Abstract
Meeting nutritional needs of children with food allergy (FA) may be challenging without affordable, quality foods. Food purchase location may impact availability of FA-safe foods; however, no research examining food purchase location in families of children with FA exists. This study compared caregiver report of food insecurity (FIS; food insecure vs. food secure), FA risk, and history of food-induced anaphylaxis (FIA) in families of children with FA, who primarily purchase food items at grocery/supermarkets (n = 140) or convenience marts/bodegas (CB; n = 32). Caregivers (N = 172; 49% mothers, 49% fathers, 2% grandparent/other relative) of children with FA (57% male; Mage = 7.5 years; 66% White [22% Latinx and 44% non-Latinx] and 23% Black) completed an online survey. Variables included demographics, history of FIA, and caregiver perceptions of FIS and FA risk. Caregivers who purchased food items from CB versus supermarkets reported higher perceived risk of accidental ingestion (χ2 = 20.49, p < .001, 94% vs. 50%), severe reaction (χ2 = 15.05, p < .001, 97% vs. 61%), death (χ2 = 27.48, p < .001, 91% vs. 49%), FIS (χ2 = 21.69, p < .001, 94% vs. 49%), and FIA (χ2 = 11.96, p = .001, 94% vs. 32%). Effect sizes were small–moderate (Cramer’s V = .26–.40). Families who purchased food at CB reported greater food allergen concerns and FIS than families who purchased food at supermarkets. Differences in FA-related perceived risks may reflect the health disparity and adversity these families face to meet basic nutritional needs, such as FA-related constraints. Point-of-care efforts are needed to provide early screening for families who may be at risk for experiencing FIS.
Keywords: Food-induced anaphylaxis, Food insecurity, Food allergy, Food allergen exposure
Caregivers of children with food allergy may experience food insecurity and food purchase location may limit the ability to purchase allergen safe foods.
Implications.
Practice: Many families of children with food allergy report food insecurity and increased concerns about food allergen exposure, so practitioners should routinely assess for food insecurity at point of care.
Policy: Policymakers who want to decrease the incidence of food insecurity in pediatric food allergy should explore supplemental options for providing additional nutritional resources to families of children with food allergy, despite household income.
Research: Continued research is needed to examine and identify specific predictors outside of household income (e.g., medical costs), which may increase food insecurity risk in pediatric food allergy, to identify potential areas for intervention.
INTRODUCTION
In the United States, food allergy affects around 4%–8% of children [1] and is increasing in prevalence [2, 3]. The financial costs and emotional stress of food allergy increase burden for many families [4]. Over the past decade, numerous studies have highlighted the various difficulties families face when managing a pediatric food allergy (e.g., decreases in health-related quality of life (e.g., school restrictions [5, 6]), increased anxiety and/or stress associated with meal preparation [7, 8], and time required to complete daily activities associated with illness management (e.g., restaurants, travel, caution outside of the home environment [9–11]). The cost of managing pediatric food allergy may also be a significant burden for many families. Gupta and colleagues [1] conducted a nationally representative survey of caregivers of children with food allergy in the United States and estimates indicated that direct medical costs were approximately $3.8 billion annually (e.g., copayments, medications) and purchasing allergen-free foods costs were $1.7 billion annually [1]. Thus, this significant out-of-pocket financial burden for medical and food costs (around $4,184 per year per child [1]) may affect a family’s ability to purchase or meet the nutritional and allergen-free needs of all family members. However, limited research [12, 13] has focused on the impact these financial constraints have on the ability to purchase allergen-safe foods. This study aims to provide a preliminary examination of the associations between food purchase location, food insecurity, and perceived risks of food allergen exposure among a convenience sample of caregivers of children with food allergy.
The U.S. Department of Agriculture identifies food insecurity as the uncertainty of having, or the inability to acquire, enough food for all household members because of financial or resource constraints [14, 15]. In the United States, it is estimated that one in five households are food insecure [15]. Reduced access to food is associated with poor health outcomes and decreased health care access for children [13, 16]. Therefore, allergen avoidance may be particularly challenging for food-insecure families. In a sample of caregivers of children with food allergies, many reported greater barriers to obtain food, and 21% reported food insecurity [13]. Decreased access to food may result in increased frequency or perceived risk of allergic reactions [12]. However, higher socioeconomic and educational status may not necessarily augment access like food [12]. Increased food allergy-specific expenditures (e.g., epinephrine pens, allergen-free foods) may place all families at greater risk for food insecurity.
Food insecurity is an understudied phenomenon in pediatric food allergy and the inability to access or purchase allergen-free foods could place children with food allergy at risk for allergen exposure. Over the past several decades, pediatric hospitalizations for food allergy have more than doubled [17, 18] and as such, increases in associated health care costs have also substantially increased [2, 17–20]. Allergic reactions to food can vary from mild reactions (e.g., hives, rash) to the most severe reaction and potentially life threatening, food-induced anaphylaxis [21–24]. As a result, the standard recommendation to families is to avoid the food allergen, which can be complicated when eating outside the home or grocery shopping in a location with limited food options (e.g., restaurants, food prepared at convenience marts or bodegas). Given the risk of allergen exposure by cross-contamination or exposure, a high level of illness management education and diligence is needed to safely reduce and avoid allergen exposure [25]. However, for families experiencing food insecurity, the risk for allergen exposure may be greater given limited options to purchase or obtain allergen-free foods.
The majority of youth diagnosed with food allergy are under the age of 12 [26, 27], therefore most caregivers assume the responsibility of allergen avoidance and are the primary purchaser of food or nutritional items. The emotional impact of an allergic reaction can leave a lasting impression on many caregivers [8, 28]. Akeson and colleagues [8] found that the majority of caregivers interviewed could describe, in-detail, the severity and frequency of their child’s reaction and report significant stress on daily activities associated with managing their child’s food allergy [8]. Alternatively, many youth denied ever having an allergic reaction and reported no daily stress or concerns with regard to managing their food allergy [8]. Given the primary role caregivers play managing their child’s food allergy and purchasing food for family consumption, assessing caregivers’ perceptions of food allergen risk associated with food purchase location is needed.
The majority of the pediatric food allergy literature has focused on examining psychosocial distress, familial and/or financial burden, and food-induced anaphylaxis in primarily White and upper-income families (e.g., over $100,000 [29]). To extend the current literature, a more diverse or representative population of children with food allergy is needed to elucidate the specific burdens or barriers families of children with food allergy experience. Therefore, the primary goal of this study is to provide a preliminary investigation of food insecurity, perceived risk of food allergen exposure, and the primary food purchase location (i.e., gas stations, convenience marts, or bodegas compared to supermarkets or grocery stores) in a diverse sample of children with food allergy. We hypothesized that food-insecure families that primarily purchased food items at gas stations, bodegas, or convenience marts would be more likely to report a history of food-induced anaphylaxis due to their limited control over food selection. Demographic characteristics (i.e., ethnicity/race, income, education, caregiver relationship to child) were also examined by food purchase location and food insecurity status, given the impact socioeconomic challenges may have on obtaining allergen-free and nutritional foods.
METHODS
Participant recruitment and data collection were conducted from January to February 2017 using Toluna, an online platform for survey research. Participants are able to register for free on the Toluna website and complete online surveys via computer- or mobile-based applications. Due to the need for research of racially and ethnically diverse samples in the food allergy literature, it was requested that Toluna recruit to oversample participants from diverse backgrounds. Based on estimates from the U.S. Census Data [30], the requested recruitment sampling parameter goal was 55% non-Hispanic/Latinx Caucasian/White, 20% Black, 5% Asian/Pacific Islander, and 20% Hispanic/Latinx. An invitation to participate in the current study with a unique identification code was sent to the participants to restrict completing the survey more than once. Recruitment was conducted across the United States because the study was accessible online. The security protocols conducted by Toluna protect participants’ personal identifiable information, which surpasses the current research standards of the Council of American Survey Research Organizations and the European Society for Opinion and Market Research.
PARTICIPANTS
Caregivers were screened for eligibility with a three-item questionnaire assessing the following: (i) being 18 years or older, (ii) fluency in English, and (iii) having a child between 1 month and 12 years of age with a diagnosed food allergy. The child’s food allergy diagnosis was determined via caregiver report. If they met study criteria, the caregivers completed informed consent and online questionnaires about location of food purchases, food insecurity, and history of food-induced anaphylaxis. After completing the study, participants received $8.00 as compensation. This study was approved by the institutional review board at the Northeastern academic medical center where the study was conducted.
Four-hundred and ninety-two caregivers completed the screener, but 226 did not meet study eligibility requirements and did not complete the rest of the study. The completed data from the eligible caregivers were examined for indications of invalid responding, such as patterned responding and completing the survey too quickly. There were no observed patterned responses. The questionnaires were estimated to be completed in 5–12 min so participants with a completion time less than 4 min were excluded (n = 53). Participants who met eligibility requirements but terminated the survey early (n = 41) were excluded for incomplete data. There were no significant statistical differences in the demographic variables (age, ethnicity/race, socioeconomic status) between caregivers who were excluded (n = 94) and those who were included in the sample for analyses (N = 172).
MEASURES
Demographics
Demographic information was provided by caregivers. Items included ethnicity, race, age, education, and gross household income. Information regarding utilization of governmental benefits (Supplemental Nutrition Assistance Program [SNAP] and Woman, Infants, and Children [WIC] program) were also collected. Please see Table 1 for additional demographic information.
Table 1.
Caregiver/child demographics
| Variable | Percent | N |
|---|---|---|
| Child age (years), M (SD) | 7.5 (Median = 8.0) | 172 |
| Relationship to child | ||
| Mother | 49 | 85 |
| Father | 49 | 83 |
| Grandparent/other relative | 2 | 4 |
| Child gender | ||
| Male | 58 | 99 |
| Female | 42 | 73 |
| Child ethnicity | ||
| Hispanic or Latinx | 22 | 37 |
| Non-Hispanic or Latinx | 77 | 135 |
| Child race | ||
| American Indian or Alaska Native | 3 | 5 |
| Asian | 4 | 7 |
| Black/African American | 23 | 40 |
| White | 66 | 114 |
| Multiracial | 4 | 6 |
| Child asthma diagnosis | 45 | 77 |
| Number of children in the household with food allergies | ||
| 1 child | 85 | 146 |
| 2 children | 13 | 22 |
| 3 or more children | 2 | 4 |
| Annual family income | ||
| Less than $10,000 | 2 | 4 |
| $10,000–19,999 | 4 | 6 |
| $20,000–29,999 | 6 | 10 |
| $30,000–39,999 | 5 | 8 |
| $40,000–49,999 | 6 | 10 |
| $50,000–59,999 | 8 | 14 |
| $60,000–69,999 | 8 | 13 |
| $70,000–79,999 | 19 | 32 |
| $80,000–89,999 | 8 | 13 |
| $90,000–99,999 | 8 | 13 |
| $100,000 and over | 29 | 49 |
| Caregiver education level | ||
| Some high school | 3 | 5 |
| High school graduate | 7 | 12 |
| Vocational school or some college | 11 | 18 |
| College degree | 41 | 71 |
| Professional or graduate degree | 38 | 66 |
| Caregiver marital status | ||
| Married/living as married | 78 | 134 |
| Separated/divorced | 4 | 6 |
| Never married | 16 | 27 |
| Widower/widowed | 1 | 2 |
| Governmental and state supplemental aid | ||
| Supplemental Nutrition Assistance Program (SNAP) utilization | 38 | 66 |
| Women, Infants, and Children (WIC) Past 12-month utilization | 34 | 58 |
| WIC 30-day utilization | 36 | 62 |
Percent of participants reported, unless otherwise noted.
Food purchase location
Caregivers reported locations where they primarily purchased food items (i.e., “Where do you typically purchase your groceries or food items?”) with response options of (i) gas stations, convenience marts, or bodegas, or (ii) supermarkets/grocery stores. Primary food purchase location assesses the availability of affordable, quality, fresh foods. For example, supermarkets/grocery stores are more likely to have greater availability of food options and healthy food items than gas stations, convenience marts, or bodegas. Participants were also asked to indicate the main reason for using this food purchase location. Responses included, “It’s easy and close to where I live,” “It’s the only location where I live,” “Best prices,” or “Fresh meats, fruits/vegetables.”
History of food-induced anaphylaxis
Information about their child’s food allergy and history of their child’s food-induced anaphylaxis were completed by caregivers. Caregivers reported the number of children within the household with food allergies, age of child’s food allergy diagnosis, history of food-induced anaphylaxis, food allergy reaction symptoms, and additional comorbid diagnoses that could have related symptoms (i.e., asthma). The occurrence of food-induced anaphylaxis was assessed by caregiver report of yes or no to “Has your child had an anaphylactic reaction? (Anaphylaxis is a severe allergic reaction that can happen very quickly).” An endorsement of yes to this item was categorized as a positive history of food-induced anaphylaxis. Epinephrine use was also assessed by caregiver report of yes or no to “Has your child ever used an Epipen?” “If yes, how many times.” The presence and severity of allergic reactions was also measured by asking parents about the occurrence of specific symptoms (e.g., vomiting, hives, itching in the throat). Please see Table 2 for a list of these allergic reactions and caregiver report of frequency.
Table 2.
Caregiver report of child food allergen symptoms
| Symptom | Ever experienced, % (N) | Most severely experienced, % (N) |
|---|---|---|
| Arrhythmia (irregular or weak heartbeat) | 5 (9) | 6 (11) |
| Appearing pale or blue | 5 (8) | 6 (10) |
| Fainting | 5 (8) | 4 (6) |
| Swelling in the face (eyes, lips) | 24 (42) | 27 (46) |
| Swelling in the mouth or tongue | 16 (28) | 20 (34) |
| Throat tightening/difficulty swallowing | 17 (29) | 19 (32) |
| Hoarseness | 11 (18) | 12 (21) |
| Difficulty breathing | 23 (39) | 16 (28) |
| Cough | 24 (41) | 20 (34) |
| Wheeze | 12 (21) | 9 (16) |
| Nausea | 15 (26) | 11 (18) |
| Stomach pain | 15 (25) | 9 (15) |
| Vomiting | 17 (29) | 19 (32) |
| Itching in the mouth | 46 (79) | 41 (70) |
| Itching in the throat | 42 (73) | 34 (58) |
| Runny nose | 38 (66) | 26 (45) |
| Sneeze | 37 (64) | 28 (48) |
| Itchy/red eyes | 37 (64) | 31 (54) |
| Itching of the skin | 47 (80) | 36 (61) |
| Redness of the skin | 42 (72) | 38 (66) |
| Increased eczema | 14 (24) | 11 (18) |
| Hives | 17 (30) | 16 (28) |
| Diarrhea | 9 (16) | 8 (13) |
| Light headed or dizziness | 8 (14) | 7 (12) |
Participants were given the option to endorse all symptoms that applied to their child’s experience. Therefore, some percentages may differ and not equal to 100%.
Food Allergy Independent Measure
The caregivers’ perceptions of their child’s food allergy severity and associated risks were assessed using the Food Allergy Independent Measure (FAIM) [31]. The FAIM is a four-item caregiver report questionnaire on a seven-point Likert scale from 1 – not at all to 7 – extremely likely. Items addressed caregivers’ perceived risk of allergen exposure, severe allergic reactions following allergen exposure, and dying as a result of allergen exposure (e.g., “What chance do you think your child has of having a severe reaction if food is accidentally ingested?”). The FAIM has good validity as a measure of caregiver report of food allergy risk (α > .70) [31]. The responses were categorized into no/low risk (i.e., 1–2 was no/low risk) and moderate/high risk (i.e., responses 3–7 was moderate/high risk) [31].
National Health and Nutrition Examination Survey – Household Food Security Questionnaire
Household food security status was measured using the National Health and Nutrition Examination Survey (NHANES) [32, 33], an 18-item questionnaire with items including food access problems, limitations, food sufficiency/food shortage, food quality, food variety, desirability of diet, and disrupted eating patterns (e.g., “We were worried whether our food would run out before we got money to buy more,” and “We couldn’t afford to eat balanced meals”). A balanced meal comprises a milk/milk product, vegetables, fruits, grains, and meat/beans. Family food security was coded as: full food security (no affirmative response on any items: 23%), marginal food security (1–2 affirmative responses: 20%), low food security (3–7 affirmative responses: 17%), and very low food security (8–18 affirmative responses: 42%). For the present analyses, food security was dichotomized into food-secure (i.e., no or marginal issues in obtaining food: n = 74, 43%) and food-insecure families (i.e., moderate to high issues in obtaining food: n = 98, 57%).
ANALYSIS PLAN
Chi-square analyses were conducted to assess differences between caregiver food purchasing location (supermarkets/grocery stores vs. gas stations, convenience marts, or bodegas) and parental perception of food allergen-related risks, food insecurity, and history of food-induced anaphylaxis. T-test analyses were conducted to assess differences in the child’s age between food security status and food purchase location. Effect sizes were demonstrated as Cramer’s V/Phi, and characterized as small (0.1), medium (0.3), or large (0.5). SPSS version 22 was used to conduct all analyses.
RESULTS
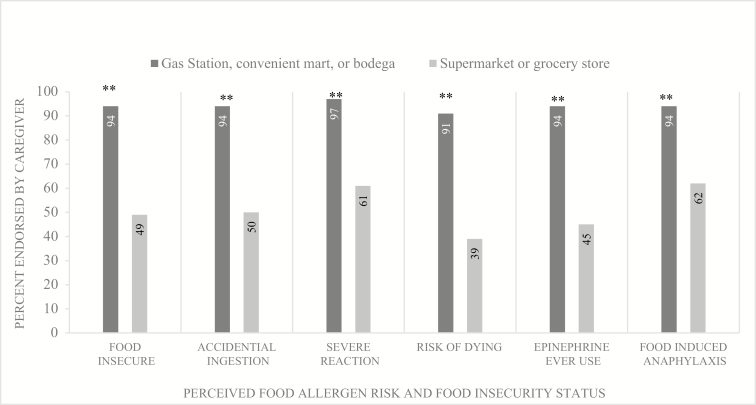
Please see Tables 1 and 2 for a summary of participant characteristics, demographics, and a summary of allergen reactions. For a visual representation of each of these findings, please see Fig. 1.
Fig. 1.
Food purchase location, food allergen risk perceptions, food security status, and history of food-induced anaphylaxis in caregivers of children with pediatric food allergy. Percentages endorsed by caregivers reflect the percent within each respective food purchase location. **Significant at p <.001.
Participant characteristics
The final sample (N = 172) was comprised of equal numbers of mothers (49%) and fathers (48%), 2% grandparent or other relative respondent, and were mostly college-educated (80% college graduate). Child race/ethnicity of consisted of Caucasian/White (66% total; 22% Hispanic/Latinx and 44% non-Hispanic/Latinx), Black (23%), Asian (4%), and American Indian/Alaska Native (3%), and 4% reported more than one race/ethnicity. All children (Mage = 7.5 years; SD = 3.1 years; 57% male) were reportedly diagnosed with food allergy prior to 6 years of age and the average age of diagnosis was 5.1 years (SD = 3.1). Sixty-eight percent of the sample reported their child had a history of food-induced anaphylaxis and 58% reported use of self-injectable epinephrine with a mean of 3.3 times (SD = 1.9). The most commonly reported food allergen symptoms were: itching in the mouth (46%), skin (47%), and throat (42%), and redness of skin (42%). Similarly, the most commonly reported severe symptoms included itching in the mouth (41%), skin (36%), and redness of skin (38%). Please see Table 2 for a full list of all symptoms reported.
Differences were observed for food security status and child gender (χ2= 4.22, p = .04; Cramer’s V = .16), such that more male children were observed in the food-insecure group than female children (food-insecure female children = 51%; food-insecure male children = 64%). No differences were observed in family food security status (i.e., food secure vs. food insecure) and gross household income (χ2= 16.53, p = .09), caregiver education (college graduate vs. high school diploma/some college; χ2= 2.41, p = .12), child ethnicity (χ2= 5.21, p = .27), or child age (t(170) = −.21, p = .84). Similar to food security status, no differences were observed for food purchase location (i.e., gas stations, convenience marts, or bodegas vs. supermarkets/grocery stores) and child age (t(170) = .84, p = .40), child gender (χ2= 2.02, p = .16), child ethnicity (χ2= 2.48, p= .29), or caregiver education (χ2= 0.54, p = .46). Caregivers in this sample reported purchasing grocery items at a supermarket/grocery store significantly more than at gas stations/convenience marts/bodegas (χ2= 18.43, p = .05; 81% vs. 19%). A large proportion of caregivers indicated utilization of governmental benefits (i.e., SNAP [38%; n = 66] and WIC [36%; n = 62]).
Lastly, given the high percentage of fathers in the present sample (49%), we also examined potential differences between caregiver respondents (i.e., mother vs. father respondents) and food purchase location, food insecurity status, perceptions of food allergen risk, and history of food-induced anaphylaxis. No differences were observed for food purchase location, food insecurity status, allergen risk (i.e., accidental ingestion or severe reaction), or history of food-induced anaphylaxis. Interestingly, father respondents perceived a greater risk of their child dying from an allergen exposure than mothers (χ2= 7.94, p = .047, Cramer’s V = .22, 58% vs. 42%). It should be noted that for the caregiver analyses, grandparent/other relative respondents were excluded given the low representation (i.e., n = 4).
Food purchase location and food insecurity
A higher frequency of caregivers who purchased food items from gas stations, convenience marts, or bodegas reported being food insecure (χ2= 21.7, p < .001, Cramer’s V = .36; 94% food insecure) compared to caregivers who purchased food items at supermarkets/grocery stores (49% food insecure).
Food purchase location and food allergen-related risks
Compared to caregivers who purchased food items at supermarkets/grocery stores, caregivers who purchased food items from gas stations, convenience marts, or bodegas reported greater perceived risk of accidental ingestion (χ2= 20.5, p < .001, Cramer’s V = .34; 94% vs. 50%), severe allergic reaction (χ2 = 15.1, p < .001, Cramer’s V = .30; 97% vs. 61%), and death (χ2= 27.5, p < .001, Cramer’s V = .40, 91% vs. 49%).
Food purchase location and food-induced anaphylaxis
Caregivers who purchased food items from gas stations, convenience marts, or bodegas reported a greater frequency of food-induced anaphylaxis than caregivers who purchased food at supermarkets/grocery stores (χ2= 11.96, p = .001, Cramer’s V = .26; 94% vs. 32%).
Food insecurity, food purchase location, and the primary reason for utilization
The majority of respondents indicated that purchasing food at their specified location (i.e., gas stations, convenience marts, or bodegas [75%]; supermarkets/grocery stores [50%]) was due to convenience (i.e., “It’s easy and close to where I live”). For participants who indicated they obtained grocery items at gas stations, convenience marts, or bodegas, 22% reported “It’s the only location where I live,” and only 3% indicated “Best prices” as the primary reason of shopping at gas stations, convenience marts, or bodegas. For respondents who endorsed supermarkets/grocery stores, 21% indicated the supermarkets/grocery stores offered the “Best prices,” 20% indicated that “Fresh meats, fruits/vegetables”, and only 9% indicated, “It’s the only location where I live,” as the primary reason of shopping at a supermarket/grocery store.
The majority of all respondents indicated that location (“It’s easy and close to where I live”) was the primary reason for utilizing their food purchase location (food secure: 58%; food insecure: 52%). For families who were food insecure, “Best prices” (26%) and “It’s the only location where I live” (16%) were the next highest endorsed reasons for food purchase location, with only 6% indicating “Fresh meat/fruits/vegetables” as the primary reasons for food purchase location. For food-secure families, “Fresh meat, fruits/vegetables” (30%) was the next highest response, with only 8% indicating “Best prices” as the primary reason for purchase location, and 4% indicating “It’s the only location where I live”.
Discussion
We sought to evaluate the association between food purchase location and (i) food security status (i.e., food secure vs. food insecure), (ii) caregivers’ perception of their child’s food allergen risk, and (iii) history of food-induced anaphylaxis in children with food allergy. First, in this sample, food insecurity was reported by the majority of caregivers (57%), regardless of household income, caregiver education (i.e., 80% college graduates), child demographic characteristics, or child age. This is consistent with the limited literature examining food insecurity in pediatric food allergy [12, 13] and may be associated with the well-documented financial burden associated with managing pediatric food allergy, including out-of-pocket medical expenses [1, 34] and special allergen-free diets [1, 7, 35]. When examining differences within purchase location, more caregivers who purchased food items from gas stations, convenience marts, or bodegas reported being food insecure (94% vs. 6%; supermarket purchase location = 51% food secure vs. 49% food insecure). Respondents indicated the primary reason for choosing to purchase food at their specified location was convenience, with over 50% of both food-secure and -insecure caregivers endorsing it. For caregivers who were food insecure, the price of food items (i.e., “Best prices,” 26%) and the lack of availability for other food purchase options (i.e., “It’s the only location where I live,” 16%) were the next highest endorsed reasons. Alternatively, food-secure families indicated “Fresh meat, fruits/vegetables” (30%) was the next highest endorsed reason. The prices of food choices (8%) and lack of purchase options (4%) were not endorsed as often for food-secure families and very few food-insecure families indicated “Fresh meat, fruits/vegetables” (6%) as a primary reason for utilizing their specified purchase location. These findings support our hypotheses and are logical given the restricted range of nutritional items for selection at gas stations, convenience marts, or bodegas. Interestingly, almost half (49%, n = 68) of families who indicated supermarkets/grocery stores as their primary food purchase location also were food insecure.
Second, greater risk of accidental ingestion (94%), severe allergic reaction (97%), and food allergen-related death (91%) were perceived by caregivers who primarily purchased food items at gas stations, convenience marts, or bodegas than families who primarily purchased food items at supermarkets or grocery stores. When examined by caregiver relationship to child (i.e., mothers compared to fathers), risk of food allergen-related death was perceived as a greater risk by fathers (58%) than mothers (42%). The association may be due to family roles (e.g., domestic, cultural, who attends medical appointments) or the perception of their child’s illness severity. Few studies have examined differences in mothers/fathers’ responsibility and perceptions regarding their child’s food allergy [36–39]. Given the underrepresentation of fathers in pediatric research [40–42], future studies should make efforts to include father or co-parent respondents to assess potential differences in their perceptions and/or behaviors related to their child’s illness. Lastly, caregivers who purchased food items from gas stations, convenience marts, or bodegas reported a higher frequency of food-induced anaphylaxis (94%). These associations highlight the limited availability of allergen-free and/or fresh, quality foods available for purchase and the risk this may place families for perceived or actual food allergen exposure and food-induced anaphylaxis. To our knowledge, these findings are the first to assess the association between food purchase location and perceived or actual food allergen exposure.
Interestingly, no differences were observed between food purchase location and food insecurity status with caregiver education, household income, child age, or ethnicity. Johns and Savage [13] found similar associations with food insecurity status, such that families with food allergy reported more difficulty accessing food when compared to families without food allergy. Additionally, Johns and Savage also demonstrated non-White children with food allergies were more likely to experience low food security and reported greater financial difficulty affording medical care and medications [13]. This may reflect food allergy-specific expenditures and difficulties these families face. Additional research, as well as longitudinal assessment, is needed to identify specific risk factors, perceptions of food-related burdens, and the disparities that may be specific to pediatric food allergy. Observed differences in perceptions of food allergy-related risks may be a consequence of the adversity these families face to meet basic nutritional needs, given the primary location of food purchase (i.e., gas stations, convenience marts, or bodegas vs. supermarkets/grocery stores). Families who typically purchase food or nutritional items at supermarkets or grocery stores likely have a wider range of allergen-free items to choose from and have the advantage to dedicate more time/resources to examine food items for potential allergens.
LIMITATIONS
While this study provides important preliminary insights of the associations of food insecurity, perceptions of food allergen risks, and food-induced anaphylaxis by food purchase location, we have several limitations to note. First, the study design is cross-sectional. Utilizing longitudinal and objective measures to assess food purchase location and food allergen-related risks or exposures is a first step in developing interventions to address these relationships and provide resources to families of children with food allergy. Caregiver report was the primary and sole means to obtain household status of food (in)security, food purchase location, and history of their child’s food allergy diagnosis and allergic reactions. Further, information was not collected about the total number of individuals in the household in order to obtain an estimate of poverty status. In the present study, caregivers provided information regarding the number of children with food allergy, household income, and marital status to determine the number of individuals in the household. Therefore, differences were examined using the total gross household income. Future studies that incorporate more rigorous methods of assessing financial status and utilization of government benefits or assistance are needed to provide a more detailed assessment of the relationship of poverty and food insecurity in larger sample of caregivers of children with food allergy.
All data were collected online and via self-report, thus we were unable to verify physician diagnosis of food allergy and age at which the child was diagnosed. Additionally, parental report of frequency of food-induced anaphylaxis and allergic reactions related to food-induced anaphylaxis is not the most rigorous method of data collection. It should be noted, however, that some studies have highlighted that the anonymity of online data collection provides respondents with more confidence and comfortability with responding to sensitive questions [43–45]. Lastly, data were not weighted to adjust for oversampling minority respondents and no information was collected regarding the geographical location of respondents or where children with food allergy received their allergy care (e.g., pediatrician, allergist/specialty care, emergency department only). It is likely that the associations identified in the present study likely represent a constellation of variables associated with both food allergy and the economics of the household. In future analyses, with larger sample sizes, it will be important to examine these variables with more rigorous statistical methods. Additionally, future studies conducted at point-of-care, that incorporate physician-confirmed allergic status and include objective methods of documenting allergen exposure, are needed to further assess the associations highlighted in the present study.
CONCLUSION
Associations between understudied variables like food (in)security, food purchase location, and perceived allergen risks were observed in this study. Future research should consider incorporating these constructs to further examine how these variables may significantly impact the management of pediatric food allergy. Specifically, this study aimed to advance the pediatric food allergy literature by examining associations between (i) food (in)security and (ii) perceptions and actual risk of allergen exposure by primary food purchase location with a representative, convenience sample of caregivers of children with food allergy. Many families reported food insecurity and increased concerns about food allergen exposure. Additionally, families who purchased food primarily at gas stations, convenience marts, or bodegas reported significantly higher perceptions of food allergen risk, food-induced anaphylaxis, and food insecurity. Continued research is needed to examine and identify specific predictors which may increase food insecurity risk in pediatric food allergy to identify potential areas of intervention.
Acknowledgments
This study was funded by internal funds provided to A. P. Tackett by the Clinical Psychology Training Consortium, Alpert Medical School of Brown University. F32 HL138734 (PI: A. P. Tackett) also provided support for A. P. Tackett.
Compliance with Ethical Standards
Conflict of Interest: The authors declare that they have no conflicts of interest.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
References
- 1. Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 2013;167(11):1026–1031. [DOI] [PubMed] [Google Scholar]
- 2. Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics. 2009;124(6):1549–1555. [DOI] [PubMed] [Google Scholar]
- 3. Sicherer SH, Sampson HA. Food allergy: a review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018;141(1):41–58. [DOI] [PubMed] [Google Scholar]
- 4. Protudjer JL, Jansson SA, Heibert Arnlind M, et al. . Household costs associated with objectively diagnosed allergy to staple foods in children and adolescents. J Allergy Clin Immunol Pract. 2015;3(1):68–75. [DOI] [PubMed] [Google Scholar]
- 5. Muraro A, Dubois AEJ, DunnGalvin A, et al. . EAACI Food Allergy and Anaphylaxis Guidelines. Food allergy health‐related quality of life measures. Allergy. 2014;69(7):845–853. [DOI] [PubMed] [Google Scholar]
- 6. Walkner M, Warren C, Gupta RS. Quality of life in food allergy patients and their families. Pediatr Clin North Am. 2015;62(6):1453–1461. [DOI] [PubMed] [Google Scholar]
- 7. Bollinger ME, Dahlquist LM, Mudd K, Sonntag C, Dillinger L, McKenna K. The impact of food allergy on the daily activities of children and their families. Ann Allergy Asthma Immunol. 2006;96(3):415–421. [DOI] [PubMed] [Google Scholar]
- 8. Akeson N, Worth A, Sheikh A. The psychosocial impact of anaphylaxis on young people and their parents. Clin Exp Allergy. 2007;37(8):1213–1220. [DOI] [PubMed] [Google Scholar]
- 9. Klinnert MD, McQuaid EL, Fedele DA, et al. . Children’s food allergies: development of the Food Allergy Management and Adaptation Scale. J Pediatr Psychol. 2015;40(6):572–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Herbert L, Shemesh E, Bender B. Clinical management of psychosocial concerns related to food allergy. J Allergy Clin Immunol Pract. 2016;4(2):205–213; quiz 214. [DOI] [PubMed] [Google Scholar]
- 11. DunnGalvin A, Koman E, Raver E, et al. . An examination of the Food Allergy Quality of Life Questionnaire performance in a countrywide American sample of children: cross-cultural differences in age and impact in the United States and Europe. J Allergy Clin Immunol Pract. 2017;5(2):363–368.e2. [DOI] [PubMed] [Google Scholar]
- 12. Tackett AP, Farrow ML, McQuaid EL. Food security, utilization of Food Assistance Programs, and caregiver perceptions of food-induced anaphylaxis risk in children with food allergies. Pediatr Allergy Immunol Pulmonol. 2018;31(2):91–96. [Google Scholar]
- 13. Johns CB, Savage JH. Access to health care and food in children with food allergy. J Allergy Clin Immunol. 2014;133(2):582–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Coleman-Jensen A, Gregory C, Singh A. Household food security in the United States in 2013 2014. Available at https://www.ers.usda.gov/webdocs/publications/45020/30968_err-141-summary.pdf?v=41165. Accessibility verified August 7, 2018.
- 15. Nord M, Andrews M, Carlson S.. Household food security in the United States, 2003. Food Assistance and Nutrition Research report. Washington, DC: US Department of Agriculture, Food and Consumer Service; 2004. [Google Scholar]
- 16. Baiardini I, Braido F, Brandi S, Canonica GW. Allergic diseases and their impact on quality of life. Ann Allergy Asthma Immunol. 2006;97(4):419–428; quiz 429. [DOI] [PubMed] [Google Scholar]
- 17. Rudders SA, Banerji A, Vassallo MF, Clark S, Camargo CA Jr. Trends in pediatric emergency department visits for food-induced anaphylaxis. J Allergy Clin Immunol. 2010;126(2):385–388. [DOI] [PubMed] [Google Scholar]
- 18. Rudders SA, Arias SA, Camargo CA Jr. Trends in hospitalizations for food-induced anaphylaxis in US children, 2000-2009. J Allergy Clin Immunol. 2014;134(4):960–962.e3. [DOI] [PubMed] [Google Scholar]
- 19. Clark S, Espinola JA, Rudders SA, Banerji A, Camargo CA. Favorable trends in the frequency of US emergency department visits for food allergy, 2001–2009. Allergy Asthma Proc. 2013;34 (5):439–445. [DOI] [PubMed] [Google Scholar]
- 20. Lin RY, Anderson AS, Shah SN, Nurruzzaman F. Increasing anaphylaxis hospitalizations in the first 2 decades of life: New York State, 1990–2006. Ann Allergy Asthma Immunol. 2008;101(4):387–393. [DOI] [PubMed] [Google Scholar]
- 21. Bohlke K, Davis RL, DeStefano F, Marcy SM, Braun MM, Thompson RS; Vaccine Safety Datalink Team Epidemiology of anaphylaxis among children and adolescents enrolled in a health maintenance organization. J Allergy Clin Immunol. 2004;113(3):536–542. [DOI] [PubMed] [Google Scholar]
- 22. Bangash SA, Bahna SL. Pediatric food allergy update. Curr Allergy Asthma Rep. 2005;5(6):437–444. [DOI] [PubMed] [Google Scholar]
- 23. Avery NJ, King RM, Knight S, Hourihane JO. Assessment of quality of life in children with peanut allergy. Pediatr Allergy Immunol. 2003;14(5):378–382. [DOI] [PubMed] [Google Scholar]
- 24. Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. 2001;155(7):790–795. [DOI] [PubMed] [Google Scholar]
- 25. Versluis A, Knulst AC, Kruizinga AG, et al. . Frequency, severity and causes of unexpected allergic reactions to food: a systematic literature review. Clin Exp Allergy. 2015;45(2):347–367. [DOI] [PubMed] [Google Scholar]
- 26. Boyce JA, Assa’ad A, Burks AW, et al. ; NIAID-Sponsored Expert Panel Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-Sponsored Expert Panel Report. J Allergy Clin Immunol. 2010;126(6):1105–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hill DA, Grundmeier RW, Ram G, Spergel JM. The epidemiologic characteristics of healthcare provider-diagnosed eczema, asthma, allergic rhinitis, and food allergy in children: a retrospective cohort study. BMC Pediatr. 2016;16:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gupta RS, Springston EE, Smith B, et al. . Food allergy knowledge, attitudes, and beliefs of parents with food-allergic children in the United States. Pediatr Allergy Immunol. 2010;21(6):927–934. [DOI] [PubMed] [Google Scholar]
- 29. McQuaid EL, Farrow ML, Esteban CA, Jandasek BN, Rudders SA. Topical review: pediatric food allergies among diverse children. J Pediatr Psychol. 2016;41(4):391–396. [DOI] [PubMed] [Google Scholar]
- 30. US Census Bureau. Annual estimates of the resident population: April 1, 2010 to July 1, 2017–2017 population estimates 2010. Available at http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml. Accessibility verified August 7, 2018.
- 31. van der Velde JL, Flokstra-de Blok BM, Vlieg-Boerstra BJ, et al. . Development, validity and reliability of the Food Allergy Independent Measure (FAIM). Allergy. 2010;65(5):630–635. [DOI] [PubMed] [Google Scholar]
- 32. Kohn MJ, Bell JF, Grow HM, Chan G. Food insecurity, food assistance and weight status in US youth: new evidence from NHANES 2007-08. Pediatr Obes. 2014;9(2):155–166. [DOI] [PubMed] [Google Scholar]
- 33. McGowan EC, Keet CA. Prevalence of self-reported food allergy in the National Health and Nutrition Examination Survey (NHANES) 2007-2010. J Allergy Clin Immunol. 2013;132(5): 1216–1219.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gupta RS, Kim JS, Springston EE, Pongracic JA, Wang X, Holl J. Development of the Chicago Food Allergy Research Surveys: assessing knowledge, attitudes, and beliefs of parents, physicians, and the general public. BMC Health Serv Res. 2009;9:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Groetch M, Nowak-Wegrzyn A. Practical approach to nutrition and dietary intervention in pediatric food allergy. Pediatr Allergy Immunol. 2013;24(3):212–221. [DOI] [PubMed] [Google Scholar]
- 36. Gillespie CA, Woodgate RL, Chalmers KI, Watson WT. “Living with risk”: mothering a child with food-induced anaphylaxis. J Pediatr Nurs. 2007;22(1):30–42. [DOI] [PubMed] [Google Scholar]
- 37. Mandell D, Curtis R, Gold M, Hardie S. Anaphylaxis: how do you live with it? Health Soc Work. 2005;30(4):325–335. [DOI] [PubMed] [Google Scholar]
- 38. Warren CM, Gupta RS, Sohn MW, et al. . Differences in empowerment and quality of life among parents of children with food allergy. Ann Allergy Asthma Immunol. 2015;114(2):117–125. [DOI] [PubMed] [Google Scholar]
- 39. Hoehn JL, Dahlquist LM, Hahn AL, Bollinger ME. Parents of children with food allergy: gender differences in perceived impact and perceived food allergy severity. J Pediatr Psychol. 2017;42(2):186–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Blumberg SJ, Halfon N, Olson LM. The National Survey of Early Childhood Health. Pediatrics. 2004;113(Suppl. 6):1899–1906. [PubMed] [Google Scholar]
- 41. Goldbeck L. Parental coping with the diagnosis of childhood cancer: gender effects, dissimilarity within couples, and quality of life. Psychooncology. 2001;10(4):325–335. [DOI] [PubMed] [Google Scholar]
- 42. Mitchell SJ, See HM, Tarkow AKH, Cabrera N, McFadden KE, Shannon JD. Conducting studies with fathers: challenges and opportunities. Appl Develop Sci. 2007;11(4):239–244. [Google Scholar]
- 43. Cantrell MA, Lupinacci P. Methodological issues in online data collection. J Adv Nurs. 2007;60(5):544–549. [DOI] [PubMed] [Google Scholar]
- 44. Duffy M. Web-based research: an innovative method for nursing research. Can Oncol Nurs J. 2000;10(2):45–49. [PubMed] [Google Scholar]
- 45. Duffy ME. Methodological issues in web-based research. J Nurs Scholarsh. 2002;34(1):83–88. [DOI] [PubMed] [Google Scholar]