Abstract
Objective
Intrusive thoughts, defined as unwanted and recurrent thoughts about a stressful experience, are associated with psychological distress in women with breast cancer. This study assessed moderating effects of various social support dimensions on associations between intrusive thoughts and psychological distress among Latina breast cancer survivors.
Methods
We used baseline data from a randomized controlled trial of a stress management intervention delivered to 151 Spanish‐speaking Latinas with nonmetastatic breast cancer within 1 year of diagnosis. Intrusive thoughts, four dimensions of social support (emotional/informational, tangible, affectionate, and positive social interaction), and symptoms of anxiety and depression were assessed through in‐person interviews. Information on age, time since diagnosis, breast cancer variables, history of depression, and marital status served as covariates. Generalized linear models were used to investigate bivariate and multivariate associations and to explore moderation effects of the four dimensions of social support.
Results
In bivariate models, intrusive thoughts were associated positively with depression (β = .024, .001) and anxiety (β = .047, P < .001) symptoms. Adjusting for other factors, intrusive thoughts remained associated with depression symptoms (β = .022, .008), regardless of level of social support (for all support dimensions). For anxiety, there were significant interactions of tangible (β = −.013, .034) and affectionate (β = −.022, .005) support with intrusive thoughts. Intrusive thoughts were associated more strongly with anxiety symptoms among women reporting less tangible and affectionate support than those with higher levels of these types of support.
Conclusions
Tangible and affectionate support have protective effects on anxiety symptoms among Spanish‐speaking Latina breast cancer survivors experiencing intrusive thoughts, but not depression symptoms.
Keywords: anxiety, breast cancer, depression, Latina/Hispanic, social support
1. BACKGROUND
More than 250 000 women in the United States are diagnosed with breast cancer every year.1 Many women experience intrusive thoughts at the time of diagnosis and during and after treatment. Intrusive thoughts, defined as unwanted and recurrent thoughts about a stressful experience, are a common occurrence among women with breast cancer and often persist if not addressed early.2, 3, 4 Even after treatment is completed, women with breast cancer continue to suffer psychologically from fears of recurrence and dying of the disease.1
While intrusive thoughts are a common component of the cognitive processing of breast cancer, they are also associated with worse health‐related quality of life (HrQoL) later in treatment.5 In a psychoeducation intervention trial given to women with breast cancer, intrusive thoughts were associated with higher levels of pain, breast cancer‐specific symptoms, and depression symptoms.2 Additionally, intrusive thoughts have been found to be a predictor of anxiety and depression in cancer patients.6
Past studies have shown that social support has a protective effect on health and is positively associated with HrQoL among women with breast cancer.7 Further, lack of social support has been shown to play a role in the development of depression and anxiety among women with breast cancer. A study of women with primary breast cancer found that low levels of social support independently predicted depression or anxiety in the year after diagnosis.8 Another study found that social support moderated the relationship between depression symptoms and quality of life in breast cancer survivors. In other words, depression symptoms had a more deleterious effect on the quality of life of breast cancer survivors who reported little or no social support.9 While there is evidence that social support impacts health outcomes among women with breast cancer, few studies evaluate how different dimensions of social support relate to health outcomes.
A possible mechanism explaining the linkage between social support and positive psychological outcomes has been offered by Cohen's model of stress‐buffering. This model states that social support serves as a “buffer” and attenuates the potentially pathologic effects of stressful events.10 This buffering effect of social support has been shown in women with breast cancer. For example, one study showed that an intervention providing emotional and social support improved HrQoL and decreased psychological distress among women with breast cancer.11
To our knowledge, no studies have examined social support as a potential moderator of the relationship between intrusive thoughts and psychological distress among Spanish‐speaking Latina women with breast cancer. Consistent with Cohen's model of stress‐buffering, social support could moderate the relationship between intrusive thoughts and psychological distress by decreasing the impact of intrusive thoughts, which in turn, leads to decreased psychological distress. Specifically, the disclosure of one's thoughts and feelings about cancer can allow the survivor to process their experience and increase the belief that there are resources available. Through processing and integrating their experience, their perception of cancer as a threat is decreased, which leads to less psychological distress.
Latinas with breast cancer are an important population to focus on because they are an understudied and high‐risk group of survivors. Compared with their White counterparts, Latinas are at higher risk for psychosocial and physical sequelae of breast cancer, reporting higher rates of anxiety, depression, fear of recurrence, and worse HrQoL.12, 13, 14 Sources of increased distress for this population include inadequate insurance coverage and transportation and problems paying for treatment. Anxiety is common among limited English proficient patients because they often do not understand their diagnosis or treatment and are less involved in patient‐centered decision‐making.15 Additionally, there is a lack of culturally and linguistically competent cancer support services for this population.16
This study aimed to assess the moderating effects of different dimensions of social support on the association between intrusive thoughts and psychological distress in this population. In this study, we assessed psychological distress, ie, symptoms of depression and anxiety, among Spanish‐speaking Latinas within the first year of diagnosis of breast cancer. To address a limitation of prior work, we sought to assess the differential effects of various types of social support on distress.17, 18 We hypothesized that intrusive thoughts would be positively associated with depression and anxiety symptoms. Furthermore, we hypothesized that social support dimensions moderate the associations between intrusive thoughts and psychological distress, such that higher levels of support buffer the negative effects of intrusive thoughts on psychological distress.
2. METHODS
2.1. Sample participants
Analyses were performed using baseline data from a randomized controlled trial of a stress management intervention delivered to 151 Spanish‐speaking Latinas with nonmetastatic breast cancer. Participants were diagnosed with Stage 0 to Stage 3C primary breast cancer within the past year. Women with ductal carcinoma in situ (DCIS or Stage 0) breast cancer were included since past literature has shown that women with DCIS display similar levels of distress as those with other nonmetastatic breast cancers .19, 20 Additionally, Latinas are less likely to understand the distinction between DCIS and invasive breast cancer, therefore experience substantial distress associated with a DCIS diagnosis.21 Women resided in five Northern California counties and were recruited from clinical and community settings to participate in an 8‐week cognitive‐behavioral stress management program called Nuevo Amanecer (A New Dawn), using community‐based participatory research methods. Details on study procedures22 and the intervention23 are described elsewhere. The study protocol was approved by the University of California San Francisco Institutional Review Board (approval number 10‐03030, and written informed consent was obtained from all participants. This trial is registered with ClinicalTrials.gov (NCT01383174).
2.2. Measures
Women completed a 60‐minute baseline in‐person interview and received $30 as compensation. Interviews were conducted in Spanish by trained bilingual‐bicultural community‐based recruiters either at participants' homes or clinic sites where they received their breast cancer care. Copies of medical records were obtained and used for verification of cancer variables. All the variables for the current study were taken from the baseline, which occurred between February 2011 and November 2013. Intrusive thoughts were measured with the 7‐item Intrusive Thoughts Scale, a subscale of the Revised Impact of Event Scale.24 The intrusive thoughts scale measures the extent of unwanted thoughts and images related to the stressor, in this case, breast cancer. The intrusive thoughts scale has been proven to be sensitive to change in women with breast cancer who are receiving psychosocial interventions.25 Items were specific to the breast cancer experience, such as “I had waves of strong feelings about my breast cancer” or “Pictures about my breast cancer popped into my mind.” Participants were asked how often the thoughts and feelings had occurred in the past 7 days (response options: 0 = not at all, 1 = rarely, 2 = sometimes, and 3 = often). Using the published scoring algorithm, responses were recoded to 0, 1, 3, and 5 and summed for a total score. The possible range was 0 to 35, with higher scores indicating more intrusive thoughts. Internal consistency reliability was 0.89 in this sample.
Social support was assessed using the 19‐item Medical Outcomes Study Social Support Survey that contains four scales representing various dimensions of social support: emotional/informational, tangible, affectionate, and positive social interaction.26 Women were asked how often each of the listed kinds of support was available to them when they needed it (response options: 1 = not at all, 2 = a little of the time, 3 = some of the time, 4 = most of the time, 5 = all of the time). Examples of the statements include “Someone you can count on to listen to you when you need to talk” (emotional/informational support), “Someone to take you to the doctor if you needed it” (tangible support), “Someone who shows you love and affection” (affectionate support), and “Someone to do something enjoyable with” (positive social interaction). Each scale was scored as the mean of nonmissing items with a possible range of 1 to 5, with higher scores indicating greater support. Internal consistency reliabilities were 0.93 for emotional/informational support, 0.93 for tangible support, 0.83 for affectionate support, and 0.92 for positive social interaction in this sample.
Psychological distress was assessed using the two subscales from the Brief Symptom Inventory‐18 (BSI‐18) assessing depression and anxiety symptoms. The National Comprehensive Cancer Network defines psychological distress as a continuum, ranging from common normal feelings of vulnerability and sadness to problems that can be disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis.27 The BSI‐18 has been validated for use as a brief psychological distress screening tool for cancer survivors.28, 29 The reliability and validity of the BSI‐18 have been supported in a Spanish‐speaking breast cancer sample.30 Women were asked how much the stated problems have distressed or bothered them during the past 7 days. Statements included “Feeling no interests in things” (depression) and “Nervousness or shakiness inside” (anxiety). Responses were 0 (not at all), 1 (a little bit), 2 (moderately), 3 (quite a bit), or 4 (extremely). Scale scores were calculated as the mean of the nonmissing items, with a possible range of 0 to 4, with higher scores indicating more psychological distress. Internal consistency reliabilities were 0.85 for anxiety and 0.83 for depression symptoms in this sample.
Covariate measures included information on age (continuous), time since diagnosis in months (continuous), adjuvant breast cancer treatment (both chemotherapy and radiation, only radiation, only chemotherapy, no treatment), type (lumpectomy or mastectomy), breast cancer stage (0, 1, 2, 3), history of depression (no history of depression, pre‐diagnosis history of depression), and marital status (single, married or living with partner). Medical information was verified using medical records. History of depression was assessed in the baseline survey by asking if they had ever been told by a doctor or mental health professional that they suffered from depression and whether it was before or after their breast cancer diagnosis.
2.3. Statistical analyses
Means were calculated for continuous variables and frequencies for categorical variables. Generalized linear models were used to investigate bivariate and multivariate associations and to explore moderation effects of the four dimensions of social support.
Separate multivariate models were constructed for each distress outcome, depression, or anxiety symptoms. Initially, we ran four generalized linear models for each outcome. These four models included intrusive thoughts, covariates, and one of the four social support subscale scores (hypothesized moderators), and the corresponding social support × intrusive thoughts interaction term. Each model included only one of the social support subscales due to the high correlation between each social support dimension. Interaction terms that were not statistically significant (P < .05) were dropped from the final models predicting each distress outcome.
3. RESULTS
3.1. Sample
The mean age in our sample was 50.5 years (SD = 10.9; range = 28 to 81 years) (Table 1). More than half (53%) was married or lived with a partner. At baseline, the mean time since breast cancer diagnosis was 3.8 months (SD = 2.7). Almost three fourths (73.5%) was diagnosed with invasive breast cancer (Stages 1, 2, and 3). More than half (55.6%) had a lumpectomy, and the most common adjuvant treatment was receiving both chemotherapy and radiation (39.7%). The majority (82.1%) reported having no history of depression before breast cancer diagnosis. The mean intrusive thoughts score was 8.3 (SD = 8.7). Within our sample, the full range was observed for the intrusive thoughts scale. Mean scores on the four social support scales ranged from 3.8 (SD = 1.0) for emotional/informational support to 4.2 (SD = 1.1) for affectionate support. The full range (range = 1‐5) was observed for all dimensions of support, except emotional/informational support (range = 1.25‐5). Mean scores were 0.8 (SD = 0.8) for depression symptoms and 1.0 (SD = 0.9) for anxiety symptoms. The full range for depression and anxiety symptoms was observed within our sample.
Table 1.
Descriptive characteristics of Spanish‐speaking Latina breast cancer survivors within one‐year of diagnosis, the Nuevo Amanecer study, Northern California, N = 151
| Characteristics | N = 151 |
|---|---|
| Age at baseline (mean; SD) | 50.5 (10.9) |
| Marital status (N; %) | |
| Married or living with partner | 80 (53.0) |
| Single | 71 (47.0) |
| Months since diagnosis (mean; SD) | 3.8 (2.7) |
| Stage (N; %) | |
| 0 | 40 (26.5) |
| 1 | 23 (15.2) |
| 2 | 57 (37.8) |
| 3 | 31 (20.5) |
| Surgery (N; %) | |
| Lumpectomy | 84 (55.6) |
| Mastectomy | 67 (44.4) |
| Adjuvant breast cancer treatment (N; %) | |
| Both radiation and chemotherapy | 60 (39.7) |
| Only radiation | 42 (27.8) |
| Only chemotherapy | 25 (16.6) |
| Neither radiation and chemotherapy | 24 (15.9) |
| History of depression (N; %) | |
| No history of depression | 124 (82.1) |
| Pre‐diagnosis history of depression | 27 (17.9) |
| Intrusive thoughts (mean; SD)a | 8.3 (8.7) |
| Social Support (mean; SD)b | |
| Emotional/informational support | 3.8 (1.0) |
| Tangible support | 3.9 (1.2) |
| Affectionate support | 4.2 (1.1) |
| Positive social interaction | 4.0 (1.1) |
| Psychological distress (mean; SD)c | |
| Depression symptoms | 0.8 (0.8) |
| Anxiety symptoms | 1.0 (0.9) |
Seven‐item Intrusive Thoughts Scale, a subscale of the Revised Impact of Event Scale; response options were 0 (not at all), 1 (rarely), 2 (sometimes), and 3 (often), and using the published scoring algorithm, responses were recoded to 0, 1, 3, and 5 and summed for a total score with a possible range = 0 to 35, with higher scores = more intrusive thoughts.24
19‐item Medical Outcomes Study Social Support Survey with four scales assessing emotional/informational, tangible, affectionate, and positive interaction support26; scales were scored as the mean of nonmissing items with a possible range of 1‐5; higher scores = more support.
Brief Symptom Inventory‐18 with two scales assessing anxiety and depression symptoms30; response options were 0 (not at all), 1 (a little bit), 2 (moderately), 3 (quite a bit), or 4 (extremely); scale scores were calculated as the mean of the nonmissing items, with a possible range of 0 to 4; higher scores = more psychological distress.
3.2. Bivariate analyses
In bivariate models, intrusive thoughts were associated positively with depression (β = .024, .001) and anxiety (β = .047, P < .001) symptoms.
Emotional/informational support (β = −.167, .014), tangible support (β = −.124, .025), and positive social interaction (β = −.127, .027) were significantly and inversely associated with depression symptoms.
Tangible support (β = −.161, .006), affectionate support (β = −.210, .001), and positive social interaction (β = −.139, .024) were inversely associated with anxiety symptoms. Women who had a history of depression prior to their breast cancer diagnosis reported more anxiety symptoms (β = .360, .048) than women who had no history of depression before breast cancer diagnosis.
3.3. Multivariate analyses
For the depression symptoms outcome, none of the intrusive thoughts × social support interaction terms were statistically significant, thus they were dropped from the final model presented in Table 2. In this final model, intrusive thoughts were positively associated with depression symptoms (β = .022, .008) regardless of the level of support for all types of support. Women with Stage 3 breast cancer were less likely to report depression symptoms (β = −.667, .017), compared with women with Stage 0 breast cancer. Compared with women who had neither radiation nor chemotherapy, women who had both radiation and chemotherapy reported more depression symptoms, independent of other factors (β = .654, .009).
Table 2.
Bivariate and multivariate correlates of depression and anxiety symptoms
| Depression Symptomsa | Anxiety Symptomsa | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Bivariate Model | Multivariate Model | Bivariate Model | Multivariate Model 1 | Multivariate Model 2 | |||||
| β | P value | β | P value | β | P value | β | P value | β | P value | |
| R2 = 0.236 | R2 = 0.367 | R2 = 0.344 | ||||||||
| Age at baseline | 0.002 | 0.804 | 0.003 | 0.707 | −0.001 | 0.890 | 0.004 | 0.545 | 0.004 | 0.547 |
| Marital status | ||||||||||
| Married or living with partner | −0.072 | 0.584 | −0.072 | 0.627 | −0.155 | 0.270 | −0.211 | 0.139 | −0.194 | 0.169 |
| Single | REF | REF | REF | REF | REF | |||||
| Months since diagnosis | −0.012 | 0.623 | −0.023 | 0.364 | −0.015 | 0.550 | −0.027 | 0.274 | −0.026 | 0.287 |
| Stage | ||||||||||
| 0 | REF | REF | REF | REF | REF | |||||
| 1 | −0.224 | 0.293 | −0.406 | 0.124 | −0.137 | 0.545 | −0.201 | 0.429 | −0.148 | 0.553 |
| 2 | −0.119 | 0.476 | −0.408 | 0.078 | 0.085 | 0.633 | −0.051 | 0.819 | −0.082 | 0.708 |
| 3 | −0.195 | 0.315 | −0.667 | 0.017 | 0.120 | 0.563 | −0.112 | 0.674 | −0.073 | 0.782 |
| Surgery | ||||||||||
| Mastectomy | −0.029 | 0.828 | 0.240 | 0.167 | 0.189 | 0.182 | 0.321 | 0.056 | 0.300 | 0.070 |
| Lumpectomy | REF | REF | REF | REF | REF | |||||
| Adjuvant breast cancer treatment | ||||||||||
| Both radiation and chemotherapy | 0.190 | 0.332 | 0.654 | 0.009 | −0.051 | 0.806 | 0.161 | 0.499 | 0.125 | 0.594 |
| Only radiation | 0.006 | 0.978 | 0.194 | 0.387 | −0.271 | 0.220 | −0.076 | 0.726 | −0.084 | 0.692 |
| Only chemotherapy | −0.019 | 0.936 | 0.340 | 0.209 | −0.191 | 0.439 | −0.027 | 0.916 | −0.091 | 0.723 |
| Neither radiation and chemotherapy | REF | REF | REF | REF | REF | |||||
| History of depression | ||||||||||
| Pre‐diagnosis history of depression | 0.268 | 0.117 | 0.169 | 0.342 | 0.360 | 0.048 | 0.243 | 0.158 | 0.272 | 0.111 |
| No history of depression | REF | REF | REF | REF | REF | |||||
| Intrusive thoughts (continuous)b | 0.024 | 0.001 | 0.022 | 0.008 | 0.047 | <0.001 | 0.094 | <0.001 | 0.134 | <0.001 |
| Social support (continuous)c | ||||||||||
| Emotional/informational support | −0.167 | 0.014 | −0.111 | 0.273 | −0.119 | 0.102 | 0.028 | 0.771 | 0.023 | 0.812 |
| Tangible support | −0.124 | 0.025 | −0.061 | 0.416 | −0.161 | 0.006 | 0.083 | 0.396 | −0.070 | 0.330 |
| Affectionate support | −0.116 | 0.060 | 0.113 | 0.339 | −0.210 | 0.001 | −0.126 | 0.268 | 0.129 | 0.363 |
| Positive social interaction | −0.127 | 0.027 | −0.052 | 0.630 | −0.139 | 0.024 | 0.090 | 0.384 | 0.091 | 0.375 |
| Interaction termsd | ||||||||||
| Emotional support × intrusive thoughts | ns | ns | ns | |||||||
| Tangible support × intrusive thoughts | ns | −0.013 | 0.034 | ns | ||||||
| Affectionate support × intrusive thoughts | ns | ns | −0.022 | 0.005 | ||||||
| Positive social interaction × intrusive thoughts | ns | ns | ns | |||||||
Note. Significant P values are listed in bold.
Brief Symptom Inventory‐18 with two scales assessing anxiety and depression symptoms30; response options were 0 (not at all), 1 (a little bit), 2 (moderately), 3 (quite a bit), or 4 (extremely); scale scores were calculated as the mean of the nonmissing items, with a possible range of 0 to 4; higher scores = more psychological distress.
7‐item Intrusive Thoughts Scale, a subscale of the Revised Impact of Event Scale; response options were 0 (not at all), 1 (rarely), 2 (sometimes), and 3 (often), and using the published scoring algorithm, responses were recoded to 0, 1, 3, and 5 and summed for a total score with a possible range = 0 to 35, with higher scores = more intrusive thoughts.24
19‐item Medical Outcomes Study Social Support Survey with four scales assessing emotional/informational, tangible, affectionate, and positive interaction support26; scales were scored as the mean of nonmissing items with a possible range of 1 to 5; higher scores = more support.
ns = Interaction terms that were not significant at the multivariate level and were dropped from the final multivariate models.
In the multivariate models for anxiety, both the intrusive thoughts × tangible support (multivariate model 1) and intrusive thoughts × affectionate support (multivariate model 2) interaction terms were significant and thus were retained in two separate final models. Tangible support (β = −.013, .034) was found to moderate the relationship between intrusive thoughts and anxiety symptoms, such that intrusive thoughts were more strongly associated with anxiety symptoms among women reporting less tangible support than those with higher levels of this type of support (Figure 1). Similarly, affectionate support (β = −.022, .005) was found to moderate the relationship between intrusive thoughts and anxiety symptoms, such that intrusive thoughts were associated more strongly with anxiety symptoms among women reporting less affectionate support than those with higher levels of this type of support (Figure 1).
Figure 1.
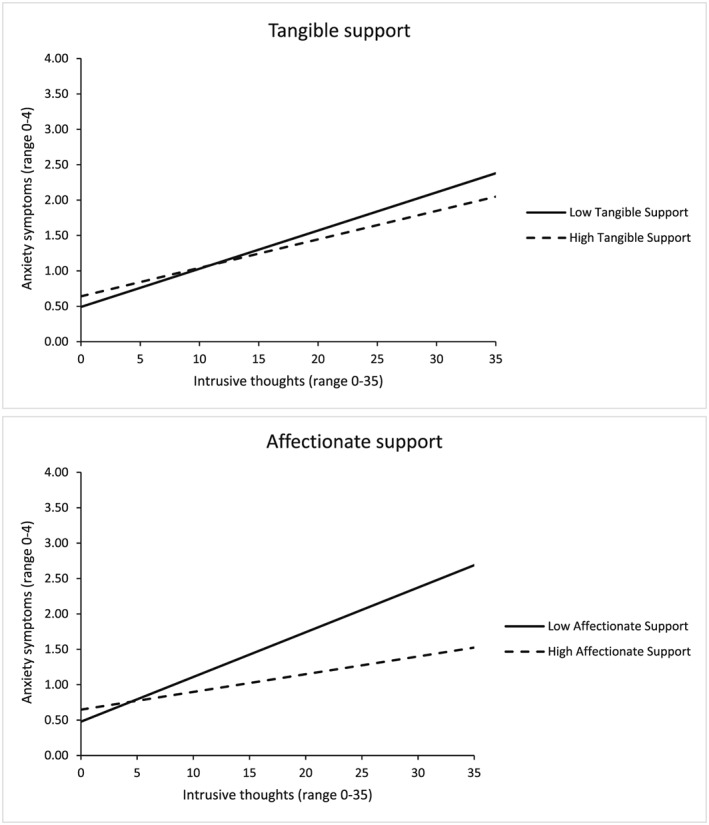
Moderating effects of affectionate support and tangible support on the relationship between intrusive thoughts and anxiety symptoms
4. CONCLUSIONS
This study aimed to assess the relationship between intrusive thoughts and breast cancer distress, and if this relationship varies depending on the levels of various types of social support among Spanish‐speaking Latinas with breast cancer. We hypothesized that intrusive thoughts would be positively associated with depression and anxiety symptoms, especially among women with lower levels of support. We found that intrusive thoughts were positively and independently associated with depression symptoms, regardless of the level of social support for all dimensions of support, and that social support was not significantly associated with depression symptoms. Thus, the buffering effects of social support were not supported for depression symptoms. Regarding anxiety symptoms, we found significant interactions between tangible and affectionate support and intrusive thoughts. Intrusive thoughts were associated more strongly with anxiety symptoms among women reporting less tangible and affectionate support than those with reporting higher levels of these types of support, suggesting that such support may buffer the negative effects of intrusive thoughts on anxiety levels.
Our findings that intrusive thoughts were associated with distress are consistent with past studies conducted among predominantly White samples of women with breast cancer.2, 31 Also, the mean level of intrusive thoughts in this study was higher than levels found in past studies with predominantly White samples. For example, the mean intrusive thoughts score in past studies ranged between 4.59 and 4.70, compared with the mean score of 8.30 observed in our sample.2, 31, 32, 33 A possible explanation is that compared with White breast cancer survivors, Latina breast cancer survivors report significantly lower social support, which in turn could lead them to experience more intrusive thoughts. However, social support levels in our study were fairly high, so these relationships require further clarification.
According to the BSI manual, positive cases of distress can be identified by a T score greater than or equal to 63 on any two of its nine subscales.34 To compare the mean values of anxiety and depression symptoms obtained in our study with other studies, we converted our raw scores to T scores, as described in the BSI manual.34 In our sample, mean T scores for both the anxiety and depression subscales were between 61 and 62. Therefore, our sample overall was very close to the clinical cut‐off for psychological distress. Additionally, based on mean T scores, women in our sample experienced higher depression and anxiety levels compared with a past study of primarily White breast cancer survivors (mean depression T score = 52.65 and mean anxiety T score = 55.68).28 The distribution of both subscale scores in our sample was skewed toward lower values, and thus, may underestimate the burden of psychological distress among the population of Latina breast cancer survivors. Alternatively, BSI cutoffs established for the general population may need to be validated and potentially modified for use among Latina breast cancer survivors, or the existing items may not capture the full breadth of the constructs of depression and anxiety in this group.
In our study, social support was associated with anxiety, but not depression symptoms. One possible explanation is that anxiety is a more culturally acceptable expression of distress than depression. Prior studies have demonstrated that Latinos share culturally prescribed meanings of acceptable or unacceptable ways of expressing psychological distress such that its verbal expression is discouraged and even stigmatized leading to emotional restraint.35 Other research has demonstrated that a more culturally acceptable way of expressing psychological distress is to use idioms such as nervios or nerves because this concept implies a transient condition that is socially understood.35 The anxiety items used in this study closely resemble the concept of nervios (nervousness, fearful, tense); therefore, Latinas may have viewed it as more acceptable to seek support from others for anxiety than depression (depression items reflected a sense of hopelessness, worthlessness). Another possible explanation is that the anxiety items tap into symptoms that are more severe in intensity than the depression items, eg, “spells of terror or panic” versus “feeling lonely.” Perhaps symptoms must attain enough intensity for Latinas to ask for help from others, which might explain why social support was associated with anxiety, but not depression.
Affectionate support was found to be an important protective factor for anxiety symptoms, but not for depression symptoms. It could be that affectionate or more intimate relationships play a more critical role for more intensive experiences of distress, such as anxiety (nervousness, fearful, tense), than for depression symptoms (hopelessness, worthlessness). While past literature describes social support as a potential moderator between intrusive thoughts and psychological adjustment in cancer patients,36, 37 little research has explored the specific role of affectionate support. A past study found that low affectionate support predicted worse quality of life in those with early stage breast cancer.7 However, among women with late stage cancer, affection appeared to be related to worse quality of life outcomes. Our findings indicate that having an intimate partner or friends who demonstrate love and affection toward you may be especially important in the case of Latina breast cancer survivors.
Our findings indicate that high levels of tangible support are protective against anxiety symptoms. These findings are consistent with prior studies that have shown that tangible support eases stress among women with breast cancer who are the primary caregivers. A qualitative study showed that the stress of caregiving compounded by the need to care for themselves led to more depression and anxiety symptoms among women with breast cancer.38 Another study observed that tangible support was important for physical and social well‐being and related in particular to the ability to meet family needs.7 Specifically, tangible support can be an important need for Latinas with breast cancer since some report that they do not ask their families for help because they do not want to worry family members about their cancer.14 Latina survivors also report that family members often expect them to continue to meet their household responsibilities at the same level as before their diagnosis or treatments. Therefore, tangible support may reduce the stress caused by caregiver responsibilities and traditional role functions of Latina women.
In a prior mixed methods study among Spanish‐speaking Latina breast cancer survivors, we found feelings of fear of impending death and lack of control and support contribute to their higher levels of anxiety.16 These feelings are often attributed to the lack of information about their condition and treatment in Spanish that they can understand. Our results demonstrate the importance of providing culturally and linguistically appropriate cancer supportive services to prevent future anxiety.
Regarding clinical applications, Hirschman et al. recommend that health‐care providers discuss the gaps in tangible support and help patient's assess role responsibilities as they adapt to their breast cancer.38 However, asking for tangible support with household duties might also negatively affect family relations in traditional Latino households where roles may be more clearly defined along gender lines.23 Family‐based interventions may be indicated for Latinas with breast cancer. Future research on the impact of breast cancer on role functions and related stress among minority groups is necessary.
4.1. Study limitations
A strength of our study was that we were able to collect data from a vulnerable population that is not often studied. One limitation of our study is the relatively small sample size. Also, our sample lived in urban counties within northern California. Latinas living in urban settings may differ from those living in rural communities or outside of the California region in which this study took place. The distributions of the anxiety and depression scores in our sample were skewed toward lower values, suggesting that our results may not generalize to women with more elevated levels, or that the subscales may need further psychometric evaluation in other Latina breast cancer survivor samples. Additionally, since this was a cross‐sectional study using baseline data, we were unable to provide definitive information on cause‐and‐effect relationships.
4.2. Clinical implications
This study makes a novel contribution by identifying a subset of Latina breast cancer survivors who are at higher risk of experiencing symptoms of anxiety, those with lower levels of tangible and affectionate support. These findings support the critical importance of distress screening of Spanish‐speaking Latinas within the first year of survivorship. Such screening should also include a comprehensive assessment of available sources of support and potential needs. Future interventions should focus on reducing intrusive thoughts to potentially reduce psychological distress. Tangible and affectionate support could be possible protective factors that can also be integrated into socio‐behavioral interventions to benefit this vulnerable population. Future studies could aim to increase our understanding of the specific supportive actions performed by the social networks of these breast cancer patients who report high tangible and affectionate support. This added information might help us inform family members and friends on how best to provide effective support. Finally, more studies on the development and testing of culturally and linguistically competent interventions for Spanish‐speaking Latina women with breast cancer and their caregivers, intimate partners, and friends to encourage exchanges of tangible and affectionate support are needed.
CONFLICT OF INTERESTS
The authors declare that they have no conflict of interest.
DISCLAIMER
The contents and views in this manuscript are those of the authors and should not be construed to represent the views of the National Institutes of Health.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
ACKNOWLEDGMENTS
This research was supported by the Division of Intramural Research, National Institute of Minority Health and Health Disparities, California Breast Cancer Research Grants Program Office of the University of California grants 15BB‐1300 and 15BB‐1301, and grant 2P30AG015272‐21 from the National Institute on Aging.
Escalera C, Santoyo‐Olsson J, Stewart AL, Ortiz C, Nápoles AM. Social support as a moderator in the relationship between intrusive thoughts and anxiety among Spanish‐speaking Latinas with breast cancer. Psycho‐Oncology. 2019;28:1819–1828. 10.1002/pon.5154
REFERENCES
- 1. Hewitt M, Herdman R, Holland J. Institute of Medicine (US) Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting In: Adler NE, Page AEK, eds. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: National Academies Press (US); 2008. PubMed PMID: 20669419. [PubMed] [Google Scholar]
- 2. Dupont A, Bower JE, Stanton AL, Ganz PA. Cancer‐related intrusive thoughts predict behavioral symptoms following breast cancer treatment. Health Psychol. 2014;33(2):155‐163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Horowitz MJ. Stress‐response syndromes: a review of posttraumatic and adjustment disorders. Hosp Community Psychiatry. 1986;37(3):241‐249. [DOI] [PubMed] [Google Scholar]
- 4. Matsuoka Y, Nakano T, Inagaki M, et al. Cancer‐related intrusive thoughts as an indicator of poor psychological adjustment at 3 or more years after breast surgery: a preliminary study. Breast Cancer Res Tr. 2002;76(2):117‐124. [DOI] [PubMed] [Google Scholar]
- 5. Golden‐Kreutz DM, Thornton LM, Wells‐Di Gregorio S, et al. Traumatic stress, perceived global stress, and life events: prospectively predicting quality of life in breast cancer patients. Health Psychol. 2005;24(3):288‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nordin K, Berglund C, Glimelius B, Sjoden PO. Predicting anxiety and depression among cancer patients: a clinical model. Eur J Cancer. 2001;37(3):376‐384. [DOI] [PubMed] [Google Scholar]
- 7. Kroenke CH, Kwan ML, Neugut AI, et al. Social networks, social support mechanisms, and quality of life after breast cancer diagnosis. Breast Cancer Res Treat. 2013;139(2):515‐527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hill J, Holcombe C, Clark L, et al. Predictors of onset of depression and anxiety in the year after diagnosis of breast cancer. Psychol Med. 2011;41(7):1429‐1436. [DOI] [PubMed] [Google Scholar]
- 9. Huang CY, Hsu MC. Social support as a moderator between depressive symptoms and quality of life outcomes of breast cancer survivors. Eur J Oncol Nurs. 2013;17(6):767‐774. [DOI] [PubMed] [Google Scholar]
- 10. Cohen S, Wills TA. Stress, Social Support, and the Buffering Hypothesis. Psychol Bull. 1985;98(2):310‐357. [PubMed] [Google Scholar]
- 11. Badger TA, Segrin C, Hepworth JT, Pasvogel A, Weihs K, Lopez AM. Telephone‐delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners. Psycho‐Oncology. 2013;22(5):1035‐1042. [DOI] [PubMed] [Google Scholar]
- 12. Apollo AJ, Crew KD, Campbell J, et al. High rates of psychosocial stress among Hispanic breast cancer survivors. J Clin Oncol. 2007;25(18):9113. [Google Scholar]
- 13. Ashing‐Giwa KT, Padilla G, Tejero J, et al. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho‐Oncology. 2004;13(6):408‐428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ashing‐Giwa KT, Padilla GV, Bohorquez DE, Tejero JS, Garcia M. Understanding the breast cancer experience of Latina women. J Psychosoc Oncol. 2006;24(3):19‐52. [DOI] [PubMed] [Google Scholar]
- 15. Moore RJ, Butow P. Culture and oncology: impact of context effects. New York, NY: Kluwer Academic/Plenum Publishers; 2004. [Google Scholar]
- 16. Napoles‐Springer AM, Ortiz C, O'Brien H, Diaz‐Mendez M. Developing a culturally competent peer support intervention for Spanish‐speaking Latinas with breast cancer. J Immigr Minor Health. 2009;11(4):268‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Puigpinos‐Riera R, Graells‐Sans A, Serral G, et al. Anxiety and depression in women with breast cancer: social and clinical determinants and influence of the social network and social support (DAMA cohort). Cancer Epidemiol. 2018;55:123‐129. [DOI] [PubMed] [Google Scholar]
- 18. Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina and Caucasian breast cancer survivors: a comparative study. Oncol Nurs Forum. 2010;37(1):93‐99. [DOI] [PubMed] [Google Scholar]
- 19. Lester J, Crosthwaite K, Stout R, et al. Women with breast cancer: self‐reported distress in early survivorship. Oncol Nurs Forum. 2015;42(1):E17‐E23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Worni M, Akushevich I, Greenup R, et al. Trends in treatment patterns and outcomes for ductal carcinoma in situ. J Natl Cancer Inst. 2015;107(12):djv263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Napoles‐Springer AM, Livaudais JC, Bloom J, Hwang S, Kaplan CP. Information exchange and decision making in the treatment of Latina and White women with ductal carcinoma in situ. J Psychosoc Oncol. 2007;25(4):19‐36. [DOI] [PubMed] [Google Scholar]
- 22. Napoles AM, Santoyo‐Olsson J, Ortiz C, et al. Randomized controlled trial of Nuevo Amanecer: a peer‐delivered stress management intervention for Spanish‐speaking Latinas with breast cancer. Clinical trials (London, England). 2014;11(2):230‐238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Napoles AM, Ortiz C, Santoyo‐Olsson J, et al. Nuevo Amanecer: results of a randomized controlled trial of a community‐based, peer‐delivered stress management intervention to improve quality of life in Latinas with breast cancer. Am J Public Health. 2015;105(Suppl 3):e55‐e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209‐218. [DOI] [PubMed] [Google Scholar]
- 25. Antoni MH, Wimberly SR, Lechner SC, et al. Reduction of cancer‐specific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiatry. 2006;163(10):1791‐1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705‐714. [DOI] [PubMed] [Google Scholar]
- 27. National Comprehensive Cancer Network . NCCN Clinical Practice Guidelines in Oncology: Distress Management. Version 1.2011 ed. Fort Washington, PA: NCCN; 2010. [Google Scholar]
- 28. Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho‐Oncology. 2001;10(1):19‐28. [DOI] [PubMed] [Google Scholar]
- 29. Zabora J, BrintzenhofeSzoc K, Jacobsen P, et al. A new psychosocial screening instrument for use with cancer patients. Psychosomatics. 2001;42(3):241‐246. [DOI] [PubMed] [Google Scholar]
- 30. Galdon MJ, Dura E, Andreu Y, et al. Psychometric properties of the Brief Symptom Inventory‐18 in a Spanish breast cancer sample. J Psychosom Res. 2008;65(6):533‐539. [DOI] [PubMed] [Google Scholar]
- 31. Vickberg SMJ, Bovbjerg DH, DuHamel KN, Currie V, Redd WH. Intrusive thoughts and psychological distress among breast cancer survivors: global meaning as a possible protective factor. Behav Med. 2000;25(4):152‐160. [DOI] [PubMed] [Google Scholar]
- 32. Cohee AA, Adams RN, Johns SA, et al. Long‐term fear of recurrence in young breast cancer survivors and partners. Psycho‐Oncology. 2017;26(1):22‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lewis JA, Manne SL, DuHamel KN, et al. Social support, intrusive thoughts, and quality of life in breast cancer survivors. J Behav Med. 2001;24(3):231‐245. [DOI] [PubMed] [Google Scholar]
- 34. Derogatis LR. Brief Symptom Inventory (BSI): Administration, Scoring, and Procedures Manual. 3rd ed. Minneapolis, MN: NCS Pearson; 1992. [Google Scholar]
- 35. Varela RE, Weems CF, Berman SL, Hensley L, de Bernal MCR. Internalizing symptoms in Latinos: the role of anxiety sensitivity. J Youth Adolesc. 2007;36(4):429‐440. [Google Scholar]
- 36. Devine D, Parker PA, Fouladi RT, Cohen L. The association between social support, intrusive thoughts, avoidance, and adjustment following an experimental cancer treatment. Psycho‐Oncology. 2003;12(5):453‐462. [DOI] [PubMed] [Google Scholar]
- 37. Lepore SJ, Helgeson VS. Social constraints, intrusive thoughts, and mental health after prostate cancer. J Soc Clin Psychol. 1998;17(1):89‐106. [Google Scholar]
- 38. Hirschman KB, Bourjolly JN. How do tangible supports impact the breast cancer experience? Soc Work Health Care. 2005;41(1):17‐32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


