Abstract
Objective
To evaluate whether improvement of proprioception, pain, or dynamic knee instability mediates the effect of wearing a soft knee brace on activity limitations in patients with knee osteoarthritis (OA).
Methods
We conducted an analysis of data for 44 patients with knee OA who were enrolled in a laboratory‐based trial evaluating the effect of wearing a commercially available soft knee brace. Activity limitations were assessed with the 10‐meter walk test and the Get Up and Go test. Knee joint proprioception was assessed by an active joint position sense test; pain was assessed on a numeric rating scale (NRS) (range 0–10); pressure pain threshold (PPT) was assessed with a hand‐held pressure algometer; dynamic knee instability was expressed by the perturbation response, i.e., a measure reflecting a deviation in mean knee varus–valgus angle after a controlled mechanical perturbation on a treadmill, with respect to level walking. Mediation analysis was conducted using the product of coefficients approach. Confidence intervals were calculated with a bootstrap procedure.
Results
A decrease in pain (scored on an NRS) and a decrease in dynamic knee instability mediated the effect of wearing a soft knee brace on the reduction of activity limitations (P < 0.05), while changes in proprioception and PPT did not mediate this effect (P > 0.05).
Conclusion
This study shows that decreased pain and reduced dynamic knee instability are pathways by which wearing a soft knee brace decreases activity limitations in patients with knee OA.
Introduction
Soft knee braces, which are elastic, nonadhesive orthoses, are often used to reduce activity limitations in patients with knee osteoarthritis (OA) 1. We recently confirmed in a laboratory‐based setting that wearing a soft knee brace indeed reduced activity limitations in patients with knee OA 2. Potential underlying mechanisms by which a soft knee brace could act on activity limitations in patients with knee OA were recently described 3. However, to our knowledge, no study has identified mechanisms that might underlie the effects of soft braces on activity limitations in patients with knee OA.
Significance & Innovations.
This is the first study that identified mechanisms underlying the beneficial effect of wearing a soft knee brace in patients with knee osteoarthritis (OA).
Decreased pain and reduced dynamic knee instability might be pathways by which wearing a soft knee brace decreases activity limitations in patients with knee OA.
This knowledge can be used to refine designs of soft knee braces intended for use in patients with knee OA.
Potential underlying mechanisms of the effect of a soft knee brace on activity limitations are the improvement of knee joint proprioception or a reduction in knee pain or knee joint instability 3. Soft braces are supposed to act on cutaneous mechanoreceptors that may contribute to improvements in proprioception 4. It has been reported that proprioception is either directly related to activity limitations in patients with knee OA or acts on activity limitations via improvement of muscle strength 5. A decrease in pain has also been suggested to underlie the effect of soft knee braces on activity limitations 6. Pain is strongly associated with activity limitations in patients with knee OA 7. Tactile stimulation provided by a soft brace can cause neural inhibition leading to the reduction of pain signals 4 and thereby to the reduction of activity limitations. Finally, it has been suggested that wearing a soft knee brace can reduce activity limitations via improvement in knee joint stability 3. Knee joint instability has been associated with activity limitations in patients with knee OA 8, 9. Although a mechanical effect is not to be expected from a soft knee brace, it has been suggested that a reduction in knee joint instability could be the result of additional sensory input from a soft knee brace, leading to improvements in proprioception 4.
Thus, we hypothesized that improvements in proprioception, pain, or dynamic knee instability mediate the effect of wearing a soft knee brace on activity limitations in patients with knee OA. The aim of the current study was to test these hypotheses.
Patients and Methods
Trial design
This was a secondary analysis of data for 44 patients with knee OA who were enrolled in a laboratory‐based experimental study. A within‐subject design was used, comparing a soft brace with no soft brace, and comparing a non‐tight brace with a tight soft brace 2. Mediation assumes that a precursor variable (i.e., soft knee brace) has an effect on a mediating variable (proprioception, pain, and joint instability), which in turn affects the outcome variable 10. To be considered a mediator, a variable needs to change because of an intervention and therefore must be measured before and after an intervention is administered 10.
Patients
Patients were recruited through telephone‐based screening between August 2015 and April 2016. Inclusion criteria for the current study were a diagnosis of knee OA according to the American College of Rheumatology (ACR) clinical criteria 11, ages 50–80 years old, and presence of self‐reported knee instability in the past 3 months. Self‐reported knee instability was defined as at least 1 episode of buckling, shifting, or giving way of the knee 9. Exclusion criteria for the current study were total knee replacement and/or inflammatory arthritis (including rheumatoid arthritis, crystal arthropathy, septic arthritis, and spondylarthropathy); radiographic patellofemoral joint OA 2; and presence of comorbidity resulting in severe activity limitations (e.g., a neurologic condition resulting in difficulty walking).
All patients provided written informed consent according to the Declaration of Helsinki. Ethics approval was obtained from the Medical Research Ethics Committee of the VU University Medical Center Amsterdam. Data extraction from the Amsterdam‐OA cohort was approved by the Slotervaart Hospital/Reade Institutional Review Board.
Intervention
A commercially available soft knee brace (GenuTex A2, Human I; Centrum Orthopedie) was used. A tight brace was defined as one that was fitted based on shank and thigh circumferences measured according to instructions provided by the distributor (standard fit). A non‐tight brace was defined as being 1 size larger than a tight brace. A full description of the fitting and positioning of the brace was provided in a previous study by our group 2.
Outcome measures
Activity limitations were assessed with 2 standardized physical performance tests: the 10‐meter walk test 12 and the Get Up and Go (GUG) test 13. The 10‐meter walk test assesses the time required to walk a distance of 10 meters along a level and unobstructed corridor 12. Patients were instructed to walk as fast as possible and were timed with a stopwatch. The GUG test measures the time it takes for an individual to get up from a chair and walk 15 meters as fast as possible along a level and unobstructed corridor 13. The intraclass correlation coefficient (ICC) of the GUG test is 0.98 for intratester reliability and 0.98 for intertester reliability 13. The 10‐meter walk test has shown excellent interrater reliability (ICC 0.980) in healthy older adults 14.
Potential mediators
Proprioception
Knee joint proprioception was assessed by the Active Movement Extent Discrimination Apparatus, which constitutes a test of an active joint position sense 15. Each patient had a familiarization session for both knees before data collection. During the familiarization session, the patients were informed that they were going to experience 5 knee movement displacement distances in order, from the smallest knee flexion (moving to position 1) to the largest knee flexion (moving to position 5), for 15 movements in total (3 times for each position). Patients thereafter undertook 30 trials, without feedback, at each site. The order of testing at the 2 sites, right knee and left knee, was randomized with computer‐generated random sequences. During each test set, trials were presented in a random sequence, 6 at each of the 5 different knee movement displacements. Specifically, while standing upright, with eyes looking forward at a point on the opposite wall, patients made an active knee flexion movement at a steady pace from a neutral standing position (full knee extension) until their patella touched the stepper motor plate. After returning to the upright position at the same pace, patients gave a verbal judgment regarding the position of the knee being tested (position 1, 2, 3, 4, or 5), and the number of correctly identified positions of the affected knee was recorded and used in the analysis. The affected knee was the one indicated as being most painful by the patient or the knee of the dominant leg in the case of similar symptoms in both knees.
Pain
Knee pain during walking on a treadmill was assessed using an 11‐point numerical rating scale (scored on an NRS), with higher scores representing more pain 16. The following question was asked during both level and perturbed walking: “On a scale from 0 to 10, how would you score the level of your left/right knee pain while walking on the treadmill?” Patients walked on the treadmill for ~2 minutes under both conditions. Data for the affected knee during level walking were used in the analysis. High test–retest reliability has been observed in patients with rheumatoid arthritis (r = 0.96) 17.
Pressure pain threshold
The pressure pain threshold (PPT) was assessed with a hand‐held pressure algometer (Wagner Instruments FDX) 18 over 3 knee test sites: 3 cm lateral to the midpoint on the lateral edge of the patella, 3 cm medial to the midpoint on the medial edge of the patella, at the center of the patella, and on 1 control site (on the tibialis anterior 5 cm distal to the tibial tuberosity). A hard rubber probe (1 cm2) was placed perpendicular to the skin, and pressure was applied at a steady pace until the patient defined the pressure as pain. The PPT was measured twice at each site, and the mean of the pressure in Newtons (N) of the 2 measurements for the affected knee was used in the analysis 19. Excellent interrater reliability of algometry (ICC 0.910) in measuring PPTs has been shown in healthy humans 20.
Dynamic knee instability
Dynamic knee instability was expressed by the perturbation response (PR) 21, a measure derived from the gait sensitivity norm 22. PR reflected deviation in the mean knee varus–valgus angle during level walking after a controlled mechanical perturbation, standardized to the mean ± SD varus–valgus angle. Mechanical perturbations on the treadmill comprised 5 lateral and 5 medial translations (2‐cm displacements) of the treadmill belts occurring during 20–50% of the gait cycle 23. PR values are positive values and reflect absolute changes. Lower PR values indicated less deviation in the mean varus–valgus angle during the stance phase of the affected (perturbed) knee. The stance phase was defined as the phase of the gait cycle from initial contact to toe‐off. PR was calculated with the equation gᵢ(k) − gᵢ¯* divided by σgᵢ* to normalize for physiologic variability during unperturbed walking in humans 22.
Equation 1: gᵢ(k) ‐ the mean varus/valgus angle of a perturbed gait cycle; gᵢ¯*‐ the mean varus/valgus angle of all unperturbed gait cycles from a baseline, level walking trial; σgᵢ* ‐ SD of the gᵢ¯*
To obtain the PR, the varus–valgus angles of the affected knee (perturbed leg) were calculated from marker data using custom‐made MatLab‐based software (BodyMech; www.bodymech.nl), with anatomic coordinate systems defined according to those described by Cappozzo et al 24. Force plate data were used to determine the stance phase of the gait cycle and the timing of perturbations. Marker position data were filtered at 6 Hz to remove high‐frequency artefacts. Force data were filtered at 10 Hz with a second order bi‐directional filter. A force threshold of 25N was used to establish gait events. All data were time‐normalized to 100% of the gait cycle (from initial contact to initial contact). Given the natural variation in gait cycle duration within (and between) patients, it was necessary to use time normalization so that a point‐by‐point comparison of information between the cycles was possible.
Other measures
The demographic and clinical characteristics of the patients were recorded prior to testing and included age, sex, body mass index (BMI), duration of symptoms, average pain last week 16, muscle strength assessed isokinetically (Nm/kg), knee OA radiographic severity (Kellgren/Lawrence grade) 25, and Western Ontario and McMaster Universities Osteoarthritis Index 26, 27. A full description of these measures was provided in a previous study by our group 2.
Procedure
Patients were subjected to 4 blocks of assessments. In the first block, the outcome measure and studied mediators were assessed while the patient was not wearing a brace. Proprioception and PPT were assessed in an examination room. Following the assessment of proprioception and PPT, the 10‐meter walk test and the GUG test were assessed in an unobstructed corridor. Subsequently, dynamic knee instability and pain (NRS) were assessed on a treadmill, which is integrated in the GRAIL system (MotekForce). The GRAIL system is made up of the treadmill with a dual belt, placed in a virtual reality environment (GRAIL system). Patients had a familiarization session on the treadmill that lasted at least 1 minute. Comfortable walking speed was determined during the familiarization session by incrementing the speed slowly until the speed was agreed upon by the patient. Following the familiarization session, patients were subjected to 2 tasks: 1) level walking for 2 minutes and 2) walking with mechanical perturbations on the treadmill. Patients were verbally informed about the mechanical perturbations prior to the task. During the walking trials, 3‐dimensional movements of the lower legs, pelvis, and trunk were captured via markers on anatomic landmarks 24 at 100 Hz using a motion‐capture system (Vicon).
After randomization to receive either a non‐tight or a tight brace, patients entered the second assessment block. Outcome measures and potential mediators were assessed while the patient was wearing a brace, while proprioception and PPT were assessed following exposure to the soft brace. The braces were worn for ~10 minutes in each of the intervention blocks. After a 30‐minute rest period, the procedure crossed over to the third and fourth blocks of the assessments comprising a second baseline trial with no brace and an intervention trial with the other type of soft brace (tight or non‐tight). The study procedure is shown in Table 1.
Table 1.
Study procedurea
| Baseline assessmentb | Intervention assessmentc | Rest, minutes | Baseline assessment | Intervention assessment |
|---|---|---|---|---|
| Outside the treadmill: | On the treadmill: | Outside the treadmill: | On the treadmill: | |
| Proprioception | Dynamic knee instabil | 30 | Proprioception | Dynamic knee instabil |
| PPT | Pain (NRS) | 30 | PPT | Pain (NRS) |
| 10‐minute walk test | Outside the treadmill: | 10‐minute walk test | Outside the treadmill: | |
| GUG test | 10‐minute walk test | 30 | GUG test | 10‐minute walk test |
| On the treadmill: | GUG test | 30 | On the treadmill: | GUG test |
| Pain (NRS) | Proprioceptiond | 30 | Pain (NRS) | Proprioceptiond |
| Dynamic knee instabil | PPTd | 30 | Dynamic knee instabil | PPTd |
Instabil = instability; PPT = pressure pain threshold; NRS = numerical rating scale; GUG = Get Up and Go test.
Without a tight or a non‐tight brace.
With a tight or a non‐tight brace.
Assessed without a soft brace applied.
Statistical analysis
Descriptive statistics were used to characterize the study population. Numbers and percents were used for categorical variables and means ± SDs were used for continuous variables. Prior to the statistical analysis, outcome measures were checked for normality with Shapiro‐Wilk and Kolmogorov‐Smirnov tests. Data on activity limitations were analyzed as person‐level variables. Data on proprioception, pain (NRS), PPT, and dynamic knee instability were analyzed as knee‐level variables, and data for the affected knee were used in the analysis. Linear mixed‐effects model analysis was used to calculate the main effect of wearing a soft knee brace on activity limitations reported in our previous study 2.
The mediation effect was analyzed under 3 conditions: 1) brace versus no brace, 2) tight brace versus no brace (i.e., baseline before tight), and 3) non‐tight brace versus no brace (i.e., baseline before non‐tight). The mediation model is shown in Figure 1. Path A represents the effect of wearing the brace on change in a mediator variable. Path B represents the association between change in the mediator variable and change in the dependent variable. Path C represents the direct effect of wearing the brace on change in the dependent variable, adjusted for the mediator variable. The mediation effect (indirect effect) was calculated based on the product of coefficient approach 28 and on single mediator models. For instance, improvement of proprioception is shown to be a mediator of the effect of wearing the brace on reduction in activity limitations if the indirect effect of wearing the brace on change in activity limitations (path A × path B) differs significantly from zero 28 (Figure 1). To determine the Monte Carlo 95% confidence intervals (95% CIs) and significance of the mediation, a bootstrap procedure (data re‐sampling) with 5,000 re‐samples was used 29. All analyses were performed using SPSS software, version 22.0.
Figure 1.
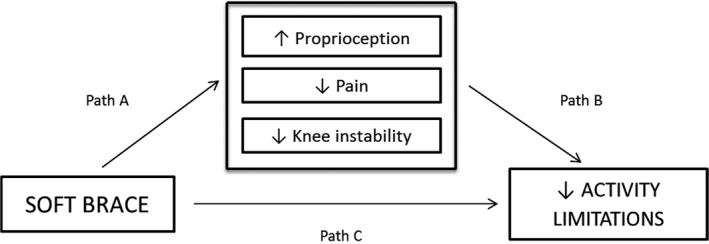
Mediation model. Path A represents the effect of wearing the brace on change in a mediator variable. Path B represents the association between change in the mediator variable and change in the dependent variable. Path C represents the direct effect of wearing the brace on change in the dependent variable, adjusted for the mediator variable.
Results
The mean ± SD age of the patients was 65.7 ± 9.3 years, the mean ± SD BMI was 29.8 ± 5.5 kg/m², and 29 (65.9%) of the patients were women. Full demographic and clinical characteristics were described in our previous study 2. Table 2 shows the results per outcome measure and per studied mediator in all 3 conditions. Full results from the analysis are presented in Supplementary Material 1 (available on the Arthritis Care & Research web site at http://onlinelibrary.wiley.com/doi/10.1002/acr.23722/abstract). The change scores for the 10‐meter walk test and the GUG test were previously published 2 and, in the current article, are shown in both Table 2 and Supplementary Material 1 (available on the Arthritis Care & Research web site at http://onlinelibrary.wiley.com/doi/10.1002/acr.23722/abstract) as “Total effect.” The change scores for all mediators are provided in Supplementary Material 1, under the heading “path A” (available on the Arthritis Care & Research web site at http://onlinelibrary.wiley.com/doi/10.1002/acr.23722/abstract).
Table 2.
Mediation effects, per condition, on the change in time (seconds) to complete the 10‐meter walk test and the GUG testa
| Total effect, B (95% CI) | Mediated effect, B (95% CI) | ||||
|---|---|---|---|---|---|
| Proprioception | Pain (NRS) | PPT | PR | ||
| Conditions | |||||
| 10‐minute walk test | |||||
| SB vs.no SB | −0.23 (−0.31, −0.13)b | −0.02 −0.06, 0.01) | –0.10 (–0.1, –0.04)b | –0.004 (–0.03, 0.01) | –0.03 (–0.1, –0.01)b |
| TB vs. no TB | −0.22 (−0.33, −0.10)b | −0.0001 (−0.03, 0.03) | –0.13 (–0.3, –0.03)b | –0.003 (–0.05, 0.05) | –0.01 (–0.1, –0.02) |
| NTB vs. no NTB | −0.23 (−0.31, −0.14)b | −0.02 (−0.08, 0.02) | –0.12 (–0.23, –0.03)b | –0.01 (–0.08, 0.04) | –0.008 (–0.23, 0.03) |
| GUG test | |||||
| SB versus no SB | −0.23 (−0.38, −0.07)b | −0.01 (−0.07, 0.01) | –0.10 (–0.2, –0.02)b | –0.003 (–0.03, 0.02) | –0.06 (–0.2, –0.01)b |
| TB vs. no TB | −0.08 (−0.25, 0.08) | −0.0004 (−0.04, 0.1) | –0.008 (–0.0, 2.01) | –0.005 (–0.03, 0.01) | –0.005 (–0.03, 0.01) |
| NTB vs. no NTB | −0.38 (−0.57, −0.17)b | −0.001 (−0.07, 0.01) | –0.16 (–0.4, –0.03)b | –0.03 (–0.17, 0.08) | –0.18 (–0.4, –0.03)b |
Mediated effect is the association between wearing a brace and a change in an outcome measure via change in a mediator (path A × path B). Total effect is the association between wearing a brace and change in an outcome measure, accounting for all mediated effects. GUG = Get Up and Go; 95% CI = 95% confidence interval; NRS = numerical rating scale; PPT = pressure pain threshold; PR = perturbation response; SB = soft brace; TB = tight brace; NTB = non‐tight brace.
Significant at P < 0.05.
Ten‐meter walk test
For the comparison between wearing the brace and not wearing the brace, both decrease in pain (NRS) and reduction of dynamic knee instability mediated the effect of wearing a soft knee brace on decrease in time to complete the 10‐meter walk test (mediated effects: B = −0.10 [P < 0.05] and B = −0.03 [P < 0.05], respectively). These values correspond to a proportion mediated of 43% and 13% of the total effect of wearing a brace on reduction of time to complete the 10‐meter walk test, respectively. Change of proprioception or PPT did not mediate this effect.
For the comparison between wearing a non‐tight or a tight brace and not wearing the brace, decrease in pain (NRS) mediated the effect of wearing a tight brace (mediation effect B = −0.13 [P < 0.05]) and the effect of wearing a non‐tight brace (mediation effect: B = −0.12 [P < 0.05]) on reduction of time to complete the 10‐meter walk test. These values correspond to a proportion mediated of 59% and 52% of the total effects on reduction of time to complete the 10‐meter walk test, respectively. Changes in proprioception, PPT, or dynamic knee instability did not mediate these effects.
GUG test
For the comparison between wearing the brace and not wearing the brace, both decrease in pain (NRS) and decrease in dynamic knee instability mediated the effect of wearing a soft knee brace on reduction of time to complete the GUG test (mediation effects: B = −0.10 [P < 0.05] and B = −0.06 [P < 0.05], respectively). These correspond to a proportion mediated of 44% and 26% of the total effect of wearing a brace on reduction of time to complete the GUG test, respectively. Change in proprioception and PPT did not mediate this effect.
For the comparison between wearing a non‐tight or a tight brace and not wearing the brace, changes in proprioception, pain (NRS), PPT, or dynamic knee instability did not mediate the effect of wearing a tight brace on reduction of time to complete the GUG test. However, both decrease in pain (NRS) and decrease in dynamic knee instability mediated the effect of wearing a non‐tight brace on reduction of time to complete the GUG test (mediation effects: B = −0.16 [P < 0.05] and B = −0.18 [P < 0.05], respectively). These correspond to a proportion mediated of 42% and 47% of the total effect of wearing a non‐tight brace on reduction in time to complete the GUG test, respectively. Change of proprioception or PPT did not mediate this effect.
Discussion
This is the first study showing that the beneficial effect of wearing a soft knee brace on activity limitations in patients with knee OA is mediated by decreased pain and reduced dynamic knee instability. Reduction of pain accounted for 43% and 44% of the decrease in time to complete the 10‐meter walk test and the GUG test, respectively. This effect can be explained by the tactile stimulation of the knee skin provided by a soft brace. Such stimulation may cause neural inhibition, facilitating the entry of impulses through the large afferent nerve fibers 4. Consequently, such stimulation may lead to a reduction in transmission of pain signals 4. Self‐reported limitations in activities in patients with knee OA are largely dependent on pain 7; therefore, it seems that reduced pain, by means of a soft knee brace, leads to walking at a higher speed. We did not find evidence that pain, as assessed by the PPT test, mediated the effect of wearing a brace on activity limitations. A likely explanation could be that for practical reasons PPT was not measured while the patient was wearing a brace but instead after wearing a brace.
A reduction in dynamic knee instability accounted for 13% and 26% decreases in time to complete the 10‐meter walk test and the GUG test, respectively, while wearing a brace. It has been suggested that the tactile stimuli of the skin mechanoreceptors provided by a soft brace contribute to the signaling of limb movements to the brain, which processes these sensory inputs to create perceptual representations of limb movements 30. Primary sensorimotor cortex activity has been shown to be influenced by peripheral sensory input to the knee joint by means of a soft brace 31. It is therefore plausible that the central nervous system uses this additional sensory information to elaborate on descending motor strategies (i.e., improved muscle activity), resulting in enhanced knee joint stability. It is plausible that improved instability, i.e., limiting excessive joint movement, translates into an ability to walk faster.
Generalizability of the results to other braces will be dependent on the type of knee brace. The results might be generalizable to other types of soft braces, because soft braces are thought to elicit their effects via skin stimulation and subsequent activation of cutaneous mechanoreceptors. The results are not generalizable to unloading braces, which are thought to elicit their effects via unloading the knee joint by mechanical realignment.
Proprioception was not shown to mediate the effects of wearing the soft brace on activity limitations. A possible explanation is that proprioception was not measured while the patient was wearing the brace but instead following exposure to wearing a brace. It has been shown that mechanical stimulation of the cutaneous mechanoreceptors has lasting effects, through a phenomenon called “after‐discharge” 32, 33. The cutaneous low‐threshold mechanoreceptors after‐discharge is said to reflect an inverse stimulation, in which it is the indented and/or stretched skin returning to its original position (in this case, via removal of the brace) that activates cutaneous low‐threshold mechanoreceptor terminals, thus producing after‐discharge 34. Future studies assessing proprioception while the patient is wearing a soft knee brace are required to determine whether proprioception plays a role in soft brace–induced effects in patients with knee OA.
Our previous study did not support the hypothesis that wearing a non‐tight brace will have stronger effects on activity limitations compared with wearing a tight brace 2. This study showed similar mediation effects when the patient was wearing a tight or non‐tight brace during the 10‐meter walk test. However, improvements in pain (rated on an NRS) and dynamic knee instability were mediators when the patient was wearing a non‐tight brace during the GUG test but not when wearing a tight brace. It is plausible that a non‐tight brace elicited a continuous response from cutaneous receptors and provided more recurrent sensory stimuli from the skin to the brain 4. The GUG test is a more demanding task than the 10‐meter walk test and likely requires greater input from the sensorimotor system.
This study might have important implications for the design and manufacturing of soft knee braces. Refinements to the design of soft knee braces may be required in order to maximize effects on knee pain and knee instability. To complement the sensorimotor system in providing knee joint stability, soft knee braces could be combined with stochastic resonance electrical stimulation. A soft knee brace combined with stochastic resonance has previously been shown to improve proprioception and muscle activity 35, 36, which are key determinants of dynamic knee stability 37. Many patients with knee OA reported that cold aggravates their knee pain 38; therefore, thermal modalities in the form of fabrics retaining heat could be used for soft braces to further enhance the effect on pain 39.
Some limitations of the study should be acknowledged. Apart from the method of the assessments, the absence of the mediation effects of proprioception and PPT could be a consequence of inadequate power due to the small sample size of the study. However, recent evidence suggests that the statistical test of the indirect effect has more power than the test of the total effect, contradicting the belief that mediation analyses are normally underpowered 40. Due to our study design, it cannot be excluded that improvement in physical function mediated improvement in pain and dynamic knee stability, instead of the other way around. Although theoretically unlikely, this limitation should be acknowledged. Moreover, it is important to acknowledge the possibility that the mediators might have been affecting each other, and/or that there were additional mediating/moderating effects. Our study was not powered to assess more detailed models. Finally, activity limitations were assessed during level walking in a corridor, and dynamic knee instability was assessed when walking during mechanical perturbations on the treadmill. It is therefore not known whether dynamic knee instability would also be found to be a mediator when it was assessed by a different measure during level walking.
In conclusion, this study shows that decreasing pain and reducing dynamic knee instability are pathways by which wearing a soft knee brace decreases activity limitations in patients with knee OA.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Cudejko had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Cudejko, van der Esch, Dekker.
Acquisition of data
Cudejko, van der Esch, Dekker.
Analysis and interpretation of data
Cudejko, van den Noort, Rijnhart, van der Leeden, Roorda, Lems, Waddington, Harlaar.
Supporting information
Acknowledgments
We gratefully thank Djody van Swaal (Centrum Orthopedie Rotterdam) for providing the soft braces. We thank Jos Twisk, PhD, for his assistance with statistical analyses. We gratefully acknowledge Marjolein Booij, MSc, Linda van Gardner, MSc, and Anke Hofste, MSc, for their help during data collection. We thank Johannes Gijsbers, PhD, for his help developing the application for treadmill perturbations.
Nederlands Trialregister, trialregister.nl NTR6363.
Supported by the European Union, Seventh Framework Programme (grant 607510).
No potential conflicts of interest relevant to this article were reported.
References
- 1. Beaudreuil J, Bendaya S, Faucher M, Coudeyre E, Ribinik P, Revel M, et al. Clinical practice guidelines for rest orthosis, knee sleeves, and unloading knee braces in knee osteoarthritis. Joint Bone Spine 2009;76:629–36. [DOI] [PubMed] [Google Scholar]
- 2. Cudejko T, van der Esch M, van der Leeden M, van den Noort JC, Roorda LD, Lems W, et al. The immediate effect of a soft knee brace on pain, activity limitations, self‐reported knee instability, and self‐reported knee confidence in patients with knee osteoarthritis. Arthritis Res Ther 2017;19:260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cudejko T, van der Esch M, van der Leeden M, Roorda LD, Pallari J, Bennell KL, et al. Effect of soft braces on pain and physical function in patients with knee osteoarthritis: systematic review with meta‐analyses. Arch Phys Med Rehabil 2018;99:153–63. [DOI] [PubMed] [Google Scholar]
- 4. Hassan BS, Mockett S, Doherty M. Influence of elastic bandage on knee pain, proprioception, and postural sway in subjects with knee osteoarthritis. Ann Rheum Dis 2002;61:24–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holla JF, van der Leeden M, Peter WF, Roorda LD, van der Esch M, Lems WF, et al. Proprioception, laxity, muscle strength and activity limitations in early symptomatic knee osteoarthritis: results from the CHECK cohort. J Rehabil Med 2012;44:862–8. [DOI] [PubMed] [Google Scholar]
- 6. Pajareya K, Chadchavalpanichaya N, Timdang S. Effectiveness of an elastic knee sleeve for patients with knee osteoarthritis: a randomized single‐blinded controlled trial. J Med Assoc Thai 2003;86:535–42. [PubMed] [Google Scholar]
- 7. Van Dijk GM, Veenhof C, Lankhorst GJ, Dekker J. Limitations in activities in patients with osteoarthritis of the hip or knee: the relationship with body functions, comorbidity and cognitive functioning. Disabil Rehabil 2009;31:1685–91. [DOI] [PubMed] [Google Scholar]
- 8. Van der Esch M, Knoop J, van der Leeden M, Voorneman R, Gerritsen M, Reiding D, et al. Self‐reported knee instability and activity limitations in patients with knee osteoarthritis: results of the Amsterdam osteoarthritis cohort. Clin Rheumatol 2012;31:1505–10. [DOI] [PubMed] [Google Scholar]
- 9. Felson DT, Niu J, McClennan C, Sack B, Aliabadi P, Hunter DJ, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med 2007;147:534–40. [DOI] [PubMed] [Google Scholar]
- 10. Judd CM, Kenny DA, McClelland GH. Estimating and testing mediation and moderation in within‐subject designs. Psychol Methods 2001;6:115–34. [DOI] [PubMed] [Google Scholar]
- 11. Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. From the Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum 1986;29:1039–49. [DOI] [PubMed] [Google Scholar]
- 12. Lin YC, Davey RC, Cochrane T. Tests for physical function of the elderly with knee and hip osteoarthritis. Scand J Med Sci Sports 2001;11:280–6. [DOI] [PubMed] [Google Scholar]
- 13. Piva SR, Fitzgerald GK, Irrgang JJ, Bouzubar F, Starz TW. Get up and go test in patients with knee osteoarthritis. Arch Phys Med Rehabil 2001;85:284–9. [DOI] [PubMed] [Google Scholar]
- 14. Wolf SL, Catlin PA, Gage K, Gurucharri K, Robertson R, Stephen K. Establishing the reliability and validity of measurements of walking time using the Emory Functional Ambulation Profile. Phys Ther 1999;79:1122–33. [PubMed] [Google Scholar]
- 15. Han J, Waddington G, Adams R, Anson J. Ability to discriminate movements at multiple joints around the body: global or site‐specific. Percept Mot Skills 2013;116:59–68. [DOI] [PubMed] [Google Scholar]
- 16. Cruz‐Almeida Y, King CD, Goodin BR, Sibille KT, Glover TL, Riley JL, et al. Psychological profiles and pain characteristics of older adults with knee osteoarthritis. Arthritis Care Res (Hoboken) 2013;65:1786–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol 1990;17:1022–4. [PubMed] [Google Scholar]
- 18. Lacourt TE, Houtveen JH, Veldhuijzen van Zanten JJ, Bosch JA, Drayson MT, Van Doornen LJ. Negative affectivity predicts decreased pain tolerance during low‐grade inflammation in healthy women. Brain Behav Immun 2015;44:32–6. [DOI] [PubMed] [Google Scholar]
- 19. Arendt‐Nielsen L, Nie H, Laursen MB, Laursen BS, Madeleine P, Simonsen OH, et al. Sensitization in patients with painful knee osteoarthritis. Pain 2010;149:573–81. [DOI] [PubMed] [Google Scholar]
- 20. Chesterton LS, Sim J, Wright CC, Foster NE. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain 2007;23:760–6. [DOI] [PubMed] [Google Scholar]
- 21. Van den Noort JC, Sloot LH, Bruijn SM, Harlaar J. How to measure responses of the knee to lateral perturbations during gait? A proof‐of‐principle for quantification of knee instability. J Biomech 2017;61:111–22. [DOI] [PubMed] [Google Scholar]
- 22. Thangal SN, Talaty M, Balasubramanian S. Assessment of gait sensitivity norm as a predictor of risk of falling during walking in a neuromusculoskeletal model. Med Eng Phys 2013;35:1483–9. [DOI] [PubMed] [Google Scholar]
- 23. Zeni JA Jr, Richards JG, Higginson JS. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008;27:710–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cappozzo A, Catani F, Croce UD, Leardini A. Position and orientation in space of bones during movement: anatomical frame definition and determination. Clin Biomech (Bristol, Avon) 1995;10:171–8. [DOI] [PubMed] [Google Scholar]
- 25. Kellgren JH, Lawrence JS. Radiological assessment of osteo‐arthrosis. Ann Rheum Dis 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–40. [PubMed] [Google Scholar]
- 27. Roorda LD, Jones CA, Waltz M, Lankhorst GJ, Bouter LM, van der Eijken JW, et al. Satisfactory cross cultural equivalence of the Dutch WOMAC in patients with hip osteoarthritis waiting for arthroplasty. Ann Rheum Dis 2004;63:36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002;7:83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Selig J, Preacher K. Monte Carlo method for assessing mediation: an interactive tool for creating confidence intervals for indirect effects. URL: http://quantpsy.org/.
- 30. Pegoretti KS, Moraes R, Masullo CL, Chagas‐Neto FA, Miranda A, Kfuri MJ, et al. Additional sensory input improves the strategy of stepping over obstacle in individuals with knee osteoarthritis. J Back Musculoskelet Rehabil 2015;28:689–97. [DOI] [PubMed] [Google Scholar]
- 31. Thijs Y, Vingerhoets G, Pattyn E, Rombaut L, Witvrouw E. Does bracing influence brain activity during knee movement: an fMRI study. Knee Surg Sports Traumatol Arthrosc 2010;18:1145–9. [DOI] [PubMed] [Google Scholar]
- 32. Zotterman Y. Touch, pain and tickling: an electro‐physiological investigation on cutaneous sensory nerves. J Physiol 1939;95:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Iggo A. Cutaneous mechanoreceptors with afferent C fibres. J Physiol 1960;152:337–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Iggo A, Kornhuber HH. A quantitative study of C‐mechanoreceptors in hairy skin of the cat. J Physiol 1977;271:549–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Collins A, Blackburn JT, Olcott C, Yu B, Weinhold P. The impact of stochastic resonance electrical stimulation and knee sleeve on impulsive loading and muscle co‐contraction during gait in knee osteoarthritis. Clin Biomech (Bristol, Avon) 2011;26:853–8. [DOI] [PubMed] [Google Scholar]
- 36. Collins AT, Blackburn JT, Olcott CW, Miles J, Jordan J, Dirschl DR, et al. Stochastic resonance electrical stimulation to improve proprioception in knee osteoarthritis. Knee 2011;18:317–22. [DOI] [PubMed] [Google Scholar]
- 37. Riemann BL, Lephart SM. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. J Athl Train 2002;37:80–4. [PMC free article] [PubMed] [Google Scholar]
- 38. Davis MA, Ettinger WH, Neuhaus JM, Barclay JD, Segal MR. Correlates of knee pain among US adults with and without radiographic knee osteoarthritis. J Rheumatol 1992;19:1943–9. [PubMed] [Google Scholar]
- 39. Mazzuca SA, Page MC, Meldrum RD, Brandt KD, Petty‐Saphon S. Pilot study of the effects of a heat‐retaining knee sleeve on joint pain, stiffness, and function in patients with knee osteoarthritis. Arthritis Rheum 2004;51:716–21. [DOI] [PubMed] [Google Scholar]
- 40. O'Rourke HP, MacKinnon DP. Reasons for testing mediation in the absence of an intervention effect: a research imperative in prevention and intervention research. J Stud Alcohol Drugs 2018;79:171–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


