analysis: estimates of θ for alternative outcome variables
Figure Appendix S3A: Assessment of pre‐ and post‐move trends for alternative outcome variables
Table Appendix S3B: Event‐study Analysis: estimates of θ using GHOR regions
Table Appendix S3C: Event‐study Analysis: estimates of θ , additional robustness checks
Appendix S4. Assessment of threats to the exogeneity assumption
Figure Appendix S4A: Testing the linearity assumption on δi
Table Appendix S4A: Event‐study Analysis: estimates of θ, assessing model assumptions
Appendix S5. Decomposition Analysis per type of care
Table Appendix S5: Additive decomposition by type of care, GP and Hospital
Appendix S6. Decomposition Analysis using GHOR regions
Table Appendix S6: Additive decomposition of log total healthcare expenditures using GHOR regions
Appendix S7. Histograms of δi by type of care
Figure Appendix S7: Distribution of destination‐origin difference in expenditures by type of care (δi)
OnlineAppendix.tex


