Abstract
Background
The caries arrest that can be achieved by using silver diamine fluoride (SDF) offers a minimally invasive and inexpensive alternative to traditional restorative caries treatment. The authors evaluated how the dentinal staining that is associated with SDF influences the acceptance of this treatment among parents of young children in the New York City metropolitan area.
Methods
The authors invited the parents of children who had experienced dental caries and who had appointments at the New York University Pediatric Dentistry Clinic and at several private clinics in New Jersey to participate in a Web-based survey designed to assess parents’ demographics, perceptions of photographs of SDF-treated carious teeth, and acceptability of treatment in different behavior management scenarios.
Results
Ninety-eight mothers and 22 fathers from diverse backgrounds participated. Most parents (67.5%) judged SDF staining on the posterior teeth to be esthetically tolerable, but only 29.7% of parents made this same judgment about anterior teeth (P < .001). In the absence of their child having behavioral barriers to conventional restorations, 53.6% of parents reported that they were likely to choose SDF to treat their child’s posterior teeth, but only 26.9% of parents were likely to choose SDF to treat their child’s anterior teeth. As the number of children’s behavioral barriers increased, so did the parents’ level of acceptance. In extreme cases, in which parents had to decide whether their children should undergo general anesthesia during treatment, parents’ acceptance rate of SDF as a treatment method increased to 68.5% on posterior teeth and to 60.3% on anterior teeth. Parents’ acceptance of the treatment also varied according to their socioeconomic status.
Conclusions
Staining on posterior teeth was more acceptable than staining on anterior teeth. Although staining on anterior teeth was undesirable, most parents preferred this option to advanced behavioral techniques such as sedation or general anesthesia.
Practical Implications
Clinicians need to understand parental sensitivities regarding the staining effect of SDF to plan adequately for the use of SDF as a method of caries management in pediatric patients.
Keywords: Caries arrest, silver diamine fluoride, parental perceptions, dental esthetics
Silver diamine fluoride (SDF) is effective for caries arrest and prevention,1 particularly for the treatment of early childhood caries,2–4 a disease that continues to affect certain high-risk populations at a disproportionately high rate.5 The results of systematic reviews of human randomized controlled trials6,7 substantiate that SDF is a minimally invasive therapy that is inexpensive, does not require caries removal, is easy to apply, and poses minimal risk to patients.
The clinical observation that SDF causes dark staining of carious enamel and dentin may be a significant deterrent to its use.8,9 The investigators of some clinical trials10,11 have reported that parental concern about staining is low (less than 7%12), but the investigators who conducted these studies did so in settings where esthetic concerns may be different than those of parents in the United States.13
In a 2016 survey of pediatric dentistry program directors,14 most of those who were surveyed agreed that SDF could be used to arrest caries in primary (87%) and permanent (66%) teeth in patients who were at high risk of experiencing caries. More than 90% of the survey respondents believed that SDF would be useful in treating patients who experience difficulty undergoing conventional restorative treatment (including those who were in a precooperative state, who had behavioral problems, who were medically fragile, and who had logistical challenges). However, the survey respondents expressed concerns regarding staining of teeth and the expected poor parental acceptance of esthetics after treatment. In fact, the most frequently reported perceived barrier to the use of SDF was the concern of parental acceptance (91.8%).14
When it comes to parental acceptance of any new technique or restorative material, esthetics is a prime concern. Investigators who sent a survey to 500 randomly selected active members of the American Academy of Pediatric Dentistry found that the survey respondents’ perceptions of parental concerns about restorative materials were (in decreasing order) esthetics, cost, toxicity, and durability.15 Among the survey respondents, 43% of the pediatric dental providers reported that, when challenged, they followed parental preferences even when the decision was contrary to their clinical judgment,15 and 28% reported that they never used amalgam, owing to the esthetic concerns of parents.15 However, the investigators surveyed only pediatric dentists’ perceptions and did not report the direct opinion of the parents.15
To our knowledge, there are no previously published reports in the literature regarding parental perceptions or the acceptance of SDF on the basis of its benefits or on the side effect of staining. As SDF appears to be a useful tool for caries management, we examined parental perceptions and attitudes toward its staining effects. In this study, we aimed to assess parental perceptions of SDF staining and to determine whether parents’ level of acceptability of SDF would change according to the location of the staining, the child’s behavior, and demographic factors. Understanding parents’ thoughts about SDF staining, the circumstances in which they would find it acceptable or unacceptable, and the factors that may affect their level of acceptance could aid clinicians in developing treatment plans that meet patients’ and parents’ needs and circumstances.
METHODS
The University Committee on Activities Involving Human Subjects at New York University (NYU) (IRB-FY2016–318) determined that this study was exempt from the need for oversight.
We selected our sample from parents who were waiting for their children’s appointments at the NYU Pediatric Dental Clinic located in New York City and at private pediatric dentistry clinics located in New Jersey, within the New York City metropolitan area. Practitioners at the NYU clinic mainly treated patients with Medicaid insurance, whereas practitioners at the 4 private practice sites, located in suburban New Jersey, mainly treated patients with private insurance. We chose these private practices because we recognized that the practitioners in these clinics serve a diverse patient population (educational and socioeconomic). We used a uniform recruiting statement (Box) to invite each parent to participate in our electronic survey (English and Spanish). To be included, parents must have had children who had caries experience, spoke English or Spanish, and agreed to participate in the survey. We provided no compensation for participation. At all of the locations at which we recruited study participants, we followed the same script and systematically sampled all of the parents who were in the waiting area.
BOX. Recruiting statement and silver diamine fluoride description information.
SCRIPT FOR RECRUITING
“We are conducting a study to evaluate parents’ opinions on a new type of treatment that stops cavities from growing. The study is a questionnaire that will take about 10 minutes of your time, and will allow us to get an idea of what parents think of the effects of this new treatment. Your opinion is important because you have children that go to the dentist and knowing what parents expect and find acceptable helps to establish treatments that fit the needs of children and their caregivers. Nobody will be able to identify you or your child by your answers to this survey.”
INFORMATION PROVIDED ABOUT SILVER DIAMINE FLUORIDE WITHIN THE SURVEY
“Cavities are caused by germs that produce acid that breaks down the teeth. We have a new way to treat cavities. We can paint a liquid on the cavity that stops it from getting bigger. However, the liquid changes the color of the cavity, making it darker. The darker color tells us that the treatment is effective. We are going to show you some pictures of cavities before and after the treatment. We would like to know if this treatment is okay with you.”
We conducted an a priori power analysis to evaluate the hypothesis that SDF acceptability varies between a cooperative scenario and any other scenario that presents a barrier to the provision of conventional treatment. We determined that a sample of at least 94 study participants was necessary to detect a difference of at least 0.3 standard deviations (SD) in the mean rating of acceptability when using a Wilcoxon signed rank test, with a 2-tailed, type 1 error rate of 5% and a power of 80%. The preliminary data we collected indicated that the rating scale had a within-cell SD of 1.0, and so a change of 0.3 SDs also implied a rating change of 0.3 units, or a change of 10% to 20% from a cooperative rating that averaged between 2.0 and 3.0.
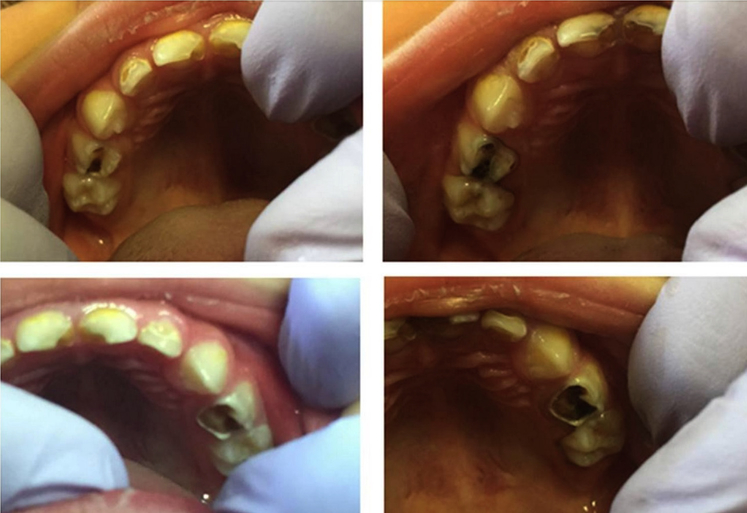
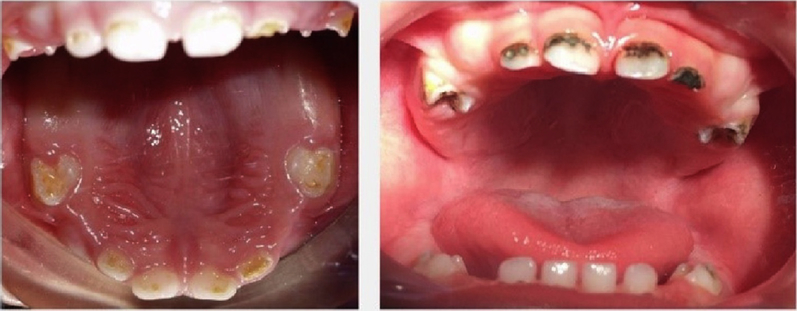
To evaluate esthetics and parents’ acceptance of the esthetics, we presented standard sets of photographs to all of the participants. The photographs showed severe staining in decalcified enamel as well as carious dentin in both anterior and posterior teeth after SDF treatment next to photographs of the same teeth before treatment for comparison. The photographs in eFigures 1 through 3 (available online at the end of this article) show the before-and-after sets of photos that we included in the electronic survey, and the photographs in eFigures 4 and 5 (available online at the end of this article) show the before-and-after sets of photos we printed to accompany the printed surveys. On the basis of parents’ responses to the survey, we evaluated the parents’ opinion of the esthetics of the staining and their acceptance of the SDF staining when they determined that their child would have increasing barriers to receiving conventional restorations. Starting with the parents of children who were cooperative, we explained to the parents that these barriers could include the child crying, screaming, or kicking, and the barriers could progress to the child’s need for conscious sedation or general anesthesia (GA). In all of these scenarios, we asked parents to answer separate questions about anterior and posterior teeth. We included questions to capture demographic data, including the parent’s age, socioeconomic level, educational level, ethnic background, type of insurance, and residence location (urban, suburban, or rural), so that we could evaluate whether any of these variables had an impact on the level of parental acceptance of the staining produced by SDF. We also asked parents about the level of importance they placed on restoring their child’s primary teeth, and we asked them to describe their child’s past behavior when undergoing treatment for caries.
eFigure 1.
Posterior teeth before (left) and after (right) treatment.
eFigure 3.
Anterior and posterior teeth before (left) and after (right) treatment.
eFigure 4.
Anterior teeth before (left) and after (right) treatment.
eFigure 5.
Posterior teeth before (left) and after (right) treatment.
We tested the questionnaire for clarity, ease of completion, and timing, and we modified it according to parental comments. We translated it to Spanish, and a second bilingual pediatric dental care provider reviewed it to ensure the identical intent of each question. Most parents completed the surveys on a tablet computer. We provided printed surveys to parents who were uncomfortable with using a tablet computer, and we immediately recorded their answers electronically. We provided all of the parents with a set of the printed photographs so that they would not have to switch screens to view the photographs while they were answering the questions.
Within the survey itself, we gave minimal information about the “new treatment for cavities.” Our specific intent was to capture only the participant’s opinion of the staining and their acceptance of the treatment only on the basis of their esthetic considerations and their child’s cooperation for treatment (Box). The Appendix (available online at the end of this article) provides the consent form we used for this study.
We used IBM SPSS Statistics (Version 22, IBM) for all of the statistical analysis; we set the level of significance at 5%. Depending on the level of measurement, we used means, SDs, or proportions to describe the demographics of the respondents and their responses to the survey questions. For example, as a function of location, we compared differences in proportions by means of using the McNemar test. We used Pearson product moment correlations to quantify the relationships among demographic indicators. We used a linear mixed model to compare variations among mean acceptance levels—first, as a function of fixed factors of location, treatment barriers, and a random intercept, and second, by means of introducing additional fixed covariates of age, ethnicity, income, and education (each individually)—to evaluate potential moderating influences. Given an omnibus test result of P < .05, we based our post hoc comparison of means and 95% confidence intervals (CIs) on the pooled estimate of the residual error.
RESULTS
As shown in the table, 120 parents completed the survey and provided their demographic information. All of the parents had at least 1 child who had experienced dental caries in the past; therefore, they were familiar with the process of having teeth with caries restored. Ninety percent of parents thought it was “important” or “very important” to “fix baby teeth.” When asked about their child’s behavior, 55% of parents reported that their child had cooperated with restorative treatment, whereas 38% reported that their child had experienced some level of difficulty (child was upset, cried, kicked, or screamed). Seventy-four percent of the parents reported that their children had required advanced techniques to complete dental treatment: 40% reported the use of nitrous oxide, 11% physical restraint, 15% oral sedation, and 8% GA. In addition, 7% reported that their child did not complete treatment owing to a lack of cooperation. Most of the parents whom we approached to participate in the study agreed to do so; however, we experienced a minor recruitment loss among those potential study participants who were called into the treatment area before we could obtain their consent to participate in the study.
TABLE.
Demographic characteristics of parents responding to the survey (N = 120).
| VARIABLE | NO. (%) |
|---|---|
| Sex | |
| Male | 22 (18.3) |
| Female | 98 (81.7) |
| Age* | |
| 20 y or younger | 4 (3.4) |
| 21–30 y | 17 (14.3) |
| 31–40 y | 34 (28.6) |
| 41–50 y | 52 (43.7) |
| 51 y or older | 12 (10.1) |
| Ethnicity† | |
| White | 51 (42.5) |
| Hispanic | 44 (36.7) |
| Black | 14 (11.7) |
| Asian | 12 (10.0) |
| Native American | 1 (0.8) |
| Prefer not to answer | 4 (3.3) |
| Level of Education‡ | |
| Finished elementary school | 3 (2.5) |
| Finished middle school | 13 (10.9) |
| Graduated high school | 14 (11.8) |
| Some college | 18 (15.1) |
| Graduated college | 42 (35.3) |
| Some graduate school | 7 (5.9) |
| Completed graduate school | 22 (18.5) |
| Household Income§ | |
| $0-$19,999 | 16 (15.2) |
| $20,000-$39,999 | 12 (11.4) |
| $40,000-$64,999 | 22 (21.0) |
| $65,000-$103,999 | 14 (13.3) |
| $104,000-$ 199,999 | 19 (18.1) |
| $200,000 or more | 22 (21.0) |
| Type of Insurance | |
| Private insurance | 58 (48.3) |
| Government-funded insurance | 51 (42.5) |
| No insurance | 6 (5.0) |
| Other | 5 (4.2) |
| Number of Children in the Family | |
| 1 | 20 (16.7) |
| 2 | 48 (40.0) |
| 3 | 38 (31.7) |
| 4 or more | 14 (11.7) |
One participant did not respond.
Six participants marked more than 1 selection.
One participant did not respond.
Fifteen participants did not respond.
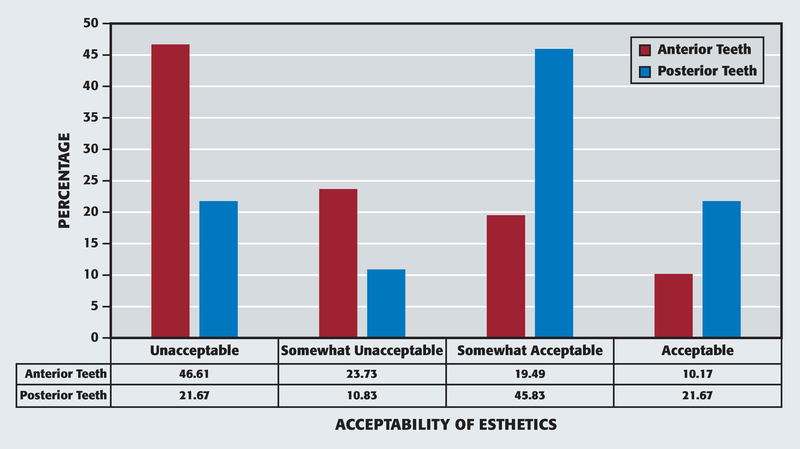
First, we queried parents about their opinion of the esthetics only, and then we asked them about the likelihood that they would accept the treatment, considering their child’s behavior. When we asked their opinion about the staining shown in the photographs, we found that 67.5% (95% CI, 58.7 to 75.2) of parents judged staining on the posterior teeth to be esthetically “acceptable” or “somewhat acceptable.” In contrast, only 29.7% (95% CI, 22.2 to 38.4; P < .001) of parents reported that staining on the anterior teeth met these criteria (Figure 1). Consistent with these opinions regarding esthetics 53.6% of parents reported they were “somewhat likely” or “very likely” to choose SDF to treat posterior teeth, but only 26.9% would choose SDF to treat anterior teeth, in the absence of behavioral barriers to conventional restoration. The level of acceptance for SDF treatment varied depending on the tooth’s location and the child’s barriers to receiving conventional restoration. In extreme cases, in which treatment would require the child to undergo GA, parents’ level of acceptance of staining increased to 68.5% (95% CI, 59.6 to 76.0; P < .001) on posterior teeth and to 60.3% (95% CI, 51.2 to 68.5; P < .001) on anterior teeth. Nevertheless, approximately one-third of the parents found the treatment unacceptable under any circumstance: 31.5% for posterior teeth and 39.6% for anterior teeth.
Figure 1.
Percentage of acceptability on the basis of staining only.
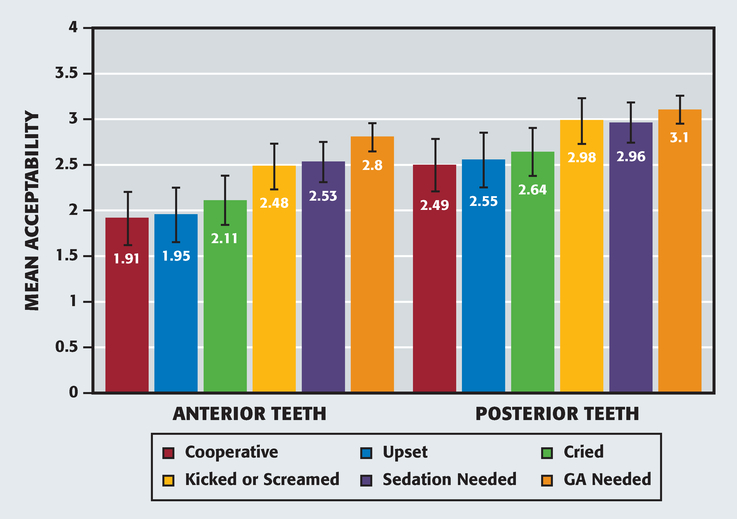
In a more detailed analysis of SDF acceptability, we compared the mean parental ratings of treatment acceptability as a function of the tooth’s location (anterior versus posterior) with the increasing difficulty of receiving conventional treatment (Figure 2). Levels of acceptability averaged 2.0 rating scale units for anterior teeth and 2.5 rating scale units for posterior teeth (range was from 1 to 4 rating scale units, with 1 being “unacceptable” and 4 being “acceptable”) in situations for which the child had no barriers to receiving conventional treatment (that is, parents indicated ratings between “somewhat unacceptable” and “somewhat acceptable”). Moreover, parents’ level of acceptance increased according to the level of increased difficulty that their child would experience in order to receive treatment—in particular, at the point at which the child was no longer able to sit still and would require sedation. In extreme cases, in which the child would need to undergo GA to receive treatment, parental ratings averaged approximately 2.8 rating scale units for the anterior teeth and 3.1 rating scale units for the posterior teeth; both ratings were in the range of “somewhat acceptable.” Our analysis of the results confirmed these observations, showing the effects of both tooth location (P < .001) and difficulty with receiving treatment (P < .001). In terms of tooth location, we found that parental acceptance was significantly lower for anterior teeth (mean, 2.3; 95% CI, 2.1 to 2.4) than for posterior teeth (mean, 2.7; 95% CI, 2.5 to 2.9). In terms of difficulty with receiving treatment, we found that parental acceptance varied in 2 significantly different tiers: in a group who reported lower acceptability for children in a scenario of being cooperative, upset, or crying (mean, 2.2; 95% CI, 2.0 to 2.4; mean, 2.2; 95% CI, 2.1 to 2.4; and mean, 2.3; 95% CI, 2.1, 2.5; respectively), and in a group who reported higher acceptability in a scenario in which the child would kick and scream or would require sedation or GA (mean, 2.7; 95% CI, 2.5 to 2.9; mean, 2.6; 95% CI, 2.5 to 2.8; and mean, 2.8; 95% CI, 2.7 to 3.0; respectively). Our analysis of the results failed to show interaction (P = .11); we believe this outcome suggests that a posterior tooth location added a similar increment to parental acceptability at each level of difficulty with receiving treatment. Thus, parental acceptance of SDF staining was not uniform; acceptance increased for teeth in less visible locations and as the level of difficulty the child would experience in order to conventional treatment increased.
Figure 2.
Acceptance according to behavior for treatment. In the rating scale, a score of 1 indicated “unacceptable” and 4 indicated “acceptable.” Error bars indicated 95% confidence intervals. GA: General anesthesia.
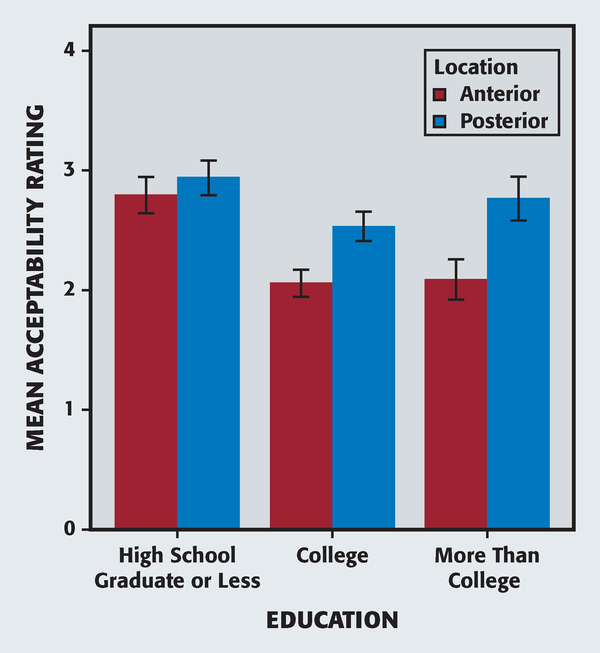
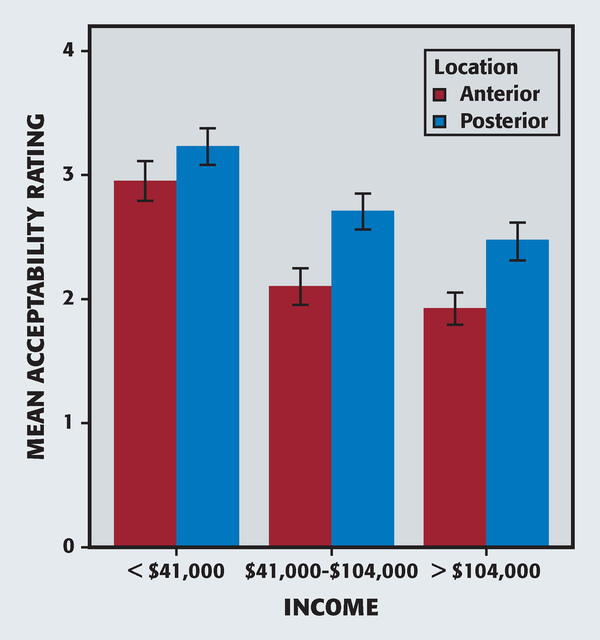
In our additional analyses, we added parental age, income, education, and ethnicity—each as a third co-variate—to determine the potential moderating effects on parental acceptance ratings. Each covariate interacted with location (from P = .03 to P < .001), such that acceptance of staining on the anterior teeth increased toward the level already reported on the posterior teeth among parents who were younger, had lower income, were less educated, or who reported Hispanic ethnicity. In Figure 3 one can see the generally higher levels of parental acceptance and the lower level of difference between anterior and posterior tooth location among those with less than a college education. Our analysis supported these observations; we noted that parents in the group with the lowest level of education had higher mean ratings of acceptability, and less differences between anterior and posterior teeth, than parents in either of the groups that had higher levels of education (P < .05), as well as with the increasing acceptability regarding anterior teeth and posterior teeth in the 2 groups with higher levels of the higher education groups (P < .05), but not in the group with the lowest level of education. Similar trends were evident for the groups defined by lower income (Figure 4), as well as the groups defined by younger age or Hispanic ethnicity.
Figure 3.
Acceptance of treatment according to level of education. In the rating scale, a score of 1 indicated “unacceptable” and 4 indicated “acceptable.” Error bars indicated 95% confidence intervals.
Figure 4.
Acceptance of treatment according to level of income. In the rating scale, a score of 1 indicated “unacceptable” and 4 indicated “acceptable.” Error bars indicated 95% confidence intervals.
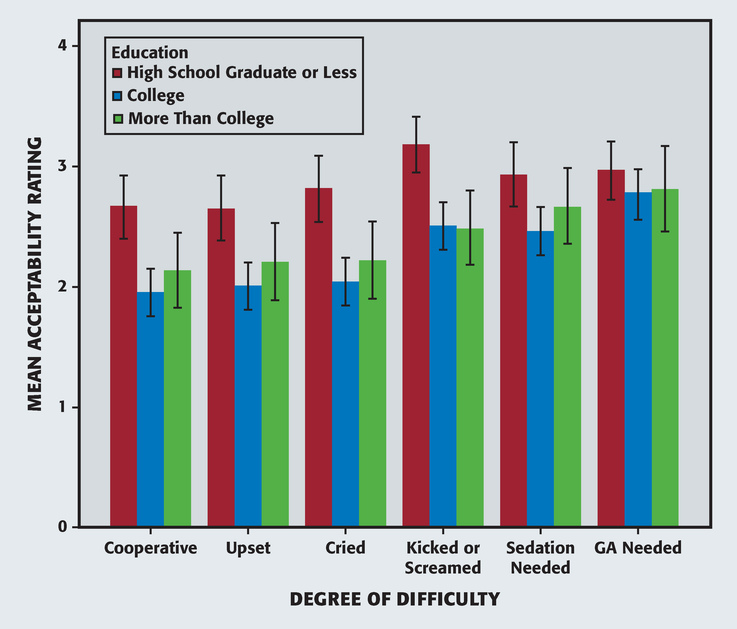
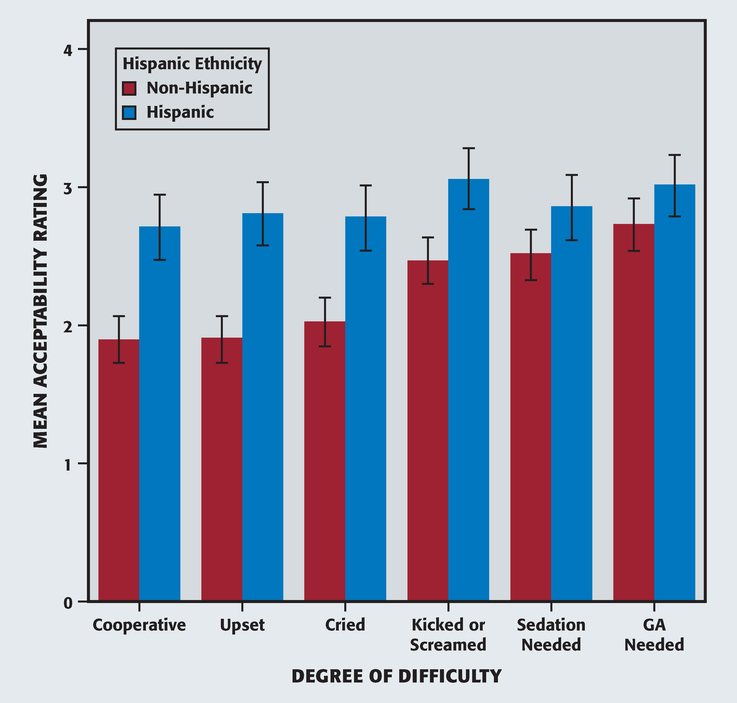
In our analysis of the results, we also found that the effect of the level of difficulty that the child had to receiving treatment on parental acceptance of SDF treatment varied according to the parent’s level of education (P = .008) and Hispanic ethnicity (P < .001). Figure 5 shows the effects of education on acceptance of treatment; it was evident that parents had a higher acceptance of staining, even for children who were not difficult, if they had a lower level of education and that the level of acceptance by these parents did not vary much as the level of difficulty related to receiving treatment increased. In contrast, the level of acceptance increased with difficulty related to receiving treatment among those parents who had more education, and we noticed that education-related differences in acceptability disappeared when parents had to consider their child’s need for GA (all, P > .05), and to a lesser extent, oral sedation (high school versus college, P < .05; but high school versus more than a college education, P > .05). We noted a similar trend when we substituted Hispanic ethnicity in the analysis (Figure 6). In contrast with the effects of tooth location, a parent’s income and age did not interact with the level of difficulty that the child had to receiving treatment to affect the parent’s acceptance of SDF treatment (P = .26 and P = .18, respectively). In addition, we did not find an indication that acceptability varied with the 3-way interaction of education, location, and treatment difficulty (P = .998). Taken together, these data suggest that the effects of location and treatment difficulty on SDF acceptance each can be moderated by means of considering socioeconomic factors.
Figure 5.
Effects of education on treatment acceptance. In the rating scale, a score of 1 indicated “unacceptable” and 4 indicated “acceptable.” Error bars indicated 95% confidence intervals. GA: General anesthesia.
Figure 6.
Effects of ethnicity on treatment acceptance. In the rating scale, a score of 1 indicated “unacceptable” and 4 indicated “acceptable.” Error bars indicated 95% confidence intervals. GA: General anesthesia.
Our analysis also showed that these indicators were correlated in the sample. Thus, age increased with education (r = 0.29) and income (r = 0.40) and decreased in people with Hispanic ethnicity (r = −0.32). Education increased with income (r = 0.56) and decreased with Hispanic ethnicity (r = −0.58), and income decreased in people with Hispanic ethnicity (r = −0.61). Thus, parents with lower levels of education also tended to be younger, had lower income than their counterparts in this study, and had Hispanic ethnicity. When we viewed the results differently, we found that the results of a principal components analysis indicated that these 4 variables yielded only 1 component with an eigenvalue greater than 1, which indicates that only a single concept is needed to explain this pattern of correlations. Because these characteristics tended to be confounded, one cannot isolate the greater acceptance of SDF to the effect of lower income, less education, younger age, or Hispanic ethnicity.
DISCUSSION
To our knowledge, our study is the first to focus on parents’ acceptance of SDF staining and how that acceptance level varies according to their child’s behavioral challenges related to receiving conventional treatment. We recruited a diverse sample of 120 parents of children who were at high risk of experiencing dental caries at a pediatric dental university clinic and several private pediatric practices in the New York City metropolitan area. Our results supported the following 4 major findings: acceptance of SDF staining was greater for posterior teeth than for anterior teeth, acceptance level increased as the child required more advanced methods of behavior guidance, these effects of location and cooperation varied with the parent’s socioeconomic status, and only approximately one-third of the parents found SDF to be unacceptable under any circumstance.
The level of parental acceptance of staining was higher for posterior teeth than for anterior teeth under all circumstances, perhaps because parents understood that the staining would be much less visible in posterior segments; nevertheless, 30% of parents found staining of anterior teeth to be somewhat acceptable or acceptable from the start. Dentists assume that parents will demand the best esthetic appearance for their children,15 and the results of many studies support that assumption, with investigators reporting that parents prefer tooth-colored restorations over amalgams and silver metal crowns16 and zirconia esthetic crowns over other anterior resto-rations.17,18 However, all of these restorations require the use of local anesthetics to conduct tooth reduction in addition to caries removal, for which patient cooperation is imperative.
It is an important finding that many parents who found staining to be unacceptable would approve of the treatment when deciding how to address their children’s behavioral problems or to defer or avoid the possibility of their children having to undergo sedation or GA. The investigators of a study published in 2016 found that, in the past several decades, the hierarchy of parental acceptance of advanced behavior guidance techniques has changed, with decreasing approval of the physical management of behavior and increasing approval of pharmacologic management such as oral sedation and GA.19 However, it is evident from the parents’ responses in our study that many parents prefer a more conservative approach if it is available to them, even at the expense of compromising esthetics. This result seemed to be more evident in parents who were more educated and older and who were aware of the additional risks that oral sedation and GA could present to the patient. An additional finding in the acceptance ratings with increasing behavioral compromise was that parents with less than a college-level education seemed to find their child’s behavior of kicking and screaming as undesirable as the need to have the child sedated during treatment.
In our analysis, we found that the effect of the child’s difficulty with receiving treatment on the parent’s acceptability of SDF varied depending on the parent’s level of education and whether the parent had Hispanic ethnicity. Acceptance of staining, even for patients who would have no difficulty with receiving treatment, was greater among parents who had less education, and the level of acceptance among these parents did not vary as the difficulty with receiving treatment increased. In contrast, acceptance increased with difficulty receiving treatment among those parents who had more education, and education-related differences in acceptability disappeared when parents had to consider the need for their child to undergo GA and, to a lesser extent, oral sedation. We found that education and ethnicity effects were confounded in those analyses, as were age and income effects in other analyses of SDF acceptance as a function anterior or posterior location. A parsimonious interpretation of these data is that a parent’s lower level of socioeconomic status was associated with a generally greater acceptance of SDF staining in anterior locations as well as in less difficult treatment scenarios.
Of utmost importance is the finding that, on the basis of only esthetics, some parents found the treatment to be unacceptable under any circumstance (31.5% for posterior teeth and 39.6% for anterior teeth). For this reason, we strongly recommend that clinicians use a thorough consent form, preferably including photographs that show realistic staining, when discussing treatment with parents of pediatric patients. This is especially important when treating anterior teeth.
In this study, we successfully sampled a diverse group of parents in terms of income, education, ethnicity, and types of insurance (Table). We did not standardize the time of the sampling because we did not include any behavioral or specific treatment intervention for which the time of the day or the year could have had an impact on the participants’ responses. By design, however, we did not mean for the sampling frame to be representative. First, we limited the sample to the New York City metropolitan area, and we will need to do additional work to extend these findings nationally. Second, we designed the sample to “oversample” a population of parents of children who are at high risk of experiencing caries and who would be seeking treatment in a pediatric specialty practice. Indeed, the sample contained a high proportion of parents (74%) whose children already had been exposed to some form of advanced behavioral method to complete dental treatment. Opinions may differ in parents whose children have had less severe effects from previous dental treatment. Third, in our sample, the percentage of parents who identified themselves as having Hispanic ethnicity was larger than that of the general population (36.7%, compared with 17.0%, respectively). This result may be related to sampling patients in the New York City metropolitan area; however, the result also reflects the higher rates and earlier onset of caries in Hispanic minority populations, which investigators have reported nationally,5,20 and who are more likely to require care at specialty clinics. Fourth, 81.7% of respondents were women (mothers) and 18.3% were men (fathers). This discrepancy may preclude insight into the differences among the esthetic perceptions of male and female parents, but it is representative of the reality that the parent who usually takes the child to dental appointments is, most likely, to be the parent who ultimately makes the decisions about the treatment to be provided. Thus, this sample represents that segment of the treatment-seeking population who have a high risk of experiencing caries in the United States and who are likely to derive a major benefit from SDF treatment. Insights about the perception and acceptance of SDF therapy from this group of parents whose children were at high risk of experiencing caries should be among the most salient when considering this innovative approach to caries management.
When we designed this study, we wanted to remove all of the other variables that could influence parental acceptance of the treatment to focus on the perceptions of the esthetics exclusively and to study acceptance of the treatment in light of the child’s cooperation for treatment. In clinical situations, many more variables, including cost, safety, parents’ preconceptions of fluoride products, parents’ desire to have their child receive more permanent treatment, and options for more esthetic restorations as their child’s cooperation improves, may come into play.
CONCLUSIONS
Staining on posterior teeth is more acceptable to parents than staining on anterior teeth. Although most parents may perceive the staining from SDF in anterior teeth as being esthetically unacceptable, many of them will accept the treatment to avoid having their children undergo GA. The results of this study suggest that many parents are open to compromise esthetics in favor of a using a less invasive approach in cases in which the child’s cooperation is a barrier for traditional treatment. To identify parents who find the treatment unacceptable under any circumstance, clinicians should provide informed consent forms that include photographs of the staining, especially when treating anterior teeth. ■
Supplementary Material
eFigure 2.
Anterior teeth before (left) and after (right) treatment.
Acknowledgments
This study was funded, in part, by grant U24 006964 from the National Institute on Minority Health and Health Disparities, National Institutes of Health, and by New York University Clinical and Translational Science Award grant iULiTR001445 from the National Center for Advancing Translational Science, National Institutes of Health.
The authors thank Edda Higuita, CDA, RDA, for her help as a research assistant and William Lieberman, DDS, Max Sulla, DDS, and Mary Flanagan, DDS, for allowing the data collection to be conducted at their practices.
ABBREVIATION KEY
- GA
General anesthesia
- NYU
New York University
- SDF
Silver diamine fluoride
Footnotes
Disclosure. None of the authors reported any disclosures.
SUPPLEMENTAL DATA
Supplemental data related to this article can be found at: http://dx.doi.org/10.1016/j.adaj.2017.03.013.
This article has an accompanying online continuing education activity available at: http://jada.ada.org/ce/home.
Contributor Information
Yasmi O. Crystal, clinical associate professor, Department of Pediatric Dentistry, New York University College of Dentistry, New York, NY..
Malvin N. Janal, senior research scientist, Department of Epidemiology and Health Promotion, New York University College of Dentistry, New York, NY..
Dylan S. Hamilton, pediatric dentistry resident, New York University College of Dentistry, New York, NY..
Richard Niederman, professor and the chair, Department of Epidemiology and Health Promotion, New York University College of Dentistry, New York, NY..
References
- 1.Chu CH, Lo EC. Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev Dent. 2008;6(4):315–321. [PubMed] [Google Scholar]
- 2.Niederman R, Feres M, Ogunbodede E. Dentistry In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, eds. Essential Surgery. Washington, DC: World Bank; 2015:173–195. Disease Control Priorities; vol. 1, 3rd ed. [Google Scholar]
- 3.Sharma G, Puranik MP, K RS. Approaches to arresting dental caries: an update. J Clin Diagn Res. 2015;9(5):ZEo8–ZE11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mei ML, Lo EC, Chu CH. Clinical use of silver diamine fluoride in dental treatment. Compend Contin Educ Dent. 2016;37(2):93–98. [PubMed] [Google Scholar]
- 5.Dye BA, Vargas CM, Fryar CD, Ramos-Gomez F, Isman R. Oral health status of children in Los Angeles County and in the United States, 1999–2004. Community Dent Oral Epidemiol. 2017;45(2):135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao SS, Zhao IS, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Trans Res. 2016;1(3):201–210. [DOI] [PubMed] [Google Scholar]
- 7.Rosenblatt A, Stamford TC, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet”. J Dent Res. 2009;88(2):116–125. [DOI] [PubMed] [Google Scholar]
- 8.Llodra JC, Rodriguez A, Ferrer B, Menardia V, Ramos T, Morato M. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 2005;84(8):721–724. [DOI] [PubMed] [Google Scholar]
- 9.Peng JJ, Botelho MG, Matinlinna JP. Silver compounds used in dentistry for caries management: a review. J Dent. 2012;40(7):531–541. [DOI] [PubMed] [Google Scholar]
- 10.Yee R, Holmgren C, Mulder J, Lama D, Walker D, van Palenstein Helderman W. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res. 2009;88(7):644–647. [DOI] [PubMed] [Google Scholar]
- 11.Zhi QH, Lo EC, Lin HC. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 2012;40(11):962–967. [DOI] [PubMed] [Google Scholar]
- 12.Chu CH, Lo EC, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81(11):767–770. [DOI] [PubMed] [Google Scholar]
- 13.Crystal YO, Niederman R. Silver diamine fluoride treatment considerations in children’s caries management. Pediatr Dent. 2016;38(7): 466–471. [PMC free article] [PubMed] [Google Scholar]
- 14.Nelson T, Scott JM, Crystal YO, Berg JH, Milgrom P. Silver diamine fluoride in pediatric dentistry training programs: survey of graduate program directors. Pediatr Dent. 2016;38(3):212–217. [PubMed] [Google Scholar]
- 15.Zimmerman JA, Feigal RJ, Till MJ, Hodges JS. Parental attitudes on restorative materials as factors influencing current use in pediatric dentistry. Pediatr Dent. 2009;31(1):63–70. [PubMed] [Google Scholar]
- 16.Holan G, Rahme MA, Ram D. Parents’ attitude toward their children’s appearance in the case of esthetic defects of the anterior primary teeth. J Clin Pediatr Dent. 2009;34(2):141–145. [DOI] [PubMed] [Google Scholar]
- 17.Pani SC, Saffan AA, AlHobail S, Bin Salem F, AlFuraih A, AlTamimi M. Esthetic concerns and acceptability of treatment modalities in primary teeth: a comparison between children and their parents. Int J Dent. 2016;2016:3163904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holsinger DM, Wells MH, Scarbecz M, Donaldson M. Clinical evaluation and parental satisfaction with pediatric zirconia anterior crowns. Pediatr Dent. 2016;38(3):192–197. [PubMed] [Google Scholar]
- 19.Patel M, McTigue DJ, Thikkurissy S, Fields HW. Parental attitudes toward advanced behavior guidance techniques used in pediatric dentistry. Pediatr Dent. 2016;38(1):30–36. [PubMed] [Google Scholar]
- 20.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat. 2007;(248):1–92. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.