We thank Yuan et al. for their interest in our study. Indeed, population‐based differences are evident between central Europe and Asia, which should certainly be acknowledged when evaluating our data.1 Of note, we aimed to address this issue in our initial analyses by separately assessing patients with hepatocellular carcinoma. However, to further elucidate the importance of microRNA (miRNA)‐based prediction of postoperative liver dysfunction (LD), we now investigated the group of patients with cirrhosis more closely. We observed a significant predictive potential of both the individual miRNAs and the miRNA signature within this small subgroup consisting of 20 patients with liver cirrhosis, of whom 20% developed postoperative LD (Fig. 1). In addition, both cutoffs for the combined ratio were found to stratify patients with cirrhosis at risk for LD (Fig. 1). Although the sample size for this analysis is clearly not sufficient to allow relevant conclusions, this exploratory analysis suggests that our results might be valid also in this high‐risk subgroup. However, we would like to stress that we are currently aiming to validate our results on an international level.
Figure 1.
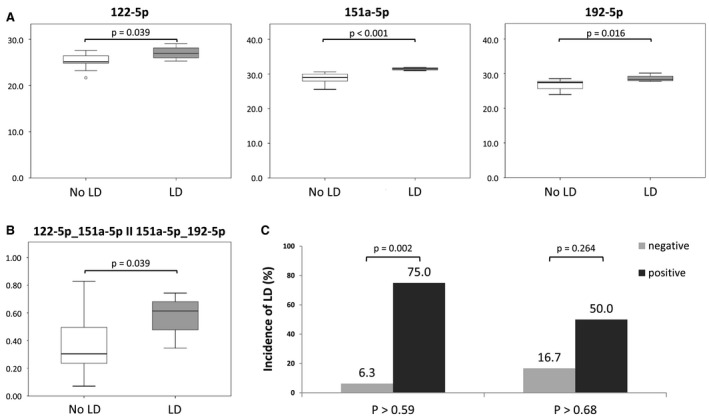
Predictive potential of miRNA signatures for postoperative Ld in patients suffering from liver cirrhosis. Twenty patients with liver cirrhosis were included in this analyses (4 suffering from postoperative LD). (A) The three miRNAs with respect to development of postoperative LD. (B) The miRNA signature of the three miRNAs with respect to development of postoperative LD. Respective cutoffs and their performance in identifying patient suffering from postoperative LD is depicted in (C).
We also thank Li et al. for their interest in our analyses and enthusiastically agree with the authors that our miRNA signatures seem to represent a vital marker to assess preoperative liver function, given that this is the main finding of our analyses. However, we strongly disagree with the suggestion of including intra‐ and postoperative parameters in our analyses. We believe it is a particular strength of our study that we performed an unbiased approach including patients that were comparable in terms of preoperative characteristics. Stratifying patients according to intraoperative characteristics, as suggested by Yuan and Li et al., is not legitimate given that this would introduce a major bias. Our ultimate goal is to tailor surgical strategies to the specific risk profile of patients, which makes it impossible to include surgery‐related factors in the performed analyses.
Ultimately, Li et al. suggest that the additional assessment of future liver remnant function could improve outcome prediction of our model. In this context, a plethora of parameters have already been identified that seem to improve preoperative risk assessment of patients undergoing liver resection.2, 3, 4, 5 Indeed, the combination of preoperative liver function assessment might be beneficial to further characterize patients’ risk for adverse postoperative outcome. However, the central aim of the presented study was to define a preoperative parameter that is easily assessable and highly standardized to provide a reliable and internationally available tool. Future research will have to determine whether additional preoperative assessments will further improve risk stratification in patients undergoing liver resection.
Potential conflict of interest: Dr. Hackl is employed by, owns stock in, and holds intellectual property rights with Tamirna.
References
- 1. Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol 2019;70:674‐683. [DOI] [PubMed] [Google Scholar]
- 2. Haegele S, Fuxsteiner J, Pereyra D, Koeditz C, Rumpf B, Schuetz C, et al. Elevated ADAMTS13 activity is associated with poor postoperative outcome in patients undergoing liver resection. Sci Rep 2018;8:16823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pereyra D, Rumpf B, Ammann M, Perrodin SF, Tamandl D, Haselmann C, et al. The combination of APRI and ALBI facilitates preoperative risk stratification for patients undergoing liver surgery after neoadjuvant chemotherapy. Ann Surg Oncol 2019;26:791‐799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Starlinger P, Pereyra D, Haegele S, Braeuer P, Oehlberger L, Primavesi F, et al. Perioperative von Willebrand factor dynamics are associated with liver regeneration and predict outcome after liver resection. Hepatology 2018;67:1516‐1530. [DOI] [PubMed] [Google Scholar]
- 5. Starlinger P, Assinger A, Haegele S, Wanek D, Zikeli S, Schauer D, et al. Evidence for serotonin as a relevant inducer of liver regeneration after liver resection in humans. Hepatology 2014;60:257‐266. [DOI] [PubMed] [Google Scholar]


